Abstract
Background
Small birth size - an indicator of a sub-optimal prenatal environment - and variation in growth after birth have been associated with non-communicable diseases in later life. We tested whether birth size or growth in childhood associated with the risk of hospital admission for alcohol use disorders (AUDs) from early to late adulthood.
Methods
The sample comprised 6544 men and 6050 women born between 1934 and 1944 in Helsinki, Finland. Data on anthropometric measures were extracted from medical records and diagnoses of AUD from the Finnish Hospital Discharge Register and Causes of Death Register covering a 40-year period from 1969 to 2008.
Results
Altogether 171 women (2.8%) and 657 men (10.0%) were diagnosed at a hospital with AUD. After adjusting for major confounders, shorter length at birth, shorter height up to two years of age, and lower weight at two years associated with hospitalization for AUD in women. In men, slower growth in height, particularly from 2 to 7 years, and slower weight gain from 7 to 11 years as well as shorter height and lower weight at 7 and 11 years associated with a diagnosis of AUD in men.
Conclusions
Pre- and postnatal growth associates with the risk for AUD later in life differently in women than in men: the fetal period and infancy seem to be the sensitive periods for women, whereas those for men the occur from toddlerhood onwards.
Introduction
In Western European societies, the lifetime prevalence of alcohol dependence is around 5% to 8% with rates four to five times higher for men than for women [1], [2]. Alcohol use ranks among the top causes of disease burden [3] and its impact in the developed world is projected to increase [4]. Since alcohol use can be an important causal factor in the development of a multitude of medical conditions [5], identifying early risk factors for alcohol use disorders (AUD) could help in preventive action.
Within the developmental origins of health and disease framework (DOHaD), the associations between small birth size or slower growth in childhood and health outcomes in later life have been attributed to suboptimal environmental conditions during sensitive time periods that alter the structure and function of key organs such as the brain [6]. These environmental conditions include psychosocial stress and malnutrition, which are amenable to intervention [6], [7].
Various non-communicable health conditions, such as hypertension and several psychiatric conditions, show high comorbidity with AUDs [5], [8]–[10] and have been linked to small body size at birth [7], [11]–[16] as well as growth patterns in childhood [7], [12], [15], [17], [18]. However, whether body size at birth or later in life associates with the risk for AUDs remains uncertain. In addition, the few existing studies show conflicting results and focus on those who were born at the extreme low end of the birth weight distribution [19]–[23] or on those who were obese in childhood [24]. Birth cohort studies have suggested that those born at the extreme low end of the birth weight distribution are at around 40% higher risk for alcohol abuse or substance-related disorders [19], [20] while one study showed an inverse gradient across decreasing birth weight [25]. Studies focusing on those born prematurely and with very low birth weight (<1500 grams; VLBW) suggest that VLBW is associated with less frequent alcohol consumption in young adulthood [21]–[23]. To our knowledge, no studies have examined the associations between body size or growth in childhood and subsequent AUDs in adulthood, and few studies point to such associations with respect to other psychiatric morbidity [24], [26], [27].
Our study aimed to investigate whether length of gestation, body size at birth and physical growth measured serially from birth to 11 years of age associate with hospitalization for or death due to AUDs in the Helsinki Birth Cohort Study (HBCS) sample. In addition to testing for linear effects, we examined whether nonlinear associations existed between birth size and hospitalization for AUDs. We also tested whether associations between physical growth and AUDs stem from comorbid mental disorders.
Materials and Methods
Subjects
The original study cohort comprised 13345 subjects who were born in Helsinki, Finland at one of the two public maternity hospitals, who visited child welfare clinics, and who received a Finnish personal ID number. Of these participants, we excluded 191 individuals because they moved abroad or died before data collection for the Finnish Hospital Discharge Register (HDR) began in 1969, 226 who were missing data on AUDs, and 334 who were missing data on childhood socioeconomic position (SEP). The cohort available for the analyses comprised 12 594 subjects (6544 men and 6050 women together comprising 94.3% of the original cohort). The excluded participants had an earlier year of birth (p<0.02), were more often women (p<0.004) and were lighter (p = 0.03) and thinner at birth (p<0.001), but showed no differences from the included participants in childhood SEP, length of gestation, placental weight, or length and head circumference at birth (p-values >0.05). Furthermore, 847 participants were excluded from the analysis of neonatal characteristics due to missing data on the length of gestation. The Ethics Committee of the National Public Health Institute and the Ethics Committee of the Helsinki and Uusimaa Hospital District approved the HBCS. The study has was conducted in adherence to the Declaration of Helsinki.
Measures of neonatal characteristics and physical growth
Data on year of birth, weight (g), length (cm), head circumference (cm), placental weight (g), and date of the mother's last menstrual period were collected from the birth records. Data on monthly changes in weight (kg) and height (cm) from birth to 2 years and annual changes from 2 to 11 years were estimated from child welfare clinic and school health records as described previously [28]. From these measures we calculated the ponderal index at birth (kg/m3) and body mass index (BMI: kg/m2).
Our primary indicator of SEP in childhood was occupational status of the father. These data were derived from school, child welfare clinic, and birth records (inferred from the last two, respectively, if data from school records were not available) and were classified as low SEP (manual workers: 62.3%), middle SEP (lower middle class: 22.6%), and high SEP (upper middle class: 15.2%). We used highest maternal SEP as secondary indicator of childhood socio-economic environment due to higher number of those belonging to unclassified category (e.g. housewives or students). Of the mothers, 50.9%, 34.2%, 3.8%, 11.1% belonged to low SEP, middle SEP, high SEP, and other/unclassified SEP, respectively [29].
Definition of hospitalization for alcohol use disorder (AUD) and of other mental disorders
Diagnoses were extracted from the HDR, which contained data on all hospitalizations in psychiatric and general hospitals in Finland between 1969 and 2008. The HDR also includes personal and hospital ID numbers, dates of hospital admission and discharge, and primary as well as up to three subsidiary diagnoses at discharge. The HDR is a valid and reliable tool for research [30], and studies have shown that diagnoses based on the HDR are more reliable than those based on medical examination or interview- or questionnaire-based measures, especially when a combined best-estimate diagnosis served as the validation criteria [31]. Accuracy of the HDR data with respect to AUDs proved high [32], and hospitalization for AUDs have served as an outcome in several studies [33], [34]. The HDR has also shown high validity with regard to psychotic disorders in general [31] and schizophrenia in particular [35]. We also identified AUDs as causes of death from the National Causes of Death-Register (CDR), which contains records of primary and subsidiary causes of death from all deaths in Finland.
