Abstract
In the absence of an iron chelating agent, patients with beta-thalassemia on regular transfusions present complications of transfusion-related iron overload. Without iron chelation therapy, heart disease is the major cause of death; however, hepatic and endocrine complications also occur. Currently there are three iron chelating agents available for continuous use in patients with thalassemia on regular transfusions (desferrioxamine, deferiprone, and deferasirox) providing good results in reducing cardiac, hepatic and endocrine toxicity. These practice guidelines, prepared by the Scientific Committee of Associação Brasileira de Thalassemia (ABRASTA), presents a review of the literature regarding iron overload assessment (by imaging and laboratory exams) and the role of T2* magnetic resonance imaging (MRI) to control iron overload and iron chelation therapy, with evidence-based recommendations for each clinical situation. Based on this review, the authors propose an iron chelation protocol for patients with thalassemia under regular transfusions.
Keywords: Blood transfusion, Chelation therapy, Deferiprone, Deferasirox, Iron/metabolism, beta-Thalassemia, Iron overload, Iron chelating agents, Magnetic resonance imaging, Practice guidelines as topic, Protocols, Brazil
Introduction
Transfusion-dependent patients with thalassemia major(TM) develop iron overload which leads to damage of the liver, heart, and endocrine organs and related morbidity and mortality(1,2). Improvements in survival have been achieved over the last 40 years due to iron chelation therapy and iron assessment by serum ferritin, and liver/cardiac magnetic resonance imaging (MRI) techniques(3).
The need to have an iron chelation protocol in Brazil to guide the treatment led to the development of this guideline.
Iron chelation therapy
Iron chelation therapy with desferrioxamine (DFO), available since the late 1960s and the most widely used iron chelator, decreased iron overload-related complications and mortality rate of patients with TM(4-6). However, the long-term survival rate remained low and 50% of patients did not reach 35 years of age(7). Although available in many countries, one third of the patients developed signs of iron overload, such as delayed or absent puberty, growth disorders, hypothyroidism, hypogonadism, bone abnormalities, cirrhosis and heart disease (main cause of death in transfusion dependent patients with TM). These complications are related to a poor compliance to treatment, due to the subcutaneous administration (SC) of DFO over at least 12 hours, 5-6 days per week(1,2). However, some patients with good compliance to DFO still develop these problems(2,8).
Deferiprone (DFP), an oral iron chelator, has been available for use in Europe and other countries since 1999. Several studies showed that DFP (75 mg/kg/day)leads to a negative iron balance in patients with TM and reduces the iron measured by ferritin level or liver iron concentration (LIC)(9,10).
Higher doses of DFP (100 mg/kg/day) or combination therapy with DFO make the treatment more effective in reducing iron overload(10-18). DFP plays an important role in protecting the heart(14,16,18,19). In an eight-year follow up, no cardiac event was found in patients with TM receiving DFP, while ten deaths were recorded related to heart failure in patients treated with DFO(20). A randomized controlled trial in patients with cardiac T2* MRI values from 8-20 ms and normal cardiac function showed that DFP monotherapy was superior to DFO in improving the cardiac T2* MRI and cardiac function(21). DFP combined with SC DFO led to lower serum ferritin levels, suggesting an additive or synergic effect between the two chelators(11-18). Combination therapy can slowly improve the cardiac dysfunction in patients with severe iron overload and asymptomatic or symptomatic heart disease(22,23). Continuous intravenous DFO is slower than combined therapy in reducing cardiac iron and the adverse events related to the catheter device make such therapy difficult. However, continuous DFO can be used when DFP is contraindicated(24,25).
Deferasirox (DFX), an oral iron chelator, is approved worldwide for over two-year-old patients with the advantage of being administered once a day because its plasma half-life is 11-19 hours, thus it offers 24-hour protection against labile plasma iron and reduces tissue injuries(25). A phase III prospective randomized clinical trial, comparing DFO and DFX, brought new alternatives to the treatment of patients with transfusion related iron overload. DFX (20-30 mg/kg/day) proved to be as effective as DFO (40-50 mg/kg/day) in inducing a negative iron balance as measured by ferritin level and LIC(26). DFX safety and efficacy were confirmed over time(27,28). DFX can remove cardiac iron(29-32). The Evaluation of Patients' Iron Chelation with Exjade (EPIC) trial(30-32) demonstrated, in a prospective, multicenter trial with 192 patients randomized in two arms, that DFX can prevent or remove cardiac iron. The improvement in myocardial T2* MRI in patients with cardiac iron overload was associated with maintained left ventricular ejection fraction (LVEF), while in patients without cardiac iron overload (prevention arm), LVEF improved significantly. The DFX optimal dose for cardiac iron chelation is 30-40 mg/kg/day.
Patients with TM can have iron overload in the liver and not in the heart(33). Younger patients usually have detectable cardiac iron overload after the age of 9.5 years(34,35). However, patients with suboptimal chelation therapy can develop cardiac iron overload earlier, suggesting a need for MRI screening at 7 years of age if poor chelation is assumed, even in the absence of heart disease symptoms(36). An individual assessment of iron overload is important for the appropriate chelation therapy(33). The chelation therapy must reduce the free iron and, as a consequence, reduce cellular damage.
