Abstract
Purpose
The goal of this study is to compare the therapeutic effectiveness of percutaneous cervical discectomy, percutaneous cervical disc nucleoplasty, and a combination of the two for the treatment of cervical disc herniation and the effective stabilization of the cervical vertebral column.
Methods
A retrospective study was performed from February 2003 to April 2011. One hundred and seventy-one cervical disc herniation patients with a mean age of 47.8 years (ranging from 21 to 74 years) participated in the study and were treated with the three types of percutaneous minimally invasive techniques: percutaneous cervical discectomy (PCD, 97 cases), percutaneous cervical disc nucleoplasty (PCN, 50 cases), and a combination of the two (PCDN, 24 cases). After treatment, the postoperative clinical results and the stability of the cervical vertebral columns of these three groups were evaluated and compared.
Results
Patients in the PCD group received follow-up care for approximately 4.1 years (ranging from 0.2 to 8.5 years), while those in the PCN group received only an average of 2.6 years (ranging from 0.3 to 7.8 years), and the PCDN group received an average of 3.3 years (ranging from 0.2 to 8 years of follow-up). According to the Japanese Orthopedic Association scoring system, the functional scores (JOA scores) differed significantly between the pre- and postoperative patients within the three groups (PCD t = 21.849, P = <0.05; PCN t = 14.503, P < 0.05; PCDN t = 8.555, P < 0.05). All patients had been successfully operated on by the same spinal surgeon team. According to the Odom criterion, the clinical outcomes were not significantly different for any of the three groups (the recovery rate using the JOA standard evaluation, F = 2.19, P = 0.116, P > 0.05). The percentages of each procedure that received either an excellent or a good rating were PCD at 81.35 %, PCN at 82.44 % and PCDN at 83.19 %. In addition, the clinical success rates among the three were not significantly different (P > 0.05). Notably, there was no postoperative instability of the cervical vertebral column in any of the patients (P > 0.05), and there was no difference in the pre- or postoperative stability of the cervical vertebral columns in each group.
Conclusions
Each group achieved good clinical outcomes with this safe, minimally invasive spinal surgery for the treatment of cervical disc herniation. In addition, no postoperative risk of cervical instability was found.
Keywords: Cervical spine, Disc herniation, Discectomy, Nucleoplasty
Introduction
There has been a long history of spinal surgery; however, currently there is a trend toward less-invasive techniques. Stookey [1] described the clinical symptoms and anatomic location of cervical disc herniation in 1928. Mixter and Barr [2] later found a relationship between herniated discs and symptoms of sciatica and provided convincing evidence that laminectomy and disc excision can successfully relieve the pain associated with radiculopathy. With the passage of time, the anterior approach of employing interbody fusion to cervical vertebra has become common place [3–5]. However, other studies conducted by Hirsch, Robertson and Johnson [6, 7] recommended cervical discectomy without fusion. Around this time, the conception of minimally invasive spinal surgery had taken hold. In 1973, Fukushima et al. [8] introduced the ventriculofiberscope, which greatly enhanced percutaneous endoscopic cervical discectomy [9]. In this type of surgery, minimally invasive treatments to remove nucleated material and to lower intradiscal pressure through devices were inserted percutaneously into intervertebral discs. A number of techniques have recently been developed that are applicable to the treatment of disc herniation. For example, Smith et al. [10, 11] introduced chymopapain chemonucleolysis to treat herniated nucleus pulposus, Hijikata [12] described percutaneous lumbar discectomy, and Ascher [13] studied the novel technique of laser discectomy in the treatment of cervical spondylosis.