Diagnoses were entered into the HDR and CDR according to the International Classification of Diseases, Eighth Revision (ICD-8) until 1986, according to the ICD-9 using the Diagnostic and Statistical Manual of Mental Disorders, Revised Third Edition (DSM-III-R) criteria until 1995, and according to the ICD-10 since 1996. In the current study, the primary diagnoses of alcohol intoxication (ICD-9: 3050A and ICD-10: F10.0) as well as the primary and subsidiary diagnoses of harmful alcohol use, alcohol dependence, and psychotic disorder due to alcohol abuse (ICD-8/9: 291, 303 and ICD-10 F10.1-F10.9) from either register served to index the AUDs. In our sample, we identified 746 and 34 AUD cases based solely on the HDR and CDR, respectively, and identified 48 based on both registers (6.6% of the total sample).
We examined the different AUDs together as one broad diagnostic outcome rather than as separate entities (such as alcohol dependence and harmful use of alcohol) to make our definition of AUDs more comparable with the definition of AUDs in the DSM-5, that was introduced in 2013. However, in correspondence with ICD-10, our definition of AUDs includes also the primary and subsidiary diagnoses of alcohol psychoses, amnesic syndrome due to alcohol use, and other and unspecified mental and behavioural disorders due to alcohol use, and the primary diagnoses of alcohol intoxification.
The primary and up to three subsidiary diagnoses of mental disorders other than those due to alcohol use were drawn with the following codes: 295–302, 304–305, 306.4–306.5, 306.8, 306.98, and 307 from ICD-8; 292, 295–298, 300–302, 304, 3051–3059, 3071A, 3074, 3075A–3075B, 3078A, 3079X, 3090A, 3092C–3099X, and 312 from ICD-9; and F11–F69 from ICD-10 [36].
Statistical analyses
First, we used logistic regression analyses to test whether neonatal characteristics and body size or growth from birth to age 11 were associated with hospitalization for AUDs in adulthood. We tested for nonlinear associations between birth size and hospitalization for AUDs using a model that included a squared term of the variable centered around the grand mean together with a non-squared linear variable. We focused on measurements conducted at birth, at 6 months of age, and at 1, 2, 7, and 11 years of age to represent growth in the prenatal period (at birth), in infancy (up to 2 years), and in childhood (up to 11 years). Physical size measurements served as continuous variables to test for linear and nonlinear associations. All the neonatal characteristics and the measures on attained size at different ages were converted to z-scores by sex. Postnatal growth variables were standardized residuals from linear regression models of weight, height, and BMI where body size at each point in time was regressed on corresponding measures at all earlier points in time, creating completely uncorrelated residuals reflecting growth conditional on history (i.e. conditional growth) [37]. In Model 1, we adjusted for year of birth and SEP in childhood in all analyses, and in analyses of birth size, we further adjusted for length of gestation. In Model 2, we further adjusted for maternal SEP. To test whether associations between physical growth and AUDs are attributable to comorbid mental disorders, in Model 3 we adjusted for other mental disorders in addition to those variables in Model 1. In addition, we reran all the Model 1 analyses in a sample comprising only those with any mental disorder (i.e. contrasting those with AUDs to those with other mental disorders).
Although we found no statistically significant interactions between body size or growth by sex (p-values for interactions >0.08), we conducted all the analyses separately for men and women, since previous studies have found major sex differences in the prevalence of AUDs [2] and in factors influencing alcohol use [38] as well as sex-specific associations between body size or growth and mental disorders [11], [24], [26], [27], [39]–[47].
Results
Table 1 presents neonatal and adulthood characteristics according to sex. In men, low childhood SEP associated with 46.1% higher odds (95% Confidence Interval [CI] 11.4–86.6%, p = 0.002) for AUDs than for high childhood SEP. We found no associations between childhood SEP and AUDs in women (p>0.54).
Table 1. Characteristics of the sample.
| Characteristic | Males | Females | ||
| N | Mean (SD) | N | Mean (SD) | |
| At Birth: | ||||
| Weight (kg) | 6544 | 3.5 (0.5) | 6050 | 3.3 (0.5) # |
| Length (cm) | 6490 | 50.6 (1.9) | 5995 | 49.9 (1.8) # |
| Body Mass Index (kg/m2) | 6484 | 13.5 (1.2) | 5992 | 13.4 (1.2) # |
| Ponderal index (kg/m3) | 6490 | 26.7 (2.2) | 5995 | 26.8 (2.2) |
| Head circumference (cm) | 6474 | 35.3 (1.5) | 5988 | 34.7 (1.4) # |
| Gestational age (days) | 6420 | 279.0 (14.3) | 5935 | 279.7 (13.7)# |
| Placental weight (g) | 6520 | 651.2 (119.9) | 6040 | 639.2 (118.9)# |
| At age 6 months: | ||||
| Height (cm) | 6534 | 67.8 (2.3) | 6043 | 66.1 (2.3) # |
| Weight (kg) | 6539 | 7.9 (0.9) | 6049 | 7.4 (0.8) # |
| Body Mass Index (kg/m2) | 6535 | 17.2 (1.4) | 6045 | 16.8 (1.4) # |
| At age 1 year: | ||||
| Height (cm) | 6534 | 76.5 (2.6) | 6043 | 74.8 (2.6) # |
| Weight (kg) | 6539 | 10.5 (1.1) | 6049 | 9.8 (1.0) # |
| Body Mass Index (kg/m2) | 6535 | 17.9 (1.4) | 6045 | 17.5 (1.4) # |
| At age 2 years: | ||||
| Height (cm) | 6536 | 86.6 (3.2) | 6044 | 85.5 (3.2) # |
| Weight (kg) | 6542 | 12.4 (1.2) | 6049 | 11.9 (1.2) # |
| Body Mass Index (kg/m2) | 6538 | 16.7 (1.2) | 6046 | 16.4 (1.2) # |
| At age 7 years: | ||||
| Height (cm) | 4909 | 120.7 (4.9) | 4521 | 119.9 (4.8) # |
| Weight (kg) | 4917 | 22.5 (2.7) | 4527 | 22.2 (2.9) # |
| Body Mass Index (kg/m2) | 4903 | 15.5 (1.1) | 4512 | 15.5 (1.2) |
| At age 11 years: | ||||
| Height (cm) | 4814 | 141.3 (6.0) | 4409 | 141.4 (6.4) |
| Weight (kg) | 4817 | 33.6 (4.6) | 4407 | 34.3 (5.7) # |
| Body Mass Index (kg/m2) | 4809 | 16.8 (1.5) | 4403 | 17.1 (1.9) # |
| Father's SEP | * | |||
| Low | 4022 (61.5%) | 3819 (63.1%) | ||
| Middle | 1469 (22.4%) | 1372 (22.7%) | ||
| High | 1053 (16.1%) | 859 (14.2%) | ||
| Mother's SEP | ||||
| Low | 3290 (56.4%) | 3120 (58.2%) | ||
| Middle | 2299 (39.4%) | 2008 (37.4%) | ||
| High | 247 (4.2%) | 234 (4.4%) | ||
| Other (e.g.housewives) | 708 (10.8%) | 688 (11.4%) | ||
| In adulthood | ||||
| Hospitalization for alcohol use disorders (yes) | 657 (10.0%) | 171 (2.8%) # | ||
| Hospitalization for other mental disorders (yes) | 565 (8.6%) | 506 (8.4%) | ||
: p<0.05; #: p<0.001.
