Abstract
Introduction: The aim of the present study is to review the economic burden of varicella disease and the benefit of universal varicella vaccination in different settings pending its implementation in all Italian regions.
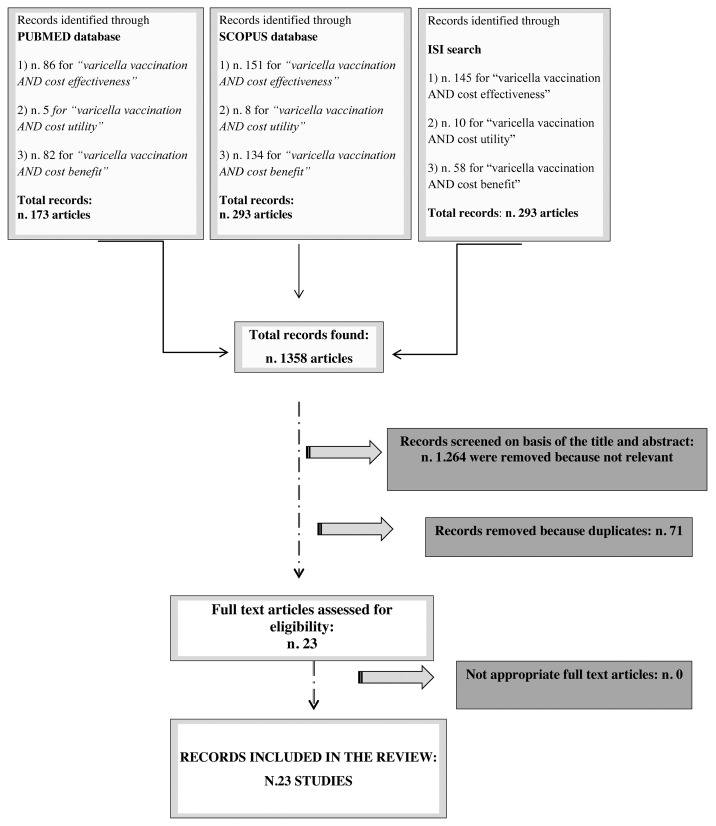
Materials and Methods: Research was conducted using PubMed, Scopus and ISI databases. Score quality and data extraction were performed for all included studies.
Results: Twenty-three articles met the criteria: 15 cost-effectiveness, 8 cost-benefit and one cost-utility analysis. Varicella vaccination could save the society from €637,762 (infant strategy) to 53 million annually (combined infant and adolescent strategy). The median and the mean quality scores resulted in 91.8% and 85.4% respectively; 11 studies were considered of high quality and 12 of low quality.
Discussion: The studies are favorable to the introduction of universal varicella vaccination in Italy, being cost saving and having a positive impact on morbidity. The quality score of the studies varied greatly: recent analyses were of comparable quality to older studies.
Keywords: varicella, vaccination, economic evaluation, cost effectiveness, cost utility, cost benefit
Introduction
Varicella or chickenpox is a common childhood exanthematic disease caused by the Varicella zoster virus (VZV) -a member of the herpesvirus family- which in most cases affects 5–10 y old children. Although benign, is highly contagious, pandemic and causes several complications that are frequently underestimated.1
Vaccination is one of the most effective and safe Public Health interventions available for the primary prevention of infectious diseases. This practice brings benefits not only to the vaccinated subjects, but also indirectly by inducing protection to non-vaccinated: herd immunity.
Since 1992 a varicella vaccine, consisting of live attenuated virus, is available and recommended for all children in the second year of life. The efficacy of varicella vaccination is about 95% in the prevention of moderate or severe cases and between 70–85% in the prevention of mild forms. The vaccine is safe, well tolerated and protection appears to be of long duration; it is now recommended as a two-dose schedule starting after the first year of life (second dose 1–3 mo apart or administered at 4–6 y).
The trend of varicella in Italy shows a series of fluctuation and basically increased until the mid-nineties. The maximum number of cases was reported in 2004 and amounted to more than 126.000 infected subjects. Following that peak, there was a decrease in cases, especially in 2005. Generally, the trend of varicella in Italy shows a decrement from 1996 to 2006 due to the introduction of the vaccine in some Regions (104.216 vs 97.634), but the number is still high.1
The reform of the V Title of the Constitution (Constitutional Law n.3/2001) endows all 21 Italian Regions with the responsibility of organizing and delivering health services while the State determines the essential health care interventions that all Regions have to offer to the population.2 Both mandatory (diphtheria, tetanus, poliomyelitis, hepatitis B) and non-mandatory vaccinations (pertussis, Hemophilus influenzae type b, measles, mumps and rubella) are included in essential health services. Nevertheless, vaccination policies in Italian Regions have been extremely heterogeneous in the last few years, with the same vaccine offered free of charge to all newborns and susceptible adolescents in seven regions, and only to people at risk in the remaining 14 Regions. There are even differences within the same region, related to the disparate vaccination strategies of Local Health Units.
In several countries routine varicella vaccination for all children has been introduced into the national immunisation schedule, e.g., Germany,3 Greece,4 Australia,5 Canada,6 Republic of Korea,7 Saudi Arabia8 and the United States of America (USA).9 In Spain, as in Italy, it’s only at regional level.10
Along with the adoption of routine vaccination program, a two dose schedule has been recommended in Greece and by the Spanish Association of Pediatrics.11 In Germany, the combined MMRV (measles-mumps-rubella-varicella) vaccine can be used, in place of separate injections of measles mumps- rubella (MMR) and varicella vaccines, with the two doses administered close together (at least 1 mo apart). A short interval between the doses enhanced compliance and vaccine coverage. Also, a good immune response has been obtained when the MMRV vaccine was given to children with an interval of 1 to 6 y, as in Finland.12 In other European countries (e.g., Belgium, Norway), MMR vaccines are administered with a longer schedule (7 to 12 y apart). A long interval for the second dose of varicella-containing vaccine is associated with higher risk of breakthrough disease between doses and could have negative impact on vaccine coverage.13
In the USA, a two-dose schedule for varicella vaccination has already been implemented, and a decrease in the number of patients with varicella -including those with breakthrough disease- has been observed.14,15 The Advisory Committee on Immunization Practices (ACIP) recommends the first dose of vaccine administered at 12 to 15 mo and the second dose at 4 to 6 y or at an earlier age, provided the interval between the two doses is 3 mo.9 Furthermore, the American Academy of Pediatrics recommends either MMR and varicella vaccines separately, or the MMRV be used for the first dose. Generally, the use of MMRV for dose 2 is preferred over separate injections.16
Regarding varicella vaccination coverage, data are not routinely collected by all Italian Regions; hence, the national coverage is assessed every 5 y by survey method. The survey conducted in 2008, among children aged 12–24 mo, showed a rate of 17%.17 The rate is very low compared with other developed countries with routine varicella vaccination program, such as the USA (90.8% among children aged 19–35 mo in 2011)18 and Australia (83% among children aged 24 mo in 2011).19 The Italian coverage rate is also lower than in Japan, which has a voluntary varicella vaccination program (90% for children up to 4 y old and 35% among those 1 y of age, in 2011).20
The Italian National Immunization Plan 2012–2014 (NIP), approved in February 2012, has the primary objective to harmonize vaccine strategies, and to ensure an active offer and free vaccination priority for the general population. In particular, the Plan states that varicella vaccination should become universally recommended in all Regions, albeit from 2015, after obtaining the results of the pilot programs activated in eight regions (Basilicata, Calabria, Puglia, Sardinia, Sicily, Tuscany, Veneto and the Province of Bolzano).21
The aim of the present study is to evaluate the economic burden of varicella disease and the benefit of universal varicella vaccination pending its implementation in all Italian regions.
