Abstract
Purpose
Most studies of perceived discrimination have been cross-sectional and focused primarily on mental rather than physical health conditions. We examined the associations of perceived racial and gender discrimination reported in adulthood with early life factors and self-reported physician-diagnosis of chronic physical health conditions.
Methods
We used data from a racially diverse birth cohort of U.S. women (N=168, average age=41 years) with prospectively collected early life data (e.g., parental socioeconomic factors) and adult reported data on perceived discrimination, physical health conditions, and relevant risk factors. We performed modified robust Poisson regression due to the high prevalence of the outcomes.
Results
Fifty-percent of participants reported racial and 39% reported gender discrimination. Early life factors did not have strong associations with perceived discrimination. In adjusted regression models, participants reporting at least three experiences of gender or racial discrimination had a 38% increased risk of having at least one physical health conditions (RR=1.38, 95% CI: 1.01-1.87). Using standardized regression coefficients, the magnitude of the association of having physical health conditions was larger for perceived discrimination than for being overweight or obese.
Conclusion
Our results suggest a substantial chronic disease burden associated with perceived discrimination, which may exceed the impact of established risk factors for poor physical health.
Introduction
Chronic diseases are the leading causes of morbidity and mortality among U.S. women, with nearly one of every two adults being affected by at least one chronic disease (Centers for Disease Control and Prevention, 2012a). Racial/ethnic minority populations in the U.S. bear an even higher burden, experiencing a higher prevalence, and greater morbidity and/or mortality for many common chronic diseases. For example, as compared with non-Hispanic white women, African American women are almost twice as likely to have a stroke (Office of Women’s Health), and both African American and Hispanic women are twice as likely to have diabetes (Office of Minority Health).
Extensive research has identified a number of biomedical and behavioral risk factors for chronic diseases, which include sedentary lifestyle, poor nutrition, smoking, and excessive alcohol consumption (Centers for Disease Control and Prevention, 2012a). In recent years, with growing interest in social determinants of health, research has also begun to investigate the social factors that shape these risk factors and contribute to health disparities. One such factor includes experiences of unfair treatment attributed to one’s social status such as race/ethnicity and gender (hereafter referred to as perceived discrimination). According to Krieger (Krieger, 1999), experiences of unfair treatment “creates and structures exposures to noxious physical, chemical, biological, and psychosocial insults, all of which can affect biological integrity at numerous integrated and interacting levels, simultaneously comprised of genes, cells, tissues, organs, and organ systems.” Thus, discrimination may impact health through multiple pathways resulting in the “biology of inequality” (Krieger, 1999; D. R. Williams & Mohammed, 2009).
The current empirical research on perceived discrimination and health is limited in several areas. First, most studies have focused on racial discrimination, with little attention given to gender discrimination. Examining discrimination experiences related to different social statuses may be salient in racially diverse populations experiencing different prevalence and type of discrimination (Hartman, Hoogstraten, & Spruijt-Metz, 1994). For example, African American and white women have shown to have similar experiences of gender discrimination, but few white women report racial discrimination (Krieger, 1990; Watson, Scarinci, Klesges, Slawson, & Beech, 2002). Second, the majority of research has considered mental health and behavioral outcomes, with far fewer studies of physical health states (Paradies, 2006; Pascoe & Smart Richman, 2009; D. R. Williams & Mohammed, 2009). Studies that have examined the associations between discrimination and physical health have mostly examined only one type of physical health condition or used global proxies of physical health. Therefore, these studies have been unable to demonstrate the overall impact of discrimination experiences on clinical outcomes such as chronic physical health conditions. Third, discrimination experiences have rarely been examined from a life course perspective. As a result, very little is known about whether circumstances and exposures encountered in early life periods, such as in childhood, influence discrimination experiences. For example, early age at pubertal development in girls is associated with early breast development and menstruation (Beunen, Rogol, & Malina, 2006). These physical changes may result in early exposure to unfair treatment and discrimination in the school and public environments. Furthermore, parental socioeconomic status in childhood may shape economic and social circumstances that may impact experiences of discrimination (e.g., residential segregation) (Duncan, Ziol-Guest, & Kalil, 2010; Krieger, 1999).
To address these limitations, we used early life and adult data from a racially diverse birth cohort of U.S. women to examine the associations of perceived racial and gender discrimination in relation to early life factors and a wide range of chronic physical health conditions reported in adulthood.
Methods
Study population and data collection
We used data from the New York Women’s Birth Cohort, an adult follow-up study of former child participants of the National Collaborative Perinatal Project who were born between 1959 and 1963 in New York City. Detailed information regarding study design and recruitment of study participants have been described elsewhere (Broman, 1984; Hardy, 2003; Terry, Flom, Tehranifar, & Susser, 2009). Briefly, we attempted to locate former child participants who were followed from birth through age 7 (n=841) as adults between 2001 and 2006. We traced 375 (45%) and enrolled 262 (70% of those traced) participants in an adult follow-up study. Of this group, 168 participants (64%) completed a questionnaire that included questions on perceived discrimination. This study sample consisted of 37% Hispanic women, 33% non-Hispanic African American, and 30% non-Hispanic white women, and had an average age of 41 years (range: 38-46 years).