Neonatal characteristics and hospitalization for AUDs
Table 2 shows that after adjusting for birth year, SEP in childhood and length of gestation, shorter length at birth increased the risk of hospitalization for AUDs linearly (p = 0.03) among women, and birth weight also shows a similar trend (p = 0.054). The ponderal index and head circumference at birth showed no association with the risk of hospitalization for AUDs in women (p-values>0.17; data not shown). Birth size showed nonlinear associations with the risk of hospitalization for AUDs in women (p-values >0.25). In men, we found neither linear (p-values >0.11) nor nonlinear (p-values >0.054) associations between body size at birth and the risk of hospitalization for AUDs. These associations are further illustrated in Figure 1. Moreover, we found no associations between gestational age and AUDs in men (linear: Odd's Ratio [OR] = 1.04, 95% CI = 0.95 to 1.12, p = 0.39; non-linear: OR = 1.03, 95% CI = 0.98 to 1.09, p = 0.30) or in women (linear: OR = 1.03, 95% CI = 0.88 to 1.21, p = 0.70; non-linear: OR = 1.01, 95% CI = 0.91 to 1.13, p = 0.80). Further adjusting for maternal SEP (Model 2) or comorbid mental disorders (Model 3) changed none of the significance levels (Table 2), but restricting the sample to those with mental disorders rendered non-significant all associations between neonatal characteristics and AUDs in women (p-values >0.09) and in men (p-values >0.25).
Table 2. Odd's ratio (OR) of hospitalization for alcohol use disorders according to the decrease in standardized weight, length/height, and BMI from birth to 11 years of age.
| Men | Women | ||||||||||||||
| Model 1 | Model 2 | Model 3 | Model 1 | Model 2 | Model 3 | ||||||||||
| N | OR | 95% CI | p | p | p | p | N | OR | 95% CI | p | p | p | |||
| Height/Length | |||||||||||||||
| Birth | 6055 | 1.02 | 0.93 | 1.12 | 0.72 | 0.77 | 0.66 | Birth | 5609 | 1.22 | 1.02 | 1.46 | 0.03 | 0.03 | 0.05 |
| 6 months | 6534 | 1.02 | 0.94 | 1.11 | 0.57 | 0.57 | 0.61 | 6 months | 6043 | 1.18 | 1.02 | 1.38 | 0.03 | 0.03 | 0.05 |
| 1 year | 6534 | 1.04 | 0.96 | 1.12 | 0.40 | 0.39 | 0.50 | 1 year | 6043 | 1.20 | 1.03 | 1.40 | 0.02 | 0.02 | 0.02 |
| 2 years | 6536 | 1.08 | 0.99 | 1.17 | 0.07 | 0.07 | 0.11 | 2 years | 6044 | 1.22 | 1.05 | 1.42 | 0.01 | 0.01 | 0.01 |
| 7 years | 4909 | 1.13 | 1.03 | 1.24 | 0.01 | 0.02 | 0.03 | 7 years | 4521 | 1.12 | 0.95 | 1.33 | 0.18 | 0.21 | 0.30 |
| 11 years | 4814 | 1.14 | 1.04 | 1.26 | 0.01 | 0.01 | 0.01 | 11 years | 4409 | 1.07 | 0.90 | 1.27 | 0.44 | 0.49 | 0.64 |
| Weight | |||||||||||||||
| Birth | 6094 | 1.06 | 0.97 | 1.17 | 0.21 | 0.25 | 0.18 | Birth | 5653 | 1.19 | 1.00 | 1.42 | 0.05 | 0.06 | 0.05 |
| 6 months | 6539 | 1.03 | 0.95 | 1.11 | 0.55 | 0.55 | 0.88 | 6 months | 6049 | 1.16 | 1.00 | 1.35 | 0.06 | 0.06 | 0.07 |
| 1 year | 6539 | 1.04 | 0.96 | 1.13 | 0.32 | 0.33 | 0.44 | 1 year | 6049 | 1.13 | 0.97 | 1.32 | 0.11 | 0.12 | 0.13 |
| 2 years | 6542 | 1.07 | 0.99 | 1.16 | 0.10 | 0.11 | 0.14 | 2 years | 6049 | 1.19 | 1.02 | 1.50 | 0.02 | 0.03 | 0.02 |
| 7 years | 4917 | 1.10 | 1.00 | 1.20 | 0.05 | 0.07 | 0.09 | 7 years | 4527 | 1.13 | 0.95 | 1.34 | 0.16 | 0.18 | 0.23 |
| 11 years | 4817 | 1.13 | 1.03 | 1.24 | 0.01 | 0.01 | 0.03 | 11 years | 4407 | 1.07 | 0.90 | 1.26 | 0.46 | 0.49 | 0.75 |
| BMI | |||||||||||||||
| Birth | 6049 | 1.07 | 0.98 | 1.17 | 0.13 | 0.16 | 0.11 | Birth | 5606 | 1.12 | 0.95 | 1.33 | 0.17 | 0.18 | 0.15 |
| 6 months | 6535 | 1.01 | 0.93 | 1.10 | 0.81 | 0.83 | 0.87 | 6 months | 6045 | 1.05 | 0.90 | 1.23 | 0.51 | 0.51 | 0.50 |
| 1 year | 6535 | 1.02 | 0.94 | 1.10 | 0.66 | 0.69 | 0.56 | 1 year | 6045 | 0.99 | 0.85 | 1.15 | 0.87 | 0.86 | 0.85 |
| 2 years | 6538 | 1.03 | 0.95 | 1.11 | 0.51 | 0.55 | 0.49 | 2 years | 6046 | 1.04 | 0.89 | 1.21 | 0.65 | 0.66 | 0.55 |
| 7 years | 4903 | 1.01 | 0.92 | 1.11 | 0.84 | 0.88 | 0.88 | 7 years | 4512 | 1.05 | 0.88 | 1.24 | 0.61 | 0.61 | 0.56 |
| 11 years | 4809 | 1.05 | 0.95 | 1.15 | 0.35 | 0.35 | 0.50 | 11 years | 4403 | 1.02 | 0.86 | 1.21 | 0.79 | 0.79 | 0.97 |
CI: Confidence interval. All models are adjusted for year of birth and socioeconomic position in childhood, and models pertaining to body size at birth are also adjusted for gestational age (Model 1). In addition to those variables in Model 1, Model 2 and Model 3 are adjusted for maternal socioeconomic position or other mental disorders, respectively.
