Abstract
Background:
Although the prevalence of aspirin-exacerbated respiratory disease (AERD) in western populations is high, AERD is rather rare in China, and few related studies have been published to date.
Methods:
We performed a prospective cohort investigation on the incidence of AERD in patients with chronic rhinosinusitis (CRS) in southern China. A literature search of the China Academic Journal Network Publishing Database was conducted to obtain an overview of the incidence of AERD in the Chinese population, and previous studies on the incidence of AERD were reviewed.
Results:
We found 2 patients with aspirin hypersensitivity among 351 consecutive CRS (309 with nasal polyps [NPs]) patients, suggesting a rate of 0.57% in the CRS population. Forty-five articles about AERD were obtained by Chinese-language literature searches. In total, 346 cases of AERD were reported during the past 30 years.
Conclusion:
Given the large population of NPs in China, the prevalence of AERD is very low, and this may be related to the reduced levels of nasal tissue eosinophilia and subsequent low asthma comorbidity.
Keywords: Aspirin-exacerbated respiratory disease, aspirin-induced asthma, aspirin intolerance, China, Chinese population, chronic rhinosinusitis, nasal polyps, Samter triad
Chronic rhinosinusitis (CRS) is one of the most frequent chronic inflammatory disease entities, with an estimated prevalence of 5–10%.1 Based on the existence of nasal polyps (NPs), it can be classified as CRS without NPs (CRSsNP) and CRS with NPs (CRSwNP). The etiology of CRS is complex and multifactorial (involving infection, allergy, and other elements). Arachidonic acid metabolism is also recognized to be involved in the pathophysiology of certain subtypes of CRS.
Aspirin-exacerbated respiratory disease (AERD) is a distinct clinical syndrome characterized by aspirin hypersensitivity, asthma, and/or NPs.2 It has been reported that the estimated incidence of AERD is 1% in the general population and 10% among asthmatic patients in the western population.3 However, AERD is relatively rare in China, and there is limited literature concerning the prevalence of AERD among the Chinese CRS population. This article thus aims to provide a useful summary of the epidemiology of AERD in the CRS population in China based on individual case reports and an extensive literature review. In this study, we first provided our cohort findings on AERD incidence by screening 351 patients with CRS in southern China. To further expand our understanding about the low incidence of AERD, we then conducted a systematic literature review of studies that have reported on sporadic cases that arose during the treatment of CRSsNP and CRSwNP.
MATERIALS AND METHODS
Clinical Investigation
This study was approved by the local ethics committee, and informed consent was obtained from all subjects. A total of 351 patients with CRS were enrolled, ranging from 14 to 76 years old (mean, 43.7 years old). For all patients, a full ear, nose, and throat examination was performed, as described in previous reports.4 Patients with CRS were identified based on medical histories and endoscopic and radiographic criteria. CRSsNP was defined as continuous symptoms of rhinosinusitis for >12 consecutive weeks and computed tomography analysis of the sinuses that revealed isolated or diffuse sinus mucosal thickening and/or air fluid levels. CRSwNP was defined by endoscopy findings of bilateral polyps originating from the middle meatus and/or confirmation of polyps by computerized tomography. Asthma was defined by a history of recurrent dyspnea, wheezing or cough episodes, positive results in airway reversibility tests (forced expiratory volume in 1 second [FEV1] increasing ≥12% and reaching 200 mL after inhalation of 400 μg of salbutamol), or positive results in airway responsiveness tests (FEV1 decreasing ≥20% when a cumulative dose of histamine ≤7.8 μmol was administered), confirmed by a physician.
For all patients, history of asthma, history of drug hypersensitivity (especially for anti–cold medications), history of allergic rhinitis, surgical history if rhinopathy, and history of hospitalization for lower airway disease were investigated using a questionnaire. The pulmonary function test was performed using a Jaeger MS diffusion lung function device and aerosol activation system (Erich Jaeger GmbH, Germany), as described elsewhere for use when asthma is suspected.4 The main examination indices included FEV1, forced vital capacity (FVC), and the ratio of FEV1/FVC. Once asthma was diagnosed, the oral aspirin challenge protocol was performed as described elsewhere.5 A positive reaction is defined as a 15% decrease in the FEV1 from baseline, with or without other associated symptoms.
Literature Search
Literature searches of the China Academic Journal Network Publishing Database were conducted from January 1979 through December 2010, during a continuing Samter clinical research trial. The search sought to identify primary articles about the epidemiology and current medical and surgical treatment modalities of aspirin-hypersensitive NPs. The key word for the first-level search was “Xiao Chuan” (asthma in Chinese); the second-level key word was “A Si Pi Lin” (aspirin in Chinese); the parallel second-level words were “Bi Xi Rou” (NPs in Chinese) or “San Lian Zheng” (triad in Chinese) or “Samter San Lian Zheng” (Samter triad in Chinese). This electronic search was supplemented by manual searches of the reference lists of articles identified as relevant. References in the retrieved articles were reviewed to identify additional potentially relevant studies that the search strategy might have missed. The search was restricted to Chinese-language publications.
