Abstract
Background:
Chronic rhinosinusitis (CRS) and allergic rhinitis are associated with functional limitations, but these impacts are not known on a population basis. Our objective was to epidemiologically determine functional limitations and workdays lost that are associated with CRS and allergic rhinitis in adults.
Methods:
The Medical Expenditure Panel Survey for calendar year 2007 was examined to identify cases of CRS and allergic rhinitis. Functional limitation variables for activity limitation, work limitation, social limitation, and cognitive limitation determined by the survey also were extracted. Using multivariate models adjusting for age, gender, race, ethnicity, education level, insurance status, geographic region, as well as the Charlson comorbidity index, incremental differences in workdays lost and these functional limitations were determined for patients with and without CRS and allergic rhinitis.
Results:
Among 225.1 million adults, the prevalences of CRS and allergic rhinitis were 4.9 ± 0.2% and 7.9 ± 0.3%, respectively. Patients with CRS demonstrated an incremental 1.04 ± 0.3 workdays lost per year along with significant increased adjusted odds ratios for activity limitation (odds ratio, 1.54), work limitation (1.50), and social limitation (1.49, all p < .005) but not cognitive limitation (1.05, p = .213). Patients with allergic rhinitis demonstrated an incremental 0.60 ± 0.45 workdays lost along with significant increased adjusted odds ratios for activity limitation (1.42), work limitation (1.43), social limitation (1.47), and cognitive limitation (1.32, all p < .019).
Conclusions:
Both CRS and allergic rhinitis impart significantly increased odds ratios for activity, work, and social limitations. Allergic rhinitis also carries with it statistically significant odds of functional cognitive limitation. The total aggregate workdays missed in the United States may be estimated at 11.5 million workdays and 10.7 million workdays for CRS and allergic rhinitis, respectively.
Keywords: Chronic rhinosinusitis, allergic rhinitis, functional limitation, disability, workdays, disease impact, costs, activity limitation, social limitation, work limitation, health administration data
Chronic rhinosinusitis (CRS) and allergic rhinitis (AR) are among the most common and burdensome chronic conditions in the United States. Recent data suggest that an estimated 11.1 million Americans suffer from CRS each year, and AR affects an estimated 17.8 million Americans annually.1,2 The burden of these illnesses in terms of direct costs to the health care system is tremendous.3–5 Reflective of their associated health care disease burdens, both CRS and AR impart a substantial individual quality of life burden on affected subjects.
Many studies have been conducted to examine the decreases in quality of life experienced by patients suffering from CRS or AR.6–9 These have most commonly consisted of cohort studies often selected from tertiary care medical centers and subspecialty rhinology practices. There are limited data regarding the overall quality of life burdens from CRS and AR, particularly in a nonreferral and nonsurgical population. We sought to examine the quality of life burdens of CRS and AR in terms of functional limitations on a national, epidemiologic scale. This would provide national estimates of the patients' burden with these illnesses, likely overcoming selection and ascertainment biases that may be present in previous reports.
METHODS
The data source for this study consisted of the Medical Expenditure Panel Survey (MEPS) for 2007 as administered by the Agency for Healthcare Research and Quality under the U.S. Department of Health and Human Services. The MEPS is an overlapping panel design survey following a nationally representative sample of the U.S. civilian, noninstitutionalized population over the course of 2 years.10 The MEPS household component contains detailed self-reported information on demographic and socioeconomic characteristics as well as health conditions, insurance status, use of health care services employment, and missed workdays. Data are obtained at the household level and completed by one household member, who may be a proxy. Upon completion of the household MEPS component, a sample of medical providers are contacted by telephone to obtain supplemental information regarding dates of provider visits, diagnoses and procedure codes, charges and payments. These data are contained in the medical provider component of the MEPS.
This study was reviewed by our hospital's committee on clinical investigations and designated as exempt from review. In accordance with data access agreements, precautions were taken to avoid individual patient identification. The 2007 household component of the MEPS was merged with the 2007 medical provider component according to the appropriate linkage variables in SPSS 17.0 (Chicago, IL). Because patients may report more than one medical condition, up to 34 medical condition variables were allowed per patient after the data files were merged.
Next, patients were identified as suffering from CRS or AR by examining the ICD9CODX data field for each listed medical condition. This field consists of the three-digit International Classification of Diseases version 9 code for a given medical condition based on an assessment of medical conditions recorded as verbatim text and then coded by a professional coder. Patients for whom any one of the 34 medical condition codes corresponded to 473.x and 477.x were considered as having CRS or AR, respectively; the remaining patients were considered as not reporting either of these two conditions.