Results
Identification of relevant research
Using the aforementioned inclusion criteria we found (see Figure 1):
Figure 1. Flow-chart of the selection process
- 173 articles for Pubmed search;
- 293 articles for Scopus search;
- 213 articles for ISI search.
A total of 1358 articles were found for all strings, of which 1264 were removed because they were not relevant and 71 articles were duplicates in two or all search engines. At the end of the evaluation, 23 articles met the pre-determined criteria described above.22-44
Quality Assessment
The 23 articles reviewed, with the assigned score quality, are shown in Table 1. The maximum quality score of 113/113 (100%) was obtained by Coudeville L. et al. 200436 and Brisson M. et al. 2002,26 and the lowest score was 71/107 (66.3%) assigned to Jean-Jasmin LM et al. 2004.35 The median score resulted in a value of 91.8% (Table 1).
Table 1. Score quality of the included studies by year of publication (according to the Drummond’s checklist modified by La Torre et al.).
| Authors (year of publication) |
Scuffham et al. 1999. | Domingo D. et al. 1999 | Coudeville L. et al. 1999 | Scuffham et al. 1999. | Brisson M. et al.2002 | Wutzler P. et al. 2002 |
Getsios D. et al. 2002 | Hui-Chun Hsu et al. 2003 |
Brisson M. et al.2003 | Banz K. et al. 2003 |
Hanslik T. et al.2003 | Thiry N. et al. 2004 |
Ginsbe-rg GM. et al. 2004 | Jasmin LM et al. 2004 | Coudeville L. et al. 2004 | Tseng HF et al. 2005 | Coudeville L. et al. 2005 | Lenne X. et al. 2006 | Hammerschmidt T. et al. 2007 | Valentim J. Et al. 2008 | Bonanni P. et al. 2008 | Banz K. et al. 2009 |
Zhou F. et al. 2008 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Study Design SCORE /ITEMS (26 score items) |
26/26 | 26/26 | 26/26 | 19/26 | 26/26 | 23/26 | 23/26 | 26/26 | 26/26 | 26/26 | 26/26 | 26/26 | 22/26 | 18/26 | 26/26 | 26/26 | 26/26 | 22/26 | 19/26 | 23/26 | 26/26 | 26/26 | 19/26 |
|
Data Collection SCORE/ ITEMS (45 score items) |
33/36 | 39/42 | 42/45 | 32/45 | 42/42 | 39/39 | 39/39 | 32/45 | 45/45 | 42/42 | 42/42 | 45/45 | 45/45 | 35/42 | 42/42 | 38/42 | 42/45 | 33/39 | 33/36 | 39/39 | 39/45 | 45/45 | 36/42 |
|
Analysis and interpretation of results SCORE/ ITEMS (48 score items) |
35/42 | 39/45 | 41/48 | 39/48 | 45/45 | 39/45 | 45/45 | 36/45 | 42/48 | 42/45 | 42/45 | 45/48 | 32/48 | 18/39 | 45/45 | 26/39 | 42/45 | 39/45 | 32/45 | 42/45 | 44/48 | 45/48 | 36/42 |
|
TOTAL SCORE/ ITEMS (119 total score) |
94/ 104 = 90.3% |
104/ 113 = 92% |
109/ 119 = 91.5% |
90/ 119 = 75.6% |
a113/ 113 = 100% |
b101/ 110 = 91.8% |
107/ 110 = 97.2% |
94/ 116 = 81% |
113/ 119 = 94.9% |
110/ 113 = 97.3% |
110/ 113 = 97.3% |
116/ 119 = 97.4% |
99/ 119 = 83.1% |
c71/ 107 = 66.3% |
a113/ 113 = 100% |
90/ 107 = 84.1% |
110/ 116 = 94.8% |
94/ 110 = 85.4% |
84/ 107 = 78,5% |
104/ 110 = 94.5% |
109/ 119 = 91.5% |
116/ 119 = 97.4% |
91/ 110 = 82.7% |
a Highest score; bMedian score; cLowest score
Considering the median score of the 23 articles, we found that 11 were of high quality (articles with assigned score over the median value), while the remaining 12 were of low quality (articles with assigned score under the median value). The mean score quality for all 23 articles considered was 85.41%.
The review evidenced that the quality score of the studies varied over years, even in the same year and in analyses conducted by the same authors: Scuffham et al.22 vs. Scuffham et al.23 got 90.3% and 75.6% respectively; Coudeville L. et al. in 1999,25 in 2004,36 and 2005,38 obtained respectively 91.5%, 100% and 94.8%. The differences are especially evident in the 3rd section - analysis and interpretation of results - of the Drummond’s checklist. No difference is evident in the quality of the examined studies along the years.
Type of Economic evaluation of the included studies
The classification of the studies is based on the type of economic evaluation:
- CEA (cost-effectiveness analysis) was performed in 15 economic evaluation studies;22,23,26-28,31-34,37-39,41,42,44
- CBA (cost-benefit analysis) was evaluated by 8 studies;24,25,29,35-37,40,43
- CUA (cost-utility analysis) was considered in the study performed by Brisson M. et al. 2003.38
Among the CEA, nine studies demonstrate the cost-effectiveness of childhood varicella vaccination compared with no vaccination.26,27,31,34,38,39,41,42,44 The results of Scuffham et al.22,23 varied in different environments: in 1999 they affirmed that the introduction of varicella program is cost saving for the New Zealand society, while in Australia, the childhood vaccine program is still preferred but has greater costs than the no vaccination program. Furthermore, according to Getsios et. al.,28 the childhood vaccination program is not cost-effective for the Canadian healthcare system.
Thiry et al.33 underlined the economic savings of an adolescent program in Italy, while Hanslik T. et al.32 concluded that targeted vaccination of non-immune adolescents and adults could reduce medical and financial burden of varicella in countries where no routine childhood immunization is implemented.
