Abstract
Despite being recognized as one of the most successful public health measures, vaccination is perceived as unsafe and unnecessary by a growing number of individuals. Lack of confidence in vaccines is now considered a threat to the success of vaccination programs. Vaccine hesitancy is believed to be responsible for decreasing vaccine coverage and an increasing risk of vaccine-preventable disease outbreaks and epidemics. This review provides an overview of the phenomenon of vaccine hesitancy. First, we will characterize vaccine hesitancy and suggest the possible causes of the apparent increase in vaccine hesitancy in the developed world. Then we will look at determinants of individual decision-making about vaccination.
Keywords: decision-making, psychosocial factors, review, socio-cultural factors, vaccination, vaccine-hesitancy
Introduction
Vaccination is considered to be one of the greatest achievements of public health. Vaccination programs have contributed to the decline in mortality and morbidity of various infectious diseases, and are credited with the elimination of poliomyelitis in the Americas and the worldwide eradication of smallpox.1 To be successful in reducing the prevalence and incidence of vaccine-preventable diseases (VPD), vaccination programs rely on a high uptake level. In addition to direct protection for vaccinated individuals, high vaccination coverage rates induce indirect protection for the overall community, or herd immunity, by slowing transmission of VPD, thereby decreasing the risk of infection among those who remain susceptible in the community.2
The high rate of childhood vaccination coverage in most developed countries indicates that vaccination remains a widely accepted public health measure.3 However, these national estimates may hide clusters of under-vaccinated individuals.4 Indeed, recent outbreaks of VPD, including measles,5,6 poliomyelitis,7 and pertussis8 in several parts of the developed world have been linked mainly to under-vaccinated or non-vaccinated communities.9 In addition, results of many studies have shown that even vaccinated individuals can have important doubts and concerns regarding vaccination.10-13 For instance, in a recent pan-Canadian survey, half of the parents were concerned that new vaccines are not as safe as older vaccines and one-third felt that children today receive too many vaccines, even if nine out of ten of these parents indicated their child’s vaccination was up to date.14 Indeed, many experts consider that vaccination programs are threatened by growing concerns among the population regarding the safety and usefulness of vaccines.15-18 It is estimated that less than 5–10% of individuals have strong anti-vaccination convictions.19 However, a more significant proportion could be categorized as being hesitant regarding vaccination.20 In this review, we will define vaccine hesitancy and look at the potential causes and determinants of the apparent increase in vaccine hesitancy in the developed world.15,16,19 Then, we will look at determinants of individual decision-making regarding vaccination and try to synthesize the wealth of data already published on factors influencing vaccine acceptance.
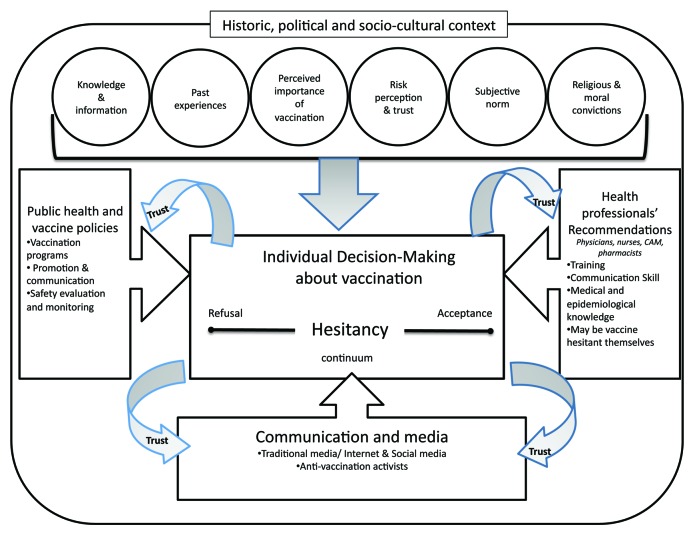
Figure 1 presents a conceptual model that has framed this review. This model consists of 3 domains of factors that interact and could lead to vaccine hesitancy at the individual level. This model was adapted from a schema summary of discussions held during a workshop on the cultural and religious roots of vaccine hesitancy in Canada in which some 40 experts from various fields (social sciences, humanities, public health, biomedical sciences) met to share their views on vaccine hesitancy in the Canadian context.21 As we will discuss in this review, this model illustrates that vaccine hesitancy is an individual behavior influenced by a range of factors, such as knowledge or past experiences. Vaccine hesitancy is also the result of broader influences and should always be looked at in the historical, political and socio-cultural context in which vaccination occurs. Trust placed in the system that delivers vaccines, in the health professionals who recommend and administer the vaccines, in the policy-makers who decide about vaccination programs and in the different types of information about vaccines conveyed in the media also mediates the impact of these factors on vaccine hesitancy.22
Figure 1. Conceptual model of Vaccine Hesitancy. Adapted from the Schema summary of discussions held during the Workshop on the cultural and religious roots of vaccine hesitancy: Explanations and implications for the Canadian healthcare. Accessible online: http://www.usherbrooke.ca/dep-sciences-sante-communautaire/fileadmin/sites/dep-sciences-sante-communautaire/documents/HesitationVaccination/AfficheMG-anglais.pdf
Vaccine Hesitancy: A Definition
Studies examining determinants of vaccination decision-making have resulted in several proposed models of acceptance and resistance, most focusing on parental decision-making.11,23-29 For instance, Nichter has differentiated active demand for vaccinations—adherence by an informed public—from passive acceptance of vaccinations—compliance by a public which yields to recommendations and social pressure.24 Looking at responses to 44 questions (related to, for example, belief in vaccination and vaccine safety, interest and involvement in health issues, influence of family and friends on vaccination decisions, etc.), Gust and collaborators have identified five types of parental attitudes regarding vaccination, in decreasingly positive order: the ”immunization advocates,” the “go alongs to get alongs,” the “health advocates,” the “fence-sitters” and the “worrieds.”27 Keane and collaborators have distinguished four parent profiles: the “vaccine believer” parents who were convinced of the benefits of vaccination, the “cautious” parents emotionally involved with their child and who have an hard time watching them being vaccinated, the “relaxed” parents who were characterized by some skepticism about vaccines and the “unconvinced” parents who distrusted vaccinations and vaccination policy.30 Finally, based on a combination of mothers’ actions and attitudes, Benin and collaborators have categorized the participants of their study into four categories: the “accepters” who agreed with or did not question vaccination, the “vaccine-hesitant” who accepted vaccination but had significant concerns about vaccinating their infants, the “late vaccinators” who purposely delayed vaccinating or chose only some vaccines and the “rejecters” who completely rejected vaccination.26
Challenges in Defining Vaccine-Hesitancy
The differences between these different models illustrate the difficulty of categorizing attitudes about vaccination. Because these models are often rooted in individual studies and because of the complex interaction of different social, cultural, political and personal factors in vaccine decision, it is hard to have a clear picture of the range of possible attitudes about vaccination. However, the common ground among these models is the fact that attitudes toward vaccination should be seen on a continuum ranging from active demand for vaccines to complete refusal of all vaccines. Generally speaking, vaccine-hesitant individuals are a heterogeneous group in the middle of this continuum. Vaccine-hesitant individuals may refuse some vaccines, but agree to others; they may delay vaccines or accept vaccines according to the recommended schedule, but be unsure in doing so.26,31 Despite the growing number of articles referring to vaccine hesitancy published in recent years,32-37 there are some discrepancies among publications about what exactly falls under the umbrella of “vaccine hesitancy.” The expression can be used to refer to a “gap in parental knowledge”36 or refer to “reflection and deliberation about the benefits of specific vaccines.”38 It is hard to have a clear picture of vaccine hesitancy at the population level because hesitancy is not directly related to vaccine uptake (as vaccine-hesitant individuals may accept all recommended vaccines in a timely manner, but still have significant doubts in doing so). In addition, hesitancy can vary according to the vaccine involved (one can be hesitant regarding the flu vaccine but accept with confidence all other vaccines), with newer vaccines usually engendering more hesitancy.39-41 Thus, caution is needed when trying to draw a general picture of vaccine-hesitant individuals’ characteristics. For example, in one study aimed at assessing attitudinal barriers to MMR vaccination among vaccine-hesitant parents, eligible parents were those who were “unsure” or “did not want” to get their child vaccinated against MMR.42 In contrast, in another study aimed at identifying the reasons why parents hesitate to have their children vaccinated, eligible parents needed to have been present in a clinic with a child requiring a minimum of one vaccination that was at least 6 mo overdue.37 Both these studies were presenting characteristics of vaccine-hesitant parents, but their inclusion criteria were quite different which limits the comparability of results on attitudes and perceptions of vaccination.
