Abstract
Background:
The cesarean section (C-section) has higher risk compared to normal vaginal delivery (NVD). The aim of this population-based study was to evaluate the frequency of mothers’ tendency toward the mode of delivery and the factors that can affect this inclination.
Materials and Methods:
This cross-sectional study was conducted from August 2011 to June 2012 in Fars Province, Iran, and comprised mothers in their 20th to 30th weeks of pregnancy. A questionnaire was designed to include, sociodemographic information, maternal knowledge, main sources of knowledge, attitude of the mother, husband, parents, close friends, and gynecologist, regarding the route of delivery, convenience factors, and barriers to choosing NVD, and mother's preference for the route of delivery.
Results:
Of 6921 participants, 2197 (31.7%) preferred C-section and 4308 (62.2%) favored NVD while 416 (6%) had no idea regarding the preferred route of delivery. Score of knowledge in 904 (13.1%) participants was zero, and 1261 women (18.2%) achieved an acceptable level of knowledge. Using binary logistic regression, positive history of previous abortion and/or infertility, higher education level of mother and husband, mother's unacceptable level of knowledge regarding complications of C-section, and mother's and husband's positive attitude toward C-section were determinant factors in choosing C-section as a preferred route of delivery.
Conclusion:
Appropriate measures should be taken to raise awareness and knowledge of mothers and all families about complications of the C-section. Establishment of clinics for painless NVD and assuring mothers of benefits and lower complications of NVD can reduce the tendency for C-sections.
Keywords: Attitude, barrier, cesarean section, knowledge, normal vaginal delivery
INTRODUCTION
The improved safety of surgical and anaesthetic skills is some of the major reasons for rapidly increasing rates of cesarean section (C-section) in many countries.[1,2,3] Other reasons are changing attitudes toward C-section among staff and patients.[4] The C-section has been regarded as a global epidemic and is the main concern for both health professionals and researchers.[5]
Mothers experience discomfort after C-section, which has higher risk compared to normal vaginal deliveries (NVD). The deliveries by C-section also have a negative impact on the health care system, which is due to its higher cost and requirement of additional resources.[6,7] It has also been reported that the increasing rate of C-section is accompanied by the higher incidence of some complications such as placental accreta.[8,9] Furthermore, compared to a planned vaginal delivery, transfer to a neonatal intensive care unit and risk of respiratory problems are doubled in a planned C-section.[10] Neonatal data suggest that infants born by scheduled C-sections are more likely to require advanced neonatal intensive support than those born to mothers via vaginal delivery. Clearly, this will further exacerbate the negative financial impact of a rising rate of C-section.[11]
C-section rates have continued to increase in the United States despite the national goal of Healthy People 2010, which aimed to reduce the rate of C-section delivery to 15%. Walker et al. reported a 35% increase in the rate of C-section from 1990 to 2000 in Australia.[12] In addition, 1.2 millions (29.1%) of births in the United States in 2004 were by C-section delivery.[13]
While C-section rates continue to rise, the rate of increase appears to be slowing down in most industrialized countries[14] like European communities where C-section rates are between 13% and 25%.[15,16]
The C-section rate is high in Iran, where based on the report of World Health Organization (WHO), 41.9% of deliveries were by C-section in 2008.[17] In 2009, a study conducted on 17,991 women in Iran showed that 35% of deliveries were done by C-section.[18] Another survey carried out in south west of Iran showed a rising trend of the C-section rate from 51.6% in 2007 to 53.3% in 2010.[19] On the basis of the WHO recommendations, the C-section rate should be kept between 10% and 15% of all deliveries.[20] In order to achieve this rate, it is necessary to determine the factors influencing the mode of delivery.
Apart from medical indications for C-section, it has been reported that C-section preference by women is generally related to cultural, social, psychological, and ethnic factors.[21] In Thailand, Muslim women were less likely to have C-section and older women mostly prefer to have C-section.[22] In Finland, the C-section rate was 15% among health professionals which was lower than normal population and less than other professionals such as teachers. It was concluded that health professionals have relatively conservative opinions about C-sections.[23] A Canadian study concluded that variations in the rate of C-section cannot be explained by patient illness or preferences. This variation is likely to reflect differences in practitioners’ approach to medical decision-making.[24] In addition, an Italian survey showed that one in five of Italian women preferred to have C-section and the factors associated with this choice were nulliparity, youth, lower education, and a previous C-section.[25] Furthermore, mothers’ preference for NVD versus C-section is mostly associated with their knowledge about maternal and neonatal complications of each mode.[26,27] According to a recent report from Iran, an older age, higher level of education, and marriage at older age were associated with a significantly higher rate of C-section.[18] In addition, advanced urbanization and socioeconomic status and delayed pregnancies are causes of high rates of C-section in Iran.[28] Therefore, the aim of this population-based study was to evaluate the frequency of mothers’ preference toward the mode of delivery and the factors affecting this tendency.