Early life data were collected prospectively following a standardized protocol through interviews and clinical visits with child participants and their parents or guardians (Broman, 1984; Hardy, 2003; Terry et al., 2009). All other data used in this analysis were collected through a questionnaire completed by participants as adults. Study procedures were approved by the internal review board [name of IRB blinded by WHI editors for peer review].
Measures
Discrimination
We used the Experiences of Discrimination scale developed by Krieger et al. to collect data on self-reported discrimination experiences (Krieger, 1990). Thus, our results and discussion are in the context of perceived discrimination. In separate questions, participants were asked if they had ever been prevented from doing something, or had been hassled or made to feel inferior because of their race/ethnicity and gender in the following experiences: at school, getting a job, getting housing, getting medical care, in a public setting, or from the police or in the courts (the latter item asked for racial discrimination only). Based on responses to these questions we developed three measures: reports of racial discrimination, reports of gender discrimination, and reports of any (racial or gender) discrimination (hereafter referred to as overall discrimination). Consistent with prior research, we created the following categorical variables for each discrimination measure (Krieger, Smith, Naishadham, Hartman, & Barbeau, 2005): 1) a three-level variable corresponding to no reports of discrimination, reports of 1-2 discrimination experiences, and reports of 3 or more discrimination experiences, and 2) a dichotomous variable of no reports of discrimination and any report of discrimination.
Early Life Factors
We selected early life factors that have been found to be associated with chronic physical health conditions and/or discrimination based on existing literature and our prior research in this study population (James-Todd, Tehranifar, Rich-Edwards, Titievsky, & Terry, 2010; Krieger, Rowley, Herman, Avery, & Phillips, 1993; Tehranifar, Liao, Flom, & Terry, 2009; Terry, Wei, & Esserman, 2007). These included the following factors measured around the time of participants’ births: birth weight (in kg, divided into tertiles), maternal education (less than high school degree versus high school or higher degree), and parental socioeconomic status (SES) at birth. SES at birth was based on father’s education and occupation and family income, and was assessed as scores ranging from 0 to 100 with higher scores corresponding to higher SES (divided into tertiles in the current analysis) (James-Todd et al., 2010). Other early life factors collected through the adult follow-up questionnaire included childhood family structure (single versus 2-parent household up to the age of 13), and age at menarche (years, continuous).
Adult Factors
We considered adult factors that have been associated with chronic physical health conditions (Ferris, Flom, Tehranifar, Mayne, & Terry, 2010; Tehranifar et al., 2009; Terry et al., 2007). These included self-identified race (African American, Hispanic, or white), marital status (never married, married or living as married, other), current household income (<50,000, 50,000-<90,000, ≥90,000), highest educational attainment (less than college degree, college or higher degrees), current smoking status (nonsmoker, former, current) and body mass index (BMI, <25, 25-29.9, or ≥30 kg/m2).
Chronic Physical Health Conditions
We assessed chronic physical conditions (hereafter referred to as physical health conditions) using the Center for Disease Control and Prevention Measures that assess health conditions and medical history (Centers for Disease Control and Prevention, 2000). We asked participants whether they had ever been diagnosed by a physician as having the following conditions: heart disease or angina, heart attack, high cholesterol, hypertension, diabetes, asthma, thyroid disease, rheumatoid arthritis, pain, cancer, or any other illness or condition not listed. The only conditions excluded were psychiatric and mental health outcomes. Interpersonal discrimination has been broadly conceptualized as a psychosocial stressor that can elicit different physiological changes, and potentially lead to different disease manifestation (D. R. Williams & Mohammed, 2009). Thus, considering different physical conditions may be a reasonable method for evaluating the overall physical health burden of discrimination. We classified participants as having no physical conditions, having a single physical condition, and having multiple physical conditions.
Data Analysis
In addition to generating descriptive statistics, we performed modified robust Poisson regression, in lieu of logistic regression models that tend to overestimate common outcomes such as discrimination and physical health conditions in our sample (Zou, 2004). First, we examined whether early life factors (e.g., birth weight, parental SES) as well as adult social and behavioral factors (e.g., adult education, BMI) predicted reports of racial discrimination and gender discrimination separately. Next, we investigated the associations between reports of discrimination (racial, gender and overall discrimination) and having physical conditions. We repeated our analyses using physical condition as a dichotomous variable (no physical conditions or any number of physical conditions) and a 3-level categorical variable (no physical condition, single physical condition, and more than one physical condition). Because there were no material differences in inference when using the dichotomous variable and the 3-level variable of physical conditions, we present the former for greater statistical power. We included variables that altered the associations for the main exposure variables (e.g., early life factors or adult factors altering associations for perceived discrimination and physical conditions) by at least 10% in multivariable models.
Results
Sixty-percent of the participants reported at least one physical condition, with 27% reporting a single condition and 33% reporting multiple conditions. Cardiovascular diseases and asthma were the most prevalent conditions in the total sample and amongst those with a single physical condition (6% and 6%, respectively). Among those with multiple conditions, 21% reported cardiovascular diseases and 15% reported pain as one of their physical conditions (Figure 1). Nearly 68% of Hispanic and African American participants reported at least one physical condition whereas 58% of white participants reported no physical conditions. African American participants were also more likely to report multiple conditions (43% vs. 31% of Hispanic and 26% of white participants). Participants with the middle category of household income ($50,000-<90,000) had the highest prevalence of no physical conditions (53%) while participants earning the lowest income category (<50,000) had the highest prevalence of having multiple physical conditions (49%). Participants with BMI≥25 kg/m2 were more likely to report multiple physical conditions in comparison to participants with a BMI<25 kg/m2 (41% for BMI 25-29.9 and 44% for BMI≥30 vs. 19% for BMI<25 kg/m2) (Table 1).