The development of minimally invasive percutaneous technology of spinal percutaneous cervical discectomy (PCD) and percutaneous cervical disc nucleoplasty (PCN) was used to treat cervical spondylopathy and obtained encouraging clinical curative effects. The developments listed above have allowed many spinal surgeons to conduct pilot studies on percutaneous minimally invasive techniques for cervical disc herniation. PCD was developed in 1993 with a clinical success rate of 79.5–83.73 % [14, 15], and PCN was developed in 2003 with a clinical success rate of 76.2–77.8 % [14, 15]. According to our knowledge of both domestic and foreign literature, there have been no reports of studies combining these percutaneous minimally invasive techniques. For this reason, we recruited patients with symptoms of cervical protrusion who could benefit from percutaneous cervical minimally invasive surgery. Then we randomly divided them into three groups as follows: PCD group, PCN group, PCDN group(PCD+PCN). A retrospective study was done to analyze the 171 patients who received these treatments from February 2003 to April 2011 to evaluate the clinical results and the effectiveness of the procedures on the stability of the cervical spinal columns in each group.
Materials and methods
General information
Patients included in this research complained of radicular pain with or without neck pain and were diagnosed with cervical disc herniation after an MRI. All the patients received conservative therapy (i.e., physical therapy combined with anti-inflammatory medications and muscle relaxants at the manufacturer’s recommended therapeutic dose for no less than 8 weeks), which resulted in no improvement of symptoms.
Patients who suffered from extruded disc fragmentation, hemorrhagic disease, spondylolisthesis, spinal canal stenosis, ossification of the longitudinal ligament, who had undergone previous surgery at the indicated level, or had cases of myelopathy were all excluded.
All 171 patients were retrospectively studied, 97 of which had previously undergone the PCD treatment. Group 1 included 53 men and 44 women with an average age of 47.8 (and a range of ±10.8 years), 50 of which received the PCN treatment. Group 2 included 29 men and 21 women with an average of age 48.5 (and a range of ±9.4 years), 24 of which had been treated with the PCDN. Group 3 included 15 men and 9 women with an average age of 46.5 (and a range of ±10.4 years). Surprisingly, there were no differences in clinical success rates among each group (P < 0.05). The characteristics of this retrospective cohort study are shown in Table 1.
Table 1.
Comparison of the general data among PCN, PCD and PCDN groups (χ ± s)
| Group | Y/A (years of age) | Number | Sex | Follow-up time (years) | Level | ||||
|---|---|---|---|---|---|---|---|---|---|
| Male | Female | C3–4 | C4–5 | C5–6 | C6–7 | ||||
| PCD | 47.8 ± 10.8 | 97 | 53 | 44 | 4.2 | 5 | 22 | 41 | 30 |
| PCN | 48.5 ± 9.4 | 50 | 29 | 21 | 2.6 | 2 | 18 | 24 | 6 |
| PCDN | 46.5 ± 10.4 | 24 | 15 | 9 | 3.3 | 1 | 5 | 17 | 0 |
| Statistic analyses |
F = 0.267 P = 0.766 |
χ
2 = 0.531 P = 0.767 |
χ
2 = 1.9 P = 0.387 |
χ 2 = 18.61, P = 0.003 | |||||
Surgical method
The patent numbers for the surgical equipment used in the PCD procedure were 97208502.5, and 97208501.7. The instruments included the work needle, the Perc-DC SpineWand, the microscopic clamp for the nucleus pulposus, and the cutting and suction machines (Fig. 1). The PCN procedure made use of the plasma surgery system from ArthroCare2000.
Fig. 1.
