Abstract
Purpose
Anterior cervical fixation is a procedure widely employed in medical practice, with different fixation systems in use. This study aimed to perform a systematic review of the literature comparing the use of rigid and dynamic cervical plates regarding the fusion rate and complications.
Methods
A search was conducted in PubMed, Lilacs, and Cochrane databases and selecting comparative studies on the use of rigid and dynamic cervical plates. Prospective randomized studies were selected to describe the final results regarding the clinical and radiological outcomes; comparative observational studies were also cited. Complications of using the dynamic cervical plate were also evaluated.
Results
Seven comparative studies were included in the review. Five of these were prospective and randomized studies that did not report significant differences in the clinical outcome. One study reported a faster fusion rate when dynamic cervical plate was used, and another study showed a higher fusion rate when a dynamic cervical plate was applied on multiple levels. Four studies investigated the complications of using a dynamic plate and reported that changes in the cervical curvature angle and material failure were the most frequent complications.
Conclusions
There were no clinical differences between the two types of cervical fixation systems. A difference in the fusion rates could not be found at any follow-up time or in any of the studies. There was a loss of lordotic correction in the dynamic systems and a higher rate of complications in patients with a loss of lordotic correction.
Keywords: Cervical spine, Surgery, Implants, Static and dynamic plates, Complications
Introduction
Anterior cervical plate fixation is a widely used procedure for surgically stabilizing the cervical spine in degenerative diseases such as myelopathy and radiculopathy [1, 2]. The anterior cervical fixation procedure has been used since 1950s, mainly to obtain the fusion of the fixed segment [2, 3]. The plates-and-screws system for anterior fixation was introduced in 1964, but it was in the early 1980s that Cáspar developed a commercially released system [3]. This technique expanded among the cervical surgical procedures, and complications associated with the instrumentation material, such as screw and plate displacement, were reported, reaching rates of 22–44 % [4, 5]. The instrumentation failure rate due to pseudarthrosis reaches over 40 % in some studies [2, 3]. In an attempt to avoid such complications and to increase the fusion rate, several types of materials have been developed [1–6].
The first fixation systems used plates and non-constrained screws. After numerous problems, a system of locks was developed for the plate screws, thereby reducing the number of failures [1, 7]. These systems were called static or rigid systems. Later studies showed a lower fusion rate using these systems [5], and based on Wolff’s theory that states that a greater axial load on the graft leads to a faster and more effective fusion [1, 3, 4, 6–9], fixation systems with mobile plates and screws were created aiming to increase the fusion rate [1, 3]. These plates are usually referred to as dynamic plates [1–9].
The present study aimed to conduct a systematic review of the literature demonstrating the differences between the rigid and dynamic systems that are used for anterior cervical fixation.
Methods
A search was performed in the main electronic databases PubMed/MedLine, Central Cochrane of Randomized Trials and Lilacs Database. The references of the selected studies were analyzed, and a manual search was performed in journals related to spine surgery, using a search protocol for articles that compare the use of rigid (or semi-rigid) versus dynamic cervical plates.
A specific search protocol was conducted to study the complications resulting from the use of these systems (“Appendices 1 and 2”).
Types of study
To show evidence of differences in the clinical and radiological outcomes, randomized trials that compared the use of a dynamic (or semi-rigid) cervical plate and a rigid cervical plate were included. To analyze the complications, all types of study designs for semi-rigid or dynamic systems were included. The results of non-randomized comparative studies were described to demonstrate real-life practice results. Surgeries performed on one or more treated segments were considered for the study.
Participants and intervention type
Studies that evaluated adults, who were operated on using a cervical plate to fixate the operated segment, and compared rigid, semi-rigid, or dynamic plates were considered for the present investigation.
Outcomes evaluated
Criteria that evaluated the clinical and radiological outcomes of both fixation systems were used. All complications related to the use of the dynamic plate were listed.