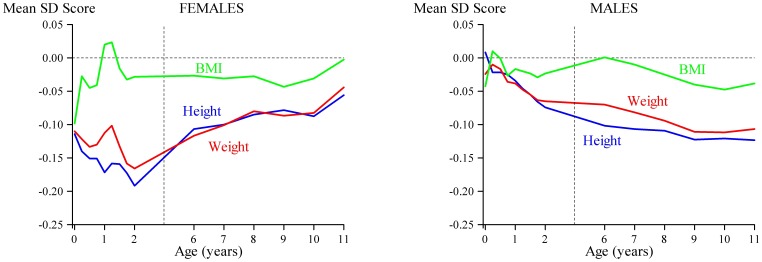
Figure 1. Trajectories of height (blue line), weight (red line), and BMI (green line) in those who were hospitalized for alcohol use disorder in adulthood.
The mean values for height, weight and BMI of the monthly measures from birth to 2 years, and the yearly measures from 6 to 11 years, are set at zero with deviations from the mean expressed as standard deviations (z scores).
Body size and conditional growth after birth and hospitalization for AUDs
Table 2 also shows that after adjusting for birth year and SEP in childhood, increased risk of hospitalization for AUDs was associated with shorter height from six months to two years in women (p-values<0.03). Moreover, in women, lower weight at two years increased the risk of hospitalization for AUDs (p = 0.02), and weight at six months showed a similar trend (p = 0.057). In men, shorter height and lower weight at 7 and 11 years associated with increased risk of hospitalization for AUDs (p-values<0.05; Figure 1). Further adjusting for maternal SEP (Model 2) or comorbid mental disorders (Model 3) did not change the significance levels (Table 2), except for one: in men, the association between lower weight at seven years and AUDs became non-significant in both models (p-values >0.07). Restricting the sample to those with mental disorders had no effect on the significance levels of the associations between body size after birth and AUDs in women (p-values<0.04), whereas in men, it rendered all associations non-significant (p-values >0.21).
We then tested whether growth conditional on history associated with hospitalization for AUDs. Among men we found that after adjusting for birth year and SEP in childhood, hospitalization for AUDs was associated with slower growth in height from two to seven years (OR = 1.10, 95% CI = 1.00 to 1.22, p = 0.048) and with slower weight gain from seven to 11 years (OR = 1.12, 95% CI = 1.01 to 1.23, p = 0.03), while weight gain from two to seven years showed a similar trend (OR = 1.10, 95% CI = 1.00 to 1.21, p = 0.06). We found no significant associations between growth conditional on history and AUDs in women. Further adjusting for maternal SEP (Model 2) or comorbid mental disorders (Model 3) yielded only one change in significance levels: in men, slower growth in height from two to seven years became non-significant (Model 2: OR = 1.1, 95% CI = 1.00 to 1.22, p = 0.06; and Model 3: OR = 1.09, 95% CI = 1.00 to 1.21, p = 0.09). Restricting the sample to those with mental disorders rendered all significant associations non-significant (p-values >0.19).
Discussion
We explored whether length of gestation and body size or physical growth up to 11 years of age associated with hospitalization for AUDs in adulthood in 12594 women and men participating in the Helsinki Birth Cohort Study. Different growth periods were associated with increased risk for AUDs in both women and men. After adjusting for gestational age, birth year, and SEP in childhood, shorter length at birth associated linearly with increased risk of hospitalization for AUDs in women. This association was unattributable to maternal SEP or comorbid other mental disorders, although restricting the sample to those with any mental disorders rendered the association non-significant. AUDs showed no association with growth after birth, although women who were hospitalized for AUDs remained on average shorter up to two years of age, and weighed less at two years of age. These results were unattributable to maternal SEP or comorbid mental disorders. In men, birth characteristics showed no association with the risk for AUDs. However, men who were hospitalized because of AUDs had slower growth in height between two and seven years of age; they also gained less weight from seven to 11 years and, as a consequence, were shorter and weighed less at age 7 and 11 years. Similar findings related to weight and height are likely the result of slower growth in height, as there was no relationship with BMI in childhood. In men, maternal SEP or comorbid mental disorders had little effect on these associations, but restricting the sample to those with any mental disorders rendered the associations non-significant.
These results are in line with those of previous studies on population-based birth cohorts that have shown an inverse gradient between birth weight and substance-related disorders in young adulthood [25], and increased risk for AUDs [19] or substance-related disorders [20], [25]_ENREF_15 in those who were born with low birth weight [19] or were small for their gestational age [20], [25]. Our results add the previous literature by showing not only that the associations extend beyond birth weight, but also that slower intrauterine skeletal growth seemed to play a role in increasing the risk of hospitalization for AUDs in adulthood. Furthermore, the follow-up periods in previous research extend only into young adulthood, while our findings show that the effects persist across several decades into older adulthood. Our findings disagree with those found in young adults born prematurely: in previous studies, those born at VLBW reported less frequent heavy alcohol use or lower consumption of alcohol than did their peers born at term [21], [22]. However, these findings may be limited to those born the smallest and most immature, who were unlikely to survive when the subjects in the present cohort were born. As in this study, previous research has also shown that associations of birth size with mental health vary between men and women: some studies have reported stronger inverse associations between birth weight and emotional or attention problems in women than in men [40]–[43], while other studies show links between lower birth weight and depression in men, but not in women [44]–[47].