MATERIALS AND METHODS
Study design and population
This was an analytic cross-sectional study conducted from August 2011 to June 2012 in Fars, the fifth populated province in Iran. The study was approved by the Ethics committee of Shiraz University of Medical Sciences. Mothers participating in our program were in their 20th to 30th weeks of pregnancies and lived in the Fars province for at least 6 months prior to enrolling into the study. Considering 68,000 births in the Fars province in preceding year, the sample size was estimated about 6800. By adding 700 to our sample size, it was increased to 7500 to account for the probability of incomplete filling of questionnaires. The sampling method was stratified random sampling. In this study, we considered four strata for maternity services including urban versus rural areas, and private versus public sectors. On the basis of the data recorded in the Family Health Unit affiliated to Shiraz University of Medical Sciences in 2010, the sample size devoted to each stratum was calculated according to the proportion of the mothers who received care in each stratum. Thus, we distributed the questionnaires randomly in the first 3 days of each week for 11 months.
Data collection form
The data gathering form was designed by interviewing a number of pregnant ladies, as well as five gynecologists, and reviewing the related articles. Two community medicine specialists and a psychologist verified the questionnaire and its content validity. Pilot testing of the questionnaire with 57 Iranian women in their 20-30 weeks of pregnancy demonstrated good reliability (r = 0.86)
The questionnaire consisted of nine parts. These included sociodemographic information, maternal knowledge regarding C-section versus NVD complications, main source(s) of their knowledge, attitude of the mother, husband, parents, close friends, and gynecologist regarding the route of delivery, convenience factors as well as barriers in choosing NVD, and mother's preference toward the route of delivery.
The first part comprised 25 questions about mother's demographic and social information as well as obstetric and gynecologic history. The demographic questions included mother's name, national code, city of residence, cell phone number, the spouse's age, marriage age, birth place, and ethnicity. The socioeconomic class was determined according to the level of parents’ education, occupation, monthly income, expenditure, and insurance status. In addition, obstetric and gynecologic history included the number of gravidities, parities, abortions, still births, previous anomalous children, preceding routes of delivery and, if applicable, years of infertility. Additionally, mothers were asked to specify, if applicable, the type of clinic for receiving maternity care including private versus public hospitals, where they had their previous deliveries. In the second part, mother's knowledge about C-section was scored by means of 12 questions using 1- to 5-point Rating Scale. Each question related to one maternal or neonatal complication of NVD or C-section, with correct and wrong answers receiving 1 and 0 points, respectively. Therefore, the knowledge questions had scores ranging from 0 to 12. The third part assessed the importance of different sources of knowledge for mothers using a 6-point rating score scale ranging from “a subtle role” to “a substantial role”. The sources included television, radio, Internet, satellite, books, magazines, newspapers, DVDs, family, close friends, healthcare workers, gynecologist, and self-experience. The fourth part involved mother's perspective about the best route of delivery, assessed by using 12 questions. The fifth part represented peer's pressure, where we asked the mothers about the opinions of their husband, parents, close friends, and gynecologist about maternal and neonatal complications of C-section by eight questions. The barriers of choosing NVD were evaluated in part 7 that consisted of eight questions. Part 8 included four questions related to convenience, so called facilitating factors that evaluated preference for NVD. Parts 4 to 8 involved five-category responses ranging from “strongly agree” to “strongly disagree” which were scored from 5 to 1, respectively. One question in the last part with three options of NVD, C-section, and have not decided yet, concerned mother's preference for the route of delivery,
Statistical analysis
The data were analyzed with SPSS version 18 software. All the participants were categorized into three groups based on their preference toward mode of delivery; mothers who preferred NVD, those who preferred C-section, and mothers who did not make their mind at the time of interview. All the comparisons were among these three groups. The analysis of variance (ANOVA) test was used to compare mothers’ age, marriage age, number of living children, and abortions among the mentioned groups. In addition, ANOVA test was used to compare score of knowledge, attitude, barriers, and convenience factors among the three groups. The chi-square test was used to identify differences in mother's job, mothers’ education degree, husbands’ education degree, mothers’ insurance status, history of infertility (positive versus negative), and type of clinic for receiving service among the mentioned groups. Outcome-specific multivariate logistic regression models with the backward and forward stepwise method were used to identify the main reasons why mothers chose cesarean delivery. Differences with a P < 0.05 were considered statistically significant. The data are reported as the mean ± standard deviation, percentages, odds ratio, and confidence interval.
RESULTS
This study comprised a total of 6921 subjects with the response rate of 92.3%. The mean age of subjects was 27 ± 5.1 SD years. On the basis of the women's preference for mode of delivery subjects were divided into three groups. Of these subjects, 2197 (31.7%) preferred to have C-section and 4308 (62.2%) favored a normal vaginal delivery (NVD) and 416 (6%) had no idea regarding the route of delivery. The score of knowledge in 904 (13.1%) subjects was zero and equal score of knowledge which was less than 4 was found in 3710 (53.6%) participants. Although the maximum achievable score of knowledge was 12, only 1261 (18.2%) women achieved an acceptable level of knowledge which was 8 and higher.