Iron overload assessment
1. Serum ferritin and transferrin saturation
Serum ferritin is an indirect measure of body iron and is useful to monitor iron chelation over time. Ferritin is also an acute-phase serum protein, so it can be naturally high during acute or chronic inflammation and infections; or decreased in ascorbate deficiency(37). There is a correlation between serum ferritin and LIC(38). Ferritin levels ≤ 2.500 ng/mL are significantly correlated to higher cardiac disease-free survival rates(1,5,6). Some patients may develop cardiac iron overload even with low serum ferritin because there is lack of a clinically useful correlation between serum ferritin and cardiac iron overload measured by MRI in patients with TM on regular transfusions(8), justifying the need to monitor iron overload with both tests.
Frequent blood transfusions cause a gradual increase in transferrin saturation, which leads to the presence of non-transferrin-bound iron (NTBI) in the plasma(39). The toxic component is called labile plasma iron (LPI) and is prevalent when transferrin saturation is > 70%.
2. Liver iron concentration
Liver iron can predict a clinical outcome, as patients with less LIC survive longer(4) and have more cardiac disease-free survival(5). LIC can be measured by biopsy, superconducting quantum interference device (SQUID) and MRI (R2/R2*). As MRI R2/R2* is a non-invasive procedure compared to liver biopsy and shows good correlation with liver iron, this exam should be used to measure LIC(40). If LIC is severe, the MRI should be repeated in 6 months.
3. Myocardial iron concentration
Cardiac function must be assessed by echocardiogram(41). Decreased LVEF or increased end-systolic volume are related to potential cardiac iron overload, increasing the risk of developing heart disease(42). These changes must be detected early because they are associated with a high mortality rate(1,22). Cardiac MRI, using the relaxation time T2* measured in the heart interventricular septum, is a technique that is reproducible and accurate(33,43,44) and has improved the knowledge on cardiac disease in transfusion-dependent patients(3,33-36). Low myocardial T2* predicts a high risk of developing heart failure and arrhythmia. Heart failure occurred in 47% of patients within one year of a cardiac T2* values < 6 ms with a relative risk of 270 (95% confidence interval: 64-1129). All patients with reduced LVEF had cardiac iron overload and only 0.2% of them developed heart failure with T2* values > 10 ms(3).
4. Iron assessment
Proper management requires access to cardiac MRI. If the first MRI shows a T2* > 20 ms, the exam should be repeated in one year. If T2* < 20 ms, the MRI should be performed annually or more frequently according to chelation therapy and the severity of cardiac iron overload. By using T2* MRI, it is possible, in the same procedure, to determine the degree of iron overload of different organs besides the heart, such as the liver, pituitary gland and pancreas as well as gain information on cardiac volumes and function. LIC(45) and myocardial iron concentration (MIC)(46) values are calculated according to previously published data that correlate MRI values to directly measured iron by biopsy (Table 1):
Table 1.
Correlation between iron overload detected by magnetic resonance imaging (ms) and tissue (mg Fe/g dry weight)
| Liver(45) | Normal | Mild | Moderate | Severe |
| T2* (ms) | > 11.4 | 3.8 - 11.4 | 1.8-3.8 | < 1.8 |
| R2* (Hz) | < 88 | 88-263 | 263-555 | > 555 |
| LIC (mg Fe/g dry wet) | < 2 | 2-7 | 7-15 | > 15 |
| Cardiac(46) | Normal | Mild | Moderate | Severe |
| T2* (ms) | > 20 | 15-20 | 10-15 | < 10 |
| R2* (Hz) | < 50 | 50-66.5 | 66.6-100 | > 100 |
| MIC (mg Fe/g dry wet) | < 1.16 | 1.16 - 1.65 | 1.65 - 2.71 | > 2.71 |
LIC: liver iron concentration; MIC: myocardial iron concentration
Iron chelators: characteristics
The characteristics of iron chelators are listed in Table 2. The dose must be reduced if ferritin levels are consistently < 500 ng/mL(47,48) unless there is evidence or iron overload by T2* MRI. Anticontraceptive methods should be used by fertile age female patients.
Table 2.
Main characteristics of iron chelators
| Desferrioxamine(41) | Deferiprone(9,10,12,16,17,49,50) | Deferasirox(26,28,31,32) | |
| Indications | Thalassemia major or intermedia on regular blood transfusions (> 10 transfusions) Ferritin levels > 1000 ng/mL | ||
| Age | All | > 6 years | > 2 years |
| Adverse events | Skin - local reactions; | Skin rash; Gastrointestinal disturbances; Mild non-progressive increases in serum creatinine; Increased liver enzymes | |
| Hearing loss to high frequencies; | Neutropenia; | ||
| Visual disturbances; | Agranulocytosis (0.6/100 patients/year); | ||
| Allergy; | Thrombocytopenia; | ||
| Growth failure; | Gastrointestinal disturbances; | ||
| Osteoporosis; | Increased liver enzymes; | ||
| Yersinia and Klebsiella infections; Pneumonitis or renal failure due to high doses or fast infusion rates (rare) | Arthropathy | ||
| Monitoring | |||
| Weekly | Neutrophil count | ||
| Monthly | Ferritin Transaminases Serum creatinine Proteinuria | ||
| Every 3 months | Ferritin | Ferritin and transaminases (monthly in the first three months); Clinical signs of zinc deficiency | |
| Transaminases | |||
| Every 6 months | Height and sitting height (Harpender Stadiometer) | ||
| Audiometric and ophthalmologic exams; Bone densitometry (begin at 10 years); | |||
| Annually | X-ray of long bones and spine | Audiometric and ophthalmologic exams; Growth in children | |
| Contraindications | |||
| Discontinue therapy before pregnancy and resume after delivery; | Previous neutropenia and/or agranulocytosis (excluding hypersplenism); | Pregnancy or breast-feeding | |
| If the woman presents severe iron overload or cardiac failure, therapy can be resumed in the third trimester of pregnancy; | Concomitant medication that causes neutropenia or agranulocytosis; | ||
| Allergy; Bone lesions that may impair growth | Pregnancy or breast-feeding | ||
DFO dose must be adjusted according to ferritin levels when started in under three-year-old children; it is important to use reduced doses and monitor bone growth. Yersinia and Klebsiella infections can be fatal if not recognized and treated early. DFO should be discontinued in the presence of fever, until there is no more risk of infection by these agents(41). Good compliance to DFO is considered when > 250 infusions/year are administered (five infusions/week)(6) and/or the compliance index is > 0.60(41).