Selection of the studies
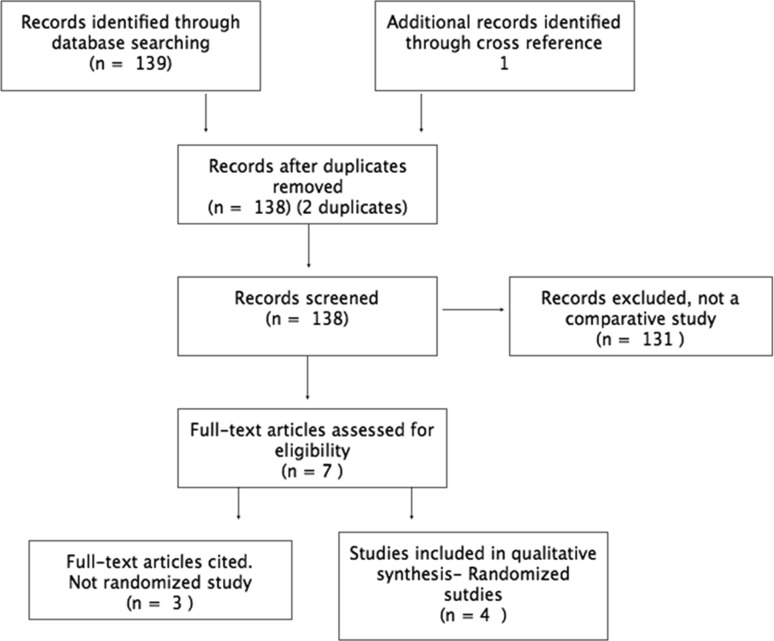
Both authors independently reviewed the titles and abstract and thereafter selected the studies for analysis. Only comparative studies evaluating dynamic and rigid plates were selected. Duplicated published papers in different times were removed. Disagreements in selection of papers by both authors were resolved under full evaluation of papers and discussion by both investigators (Fig. 1).
Fig. 1.
Flow diagram for comparative studies
Results
The search performed in the PubMed database yielded 133 related items (Fig. 1). In the Cochrane Central database, six initial articles were found. The Lilacs [Literatura Latino-Americana e do Caribe em Ciências da Saúde (Latin American and Caribbean Health Sciences Literature)] database did not yield any comparative studies on the topic.
The analysis of the titles identified 10 potential articles. An additional article [10] was added to the reference evaluation, resulting in 11 full-text articles evaluated. Four studies were not comparative and were therefore excluded. Ultimately, seven full-text articles were evaluated. Four randomized studies were included in the qualitative evidence synthesis (Table 1).
Table 1.
Randomized clinical trials evaluated
Three studies compared the effect of the static and dynamic systems in a non-randomized or retrospective way. These studies were not included in the quantitative evidence analysis, but they were described to evaluate the effectiveness in real-life clinical conditions. Table 2 shows their description. The outcomes were divided into clinical and radiological outcomes.
Table 2.
Observational studies evaluated
Clinical outcomes
Odom’s scale was used in two studies [2, 6], and the NDI (neck disability index) and the visual analog scale (VAS) were used in one of the studies [1]. Two of the studies did not evaluate clinical outcomes [4, 5]. All of the studies assessed radiological criteria. Table 3 lists the outcomes studied for each author.
Table 3.
Outcomes evaluated
| References | Outcomes evaluated | |
|---|---|---|
| Clinical | Radiological | |
| Randomized clinical trials—outcomes | ||
| Nunley et al. [1] | VAS/NDI | Fusion |
| Stulik et al. [4] | N/A | Fusion and mobility |
| Pitzen et al. [5] | VAS/NDI | Fusion and mobility |
| Ragab et al. [10] | N/A | Fusion |
| Observational studies—outcomes | ||
| DuBois et al. [2] | ODOM | Fusion |
| Goldberg et al. [12] | N/A | Fusion |
| Stancić et al. [6] | ODOM/NDI/SF-36 | Fusion |
Data extraction from the studies
Prospective and randomized studies
Nunley et al. [1], Pitzen et al. [5], Stulik et al. [4], and Ragab et al. [10] randomly compared the use of dynamic and rigid cervical plates. Table 1 lists the characteristics of the studies. The studies by Pitzen et al. and Stulik et al. were considered duplicate results from the same sample, and the study by Pitzen et al. was considered for analysis in the present review due to the longer follow-up period (2 years) and the greater number of cases. The study by Stulik occurred within the first 6 months of follow-up of the study by Pitzen et al.