To the best of our knowledge, this study is the first to explore body size or physical growth in childhood with respect to AUDs in adulthood; consequently, the current findings cannot be directly compared to the previous ones. Cross-sectional studies on associations between body size and psychiatric morbidity show conflicting results, with some linking obesity with psychiatric problems [26], [48]–[51], and others showing no association [52] or an inverse association between BMI and mental disorders [53], [54]. Longitudinal studies suggest sex-specificity in associations between childhood body size or physical growth and psychiatric morbidity in later life [24], [26], [27]. In girls, but not in boys, higher BMI and gain in BMI in childhood linked with anxiety disorders and depression in adulthood [26]. Moreover, chronic obesity in childhood increased the risk for depression in adolescence only in boys, but for oppositional disorder in both sexes [24]. Another study also found no association between childhood overweight and subsequent depression [52]. Furthermore, still other studies have shown that these associations may be not only sex-specific, but also specific to a particular growth period. Physical growth in infancy and in childhood show different patterns with respect to risk of hospitalization for personality disorders in adulthood in both boys and girls [27]. Thus, some of the inconsistencies in the findings may stem from a lack of physical growth data on specific age periods.
Our finding that restricting the sample to those with mental disorders attenuated many of the associations is in line with earlier findings that smaller birth size associates with a wide range of mental disorders [25] and may therefore be considered a marker more for overall vulnerability than for a specific disorder. However, our findings that in women shorter height in early childhood and lower weight at two years associated with increased risk of hospitalization for AUDs after adjusting for other mental disorders and after restricting the sample to those with any mental disorder, suggest that these associations may be more specific and confined to AUDs.
Our results cannot determine the biological and psychosocial mechanisms that underlie the associations between smaller body size and the risk for AUDs. The DOHaD framework postulates that these conditions may relate to environmental psychosocial stress and/or malnutrition that alter the structure and function of the brain [6], [7]. Indeed, in animal studies, prenatal stress [55], [56] and the prenatal administration of synthetic glucocorticoids [57], probably mediated via hypothalamic pituitary adrenocortical (HPA) axis activity, have associated with a variety of alterations in hormonal axes, in monoamine neurotransmission, and in the morphology of the offspring [56]. In addition, human studies have linked several indicators of extreme small birth size with structural or functional alterations in the brain. Greater birth weight within the normal range was recently linked with generalized increase in brain volume, which in the cortical sheet, seems to be driven by increased surface area [58] as well as with increase in the volume of several striatal areas [59]. Similar results were found in monozygotic twins, suggesting that environmental factors underlie these associations [58], and in singletons [59]. Intrauterine growth retardation has been linked with metabolic disturbances in brain serotonin synthesis [60], low birth weight with increased lateral ventricular volume [61], and preterm birth with a smaller hippocampus [62], [63]. Moreover, a recent meta-analysis showed children who were very premature and/or of very low birth weight to have significantly smaller total brain volume than term-born comparison group, less white and grey matter volume, and smaller cerebellum, hippocampus, and corpus callosum [64]. Roza et al. [65] showed that reduced fetal growth in head circumference and biparietal diameter predicted lower ventricular volume in infancy. Interestingly, previous studies have implicated serotonin genes in alcohol dependence [66] and have linked alcohol use with alterations in HPA axis activity [67] and hippocampal volume [68] in adolescents.
Our findings suggest that sensitive periods with respect to the risk for AUDs may differ for men and women. Exposures in utero and in infancy may have greater effects for women, whereas for men, the sensitive periods occur later, from toddlerhood onwards. Consistent with these results, exposure to prenatal stress associated with larger alterations in monoamine neurotransmission [69] and HPA axis function [70], and increased anxiety-like behaviors [71] in female animals, whereas males exhibited more learning deficits [71].
The strengths of our study are its longitudinal study design, its relatively large sample of participants derived from the general population, and its use of comprehensive register data. Moreover, we measured growth at several points in time, which permitted us to track critical periods of growth with respect to subsequent AUDs. Our study also has its limitations. First, we have no data on parental mental disorders or risk behaviors such as alcohol use or smoking. Since smoking or alcohol use during pregnancy may increase the risk for small birth size [72] as well as the risk for psychiatric disorders in the offspring [73], [74], the associations observed may have resulted from prenatal exposures. Moreover, the lack of data on parental alcohol use after birth for our sample precluded us from investigating and accounting for the role of social learning in the development of AUDs. Second, our data on diagnoses were based on hospital records and not everyone with AUD requires hospitalization. Moreover, the HDR data do not cover the years between 1934 and 1969. Consequently, participants with AUDs may have had severe disorders, so our results may not be generalized to less severe disorders. However, the proportion of participants in our sample diagnosed with AUDs (6.6%) is only slightly lower than the lifetime prevalence of 7.9% reported recently in a population-based sample of Finns over 30 years of age [1]. Third, although our participants correspond to 94.3% of the original cohort, one limitation of the external validity of our findings is that they do not include those who died or emigrated before assignment of personal ID numbers and those who did not attend free-of-charge, voluntary child welfare clinics. Moreover, loss to follow-up is inevitable. Compared with the original cohort, participation was unrelated to childhood SEP, length of gestation, placental weight, or length and head circumference at birth, but the participants of this study were born later, were more often men, and tended to be heavier at birth. These differences could, however, introduce bias only if the associations between growth and AUDs in people included in the sample differed from such associations in those who were not. Furthermore, one should be cautious about generalizing our findings to people living in other types of societies or to those born in later decades.
In summary, the associations between anthropometric traits, indicators of the prenatal and childhood nutritional and psychosocial environment, and AUDs showed differences between women and men: shorter length/height at birth and in infancy in girls and in childhood in boys, associated with increased risk for AUDs in later life.
Acknowledgments
Professor Barker (now deceased) contributed actively to the design of this study, to discussion of the interpretation of the results, and he saw drafts up to the latest Researchers interested in using HBCS data must obtain approval from the Steering Committee of the Helsinki Birth Cohort Study. Researchers using the data are required to follow the terms in a number of clauses designed to ensure protection of privacy and compliance with relevant Finnish laws. For further information, contact Johan Eriksson (johan.eriksson@helsinki.fi).