Figure 1.
Percentage of participants reporting chronic physical health conditions by the number and type of conditions reported
Table 1. Distribution of Early Life Factors and Perceived Discrimination by the Number of Chronic Physical Health Conditions, New York Women’s Birth Cohort Adult Follow-Up, 2001-2006.
| Reports of chronic physical conditions |
||||||||
|---|---|---|---|---|---|---|---|---|
| Characteristic | No Condition |
Single Condition |
Multiple |
|||||
| N=67 | N=45 | Conditions N=56 | ||||||
| No. (%) | Mean (SD) |
No. (%) | Mean (SD) |
No. (%) | Mean (SD) |
P Value | ||
| Race/Ethnicity | Hispanic African American White |
20 (32) 18 (32) 29 (58) |
23 (37) 14 (25) 8 (16) |
19 (31) 24 (43) 13 (26) |
0.01 | |||
| Age (years) | Continuous | 41.13 (1.55) |
41.24 (1.35) |
41.38 (1.51) |
0.63 | |||
| Early Life Factors | ||||||||
| Birth weight (kg) tertile |
1(<2.92) 2(2.92-<3.29) 3(≥3.29) |
21 (39) 21 (39) 25 (42) |
13 (24) 15 (28) 17 (28) |
20 (37) 18 (33) 18 (30) |
0.93 | |||
| SES at birth tertile |
Low tertile Medium tertile High tertile |
25 (38) 20 (38) 22 (45) |
18 (27) 15 (29) 11 (22) |
23 (35) 17 (33) 16 (33) |
0.37 | |||
| Maternal education |
High school or higher degree Less than high school degree |
39 (42) 28 (38) |
21 (23) 23 (31) |
32 (35) 23 (31) |
0.49 | |||
| Age at menarche (years) |
Continuous | 12.6 (1.6) |
12.7 (1.6) |
12.5 (2.0) |
0.85 | |||
| Childhood family structure |
Single parent Two parent |
14 (38) 53 (40) |
9 (24) 36 (27) |
14 (38) 42 (32) |
0.80 | |||
| Adult Factors | ||||||||
| Marital statusa | Never Married Marriedor living as married Other |
12 (35) 41 (40) 14 (44) |
7 (21) 33 (32) 5 (16) |
15 (44) 28 (27) 13 (41) |
0.18 | |||
| Adult household income |
< 50K 50K-<90K ≥ 90K |
16 (31) 31 (53) 20 (34) |
10 (20) 13 (22) 22 (37) |
25 (49) 14 (24) 17 (29) |
0.01 | |||
| Adult education | College or higher degree Less than college degree |
31 (40) 36 (40) |
25 (32) 20 (22) |
21 (27) 35 (38) |
0.19 | |||
| BMI (kg/m2) | <25 25-29.9 ≥30 |
35 (49) 16 (33) 16 (36) |
23 (32) 13 (26) 9 (20) |
14 (19) 20 (41) 20 (44) |
0.03 | |||
| Current smoking status |
Nonsmokers Former Smoker Current smoker |
27 (35) 20 (42) 20 (45) |
27 (35) 10 (21) 8 (18) |
23 (30) 17 (36) 16 (36) |
0.28 | |||
| Have you ever experienced discrimination due to race? |
0 1-2 3+ |
43 (51) 14 (31) 10 (26) |
18 (21) 12 (27) 15 (38) |
23 (27) 19 (42) 14 (36) |
0.03 | |||
| Have you ever experienced discrimination due to gender? |
0 1-2 3+ |
44 (43) 18 (42) 5 (22) |
28 (27) 8(19) 9(39) |
30 (29) 17 (39) 9 (39) |
0.21 | |||
Abbreviation: SD, standard deviation; SES, socioeconomic status
Other category includes women who are not living with spouse/partner, separated, or widowed.
Fifty-percent of the cohort reported at least one racial discrimination experience and 39% reported at least one gender discrimination experience (Table 1). Thirty-four percent of participants reported multiple experiences of racial discrimination and 27% reported multiple experiences of gender discrimination, while 29% reported experiencing both forms of discrimination.
Life course factors and perceived discrimination
African American and Hispanic participants were more likely to report racial discrimination than those who identified as white (relative risk [RR]=4.36, 95% Confidence Interval (CI): 2.37, 8.02 for African Americans and RR=2.78, 95% CI: 1.46, 5.29 for Hispanic, both relative to whites), but there were no racial differences in reports of gender discrimination (Table 2). There was no statistically significant association between parental SES and maternal education at birth and perceived discrimination. Marginally statistically significant associations were observed between later age at menarche and reports of racial and gender discrimination (RR=1.08, 95% CI: 0.99, 1.17; RR=1.12, 95% CI: 1.01, 1.24, respectively). Adult risk factors (BMI, smoking status) and sociodemographic factors (marital status, adult income and education) similarly did not have statistically significant associations with perceived racial or gender discrimination (data not shown). The strongest associations for adult risk factors were found for adult BMI with overweight and obese participants being more likely to report racial discrimination than participants with a BMI<25 kg/m2 (RR=1.32, 95% CI: 0.91, 1.92; RR=1.39, 95% CI: 0.96, 2.01 for BMI 25-29.9 and BMI≥30 respectively, vs. BMI<25 kg/m2).