DFP can be started when the absolute neutrophil count (ANC) > 1500/mm3 and platelets > 100,000/mm3; it must be temporary discontinued when ANC is 500-1500/mm3 and resumed when ANC is > 1500/mm3. An adverse event such as ANC < 500/mm3 is a contraindication for the use of DFP. Patients with repeatedly low ANC should be investigated for infections such as human erythrovirus (parvovirus) B19, cytomegalovirus CMV) or Epstein- Barr virus (EBV). If agranulocytosis persists for more than 72 hours or is associated with severe infection, granulocyte stimulating factor may be required(17,49). Early treatment of infections is recommended. In splenectomized patients, the ANC is calculated considering the white cell count minus erythroblasts, and counting only neutrophils(10,16,25,50). When necessary, replace zinc sulfate 200 mg two times per week(16).
DFX dose adjustment is done every three months based on ferritin. If serum creatinine has a non-progressive increase > 33% over baseline value for adult patients or above the maximum value for the age for pediatric patients in two consecutive measurements and cannot be attributed to other causes, the dose must be reduced to 10 mg/kg/day. If there is a progressive increase in serum creatinine beyond the upper limit of the normal range, DFX should be discontinued. Therapy may be resumed according to individual circumstances. Intermittent proteinuria does not need discontinuation, but monthly control is recommended. Abdominal pain, nausea, vomiting or diarrhea can be controlled taking deferasirox in the evening. For mild-to-moderate skin rash, deferasirox may be continued without dose adjustment. For severe rash, where interruption of treatment may be necessary, deferasirox can be resumed after resolution of the rash at a lower dose followed by gradual dose escalation. For persistent and progressive increase in serum transaminase that cannot be attributed to other causes, deferasirox should be interrupted. After resolution, DFX can be resumed at a lower dose followed by gradual dose escalation.
Protocol
Based on the medical literature, the Scientific Committee of the Brazilian Association of Thalassemia (ABRASTA) is suggesting an iron chelation therapy protocol for transfusional iron overload and thalassemia. The objective is to help hematologists to choose the most appropriate chelation therapy for their patients. The trials were carefully selected and they provide consistent evidence on strategies to be adopted for patients with iron overload.
The classification criteria for the recommendations (grades A, B, C and D) listed in this protocol are similar to those adopted by the 'Projeto Diretrizes', guidelines developed by the Associação Médica Brasileira (AMB) and the Conselho Federal de Medicina (CFM)(51).
These guidelines are based on changes in the MIC and LIC measured by the T2* MRI method, LVEF and serum ferritin. We are proposing four situations: naïve iron chelation, cardiac T2* value > 20 ms, cardiac T2* value < 20 ms and MRI not available. If the patient is hepatitis C virus (HCV)-RNA-positive, iron chelation must be intensified in order to reduce LIC to decrease the potential for liver fibrosis and allow response to antiviral therapy (A)(52), (B)(53). Antiviral therapy administered concomitantly with DFP needs careful control.
Chelator dose adjustment is done based on transfusional iron intake and ferritin levels measured each three months.
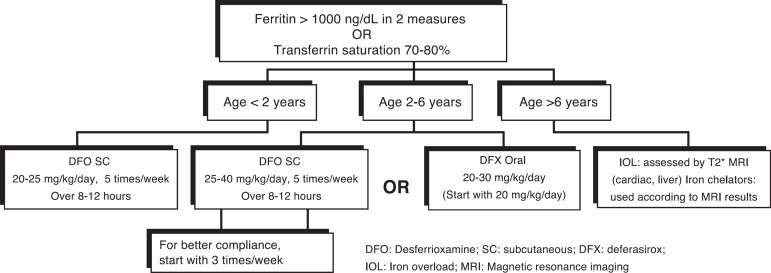
1. Patients naïve to iron chelation
The serum ferritin must be assessed after ten blood transfusions and when ferritin > 1000 ng/mL in two measures within 60 days, or if the transferrin saturation is > 70-80% (free iron in the plasma)(54-56), the recommendation is to follow Figure 1. Monitor DFO and DFX toxicity.
Figure 1.