Recent work in developing a survey instrument to directly measure the level of vaccine hesitancy among parents has shown promising results.31,43 The 15-item survey instrument, designed by Opel and collaborators for the US context, measures 4 domains linked to vaccine hesitancy: vaccination behavior, beliefs about vaccine safety and efficacy, attitudes about vaccine mandates and exemptions and trust. After having pre-tested their instrument among 230 parents, the authors found a statistically significant linear association between a parent’s total score on the 15-item survey and their child’s vaccination status (in terms of days of under-vaccination for 6 recommended vaccines from birth to 19 mo of age). In comparison, using data from a large population-based survey conducted among parents of children aged 24–35 mo, Smith and collaborators have concluded that the four psychosocial domains of the health belief model (perceived susceptibility to and seriousness of VPD, perceived efficacy of vaccines and concerns and influences that facilitate or discourage vaccination) allowed for measurement of beliefs linked with vaccine hesitancy and could be useful for predicting the parental decision to delay or refuse vaccines for their child.44 In fact, the Health Belief Model was originally developed in the 1950s to look at barriers to polio vaccination among parents.45
Potential Causes of Vaccine Hesitancy
The importance of the historical, political and socio-cultural context
Social science research has shown that vaccination decision-making should be understood in a broader socio-cultural context.25,46-48 In fact, vaccination is part of a “wider social world”49 which means that different factors (past experiences with health services, family histories, feelings of control, conversations with friends, etc.) can influence the decision-making process regarding vaccination. As stressed by Hobson-West, “vaccination is just one decision of many that parents are faced with. Other day-to-day concerns about child health and nutrition may take priority at certain times, or influence willingness to vaccinate.”47 Streefland and collaborators use the expression “local vaccination cultures” to characterize how “shared beliefs about disease aetiology, ideas about the potency and efficacy of modern medicine and views on the need for preventive measures” as well as “local health services experiences and vaccination settings” influence the individual decision about vaccination.25 In the actual postmodern context that questions the legitimacy of science, expertise and medical authority,50 it is not surprising that more and more individuals question the relevance of vaccination. Vaccine hesitancy may be a consequence of the focus of health promotion on lifestyle and individual action and the growth of “consumerism” in health-care, which means patients’ involvement in their own health decisions.51 The rise of the informed patient has shifted the traditional locus of power from doctors as sole directors of patient care to shared decision-making between health professionals and patients who want to be active participants in the decision-making process concerning their health.
In addition, since its introduction, vaccination has been the subject of many different controversies and vaccination scares.52 These controversies have affected vaccine acceptance to varying degrees and have often occurred within a particular context—such as the association between the hepatitis B vaccine and multiple sclerosis in France that resulted in the suspension of the universal vaccination program in the 1990s, despite the fact that many studies have found no evidence of such an association.53 Some of these vaccination scares have transcended frontiers. The most recent and well-known is the fraudulent association between the MMR vaccination and autism that was first highly publicized in the United Kingdom, but then rapidly diffused worldwide. Fear of autism is still today a frequently reported vaccine safety concern among parents in different settings.54,55 Despite the fact that there are as many causes of hesitancy as there are contexts, we have hypothesized that some factors are playing a key role in the apparent increase of this phenomenon in the developed world. We will look specifically at the roles of media and communication, of public health and vaccine policies and of health professionals.
The Role of Media and Communication
In a well-written book, the journalist Seth Mnookin explains how vaccination has become a source of fear and a target for misinformation.56 Looking at the history of vaccination in the United States and the United Kingdom, he shows how media have played a role in keeping vaccination scares alive, even in face of strong evidence of the safety and effectiveness of vaccines. Indeed, many scientific studies have demonstrated the negative influence of media controversies on vaccine uptake.57-59 Research looking at pertussis incidence in many developed countries has shown that, in countries where vaccine uptake for pertussis vaccination programs decreased because of controversies regarding vaccine safety (actively circulated in news stories, television interviews, popular articles, etc.), the incidence of pertussis was 10 to 100 times higher than in countries where high vaccine coverage was maintained.58
In addition to traditional media, the Internet has offered an opportunity for vocal anti-vaccination activists to diffuse their message.60-65 Many consider that the omnipresence of anti-vaccination content on the World Wide Web has contributed to a broader and faster dissemination of rumours, myths and “inaccurate” beliefs regarding vaccines that have had a negative impact on vaccine uptake.50,61,66 Indeed, even if health professionals are still frequently consulted by the majority of individuals with health concerns, the Internet has become an essential source of information.66,67 In addition, with Web 2.0 functions which allow users to create and share content using social networks (such as Facebook, Twitter, Youtube or Wikipedia), individuals can share their personal experiences of vaccination. These narratives add a new dimension to health information: a personal and embodied view of vaccine-preventable disease, vaccines and their potential (often negative) consequences.66 Indeed, studies reviewing the content of websites or social networks concerning vaccination have shown that information is of variable quality and that inexact or negative content is predominant.61,62,64 For example, in a study simulating a patient’s search for advice on the potential link between MMR and autism using the Google search engine, Scullard and collaborators have reported that only 51% of the websites provided the correct information about the fact that no association has ever been demonstrated between MMR vaccination and autism.65
Kata has shown that anti-vaccination websites shared common characteristics and used similar arguments and strategies to disseminate their message.50,68 For instance, most anti-vaccination websites argue against vaccination safety and usefulness, using arguments such as the existence of “hot lots” of vaccines or the presence of poisons in vaccines and use emotive appeals such as personal stories of vaccine damage.68 Most of the arguments used by anti-vaccination activists can be seen as part of a larger phenomenon of “denialism.” Denialism can be defined as “the employment of rhetorical arguments to give the appearance of legitimate debate where there is none, an approach that has the ultimate goal of rejecting a proposition on which a scientific consensus exists.”69 Whether it is to deny evolution, climate change or the fact that vaccines do not cause autism, Diethelm and McKee have shown that denialists employ similar tactics such as relying on “conspiracy theories,” using fake experts, purposively selecting only supportive evidence and discrediting all other, creating impossible expectations of what research can deliver or using logical fallacies.69
Finally, despite concerns regarding the increasing influence of the Internet on vaccine acceptance, there is little data examining exposure to anti-vaccine websites on vaccine decision-making. Studies have shown that individuals who delayed or refused vaccines are significantly more likely to have looked for vaccine information on the Internet.44,70 The results of one large-scale experimental study done by Betsch and collaborators have shown that surfing on an anti-vaccination website for 5–10 min had a negative influence on risk perceptions regarding vaccinations and on the decision to vaccinate one’s child.71 However, more research is needed to assess whether individuals who already have concerns regarding vaccination are more likely to search for information on the Internet from a range of sources or whether it is the Internet searches themselves that generate concerns regarding vaccination.
The Role of Public Health and Vaccine Policies
Before the 21st century, vaccination programs were commonly recognized as one of the most cost-effective public health intervention and the arrival of new vaccines was almost always welcomed by public health decision-makers and clinicians.72,73 However, in recent years we have seen an increase in the number of new vaccines licensed and commercialized on the market.74 In the United States, the number of vaccines included in the publicly funded vaccination program for children from birth to 18 y of age has more than tripled between 1990 and 2012 (Fig. 67–3 in ref. 74). The increase in the number of vaccines has resulted in differences in regard to addition of new vaccines in regular programs or use of different vaccination schedules. Some have argued that differences between vaccination schedules and programs adopted in different countries, or even in different jurisdictions of the same country, could increase individuals’ negative perception of the relevance of particular vaccines or vaccine schedules.15,22
In order to achieve high vaccine coverage, some countries have introduced laws to require children to be vaccinated before school entry. Policies that mandate vaccination have always been controversial.75 However, there seems to be an increasing trend of opposition toward mandatory vaccination, as shown for instance by the increase in exemption rates in United States.4 Results of population-wide survey conducted in the United States have indicated that more than 10% of parents were opposed to compulsory vaccination. Not surprisingly, parents who disapproved of compulsory vaccination were significantly more likely to hold negative beliefs regarding the safety of vaccines and their utility to protect their child’s health.76
Public health has a role to play in communicating adequately with the population. High quality vaccine safety surveillance is in place in developed countries. However, the strength and reliability of these systems is not well-understood by the population or even by some healthcare providers. Inaccurate information regarding both vaccine safety and the process leading to vaccine licensure and inclusion in universal programs circulates widely, leading to significant problems for public health clinicians, policy makers and patients.77,78 A recent example of pitfalls in communicating vaccine safety to the public is the controversy surrounding the removal of thimerosal, a mercury-containing preservative, from vaccines for children in the US. Due to awareness of the theoretical potential for neurotoxicity of even low levels of organomercurials and because of the increased number of thimerosal-containing vaccines added to the childhood vaccination schedule in the US, concerns about the use of thimerosal in vaccines and other products have been raised.79,80 Because of these concerns, the Food and Drug Administration has worked with vaccine manufacturers to reduce or eliminate thimerosal from vaccines. As Jacobson and collaborators have illustrated, despite the fact that this information, including the fact that the risk was only theoretical and that it was recommended to pursue vaccination during the transition period, was communicated to health professionals, “vaccine providers across the nation in fact withheld hepatitis B vaccination of newborn infants, premature or not, in a mistaken belief that they were preventing mercury poisoning of these infants.”81 The call for the production of thimerosal-free vaccines by health authorities was also seized upon by anti-vaccination movements as a proof that ‘there was something wrong’ with vaccines and that public health authorities were ‘hiding the truth about vaccines’.56 This illustrates the importance for public health authorities to work in collaboration with communication experts so that their messages, while being scientifically rigorous, can be effectively communicated to the public and to health-care providers.22