Standard demographic information including age and gender distribution was compiled for those patients reporting and not reporting AR. The additional demographic information extracted and compared included race, ethnicity, level of education, insurance status, geographic region, and marital status (Table 1). In addition, the adaptation by D'Hoore et al11 of the Charlson comorbidity index was calculated based on comorbid medical conditions for each subject. This index adjusts for comorbidities that include myocardial infarction, congestive heart failure, peripheral vascular disease, dementia, cerebral vascular disease, asthma, chronic obstructive pulmonary disease, peptic ulcer disease, and liver disease, among others. It allows patients to be compared with “like” patients with similar comorbidities.
Table 1.
Demographics of study population
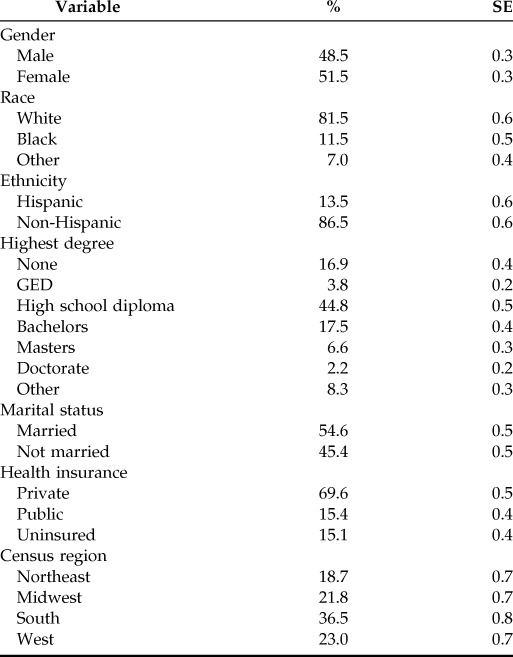
Data are reported as mean or proportion ± SE of the estimate. Because the survey sample design of the MEPS survey includes stratification, clustering, multiple stages of selection, and disproportionate sampling, statistical methods that take into account stratification, clustering, and the sampling methods used in MEPS data collection (i.e., the complex samples algorithm in SPSS) were used to determine nationally representative means and SEs.10 Estimates were considered reliable if the relative SE of the estimate was less than 30%.
The limitations imparted by CRS and AR were determined from the presence of four specific dichotomous assessment variables within the MEPS survey: activity limitation, work limitation, social limitation, and cognitive limitation as reported by the patient. These limitation variables have been validated and used previously to assess the limitations associated with several chronic conditions including asthma, diabetes, and rheumatoid arthritis. Differences in these functional limitations were determined for those patients with and without CRS and with and without AR, with a multivariate model that adjusted for age, gender, race, ethnicity, education, insurance, region, marital status, and Charlson comorbidity index score with statistical significance set at p = .05.
RESULTS
The population demographics are presented in Table 1, encompassing 225.1 million adults. The average age was 46.1 ± 0.2 years. The estimated prevalences of CRS and AR were 4.9 ± 0.2% and 7.9 ± 0.3%, respectively (11.1 ± 0.5 million and 17.8 ± 0.7 million cases, respectively). In Table 2 an analysis is presented of functional limitations incrementally attributable to CRS for the study population. Patients with CRS suffered from significant increased difficulties with activity limitations, work limitations, and social limitations; there was no identifiable cognitive limitation. CRS also was associated with an incremental additional loss of 1.04 ± 0.39 workdays per year relative to those patients without CRS.
Table 2.
Functional limitations for patients with CRS
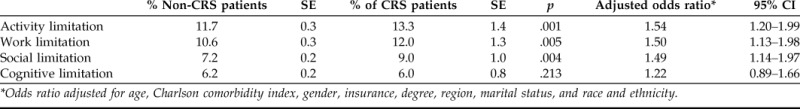
*Odds ratio adjusted for age, Charlson comorbidity index, gender, insurance, degree, region, marital status, and race and ethnicity.
In Table 3 an analysis is presented of functional limitations in the study population incrementally attributable to AR. AR was incrementally associated with statistically significant increases in activity limitation, work limitation, social limitation, and cognitive limitation for affected adults. AR also was associated with an incremental additional loss of 0.60 ± 0.45 workdays per year relative to those patients without AR.
Table 3.