The only CUA included in the review (Brisson M. et al.30) does not consider the childhood program as a cost saving strategy compared with the adolescent one.
Finally, all the CBA substantially reported that varicella vaccine can reduce the number of cases, complications and hospitalizations.
The population and the countries considered were different in the studies: 14 analyses were conducted in Europe, 3 in America, 4 in Asia and 2 in Oceania.
Discussion
The present review includes 23 studies on varicella vaccination, which highlight the importance of varicella vaccine and the economic burden of the disease both from the societal and the healthcare perspective. Generally, varicella vaccination is cost saving from the societal perspective, infact BCR ranges between €637,762 (childhood strategy)22 and 53 million annually (combined childhood and adolescent strategy).27
The three studies conducted in Italy33,36,43 support a routine varicella vaccination program, being cost saving and having a positive impact on morbidity. For recommended vaccination of adolescents to be cost saving for the NHS - up to €292.134 savings in direct treatment costs- the overall price of the vaccine would have to decrease below €25.10. The society will definitely benefit from a catch-up program, targeting children aged 2–11 y old, which can prevent the greatest number of varicella outcomes and avoid 45% of cases.33
The analysis by Coudeville et al.36 states that a routine childhood immunization represents a good option for Italy. Similarly, the study by Bonanni et al.43 demonstrates that the introduction of universal varicella vaccination in young children (with or without an adolescent catch-up program) would be very effective in reducing the high disease burden in Italy. They also clarified that significant net savings are obtained from the societal perspective, while universal vaccination is not cost-saving to the Italian National Health System (NHS), but the amount needed to avoid a case or gain a year of life is very low and favorable all the same.
The introduction of MMRV vaccines given in a two-dose schedule could influence the cost-effectiveness of varicella vaccination in different settings. The analysis performed in Germany, demonstrated that two doses of MMRV vaccine are cost-saving from a societal and a health system perspective (BCR of 2.56 and 1.08, respectively) compared with an adolescent immunisation strategy with one dose of varicella vaccine.40 Furthermore, the study conducted in the USA highlighted that, compared with no intervention, the two-dose regimen is cost-saving from a societal perspective (BCR = 2.73). However, compared with 1-dose program, the incremental second dose was not cost saving from a societal perspective (BCR = 0.56).42
In addition, the MMRV vaccine provides other benefits by increasing the level of protection and, thus, limiting the risk of breakthrough cases. It also reduces the number of injections to complete vaccination, leading to major vaccine acceptance and improvement of the vaccination coverage rate13,40,41. Consequently, adding varicella vaccination to the routine vaccination program and implementation of the two-dose schedule with MMRV should be taken into account in countries where it has not been implemented.
In conclusion, the scenarios presented by the 23 articles analyzed are heterogeneous but are also undoubtedly favorable to the introduction of universal varicella vaccination. The results should be handled in consideration of the studies quality. Fortunately for the Italian context, the analysis by Coudeville L. et al.36 obtained the highest quality score (100%), followed by Thiry et al.33 (97.4%) and Bonanni et al.43 (91.5%). In 2003, Bonanni P.45 affirmed that compulsory varicella vaccination will not be introduced in Italy, confirmed by Thiry et al.33 in 2004, since the ultimate aim of the Italian NHS is the abolition of compulsory vaccination. It is foreseen, by the National Vaccination Plan 2012–2014, that from 2015 childhood routine vaccination will be offered free of charge during the second year of life in all Italian Regions. Further public health interventions will be therefore necessary to inform and educate the general population and to avoid a drastic drop of vaccination coverage in Italy; healthcare workers will surely have a key role in this process.
On the basis of the review results, it’s possible to conclude that the implementation of universal vaccination in all Italian regions by 2015 will be cost-saving from the societal perspective, and will imply a favorable cost-effectiveness profile from the NHS perspective.
Materials and Methods
Identification of relevant studies
A literature review was conducted using three electronic medical journal databases: Scopus, PubMed and ISI engines for published studies on economic evaluations of varicella vaccination programs. The keywords used were “vaccination”, “varicella”, “cost effectiveness,” “cost utility,” and “cost benefit”. Combined searches were performed for: “varicella vaccination AND cost effectiveness,” “varicella vaccination AND cost utility”, “varicella vaccination AND cost benefit.” Search criteria are summarized in Figure 1.
The selection was limited to articles published in English and Italian language and we applied date restrictions from 1999 to 2011 included. We selected all studies focused on the economic evaluation of varicella vaccination programs without limit of population and country.
All the review process, including search and selection (identification, screening, eligibility of included studies) was performed according to the PRISMA criteria46 (Fig. 1).
In the selection process, abstracts were initially read independently by two researchers to identify potentially eligible full text papers which were then retrieved and assessed in order to decide on the final inclusion.
Articles were examined and were excluded if: (1) the research was based on modeling the impact of a combined varicella and zoster vaccination program on the epidemiology of varicella zoster virus; (2) studies were not pertaining to varicella vaccination; (3) the full text was not available. When Medline outcomes overlapped, all duplicate articles were eliminated.
Quality assessment and data extraction
For each selected study, two researchers (RS and BU) independently assessed the quality according to the original Drummond’s checklist47 (Table 1) modified by la Torre et al.,48 weighting-median score for each item by different experts.
Discrepancies between the two investigators were solved by oral discussion and consensus with a senior investigator (GLT). Each item was assigned with the median weight attributed by the consensus, if applicable. Finally, the global score was computed summing up weights of each item. To compare different studies, global scores were referred in percentage, to the highest score achievable with the weighted Drummond’s checklist.
Drummond’s checklist is composed of 35 items divided into 3 sections: study design, data collection and analysis and interpretation of results. To weight the items, a group of experts was asked to attribute a score according to their importance. The weighted scores assigned by the consensus to study design, data collection and analysis and interpretation of results were 26, 45 and 48, respectively. For each item section, the maximum achievable score was as follows: (1) Study design (7 items): Maximum global score = 26; (2) Data collection (14 items): Maximum global score = 45; (3) Analysis and interpretation of results (14 items): Maximum global score = 48. When the item was not applicable to the study we reduced the Maximum global score from the relative weighted score item.
Two reviewers used a data collection form to independently abstract data from the studies. The information extracted was: references, publication year and type of analyses, alternatives, nation/ perspective, sample, efficacy measures/cost measure and results. The reviewers discussed any discrepancies in their results to reach an agreement. The characteristics of each study are shown in Table 2.