Clinical outcomes
Nunley et al. [1] and Pitzen et al. [5] used the VAS and NDI as the clinical outcome criterion, whereas Ragab et al. [10] did not perform a clinical analysis of the patients in the postoperative follow-up. VAS and NDI: Neither of the two studies revealed significant differences between the two groups. The studies only reported significant differences when comparing the pre- and postoperative period, regardless of the groups.
Radiological outcome
As outcomes, Nunley et al. [1] and Ragab et al. [10] described the presence of fusion or non-fusion, and Pitzen et al. [5] described the evaluation of segmental mobility, presence or absence of translucency, bone sclerosis, and bone trabeculation in the graft region as a fusion criterion in both studied groups, as presented in Table 4.
Table 4.
Randomized trials studied outcomes
Radiological outcomes
Nunley et al. [1] evaluated the fusion and reported that, when the two groups were compared regarding fusion, there was significance only when the instrumentation was performed at more than one level (p = 0.05), favoring the use of the dynamic plate.
Pitzen et al. [5] reported that there were no significant differences regarding the presence or absence of translucency, bone trabeculation, and sclerosis but that differences existed in the segmental mobility, as presented in Table 5.
Table 5.
Segmental mobility
| Pitzen et al. [5] | Segmental mobility | ||
|---|---|---|---|
| Static plate (segmental mobility in mm) | Dynamic plate (segmental mobility in mm) | ||
| Discharge | 1.0 | 1.7 | p = 0.124 |
| 3 months | 1.8 | 1.4 | p = 0.452 |
| 6 months | 1.6 | 0.8 | p = 0.02 |
| 2 years | 0.5 | 0.4 | p > 0.05 |
According to the result obtained by Pitzen et al., the use of a dynamic cervical plate caused a faster fusion rate when compared with the dynamic plate, given that at 6 months of follow-up there was a difference between the two groups, with p = 0.02 favoring the group that used the dynamic plate; however, there were no differences at 2 years of follow-up.
Ragab et al. [10] found no significant differences in fusion from the use of dynamic versus rigid plates.
Evaluation of the methodological quality
For randomized trials methodological quality assessment, the Cochrane Collaboration’s tool for assessing risk of bias was used [11] Table 6.
Table 6.
The Cochrane collaboration’s tool for assessing risk of bias
Non-randomized studies and retrospective studies
Clinical outcomes
Only the studies by Stancic et al. [6] and DuBois et al. [2] reported clinical results, and both used Odom’s scale. Both Dubois et al. and Stancić et al. reported no significant differences when the studied groups [namely, the dynamic-plate and control (rigid-plate) groups] were compared (p = 0.39 and p = 0.55, respectively) in Table 7.
Table 7.
Clinical outcome-observational studies
Radiographic outcomes
Stancić et al. [6] assessed the fusion using criteria that involved a radiological analysis regarding the rotation and translation of the screws and the Tribus grading scale for implant fixation.
During the first 6 months, Stancić obtained a fusion rate that was significantly lower in the dynamic group (1.53 ± 0.56 in the dynamic plate group versus 2.13 ± 0.62 in the rigid plate group, p = 0.000028), and there were no significant differences after analysis at 4 years of follow-up (1.13 ± 0.34 in the dynamic plate group versus 1.21 ± 0.52 in the rigid plate group, p = 0.44).
DuBois et al. [2] and Goldberg et al. [12] directly reported the presence of fusion or non-fusion.
DuBois et al. [2] demonstrated significant differences between the two groups; there were five pseudarthrosis cases in the dynamic fixation group and only one case in the group that used the rigid plate (p = 0.05).
The study by Goldberg et al. [12] revealed no significant differences in fusion between the two groups (Table 8).
Table 8.