Finally, the increase in the number of vaccines and the consequent decline in vaccine-preventable illnesses have focused attention by both health professionals and parents on vaccine usefulness and safety.53,82-85 Because vaccination programs have been successful, VPD are becoming less visible and many individuals, as well as health professionals, have no first-hand knowledge of the risks of the diseases.86 Indeed, attention is more often directed to the risk, or alleged risk, of the vaccines rather than to the risk of the diseases. That is why it can be argued that “vaccination is victim of its own success.”22,86 In addition, some new vaccines prevent diseases perceived as mild (e.g., chickenpox or gastroenteritis), which can compromise their acceptability.39-41,87 Many public health interventions to promote vaccination, especially those based on education and information, have not been successful in enhancing vaccine uptake.88 This may be explained by the fact that many interventions are designed with the assumption that resistance to vaccination can be countered by supplying probabilistic information about vaccine risks and benefits. From this perspective, individuals who have concerns or doubts regarding vaccination are often assumed to be irrational, emotional, ill-informed, or to be manipulated by anti-vaccination groups. As we will discussed in the next section of this article, individual decision-making about vaccination is influenced by many different factors, including the fact that some of those who have doubts and concerns about vaccine safety use an entirely different decision-making model or subscribe to a different set of beliefs about health and illness. Supplying additional probabilistic information may not adequately address individual concerns. Dry statements on probabilities are not as powerful as anecdote and emotion often used in anti-vaccination claims. In addition, lay people may be more at ease with a binary “yes/no” approach to risk instead of probabilities used to define risks in science.89 Suggestions have been made that public health communicators move beyond the “knowledge deficit model of communication” to develop messages tailored to the audience needs; to use new tools such as social media and to be proactive rather than reactive to vaccination scares.19,66
The Role of Health Professionals
The interaction between patients and providers is the cornerstone of maintaining confidence in vaccination.20,90,91 Health professionals’ knowledge and attitudes about vaccines have previously been shown to be an important determinant of their own vaccine uptake, their intention to recommend the vaccine to their patients and the vaccine uptake of their patients.92-97 Findings of a review on determinants of nurses’ practices regarding influenza vaccination indicate a relationship between knowledge, attitudes and vaccination practices. In the 12 research studies included in this review, higher knowledge and positive attitudes toward influenza vaccination were positively associated with vaccination coverage among nurses and there was also an association between nurses’ vaccination status and their reported promotion of vaccination to their patients.98 Results of a study conducted among physicians in Switzerland have shown that almost 5% of (non-pediatrician) physicians have declined or delayed MMR or DTP-based vaccinations for their own children. The authors concluded that fear of “immune overload” among these health care providers means that they are unlikely to answer parental concerns adequately.94
Health professionals are generally strong supporters of vaccination. However, some of them could be categorized as vaccine-hesitant.99,100 Results of a recent study conducted in Quebec, Canada, have shown that an important proportion of the 540 healthcare workers surveyed were having concerns about vaccination. Indeed, more than one third agreed that children are receiving too many vaccines (37% agreed) and that a good lifestyle can eliminate the need for vaccination (36% agreed).101 Vaccine hesitancy among health professionals is also well-illustrated by the reluctance of a significant proportion of healthcare workers to receive the flu vaccine despite strong recommendations to do so and free vaccines available at the workplace in many countries.93,102
From another point of view, vaccine hesitancy can induce strong emotional responses in health professionals, ranging from worries that trust in the relationship with patients can be endangered to medico-legal concerns.103 Despite the fact that the American Academy of Pediatrics' Committee on Bioethics discourages discontinuing care for families who refuse or delay immunization,104 studies have illustrated that some providers are doing so.105 This indicates that health professionals may need to be supported when addressing patients’ concerns regarding vaccination. Some professionals may feel overwhelmed by the concerns expressed by patients. The complexity of the vaccine schedule and the rapid development in vaccinology could be a barrier for health professionals who have to keep up to date and who may not feel comfortable discussing vaccination with patients.18,106-108
Because health professionals are the most trusted source of information on vaccination for the majority of patients, many tools and tips have been presented to help providers in their discussions with vaccine-hesitant or vaccine-refusing patients.20,29,33,109,110 Although the approaches presented in these articles vary, they do share some common characteristics, such as the importance of maintaining a trustworthy patient-provider relationship and the importance of tailoring the communication to specific patients’ concerns and doubts.
Individual Decision-Making Process
Several literature reviews have been published recently looking at factors associated with vaccination acceptance or refusal in developed countries. These reviews have mostly focused on parental decision-making regarding different childhood vaccines,9,87,111-115 on decision-making regarding the HPV vaccine among different sub-populations116-119 or on decision-making regarding pneumococcal, seasonal flu or pandemic flu vaccination.98,120-123 The overwhelming majority of studies looking at determinants of vaccine acceptance have been conducted among parents, mainly because most vaccines are targeted at children and adolescents. These reviews had different objectives and scopes, making it difficult to draw definitive conclusions regarding the most influential factors in vaccine acceptance or refusal. Although individual vaccine decision-making varies according to socio-cultural context, social circumstances and personal experience, similarities in individual determinants of vaccination acceptance or refusal can be found. Of course, the direct and indirect costs of accessing healthcare services are important determinants of sub-optimal vaccine uptake,88 but they will not be reviewed here; rather, our focus is on the psychosocial factors affecting vaccine acceptance at the individual level.
Knowledge/Information About Vaccination
Lack of awareness about “who, where and when” one should be vaccinated and self-estimated sufficiency of information about vaccination or satisfaction with information on vaccination are frequently associated with vaccination decisions. However, the association between level of knowledge about vaccination and vaccine acceptance is not straightforward. Many studies have shown that parents who choose to vaccinate their child generally have limited knowledge of vaccination and vaccine-preventable diseases compared with parents who refuse to vaccinate. These studies indicated that parents’ choice was often based on conformity – or following what is recommended – rather than based on specific knowledge about vaccine or vaccine-preventable disease.25,111,124-126 In addition, studies conducted in different settings have shown that non-compliant parents appear to have looked at a lot of information about vaccination and to have considerable interest in health-related issues.11,127,128
Past Experiences with Vaccination Services
As discussed elsewhere,88 accessibility to and convenience of vaccination services are important determinants of vaccine uptake. In addition, the quality of vaccination services could influence vaccine acceptance. Past experiences with vaccinations and vaccination services, such as negative encounters with vaccine providers, can influence future decision-making regarding vaccination. For example, results of a study conducted among parents attending a naturopathic clinic in Ontario have shown that feeling pressured by physicians to vaccinate one's child was one of the main determinants of a child’s non-vaccination or incomplete vaccine status.129 Fear of needles and of pain after vaccination is also a documented barrier to vaccination. For example, results of a study conducted by Taddio and collaborators indicated that about two-thirds of children and one-quarter of parents reported needle fears.130 In another study, the vaccine concern listed most often by parents was a child’s pain from the shots.131
Perceptions of The Importance of Vaccination in Maintaining Health
Perceived importance of vaccination is a well-known individual determinant of vaccine acceptance. For instance, in a study looking at the association between parents’ beliefs about vaccines, their decision to delay or refuse vaccines for their children and vaccination coverage of children at aged 24 mo, parents who were more likely to agree that vaccines are necessary to protect the health of children, to believe that their child might get a disease if they aren’t vaccinated, or to believe that vaccines are safe had significantly higher coverage for 10 childhood vaccines.44 Studies have shown that individuals who refuse or are hesitant regarding vaccination often share a particular worldview regarding health (e.g., a preference for natural immunity, the belief that VPD are needed to build a strong immune system, the idea that it is possible to control exposure to disease or the belief that good hygiene and personal habits can make vaccination unnecessary).128 Two studies, one ethnographic and one based on a questionnaire, have identified a “lay theory of immunity.” This theory is based on a view of the immune system as an individual characteristic needing individualized healthcare and on the idea that there is a possible risk of immune overload due to individual “weakness” of a child.49,127 As Casiday has shown in her qualitative study on parental measles, mumps and rubella (MMR) vaccination decision-making, this view often implies a “holistic notion of the immune system, (…) in which the immune system is viewed as central to the body’s overall health, but is itself intricate and delicately balanced; it must be maintained so that it can flexibly and effectively cope with a multitude of challenges from the environment.”48 From this point of view, vaccines are seen as something that would perturb rather than boost the immune system. Indeed, studies conducted among parents consistently show that concerns regarding the number of vaccines and doses as well as the age at first vaccination are associated with delayed vaccination or vaccine refusal. Results of a Dutch survey indicated that an important proportion of parents thought that children receive too many vaccines and that vaccines interfere with natural development.132
Health Professionals’ Recommendations and Use of Complementary And Alternative Medicine (CAM)
One of the main predictors of acceptance of a vaccine is a recommendation for vaccination by a health care professional.55,91,133 For example, results of a large US study indicated that the largest proportion of parents who changed their minds about delaying or not getting a vaccination for their child listed ‘information or assurances from health care provider’ as the main reason.39 In contrast, the association between use of CAM, such as homeopathy, and non-vaccination among parents on behalf of their children and among adults themselves has frequently been observed.32,44,127,134-137 Downey and collaborators found that, among non-Medicaid pediatric enrollees in two Washington State insurance companies, those who received care from naturopathic physicians or chiropractors at ages < 2 y were significantly less likely to have received the four vaccinations (measles/mumps/rubella, chickenpox, diphtheria/tetanus/pertussis and H. influenzae type B).134 In another study, consultation with a homeopath was strongly associated with parental non-compliance with MMR vaccination.127 Authors of this study noted that their study quantifies a striking influence of homeopathy on the belief that vaccinations could harm the immune system. Indeed, despite the fact that the founder of homeopathy was strongly in favor of vaccination,138 many studies performed in different countries have illustrated that homeopaths have advised their patients not to be vaccinated (see Ersnt137 for a review).