Table 2. Characteristics of the selected studies by year of publication and types of economic analysis.
| References | Type of analyses | Alternatives | Nation/ Perspective |
Sample | Efficacy Measures/ cost measures | Main Results |
|---|---|---|---|---|---|---|
| Scuffham et al. 1999 | CEA | 1. adding the varicella vaccine to the existing childhood immunization schedule 2. the current New Zealand situation: vaccine is available on a user-pays basis |
New Zealand/ societal and healthcare system | Cohort of 57.200 children 15 mo olds |
1.Direct and indirect cost; 2.aBCR; 3.bCER |
The total cost of a vaccination program is over NZD2.6 million annually (€1,658,180.821); in the absence of a program the total cost of vaccinations is over NZD3.6 million (€2,295,942.671). By introducing a varicella vaccination program, society saves NZD1 million annually (€637,761.851). |
| Domingo D, et al. 1999 | CBA | 1.Vaccination at 15 mo of age; 2. No vaccination (susceptible subject; immunized; disease) |
Spain/ 1.Societal perspective 2.healthcare system |
150 children 15 mo old | 1.Direct and indirect cost | The vaccination program was cost beneficial if vaccine price were less than PT6013 (€36.142) per dose. The total saving of the program would be PT368 million (€2,211,724.542). |
| Coudeville L. et al. 1999 | CBA | 1. Preventive strategy (vaccination for children and medical treatment of residual cases of varicella) 2. Curative strategy (no vaccination and medical treatment of patients with varicella) |
France/ 1.Society 2. Patient |
1. Children less than 6 y old 2. Individual patients presenting with varicella two specific investigations–an epidemiological model and a prospective observational study (1832 cases studied) |
1.cANB 2. Direct and indirect costs |
The analysis demonstrates the value of varicella vaccination when associated with measles-mumps-rubella (MMR) vaccination: if varicella and MMR vaccines are co-administered, the vaccination of 80% of the children against varicella leads to a reduction in medical costs associated with varicella including that of vaccination, ranging from 10 to 77% according to the values adopted for vaccination costs, varicella treatment costs, discount rate and vaccine efficacy. |
| Scuffham et al. 1999 | CEA | Four strategies were considered: 1.Being the status quo - no vaccination. 2. Under strategy II (all infants), the vaccine is given at the same time (but as a separate injection) as the trivalent measles, mumps and rubella (MMR) vaccine currently administered to children at 12 mo of age. 3. In strategy III (adolescents without a history of varicella) vaccination is offered to 12 y olds who state they have not had varicella, without serological testing. 4.In strategy IV(catch-up), the adolescent program is combined with the infant program for the first 11years, to protect older children until the first cohort of vaccinated infants reaches 12 y of age. The cost effectiveness analysis was based on modeling the costs and consequences of strategies II and III relative to strategy I and strategy IV relative to strategy II. The latter comparison was made to examine the incremental cost-effectiveness of adding a catch-up strategy for 12-y olds to the infant program. |
Australia/ 1.Health care payer’s perspective 2. Societal perspective. |
1. Annual birth cohorts of infants (12 mo old) and 2. Adolescents (12 y old). |
1. Direct costs 2.Cost-effectiveness | The average cost per case of chickenpox averted was $64, $530 and $418 (€40.8; €337.91; € 266.511) in the infant, adolescent and catch-up programs, respectively. The infant program was the most cost-effective of the three. This program could avert 4.4 million cases, 13.500 hospitalisations and 30 fatalities for chickenpox over a 30-y period. Results were sensitive to the price of the vaccine and the discount rate, but relatively insensitive to changes in vaccine efficacy, coverage rates or vaccine complication rates. Improved accuracy of a negative varicella history in adolescents would substantially reduce the costs of the adolescent and catch-up programs making these programs feasible. Conclusions: the infant vaccine program is the preferred program, but the direct costs of any of the vaccination programs considered here are greater than the direct costs of no vaccination program. |
| Brisson M. et al.2002 | CEA | Three different vaccination strategies are investigated in this study: 1. routine vaccination at 1 y of age (infant strategy); 2. infant strategy + vaccination of 5- and 11-y-old children for the first 5 y of the program (catch-up strategy); and 3. routine vaccination at 12 y (preteen strategy). These three strategies are being considered for implementation in Canada. The possible impact of zoster and breakthrough varicella is then investigated in separate analyses. |
Canada/ 1.Health payer’s perspective 2. Societal perspective |
Prospectively 179 children aged 1–9 y with absence of any major chronic disease. Costs were separated into two age categories day care (1–4 y) and school age (5–9 y). In the analysis was applied results of the school group to children 5–15 y. |
1.Direct and indirect costs 2.Cost-effectiveness 3. BCR |
Assuming no impact of vaccination on zoster, varicella vaccination is estimated to cost CAD45.000, 51.000 and 18.000 (€35.259; €39.960; €14.1043) per dLYG from the health payer’s perspective for infant, infant with catch-up campaign, and preteen programs, respectively. From the societal perspective, mass infant varicella vaccination was estimated to be highly cost saving in Canada. Importantly, infant varicella vaccination could result in a short- to medium-term increase of zoster incidence and thus cause vaccination to be highly cost-ineffective (CAD118.000 per LYG; €92.5163) under the health payer’s perspective. From a health payer’s perspective the preteen vaccination is the only strategy that is deemed cost-effective. |
| Wutzler 2002 | CEA | 1. No vaccination 2. children vaccination strategy 3. adolescent vaccination strategy 4. combined vaccination strategy: children plus a catch-up of adolescents |
Germany/ Societal and payer | 1. children 15 mo old 2. 11–12 y old 3. children 15 mo old and adolescents 11–12 y old |
1.BCR 2.Direct and indirect costs |
The most favorable strategies: children and combined vaccination (decrease of the number of varicella infections by 82.7% and 83.5% compared with no vaccination respectively). Annual net savings ranging between 8.18 million € (adolescent strategy) and 53 million € (combined vaccination strategy). |
| Getsios 2002 | CEA | Vaccination program of 1-y-old children, with and without a catch-up program for susceptible 12-y-olds, vs No vaccination strategy |
Canada/ health care system and societal | Children 12 mo old with or without catch up at age 12 | 1.Direct and indirect costs | The overall costs of varicella will reduce by 4 million CAD (€3,136,134.233), but costs to the health care system will increase by CAD2 million (€1,568,067.123). From the health care system perspective, vaccination would cost CAD42 (€32.933) per discounted case avoided. |