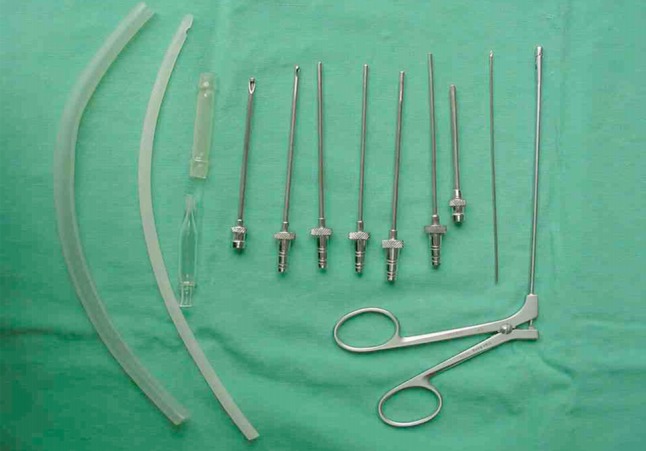
The PCD surgical instruments in the Third Affiliated Hospital of Guangzhou Medical University, China
Preoperative antibiotics and sedatives were given. Then the patient was placed in a supine position with the neck slightly extended by placing a rolled towel under the shoulders. The patient was given local anesthesia during the procedure to enable the crucial monitoring of any changes in symptoms or indications. A soft strap was placed over the forehead for stabilization. The shoulders were gently held in a downward position with tape. C-arm fluoroscopy was used in the anteroposterior and lateral planes to direct the placement of a spinal needle that was inserted into the disc. Initially, the skin and subcutaneous tissue at the point of entry, which is adjacent to the medial border of the right sternocleidomastoid muscle, were injected with 1 % lidocaine. Then, firm pressure was digitally applied to the space between the muscle and the trachea and directed toward the targeted intervertebral disc space. At this point, the surgeon pushed the trachea or larynx toward the opposite side with the index finger and then slipped the finger inside toward the front of the vertebral body until the prominence of the anterior edge of the disc to be treated was revealed. The surgeon was then able to feel the beats of the carotid artery with his or her fingers.
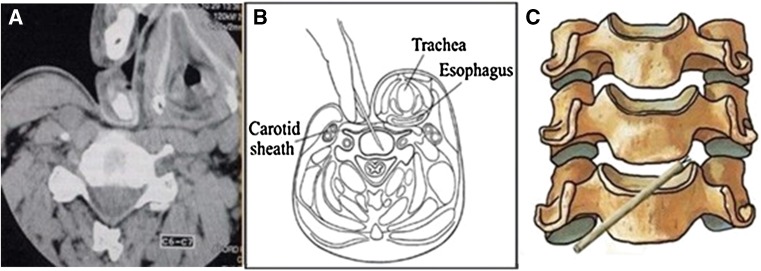
The larynx and trachea were displaced medially, while the carotid artery was displaced laterally [16] (Fig. 2a, b). An 18-gage spinal needle was then used to puncture the right side of the neck and enter into the disc space. The position was confirmed by C-arm fluoroscopy.
Fig. 2.
Schematic diagram of the percutaneous cervical surgical approach, a CT-based image-guided procedure in which the surgeon pushes the trachea or larynx toward the opposite side with the index finger and thumb and then slips the index finger inside towards the front of vertebral body until the prominence of the anterior edge of the disc to be treated is exposed. At this point, the surgeon can feel the beats of the carotid artery with his or her fingers. The tracheoesophageal tissue is displaced medially and the carotid artery is moved laterally. b Intraoperative methods of puncture. The spinal needle is inserted into the disc space. c Surgical anatomic schemes show percutaneous cervical discectomy with a microforceps inserted into the lesion site through the working cannula (see arrow in diagram.) from the opposite side of the lesion in a patient with left foraminal herniation of the cervical disc
Subsequently, the spinal needle was removed and a vertical incision was made at the puncture site, the guide wire was then placed through the incision and directed toward the herniated disc space, during which time a series of sequential cannulated soft tissue dilators were inserted over the guide wire utilizing a twisting motion in the PCD group. The final 3-mm working cannula was then inserted over the 2-mm dilator. This minimally invasive procedure has two main benefits: preventing soft tissue damage and alleviating approach-related pain. A trephine was inserted through the cannula and was used to cut an annulus. A manual discectomy was then performed using microforceps and suction under fluoroscopic guidance (Fig. 2c). The removed disc mass weighed approximately 2.1 g in our study.
