Abstract
Background:
Studies have shown the association of mood disorders and endothelial dysfunction, and increased risk of cardiovascular disease; however, mediatory mechanisms are not entirely clarified in this regard. We investigated the relationship between depression/anxiety symptoms with systemic inflammation and endothelial function.
Materials and Methods:
This cross-sectional study was performed in 2011 on employees of an oil company located in the Isfahan city (central Iran). Participants were selected with clustered random sampling. Anxiety and depression were evaluated by Hospital Anxiety Depression Scale (HADS). Systemic inflammatory status was evaluated by measuring sensitive C-reactive protein (high sensitive-CRP). To evaluate the endothelial function flow-mediated dilation (FMD) was measured.
Results:
During the study period, 254 participants (mean age = 51.4 ± 6.1 years) were evaluated. No significant relationship was found between high sensitive-CRP or FMD and any of the variables of anxiety or depression. In multivariate analysis, by controlling the possible confounding factors, no association was found between anxiety score, depression, or the overall score of HADS with high sensitive-CRP or FMD. After the separate analysis of patients with and without diabetes, depression score was correlated inversely with FMD among patients with diabetes (r = 0.525, P = 0.021).
Conclusion:
According to the results, in the studied population, there was no relationship between anxiety/depression with systemic inflammation or endothelial dysfunction, while in individuals with diabetes, depression was associated with endothelial dysfunction. In this regard more cohort studies are recommended.
Keywords: Anxiety, cardiovascular diseases, depression, inflammation, vascular endothelial
INTRODUCTION
Evidences have shown the role of psychosocial and behavioral factors in the etiology and physiopathology of cardiovascular disease (CVD)[1] While decrease in the vascular elasticity is an indicator for endothelial dysfunction, which is the first step of atherosclerosis before the plaque formation and clinical onset of disease, evidences showed that the psychological stresses can cause endothelial dysfunction.[2] In patients with endothelial dysfunction brachial artery has a higher peripheral resistance during psychological stress, and after the psychological stress the dilation of the brachial artery reduced allied with the flow of brachial artery.[3] In recent years some studies have reported the association of reduced endothelial function with clinical depression and anxiety and subclinical mood status, such as hostility or anger. Recent reports have shown that older adults, who have more anxiety characteristics are encountered with a higher risk of CVD and atherosclerosis, and probably anxiety is a predisposing risk factor for cardiovascular damage and atherosclerotic lesions in a long period.[4] The mechanisms responsible for this association remain unclear; however, inflammatory processes have been implicated[5] Low-grade systemic inflammation, accompanied with slightly increased concentrations of inflammatory markers such as C-reactive protein (CRP), is involved in the pathophysiology of several diseases including CVD.[6,7,8,9] On the contrary, several studies have shown the relationship between depression and increased levels of CRP.[5] Indeed, mood disorders including depression are associated with the secretion of pre-inflammatory cytokines such as interleukin (IL)-1 and IL-6[10] which induce the synthesis of CRP in the liver.[11]
Endothelial function has a key role in determining the clinical presentation of atherosclerosis, and it is involved in developing the atherosclerosis process before overt CVD.[12] Limited data are available about the association of CRP levels and endothelial dysfunction with mood characteristics. The aim of this study was to evaluate the relationship between depression/anxiety symptoms with CRP level, as a marker of systemic inflammation, and also with flow-mediated dilation (FMD), as a marker of endothelial function.
MATERIALS AND METHODS
Participants and setting
This cross-sectional study was performed in 2011 on employees aged 40-60 years in a major oil company located in Isfahan city (central Iran). Among 879 employees, one third were selected from all different parts of the company with clustered random sampling method. Participants with the history of ischemic heart disease, chronic renal failure, advanced liver disease, cerebrovascular accidents, any proven cancer, multiple sclerosis and major psychiatric disorders (including major depression, bipolar disorder, and psychotic disorder) were not included. A total 258 of these individuals were selected. The design of this study was confirmed by Medical Ethics Committee of Isfahan University of Medical Sciences, and written consent was obtained from all participants after explaining the objectives and methods of the study.