Risk Perceptions
In a meta-analysis, Brewer and collaborators found strong evidence that risk perceptions are predictors of adult vaccination behavior.139 In health, two dimensions are usually used to assess risk perceptions: perceived vulnerability or likelihood of harm if no action is taken and perceived severity or seriousness of the consequences if harm was to occur.140 These risks are viewed as being balanced against the perceived costs and benefits of an action to prevent this harm. Perceptions of risk can influence vaccine decision-making in two ways: perceived risks of VPD can foster vaccine acceptance and perceived risks of vaccines can contribute to vaccine refusal. This is further complicated by the fact that vaccines are administered as prophylactics to healthy individuals and the risks of vaccines (real or alleged) are visible while their benefits are impossible to evaluate from an individual perspective. In addition, the decision not to vaccinate is reversible, while the opposite is not true. Indeed, many studies have shown that individuals are more averse to the risks associated with an action – getting an ‘unsafe’ vaccine – than to the risks associated with inaction – taking a chance of contracting a VPD. This is known as the “omission bias.”109
When looking at individual risk perception regarding vaccination, it is important to note that risk is perceived differently by lay people than by experts.141 An epidemiological perspective of risk is based on a rational approach (or a probabilistic view) where risk is objective and measurable. A rational approach to risk implies that decision-making in face of a risk can be improved by ensuring that emotional, cognitive and social distortions or bias affecting judgement are corrected and that external influences, such as those triggered by media, are counteracted.46,47,108 However, many studies have shown that popular interpretation of risk is not always based on a rational approach, but rather on an “uncertainties and ambiguities” approach where doubts remain even in the face of empirical evidence.47,142,143 Risk perceptions among lay people, contrary to experts, are grounded in past experiences (such as those with other vaccines or health services) rather than on scientific data.47,48 Finally, research conducted among parents has shown that in the decision-making process regarding vaccination, most parents consider the risk of a VPD or of side effects of vaccines not from a population-based perspective as in epidemiology, but rather based on their perceptions of their own child’s health and vulnerabilities.46,49 For a review of the implications of risk perception in the decision to vaccinate at the individual level, please see Serpell and Green.144
Trust
In studies of vaccination decision-making, risk perception is often closely linked with ideas of trust in health professionals, in government or in public health institutions and the interplay between these actors.25,128,145 For example, in a qualitative longitudinal study, Benin and collaborators found that trust or lack of trust was pivotal for new mothers making decisions about vaccinating their infants.26 The authors concluded that the “reliance on trust was especially impressive, because mothers perceived that ‘diseases are not around’ or ‘not so bad’ and they had little experience with VPD.”26 However, Leach and Fairhead warned researchers of using too narrow a concept of trust when studying vaccination acceptance and refusal. After extensive field work in Brighton, UK and several countries in West Africa, they conclude that the concept of trust was rarely evoked by parents when describing their relationships with health professionals. More significant was whether parents felt supported and confident to ask questions and to express their views when discussing about vaccines with doctors or other health professionals. In contrast, parents were using the concept of trust to refer to “socially remote institution” such as pharmaceutical companies or government.46
Indeed, Brownlie and Howson provide a reliable definition of trust as “a complex relational practice happening within particular socio-political context.”146 After in-depth analysis of focus group data on trust and MMR vaccination, they conclude that trust is not only based on knowledge, but also on a ‘leap of faith’a that could only be possible because parents have a relationship with health professionals based on familiarity146
Subjective Norm, Social Pressure and Social Responsibility
Seeing vaccination as a social norm is a potentially powerful driver of vaccine acceptance. The importance of subjective norm, or the fact that those around you, whom you respect, are being vaccinated themselves or having their children vaccinated, is a factor related to vaccine acceptance in many studies.113 Based on ethnographic studies conducted in six countries, Streefland and collaborators have shown that “people have their children vaccinated because everybody does so and it seems the normal thing to do.”25 Similarly, Brown and collaborators have shown that perceiving peers and family members as pro-MMR was associated with vaccine uptake.28 Social norm can also result in social pressure to accept vaccination. Indeed, in a review of psychological factors associated with uptake of vaccination during the 2009 A(H1N1) influenza pandemic, Bish and collaborators concluded that there was “evidence of social pressure on uptake, with those believing that others wanted them to be vaccinated being more likely to do so.”123 From another point of view, social responsibility, or seeing vaccination as a duty of individuals in order to maintain herd immunity, could also be linked with vaccine acceptance. Quadri-Sheriff and collaborators have systematically searched the literature to determine if the concept of “benefit to others” was a motivator of parents’ willingness to vaccinate their child.114 They concluded that even if some parents see the role of childhood immunization in building herd immunity in a positive light, their decision to vaccinate was largely based on the perceived benefit to their own child.114
Moral or Religious Convictions
Finally, as discussed earlier in this section, vaccination refusal is sometimes linked with philosophical beliefs or moral convictions regarding health and immunity, such as a preference for “natural” over “artificial” medicines. Refusal of vaccines has also been linked with strong religious convictions. Orthodox Protestants in The Netherlands and the Amish in the United States are religious communities well-known for rejecting vaccination for religious motives.147,148 Opposition to vaccination based on religious motives dates back to the introduction of vaccination and can be explained, at least partially, by the idea that vaccination is not congruent with religious considerations regarding the “origin of illness, the need for preventive action and the search for a cure.”147
In summary, the individual decision-making process regarding vaccination is complex and multidimensional. Numerous barriers to vaccination have been identified: fear of side effects, lack of a provider recommendation to be vaccinated, beliefs regarding the efficacy and usefulness of vaccines, distrust of the motives behind, lack of awareness of the need to be vaccinated, etc. Often, these barriers are presented as discrete and measurable variables, without regard to the “processes and pathways” leading to vaccination refusal as well as to the broader socio-cultural context within which these barriers are rooted.24
Conclusion
Despite the fact that it seems impossible to quantify precisely the proportion of the population that could be categorized as vaccine-hesitant, experts worldwide acknowledge that there is an increasing trend toward vaccine hesitancy. As shown in this review, individual decision-making regarding vaccination is complex and involves emotional, cultural, social, spiritual and political factors as much as cognitive factors. Of course, individuals have been hesitant or unsure about vaccination since the first vaccines were made available.52 However, as we have tried to illustrate in this review, vaccine hesitancy can be heightened by the current “changing scientific, cultural, medico-legal and media environments.”51
As illustrated in the model, in addition to the factors affecting vaccine acceptance at the individual level, a thoughtful understanding of vaccine hesitancy needs to be grounded in the particular historical, political and socio-cultural context in which vaccination occurs. Consideration should also be given to broader influences on vaccine hesitancy such as the role of public health and vaccine policies, communication and media and health professionals.
The growing interest in vaccine hesitancy has resulted in the development of different tools and strategies to enhance vaccination acceptance. Many experts have proposed ways to counter vaccine hesitancy at the population level, including transparency in policy-making decisions regarding vaccination programs, providing education and information to the public and health providers about the rigorous process that leads to approval of new vaccines and diversified post-marketing surveillance of vaccine-related events. In addition, as stressed by Larson and collaborators, “additional emphasis should be placed on listening to the concerns and understanding the perceptions of the public to inform risk communication and to incorporate public perspectives in planning vaccine policies and programmes.”22 Finally, as their role is crucial in sustaining the success of vaccination programs, more research is needed to understand why some health professionals, trained in medical sciences, still have doubts regarding the safety and effectiveness of vaccination.
Disclosure of Potential Conflicts of Interest
No potential conflicts of interest were disclosed.
Endnote
a Generally speaking, a leap of faith could be defined as the act of believing in something intangible or improvable. In their study, Brownlie and Hobson describe how parents, who were having important knowledge gaps about MMR, were making a leap of faith by consciously or unconsciously dismissing some uncertainties in order to decide about MMR vaccination.
Footnotes
Previously published online: www.landesbioscience.com/journals/vaccines/article/24657
References
- 1.Centers for Disease Control and Prevention (CDC) Ten great public health achievements--United States, 1900-1999. MMWR Morb Mortal Wkly Rep. 1999;48:241–3. [PubMed] [Google Scholar]
- 2.Fine P, Eames K, Heymann DL. “Herd immunity”: a rough guide. Clin Infect Dis. 2011;52:911–6. doi: 10.1093/cid/cir007. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization. Immunization summary - A statistical reference containing data through 2010. 2012.