The fiber of the Perc-DC SpineWand was inserted through an 18-gage needle in the PCN group, and the wand was connected to a standard Arthrocare power generator. The power of nucleoplasty ablation was 3 W with a 1–2 s coagulation time. If the patient experienced any pain during the procedure, the Perc-DC SpineWand was repositioned in the disc space. If no pain occurred during coagulation and the patient experienced coblation for more than 10 s, the Perc-DC SpineWand was withdrawn to the annulus, coagulated first to shrink the surrounding collagen and widen the channel. This process was repeated from four to six times.
Lastly, the PCDN group was treated with a combination of the PCD and PCN procedure. When symptoms subsided after manual discectomy, the PCD group was then treated with the PCN approach as a continuation of treatment.
Postoperative care
The 2–3 mm incisions in the PCD and PCDN patients were closed with Steri-Strips, and the patients were immediately asked whether the pain decreased or disappeared, were observed for 3 h, and were permitted to go home within 24 h if there were no complications.
The length of time for the procedures was recorded and compared among the PCD, PCN and PCDN groups. All patients received antibiotics and dehydration treatment for 24 h after surgery. After their procedures, patients were allowed unlimited walking, standing, sitting time, and were asked to exercise neck muscles gradually. Return to sedentary or non-physical work was permitted 3–4 days after the surgery; however, neck braces were worn for 2 weeks.
Postoperative evaluations
The functional JOA scores were used for assessment of clinical effectiveness, the maximum score being 17 points. The score was calculated according to the following formula: Recovery rate = [(postoperative score − preoperative score)/(17 − preoperative score)] × 100 %. According to the classified assessment of Odom [17], total disappearance of symptoms with normal progress is excellent. Some recurring symptoms with normal progress are considered good. Improvement of some symptoms, slow progress with no worsening is fair. No improvement of symptoms or aggravation of symptoms is considered poor. The Katsumi standard was used for cervical stability evaluation [18]. A routine cervical spinal dynamic X-ray was taken for evaluation both preoperatively and postoperatively. Two markers were used to assess the stability of the cervical vertebra. Angular displacement (AD) refers to the intersection angle at the inferior margin of the adjacent vertebra, while horizontal displacement (HD) is the horizontal distance around the posterior edge of the adjacent vertebra. If the X-ray showed the AD ≥ 11° or the HD ≥ 3.5 mm, radiographic instability was considered. Meanwhile, the radiographic assessment was determined by two independent radiologists, who were not informed as to which group the patients had been assigned.
Statistical analyses
Statistical processing was performed via SPSS12.0 software, (produced by the American company SPSS), and measurements were taken using the mean ± standard deviation value (χ ± s). The JOA score, AD value, and HD value were used as paired sample statistics among each group. To ensure comparability of the statistical analysis of the three groups for which data existed before and after cervical stability surgery (AD, HD index), a single segment of cervical spinal surgery patients was selected. The recovery rate, measured by the JOA score, and the type of procedure were analyzed by single factor variance. Due to the fact that the follow-up time and the quantity of bleeding in surgery did not follow a normal distribution, the Kruskal–Wallis test was used in which bleeding rates of P < 0.05 are statistically significant.
Results
Clinical data
The comparison of JOA scores and the classified assessment of Odom are shown in Table 2. The JOA score improved postoperatively in each group compared to the preoperative one. (PCD t = 21.85, P < 0.05; PCN t = 14.50, P < 0.05; PCDN t = 8.56, P < 0.05). There were no statistical differences in the recovery rate and the JOA score among these three groups (P = 0.12). However, the length of time for each surgery varied significantly (P < 0.05). It is also important to note that the PCD and PCN procedures were shorter than the PCDN (P > 0.05). Therefore, the most statistically significant difference was found between the PCDN and PCD groups as well as the PCDN and PCN groups (q = 14.292, P < 0.01). That is to say, time in surgery for the PCDN procedure was significantly longer than for the other procedures, with 83.3 % of the patients bleeding 1–2 ml (χ2 = 3.58, P > 0.05).
Table 2.