Funding Statement
Funding for this study was provided by the Academy of Finland, Doctoral Programme of Psychology, Alfred Kordelin foundation, Ella and Georg Ehrnrooths Stiftelse, and Yrjö Jahnsson Foundation. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Pirkola SP, Poikolainen K, Lönnqvist JK (2006) Currently active and remitted alcohol dependence in a nationwide adult general population–results from the Finnish Health 2000 study. Alcohol Alcohol 41: 315–320. [DOI] [PubMed] [Google Scholar]
- 2. Bijl RV, Ravelli A, van Zessen G (1998) Prevalence of psychiatric disorder in the general population: results of The Netherlands Mental Health Survey and Incidence Study (NEMESIS). SocPsychiatry PsychiatrEpidemiol 33: 587–595. [DOI] [PubMed] [Google Scholar]
- 3. Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJ (2006) Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data. Lancet 367: 1747–1757. [DOI] [PubMed] [Google Scholar]
- 4. Murray CJ, Lopez AD (1997) Alternative projections of mortality and disability by cause 1990-2020: Global Burden of Disease Study. Lancet 349: 1498–1504. [DOI] [PubMed] [Google Scholar]
- 5. Rehm J, Room R, Graham K, Monteiro M, Gmel G, et al. (2003) The relationship of average volume of alcohol consumption and patterns of drinking to burden of disease: an overview. Addiction 98: 1209–1228. [DOI] [PubMed] [Google Scholar]
- 6. Gillman MW (2005) Developmental origins of health and disease. New England Journal of Medicine 353: 1848–1850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Barker DJ (2004) The developmental origins of chronic adult disease. Acta Paediatrica Supplement 93: 26–33. [DOI] [PubMed]
- 8. Ohlmeier MD, Peters K, Te Wildt BT, Zedler M, Ziegenbein M, et al. (2008) Comorbidity of alcohol and substance dependence with attention-deficit/hyperactivity disorder (ADHD). Alcohol Alcohol 43: 300–304. [DOI] [PubMed] [Google Scholar]
- 9. Green AI, Brown ES (2006) Comorbid schizophrenia and substance abuse. J Clin Psychiatry 67: e08. [PubMed] [Google Scholar]
- 10. Trull TJ, Jahng S, Tomko RL, Wood PK, Sher KJ (2010) Revised Nesarc Personality Disorder Diagnoses: Gender, Prevalence, and Comorbidity with Substance Dependence Disorders. J Pers Disord 24: 412–426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Costello EJ, Worthman C, Erkanli A, Angold A (2007) Prediction from low birth weight to female adolescent depression: a test of competing hypotheses. Archives of General Psychiatry 64: 338–344. [DOI] [PubMed] [Google Scholar]
- 12. Lahti J, Räikkönen K, Pesonen AK, Heinonen K, Kajantie E, et al. (2009) Prenatal growth, postnatal growth and trait anxiety in late adulthood - the Helsinki Birth Cohort Study. Acta Psychiatr Scand 121: 227–235. [DOI] [PubMed] [Google Scholar]
- 13. Lahti J, Räikkönen K, Sovio U, Miettunen J, Hartikainen AL, et al. (2009) Early-life origins of schizotypal traits in adulthood. Br J Psychiatry 195: 132–137. [DOI] [PubMed] [Google Scholar]
- 14. Lahti J, Raikkonen K, Kajantie E, Heinonen K, Pesonen AK, et al. (2006) Small body size at birth and behavioural symptoms of ADHD in children aged five to six years. J Child Psychol Psychiatry 47: 1167–1174. [DOI] [PubMed] [Google Scholar]
- 15. Wahlbeck K, Forsen T, Osmond C, Barker DJ, Eriksson JG (2001) Association of schizophrenia with low maternal body mass index, small size at birth, and thinness during childhood. Archives of General Psychiatry 58: 48–52. [DOI] [PubMed] [Google Scholar]
- 16. Lahti M, Räikkönen K, Wahlbeck K, Heinonen K, Forsen T, et al. (2010) Prenatal origins of hospitalization for personality disorders: the Helsinki birth cohort study. Psychiatry Res 179: 226–230. [DOI] [PubMed] [Google Scholar]
- 17. Schlotz W, Phillips DI (2009) Fetal origins of mental health: evidence and mechanisms. Brain Behav Immun 23: 905–916. [DOI] [PubMed] [Google Scholar]
- 18. Räikkönen K, Pesonen AK, Roseboom TJ, Eriksson JG (2012) Early determinants of mental health. Best Pract Res Clin Endocrinol Metab 26: 599–611. [DOI] [PubMed] [Google Scholar]
- 19. Osler M, Kriegbaum M, Christensen U, Holstein B, Nybo Andersen AM (2008) Rapid report on methodology: does loss to follow-up in a cohort study bias associations between early life factors and lifestyle-related health outcomes? AnnEpidemiol 18: 422–424. [DOI] [PubMed] [Google Scholar]
- 20. Gustafsson WM, Josefsson K, Selling KE, Sydsjö G (2009) Preterm birth or foetal growth impairment and psychiatric hospitalization in adolescence and early adulthood in a Swedish population-based birth cohort. Acta Psychiatrica Scandinavica 119: 54–61. [DOI] [PubMed] [Google Scholar]
- 21. Cooke RW (2004) Health, lifestyle, and quality of life for young adults born very preterm. ArchDisChild 89: 201–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Strang-Karlsson S, Räikkönen K, Pesonen AK, Kajantie E, Paavonen EJ, et al. (2008) Very low birth weight and behavioral symptoms of attention deficit hyperactivity disorder in young adulthood: the helsinki study of very-low-birth-weight adults. AmJPsychiatry 165: 1345–1353. [DOI] [PubMed] [Google Scholar]
- 23. Hallin AL, Stjernqvist K (2011) Adolescents born extremely preterm: behavioral outcomes and quality of life. Scand J Psychol 52: 251–256. [DOI] [PubMed] [Google Scholar]
- 24. Mustillo S, Worthman C, Erkanli A, Keeler G, Angold A, et al. (2003) Obesity and psychiatric disorder: developmental trajectories. Pediatrics 111: 851–859. [DOI] [PubMed] [Google Scholar]
- 25. Abel KM, Wicks S, Susser ES, Dalman C, Pedersen MG, et al. (2010) Birth weight, schizophrenia, and adult mental disorder: is risk confined to the smallest babies? Arch Gen Psychiatry 67: 923–930. [DOI] [PubMed] [Google Scholar]
- 26. Anderson SE, Cohen P, Naumova EN, Must A (2006) Association of depression and anxiety disorders with weight change in a prospective community-based study of children followed up into adulthood. ArchPediatrAdolescMed 160: 285–291. [DOI] [PubMed] [Google Scholar]
- 27. Lahti M, Räikkönen K, Wahlbeck K, Heinonen K, Forsen T, et al. (2011) Growth in infancy and childhood and hospitalization for personality disorders in adulthood: the Helsinki Birth Cohort Study. J Pers Disord 25: 620–633. [DOI] [PubMed] [Google Scholar]
- 28. Osmond C, Kajantie E, Forsen TJ, Eriksson JG, Barker DJP (2007) Infant growth and stroke in adult life the Helsinki birth cohort study. Stroke 38: 264–270. [DOI] [PubMed] [Google Scholar]
- 29.Mikkonen M, Salonen MK, Häkkinen A, Pesonen AK, Räikkönen K, et al. (submitted) Mother's marital status and offspring's socio-economic status in adulthood - the Helsinki Birth Cohort Study 1934–11944.