- 4.Omer SB, Salmon DA, Orenstein WA, deHart MP, Halsey N. Vaccine refusal, mandatory immunization, and the risks of vaccine-preventable diseases. N Engl J Med. 2009;360:1981–8. doi: 10.1056/NEJMsa0806477. [DOI] [PubMed] [Google Scholar]
- 5.Parent du Châtelet I, Antona D, Freymuth F, Muscat M, Halftermeyer-Zhou F, Maine C, et al. Spotlight on measles 2010: update on the ongoing measles outbreak in France, 2008-2010. Euro Surveill. 2010;15:15. [PubMed] [Google Scholar]
- 6.De Serres G, Markowski F, Toth E, Landry M, Auger D, Mercier M, et al. Largest measles epidemic in North America in a decade--Quebec, Canada, 2011: contribution of susceptibility, serendipity, and superspreading events. J Infect Dis. 2013;207:990–8. doi: 10.1093/infdis/jis923. [DOI] [PubMed] [Google Scholar]
- 7.Oostvogel PM, van Wijngaarden JK, van der Avoort HGAM, Mulders MN, Conyn-van Spaendonck MAE, Rümke HC, et al. Poliomyelitis outbreak in an unvaccinated community in The Netherlands, 1992-93. Lancet. 1994;344:665–70. doi: 10.1016/S0140-6736(94)92091-5. [DOI] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention (CDC) Notes from the field: Pertussis—California, January–June 2010. Morbidity and Mortality Weekly Report. 2010;59:817. [Google Scholar]
- 9.Falagas ME, Zarkadoulia E. Factors associated with suboptimal compliance to vaccinations in children in developed countries: a systematic review. Curr Med Res Opin. 2008;24:1719–41. doi: 10.1185/03007990802085692. [DOI] [PubMed] [Google Scholar]
- 10.Kennedy A, Lavail K, Nowak G, Basket M, Landry S. Confidence about vaccines in the United States: understanding parents’ perceptions. Health Aff (Millwood) 2011;30:1151–9. doi: 10.1377/hlthaff.2011.0396. [DOI] [PubMed] [Google Scholar]
- 11.Burton-Jeangros C, Golay M, Sudre P. [Compliance and resistance to child vaccination: a study among Swiss mothers] Rev Epidemiol Sante Publique. 2005;53:341–50. doi: 10.1016/S0398-7620(05)84616-4. [DOI] [PubMed] [Google Scholar]
- 12.Wu AC, Wisler-Sher DJ, Griswold K, Colson E, Shapiro ED, Holmboe ES, et al. Postpartum mothers’ attitudes, knowledge, and trust regarding vaccination. Matern Child Health J. 2008;12:766–73. doi: 10.1007/s10995-007-0302-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Casiday R, Cresswell T, Wilson D, Panter-Brick C. A survey of UK parental attitudes to the MMR vaccine and trust in medical authority. Vaccine. 2006;24:177–84. doi: 10.1016/j.vaccine.2005.07.063. [DOI] [PubMed] [Google Scholar]
- 14.Ekos Research Associates Inc. Survey of Parents on Key Issues Related to Immunization. Ottawa: Public Health Agency of Canada, 2011:53 p. + Appendix. [Google Scholar]
- 15.Black S, Rappuoli R. A crisis of public confidence in vaccines. Sci Transl Med. 2010;2:mr1. doi: 10.1126/scitranslmed.3001738. [DOI] [PubMed] [Google Scholar]
- 16.Poland GA, Jacobson RM, Ovsyannikova IG. Trends affecting the future of vaccine development and delivery: the role of demographics, regulatory science, the anti-vaccine movement, and vaccinomics. Vaccine. 2009;27:3240–4. doi: 10.1016/j.vaccine.2009.01.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.MacDonald NE, Smith J, Appleton M. Risk perception, risk management and safety assessment: what can governments do to increase public confidence in their vaccine system? Biologicals. 2012;40:384–8. doi: 10.1016/j.biologicals.2011.08.001. [DOI] [PubMed] [Google Scholar]
- 18.Leask J, Braunack-Mayer A, Kerridge I. Consent and public engagement in an era of expanded childhood immunisation. J Paediatr Child Health. 2011;47:603–7. doi: 10.1111/j.1440-1754.2011.02160.x. [DOI] [PubMed] [Google Scholar]
- 19.Leask J. Target the fence-sitters. Nature. 2011;473:443–5. doi: 10.1038/473443a. [DOI] [PubMed] [Google Scholar]
- 20.Leask J, Kinnersley P, Jackson C, Cheater F, Bedford H, Rowles G. Communicating with parents about vaccination: a framework for health professionals. BMC Pediatr. 2012;12:154. doi: 10.1186/1471-2431-12-154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Laberge C, Guay M, Clément P, Bramadat P, Dubé E, Roy R, et al. Workshop on the cultural and religious roots of vaccine hesitancy: Explanations and implications for the Canadian healthcare. Online: http://www.usherbrooke.ca/dep-sciences-sante-communautaire/fileadmin/sites/dep-sciences-sante-communautaire/documents/HesitationVaccination/AfficheMG-anglais.pdf Page access on January 23, 2013.
- 22.Larson HJ, Cooper LZ, Eskola J, Katz SL, Ratzan S. Addressing the vaccine confidence gap. Lancet. 2011;378:526–35. doi: 10.1016/S0140-6736(11)60678-8. [DOI] [PubMed] [Google Scholar]
- 23.Rogers A, Pilgrim D, Gust ID, Stone DH, Menzel PT. The pros and cons of immunisation. Health Care Anal. 1995;3:99–115. doi: 10.1007/BF02198210. [DOI] [PubMed] [Google Scholar]
- 24.Nichter M. Vaccinations in the Third World: a consideration of community demand. Soc Sci Med. 1995;41:617–32. doi: 10.1016/0277-9536(95)00034-5. [DOI] [PubMed] [Google Scholar]
- 25.Streefland P, Chowdhury AMR, Ramos-Jimenez P. Patterns of vaccination acceptance. Soc Sci Med. 1999;49:1705–16. doi: 10.1016/S0277-9536(99)00239-7. [DOI] [PubMed] [Google Scholar]
- 26.Benin AL, Wisler-Scher DJ, Colson E, Shapiro ED, Holmboe ES. Qualitative analysis of mothers’ decision-making about vaccines for infants: the importance of trust. Pediatrics. 2006;117:1532–41. doi: 10.1542/peds.2005-1728. [DOI] [PubMed] [Google Scholar]
- 27.Gust D, Brown C, Sheedy K, Hibbs B, Weaver D, Nowak G. Immunization attitudes and beliefs among parents: beyond a dichotomous perspective. Am J Health Behav. 2005;29:81–92. doi: 10.5993/AJHB.29.1.7. [DOI] [PubMed] [Google Scholar]
- 28.Brown K, Fraser G, Ramsay M, Shanley R, Cowley N, van Wijgerden J, et al. Attitudinal and demographic predictors of measles-mumps-rubella vaccine (MMR) uptake during the UK catch-up campaign 2008-09: cross-sectional survey. PLoS One. 2011;6:e19381. doi: 10.1371/journal.pone.0019381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Halperin SA. How to Manage Parents Unsure About Immunization. Can J Contin Med Educ. 2000;2000:62–75. [Google Scholar]
- 30.Keane MT, Walter MV, Patel BI, Moorthy S, Stevens RB, Bradley KM, et al. Confidence in vaccination: a parent model. Vaccine. 2005;23:2486–93. doi: 10.1016/j.vaccine.2004.10.026. [DOI] [PubMed] [Google Scholar]
- 31.Opel DJ, Mangione-Smith R, Taylor JA, Korfiatis C, Wiese C, Catz S, et al. Development of a survey to identify vaccine-hesitant parents: the parent attitudes about childhood vaccines survey. Hum Vaccin. 2011;7:419–25. doi: 10.4161/hv.7.4.14120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gaudino JA, Robison S. Risk factors associated with parents claiming personal-belief exemptions to school immunization requirements: community and other influences on more skeptical parents in Oregon, 2006. Vaccine. 2012;30:1132–42. doi: 10.1016/j.vaccine.2011.12.006. [DOI] [PubMed] [Google Scholar]
- 33.Opel DJ, Robinson JD, Heritage J, Korfiatis C, Taylor JA, Mangione-Smith R. Characterizing providers’ immunization communication practices during health supervision visits with vaccine-hesitant parents: a pilot study. Vaccine. 2012;30:1269–75. doi: 10.1016/j.vaccine.2011.12.129. [DOI] [PubMed] [Google Scholar]
- 34.International Conference Debates Vaccination Hesitancy and Parental Refusal. Second annual conference, Seattle, July 16, 2006.