| Hui-Chun Hsu et al. 2003 | CBA | 1.Varicella vaccination Strategy vs 2. No vaccination In the non-vaccinated group, subjects followed the disease natural history as follows: subjects are infected with chickenpox and may or may not develop into symptomatic cases after around 2-week incubation period. |
Taiwan/ 1.Health care payer’s perspective 2. Societal perspective. |
188 varicella cases that were sampled from local general practitioners and pediatricians scattered over northern, central, southern, and eastern areas of Taiwan between October 2000 and February 2001. |
1.Direct and indirect costs 2. BCR 2.Willingness-to-pay |
Taking indirect costs into account, the net saving due to vaccination program was TWD 425 million (€11,393,240.794) from the societal perspective. In terms of benefit-cost ratio, a mass varicella vaccination program could only save TWD 0.34 (€0.014) in discounted costs for each dollar incurred in a vaccination program from health care payer's perspective whereas save TWD 2.06 (€0.064) from the societal viewpoint. Results based on the willingness-to-pay (WTP) method showed the Net Present Value (NPV) of the vaccination program was estimated as -TWD 272 million (€7,291,674.104). |
| Brisson M. et al. 2003 | CUA | 1.No vaccination VS Vaccination: 2. Infant strategy (vaccination at 90% coverage). 3. Catch-up strategy: infant strategy with catch-up (at 80% coverage) 4. Adolescent strategy (at 80% coverage). |
England and Wales/ NHS e societal | 1. < 2 y 2. 2–11 y 3. Eleven years |
1.QALY 2.Direct and indirect costs |
The adolescent strategy is cost saving: £18. 000 (€22,3685) per QALY gained (NHS perspective). Infant and catch up strategy: not cost saving. |
| Banz K. et al. 2003 | CEA | Three interventions were compared with no vaccination: 1. universal vaccination of around 15 mo old healthy children 2. vaccination of susceptible adolescents (11–12 y of age) 3. the combined strategy. |
Germany/ 1.Societal perspective 2.the payers’, i.e. sickness funds, perspective. |
two age groups: 1.children between 0 and 12 y 2. adolescents/adults ≥ 13 |
1.Direct and indirect costs 2.CER 3. BCR |
Using a coverage rate of 85% and a vaccine efficacy rate of 86% routine children vaccination could prevent around 611.000 varicella cases and over 4700 major complications per year. Average yearly cost savings for the society are €51.3 million. The BCR is 4.12. From the third-party payer’s perspective, the BCR is 1.75 which is a consequence of significant reimbursement of parent’s lost earnings by German sickness funds. The adolescent vaccination strategy has a favorable BCR ratio of 8.44 from the societal perspective, but clearly inferior medical effects. The combined vaccination strategy showed similar results as the children strategy. |
| Hanslik T. et al.2003 | CEA | Vaccination strategies with and without prior serotesting: 1.No intervention 2. Strategy “Ab test, Vax negative” 3. Strategy “Vax all” |
France/ 1.Healthcare payer perspective 2.Societal perspective |
Hypothetical cohorts of persons aged 15–45 y with a negative or uncertain history of varicella |
1.Vaccination costs 2.Varicella costs in persons ≥ 15 y 3.Work loss |
With serotesting, compared with no intervention, the cost per case avoided and per year of life saved for subjects aged 15 y were €335 and €55.100, respectively. From the societal perspective, such screening and vaccination might save costs. |
| Thiry N. et al. 2004 | CEA | 1. Compulsory vaccination (without screening) 2.Recommended vaccination (anamnestic screening) 3. Vaccination (blood test) 4. Vaccination (both test: anamnestic + blood) |
Italy/ Societal and payers |
1. 11-y-old adolescents 2. Vaccination of susceptible adolescents (11yr) 3. Vaccination of 11 y adolescents 4. Vaccination of 11 y adolescents |
1.LYG, CER 2.Direct/indirect cost |
Compulsory vaccination cost = €1.476, 351. The vaccination scenarios save from €108.207 (for private vaccination) to €292.134 for compulsory vaccination. |
| Ginsberg GM. et al. 2004 | CEA | 1. No vaccination 2. Nationwide vaccination campaign of 1 y old children |
Israel/NHS and societal | Cohort of known susceptible children born in 2001, when they are 1 y old |
1.BCR 2.Direct and indirect costs |
Reduction of direct healthcare costs from $1.96 million (€152,968,197.356) to $165,000 (€128,7746). Direct benefits to the health services = $1.80 million (€1.40 million). BCR = 1.63/1. |
| Jasmin LM, et al. 2004 | CBA | Adding a varicella vaccine to the existing immunization schedule in Singapore. | Singapore/ societal and healthcare system | 15-mo old infants in 1993 | 1.Direct and indirect cost | Universal vaccination was cost beneficial, with a cost benefit ratio of 2.25: 1; the cost savings was mainly from a societal perspective rather than the health care payer’s. |
| Coudeville L. et al. 2004 | CBA | 1. routine vaccination program for children aged 1–2 y with different levels of vaccination coverage (90%, 70% and 45%) without any catch-up program 2. routine vaccination program for children aged 1–2 y with different levels of vaccination coverage (90%, 70% and 45%) completed by a catch-up program for 6-y-old children over the first 5 y of vaccine marketing 3. routine vaccination program for children aged 1–2 y with different levels of vaccination coverage (90%, 70% and 45%) completed by a catch-up program during the first year of vaccine marketing for children aged 2–11 y. |
Italy/ 1.Societal Perspective including both direct and indirect costs 2. A Health-System perspective, limited to costs supported by Italian Health Authorities |
1. Italian children aged 1–2 y with different levels of vaccination coverage 2. Italian children aged 2–11 y. |
1.Cost of varicella vaccination 2.Cost of chickenpox treatment per episode 3.Total treatment cost 4.Chickenpox-related work losses per episode of chickenpox5.Direct and indirect costs |
A routine vaccination program has a clearly positive impact on chickenpox morbidity. Respectively, 68% and 57% of chickenpox-related hospitalisations and deaths could be prevented with a 90% coverage rate. With vaccination costs being more than offset by a reduction in chickenpox treatment costs in the base case, such a program could also induce savings from both a societal and a health-system perspective (40% and 12% savings, respectively for a 90% coverage rate). A lower coverage rate reduces cost savings, but there is still a 9% decrease in overall societal costs for a 45% coverage rate. Although the reduction in total societal costs was robust to the sensitivity analyses performed, a slight uncertainty remains regarding cost reduction from a health-system perspective. However, in this latter perspective, even in the worst-case scenario of the sensitivity analysis, routine vaccination programmes may be cost effective, the worst-case scenario for cost parameters leading to cost per life-year gained of €2853. Catch-up programmes combined with routine vaccination should lead to further cost reductions from a societal perspective: 15% for a massive catch-up during the first year of vaccine marketing compared with toddlers’ vaccination alone, and 11% for a catch-up focused on 6-y-old children for a period of 5 y. However, the impact of catch-up programmes on the costs from an Italian health-system perspective remains close to zero (± 1%). |