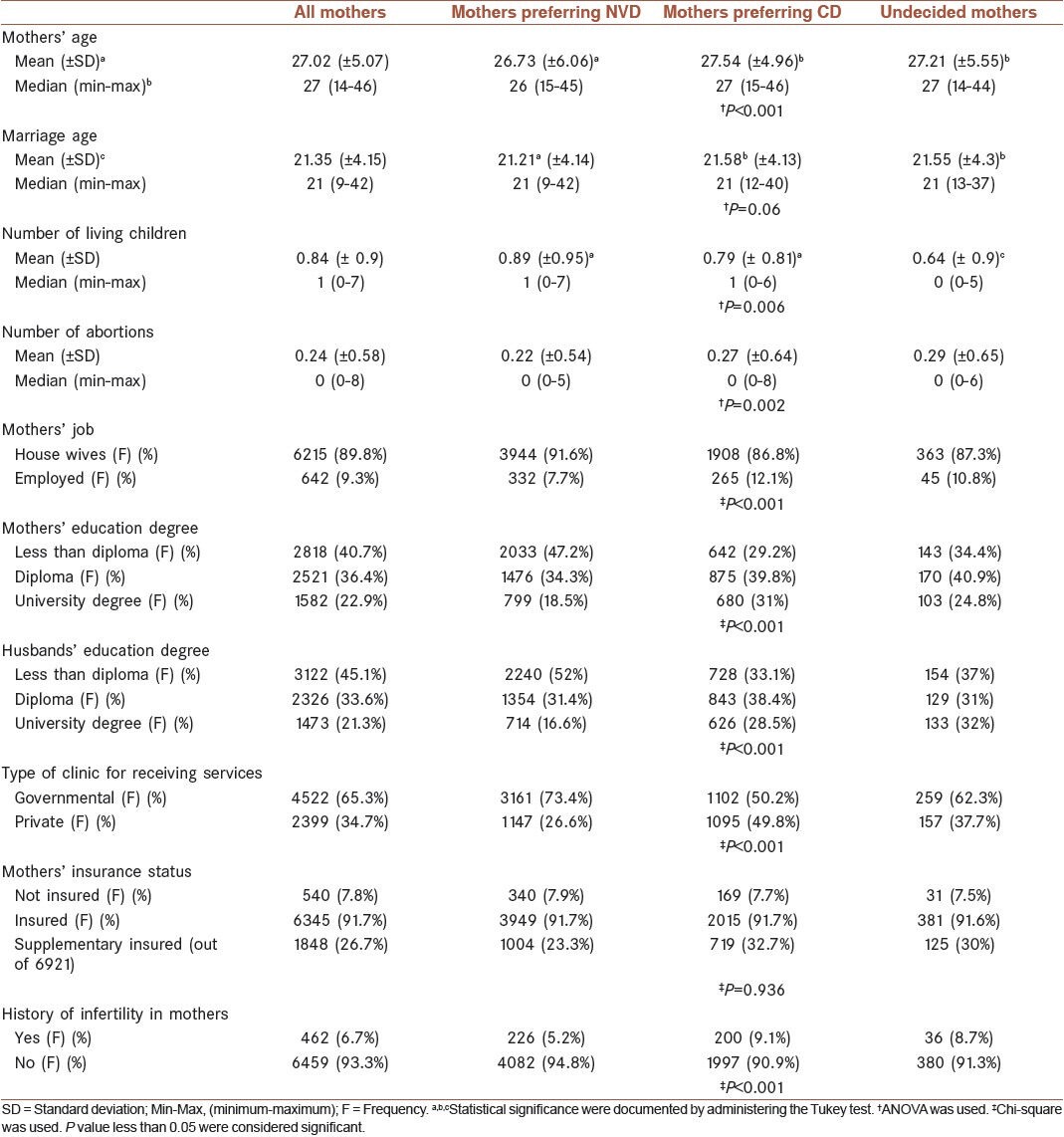
Mothers’ age (P < 0.001), number of living children (P 0.006), mothers’ job (P < 0.001) and level of education (P < 0.001), husbands’ level of education (P < 0.001), and history of infertility in mothers (P < 0.001) were significantly different among our three study groups. However, certain entities including mother's age, number of living children, and number of abortions were not clinically significant. On the other hand, mother's marriage age as well as their insurance status was not significantly different among the above-mentioned groups. Distribution of these demographic features of subject in the three groups and their statistical differences are shown in Table 1.
Table 1.