Comparison of the JOA scores and the classified assessment of Odom (χ ± s)
| Group | Number | JOA scores | Recovery rate of the grade (%) | Surgical procedure (min) | The classified assessment of Odom (%) | |
|---|---|---|---|---|---|---|
| Preoperative | Postoperative | |||||
| PCD | 97 | 10.36 ± 2.47 | 15.64 ± 1.62 | 80.2 ± 24.1 | 23.1 ± 7.0 | 81.35 |
| PCN | 50 | 10.36 ± 3.05 | 15.78 ± 1.72 | 84.7 ± 21.0 | 23.9 ± 7.9 | 82.44 |
| PCDN | 24 | 9.88 ± 2.82 | 15.04 ± 2.14 | 72.2 ± 28.7 | 40.6 ± 9.2 | 83.19 |
Comparison of cervical stability
Cervical instability remained in all cases after the PCN, PCD or PCDN procedures. Also, the outcome of AD and HD after surgery was not statistically significant compared to before surgery (P > 0.05, as shown in the Table 3).
Table 3.
Comparison of the stability of segments between pre and post operation (χ ± s)
| Group | AD | HD | ||||
|---|---|---|---|---|---|---|
| Pre | Post | Statistic analyses | Pre | Post | Statistic | |
| PCD | 6.54 ± 1.63 | 6.63 ± 1.72 | T = 1.232, P = 0.221 | 1.95 ± 0.71 | 1.90 ± 0.71 | T = 0.827, P = 0.410 |
| PCN | 6.40 ± 1.64 | 6.56 ± 1.75 | T = 1.429, P = 0.159 | 1.98 ± 0.86 | 2.04 ± 0.87 | T = 0.579, P = 0.565 |
| PCDN | 6.81 ± 1.55 | 7.02 ± 1.60 | T = −1.645, P = 0.117 | 2.22 ± 0.89 | 2.10 ± 0.83 | T = 0.904, P = 0.378 |
Complications
During a PCN procedure, the plasma knife was broken (Fig. 3), and during a PCD procedure, a knife was not removed from the surgery site. In the latest follow-up session, patients reported no discomfort, which indicated a good clinical curative effect. Three cases of disc infection occurred after surgery (two in PCD and one in PCN). All three patients suffered head or neck discomfort, local muscle spasms and high fever for 4–7 days after surgery. The physical examination revealed tenderness, redness and swelling at the puncture site. Patients also experienced neck stiffness, muscle spasms, limited energy, and a score of (++) on their extrusion tests. Some patients had to undergo a second procedure to remove the lesion completely after undergoing a pathological examination and bacteriological studies. Irrigation by gentamycin saline was discontinued when the neck pain disappeared. Patients were asked to rest in bed after the procedure, wear a neck brace for 2 weeks after surgery and take antibiotics (Forturn 1.5 g add saline 20 ml, iv, Bid, for 10–14 days).
Fig. 3.
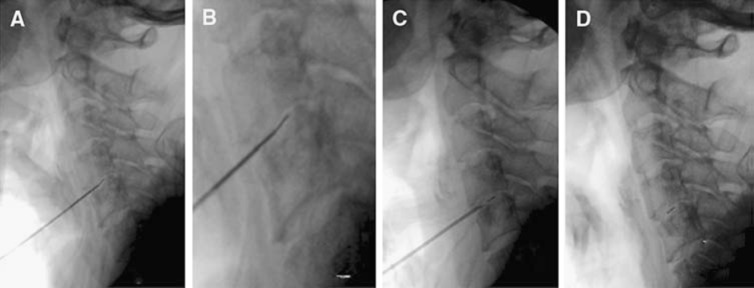
X-ray shows the tip of the Perc-DC SpineWand, which was broken in the C4–5 disc space during the procedure; a and b shows the X-ray of the partial Perc-DC SpineWand in relation to the bend (see arrow); c shows where the Perc-DC SpineWand broke in the C4–5 disc space, which could not be removed with the percutaneous cervical discectomy instruments (See arrow); d shows the exact location of the Perc-DC SpineWand that could not be removed. (see arrow)
Discussion
The clinical effects of PCD, PCN and PCDN procedures
PCD and PCN are minimally invasive procedures for mechanically reducing the disc volume and pressure around the spinal column and nerve root [14, 15]. PCD is a technique to cut out and remove the disc herniation with suction, which reduces the pressure and volume in the disc. In other words, clinical symptoms can be improved by opening a window to the prominent disc fiber to decrease the intervertebral disc pressure by cutting the section of disc and reducing the mechanical pressure around the pulp and nerve root which form the nucleus pulpous and fiber.