Table 2. Unadjusted Associations between Early Life Factors and Perceived Racial and Gender Discrimination, New York Women’s Birth Cohort Adult Follow-Up, 2001-2006.
| Racial Discrimination | Gender Discrimination | ||||
|---|---|---|---|---|---|
| RR | RR | ||||
| Variable | Level | 95% CI | 95% CI | ||
| Race/Ethnicity | White African American Hispanic |
1.00 4.36 2.78 |
Reference 2.37, 8.02 1.46, 5.29 |
1.00 1.12 0.85 |
Reference 0.71, 1.75 0.52, 1.38 |
| Age (years) | Continuous | 1.01 | 0.91, 1.12 | 0.96 | 0.85, 1.09 |
| Birth Weight (kg) Tertile | 1(<2.92) 2(2.92-<3.29)<break/>3(≥3.29) |
1.00 0.83 0.87 |
Reference 0.57, 1.21 0.61, 1.24 |
1.00 1.14 0.78 |
Reference 0.74, 1.75 0.47, 1.27 |
| SES at Birth | Low tertile Medium tertile High tertile |
1.00 1.31 1.03 |
Reference 0.93, 1.86 0.69, 1.54 |
1.00 1.50 1.10 |
Reference 0.97, 2.32 0.67, 1.82 |
| Maternal education | High school or higher degree Less than high school degree |
1.00 1.16 |
Reference 0.85, 1.57 |
1.00 0.97 |
Reference 0.67, 1.42 |
| Age at menarche (years) | Continuous | 1.08 | 0.99, 1.17 | 1.12 | 1.01, 1.24 |
| Childhood family structure |
Single parent Two parent |
1.00 0.97 |
Reference 0.67, 1.38 |
1.00 1.05 |
Reference 0.66, 1.67 |
Abbreviation: CI, confidence interval; RR, relative risk; SES, socioeconomic status
Discrimination and chronic physical health conditions
Table 3 summarizes the associations between discrimination and physical health conditions. In the unadjusted models, reporting three or more experiences of each type of discrimination was significantly associated with being diagnosed with at least one physical condition in comparison to no reports of discrimination (unadjusted models RR=1.52, 95% CI: 1.14, 2.03; RR=1.38, 95% CI: 1.05, 1.81, racial and gender, respectively). These associations were no longer statistically significant after adjustment for confounding variables (race/ethnicity, adult BMI and adult income) and mutual adjustment for each form of discrimination. Reporting three or more overall discrimination experiences (i.e., reporting any racial or gender discrimination) was significantly associated with increased risk of reporting physical conditions in unadjusted model (RR=1.45, 95% CI: 1.10, 1.91) and the adjusted model (RR=1.38, 95% CI: 1.01, 1.87).
Table 3. Unadjusted and Adjusted Associations between Perceived Racial and Gender Discrimination and Chronic Physical Health Conditions, New York Women’s Birth Cohort Adult Follow-Up, 2001-2006.
| Model |
||||||
|---|---|---|---|---|---|---|
| Unadjusted |
Adjusteda |
|||||
| RR | RR | |||||
| Form of Discrimination |
N | 95% CI | 95% CI | |||
| Racial Discrimination | ||||||
| None | No physical conditions One or more physical conditions |
43 41 |
1.00 | Reference | 1.00 | Reference |
| 1-2 Experiences | No physical conditions One or more physical conditions |
14 31 |
1.41 | 1.05, 1.90 | 1.20 | 0.85, 1.70 |
| 3 or more Experiences | No physical conditions One or more physical conditions |
10 29 |
1.52 | 1.14, 2.03 | 1.31 | 0.87, 1.96 |
|
Gender
Discrimination |
||||||
| None | No physical conditions One or more physical conditions |
44 45 |
1.00 | Reference | 1.00 | Reference |
| 1-2 Experiences | No physical conditions One or more physical conditions |
18 25 |
1.02 | 0.73, 1.39 | 1.00 | 0.73, 1.36 |
| 3 or more Experiences | No physical conditions One or more physical conditions |
5 18 |
1.38 | 1.05, 1.81 | 1.14 | 0.82, 1.58 |
|
Overall
Discrimination |
||||||
| None | No physical conditions One or more physical conditions |
32 34 |
1.00 | Reference | 1.00 | Reference |
| 1-2 Experiences | No physical conditions One or more physical conditions |
20 23 |
1.04 | 0.72, 1.50 | 0.96 | 0.66, 1.40 |
| 3 or more Experiences | No physical conditions One or more physical conditions |
15 44 |
1.45 | 1.10, 1.91 | 1.38 | 1.01, 1.87 |
Abbreviation: CI, confidence interval; RR, relative risk
The adjusted model for racial, gender, and overall discrimination are adjusted for BMI, race/ethnicity, and income. Additionally, the racial discrimination model is adjusted for gender discrimination and the gender discrimination model is adjusted for racial discrimination.