| Tseng HF et al. 2005 |
1. CEA 2. CBA |
1. Population-based data were obtained using the year 2000 annual outpatient claims and hospitalization discharge claims from the Southern branch and Kaoping branch of the Bureau of National Health Insurance (NHI), which covered 3,246,949 and 3,629,444 populations, respectively. 2. hypothetical cohort was created each year for 30 y. |
Taiwan/ 1.Health care payer’s Perspective 2. Societal perspective |
A model of the incidence and cost of varicella in a new 300,000hypothetical birth cohort was created each year in the next 30 y. These children were assumed either to have received 80% varicella vaccination coverage (as provided by the government) or 10% private coverage (current situation). |
1. Direct medical cost including outpatient visits and hospitalization 2.Indirect costs of work loss |
The benefit-cost analysis showed that one dollar invested in the program would cost extra 46 cents in direct medical expense, but would save extra 45 cents considering the societal expenses. Substantial economic benefits can occur due to the averted unproductive days for parents. |
| Coudeville L. et al. 2005 | CEA | The economic analysis is based on the comparison of epidemiological and economic consequences of a routine vaccination strategy (routine vaccination program + medical treatment of residual varicella cases) with those of a “no vaccination” strategy (medical treatment of varicella cases). | France and Germany/ 1. Societal perspective 2. a third-party payer perspective |
Entire population, divided here in 100 birth cohorts of identical size, on the number and age distribution of varicella cases. |
1.Direct/indirect costs 2.Cost-effectiveness | A routine vaccination program has a clear positive impact on varicella-related morbidity in both countries. With a 90% coverage rates, the number of varicella-related deaths was reduced by 87% in Germany and by 84% in France. In addition, with a coverage rates of 90%, routine varicella vaccination induces savings in both countries from both societal (Germany 61%, France 60%) and third-party payer perspectives (Germany 51%, France 6.7%). For lower coverage rates, routine vaccination remains cost saving from a third-party payer perspective in Germany but not in France, where it is nevertheless cost-effective (cost per life year gained of 6521 € in the base case with a 45% coverage rates). |
| Lenne X, et al. 2006 | CEA | 1. No vaccination 2. Routine vaccination program for children aged 1–2 y. 3. Routine vaccination program for children aged 1–2 y completed by a catch-up program during the first year of vaccine marketing for children aged 2–11 y. |
Spain/ 1.Societal perspective 2. healthcare system |
Cohort of 440.000 children |
1.Direct and indirect cost; 2.BCR; 3.CER |
Routine varicella vaccination program for children in Spain is cost-saving from the societal perspective and highly cost-effective for the Health Care System (cost-effectiveness ratio estimated at €3982 per LYG, with a small increase in the costs) |
| Hammerschmidt T, et al. 2007 | CBA | 1. Adolescent immunization strategy of 12–15 y old using a monovalent varicella vaccine; 2.Universal mass vaccination of any child aged 11–23 mo with a two-dose schedule MMRV vaccine (first dose between 11 and 14 mo) and a catch-up of 2–17 y old with a monovalent varicella vaccine. | Germany/ 1.Societal perspective 2. healthcare system |
German epidemiological data |
1.Direct and indirect cost; 2.BCR |
Universal mass vaccination of infants aged 11–23 mo including catch-up vaccination of older children and adolescents can significantly reduce the number of varicella cases, complications and hospitalizations by 84–90%. |
| Valentim J, 2008 | CEA | 1. Universal varicella vaccination of 12 mo-old children 2. Targeted vaccination of individuals of high risk for severe disease. |
Brazil/ 1.Societal perspective 2. healthcare system |
Population in Caieiras (Southeast of Brazil) | 1.Direct and indirect cost | The program is cost-effective (R$ 14.749 and R$ 16.582 (€5,535.447; €6,223.387) per life-year saved under the societal and the healthcare system’s perspective, respectively). The program’s cost-effectiveness is highly sensitive to the vaccine price and number of doses. |
| Bonanni P.et al. 2008 | CBA | 1. Toddlers vaccination with two doses only 2. Adolescents vaccination 3. Toddlers vaccination combined with adolescent catch-up programmes. |
Italy/ NHS and societal |
1. Toddlers 1–1.5 y old 2. Adolescents 13 y old 3. Toddlers (1–1.5 y) and adolescents (13 y) |
1. BCR 2.Direct/ indirect costs |
Strategy III resulted in the highest annual net savings of €51 million while Strategy II was found to generate the lowest annual net savings amounting to €10 million. NHS perspective: all three strategies would not determine annual net savings in Italy |
| Banz K. et al. 2009 | CEA | 1. Vaccination of adolescents 2.Universal vaccination of toddlers 3. Strategy 2 plus catch-up vaccination of susceptible adolescents. |
Switzerland/ Payer and societal |
1. 11–15 y old adolescents with a negative or uncertain history for chickenpox 2. Toddlers at age 1 to 2 y 3. Strategy 2 plus catch-up vaccination of 11–15 y old |
1.BCR and LYG 2.Direct/ indirect costs |
Both universal childhood vaccination strategies with or without catch-up result in net savings from the societal perspective: BCR = 1.22 or 1.29, respectively. In contrast, the model predicts net costs from the payer perspective (BCR of 0.27 and 0.30, respectively). |
| Zhou F, et al. 2008 | CEA | 1. One-dose vaccination program 2.Two-dose varicella vaccination program 3. No vaccination |
USA/ Societal perspective |
Hypothetical US birth cohort of 4,100,000 infants born in 2006 |
1.Direct and indirect cost 2.CER, 3.BCR |
Compared with no vaccination, both the 1-dose program (BCR = 4.37) and 2-dose program (BCR = 2.73) were estimated to be cost saving from the societal perspective. Compared with the 1-dose program, the incremental second dose was not cost saving (societal incremental BCR, 0.56). The incremental cost-effectiveness ratio for the second dose was $343 (€268 6) per case prevented, or $109,000 (€ 85,1696) per QALY saved. |
a BCR: Benefit-cost ratio; bCER: Cost-effectiveness ratio; cANB: Actualized net benefit; dLYG: life year gained. 1Exchange rate 1 New Zealand Dollar = 0.64 EUR; 2Exchange rate 1 pesetas = 0.01 EUR (until 19 June 2001); 3Exchange rate 1 Canadian Dollar = 0.78 EUR; 4Exchange rate 1 Taiwan Dollar = 0.03 EUR; 5Exchange rate 1 £ = 1.24 EUR; 6Exchange rate 1 US$ = 0.78 EUR; 7Exchange rate 1 Brazilian Real = 0.38 EUR. All exchange rates, except for Spanish pesetas, are updated to 20.11.2012.
Glossary
Abbreviations:
- VZV
Varicella zoster virus
- NIP
National Immunization Plan
- CEA
cost-effectiveness analysis
- CBA
cost-benefit analysis
- CUA
cost-utility analysis
- NHS
National Health System
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
Disclosure of Potential Conflicts of Interest
No potential conflicts of interest were disclosed.