Fusion rates on Non-randomized studies
Complications analysis
The survey conducted in the PubMed database presented 26 initial articles (the search protocol is detailed in “Appendix 2”). The analysis by title yielded five articles. The analysis by abstract led to the final result of three articles.
Two articles were found in the Cochrane Central database.
The Lilacs search did not return any study according to the search protocol.
The final evaluation revealed four studies describing complications from the use of dynamic plates (Table 9).
Table 9.
Studies describing complications from the use of dynamic plates
Data extraction from the complications
Epstein [13], employing a series of 116 patients, described one patient with adjacent-level disease, two patients with pseudarthrosis, one case of plate and graft extrusion, and seven fractures of the arthrodesis graft (11/116).
Okawa [14], in a series of 30 cases, reported six complications: two patients with graft migration, two patients with displaced screws, and two patients with a C7 body fracture.
Okawa [14] correlated the cervical lordotic angle with the complications. The patients who had major requirements for maintenance or correction of their cervical lordosis also exhibited complications (p < 0.05). The patients who were submitted to instrumentation in a greater number of levels were also associated with more complications (p < 0.05).
In a comparative, prospective, and non-randomized trial, Stancić et al. [6] reported a case of translucency >1 mm in the group that used a rigid plate and seven cases of heterotopic ossification in the group that used a dynamic plate; two of the latter cases progressed to ankylosis after 2 years of follow-up.
Among the randomized trials, only Pitzen et al. [5] described the complications separately. The author described four implant-related complications in the control group (rigid plate): one broken plate, two patients with an inferior displacement of the screw, and one patient with a broken screw; no complications were reported in the group with dynamic plates. Pitzen et al. compared the average loss of cervical lordosis between the rigid and the dynamic systems: the dynamic fixation was associated with greater loss of cervical lordosis at all follow-up periods compared (p < 0.05).
Discussion
Wolff’s theory is the basis for the development of the dynamic plates [1, 3, 4, 6–9]. According to this theory, the fusion rate is increased in grafts subjected to a greater axial load. Studies on the use of dynamic cervical plates were developed to obtain less rigid plates that would allow for axial loads on the grafts and higher fusion rates.
Only seven out of the 133 initially selected studies were comparative studies between the two types of cervical plates. Four studies were randomized, and one of them was considered a duplicate. Three randomized studies and three observational studies were analyzed.
The information hierarchy ranks randomized trials as superior in achieving the best available evidence. However, the results of observational studies have been included in the reviews because they are considered closer to real-life clinical practice, but caution is needed as the greatest bias potential is observed in these studies. The joint analysis of randomized and non-randomized studies is not a recommended procedure [11].
To extract the results from the clinical and radiological outcomes, the seven studies were separated into observational studies and randomized prospective studies. An independent search was conducted to investigate complications related to using a dynamic plate. The final result consisted of four articles.
The non-randomized and retrospective studies did not demonstrate clinical differences between the two types of systems.
The fusion rate of the dynamic system was lower than the fusion rate of rigid systems, at least in the initial evaluations of Stancić et al. [6] and throughout the follow-up of the study by DuBois et al. [2]. Stancić et al. emphasized that this difference was observed at 6 postoperative months and did not persist after 4 years, which leads to the conclusion that applying a rigid plate yields a faster fusion rate [1, 3, 4, 6–9].
The prospective randomized studies did not present any differences in the clinical outcomes. Regarding the fusion rate, Nunley et al. [1] showed differences between the two groups in favor of the dynamic plate, but only when it was used in a multilevel discectomy.
Pitzen et al. [5] observed a faster fusion rate in the dynamic plate group, and there were no differences at the 2-year follow-up.
There were no differences in the fusion rate in the study by Ragab et al. [10].
The studies do not present the absolute numbers, and their results are not stratified by group, which compromises the meta-analysis of these data.
It was not possible to group the complications described by the types of systems studied or to infer a higher incidence of any type of system. However, Pitzen et al. [5] and Okawa [14] demonstrated more complications when the cervical lordosis had to be maintained, and the dynamic plate was associated with worsening of the lordotic maintenance.