- 30. Keskimäki I, Aro S (1991) Accuracy of data on diagnoses, procedures and accidents in the Finnish Hospital Discharge Register. Int J Health Serv 2: 15–21. [Google Scholar]
- 31. Perälä J, Suvisaari J, Saarni SI, Kuoppasalmi K, Isometsä E, et al. (2007) Lifetime prevalence of psychotic and bipolar I disorders in a general population. ArchGenPsychiatry 64: 19–28. [DOI] [PubMed] [Google Scholar]
- 32. Poikolainen K (1983) Accuracy of hospital discharge data: five alcohol-related diseases. Drug Alcohol Depend 12: 315–322. [DOI] [PubMed] [Google Scholar]
- 33. Veijola J, Laara E, Joukamaa M, Isohanni M, Hakko H, et al. (2008) Temporary parental separation at birth and substance use disorder in adulthood. A long-term follow-up of the Finnish Christmas Seal Home Children. Soc Psychiatry Psychiatr Epidemiol 43: 11–17. [DOI] [PubMed] [Google Scholar]
- 34. Mäkelä P, Paljärvi T (2008) Do consequences of a given pattern of drinking vary by socioeconomic status? A mortality and hospitalisation follow-up for alcohol-related causes of the Finnish Drinking Habits Surveys. J Epidemiol Community Health 62: 728–733. [DOI] [PubMed] [Google Scholar]
- 35. Mäkikyrö T, Isohanni K, Moring J, Hakko H, Lönnqvist J (1998) Accuracy of register-based schizophrenia diagnoses in a genetic study. Eur Psychiatry 13: 57–62. [DOI] [PubMed] [Google Scholar]
- 36. Räikkönen K, Lahti M, Heinonen K, Pesonen AK, Wahlbeck K, et al. (2011) Risk of severe mental disorders in adults separated temporarily from their parents in childhood: the Helsinki birth cohort study. J Psychiatr Res 45: 332–338. [DOI] [PubMed] [Google Scholar]
- 37. Barker DJ, Osmond C, Forsen TJ, Kajantie E, Eriksson JG (2005) Trajectories of growth among children who have coronary events as adults. N Engl J Med 353: 1802–1809. [DOI] [PubMed] [Google Scholar]
- 38. Schulte MT, Ramo D, Brown SA (2009) Gender differences in factors influencing alcohol use and drinking progression among adolescents. Clin Psychol Rev 29: 535–547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Perrin MA, Chen H, Sandberg DE, Malaspina D, Brown AS (2007) Growth trajectory during early life and risk of adult schizophrenia. Br J Psychiatry 191: 512–520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. O'Keeffe MJ, O'Callaghan M, Williams GM, Najman JM, Bor W (2003) Learning, cognitive, and attentional problems in adolescents born small for gestational age. Pediatrics 112: 301–307. [DOI] [PubMed] [Google Scholar]
- 41. Hack M, Youngstrom EA, Cartar L, Schluchter M, Taylor HG, et al. (2004) Behavioral outcomes and evidence of psychopathology among very low birth weight infants at age 20 years. Pediatrics 114: 932–940. [DOI] [PubMed] [Google Scholar]
- 42. Alati R, Lawlor DA, Mamun AA, Williams GM, Najman JM, et al. (2007) Is there a fetal origin of depression? Evidence from the Mater University Study of Pregnancy and its outcomes. AmJEpidemiol 165: 575–582. [DOI] [PubMed] [Google Scholar]
- 43. Rice F, Jones I, Thapar A (2007) The impact of gestational stress and prenatal growth on emotional problems in offspring: a review. Acta Psychiatr Scand 115: 171–183. [DOI] [PubMed] [Google Scholar]
- 44. Kelly YJ, Nazroo JY, McMunn A, Boreham R, Marmot M (2001) Birthweight and behavioural problems in children: a modifiable effect? International Journal of Epidemiology 30: 88–94. [DOI] [PubMed] [Google Scholar]
- 45. Thompson C, Syddall H, Rodin I, Osmond C, Barker DJ (2001) Birth weight and the risk of depressive disorder in late life. British Journal of Psychiatry 179: 450–455. [DOI] [PubMed] [Google Scholar]
- 46. Wiles NJ, Peters TJ, Leon DA, Lewis G (2005) Birth weight and psychological distress at age 45-51 years: results from the Aberdeen Children of the 1950s cohort study. British Journal of Psychiatry 187: 21–28. [DOI] [PubMed] [Google Scholar]
- 47. Schlotz W, Jones A, Phillips NM, Godfrey KM, Phillips DI (2007) Size at birth and motor activity during stress in children aged 7 to 9 years. Pediatrics 120: e1237–1244. [DOI] [PubMed] [Google Scholar]
- 48. Lumeng JC, Gannon K, Cabral HJ, Frank DA, Zuckerman B (2003) Association between clinically meaningful behavior problems and overweight in children. Pediatrics 112: 1138–1145. [DOI] [PubMed] [Google Scholar]
- 49. Bjerkeset O, Romundstad P, Evans J, Gunnell D (2008) Association of adult body mass index and height with anxiety, depression, and suicide in the general population: the HUNT study. AmJEpidemiol 167: 193–202. [DOI] [PubMed] [Google Scholar]
- 50. Becker ES, Margraf J, Turke V, Soeder U, Neumer S (2001) Obesity and mental illness in a representative sample of young women. IntJObesRelat Metab Disord 25 Suppl 1S5–S9. [DOI] [PubMed] [Google Scholar]
- 51. Simon GE, Von Korff M, Saunders K, Miglioretti DL, Crane PK, et al. (2006) Association between obesity and psychiatric disorders in the US adult population. ArchGenPsychiatry 63: 824–830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Goodman E, Whitaker RC (2002) A prospective study of the role of depression in the development and persistence of adolescent obesity. Pediatrics 110: 497–504. [DOI] [PubMed] [Google Scholar]