- 35.Limb M. “Vaccine hesitancy” means scientists need to be more honest about risks. BMJ (Clinical research ed 2011; 342:d2479. [DOI] [PubMed] [Google Scholar]
- 36.Rees H, Madhi SA. Will the Decade of Vaccines mean business as usual? Lancet. 2011;378:382–5. doi: 10.1016/S0140-6736(11)60710-1. [DOI] [PubMed] [Google Scholar]
- 37.Luthy KE, Beckstrand RL, Peterson NE. Parental hesitation as a factor in delayed childhood immunization. J Pediatr Health Care. 2009;23:388–93. doi: 10.1016/j.pedhc.2008.09.006. [DOI] [PubMed] [Google Scholar]
- 38.Velan B. Acceptance on the move: public reaction to shifting vaccination realities. Hum Vaccin. 2011;7:1261–70. doi: 10.4161/hv.7.12.17980. [DOI] [PubMed] [Google Scholar]
- 39.Gust DA, Darling N, Kennedy A, Schwartz B. Parents with doubts about vaccines: which vaccines and reasons why. Pediatrics. 2008;122:718–25. doi: 10.1542/peds.2007-0538. [DOI] [PubMed] [Google Scholar]
- 40.Freed GL, Clark SJ, Butchart AT, Singer DC, Davis MM. Parental vaccine safety concerns in 2009. Pediatrics. 2010;125:654–9. doi: 10.1542/peds.2009-1962. [DOI] [PubMed] [Google Scholar]
- 41.Bedford H, Lansley M. More vaccines for children? Parents’ views. Vaccine. 2007;25:7818–23. doi: 10.1016/j.vaccine.2007.08.057. [DOI] [PubMed] [Google Scholar]
- 42.Gowda C, Schaffer SE, Kopec K, Markel A, Dempsey AF. Does the relative importance of MMR vaccine concerns differ by degree of parental vaccine hesitancy?: An exploratory study. Hum Vaccin Immunother. 2012;9:8. doi: 10.4161/hv.22065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Opel DJ, Taylor JA, Mangione-Smith R, Solomon C, Zhao C, Catz S, et al. Validity and reliability of a survey to identify vaccine-hesitant parents. Vaccine. 2011;29:6598–605. doi: 10.1016/j.vaccine.2011.06.115. [DOI] [PubMed] [Google Scholar]
- 44.Smith PJ, Humiston SG, Marcuse EK, Zhao Z, Dorell CG, Howes C, et al. Parental delay or refusal of vaccine doses, childhood vaccination coverage at 24 months of age, and the Health Belief Model. Public Health Rep. 2011;126(Suppl 2):135–46. doi: 10.1177/00333549111260S215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Rosenstock IM. Historical origins of the health belief model. Health Educ Monogr. 1974;2:328–86. doi: 10.1177/109019817800600406. [DOI] [PubMed] [Google Scholar]
- 46.Leach M, Fairhead J. Vaccine Anxieties - Global Science, Child Health and Society. London, 2007. [Google Scholar]
- 47.Hobson-West P. Understanding vaccination resistance: moving beyond risk. Health Risk Soc. 2003;5:273–83. doi: 10.1080/13698570310001606978. [DOI] [Google Scholar]
- 48.Casiday RE. Children’s health and the social theory of risk: insights from the British measles, mumps and rubella (MMR) controversy. Soc Sci Med. 2007;65:1059–70. doi: 10.1016/j.socscimed.2007.04.023. [DOI] [PubMed] [Google Scholar]
- 49.Poltorak M, Leach M, Fairhead J, Cassell J. ‘MMR talk’ and vaccination choices: an ethnographic study in Brighton. Soc Sci Med. 2005;61:709–19. doi: 10.1016/j.socscimed.2004.12.014. [DOI] [PubMed] [Google Scholar]
- 50.Kata A. Anti-vaccine activists, Web 2.0, and the postmodern paradigm--an overview of tactics and tropes used online by the anti-vaccination movement. Vaccine. 2012;30:3778–89. doi: 10.1016/j.vaccine.2011.11.112. [DOI] [PubMed] [Google Scholar]
- 51.Kane MA. Commentary: public perception and the safety of immunization. Vaccine. 1998;16(Suppl):S73–5. doi: 10.1016/S0264-410X(98)00302-8. [DOI] [PubMed] [Google Scholar]
- 52.Spier RE. Perception of risk of vaccine adverse events: a historical perspective. Vaccine. 2001;20(Suppl 1):S78–84, discussion S75-7. doi: 10.1016/S0264-410X(01)00306-1. [DOI] [PubMed] [Google Scholar]
- 53.François G, Duclos P, Margolis H, Lavanchy D, Siegrist CA, Meheus A, et al. Vaccine safety controversies and the future of vaccination programs. Pediatr Infect Dis J. 2005;24:953–61. doi: 10.1097/01.inf.0000183853.16113.a6. [DOI] [PubMed] [Google Scholar]
- 54.Poland GA, Spier R. Fear, misinformation, and innumerates: how the Wakefield paper, the press, and advocacy groups damaged the public health. Vaccine. 2010;28:2361–2. doi: 10.1016/j.vaccine.2010.02.052. [DOI] [PubMed] [Google Scholar]
- 55.Stefanoff P, Mamelund SE, Robinson M, Netterlid E, Tuells J, Bergsaker MA, et al. VACSATC working group on standardization of attitudinal studies in Europe Tracking parental attitudes on vaccination across European countries: The Vaccine Safety, Attitudes, Training and Communication Project (VACSATC) Vaccine. 2010;28:5731–7. doi: 10.1016/j.vaccine.2010.06.009. [DOI] [PubMed] [Google Scholar]
- 56.Mnookin S. The Panic Virus: A True Story of Medicine, Science, and Fear. New York, 2011. [Google Scholar]
- 57.Smith A, Yarwood J, Salisbury DM. Tracking mothers’ attitudes to MMR immunisation 1996-2006. Vaccine. 2007;25:3996–4002. doi: 10.1016/j.vaccine.2007.02.071. [DOI] [PubMed] [Google Scholar]
- 58.Gangarosa EJ, Galazka AM, Wolfe CR, Phillips LM, Gangarosa RE, Miller E, et al. Impact of anti-vaccine movements on pertussis control: the untold story. Lancet. 1998;351:356–61. doi: 10.1016/S0140-6736(97)04334-1. [DOI] [PubMed] [Google Scholar]
- 59.Mason BW, Donnelly PD. Impact of a local newspaper campaign on the uptake of the measles mumps and rubella vaccine. J Epidemiol Community Health. 2000;54:473–4. doi: 10.1136/jech.54.6.473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Wolfe RM, Sharp LK, Lipsky MS. Content and design attributes of antivaccination web sites. JAMA. 2002;287:3245–8. doi: 10.1001/jama.287.24.3245. [DOI] [PubMed] [Google Scholar]
- 61.Zimmerman RK, Wolfe RM, Fox DE, Fox JR, Nowalk MP, Troy JA, et al. Vaccine criticism on the World Wide Web. J Med Internet Res. 2005;7:e17. doi: 10.2196/jmir.7.2.e17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Keelan J, Pavri V, Balakrishnan R, Wilson K. An analysis of the Human Papilloma Virus vaccine debate on MySpace blogs. Vaccine. 2010;28:1535–40. doi: 10.1016/j.vaccine.2009.11.060. [DOI] [PubMed] [Google Scholar]
- 63.Witteman HO, Zikmund-Fisher BJ. The defining characteristics of Web 2.0 and their potential influence in the online vaccination debate. Vaccine. 2012;30:3734–40. doi: 10.1016/j.vaccine.2011.12.039. [DOI] [PubMed] [Google Scholar]
- 64.Davies P, Chapman S, Leask J. Antivaccination activists on the world wide web. Arch Dis Child. 2002;87:22–5. doi: 10.1136/adc.87.1.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Scullard P, Peacock C, Davies P. Googling children’s health: reliability of medical advice on the internet. Arch Dis Child. 2010;95:580–2. doi: 10.1136/adc.2009.168856. [DOI] [PubMed] [Google Scholar]
- 66.Betsch C, Brewer NT, Brocard P, Davies P, Gaissmaier W, Haase N, et al. Opportunities and challenges of Web 2.0 for vaccination decisions. Vaccine. 2012;30:3727–33. doi: 10.1016/j.vaccine.2012.02.025. [DOI] [PubMed] [Google Scholar]
- 67.Lagacé M-C, Elissalde J, Renaud L. L'utilisation des médias francophones du Québec et la perception des messages sur la santé, l'alimentation et l'activité physique: résultats de sondages dans la population québécoise. In: Lise Renaud (dir.). Les médias et la santé: de l'émergence à l'appropriation des normes sociales, ed. Québec, Presses de l'Université du Québec, 2010:323-42. [Google Scholar]
- 68.Kata A. A postmodern Pandora’s box: anti-vaccination misinformation on the Internet. Vaccine. 2010;28:1709–16. doi: 10.1016/j.vaccine.2009.12.022. [DOI] [PubMed] [Google Scholar]
- 69.Diethelm P, McKee M. Denialism: what is it and how should scientists respond? Eur J Public Health. 2009;19:2–4. doi: 10.1093/eurpub/ckn139. [DOI] [PubMed] [Google Scholar]
- 70.Dubé E, Bettinger JA, Halperin B, Bradet R, Lavoie F, Sauvageau C, et al. Determinants of parents’ decision to vaccinate their children against rotavirus: results of a longitudinal study. Health Educ Res. 2012;27:1069–80. doi: 10.1093/her/cys088. [DOI] [PubMed] [Google Scholar]
- 71.Betsch C, Renkewitz F, Betsch T, Ulshöfer C. The influence of vaccine-critical websites on perceiving vaccination risks. J Health Psychol. 2010;15:446–55. doi: 10.1177/1359105309353647. [DOI] [PubMed] [Google Scholar]
- 72.Plotkin SA. Vaccines in the 21st century. Infect Dis Clin North Am. 2001;15:307–27. doi: 10.1016/S0891-5520(05)70280-4. [DOI] [PubMed] [Google Scholar]
- 73.Poland GA, Murray D, Bonilla-Guerrero R. Science, medicine, and the future - New vaccine development. BMJ (Clinical research ed 2002; 324:1315-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Plotkin SA, Orenstein WA, Offit PA. Vaccines. Philadelphia: Saunders Elsevier, 2012. [Google Scholar]