There are numerous methodological limitations in the studies analyzed: some authors did not provide the absolute results or the data stratified by group [1] for analysis in the text, only stating the final results.
Due to the surgical nature of the treatments, none of the comparative studies was double-blinded, and the randomization method was described in two of the three studies evaluated.
While this review was being concluded, an article reviewing the effect of the dynamic plate was published [15], and it included randomized and retrospective trials for the meta-analysis. We followed the recommendation of using observational studies only when randomized trials are not present and considered inadequate the joint evaluation of sets of studies with different methodologies [1].
In conclusion, there were no clinical differences between the two types of cervical fixation systems. A difference in the fusion rates could not be found at any follow-up time or in any of the studies. There is conflicting evidence (available only in one study) that dynamic fixation provides faster arthrodesis and a higher arthrodesis rate in multilevel fixations. There was a greater loss of lordotic correction in the dynamic systems (one study) and a higher rate of complications in patients with a loss of lordotic correction (one study).
Conflict of interest
None.
Appendix 1
Search protocol to comparative studies among rigid plate and dynamic plate
MedLine search:
#1. “Cervical spine” [All Fields] AND (dynamic[All Fields] OR semirigid[All Fields]) AND ((fixation[All Fields] OR (“instrumentation”[Subheading] OR “instrumentation”[All Fields]))).
#2-((“spinal cord compression”[MeSH Terms] OR (“spinal”[All Fields] AND “cord”[All Fields] AND “compression”[All Fields]) OR “spinal cord compression”[All Fields]) OR (“arthrodesis”[MeSH Terms] OR “arthrodesis”[All Fields])) AND (dynamic[All Fields] OR static[All Fields]) AND (anterior[All Fields] AND fixation[All Fields]) AND (“neck”[MeSH Terms] OR “neck”[All Fields] OR “cervical”[All Fields]).
#3-(spinal cord disease OR arthrodesis) (dynamic OR static) AND (anterior fixation) AND cervical.
.
Central Cochrane de Ensaios Randomizados
# Cervical spine AND dynamic plate.
Lilacs:
# Cervical spine.
# Cervical spine AND plate.
# Cervical spine AND randomized.
# Cervical spine AND dynamic plate.
Appendix 2
Search protocol for complications
Medline:
(“Cervical vertebrae”[MeSH Terms] OR (“cervical”[All Fields] AND “vertebrae”[All Fields]) OR “cervical vertebrae”[All Fields] OR (“cervical”[All Fields] AND “spine”[All Fields]) OR “cervical spine”[All Fields]) AND ((dynamic[All Fields] AND fixation[All Fields]) OR (dynamic[All Fields] AND (“bone plates”[MeSH Terms] OR (“bone”[All Fields] AND “plates”[All Fields]) OR “bone plates”[All Fields] OR “plate”[All Fields]))) AND (complication[All Fields] OR (“risk”[MeSH Terms] OR “risk”[All Fields]) OR damage[All Fields] OR harm[All Fields]).
Central Cochrane:
Cervical spine AND complications AND dynamic plate.
Lilacs:
Cervical spine AND complications AND dynamic plate.
Cervical spine AND complications.