Distribution of demographic information of pregnant women
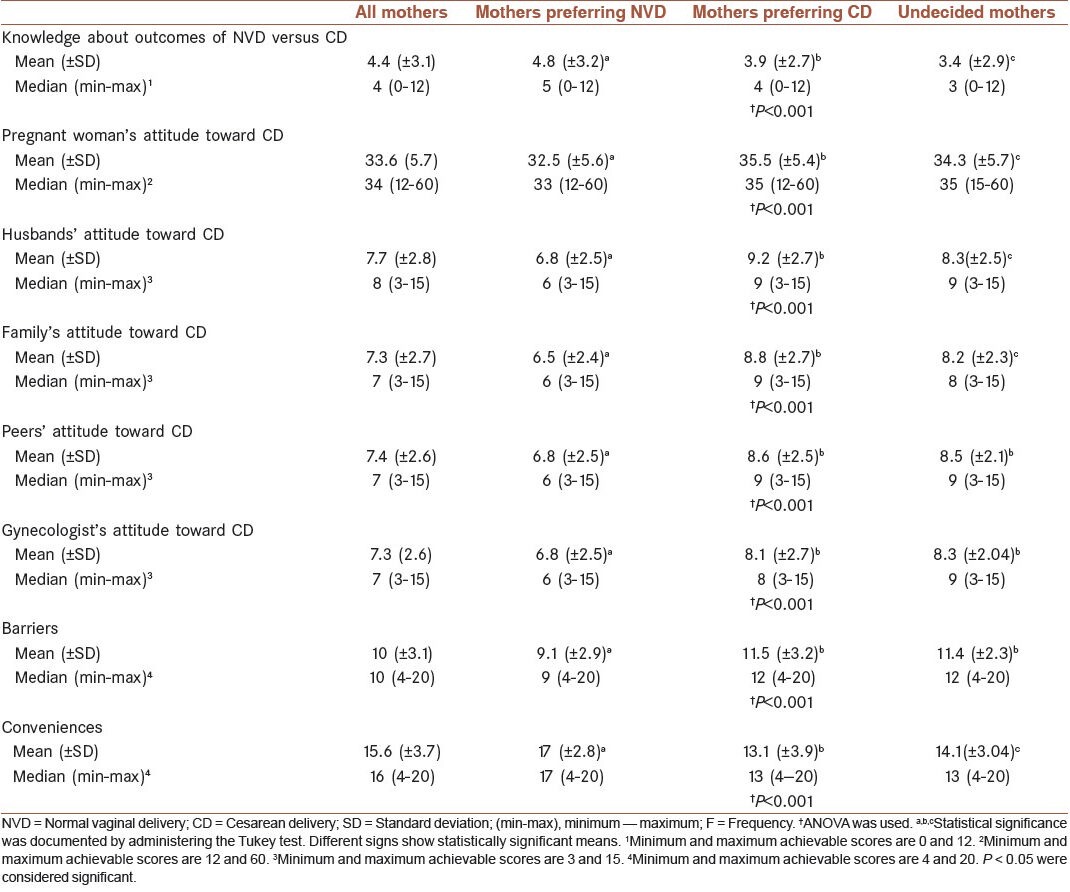
A comparative evaluation of mothers’ knowledge regarding the outcomes of C-section and NVD showed that those who preferred NVD had significantly higher knowledge (P < 0.001). As shown in Table 2, a significantly higher attitude toward the C-section was found in mothers (P < 0.001), their husbands (P < 0.001), families (P < 0.001), and their gynecologists (P < 0.001). Positive attitude toward NVD and C-section was observed in 63.7% and 28% of women respectively. Of all husbands, 61.2% had positive attitude toward NVD, while 24.3% favored C-section. The gynecologists believed that C-section was a safer mode of delivery for both mother and baby (P < 0.001). This conclusion was based on favorable response of women to C-section (23.9%) and to NVD (11.6%). These differences and their level of significance are also depicted by Table 2.
Table 2.
Comparative assessment of scores associated with knowledge, attitude, barriers, and conveniences, based on the preference of mothers for the route of delivery
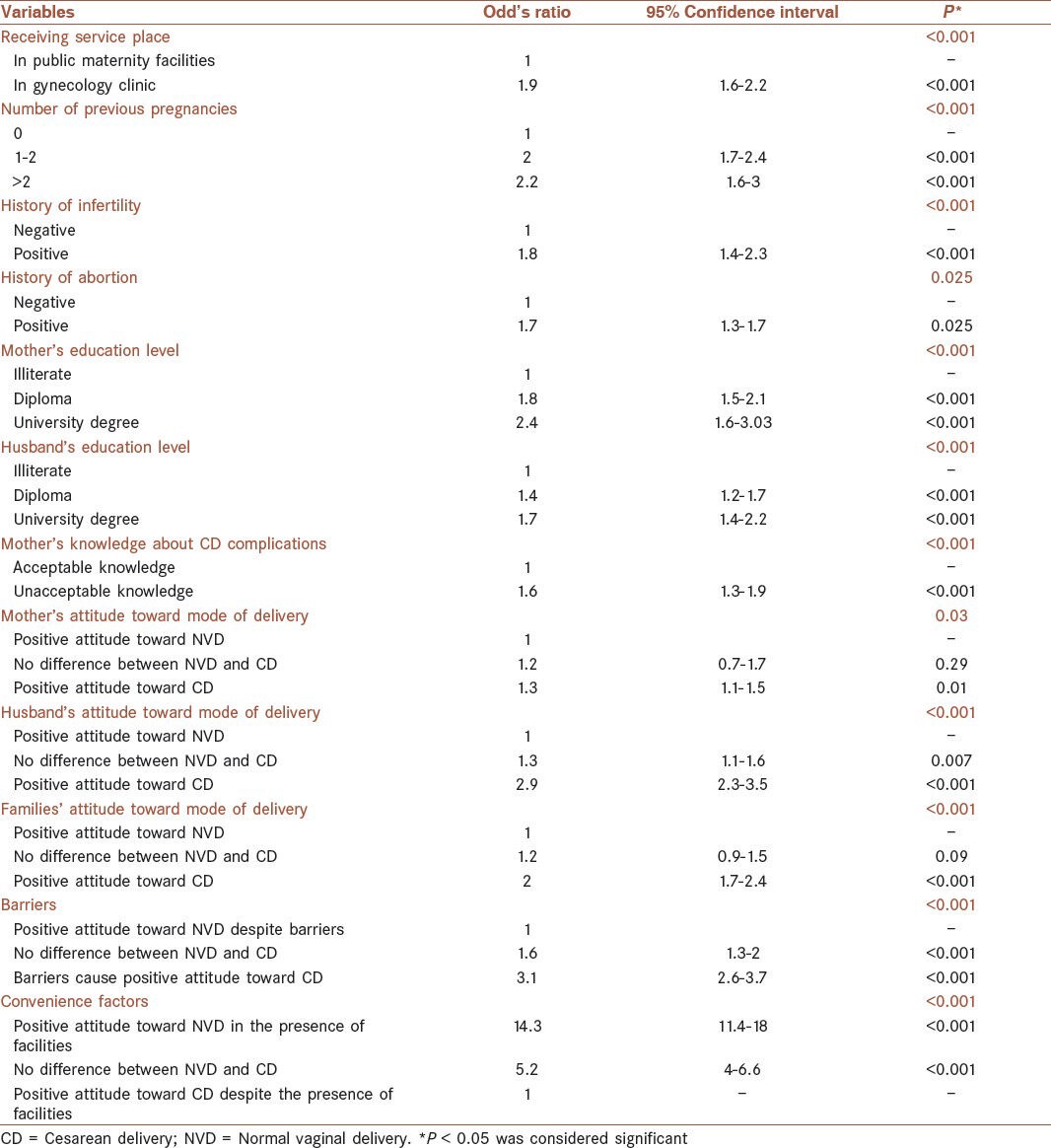
The preference for NVD or C-section was considered as dependent variable which entered into a binary logistic model together with the factors that were significantly associated with this dependent variable. The results showed that mothers receiving prenatal care in gynecology clinics were significantly (P < 0.001) more inclined to have C-section (OR = 1.9). Other factors involved in preferring C-section were positive history of previous abortion (OR = 1.7) and infertility (OR = 1.8), higher education of mothers (OR = 2.4) and their husbands (OR = 1.7), and mother's unacceptable level of knowledge about complications of C-section (OR = 1.6). Furthermore, positive attitude of mother (OR = 1.3), her husband (OR = 2.9), and their first-degree relatives (OR = 2) toward C-section were significantly associated with the higher risk of preferring C-section as a mode of delivery. While barriers such as delivery pain caused positive attitude toward C-section (OR = 3.1), mothers preferred to have NDV, if assured about some conveniences such as the presence of gynecologist during delivery, prevailing painless NVD and the safety of mother and baby (OR = 14.3). These results are shown in Table 3.
Table 3.
Determinant factors associated with preference for cesarean section by pregnant women
DISCUSSION
The majority of the subjects in this study preferred to have NVD and less than one-third favored C-section. Other studies also reported that most women preferred NVD.[25,29,30,31,32]
According to our study, C-section was considered safer for both mothers and their babies by those who favored this mode of delivery. A study conducted on women who had undergone maternal-request primary elective C-section indicated that concern for the health of baby was the main reason for choosing this mode of delivery.[33] Another study carried out in Sweden compared two groups of pregnant women, regarding their preference for C-section or vaginal delivery. The result also revealed that anxiety for the health of their baby and their own life was the main reason for selecting C-section.[34] However, Pevzner et al. reported women's attitude toward C-section and their studies showed that 95% of subjects were not in favor of C-section and 93% and 88% considered vaginal delivery to be safer for both mother and baby, respectively.[30]