Functional limitations for patients with AR
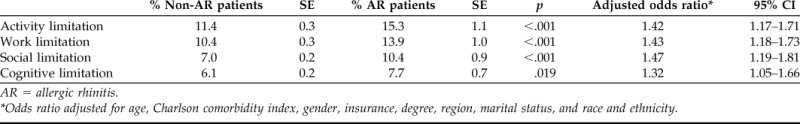
AR = allergic rhinitis.
*Odds ratio adjusted for age, Charlson comorbidity index, gender, insurance, degree, region, marital status, and race and ethnicity.
DISCUSSION
There is no question that both CRS and AR have significant footprints in health care resource consumption in the United States. Previous work has quantified the incremental per-patient, per-year health care cost burdens of CRS and AR as $772 and $1492, respectively.1,2 If patients' CRS is severe enough to approach consideration for surgery, yearly costs related to CRS may be even greater, approaching $2449.3 However, these figures examine the disease burden primarily from the health care system's vantage point.
The quality of life burdens and disease-specific quality of life burdens of CRS and AR have been well quantified using various quality of life assessment tools that measure the disease burden from the patient's standpoint.6–8 However, most of these studies have been conducted in major academic institutions, often in tertiary care referral environments. For example, there are very little data available regarding the quality of life burden due to CRS in the general population not already referred to otolaryngology. Naturally, those patients referred to otolaryngologists or rhinologists for a diagnosis of CRS are likely to have more severe disease and thereby a higher quality of life burden. The same likely holds true for AR. Therefore, we sought to examine the functional limitations imparted by a diagnosis of CRS or AR at the population level to examine disease impact on these elements of quality of life.
The functional limitations categorized herein as activity limitation, work limitation, social limitation, and cognitive limitation are specific queries within the MEPS construct. Although these are dichotomous, self-reported assessments, they have been shown to have good reliability and validity in several disease processes.10,12,13 Furthermore, by using the incremental approach, adjusting for medical comorbidity (with the Charlson comorbidity index) and demographic parameters, we are better able to distill the individual impacts of CRS or AR on these limitations.14 For example, it is well known that asthma may accompany CRS and/or AR and influence the disease burden. However, the multivariate analysis controls for the presence of asthma (and its potential impact on these limitations, etc.) through the Charlson comorbidity index as a covariate.
It is not surprising that both CRS and AR are associated with significant activity and work limitations. Previous publications have identified a substantial increase in workdays missed due to CRS, which is often remediated after endoscopic sinus surgery.15,16 The social limitations associated with CRS and AR may be more complex in nature. Patients often report social embarrassment related to constant rhinorrhea, sneezing, purulent discharge, or vocal congestion in the setting of CRS or AR.7 In addition, smell disturbances associated with these conditions may further compound social limitations.
One interesting variance between CRS and AR was that AR was associated with a statistically significant odds of cognitive limitation, whereas CRS was not. Anecdotally, patients have often reported in the outpatient clinic various symptoms that resemble cognitive limitations, such as their “head being in the clouds,” difficulty concentrating, and early fatigue of mental capabilities in the settings of both CRS and AR. The objective nature of these symptoms is yet to be discerned. We have found previously that even the nonsedating antihistamines have an increased rate of patient-reported fatigue when used regularly.17 This is likely a topic for future study.
Finally, the number of workdays missed at the population-based level associated with CRS or AR deserves some scrutiny. Although on average one or fewer days was missed in association with CRS or AR, when evaluated at the population level this is a substantial figure. Given the prevalence of CRS and AR, aggregate workdays missed in the United States would be estimated as 11.5 million workdays and 10.7 million workdays for CRS and AR, respectively. These figures further emphasize the substantial societal burden of these upper respiratory diseases.
The use of the MEPS database for the study of disease impact has been explored in several other conditions, including asthma, diabetes, and spine/back problems, and it is widely felt to be reliable.14,18,19 However, several limitations of this database for the current study merit mention. First, patients with CRS or AR were identified by a International Classification of Diseases version 9 diagnosis code. This methodology, in turn, depends on the accuracy of the diagnosis code relative to the actual presence of CRS or AR. It is possible that incorrect diagnosis codes were ascribed to patients not truly suffering from CRS or AR; this may artificially inflate the perceived limitations associated with these illnesses. A second limitation is that data for the household component of the MEPS are completed by one household member who may be a proxy, which may afford inaccuracies in reporting. Survey data are subjected to postcollection checks for consistency by survey administrators. Furthermore, the current method's linking of the household component to the medical provider component (collected independently from the proxy household member) serves as a secondary check for accuracy of reporting and code.