References
- 1.Nunley PD, Jawahar A, Kerr EJ, 3rd, Cavanaugh DA, Howard C, Brandao SM. Choice of plate may affect outcomes for single versus multilevel ACDF: results of a prospective randomized single-blind trial. Spine J. 2009;9:121–127. doi: 10.1016/j.spinee.2007.11.009. [DOI] [PubMed] [Google Scholar]
- 2.DuBois CM, Bolt PM, Todd AG, Gupta P, Wetzel FT, Phillips FM. Static versus dynamic plating for multilevel anterior cervical discectomy and fusion. Spine J. 2007;7:188–193. doi: 10.1016/j.spinee.2006.07.004. [DOI] [PubMed] [Google Scholar]
- 3.Haid RW, Foley KT, Rodts GE, Barnes B. The Cervical Spine Study Group anterior cervical plate nomenclature. Neurosurg Focus. 2002;12:E15. doi: 10.3171/foc.2002.12.1.16. [DOI] [PubMed] [Google Scholar]
- 4.Stulik J, Pitzen TR, Chrobok J, Ruffing S, Drumm J, Sova L, Kucera R, Vyskocil T, Steudel WI. Fusion and failure following anterior cervical plating with dynamic or rigid plates: 6-months results of a multi-centric, prospective, randomized, controlled study. Eur Spine J. 2007;16:1689–1694. doi: 10.1007/s00586-007-0451-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pitzen TR, Chrobok J, Stulik J, Ruffing S, Drumm J, Sova L, Kucera R, Vyskocil T, Steudel WI. Implant complications, fusion, loss of lordosis, and outcome after anterior cervical plating with dynamic or rigid plates: two-year results of a multi-centric, randomized, controlled study. Spine (Phila Pa 1976) 2009;34:641–646. doi: 10.1097/BRS.0b013e318198ce10. [DOI] [PubMed] [Google Scholar]
- 6.Stancić M, Margetić P, Elabjer E, Milosević M. Axial vs. angular dynamization of anterior cervical fusion implants. Coll Antropol. 2008;32:221–229. [PubMed] [Google Scholar]
- 7.Steinmetz MP, Warbel A, Whitfield M, Bingaman W. Preliminary experience with the DOC dynamic cervical implant for the treatment of multilevel cervical spondylosis. J Neurosurg. 2002;97(3 Suppl):330–336. doi: 10.3171/spi.2002.97.3.0330. [DOI] [PubMed] [Google Scholar]
- 8.Bose B. Anterior cervical arthrodesis using DOC dynamic stabilization implant for improvement in sagittal angulation and controlled settling. J Neurosurg. 2003;98(1 Suppl):8–13. doi: 10.3171/spi.2003.98.1.0008. [DOI] [PubMed] [Google Scholar]
- 9.Lehmann W, Briem D, Blauth M, Schmidt U. Biomechanical comparison of anterior cervical spine locked and unlocked plate-fixation systems. Eur Spine J. 2005;14:243–249. doi: 10.1007/s00586-004-0746-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ragab AA, Hodges FS, Hill CP, McGuire RA, Tucci M. Dynamic anterior cervical plating for multi-level spondylosis: does it help? Evid Based Spine Care J. 2010;1:41–46. doi: 10.1055/s-0028-1100892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Higgins JPT, Green S (eds) (2011) Cochrane handbook for systematic reviews of interventions version 5.1.0 (updated March 2011). The Cochrane Collaboration. http://www.cochrane-handbook.org. Accessed 07/20/2013
- 12.Goldberg G, Albert TJ, Vaccaro AR, Hilibrand AS, Anderson DG, Wharton N. Short-term comparison of cervical fusion with static and dynamic plating using computerized motion analysis. Spine (Phila Pa 1976) 2007;32:E371–E375. doi: 10.1097/BRS.0b013e318060cca9. [DOI] [PubMed] [Google Scholar]
- 13.Epstein NE. Complication avoidance in 116 dynamic-plated single-level anterior corpectomy and fusion. J Spinal Disord Tech. 2007;20(5):347–351. doi: 10.1097/01.bsd.0000248257.10284.3b. [DOI] [PubMed] [Google Scholar]
- 14.Okawa Okawa A, Sakai K, Hirai T, Kato T, Tomizawa S, Enomoto M, Kawabata S, Takahashi M, Shinomiya K. Risk factors for early reconstruction failure of multilevel cervical corpectomy with dynamic plate fixation. Spine (Phila Pa1976) 2011;36(9):E582–E587. doi: 10.1097/BRS.0b013e3181e0f06a. [DOI] [PubMed] [Google Scholar]
- 15.Li H, Min J, Zhang Q, Yuan Y, Wang D. Dynamic cervical plate versus static cervical plate in the anterior cervical discectomy and fusion: a systematic review. Eur J Orthop Surg Traumatol. 2013;23(Suppl 1):41–46. doi: 10.1007/s00590-013-1244-8. [DOI] [PubMed] [Google Scholar]