Iron chelation therapy for patients with thalassemia naïve to iron chelation
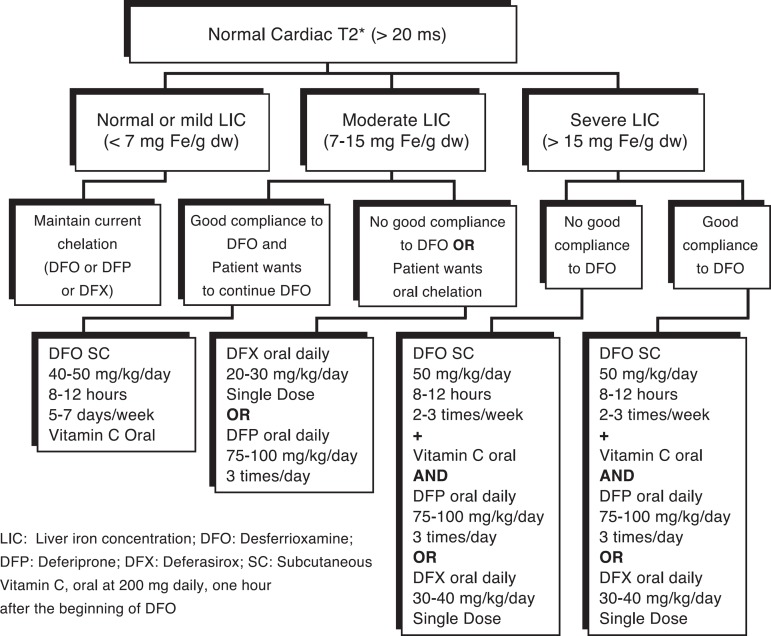
2. Patients with cardiac T2* value > 20 ms
Chelation therapy is based on cardiac and hepatic T2* values as shown in Figure 2. The liver iron clearance takes at least 12 months. Monitor DFO, DFP or DFX toxicity. Liver and cardiac MRI should be repeated every 12 months.
Figure 2.
Iron chelation therapy for patients with thalassemia without cardiac iron overload
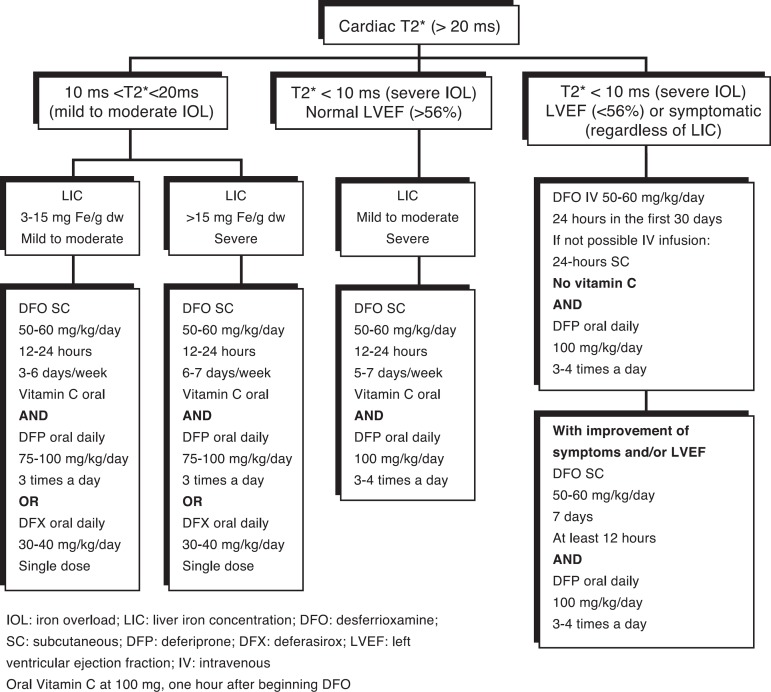
3. Patients with cardiac T2* value < 20 ms
Chelation therapy is based on cardiac and hepatic T2* values as shown in Figure 3. The liver iron clearance takes at least 12 months and cardiac iron clearance takes even longer. Monitor DFO, DFP or DFX toxicity, mainly with higher doses.
Figure 3.
Iron chelation therapy for patients with thalassemia with cardiac iron overload
When cardiac T2* value < 20 ms, liver and cardiac MRI should be repeated in 12 months and echocardiogram (ECO), electrocardiogram (ECG) and Holter every 6-12 months. If the LVEF is normal, no medication is needed to improve cardiac function.
When cardiac T2* value < 10 ms and LVEF is normal, perform ECO, ECG, Holter and cardiac MRI each six months. If cardiac T2* remains the same or decreased after 6-12 months, with worsening LVEF, change chelation as if cardiac T2* value < 10 ms.
When cardiac T2* value < 10 ms and/or LVEF < 56%, ECO and ECG should be repeated in two months, then every six months, Holter and cardiac MRI every six months. If cardiac T2* is lower after six months or LVEF is worsening, repeat continuous administration of intravenous DFO and oral DFP.
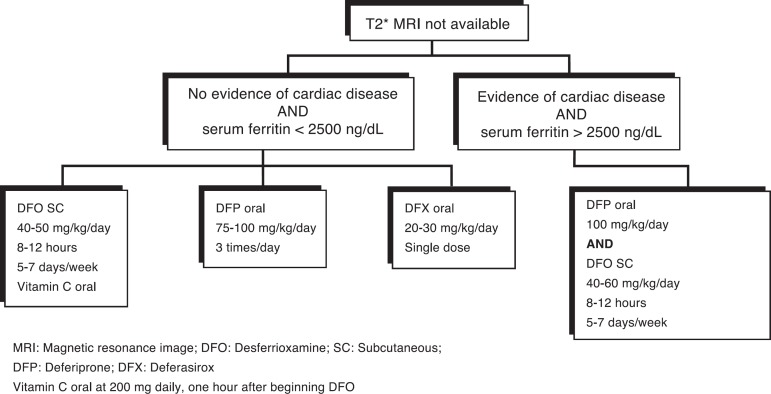
4. Magnetic resonance imaging not available
The recommendations when the MRI is not available (unable to travel to the T2* MRI center, claustrophobia, metallic implants, unable to cooperate with the procedure), are shown in Figure 4. Cardiac disease is not common in under 18-year-old patients regularly taking DFO and with a mean ferritin level < 2500 ng/mL. ECO, ECG and holter should be performed early to identify signs of left ventricular dysfunction or arrhythmias suggesting heart disease.