- 53. Crisp AH, McGuiness B (1976) Jolly fat: relation between obesity and psychoneurosis in general population. BrMedJ 1: 7–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Stewart AL, Brook RH (1983) Effects of being overweight. AmJPublic Health 73: 171–178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Huizink AC, Mulder EJ, Buitelaar JK (2004) Prenatal stress and risk for psychopathology: specific effects or induction of general susceptibility? PsycholBull 130: 115–142. [DOI] [PubMed] [Google Scholar]
- 56. Charil A, Laplante DP, Vaillancourt C, King S (2010) Prenatal stress and brain development. Brain Res Rev 65: 56–79. [DOI] [PubMed] [Google Scholar]
- 57. Slotkin TA, Kreider ML, Tate CA, Seidler FJ (2006) Critical prenatal and postnatal periods for persistent effects of dexamethasone on serotonergic and dopaminergic systems. Neuropsychopharmacology 31: 904–911. [DOI] [PubMed] [Google Scholar]
- 58. Raznahan A, Greenstein D, Lee NR, Clasen LS, Giedd JN (2012) Prenatal growth in humans and postnatal brain maturation into late adolescence. Proc Natl Acad Sci U S A 109: 11366–11371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Walhovd KB, Fjell AM, Brown TT, Kuperman JM, Chung Y, et al. (2012) Long-term influence of normal variation in neonatal characteristics on human brain development. Proc Natl Acad Sci U S A 109: 20089–20094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Manjarrez G, Cisneros I, Herrera R, Vazquez F, Robles A, et al. (2005) Prenatal impairment of brain serotonergic transmission in infants. Journal of Pediatrics 147: 592–596. [DOI] [PubMed] [Google Scholar]
- 61. Allin M, Henderson M, Suckling J, Nosarti C, Rushe T, et al. (2004) Effects of very low birthweight on brain structure in adulthood. Developmental Medicine and Child Neurology 46: 46–53. [DOI] [PubMed] [Google Scholar]
- 62. Nosarti C, Al Asady MH, Frangou S, Stewart AL, Rifkin L, et al. (2002) Adolescents who were born very preterm have decreased brain volumes. Brain 125: 1616–1623. [DOI] [PubMed] [Google Scholar]
- 63. Lodygensky GA, Seghier ML, Warfield SK, Tolsa CB, Sizonenko S, et al. (2008) Intrauterine growth restriction affects the preterm infant's hippocampus. PediatrRes 63: 438–443. [DOI] [PubMed] [Google Scholar]
- 64. de Kieviet JF, Zoetebier L, van Elburg RM, Vermeulen RJ, Oosterlaan J (2012) Brain development of very preterm and very low-birthweight children in childhood and adolescence: a meta-analysis. Dev Med Child Neurol 54: 313–323. [DOI] [PubMed] [Google Scholar]
- 65. Roza SJ, Govaert PP, Vrooman HA, Lequin MH, Hofman A, et al. (2008) Foetal growth determines cerebral ventricular volume in infants The Generation R Study. Neuroimage 39: 1491–1498. [DOI] [PubMed] [Google Scholar]
- 66. Enoch MA, Gorodetsky E, Hodgkinson C, Roy A, Goldman D (2011) Functional genetic variants that increase synaptic serotonin and 5-HT3 receptor sensitivity predict alcohol and drug dependence. Mol Psychiatry 16: 1139–1146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Evans BE, Greaves-Lord K, Euser AS, Franken IH, Huizink AC (2012) The relation between hypothalamic-pituitary-adrenal (HPA) axis activity and age of onset of alcohol use. Addiction 107: 312–322. [DOI] [PubMed] [Google Scholar]
- 68. De Bellis MD, Clark DB, Beers SR, Soloff PH, Boring AM, et al. (2000) Hippocampal volume in adolescent-onset alcohol use disorders. Am J Psychiatry 157: 737–744. [DOI] [PubMed] [Google Scholar]
- 69. Bowman RE, MacLusky NJ, Sarmiento Y, Frankfurt M, Gordon M, et al. (2004) Sexually dimorphic effects of prenatal stress on cognition, hormonal responses, and central neurotransmitters. Endocrinology 145: 3778–3787. [DOI] [PubMed] [Google Scholar]
- 70. Mccormick CM, Smythe JW, Sharma S, Meaney MJ (1995) Sex-Specific Effects of Prenatal Stress on Hypothalamic-Pituitary-Adrenal Responses to Stress and Brain Glucocorticoid Receptor Density in Adult-Rats. Developmental Brain Research 84: 55–61. [DOI] [PubMed] [Google Scholar]
- 71. Weinstock M (2011) Sex-dependent changes induced by prenatal stress in cortical and hippocampal morphology and behaviour in rats: an update. Stress 14: 604–613. [DOI] [PubMed] [Google Scholar]
- 72. Sampson PD, Bookstein FL, Barr HM, Streissguth AP (1994) Prenatal alcohol exposure, birthweight, and measures of child size from birth to age 14 years. Am J Public Health 84: 1421–1428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Sood B, Delaney-Black V, Covington C, Nordstrom-Klee B, Ager J, et al. (2001) Prenatal alcohol exposure and childhood behavior at age 6 to 7 years: I. dose-response effect. Pediatrics 108: E34. [DOI] [PubMed] [Google Scholar]
- 74. Disney ER, Iacono W, McGue M, Tully E, Legrand L (2008) Strengthening the case: prenatal alcohol exposure is associated with increased risk for conduct disorder. Pediatrics 122: e1225–1230. [DOI] [PMC free article] [PubMed] [Google Scholar]