Footnotes
Previously published online: www.landesbioscience.com/journals/vaccines/article/25228
References
- 1.Epicentro: Il portale dell'epidemiologia per la sanità pubblica. Centro Nazionale di Epidemiologia, Sorveglianza e Promozione della Salute. Available at: http://www.epicentro.iss.it/problemi/varicella/varicella.asp; last access 19.11.12.
- 2.Presidente del Consiglio dei Ministri. D.P.C.M. Definizione dei livelli essenziali di assistenza. G.U.8 Febbraio 2002, n.33, S.
- 3.Institut RK. Empfehlungen der Ständigen Impfkommission (STIKO) am Robert Koch-Institut/Stand: Juli 2006. Epidemiol Bull. 2006;30:235–54. [Google Scholar]
- 4.Childhood immunisation calendar, Greece. Available at: http://www.mohaw.gr/gr/thefuture/anakoinoseis/Timetable%202008.xls
- 5.Macartney KK, Burgess MA. Varicella vaccination in Australia and New Zealand. J Infect Dis. 2008;197(Suppl 2):S191–5. doi: 10.1086/522157. [DOI] [PubMed] [Google Scholar]
- 6.National Advisory Committee on Immunization National Advisory Committee on Immunization (NACI) update on varicella. Can Commun Dis Rep. 2004;30:1–26. [PubMed] [Google Scholar]
- 7.Sadzot-Delvaux C, Rentier B, Wutzler P, Asano Y, Suga S, Yoshikawa T, et al. Varicella vaccination in Japan, South Korea, and Europe. J Infect Dis. 2008;197(Suppl 2):S185–90. doi: 10.1086/522163. [DOI] [PubMed] [Google Scholar]
- 8.WHO vaccine preventable disease monitoring system: Immunization schedules by antigen, selection centre. Available at: http/www.who.int/immunization_monitoring/en/globalsummary/scheduleselect.cfm
- 9.Marin M, Güris D, Chaves SS, Schmid S, Seward JF, Advisory Committee on Immunization Practices, Centers for Disease Control and Prevention (CDC) Prevention of varicella: recommendations of the Advisory Committee on Immunization Practices (ACIP) MMWR Recomm Rep. 2007;56(RR-4):1–40. [PubMed] [Google Scholar]
- 10.Alfonsi V, D’Ancona F, Giambi C, Nacca G, Rota MC, Regional Coordinators for Infectious Diseases and Vaccinations Current immunization policies for pneumococcal, meningococcal C, varicella and rotavirus vaccinations in Italy. Health Policy. 2011;103:176–83. doi: 10.1016/j.healthpol.2011.10.002. [DOI] [PubMed] [Google Scholar]
- 11.Bernaola Iturbe E, Giménez Sánchez F, Baca Cots M, de Juan Martín F, Díez Domingo J, Garcés Sánchez M, et al. Spanish Association of Pediatrics [Vaccination schedule of the Spanish Association of Pediatrics: recommendations 2007] An Pediatr (Barc) 2007;66:62–9. doi: 10.1016/s1695-4033(07)70295-3. [DOI] [PubMed] [Google Scholar]
- 12.Vesikari T, Baer M, Willems P. Immunogenicity and safety of a second dose of measles-mumps-rubella-varicella vaccine in healthy children aged 5 to 6 years. Pediatr Infect Dis J. 2007;26:153–8. doi: 10.1097/01.inf.0000250689.09396.21. [DOI] [PubMed] [Google Scholar]
- 13.Bonanni P, Breuer J, Gershon A, Gershon M, Hryniewicz W, Papaevangelou V, et al. Varicella vaccination in Europe - taking the practical approach. BMC Med. 2009;7:26. doi: 10.1186/1741-7015-7-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shapiro ED, Vazquez M, Esposito D, Holabird N, Steinberg SP, Dziura J, et al. Effectiveness of 2 doses of varicella vaccine in children. J Infect Dis. 2011;203:312–5. doi: 10.1093/infdis/jiq052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kattan JA, Sosa LE, Bohnwagner HD, Hadler JL. Impact of 2-dose vaccination on varicella epidemiology: Connecticut--2005-2008. J Infect Dis. 2011;203:509–12. doi: 10.1093/infdis/jiq081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Committee on Infectious Diseases Policy statement—Prevention of varicella: update of recommendations for use of quadrivalent and monovalent varicella vaccines in children. Pediatrics. 2011;128:630–2. doi: 10.1542/peds.2011-1968. [DOI] [PubMed] [Google Scholar]
- 17.Gruppo di lavoro ICONA. ICONA 2008: Indagine di Copertura vaccinale Nazionale nei bambini e negli adolescenti. Rapporti ISTISAN 09/29. Istituto Superiore di Sanità, Roma; 2009.
- 18.Centers for Disease Control and Prevention (CDC) National, state, and local area vaccination coverage among children aged 19-35 months--United States, 2011. MMWR Morb Mortal Wkly Rep. 2012;61:689–96. [PubMed] [Google Scholar]
- 19.Ward K, Dey A, Hull B, Quinn HE, Macartney K, Menzies R. Evaluation of Australia’s varicella vaccination program for children and adolescents. Vaccine. 2013;31:1413–9. doi: 10.1016/j.vaccine.2012.12.052. [DOI] [PubMed] [Google Scholar]
- 20.Ozaki T. Varicella vaccination in Japan: necessity of implementing a routine vaccination program. J Infect Chemother. 2013;19:188–95. doi: 10.1007/s10156-013-0577-x. [DOI] [PubMed] [Google Scholar]
- 21.Piano Nazionale Prevenzione vaccinale 2012-2014. Ministero della salute. Available at: http://www.salute.gov.it/dettaglio/phPrimoPianoNew.jsp?id=339; last access 19.11.12.