Figure 4.
Iron chelation therapy for patients with thalassemia when magnetic resonance imaging is not available
Combination therapy with DFP and DFX in patients with high iron overload or evidence of cardiac disease is still experimental(56).
General guidelines
1. When combination therapy cannot be implemented, use oral monotherapy with DFX at 40 mg/kg/day or DFP at 100 mg/kg/day, but monitor carefully (A)(21,30)(B)(20,31).
2. When cardiac function returns to normal and cardiac T2* value > 20 ms, the patient can be treated as shown in Figure 2.
3. The response to antiviral therapy against HCV is better with low levels of LIC (A)(52)(B)(53).
Conclusion
The decision to prescribe an iron chelator must consider the indications and contraindications of each drug and the need to tailor therapy for each patient. These guidelines were designed to help hematologists in their decisions. However, it is essential to use their clinical judgment and to consider their patient's individual needs when deciding on the recommendations.
Footnotes
Conflict-of-interest disclosure: The authors declare no competing financial interest
References
- 1.Borgna-Pignatti C, Rugolotto S, De Stefano P, Zhao H, Cappellini MD, Del Vecchio GC, et al. Survival and complications in patients with thalassemia major treated with transfusion and deferoxamine. Haematologica. 2004;89(10):1187–1193. Comment in: Haematologica. 2004;89(10):1157-9. [PubMed] [Google Scholar]
- 2.Cunningham MJ, Macklin EA, Neufeld EJ, Cohen AR, Thalassemia Clinical Research Network Complications of beta-thalassemia major in North America. Blood. 2004;104(1):34–39. doi: 10.1182/blood-2003-09-3167. [DOI] [PubMed] [Google Scholar]
- 3.Kirk P, Roughton M, Porter JB, Walker JM, Tanner MA, Patel J, et al. Cardiac T2* magnetic resonance for prediction of cardiac complications in thalassemia major. Circulation. 2009;120(20):1961–1968. doi: 10.1161/CIRCULATIONAHA.109.874487. Comment in: Circulation. 2009;120(20):1937-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brittenham GM, Griffith PM, Nienhuis AW, McLaren CE, Young NS, Tucker EE, et al. Efficacy of deferoxamine in preventing complications of iron overload in patients with thalassemia major. N Engl J Med. 1994;331(9):567–573. doi: 10.1056/NEJM199409013310902. Comment in: N Engl J Med. 1995;332(4):270-1. N Engl J Med. 1995;332(4):271-2. N Engl J Med. 1994;331(9):609-10. [DOI] [PubMed] [Google Scholar]
- 5.Olivieri NF, Nathan DG, MacMillan JH, Wayne AS, Liu PP, McGee A, et al. Survival in medically treated patients with homozygous beta-thalassemia. N Engl J Med. 1994;331(9):574–578. doi: 10.1056/NEJM199409013310903. Comment in: N Engl J Med. 1995;332(4):271; author reply 272-3; N Engl J Med. 1995;332(4):271-2; author reply 272-3; N Engl J Med. 1994; 331(9):609-10. [DOI] [PubMed] [Google Scholar]
- 6.Gabutti V, Piga A. Results of long-term iron-chelating therapy. Acta Haematol. 1996;95(1):26–36. doi: 10.1159/000203853. [DOI] [PubMed] [Google Scholar]
- 7.Modell B, Khan M, Darlison M. Survival in beta-thalassaemia major in the UK: data from the UK Thalassaemia Register. Lancet. 2000;355(9220):2051–2052. doi: 10.1016/S0140-6736(00)02357-6. [DOI] [PubMed] [Google Scholar]
- 8.Anderson LJ, Westwood MA, Prescott E, Walker JM, Pennell DJ, Wonke B. Development of thalassaemic iron overload cardiomyopathy despite low liver iron levels and meticulous compliance to desferrioxamine. Acta Haematol. 2006;115(1-2):106–108. doi: 10.1159/000089475. [DOI] [PubMed] [Google Scholar]
- 9.Hoffbrand AV, Cohen A, Hershko C. Role of deferiprone in chelation therapy for transfusional iron overload. Blood. 2003;102(1):17–24. doi: 10.1182/blood-2002-06-1867. [DOI] [PubMed] [Google Scholar]
- 10.Victor Hoffbrand A. Deferiprone therapy for transfusional iron overload. Best Pract Res Clin Haematol. 2005;18(2):299–317. doi: 10.1016/j.beha.2004.08.026. [DOI] [PubMed] [Google Scholar]
- 11.Wonke B, Wright C, Hoffbrand AV. Combined therapy with deferiprone and desferrioxamine. Br J Haematol. 1998;103(2):361–364. doi: 10.1046/j.1365-2141.1998.01002.x. Comment in: Br J Haematol. 1999;106(1):252-3. [DOI] [PubMed] [Google Scholar]
- 12.Mourad FH, Hoffbrand AV, Sheikh-Taha M, Koussa S, Khoriaty AI, Taher A. Comparison between desferrioxamine and combined therapy with desferrioxamine and deferiprone in iron overloaded thalassaemia patients. Br J Haematol. 2003;121(1):187–189. doi: 10.1046/j.1365-2141.2003.04240.x. [DOI] [PubMed] [Google Scholar]