Mother's age did not remain significant in logistic regression as an effective factor on mother's preference. However, a population-based study from Taiwan showed that there was a direct relationship between increasing age and the request for C-section. This study reported that compared to the 25-34 years age group those younger than 25 years were less and those older than 34 years were more likely to request for C-section delivery.[35] Regardless of maternal age, advancing paternal age also appeared to be an additional independent factor that was strongly associated with increasing rates of C-section.[36] Some other studies have also reported the association between advanced age and higher request for C-section.[18,28,37,38] The mean age of 27 ± 5 years showed that our subjects were young and this could be a reason for the inconsistency regarding age between this study and other investigations. The results showed poor knowledge of mothers regarding maternal and fetal complications of C-section, and women with a lower level of knowledge and higher attitude toward C-section were more likely to prefer this mode of childbirth. The same result has also been reported by other studies.[31,39] A study in Turkey was conducted on female healthcare providers and women from the general public on attitude toward route of delivery. Vaginal delivery was favored by 48.1% of healthcare providers and 69.6% of the public group (P = 0.001). In this context, 45.3% of healthcare providers and 20.6% of the public group had undergone a C-section without any medical indications (P = 0.001). It was shown that the preference for C-section was higher in Turkish healthcare providers than in the public. In both groups, the attitude toward C-section was of high demand.[40] However, in another study from Finland the C-section rate was 15% among health professionals, which was lower than ordinary people and less than other professionals like teachers. Health professionals had relatively conservative opinions and lower attitude toward C-sections.[22] A safer mode of delivery accounted for attitude toward C-section and reported to be the main reason for preferring C-section.[37]
Our results showed that mothers with a higher level of education were more likely to prefer C-section. An Italian study showed that women with lower education were more interested in cesarean and likelier to deliver by C-section. Considering the effect of parental education, that of mothers was a stronger predictor.[41] In Brazil, highly educated women and those from high socioeconomic class had a significantly higher preference for C-section and also experienced a higher rate of C-section.[42] A previous study from Iran reported that higher level of education was associated with preference for C-section.[18] In contrast, it has been reported that housewives were more likely to choose C-section than employed women and there was an inverse relationship between women's level of education and the rate of C-section.[43]
In our study previous history of C-section, abortion, and infertility were considered as risk factors for choosing C-section, a finding consistent with the results of previous reports on C-section[4,44] and history of infertility.[37]
Our study showed that convenience at delivery was a viable option for choosing C-section. This was similar to the results of other studies where convenience was reported to be associated with r reduced recovery pain, bleeding, sexual function, and faster recovery.[12,21,24,29,31] However, a systematic review of 54 papers published between 1990 and 2005 found no major differences between primary C-section on maternal request, and planned vaginal delivery with respect to neonatal and postpartum complication such as excess bleeding.[13]
Advanced urbanization can also be a reason for preference of C-section.[21,45] However, in our study living in rural or urban areas was unrelated to the route of delivery.