- 75.Lantos JD, Jackson MA, Opel DJ, Marcuse EK, Myers AL, Connelly BL. Controversies in vaccine mandates. Curr Probl Pediatr Adolesc Health Care. 2010;40:38–58. doi: 10.1016/j.cppeds.2010.01.003. [DOI] [PubMed] [Google Scholar]
- 76.Kennedy AM, Brown CJ, Gust DA. Vaccine beliefs of parents who oppose compulsory vaccination. Public Health Rep. 2005;120:252–8. doi: 10.1177/003335490512000306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Dittmann S. Vaccine safety: risk communication--a global perspective. Vaccine. 2001;19:2446–56. doi: 10.1016/S0264-410X(00)00470-9. [DOI] [PubMed] [Google Scholar]
- 78.Plotkin SA. Lessons learned concerning vaccine safety. Vaccine. 2002;20(Suppl 1):S16–, 9. doi: 10.1016/S0264-410X(01)00303-6. [DOI] [PubMed] [Google Scholar]
- 79.Halsey NA. Limiting infant exposure to thimerosal in vaccines and other sources of mercury. JAMA. 1999;282:1763–6. doi: 10.1001/jama.282.18.1763. [DOI] [PubMed] [Google Scholar]
- 80.Physicians AAoF. Pediatrics AAo, Practices ACoI, Service USPH. Joint statement of the Amercian Academy of Family Physicians (AAFP), the American Academy of Pediatrics (AAP), the Advisory Committee on Immunization Practices (ACIP), and the United States Public Health Service (PHS). 2000. [Google Scholar]
- 81.Jacobson RM, Targonski PV, Poland GA. A taxonomy of reasoning flaws in the anti-vaccine movement. Vaccine. 2007;25:3146–52. doi: 10.1016/j.vaccine.2007.01.046. [DOI] [PubMed] [Google Scholar]
- 82.Mulholland EK, Bjorvatn B. Introduction of new vaccines in the healthcare system. In: Bloom BR, Lambert P-H, eds. The Vaccine Book. U.S.A., 2003:391-410. [Google Scholar]
- 83.Levine MM, Levine OS. Influence of disease burden, public perception, and other factors on new vaccine development, implementation, and continued use. Lancet. 1997;350:1386–92. doi: 10.1016/S0140-6736(97)03253-4. [DOI] [PubMed] [Google Scholar]
- 84.Batson A. Sustainable introduction of affordable new vaccines: the targeting strategy. Vaccine. 1998;16(Suppl):S93–8. doi: 10.1016/S0264-410X(98)00306-5. [DOI] [PubMed] [Google Scholar]
- 85.Plotkin SA. Vaccines: past, present and future. Nat Med. 2005;11(Suppl):S5–11. doi: 10.1038/nm1209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Schwartz JL, Caplan AL. Vaccination refusal: ethics, individual rights, and the common good. Prim Care. 2011;38:717–28, ix. doi: 10.1016/j.pop.2011.07.009. [ix.] [DOI] [PubMed] [Google Scholar]
- 87.Brown KF, Kroll JS, Hudson MJ, Ramsay M, Green J, Long SJ, et al. Factors underlying parental decisions about combination childhood vaccinations including MMR: a systematic review. Vaccine. 2010;28:4235–48. doi: 10.1016/j.vaccine.2010.04.052. [DOI] [PubMed] [Google Scholar]
- 88.Briss P, Shefer A, Rodewald L. Improving vaccine coverage in communities and healthcare systems. no magic bullets. Am J Prev Med. 2002;23:70–1. doi: 10.1016/S0749-3797(02)00438-5. [DOI] [PubMed] [Google Scholar]
- 89.Massé R. Culture et santé publique. Montréal: Gaëtan Morin Éditeur 1995:499. [Google Scholar]
- 90.Cooper LZ, Larson HJ, Katz SL. Protecting public trust in immunization. Pediatrics. 2008;122:149–53. doi: 10.1542/peds.2008-0987. [DOI] [PubMed] [Google Scholar]
- 91.Schmitt HJ, Booy R, Aston R, Van Damme P, Schumacher RF, Campins M, et al. How to optimise the coverage rate of infant and adult immunisations in Europe. BMC Med. 2007;5:11. doi: 10.1186/1741-7015-5-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Clark SJ, Cowan AE, Wortley PM. Influenza vaccination attitudes and practices among US registered nurses. Am J Infect Control. 2009;37:551–6. doi: 10.1016/j.ajic.2009.02.012. [DOI] [PubMed] [Google Scholar]
- 93.Hollmeyer HG, Hayden F, Poland G, Buchholz U. Influenza vaccination of health care workers in hospitals--a review of studies on attitudes and predictors. Vaccine. 2009;27:3935–44. doi: 10.1016/j.vaccine.2009.03.056. [DOI] [PubMed] [Google Scholar]
- 94.Posfay-Barbe KM, Heininger U, Aebi C, Desgrandchamps D, Vaudaux B, Siegrist CA. How do physicians immunize their own children? Differences among pediatricians and nonpediatricians. Pediatrics. 2005;116:e623–33. doi: 10.1542/peds.2005-0885. [DOI] [PubMed] [Google Scholar]
- 95.Katz-Sidlow RJ, Sidlow R. A look at the pediatrician as parent: experiences with the introduction of varicella vaccine. Clin Pediatr (Phila) 2003;42:635–40. doi: 10.1177/000992280304200710. [DOI] [PubMed] [Google Scholar]
- 96.Zimmerman RK, Bradford BJ, Janosky JE, Mieczkowski TA, DeSensi E, Grufferman S. Barriers to measles and pertussis immunization: the knowledge and attitudes of Pennsylvania primary care physicians. Am J Prev Med. 1997;13:89–97. [PubMed] [Google Scholar]
- 97.Connors CM, Miller NC, Krause VL. Universal hepatitis B vaccination: hospital factors influencing first-dose uptake for neonates in Darwin. Aust N Z J Public Health. 1998;22:143–5. doi: 10.1111/j.1467-842X.1998.tb01159.x. [DOI] [PubMed] [Google Scholar]
- 98.Zhang J, While AE, Norman IJ. Knowledge and attitudes regarding influenza vaccination among nurses: a research review. Vaccine. 2010;28:7207–14. doi: 10.1016/j.vaccine.2010.08.065. [DOI] [PubMed] [Google Scholar]
- 99.Leask J, Quinn HE, Macartney K, Trent M, Massey P, Carr C, et al. Immunisation attitudes, knowledge and practices of health professionals in regional NSW. Aust N Z J Public Health. 2008;32:224–9. doi: 10.1111/j.1753-6405.2008.00220.x. [DOI] [PubMed] [Google Scholar]
- 100.Jelleyman T, Ure A. Attitudes to immunisation: a survey of health professionals in the Rotorua District. N Z Med J. 2004;117:U769. [PubMed] [Google Scholar]
- 101.Dubé E, Defay F, Kiely M, Guay M, Boulianne N, Sauvageau C, et al. Vaccine hesitancy: attitudes of parents and health care workers. Poster presentation. 10th Canadian Immunization Conference, Vancouver, December 3-5, 2012. [Google Scholar]
- 102.Norton SP, Scheifele DW, Bettinger JA, West RM. Influenza vaccination in paediatric nurses: cross-sectional study of coverage, refusal, and factors in acceptance. Vaccine. 2008;26:2942–8. doi: 10.1016/j.vaccine.2008.03.033. [DOI] [PubMed] [Google Scholar]
- 103.Lyren A, Leonard E. Vaccine refusal: issues for the primary care physician. Clin Pediatr (Phila) 2006;45:399–404. doi: 10.1177/0009922806289581. [DOI] [PubMed] [Google Scholar]
- 104.Diekema DS, American Academy of Pediatrics Committee on Bioethics Responding to parental refusals of immunization of children. Pediatrics. 2005;115:1428–31. doi: 10.1542/peds.2005-0316. [DOI] [PubMed] [Google Scholar]
- 105.Leib S, Liberatos P, Edwards K. Pediatricians’ experience with and response to parental vaccine safety concerns and vaccine refusals: a survey of Connecticut pediatricians. Public Health Rep. 2011;126(Suppl 2):13–23. doi: 10.1177/00333549111260S203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Petousis-Harris H, Goodyear-Smith F, Turner N, Soe B. Family physician perspectives on barriers to childhood immunisation. Vaccine. 2004;22:2340–4. doi: 10.1016/j.vaccine.2003.10.037. [DOI] [PubMed] [Google Scholar]
- 107.Sherris J, Friedman A, Wittet S, Davies P, Steben M, Saraiya M. Chapter 25: Education, training, and communication for HPV vaccines. Vaccine 2006; 24 Suppl 3:S3/210-8. [DOI] [PubMed] [Google Scholar]
- 108.Brownlie J, Howson A. ‘Between the demands of truth and government’: health practitioners, trust and immunisation work. Soc Sci Med. 2006;62:433–43. doi: 10.1016/j.socscimed.2005.05.033. [DOI] [PubMed] [Google Scholar]
- 109.Healy CM, Pickering LK. How to communicate with vaccine-hesitant parents. Pediatrics. 2011;127(Suppl 1):S127–33. doi: 10.1542/peds.2010-1722S. [DOI] [PubMed] [Google Scholar]
- 110.Fredrickson DD, Davis TC, Arnould CL, Kennen EM, Hurniston SG, Cross JT, et al. Childhood immunization refusal: provider and parent perceptions. Fam Med. 2004;36:431–9. [PubMed] [Google Scholar]
- 111.Tickner S, Leman PJ, Woodcock A. Factors underlying suboptimal childhood immunisation. Vaccine. 2006;24:7030–6. doi: 10.1016/j.vaccine.2006.06.060. [DOI] [PubMed] [Google Scholar]
- 112.Mills E, Jadad AR, Ross C, Wilson K. Systematic review of qualitative studies exploring parental beliefs and attitudes toward childhood vaccination identifies common barriers to vaccination. J Clin Epidemiol. 2005;58:1081–8. doi: 10.1016/j.jclinepi.2005.09.002. [DOI] [PubMed] [Google Scholar]
- 113.Sturm LA, Mays RM, Zimet GD. Parental beliefs and decision making about child and adolescent immunization: from polio to sexually transmitted infections. J Dev Behav Pediatr. 2005;26:441–52. doi: 10.1097/00004703-200512000-00009. [DOI] [PubMed] [Google Scholar]