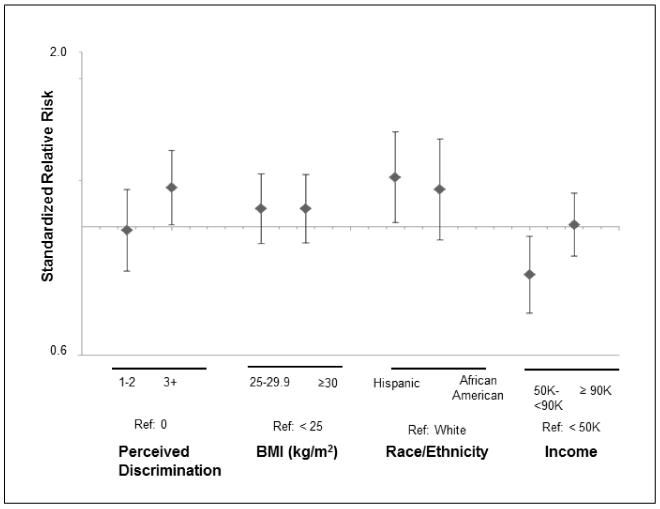
We used standardized relative risk regression estimates to compare the magnitude of the associations of physical conditions with overall discrimination, race/ethnicity, adult BMI, and adult income from the same multivariable model presented in Table 3 (Figure 2). We limit our final analysis to overall discrimination because the patterns of associations for the individual forms of discrimination and physical health conditions were similar. The relative risk estimate for having three or more discrimination experiences as compared to no reports of discrimination was of similar magnitude (RR=1.17, 95% CI: 1.01, 1.35) as the estimates for adult income (RR=0.83, 95% CI: 0.71, 0.96 for middle income vs. lowest income category), and only slightly smaller than the estimate for Hispanic ethnicity (RR=1.22, 95% CI: 1.01, 1.46). The relative risk estimates of the association for adult BMI was not statistically significant and 10% smaller than the relative risk for reporting three or more overall discrimination experiences (RR=1.07, 95% CI: 0.93, 1.23; RR=1.07, 95% CI: 0.94, 1.23 BMI=25-29.9 and BMI≥30 kg/m2, respectively).
Figure 2.
Adjusted standarized relative risk estimates from modified robust poisson regression models. filled diamonds represent coefficients and errors bars represent 95% confidence intervals.
Discussion
In a racially diverse cohort of women in their mid-life years, we observed a high prevalence of perceived discrimination. One of every two participants reported experiencing racial discrimination, and 40% and 29% of participants respectively reported gender discrimination and both racial and gender discrimination. African American and Hispanic participants were more likely to report experiencing racial discrimination than white participants, but no racial differences were observed in perceived gender discrimination. These prevalence and patterns are consistent with prior research using the same measurement of perceived discrimination in similar populations (Krieger, 1990; Watson et al., 2002).
We did not observe strong associations between perceived discrimination and parental socioeconomic factors including parental occupation and income, maternal education, and family structure. We also considered several other factors that are strongly influenced by early life social environment, including birth weight and age at menarche, and only observed some support for an influence of later menarche on perceived discrimination. Our study is one of the first to examine a range of early life factors in relation to reports of racial and gender discrimination in middle adulthood. If replicated in other research, our results may suggest that parental and childhood circumstances are not strong predictors of lifetime perceived racial and gender discrimination reported in adulthood.
Comparison of results of studies on perceived discrimination and health is challenging due to the large diversity of measurements of perceived discrimination, health outcomes and populations considered (Kressin, Raymond, & Manze, 2008). Despite these variations, the most recent meta-analysis of studies of perceived discrimination and physical health published in 1986-2007, found overall supportive evidence for adverse physical consequences of perceived discrimination (Pascoe & Smart Richman, 2009). Our results add to the evidence that discrimination may lead to a broad range of unfavorable physical health outcomes in racially diverse populations. We observed similar positive associations for perceived discrimination attributed to race and gender, with experiencing any form of discrimination associated with an increased risk of having one or more physical conditions. These findings are consistent with other studies of perceived racial and non-racial discrimination (Kessler, Mickelson, & Williams, 1999; D.R. Williams, Spencer, & Jackson, 1999) as well as studies in which the assessment of unfair treatment is not framed within any specific form of discrimination (De Vogli, Brunner, & Marmot, 2007; De Vogli, Ferrie, Chandola, Kivimaki, & Marmot, 2007).