Our results also showed that preference for C-section was related to being visited at a gynecologist private office. The role of gynecologists in preferring a particular mode of delivery has previously been investigated. It may be a result of gynecologist's attitude toward the route of delivery. A study conducted in the Netherlands s that experienced gynecologists were more in favor of C-section.[46] Flores Padilla et al. showed that women attended by a gynecologist with more than 16 years of experience and by a resident were more likely to have C-section.[44] In addition, a Canadian study concluded that variations in the rate of C-section delivery cannot be explained in terms of patient illness or preferences. This variation was likely to reflect differences in practitioners’ approach to medical decision-making, which might be due to financial benefits of gynecologists.[23] However, a report from Taiwan showed that financial incentives of physicians did not impact the rate of C-section and the request by the mother was the main reason for having this mode of delivery.[47]
Although there was no significant difference in the type of insurance between women who preferred NVD and those who favored C-section, coverage by an additional insurance could indicate preference for C-section.[43]
In conclusion, regardless of the level of education, the preference for C-section can be minimized by increasing the knowledge of mothers and all families about C-section delivery and its attending complications. Establishing and developing clinics for painless NVD in the presence of gynecologist and ensuring mothers about benefits and lower complications of NVD can decline the rate of C-sections.
Footnotes
Source of Support: Health Policy Research Center
Conflict of Interest: The authors have no conflicts of interest.
REFERENCES
- 1.Gomes UA, Silva AA, Bettiol H, Barbieri MA. Risk factors for the increasing caesarean section rate in Southeast Brazil: A comparison of two birth cohorts, 1978-1979 and 1994. Int J Epidemiol. 1999;28:687–94. doi: 10.1093/ije/28.4.687. [DOI] [PubMed] [Google Scholar]
- 2.Caesarean section on the rise. Lancet. 2000;356:1697. [PubMed] [Google Scholar]
- 3.Dosa L. Caesarean section delivery, an increasingly popular option. Bull World Health Organ. 2001;79:1173. [PMC free article] [PubMed] [Google Scholar]
- 4.Pang SM, Leung DT, Leung TY, Lai CY, Lau TK, Chung TK. Determinants of preference for elective caesarean section in Hong Kong Chinese pregnant women. Hong Kong Med J. 2007;13:100–5. [PubMed] [Google Scholar]
- 5.Savage W. The caesarean section epidemic. J Obstet Gynaecol. 2000;20:223–5. doi: 10.1080/01443610050009485. [DOI] [PubMed] [Google Scholar]
- 6.Glazener CM, Abdalla M, Stroud P, Naji S, Templeton A, Russell IT. Postnatal maternal morbidity: Extent, causes, prevention and treatment. Br J Obstet Gynaecol. 1995;102:282–7. doi: 10.1111/j.1471-0528.1995.tb09132.x. [DOI] [PubMed] [Google Scholar]
- 7.Belizan JM, Althabe F, Barros FC, Alexander S. Rates and implications of caesarean sections in Latin America: Ecological study. BMJ. 1999;319:1397–400. doi: 10.1136/bmj.319.7222.1397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wu S, Kocherginsky M, Hibbard JU. Abnormal placentation: Twenty-year analysis. Am J Obstet Gynecol. 2005;192:1458–61. doi: 10.1016/j.ajog.2004.12.074. [DOI] [PubMed] [Google Scholar]
- 9.Yang Q, Wen SW, Oppenheimer L, Chen XK, Black D, Gao J, et al. Association of caesarean delivery for first birth with placenta praevia and placental abruption in second pregnancy. BJOG. 2007;114:609–13. doi: 10.1111/j.1471-0528.2007.01295.x. [DOI] [PubMed] [Google Scholar]
- 10.Kolas T, Saugstad OD, Daltveit AK, Nilsen ST, Oian P. Planned cesarean versus planned vaginal delivery at term: Comparison of newborn infant outcomes. Am J Obstet Gynecol. 2006;195:1538–43. doi: 10.1016/j.ajog.2006.05.005. [DOI] [PubMed] [Google Scholar]
- 11.Fogelson NS, Menard MK, Hulsey T, Ebeling M. Neonatal impact of elective repeat cesarean delivery at term: A comment on patient choice cesarean delivery. Am J Obstet Gynecol. 2005;192:1433–6. doi: 10.1016/j.ajog.2005.01.010. [DOI] [PubMed] [Google Scholar]