RESULTS
Epidemiology of AERD in CRS Patients
A total of 351 patients with CRS (CRSsNP, 42 patients; CRSwNP, 309 patients) were enrolled in this study from May 2006 to April 2010. The CRS patients included 201 male and 150 female subjects, ranging from 14 to 76 years old (mean, 43.7 years old). The demographics of all subjects are listed in Table 1. Eight patients with concomitant asthma were identified from among 351 CRS patients (2.27%). Among those, 7 asthma patients were identified from 309 patients with CRSwNP. Two patients displayed aspirin hypersensitivity on oral aspirin provocation test, suggesting a lower rate of AERD in the CRS population (0.57%).
Table 1.
Demographics of CRS patients for clinical investigation
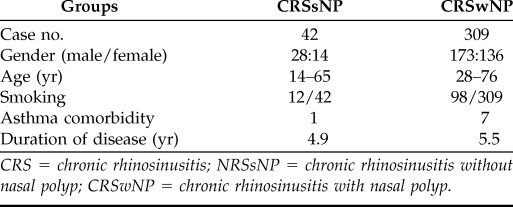
CRS = chronic rhinosinusitis; NRSsNP = chronic rhinosinusitis without nasal polyp; CRSwNP = chronic rhinosinusitis with nasal polyp.
Literature Search
We obtained 296 articles on the epidemiology of AERD in China from Chinese-language publications using the following key words: “Xiao Chuan” (asthma), “A Si Pi Lin” (aspirin), “Bi Xi Rou” (NPs), and “Samter San Lian Zhen” (Samter triad). Among these articles, 251 literature reviews or literature translations were excluded. This resulted in only 45 articles ultimately included in the systemic review.
A total of 346 cases of AERD were reported in 45 Chinese-language articles. Each article was classified as one of three types based on the level of affiliated hospital as follows. Type A (21 articles) included 187 cases of AERD; type B (19 articles) included 78 cases of AERD; type C (5 articles) included 81 cases of AERD. Most of the patients were 30–50 years old but some articles did not include this information. The available gender ratio was 193 male patients versus 147 female patients. Some articles did not include gender information.
The nonsteroidal anti-inflammatory drugs used in literatures included acetylsalicylic acid, indomethacin, flurbiprofen, ibuprofen, acetaminophen, piroxicam, sulindac, diflunisal, oxaprozin, etc. AERD was diagnosed by oral aspirin provocation test in 5 studies (48 cases); in another 18 studies, hypersensitivity symptoms occurred after aspirin administration during hospitalization (51 cases); other cases were established by previous medical history.
DISCUSSION
In the present study, we found that the prevalence of AERD in Chinese patients with CRS is rather low (0.57%) based on a preliminary cohort case analysis, and the incidence of concomitant asthma in the CRS population was also low (2.27%), which is consistent with our previous report.4 To further validate our hypothesis that asthma comorbidity and subsequent AERD are rare in Chinese patients with CRS, we conducted a systematic review of studies that reported sporadic cases during the treatment of CRS. Of the 45 available Chinese-language articles, only one study included >100 patients with AERD (102 cases; time span, 8 years).6 According to the average CRS prevalence of 5% in the general population, there should be >70,000,000 CRS patients in China. However, we obtained a total of 346 cases of AERD from 45 Chinese-language articles. In combination with our reported epidemiology of AERD in CRS patients (0.57% for AERD and 2.27% for asthma), it is interesting to note that the incidences of concomitant asthma and subsequent AERD are indeed low in China.
AERD is a very common disease in patients with CRSwNP in western industrialized countries.7 For example, Patriarca et al. investigated 154 patients with CRSwNP as the candidates for sinus surgery and found that 35% of them had AERD and 40% of them had concomitant bronchial asthma.8 Hedman et al. conducted a survey of 4300 general residents in south Finland by questionnaire and found the incidence of asthma to be 4.4%, and the incidence of AERD was 5.7%.9 Our study thus suggested a tremendous gap in prevalence of AERD when compared with other ethnic populations. However, the mechanism underlying this difference in AERD prevalence is unclear.
Currently, the etiology of aspirin hypersensitivity is complex and not fully understood. Aspirin hypersensitivity is likely related to the inhibition of cyclooxygenase by aspirin.10 Moreover, it has also been shown that eosinophil recruitment plays an essential role in the inflammatory response that characterizes AERD.11,12 For example, eosinophil numbers obtained in bronchial biopsy specimens and NPs derived from AERD patients are fourfold greater than in airway biopsy specimens from aspirin-tolerant asthmatic patients and 15-fold more numerous than in healthy subjects.13 Because there is limited literature concerning the incidence of AERD among the Chinese CRS population, it is difficult to draw a solid conclusion on risk factors underlying AERD development. Previously, we have reported that Chinese CRSwNP patients presented distinct histological and clinical characteristics (low eosinophilia, prominent neutrophil infiltration, mixed Th2/Th17 predominance, and low asthma comorbidity) when compared with the western population.4,14 These prospective studies on the immunopathological characteristics of CRSwNP might provide the initial clues to link the inflammatory patterns of CRSwNP with concomitant morbidity.