PCN is a minimally invasive percutaneous intradiscal treatment option for cervical disc herniation. Nucleoplasty is based on coblation technology using bipolar radiofrequency energy. It consists of two phases: tissue ablation and coagulation. The 1-mm Perc-DC SpineWand (ArthroCare2000) for tissue ablation and coagulation is inserted into the disc space through an 18-gage needle under fluoroscopic guidance. During ablation, a plasma field between the electrodes and the tissue is generated. As a result of the voltage gradient, charged particles accelerate within the tissue and break the molecular bonds of the disc nucleus into its constituent molecules and gases. These gases escape through the needle. For each 0.5-cm movement of the wand, a zone of thermal coagulation with a radius of 1 mm is created, leading to collagen shrinkage. The goal of both these procedures is to reduce the intradiscal pressure by removing approximately 1 g of tissue with minimal thermal damage to the surrounding tissue [19, 20].
PCDN combines the PCD and PCN procedures. In the study, first, the herniated disc was cut out and removed by suction using the PCD approach. Second, the disc was coagulated using the PCN approach. In this study, the JOA scores showed statistical differences among these three groups (P < 0.05), and all the cases obtained good clinical effects. For the analysis of variance, the recovery rate shown by the JOA score indicated no statistical differences in each group. Furthermore, PCD, PCN, and PCDN approaches were found to be the most effective minimally invasive procedures to treat cervical spondylosis. According to the classified assessment of Odom, there were no differences among these three types of surgeries.
Complications associated with the PCD, PCN and PCDN procedures
To prevent the occurrence of hematoma, all patients had been practiced to push open the gap between the visceral scabbard and carotid sheath before the surgery. During the procedure, we chose the correct size of conical guide wire, and punctured the disc slowly and carefully. The surgeon should avoid performing multiple punctures and be careful to avoid damaging the vertebral artery.
The aseptic operating environment must be strictly maintained to prevent infection at the site of the procedure. In this study, antibiotics were conventionally taken after surgery for 1–3 days after the PCD and PCDN procedures. One patient needed to undergo the PCD again to eliminate infection. There were three cases of disc infection which began to heal rapidly after suction removal by using the PCD procedure and reduced inflammation.
There is a danger of spinal cord and nerve root damage when the needle is placed too deep or too off target during an attempt to puncture the anulus fibrosus, which could result in spinal cord injury. Therefore, the position of the Perc-DC SpineWand must be confirmed during the operations and must be removed at the first sign of nerve damage. During the PCN and PCDN procedure, the SpineWand must be placed carefully and gently.
Unfortunately, equipment breakage, including the trocar and the SpineWand, did occur. Careful handling of the equipment during procedures is crucial for a successful outcome and avoiding complications. During the PCN procedure, the SpineWand was broken at the C4–5 in one case, and the device was not removed through the PCD procedure. However, this appeared to have caused no long-term damage, as the patient never complained of any discomfort.
Cervical stability
Cervical instability, or the physiological balance of the cervical spinal column, cannot be maintained after the procedure due to the fact that part of the structure is destroyed, which leads to horizontal displacement of the vertebral column. The damage to the facet joint and the joint capsule leads to a decline in the carrying capacity of the spinal column; however, this does not necessarily lead to spinal instability. All postoperative X-rays were analyzed by two independent radiologists, and no cervical instabilities were found. Onik [21] demonstrated that part of the disc tissue can be removed during the PCD procedure to decompress the spinal nerve root, which can reduce or eliminate symptoms of nerve compression. In our study, PCD, PCN and PCDN procedures were shown to aid in the resection or ablation of the nucleus pulposus, which maintains the health of the discs. The height of the disc had no influence on the outcome of surgery, and no damage to the facet joint and ligament occurred. When part of the disc protrusion is supported, this creates good cervical stability and appears to arrest disc degeneration. In addition, it appeared not to destroy the cervical stability [22].