- 12.Walker R, Turnbull D, Wilkinson C. Increasing cesarean section rates: Exploring the role of culture in an Australian community. Birth. 2004;31:117–24. doi: 10.1111/j.0730-7659.2004.00289.x. [DOI] [PubMed] [Google Scholar]
- 13.Visco AG, Viswanathan M, Lohr KN, Wechter ME, Gartlehner G, Wu JM, et al. Cesarean delivery on maternal request: Maternal and neonatal outcomes. Obstet Gynecol. 2006;108:1517–29. doi: 10.1097/01.AOG.0000241092.79282.87. [DOI] [PubMed] [Google Scholar]
- 14.Declercq E, Young R, Cabral H, Ecker J. Is a rising cesarean delivery rate inevitable. Trends in industrialized countries, 1987 to 2007? Birth. 2011;38:99–104. doi: 10.1111/j.1523-536X.2010.00459.x. [DOI] [PubMed] [Google Scholar]
- 15.Saisto T, Halmesmaki E. Fear of childbirth: A neglected dilemma. Acta Obstet Gynecol Scand. 2003;82:201–8. [PubMed] [Google Scholar]
- 16.McFarlin BL. Elective cesarean birth: Issues and ethics of an informed decision. J Midwifery Womens Health. 2004;49:421–9. doi: 10.1016/j.jmwh.2004.05.010. [DOI] [PubMed] [Google Scholar]
- 17.Gibbons L, Belizán JM, Lauer JA, Betrán AP, Merialdi M, Althabe F. WHO; 2010. [Last accessed on 2013 May 27]. The Global Numbers and Costs of Additionally Needed and Unnecessary Caesarean Sections Performed per Year: Overuse as a Barrier to Universal Coverage. Available from: http://www.who.int/healthsystems/topics/financing/healthreport/30C-sectioncosts.pdf . [Google Scholar]
- 18.Ahmad-Nia S, Delavar B, Eini-Zinab H, Kazemipour S, Mehryar AH, Naghavi M. Caesarean section in the Islamic Republic of Iran: Prevalence and some sociodemographic correlates. East Mediterr Health J. 2009;15:1389–98. [PubMed] [Google Scholar]
- 19.Maharlouei N, Moalaee M, Ajdari S, Zarei M, Lankarani KB. Caesarean delivery in south-western Iran: Trends and determinants in a community-based survey. Med Princ Pract. 2013;22:184–8. doi: 10.1159/000341762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Betran AP, Merialdi M, Lauer JA, Bing-Shun W, Thomas J, Van Look P, et al. Rates of caesarean section: Analysis of global, regional and national estimates. Paediatr Perinat Epidemiol. 2007;21:98–113. doi: 10.1111/j.1365-3016.2007.00786.x. [DOI] [PubMed] [Google Scholar]
- 21.Porreco RP. Meeting the challenge of the rising cesarean birth rate. Obstet Gynecol. 1990;75:133–6. [PubMed] [Google Scholar]
- 22.Rachatapantanakorn O, Tongkumchum P. Demographic determinants for cesarean delivery in Pattani Hospital. Southeast Asian J Trop Med Public Health. 2009;40:602–11. [PubMed] [Google Scholar]
- 23.Hemminki E, Klemetti R, Gissler M. Cesarean section rates among health professionals in Finland, 1990-2006. Acta Obstet Gynecol Scand. 2009;88:1138–44. doi: 10.1080/00016340903214957. [DOI] [PubMed] [Google Scholar]
- 24.Hanley GE, Janssen PA, Greyson D. Regional variation in the cesarean delivery and assisted vaginal delivery rates. Obstet Gynecol. 2010;115:1201–8. doi: 10.1097/AOG.0b013e3181dd918c. [DOI] [PubMed] [Google Scholar]
- 25.Torloni MR, Betran AP, Montilla P, Scolaro E, Seuc A, Mazzoni A, et al. Do Italian women prefer cesarean section? Results from a survey on mode of delivery preferences. BMC Pregnancy Childbirth. 2013;13:78. doi: 10.1186/1471-2393-13-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Akbarzadeh K, Amidi M. The effects of health education on pregnant woman's knowledge and attitude on cesarean section. J Ilam Univ Med Sci. 2005;13:9. [Google Scholar]
- 27.Mungrue K, Nixon C, David Y, Dookwah D, Durga S, Greene K, et al. Trinidadian women's knowledge, perceptions, and preferences regarding cesarean section: How do they make choices? Int J Womens Health. 2010;2:387–91. doi: 10.2147/IJWH.S12857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Badakhsh MH, Alizadeh KH. Evaluation of the prevalence of cesarian section in medical centers affiliated to universities of medical sciences. J Med Counc IRI. 2000;18:4. [Google Scholar]
- 29.Bracken JN, Dryfhout VL, Goldenhar LM, Pauls RN. Preferences and concerns for delivery: An antepartum survey. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19:1527–31. doi: 10.1007/s00192-008-0680-1. [DOI] [PubMed] [Google Scholar]