- 22.Scuffham P, Devlin N, Eberhart-Phillips J, Wilson-Salt R. The cost-effectiveness of introducing a varicella vaccine to the New Zealand immunisation schedule. Soc Sci Med. 1999;49:763–79. doi: 10.1016/S0277-9536(99)00115-X. [DOI] [PubMed] [Google Scholar]
- 23.Scuffham PA, Lowin AV, Burgess MA. The cost-effectiveness of varicella vaccine programs for Australia. Vaccine. 1999;18:407–15. doi: 10.1016/S0264-410X(99)00261-3. [DOI] [PubMed] [Google Scholar]
- 24.Díez Domingo J, Ridao M, Latour J, Ballester A, Morant A. A cost benefit analysis of routine varicella vaccination in Spain. Vaccine. 1999;17:1306–11. doi: 10.1016/S0264-410X(98)00394-6. [DOI] [PubMed] [Google Scholar]
- 25.Coudeville L, Paree F, Lebrun T, Sailly JC. The value of varicella vaccination in healthy children: cost-benefit analysis of the situation in France. Vaccine. 1999;17:142–51. doi: 10.1016/S0264-410X(98)00161-3. [DOI] [PubMed] [Google Scholar]
- 26.Brisson M, Edmunds WJ. The cost-effectiveness of varicella vaccination in Canada. Vaccine. 2002;20:1113–25. doi: 10.1016/S0264-410X(01)00437-6. [DOI] [PubMed] [Google Scholar]
- 27.Wutzler P, Neiss A, Banz K, Goertz A, Bisanz H. Can varicella be eliminated by vaccination? Potential clinical and economic effects of universal childhood varicella immunisation in Germany. Med Microbiol Immunol. 2002;191:89–96. doi: 10.1007/s00430-002-0123-4. [DOI] [PubMed] [Google Scholar]
- 28.Getsios D, Caro JJ, Caro G, De Wals P, Law BJ, Robert Y, et al. Instituting a routine varicella vaccination program in Canada: an economic evaluation. Pediatr Infect Dis J. 2002;21:542–7. doi: 10.1097/00006454-200206000-00012. [DOI] [PubMed] [Google Scholar]
- 29.Hsu HC, Lin RS, Tung TH, Chen TH. Cost-benefit analysis of routine childhood vaccination against chickenpox in Taiwan: decision from different perspectives. Vaccine. 2003;21:3982–7. doi: 10.1016/S0264-410X(03)00270-6. [DOI] [PubMed] [Google Scholar]
- 30.Brisson M, Edmunds WJ. Varicella vaccination in England and Wales: cost-utility analysis. Arch Dis Child. 2003;88:862–9. doi: 10.1136/adc.88.10.862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Banz K, Wagenpfeil S, Neiss A, Goertz A, Staginnus U, Vollmar J, et al. The cost-effectiveness of routine childhood varicella vaccination in Germany. Vaccine. 2003;21:1256–67. doi: 10.1016/S0264-410X(02)00431-0. [DOI] [PubMed] [Google Scholar]
- 32.Hanslik T, Boëlle PY, Schwarzinger M, Carrat F, Freedberg KA, Valleron AJ, et al. Varicella in French adolescents and adults: individual risk assessment and cost-effectiveness of routine vaccination. Vaccine. 2003;21:3614–22. doi: 10.1016/S0264-410X(03)00405-5. [DOI] [PubMed] [Google Scholar]
- 33.Thiry N, Beutels P, Tancredi F, Romanò L, Zanetti A, Bonanni P, et al. An economic evaluation of varicella vaccination in Italian adolescents. Vaccine. 2004;22:3546–62. doi: 10.1016/j.vaccine.2004.03.043. [DOI] [PubMed] [Google Scholar]
- 34.Ginsberg GM, Somekh E. Cost containment analysis of childhood vaccination against varicella in Israel. J Infect. 2004;48:119–33. doi: 10.1016/S0163-4453(03)00079-3. [DOI] [PubMed] [Google Scholar]
- 35.Jean-Jasmin LM, Lynette SP, Stefan M, Kai CS, Chew FT, Wah LB. Economic burden of varicella in Singapore--a cost benefit estimate of implementation of a routine varicella vaccination. Southeast Asian J Trop Med Public Health. 2004;35:693–6. [PubMed] [Google Scholar]
- 36.Coudeville L, Brunot A, Giaquinto C, Lucioni C, Dervaux B. Varicella vaccination in Italy : an economic evaluation of different scenarios. Pharmacoeconomics. 2004;22:839–55. doi: 10.2165/00019053-200422130-00003. [DOI] [PubMed] [Google Scholar]
- 37.Tseng HF, Tan HF, Chang CK. Varicella epidemiology and cost-effectiveness analysis of universal varicella vaccination program in Taiwan. Southeast Asian J Trop Med Public Health. 2005;36:1450–8. [PubMed] [Google Scholar]
- 38.Coudeville L, Brunot A, Szucs TD, Dervaux B. The economic value of childhood varicella vaccination in France and Germany. Value Health. 2005;8:209–22. doi: 10.1111/j.1524-4733.2005.04005.x. [DOI] [PubMed] [Google Scholar]
- 39.Lenne X, Diez Domingo J, Gil A, Ridao M, Lluch JA, Dervaux B. Economic evaluation of varicella vaccination in Spain: results from a dynamic model. Vaccine. 2006;24:6980–9. doi: 10.1016/j.vaccine.2006.04.051. [DOI] [PubMed] [Google Scholar]
- 40.Hammerschmidt T, Bisanz H, Wutzler P. Universal mass vaccination against varicella in Germany using an MMRV combination vaccine with a two-dose schedule: an economic analysis. Vaccine. 2007;25:7307–12. doi: 10.1016/j.vaccine.2007.08.017. [DOI] [PubMed] [Google Scholar]
- 41.Valentim J, Sartori AMC, de Soárez PC, Amaku M, Azevedo RS, Novaes HM. Cost-effectiveness analysis of universal childhood vaccination against varicella in Brazil. Vaccine. 2008;26:6281–91. doi: 10.1016/j.vaccine.2008.07.021. [DOI] [PubMed] [Google Scholar]
- 42.Zhou F, Ortega-Sanchez IR, Guris D, Shefer A, Lieu T, Seward JF. An economic analysis of the universal varicella vaccination program in the United States. J Infect Dis. 2008;197(Suppl 2):S156–64. doi: 10.1086/522135. [DOI] [PubMed] [Google Scholar]
- 43.Bonanni P, Boccalini S, Bechini A, Banz K. Economic evaluation of varicella vaccination in Italian children and adolescents according to different intervention strategies: the burden of uncomplicated hospitalised cases. Vaccine. 2008;26:5619–26. doi: 10.1016/j.vaccine.2008.07.096. [DOI] [PubMed] [Google Scholar]
- 44.Banz K, Iseli A, Aebi C, Brunner M, Schmutz AM, Heininger U. Economic evaluation of varicella vaccination in Swiss children and adolescents. Hum Vaccin. 2009;5:847–57. doi: 10.4161/hv.9898. [DOI] [PubMed] [Google Scholar]
- 45.Bonanni P. Italie-la politique de vaccination. Vax Info. 2003;36:6–8. [Google Scholar]
- 46.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Int J Public Health. 2009;4:94–131. doi: 10.7326/0003-4819-151-4-200908180-00136. [DOI] [PubMed] [Google Scholar]
- 47.Drummond MF, Jefferson TO, The BMJ Economic Evaluation Working Party Guidelines for authors and peer reviewers of economic submissions to the BMJ. BMJ. 1996;313:275–83. doi: 10.1136/bmj.313.7052.275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.La Torre G, Nicolotti N, de Waure C, Ricciardi W. Development of a weighted scale to assess the quality of cost-effectiveness studies and an application to the economic evaluations of tetravalent HPV vaccine. Int J Public Health. 2011;19:103–11. doi: 10.1007/s10389-010-0377-z. [DOI] [Google Scholar]