Suggestions for further study
Due to the fact that the number of cases in this study was small, there was little follow-up and no comparison group using a standard technique (ACDF, open laminoforaminotomy); however, larger studies in the future are required to demonstrate whether these techniques have a therapeutic effect for the treatment of cervical intervertebral disc displacement. In addition, a longer follow-up and randomized controlled trials using consistent instrumentation will be necessary to elucidate the differences between PCN and ACDF (open laminoforaminotomy).
Conclusion
PCD, PCN, and PCDN were all found to be effective, minimally invasive procedures for the treatment of cervical disc herniation in our research. PCN, the most minimally invasive included ablation, cutting, shaping, shrinkage, the use of thinner needles, and less errhysis; however, the cost was relatively high for a plasma cutter. PCD is a more intuitive and simpler procedure, in which the quantity of excision can be easily controlled (1 g). PCDN, cutting and removal by suction, is more effective in cases where a single technique is insufficient. Choy’s [23] studies revealed a moderate level of elasticity around the nucleus pulposus that was not proportional to disc pressure. For this reason, there is less concern about its effectiveness. Our conclusion is similar to that of Choy. PCD has been used for nearly 20 years, while PCN has been in use for only half that time. PCDN has not yet been in standard use for the treatment of cervical disc herniation. There are some limitations to this study, which still need to be explored by adding more participants and randomized prospective studies to further demonstrate the efficacy of these three procedures.
Acknowledgments
This study was financed by Projects of Science and Technology of Guangdong province in 2008(2008 A030201015) and by Projects of Science and Technology of Guangzhou municipality in 2011(2011J4100052).
Conflict of interest
The authors have no conflicts of interest.
References
- 1.Stookey B. Compression of the spinal cord due to ventral extradural cervical chondromas. Arch Neurol Psych. 1928;20:275–278. doi: 10.1001/archneurpsyc.1928.02210140043003. [DOI] [Google Scholar]
- 2.Mixter WJ, Barr JS. Rupture of the intervertebral disc with involvement of the spinal canal. N Engl J Med. 1934;211:210–215. doi: 10.1056/NEJM193408022110506. [DOI] [Google Scholar]
- 3.Bailey RW, Badgley CE. Stabilization of the cervical spine by anterior fusion. J Bone Joint Surg Am. 1960;42A:565–569. [PubMed] [Google Scholar]
- 4.Cloward RB. The treatment of ruptured lumbar intervertebral discs by vertebral body fusion. Clin Orthop Relat Res. 1985;193:5–15. [PubMed] [Google Scholar]
- 5.Smith GW, Robinson RA. The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Joint Surg Am. 1958;40:607–624. [PubMed] [Google Scholar]
- 6.Hirsch C. Cervical disk rupture: diagnosis and therapy. Acta Orthop. 1960;30:172–186. doi: 10.3109/17453676109149538. [DOI] [Google Scholar]
- 7.Robertson JT, Johnson SD. Anterior cervical discectomy without fusion: long-term results. Clin Neurosurg. 1980;27:440–449. doi: 10.1093/neurosurgery/27.cn_suppl_1.440. [DOI] [PubMed] [Google Scholar]