There are currently no consensus or gold standard for measuring perceived discrimination, and over 30 different measures of discrimination have been used in prior research (Kressin et al., 2008). Because much of the contemporary discriminatory interactions occur in covert and subtle manners, assessment of discrimination by means other than self-report, are nearly impossible; thus the majority of studies, including ours, rely on measures of perceived discrimination. Available evidence, including results of laboratory experiments, suggests that individuals are able to understand the concept of discrimination and that reports of perceived discrimination correspond with objective experiences of discrimination (D. M. Taylor, Wright, & Porter, 1994; J. Taylor & Jackson, 1991). We used a measure of lifetime perceived discrimination that has been validated and used in prior research (Krieger, 1990; Krieger et al., 2005). This measure captures discrimination experiences in multiple settings, but it does not specify the timing (e.g. discrimination experiences prior to or after the onset of chronic physical health conditions) or specific acts (e.g., name calling, violence) of discrimination. While we specifically asked about discrimination attributed to race or gender, other basis for discrimination, such as weight, cannot be ruled out. Indeed, we found that overweight or obese BMI was positively associated with perceived discrimination and it is possible that participants may attribute discriminatory experiences based on weight to racism or sexism.
Our study limitations include a relatively small sample size, which may have contributed to low statistical power to detect statistically significant associations between perceived discrimination and early life factors. The limited sample size also restricted our ability to examine whether any of these associations differed across racial/ethnic groups. Given that both self-reported physical health conditions and perceived discrimination were collected at the same time point, our study could not establish temporal relationship between these two measures. Our outcome measure was based on self-reports of physician-diagnosed chronic physical health conditions, which is widely used in large national surveys, including the National Health and Nutrition Examination Survey and the U.S. National Health Interview Survey (Centers for Disease Control and Prevention, 2011, 2012b). Diagnosis of medical conditions is contingent upon healthcare access. Approximately 92% of our study participants reported having healthcare insurance, reducing the possibility that these conditions would be undiagnosed.
Our study population resembles the US populations on several characteristics including the prevalence of obesity (Towfighi, Zheng, & Ovbiagele, 2010), chronic morbidity (Freid, Bernstein, & Bush, 2012), cardiovascular disease (Thom, Haase et al., 2006), and asthma (National Center for Environmental Health, 2010). Other strengths of our study include the availability of prospective data on early life factors, and measurement of multiple forms of discrimination. Furthermore, while the majority of studies focus on African American experiences of discrimination, we included a racially diverse study population.
Implications for Practice and Policy
Many experiences of social adversity originate in early life and are likely to be transmitted across generations (Gee, Walsemann, & Brondolo, 2012). Investigating how early life environment contributes to discrimination exposures and their health consequences in adulthood remains a largely unexplored and important area of future investigation. Specifically, research on the timing, accumulation, and life-stage specific type of discrimination experiences in relation to health can provide crucial information for targeting interventions. Consistent with the theory of stress proliferation that a single stressor can lead to secondary stressors (Pearlin, Schieman, Fazio, & Meersman, 2005), Gee and colleagues propose that discrimination experiences can similarly accumulate across the life course, and illustrate this process using the following example: unfair conviction of a felony resulting from racial profiling may lead to difficulties in securing social goods (e.g., housing, student loans, employment) (Gee et al., 2012). As primary caregivers to children, women’s experiences of discrimination also impact their offspring development, further warranting a life course approach to addressing perceived discrimination (Rowley, Helaire, & Banerjee, 2010).
We found overall perceived discrimination to be a stronger predictor of chronic physical health conditions than being overweight or obese. We highlight this finding because obesity is an established risk factor for many chronic diseases (Field, Coakley et al., 2001) and a great deal of primary and secondary prevention efforts focus on reducing excess weight, while very little attention is directed towards identifying and addressing perceived discrimination as a target for reducing chronic disease burden. Our findings support the need for incorporating negative interpersonal experiences as a risk factor for chronic physical disease. In addition to policies and programs for preventing bias and prejudice, interventions are needed to counter the influence of discriminatory experiences on health. Social service and healthcare providers should be educated to recognize the extent of experiences of discrimination and their potential health impact in their targeted populations. They may also be in a position to identify effective ways of addressing discrimination (e.g., organizational policies within healthcare settings to support strategies and resources for dealing with discrimination). Research has shown that discrimination is most deleterious to health when these experiences are internalized (e.g., discrimination experiences are accepted or not discussed with others) (Krieger, 1999). Interventions that address internalization or self-blame regarding discrimination may be useful in mitigating adverse health impact.
Acknowledgments
This work was supported by the US Department of Defense Breast Cancer Research Program (grant DAMD 170210357); and the National Cancer Institute (grants K07 CA90685, 5T32 CA09529). The authors do not have any financial conflict of interest in the subject matter of this manuscript.
The authors thank the following persons for their contributions to the New York Women’s Birth Cohort Study: Dr. Ezra Susser, Julie Flom, Dr. Tamarra James-Todd, Dr. Lina Titievsky-Konikov, Dipal Shah, Jennifer Ferris, Tara Kalra, Shobana Ramachandran, Julia Meurling, Sujata Narayan, Summer Wright, and Adey Tsega. We would also like to thank all the women who participated in this research.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Jasmine A. McDonald, Department of Epidemiology, Columbia University/Mailman School of Public Health, 722W 168St, R719, New York, NY 10032, Phone: 212-305-9114, Fax: 212-305-9413, jam2319@columbia.edu.
Mary Beth Terry, Department of Epidemiology, Columbia University/Mailman School of Public Health, 722W 168St, R724A, New York, NY 10032, Phone: 212-305-4915, Fax: 212-305-9413, mt146@columbia.edu.