CONCLUSION
Both CRS and AR impart significantly increased odds ratios for activity, work, and social limitations. CRS is associated with more workdays lost than is AR. However, AR carries with it a statistically significant odds ratio for functional cognitive limitation. Additional work on a population-based scale will be required to better understand the societal impact of these limitations in the setting of these commonly prevalent conditions.
Footnotes
The author has no conflicts of interest to declare pertaining to this article
REFERENCES
- 1. Bhattacharyya N. Incremental healthcare utilization and expenditures for allergic rhinitis in the United States. Laryngoscope 121:1830–1833, 2011. [DOI] [PubMed] [Google Scholar]
- 2. Bhattacharyya N. Incremental health care utilization and expenditures for chronic rhinosinusitis in the United States. Ann Otol Rhinol Laryngol 120:423–427, 2011. [DOI] [PubMed] [Google Scholar]
- 3. Bhattacharyya N, Orlandi RR, Grebner J, Martinson M. Cost burden of chronic rhinosinusitis: a claims-based study. Otolaryngol Head Neck Surg 144:440–445, 2011. [DOI] [PubMed] [Google Scholar]
- 4. Blaiss MS. Allergic rhinitis: direct and indirect costs. Allergy Asthma Proc 31:375–380, 2010. [DOI] [PubMed] [Google Scholar]
- 5. Meltzer EO, Nathan R, Derebery J, et al. Sleep, quality of life, and productivity impact of nasal symptoms in the United States: findings from the Burden of Rhinitis in America survey. Allergy Asthma Proc 30:244–254, 2009. [DOI] [PubMed] [Google Scholar]
- 6. Lu D, Zhao Y, Zheng Y, et al. Evaluation of quality of life questionnaires for adult patients with moderate to severe allergic rhinitis. Am J Otolaryngol 32:494–8, 2011. [DOI] [PubMed] [Google Scholar]
- 7. Nathan RA. The burden of allergic rhinitis. Allergy Asthma Proc 28:3–9, 2007. [DOI] [PubMed] [Google Scholar]
- 8. Rudmik L, Smith TL. Quality of life in patients with chronic rhinosinusitis. Curr Allergy Asthma Rep 11:247–252, 2011. [DOI] [PubMed] [Google Scholar]
- 9. Senior BA, Glaze C, Benninger MS. Use of the Rhinosinusitis Disability Index (RSDI) in rhinologic disease. Am J Rhinol 15:15–20, 2001. [DOI] [PubMed] [Google Scholar]
- 10. Sullivan PW, Ghushchyan VH, Slejko JF, et al. The burden of adult asthma in the United States: evidence from the Medical Expenditure Panel Survey. J Allergy Clin Immunol 127:363–369. e1–3, 2011. [DOI] [PubMed] [Google Scholar]
- 11. D'Hoore W, Bouckaert A, Tilquin C. Practical considerations on the use of the Charlson comorbidity index with administrative data bases. J Clin Epidemiol 49:1429–1433, 1996. [DOI] [PubMed] [Google Scholar]
- 12. Hill SC, Pylypchuk Y. Reports of fewer activity limitations: recovery, survey fatigue, or switching respondent? Med Care 44:I73–I81, 2006. [DOI] [PubMed] [Google Scholar]
- 13. Witt WP, Gottlieb CA, Hampton J, Litzelman K. The impact of childhood activity limitations on parental health, mental health, and workdays lost in the United States. Acad Pediatr 9:263–269, 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kamble S, Bharmal M. Incremental direct expenditure of treating asthma in the United States. J Asthma 46:73–80, 2009. [DOI] [PubMed] [Google Scholar]
- 15. Bhattacharyya N. The economic burden and symptom manifestations of chronic rhinosinusitis. Am J Rhinol 17:27–32, 2003. [PubMed] [Google Scholar]
- 16. Bhattacharyya N. Symptom outcomes after endoscopic sinus surgery for chronic rhinosinusitis. Arch Otolaryngol Head Neck Surg 130:329–333, 2004. [DOI] [PubMed] [Google Scholar]
- 17. Bhattacharyya N, Kepnes LJ. Associations between fatigue and medication use in chronic rhinosinusitis. Ear Nose Throat J 85:510, 512,, 514–515, 2006. [PubMed] [Google Scholar]
- 18. Fu AZ, Qiu Y, Radican L, Wells BJ. Health care and productivity costs associated with diabetic patients with macrovascular comorbid conditions. Diabetes Care 32:2187–2192, 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Martin BI, Deyo RA, Mirza SK, et al. Expenditures and health status among adults with back and neck problems. JAMA 299:656–664, 2008. [DOI] [PubMed] [Google Scholar]