- 30.Pevzner L, Goffman D, Freda MC, Dayal AK. Patients’ attitudes associated with cesarean delivery on maternal request in an urban population. Am J Obstet Gynecol. 2008;198:e35–7. doi: 10.1016/j.ajog.2007.10.778. [DOI] [PubMed] [Google Scholar]
- 31.Kasai KE, Nomura RM, Benute GR, de Lucia MC, Zugaib M. Women's opinions about mode of birth in Brazil: A qualitative study in a public teaching hospital. Midwifery. 2010;26:319–26. doi: 10.1016/j.midw.2008.08.001. [DOI] [PubMed] [Google Scholar]
- 32.Pevzner L, Preslicka C, Bush MC, Chan K. Women's attitudes regarding mode of delivery and cesarean delivery on maternal request. J Matern Fetal Neonatal Med. 2011;24:894–9. doi: 10.3109/14767058.2010.531797. [DOI] [PubMed] [Google Scholar]
- 33.Robson S, Carey A, Mishra R, Dear K. Elective caesarean delivery at maternal request: A preliminary study of motivations influencing women's decision-making. Aust N Z J Obstet Gynaecol. 2008;48:415–20. doi: 10.1111/j.1479-828X.2008.00867.x. [DOI] [PubMed] [Google Scholar]
- 34.Wiklund I, Edman G, Andolf E. Cesarean section on maternal request: Reasons for the request, self-estimated health, expectations, experience of birth and signs of depression among first-time mothers. Acta Obstet Gynecol Scand. 2007;86:451–6. doi: 10.1080/00016340701217913. [DOI] [PubMed] [Google Scholar]
- 35.Lin HC, Xirasagar S. Maternal age and the likelihood of a maternal request for cesarean delivery: A 5-year population-based study. Am J Obstet Gynecol. 2005;192:848–55. doi: 10.1016/j.ajog.2004.09.133. [DOI] [PubMed] [Google Scholar]
- 36.Tang CH, Wu MP, Liu JT, Lin HC, Hsu CC. Delayed parenthood and the risk of cesarean delivery--is paternal age an independent risk factor? Birth. 2006;33:18–26. doi: 10.1111/j.0730-7659.2006.00070.x. [DOI] [PubMed] [Google Scholar]
- 37.Chigbu CO, Ezeome IV, Iloabachie GC. Cesarean section on request in a developing country. Int J Gynaecol Obstet. 2007;96:54–6. doi: 10.1016/j.ijgo.2006.09.032. [DOI] [PubMed] [Google Scholar]
- 38.Coonrod DV, Drachman D, Hobson P, Manriquez M. Nulliparous term singleton vertex cesarean delivery rates: Institutional and individual level predictors. Am J Obstet Gynecol. 2008;198:694 e1–11. doi: 10.1016/j.ajog.2008.03.026. [DOI] [PubMed] [Google Scholar]
- 39.Dursun P, Yanik FB, Zeyneloglu HB, Baser E, Kuscu E, Ayhan A. Why women request cesarean section without medical indication? J Matern Fetal Neonatal Med. 2011;24:1133–7. doi: 10.3109/14767058.2010.531327. [DOI] [PubMed] [Google Scholar]
- 40.Koken G, Cosar E, Sahin FK, Tolga Arioz D, Duman Z, Aral I. Attitudes towards mode of delivery and cesarean on demand in Turkey. Int J Gynaecol Obstet. 2007;99:233–5. doi: 10.1016/j.ijgo.2007.05.031. [DOI] [PubMed] [Google Scholar]
- 41.Cesaroni G, Forastiere F, Perucci CA. Are cesarean deliveries more likely for poorly educated parents? A brief report from Italy. Birth. 2008;35:241–4. doi: 10.1111/j.1523-536X.2008.00245.x. [DOI] [PubMed] [Google Scholar]
- 42.Rebelo F, da Rocha CM, Cortes TR, Dutra CL, Kac G. High cesarean prevalence in a national population-based study in Brazil: The role of private practice. Acta Obstet Gynecol Scand. 2010;89:903–8. doi: 10.3109/00016349.2010.484044. [DOI] [PubMed] [Google Scholar]
- 43.Hsu KH, Liao PJ, Hwang CJ. Factors affecting Taiwanese women's choice of Cesarean section. Soc Sci Med. 2008;66:201–9. doi: 10.1016/j.socscimed.2007.07.030. [DOI] [PubMed] [Google Scholar]
- 44.Flores Padilla L, Gonzalez Perez GJ, Trejo Franco J, Vega Lopez G, Cabrera Pivaral CE, Campos A, et al. [Risk factors in cesarean section] Ginecol Obstet Mex. 2008;76:392–7. [PubMed] [Google Scholar]
- 45.Chen CS, Lin HC, Liu TC, Lin SY, Pfeiffer S. Urbanization and the likelihood of a cesarean section. Eur J Obstet Gynecol Reprod Biol. 2008;141:104–10. doi: 10.1016/j.ejogrb.2008.07.016. [DOI] [PubMed] [Google Scholar]
- 46.Kwee A, Cohlen BJ, Kanhai HH, Bruinse HW, Visser GH. Caesarean section on request: A survey in The Netherlands. Eur J Obstet Gynecol Reprod Biol. 2004;113:186–90. doi: 10.1016/j.ejogrb.2003.09.017. [DOI] [PubMed] [Google Scholar]
- 47.Lo JC. Financial incentives do not always work: An example of cesarean sections in Taiwan. Health policy. 2008;88:121–9. doi: 10.1016/j.healthpol.2008.02.013. [DOI] [PubMed] [Google Scholar]