- 13.Kattamis A, Kassou C, Berdousi H, Ladis V, Papassotiriou I, Kattamis C. Combined therapy with desferrioxamine and deferiprone in thalassemic patients: effect on urinary iron excretion. Haematologica. 2003;88(12):1423–1425. [PubMed] [Google Scholar]
- 14.Wu KH, Chang JS, Tsai CH, Peng CT. Combined therapy with deferiprone and desferrioxamine successfully regresses severe heart failure in patients with beta-thalassemia major. Ann Hematol. 2004;83(7):471–473. doi: 10.1007/s00277-003-0820-0. [DOI] [PubMed] [Google Scholar]
- 15.Alymara V, Bourantas D, Chaidos A, Bouranta P, Gouva M, Vassou A, et al. Effectiveness and safety of combined iron-chelation therapy with deferoxamine and deferiprone. Hematol J. 2004;5(6):475–479. doi: 10.1038/sj.thj.6200550. [DOI] [PubMed] [Google Scholar]
- 16.Origa R, Bina P, Agus A, Crobu G, Defraia E, Dessi C, et al. Combined therapy with deferiprone and desferrioxamine in thalassemia major. Haematologica. 2005;90(10):1309–1314. Comment in: Haematologica. 2005;90(10):1297A. [PubMed] [Google Scholar]
- 17.Daar S, Pathare AV. Combined therapy with desferrioxamine and deferiprone in beta thalassemia major patients with transfusional iron overload. Ann Hematol. 2006;85(5):315–319. doi: 10.1007/s00277-005-0075-z. [DOI] [PubMed] [Google Scholar]
- 18.Kattamis A, Ladis V, Berdousi H, Kelekis NL, Alexopoulou E, Papasotiriou I, et al. Iron chelation treatment with combined therapy with deferiprone and deferioxamine: a 12-month trial. Blood Cells Mol Dis. 2006;36(1):21–25. doi: 10.1016/j.bcmd.2005.11.002. [DOI] [PubMed] [Google Scholar]
- 19.Piga A, Gaglioti C, Fogliacco E, Tricta F. Comparative effects of deferiprone and deferoxamine on survival and cardiac disease in patients with thalassemia major: a retrospective analysis. Haematologica. 2003;88(5):489–496. Comment in: Haematologica. 2003;88(5):481-2. [PubMed] [Google Scholar]
- 20.Borgna-Pignatti C, Cappellini MD, De Stefano P, Del Vecchio GC, Forni GL, Gamberini MR, et al. Cardiac morbidity and mortality in deferoxamine- or deferiprone-treated patients with thalassemia major. Blood. 2006;107(9):3733–3737. doi: 10.1182/blood-2005-07-2933. [DOI] [PubMed] [Google Scholar]
- 21.Pennell DJ, Berdoukas V, Karagiorga M, Ladis V, Piga A, Aessopos A, et al. Randomized controlled trial of deferiprone or desferoxamine in beta-thalassemia major patients with asymptomatic myocardial siderosis. Blood. 2006;107(9):3738–3744. doi: 10.1182/blood-2005-07-2948. [DOI] [PubMed] [Google Scholar]
- 22.Tanner MA, Galanello R, Dessi C, Smith GC, Westwood MA, Agus A, et al. A randomized, placebo-controlled, double-blind trial of the effect of combined therapy with deferoxamine and deferiprone on myocardial iron in thalassemia major using cardiovascular magnetic resonance. Circulation. 2007;115(14):1876–1884. doi: 10.1161/CIRCULATIONAHA.106.648790. [DOI] [PubMed] [Google Scholar]
- 23.Tsironi M, Deftereos S, Andriopoulos P, Farmakis D, Meletis J, Aessopos A. Reversal of heart failure in thalassemia major by combined chelation therapy: a case report. Eur J Haematol. 2005;74(1):84–85. doi: 10.1111/j.1600-0609.2004.00335.x. [DOI] [PubMed] [Google Scholar]
- 24.Davis BA, Porter JB. Long-term outcome of continuous 24-hour deferoxamine infusion via indwelling intravenous catheters in high-risk beta-thalassemia. Blood. 2000;95(4):1229–1236. [PubMed] [Google Scholar]
- 25.Neufeld EJ. Oral chelators deferasirox and deferiprone for transfusional iron overload in thalassemia major: new data . Blood. 2006;107(9):3436–3441. doi: 10.1182/blood-2006-02-002394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cappellini MD, Cohen A, Piga A, Bejaoui M, Perrotta S, Agaoglu L, et al. A phase 3 study of deferasirox (ICL670), a once-daily oral iron chelator, in patients with beta-thalassemia. Blood. 2006;107(9):3455–3462. doi: 10.1182/blood-2005-08-3430. Comment in: Blood. 2006;108(5):1775-6; Blood. 2006;108(2):774-5; Blood. 2006;108(2):778. [DOI] [PubMed] [Google Scholar]
- 27.Deugnier Y, Turlin B, Ropert M, Cappellini MD, Porter JB, Giannone V, et al. Improvement in liver pathology of patients with β-thalassemia treated with deferasirox for at least 3 years. Gastroenterology. 2011;141(4):1202- 11, 1211.e1-3. doi: 10.1053/j.gastro.2011.06.065. Comment in: Gastroenterology. 2011;141(4):1142-3. [DOI] [PubMed] [Google Scholar]