Parisa Tehranifar, Department of Epidemiology, Columbia University/Mailman School of Public Health, 722W 168St, 8th Floor, New York, NY 10032.
References
- Beunen GP, Rogol AD, Malina RM. Indicators of biological maturation and secular changes in biological maturation. Food Nutr Bull. 2006;27(4 Suppl Growth Standard):S244–256. doi: 10.1177/15648265060274S508. [DOI] [PubMed] [Google Scholar]
- Broman S. The Collaborative Perinatal Project: an overview. In: SA M, M H, KM F, editors. Handbook of Longitudinal Research. Praeger Publishers; New York: 1984. pp. 185–215. [Google Scholar]
- Centers for Disease Control and Prevention . Behavioral Risk Factor Surveillance System Survey Questionnaire. US Department of Health and Human Services, Centers for Disease Control and Prevention; Atlanta, GA: 2000. [Google Scholar]
- Centers for Disease Control and Prevention [Accessed August 5, 2013];U.S. National Health Interview Survey (NHIS). National Center for Health Statistics. 2011 http://www.cdc.gov/nchs/nhis.htm.
- Centers for Disease Control and Prevention . Chronic Disease Prevention and Health Promotion. National Center for Chronic Disease Prevention and Health Promotion; Atlanta, GA: [Accessed August 2, 2013]. 2012a. ( http://www.cdc.gov/chronicdisease/overview/index.htm) [Google Scholar]
- Centers for Disease Control and Prevention [Accessed August 5, 2013];The National Health and Nutrition Examination Survey (NHANES) 2011-2012. National Center for Health Statistics. 2012b http://www.cdc.gov/nchs/nhanes.htm.
- De Vogli R, Brunner E, Marmot MG. Unfairness and the social gradient of metabolic syndrome in the Whitehall II Study. J Psychosom Res. 2007;63(4):413–419. doi: 10.1016/j.jpsychores.2007.04.006. [DOI] [PubMed] [Google Scholar]
- De Vogli R, Ferrie JE, Chandola T, Kivimaki M, Marmot MG. Unfairness and health: evidence from the Whitehall II Study. J Epidemiol Community Health. 2007;61(6):513–518. doi: 10.1136/jech.2006.052563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duncan GJ, Ziol-Guest KM, Kalil A. Early-childhood poverty and adult attainment, behavior, and health. Child Dev. 2010;81(1):306–325. doi: 10.1111/j.1467-8624.2009.01396.x. [DOI] [PubMed] [Google Scholar]
- Ferris JS, Flom JD, Tehranifar P, Mayne ST, Terry MB. Prenatal and childhood environmental tobacco smoke exposure and age at menarche. Paediatr Perinat Epidemiol. 2010;24(6):515–523. doi: 10.1111/j.1365-3016.2010.01154.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Field AE, Coakley EH, Must A, Spadano JL, Laird N, Dietz WH, et al. Impact of overweight on the risk of developing common chronic diseases during a 10-year period. Archives of Internal Medicine. 2001;161(13):1581–1586. doi: 10.1001/archinte.161.13.1581. [DOI] [PubMed] [Google Scholar]
- Freid VM, Bernstein AB, Bush MA. Multiple chronic conditions among adults aged 45 and over: Trends over the past 10 years. National Center for Health Statistics; Hyattsville, MD: 2012. [PubMed] [Google Scholar]
- Gee GC, Walsemann KM, Brondolo E. A life course perspective on how racism may be related to health inequities. Am J Public Health. 2012;102(5):967–974. doi: 10.2105/AJPH.2012.300666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hardy JB. The Collaborative Perinatal Project: lessons and legacy. Ann Epidemiol. 2003;13(5):303–311. doi: 10.1016/s1047-2797(02)00479-9. [DOI] [PubMed] [Google Scholar]
- Hartman Catharina A., Hoogstraten Johan, Spruijt-Metz Donna. Disentangling Discrimination: Victim Characteristics as Determinants of the Perception of Behavior as Racist or Sexist. Journal of Applied Social Psychology. 1994;24(7):567–579. [Google Scholar]
- James-Todd T, Tehranifar P, Rich-Edwards J, Titievsky L, Terry MB. The impact of socioeconomic status across early life on age at menarche among a racially diverse population of girls. Ann Epidemiol. 2010;20(11):836–842. doi: 10.1016/j.annepidem.2010.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Mickelson KD, Williams DR. The prevalence, distribution, and mental health correlates of perceived discrimination in the United States. J Health Soc Behav. 1999;40(3):208–230. [PubMed] [Google Scholar]
- Kressin NR, Raymond KL, Manze M. Perceptions of race/ethnicity-based discrimination: a review of measures and evaluation of their usefulness for the health care setting. J Health Care Poor Underserved. 2008;19(3):697–730. doi: 10.1353/hpu.0.0041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krieger N. Racial and gender discrimination: risk factors for high blood pressure? Soc Sci Med. 1990;30(12):1273–1281. doi: 10.1016/0277-9536(90)90307-e. [DOI] [PubMed] [Google Scholar]
- Krieger N. Embodying inequality: a review of concepts, measures, and methods for studying health consequences of discrimination. Int J Health Serv. 1999;29(2):295–352. doi: 10.2190/M11W-VWXE-KQM9-G97Q. [DOI] [PubMed] [Google Scholar]