Considering the bias of CRS cases and the limitation of diagnosis in this study, this low incidence of AERD among CRS patients might be underestimated to some extent. Nonetheless, it is still important to note the low epidemiology of AERD in Chinese CRS patients with an estimated AERD prevalence of 1% in the general population and of 10% among asthmatic patients in the western population. Therefore, further understanding as to whether low eosinophilia accounts for the low prevalence of AERD in China is of great interest.
CONCLUSIONS
In summary, we provided preliminary findings that the incidence of AERD is much lower in Chinese CRS patients (0.57%), which might be a consequence of low nasal tissue eosinophilia. However, additional study is required to elucidate the molecular mechanisms underlying the low AERD prevalence in China.
Footnotes
Funded by grants from the National Natural Science Grant of China (U0832007, 81070771, and 81070772), Guangdong Province Natural Science Grant (9151006001000014, S2011010004634, and S2011020002295), and Program for New Century Excellent Talents in University (NCET-10-0851)
The authors have no conflicts of interest to declare pertaining to this article
REFERENCES
- 1. Fokkens W, Lund V, Mullol J. European Position Paper on Rhinosinusitis and Nasal Polyps group. European position paper on rhinosinusitis and nasal polyps 2007. Rhinology 45(suppl):1–136, 2007. [PubMed] [Google Scholar]
- 2. Jenneck C, Juergens U, Buecheler M, et al. Pathogenesis, diagnosis, and treatment of aspirin intolerance. Ann Allergy Asthma Immunol 99:13–21, 2007. [DOI] [PubMed] [Google Scholar]
- 3. Picado C. Aspirin intolerance and nasal polyposis. Curr Allergy Asthma Rep 2:488–493, 2002. [DOI] [PubMed] [Google Scholar]
- 4. Fan Y, Chen S, Qu X, et al. A lower prevalence of asthma among patients with chronic rhinosinusitis in southern China. J Allergy Clin Immunol 127:520–522, 2011. [DOI] [PubMed] [Google Scholar]
- 5. Macy E, Bernstein JA, Castells MC, et al. Aspirin challenge and desensitization for aspirin-exacerbated respiratory disease: A practice paper. Ann Allergy Asthma Immunol 98:172–174, 2007. [DOI] [PubMed] [Google Scholar]
- 6. Zhang R, Zhang HY. The prevalence of aspirin-induced asthma. Zhong Hua Jie He He Hu Xi Za Zhi 8:187–188, 1985. [Google Scholar]
- 7. Katotomichelakis M, Riga M, Davris S, et al. Allergic rhinitis and aspirin-exacerbated respiratory disease as predictors of the olfactory outcome after endoscopic sinus surgery. Am J Rhinol Allergy 23:348–353, 2009. [DOI] [PubMed] [Google Scholar]
- 8. Patriarca G, Romano A, Schiavino D, et al. ASA disease: The clinical relationship of nasal polyposis to ASA intolerance. Arch Otorhinolaryngol 243:16–19, 1986. [DOI] [PubMed] [Google Scholar]
- 9. Hedman J, Kaprio J, Poussa T, et al. Prevalence of asthma, aspirin intolerance, nasal polyposis and chronic obstructive pulmonary disease in a population-based study. Int J Epidemiol 28:717–722, 1999. [DOI] [PubMed] [Google Scholar]
- 10. Zander KA, Saavedra MT, West J, et al. Protein microarray analysis of nasal polyps from aspirin-sensitive and aspirin-tolerant patients with chronic rhinosinusitis. Am J Rhinol Allergy 23:268–272, 2009. [DOI] [PubMed] [Google Scholar]
- 11. Haruna S, Nakanishi M, Otori N, et al. Histopathological features of nasal polyps with asthma association: An immunohistochemical study. Am J Rhinol 18:165–172, 2004. [PubMed] [Google Scholar]
- 12. Awad OG, Fasano MB, Lee JH, et al. Asthma outcomes after endoscopic sinus surgery in aspirin-tolerant versus aspirin-induced asthmatic patients. Am J Rhinol 22:197–203, 2008. [DOI] [PubMed] [Google Scholar]
- 13. Fuentes-Beltrán A, Montes-Vizuet R, Valencia-Maqueda E, et al. Chemokine CC-ligand 5 production and eosinophil activation into the upper airways of aspirin-sensitive patients. Clin Exp Allergy 39:491–499, 2009. [DOI] [PubMed] [Google Scholar]
- 14. Cao PP, Li HB, Wang BF, et al. Distinct immunopathologic characteristics of various types of chronic rhinosinusitis in adult Chinese. J Allergy Clin Immunol 124:478–484, 2009. [DOI] [PubMed] [Google Scholar]