- 28.Cappellini MD, Bejaoui M, Agaoglu L, Canatan D, Capra M, Cohen A, et al. Iron chelation with deferasirox in adult and pediatric patients with thalassemia major: efficacy and safety during 5 years' follow-up. Blood. 2011;118(4):884–893. doi: 10.1182/blood-2010-11-316646. [DOI] [PubMed] [Google Scholar]
- 29.Eleftheriou P, Tanner M, Pennel D, Porter JB. Response of myocardial T2* to oral deferasirox monotherapy for 1 year in 29 patients with transfusion-dependent anaemias; a subgroup analysis. Haematologica. 2006;91(s1):366–366. [Google Scholar]
- 30.Pennell DJ, Porter JB, Cappellini MD, El-Beshlawy A, Chan LL, Aydinok Y, et al. Efficacy of deferasirox in reducing and preventing cardiac iron overload in beta-thalassemia. Blood. 2010;115(12):2364–2371. doi: 10.1182/blood-2009-04-217455. Comment in: Blood. 2010;115(12):2333-4. [DOI] [PubMed] [Google Scholar]
- 31.Pennell DJ, Porter JB, Cappellini MD, Chan LL, El-Beshlawy A, Aydinok Y, et al. Continued improvement in myocardial T2* over two years of deferasirox therapy in β-thalassemia major patients with cardiac iron overload. Haematologica. 2011;96(1):48–54. doi: 10.3324/haematol.2010.031468. Comment in: Haematologica. 2011;96(1):5-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pennell DJ, Porter JB, Cappellini MD, Chan LL, El-Beshlawy A, Aydinok Y, et al. Deferasirox for up to 3 years leads to continued improvement of myocardial T2* in patients with β-thalassemia major. Haematologica. 2012;97(6):842–848. doi: 10.3324/haematol.2011.049957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Assis RA de, Ribeiro AA, Kay FU, Rosemberg LA, Nomura CH, Loggetto SR, et al. Pancreatic iron stores assessed by magnetic resonance imaging (MRI) in beta thalassemic patients. Eur J Radiol. 2012;81(7):1465–1470. doi: 10.1016/j.ejrad.2011.03.077. [DOI] [PubMed] [Google Scholar]
- 34.Wood JC, Tyszka JM, Carson S, Nelson MD, Coates TD. Myocardial iron loading in transfusion-dependent thalassemia and sickle cell disease. Blood. 2004;103(5):1934–1936. doi: 10.1182/blood-2003-06-1919. [DOI] [PubMed] [Google Scholar]
- 35.Wood JC, Origa R, Agus A, Matta G, Coates TD, Galanello R. Onset of cardiac iron loading in pediatric patients with thalassemia major. Haematologica. 2008;93(6):917–920. doi: 10.3324/haematol.12513. Comment in: Haematologica. 2009;94(12):1776-7 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fernandes JL, Fabron A, Jr, Verissimo M. Early cardiac iron overload in children with transfusion-dependent anemias. Haematologica. 2009;94(12):1776–1777. doi: 10.3324/haematol.2009.013193. Comment on: Haematologica. 2008;93(6):917-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Harrison PM, Arosio P. The ferritins: molecular properties, iron storage function and cellular regulation. Biochim Biophys Acta. 1996;1275(3):161–203. doi: 10.1016/0005-2728(96)00022-9. [DOI] [PubMed] [Google Scholar]
- 38.Olivieri NF, Brittenham GM, Matsui D, Berkovitch M, Blendis LM, Cameron RG, et al. Iron-chelation therapy with oral deferiprone in patients with thalassemia major. N Engl J Med. 1995;332(14):918–922. doi: 10.1056/NEJM199504063321404. Comment in: N Engl J Med. 1995;333(9):597-8; N Engl J Med. 1995;333(9):598; N Engl J Med. 1995;332(14):953-4. [DOI] [PubMed] [Google Scholar]
- 39.Hershko C, Link G, Cabantchik I. Pathophysiology of iron overload. Ann N Y Acad Sci. 1998;850:191–201. doi: 10.1111/j.1749-6632.1998.tb10475.x. [DOI] [PubMed] [Google Scholar]
- 40.Wood JC, Enriquez C, Ghugre N, Tyzka JM, Carson S, Nelson MD, Coates TD. MRI R2 and R2* mapping accurately estimates hepatic iron concentration in transfusion-dependent thalassemia and sickle cell disease patients. Blood. 2005;106(4):1460–1465. doi: 10.1182/blood-2004-10-3982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Cappellini MD, Cohen A, Eleftheriou A, Piga A, Porter J, Taher A, editors. Guidelines for the Clinical Management of Thalassaemia [Internet] 2nd rev ed. Cyprus: Thalassaemia International Federation; 2008. [cited 2011 Sep 21]. Available from: http://www.thalassaemia.org.cy/wordpress/wp-content/uploads/2012/12/Guidelines-2nd-edition-revised-ENGLISH-lo.pdf. [PubMed] [Google Scholar]