- Krieger N, Rowley DL, Herman AA, Avery B, Phillips MT. Racism, sexism, and social class: implications for studies of health, disease, and well-being. Am J Prev Med. 1993;9(6 Suppl):82–122. [PubMed] [Google Scholar]
- Krieger N, Smith K, Naishadham D, Hartman C, Barbeau EM. Experiences of discrimination: validity and reliability of a self-report measure for population health research on racism and health. Soc Sci Med. 2005;61(7):1576–1596. doi: 10.1016/j.socscimed.2005.03.006. [DOI] [PubMed] [Google Scholar]
- National Center for Environmental Health . Adult asthma data: prevalence, tables and maps - Behavioral Risk Factors Surveillance System (BRFSS) Prevalence Data 2010. National Center for Environmental Health; Atlanta, GA: [Accessed April 4, 2012]. 2010. ( http://www.cdc.gov/asthma/brfss/2010/lifetime/tableL21.htm) [Google Scholar]
- Office of Minority Health. Department of Health and Human Services . Diabetes Data/Statistics. Office of Minority Health; Washington, DC: [Accessed August 2, 2013]. 2012. ( http://minorityhealth.hhs.gov/templates/browse.aspx?lvl=3&lvlid=5) [Google Scholar]
- Office of Women’s Health. Department of Health and Human Services . Minority Women’s Health: Stroke. Office of Women’s Health; Washington, DC: [Accessed August 2, 2013]. 2010. ( http://www.womenshealth.gov/minority-health/african-americans/stroke.cfm) [Google Scholar]
- Paradies Y. A systematic review of empirical research on self-reported racism and health. Int J Epidemiol. 2006;35(4):888–901. doi: 10.1093/ije/dyl056. [DOI] [PubMed] [Google Scholar]
- Pascoe EA, Smart Richman L. Perceived discrimination and health: a meta-analytic review. Psychol Bull. 2009;135(4):531–554. doi: 10.1037/a0016059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearlin LI, Schieman S, Fazio EM, Meersman SC. Stress, health, and the life course: some conceptual perspectives. J Health Soc Behav. 2005;46(2):205–219. doi: 10.1177/002214650504600206. [DOI] [PubMed] [Google Scholar]
- Rowley Stephanie J., Helaire Lumas J., Banerjee Meeta. Reflecting on racism: School involvement and perceived teacher discrimination in African American mothers. Journal of Applied Developmental Psychology. 2010;31(1):83–92. [Google Scholar]
- Taylor Donald M., Wright Stephen C., Porter Lane E. Dimensions of perceived discrimination: The personal/group discrimination discrepency. In: Zanna MP, Olson JM, editors. The Pscohology of Prejudice: The Ontarion Symposium. Vol. 7. Lawrence Erlbaum Associates; Hillsdale, NJ: 1994. pp. 233–256. [Google Scholar]
- Taylor Jerome, Jackson Beryl B. Evaluation of a Holistic Model of Mental Health Symptoms in African American Women. Journal of Black Psychology. 1991;18(1):19–45. [Google Scholar]
- Tehranifar P, Liao Y, Flom JD, Terry MB. Validity of self-reported birth weight by adult women: sociodemographic influences and implications for life-course studies. Am J Epidemiol. 2009;170(7):910–917. doi: 10.1093/aje/kwp205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terry MB, Flom J, Tehranifar P, Susser E. The role of birth cohorts in studies of adult health: the New York women’s birth cohort. Paediatr Perinat Epidemiol. 2009;23(5):431–445. doi: 10.1111/j.1365-3016.2009.01061.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terry MB, Wei Y, Esserman D. Maternal, birth, and early-life influences on adult body size in women. Am J Epidemiol. 2007;166(1):5–13. doi: 10.1093/aje/kwm094. [DOI] [PubMed] [Google Scholar]
- Thom T, Haase N, Rosamond W, Howard VJ, Rumsfeld J, Manolio T, et al. Heart disease and stroke statistics--2006 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2006;113(6):e85–151. doi: 10.1161/CIRCULATIONAHA.105.171600. [DOI] [PubMed] [Google Scholar]
- Towfighi A, Zheng L, Ovbiagele B. Weight of the obesity epidemic: rising stroke rates among middle-aged women in the United States. Stroke. 2010;41(7):1371–1375. doi: 10.1161/STROKEAHA.109.577510. [DOI] [PubMed] [Google Scholar]
- Watson JM, Scarinci IC, Klesges RC, Slawson D, Beech BM. Race, socioeconomic status, and perceived discrimination among healthy women. J Womens Health Gend Based Med. 2002;11(5):441–451. doi: 10.1089/15246090260137617. [DOI] [PubMed] [Google Scholar]
- Williams DR, Mohammed SA. Discrimination and racial disparities in health: evidence and needed research. J Behav Med. 2009;32(1):20–47. doi: 10.1007/s10865-008-9185-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Spencer M, Jackson JS. Race Stress and Physical Health: The Role of Group Identity. In: Contrada RJ, Ashmore RD, editors. Self, Social Identity and Physical Health: Interdisciplinary Explorations. Oxford University Press; New York: 1999. pp. 71–100. [Google Scholar]
- Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159(7):702–706. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]