- 8.Fukushima T, Ishijima B, Hirakawa K, et al. Ventriculofiberscope: a new technique for endoscopic diagnosis and operation. J Neurosurg. 1973;38:251–256. doi: 10.3171/jns.1973.38.2.0251. [DOI] [PubMed] [Google Scholar]
- 9.Kahanovitz N, Viola K, Goldstein T, Dawson E, et al. A multicenter analysis of percutaneous discectomy. Spine. 1990;15:713–715. doi: 10.1097/00007632-199007000-00017. [DOI] [PubMed] [Google Scholar]
- 10.Smith L. Enzyme dissolution of the nucleus pulposus in humans. JAMA. 1964;187:137–140. doi: 10.1001/jama.1964.03060150061016. [DOI] [PubMed] [Google Scholar]
- 11.Smith L, Garvin PJ, Jennings RB. Enzyme dissolution of the nucleus pulposus. Nature. 1963;198:1311–1312. doi: 10.1038/1981311a0. [DOI] [PubMed] [Google Scholar]
- 12.Hijikata S. Percutaneous nucleotomy. A new concept technique and 12 years’ experience. Clin Orthop. 1989;238:9–23. [PubMed] [Google Scholar]
- 13.Ascher PW. Status quo and new horizons of laser therapy in neurosurgery. Lasers Surg Med. 1985;5(5):499–506. doi: 10.1002/lsm.1900050509. [DOI] [PubMed] [Google Scholar]
- 14.Li J, Yan DL, Zhang ZH. Percutaneous cervical nucleoplasty in the treatment of cervical disc herniation. Eur Spine J. 2008;17:1664–1669. doi: 10.1007/s00586-008-0786-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yan DL, Li J, Zhu HD. Percutaneous cervical nucleoplasty and percutaneous cervical discectomy treatments of the contained cervical disc herniation. Arch Orthop Trauma Surg. 2010;130:1371–1376. doi: 10.1007/s00402-009-1041-3. [DOI] [PubMed] [Google Scholar]
- 16.Ahn Y, Lee SH, Lee SC. Factors predicting excellent outcome of percutaneous cervical discectomy: analysis of 111 consecutive cases. Neuroradiology. 2004;46:378–384. doi: 10.1007/s00234-004-1197-z. [DOI] [PubMed] [Google Scholar]
- 17.Odom GL, Finney W, Woodhall B. Cervical disk lesions. Am Med Assoc. 1958;166:23–28. doi: 10.1001/jama.1958.02990010025006. [DOI] [PubMed] [Google Scholar]
- 18.Katsumi Y, Honma T, Nakamurs T. Analysis of cervical instability resulting from laminectomies for removal of spine cord tumor. Spine. 1989;14:1171–1176. doi: 10.1097/00007632-198911000-00007. [DOI] [PubMed] [Google Scholar]
- 19.Sim SE, Ko ES, Kim DK, et al. The results of cervical nucleoplasty in patients with cervical disc disorder: a retrospective clinical study of 22 patients. Korean J Pain. 2011;24:36–43. doi: 10.3344/kjp.2011.24.1.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Timmermann J, Hahn M, Krueger K. Short-term follow-up: micro-invasive therapy of the cervical herniated disk by percutaneous nucleotomy. J Back Musculoskelet Rehabil. 2011;24:89–93. doi: 10.3233/BMR-2011-0280. [DOI] [PubMed] [Google Scholar]
- 21.Onik G, Helms CA, Ginsburb L. Percutaneous lumbar discectomy using a new aspiration probe. AJNR. 1985;144:290–293. doi: 10.2214/ajr.144.6.1137. [DOI] [PubMed] [Google Scholar]
- 22.Greiner-Perth R, Böhm H, ElSaghir H, et al. The microscopic assisted percutaneous approach to posterior spine: a new minimally invasive procedure for treatment of spinal processes. Zentralbl Neurochir. 2002;63:7–11. doi: 10.1055/s-2002-31582. [DOI] [PubMed] [Google Scholar]
- 23.Choy DS. Percutaneous laser disc decompression (PLDD): twelve years’ experience with 752 procedures in 518 patients. J Clin Laser Med Surg. 1998;16:325–331. doi: 10.1089/clm.1998.16.325. [DOI] [PubMed] [Google Scholar]