- 42.Anderson LJ, Holden S, Davis B, Prescott E, Charrier CC, Bunce NH, et al. Cardiovascular T2-star (T2*) magnetic resonance for the early diagnosis of myocardial iron overload. Eur Heart J. 2001;22(23):2171–2179. doi: 10.1053/euhj.2001.2822. Comment in: Eur Heart J. 2001;22(23):2140-1. [DOI] [PubMed] [Google Scholar]
- 43.Ghugre NR, Enriquez CM, Coates TD, Nelson MD, Jr, Wood JC. Improved R2* measurements in myocardial iron overload. J Magn Reson Imaging. 2006;23(1):9–16. doi: 10.1002/jmri.20467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Fernandes JL, Sampaio EF, Verissimo M, Pereira FB, da Silva JA, Figueiredo de GS, et al. Heart and liver T2* assessment for iron overload using different software programs. Eur Radiol. 2011;21(12):2503–2510. doi: 10.1007/s00330-011-2208-1. [DOI] [PubMed] [Google Scholar]
- 45.Hankins JS, McCarville MB, Loeffler RB, Smeltzer MP, Onciu M, Hoffer FA, et al. R2* magnetic resonance imaging of the liver in patients with iron overload. Blood. 2009;113(20):4853–4855. doi: 10.1182/blood-2008-12-191643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Carpenter JP, He T, Kirk P, Roughton M, Anderson LJ, Noronha de SV, et al. On T2* magnetic resonance and cardiac iron. Circulation. 2011;123(14):1519–1528. doi: 10.1161/CIRCULATIONAHA.110.007641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Farmaki K, Tzoumari I, Pappa C, Chouliaras G, Berdoukas V. Normalisation of total body iron load with very intensive combined chelation reverses cardiac and endocrine complications of thalassaemia major. Br J Haematol. 2010;148(3):466–475. doi: 10.1111/j.1365-2141.2009.07970.x. Comment in: Br J Haematol. 2010;150(4):489-90. [DOI] [PubMed] [Google Scholar]
- 48.Porter JB, Piga A, Cohen A, Ford JM, Bodner J, Rojkjaer L, et al. Safety of deferasirox (Exjade®) in patients with transfusion-dependent anemias and iron overload who achieve serum ferritin levels < 1000 ng/mL during long-term treatment. [cited 2012 Mar 21];Blood. 2008 112(11) (ASH Annual Meeting Abstracts) [Internet] abstract 5423. Available from: http://abstracts.hematologylibrary.org/cgi/content/abstract/112/11/5423?maxtoshow=&hits=10&RESULTFORMAT=&fulltext=piga+a&searchid=1&FIRSTINDEX=0&volume=112&issue=11&resourcetype=HWCIT. [Google Scholar]
- 49.Cohen AR, Galanello R, Piga A, De Sanctis V, Tricta F. Safety and effectiveness of long-term therapy with the oral iron chelator deferiprone. Blood. 2003;102(5):1583–1587. doi: 10.1182/blood-2002-10-3280. [DOI] [PubMed] [Google Scholar]
- 50.al-Refaie FN, Wonke B, Hoffbrand AV. Deferiprone-associated myelotoxicity. Eur J Haematol. 1994;53(5):298–301. doi: 10.1111/j.1600-0609.1994.tb01323.x. [DOI] [PubMed] [Google Scholar]
- 51.Projeto Diretrizes: Associação Médica Brasileira e Conselho Federal de Medicina. São Paulo: [cited 2011 Sep 14]. Available from: http://www.projetodiretrizes.org.br/projeto_diretrizes/texto_introdutorio.pdf. [Google Scholar]
- 52.Fargion S, Fracanzani AL, Rossini A, Borzio M, Riggio O, Belloni G, et al. Iron reduction and sustained response to interferon-alpha therapy in patients with chronic hepatitis C: results of an Italian multicenter randomized study. Am J Gastroenterol. 2002;97(5):1204–1210. doi: 10.1111/j.1572-0241.2002.05705.x. Comment in: Am J Gastroenterol. 2002;97(5):1093-6. [DOI] [PubMed] [Google Scholar]
- 53.Angelucci E, Muretto P, Nicolucci A, Baronciani D, Erer B, Gaziev J, et al. Effects of iron overload and hepatitis C virus positivity in determining progression of liver fibrosis in thalassemia following bone marrow transplantation. Blood. 2002;100(1):17–21. doi: 10.1182/blood.v100.1.17. [DOI] [PubMed] [Google Scholar]
- 54.Hershko C. Pathogenesis and management of iron toxicity in thalassemia. Ann N Y Acad Sci. 2010;1202:1–9. doi: 10.1111/j.1749-6632.2010.05544.x. [DOI] [PubMed] [Google Scholar]
- 55.Piga A, Longo F, Duca L, Roggero S, Vinciguerra T, Calabrese R, et al. High non transferrin bound iron levels and heart disease in thalassemia major. Am J Hematol. 2009;84(1):29–33. doi: 10.1002/ajh.21317. [DOI] [PubMed] [Google Scholar]
- 56.Farmaki K, Tzoumari I, Pappa C. Oral chelators in transfusion-dependent thalassemia major patients may prevent or reverse iron overload complications. Blood Cells Mol Dis. 2011;47(1):33–40. doi: 10.1016/j.bcmd.2011.03.007. [DOI] [PubMed] [Google Scholar]