- 114.Quadri-Sheriff M, Hendrix KS, Downs SM, Sturm LA, Zimet GD, Finnell SM. The role of herd immunity in parents’ decision to vaccinate children: a systematic review. Pediatrics. 2012;130:522–30. doi: 10.1542/peds.2012-0140. [DOI] [PubMed] [Google Scholar]
- 115.Roberts KA, Dixon-Woods M, Fitzpatrick R, Abrams KR, Jones DR. Factors affecting uptake of childhood immunisation: a Bayesian synthesis of qualitative and quantitative evidence. Lancet. 2002;360:1596–9. doi: 10.1016/S0140-6736(02)11560-1. [DOI] [PubMed] [Google Scholar]
- 116.Brewer NT, Fazekas KI. Predictors of HPV vaccine acceptability: a theory-informed, systematic review. Prev Med. 2007;45:107–14. doi: 10.1016/j.ypmed.2007.05.013. [DOI] [PubMed] [Google Scholar]
- 117.Trim K, Nagji N, Elit L, Roy K. Parental Knowledge, Attitudes, and Behaviours towards Human Papillomavirus Vaccination for Their Children: A Systematic Review from 2001 to 2011. Obstet Gynecol Int. 2012;2012:921236. doi: 10.1155/2012/921236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Kessels SJ, Marshall HS, Watson M, Braunack-Mayer AJ, Reuzel R, Tooher RL. Factors associated with HPV vaccine uptake in teenage girls: a systematic review. Vaccine. 2012;30:3546–56. doi: 10.1016/j.vaccine.2012.03.063. [DOI] [PubMed] [Google Scholar]
- 119.Chan ZC, Chan TS, Ng KK, Wong ML. A systematic review of literature about women’s knowledge and attitudes toward human papillomavirus (HPV) vaccination. Public Health Nurs. 2012;29:481–9. doi: 10.1111/j.1525-1446.2012.01022.x. [DOI] [PubMed] [Google Scholar]
- 120.Kohlhammer Y, Schnoor M, Schwartz M, Raspe H, Schäfer T. Determinants of influenza and pneumococcal vaccination in elderly people: a systematic review. Public Health. 2007;121:742–51. doi: 10.1016/j.puhe.2007.02.011. [DOI] [PubMed] [Google Scholar]
- 121.Ward L, Draper J. A review of the factors involved in older people’s decision making with regard to influenza vaccination: a literature review. J Clin Nurs. 2008;17:5–16. doi: 10.1111/j.1365-2702.2006.01861.x. [DOI] [PubMed] [Google Scholar]
- 122.Brien S, Kwong JC, Buckeridge DL. The determinants of 2009 pandemic A/H1N1 influenza vaccination: a systematic review. Vaccine. 2012;30:1255–64. doi: 10.1016/j.vaccine.2011.12.089. [DOI] [PubMed] [Google Scholar]
- 123.Bish A, Yardley L, Nicoll A, Michie S. Factors associated with uptake of vaccination against pandemic influenza: a systematic review. Vaccine. 2011;29:6472–84. doi: 10.1016/j.vaccine.2011.06.107. [DOI] [PubMed] [Google Scholar]
- 124.Evans M, Stoddart H, Condon L, Freeman E, Grizzell M, Mullen R. Parents’ perspectives on the MMR immunisation: a focus group study. Br J Gen Pract. 2001;51:904–10. [PMC free article] [PubMed] [Google Scholar]
- 125.Benin AL, Wisler-Scher DJ, Colson E, Shapiro ED, Holmboe ES. Qualitative analysis of mothers’ decision-making about vaccines for infants: the importance of trust. Pediatrics. 2006;117:1532–41. doi: 10.1542/peds.2005-1728. [DOI] [PubMed] [Google Scholar]
- 126.Bond L, Nolan T, Pattison P, Carlin J. Vaccine preventable diseases and immunisations: a qualitative study of mothers’ perceptions of severity, susceptibility, benefits and barriers. Aust N Z J Public Health. 1998;22:441–6. doi: 10.1111/j.1467-842X.1998.tb01411.x. [DOI] [PubMed] [Google Scholar]
- 127.Cassell JA, Leach M, Poltorak MS, Mercer CH, Iversen A, Fairhead JR. Is the cultural context of MMR rejection a key to an effective public health discourse? Public Health. 2006;120:783–94. doi: 10.1016/j.puhe.2006.03.011. [DOI] [PubMed] [Google Scholar]
- 128.Guay M, Gallagher F, Petit G, Ménard S, Clément P, Boyer G. Pourquoi les couvertures vaccinales chez les nourrissons de l'Estrie sont-elles sous-optimales? Sherbrooke: Centre de santé et de services sociaux - Institut universitaire de gériatrie de Sherbrooke, 2009:62 p. [Google Scholar]
- 129.Busse JW, Walji R, Wilson K. Parents’ experiences discussing pediatric vaccination with healthcare providers: a survey of Canadian naturopathic patients. PLoS One. 2011;6:e22737. doi: 10.1371/journal.pone.0022737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Taddio A, Ipp M, Thivakaran S, Jamal A, Parikh C, Smart S, et al. Survey of the prevalence of immunization non-compliance due to needle fears in children and adults. Vaccine. 2012;30:4807–12. doi: 10.1016/j.vaccine.2012.05.011. [DOI] [PubMed] [Google Scholar]
- 131.Kennedy A, Basket M, Sheedy K. Vaccine attitudes, concerns, and information sources reported by parents of young children: results from the 2009 HealthStyles survey. Pediatrics. 2011;127(Suppl 1):S92–9. doi: 10.1542/peds.2010-1722N. [DOI] [PubMed] [Google Scholar]
- 132.Paulussen TG, Hoekstra F, Lanting CI, Buijs GB, Hirasing RA. Determinants of Dutch parents’ decisions to vaccinate their child. Vaccine. 2006;24:644–51. doi: 10.1016/j.vaccine.2005.08.053. [DOI] [PubMed] [Google Scholar]
- 133.Ridda I, Motbey C, Lam L, Lindley IR, McIntyre PB, Macintyre CR. Factors associated with pneumococcal immunisation among hospitalised elderly persons: a survey of patient’s perception, attitude, and knowledge. Vaccine. 2008;26:234–40. doi: 10.1016/j.vaccine.2007.10.067. [DOI] [PubMed] [Google Scholar]
- 134.Downey L, Tyree PT, Huebner CE, Lafferty WE. Pediatric vaccination and vaccine-preventable disease acquisition: associations with care by complementary and alternative medicine providers. Matern Child Health J. 2010;14:922–30. doi: 10.1007/s10995-009-0519-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Jones L, Sciamanna C, Lehman E. Are those who use specific complementary and alternative medicine therapies less likely to be immunized? Prev Med. 2010;50:148–54. doi: 10.1016/j.ypmed.2009.12.001. [DOI] [PubMed] [Google Scholar]
- 136.Zuzak TJ, Zuzak-Siegrist I, Rist L, Staubli G, Simoes-Wüst AP. Attitudes towards vaccination: users of complementary and alternative medicine versus non-users. Swiss Med Wkly. 2008;138:713–8. doi: 10.4414/smw.2009.12681. [DOI] [PubMed] [Google Scholar]
- 137.Ernst E. Rise in popularity of complementary and alternative medicine: reasons and consequences for vaccination. Vaccine. 2001;20(Suppl 1):S90–3, discussion S89. doi: 10.1016/S0264-410X(01)00290-0. [DOI] [PubMed] [Google Scholar]
- 138.Boyer R, Fisher P, Gallant LA, Hurley J, Joly J, Munk P. Homeopathy in the paediatric population. Paediatr Child Health. 2006;11:76–7. [PMC free article] [PubMed] [Google Scholar]
- 139.Brewer NT, Chapman GB, Gibbons FX, Gerrard M, McCaul KD, Weinstein ND. Meta-analysis of the relationship between risk perception and health behavior: the example of vaccination. Health Psychol. 2007;26:136–45. doi: 10.1037/0278-6133.26.2.136. [DOI] [PubMed] [Google Scholar]
- 140.Rosenstock IM. The health belief model: Explaining health behavior through expectancies. In: Glanz KL, F.M.; Rimer B.K., ed. Health behavior and health education - Theory research and practice. San Francisco, CA: Jossey-Bass Publishers, 1991:39-62. [Google Scholar]
- 141.Slovic P. Perception of risk. Science (New York, NY 1987; 236:280-5. [DOI] [PubMed]
- 142.Calvez M. L’analyse culturelle du risque in A Tursz, Y Souteyrand, R Salmi (eds), Adolescence et risque, Paris, Syros 1993:75-87. [Google Scholar]
- 143.Poltorak M, Leach M, Fairhead J, Cassell J. ‘MMR talk’ and vaccination choices: an ethnographic study in Brighton. Soc Sci Med. 2005;61:709–19. doi: 10.1016/j.socscimed.2004.12.014. [DOI] [PubMed] [Google Scholar]
- 144.Serpell L, Green J. Parental decision-making in childhood vaccination. Vaccine. 2006;24:4041–6. doi: 10.1016/j.vaccine.2006.02.037. [DOI] [PubMed] [Google Scholar]
- 145.Hobson-West P. ‘Trusting blindly can be the biggest risk of all’: organised resistance to childhood vaccination in the UK. Sociol Health Illn. 2007;29:198–215. doi: 10.1111/j.1467-9566.2007.00544.x. [DOI] [PubMed] [Google Scholar]
- 146.Brownlie J, Howson A. 'Leaps of Faith' and MMR: An Empirical Study of Trust. Sociology. 2005;39:221–39. doi: 10.1177/0038038505050536. [DOI] [Google Scholar]
- 147.Streefland PH. Public doubts about vaccination safety and resistance against vaccination. Health Policy. 2001;55:159–72. doi: 10.1016/S0168-8510(00)00132-9. [DOI] [PubMed] [Google Scholar]
- 148.Ruijs WL, Hautvast JL, van Ijzendoorn G, van Ansem WJ, van der Velden K, Hulscher ME. How orthodox protestant parents decide on the vaccination of their children: a qualitative study. BMC Public Health. 2012;12:408. doi: 10.1186/1471-2458-12-408. [DOI] [PMC free article] [PubMed] [Google Scholar]