Assessments
The Persian version of the Hospital Anxiety Depression Scale (HADS) which has acceptable validity and reliability (Cronbach's alpha, 0.78-0.86)[13] was used for the evaluation of anxiety and depression symptoms. The HADS is one of the most widely used instruments to rapidly measure psychological status in patient as well as non-patient populations. It includes 14 questions (7 items per subscale) that each question is scored from 0 to 3 and the final score for each subscale ranges from 0 to 21. According to studies, grades 8 and higher is indicative for the relating subtest disorder.[14]
Systemic inflammation and endothelial function: To check the status of systemic inflammation, high sensitive CRP) was measured by venous blood samples using Sigma-Aldrich, USA commercial available kit. For the evaluation of vascular endothelial function, Doppler ultrasound was used and brachial arterial diameter was measured during the blockage of artery (with the inflation of sphygmomanometer cuff at least 50 mm Hg above the systolic blood pressure) and after the removal of blockage, FMD was measured by calculating the increased percentage of the arterial diameter after the removal of blockage comparing with the blockage state. Ultrasonography was done with Ultrasound, cardiac (Sonosite, USA).
Participants categorized in three classes of SES based on the average of monthly income, job, living area, and educational status.
Blood pressure measured using a standard digital sphygmomanometer. BMI calculated by ratio of body weight per kilogram to square of height per meter and all laboratory indexes measured by fast blood sampling from all cases.
Data analyses
The obtained data were analyzed using SPSS software for windows version 16.0. To investigate the relationship between CRP and FMD with the scores of anxiety and depression Spearman test (due to their non-normal distribution) was used. Also, multivariate linear regression test was used to evaluate the independent relationship of CRP and FMD on each of the anxiety and depression scores while controlling the other factors.
RESULTS
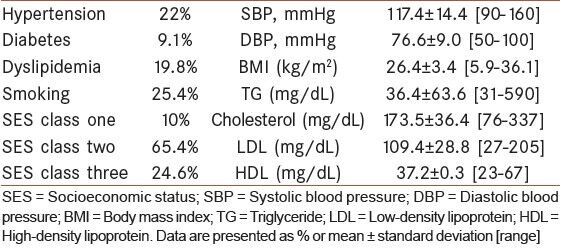
During the study, 254 participants including 252 males and 2 females aged 40-60 years, mean age = 51.4 ± 6.1 years, were investigated. Considered demographic variables and some cardiovascular risk factors are reported in Table 1.
Table 1.
Cardiovascular risk factors among participants
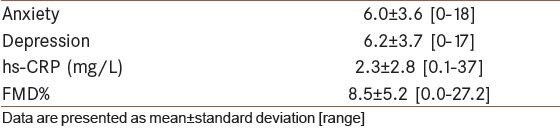
Flow-mediated dilation, serum high-sensitive C-reactive protein levels, and anxiety and depression scores are summarized in Table 2. Considering the cut-off point of ≥8 in the Hospital Anxiety Depression Scale questionnaire, 31.2% of the participants had clinical anxiety disorder and 40.1% had depressive disorder.
Table 2.
Anxiety/depression scores, high-sensitive C-reactive proteinlevel, and flow-mediated dilation in participants
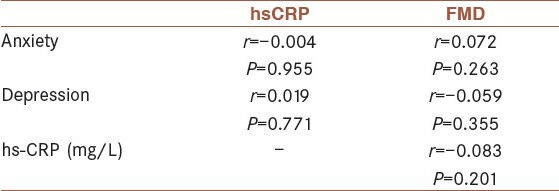
According to the Spearman test it was not any significant relationship between high-sensitive C-reactive protein (hs-CRP) or flow-mediated dilation (FMD) with any of the anxiety or depression scores. Also, no association was found between serum hs-CRP level and FMD [Table 3].
Table 3.
Correlation of each personality traits’ score with high-sensitive C-reactive protein and flow-mediated dilation in participants
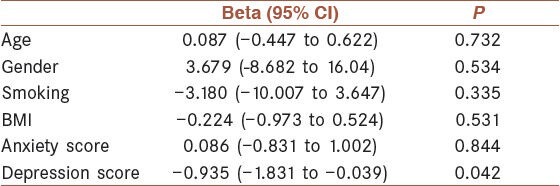
In multivariate analysis, with controlling the factors such as age, body mass index (BMI), lipid profile, history of cardiovascular disease and diabetes, no association was found between anxiety/depression, or the overall Hospital Anxiety Depression Scale scores with high-sensitive C-reactive protein or flow-mediated dilation (FMD). After the separate analysis of patients with and without diabetes, depression scores were significantly and inversely associated with FMD in patients with diabetes (r = −0.525, P = 0.021). In multivariate analysis by controlling the age, gender, smoking, BMI, and anxiety scores this association was still exist (P = 0.042). [Table 4]
Table 4.
Linear regression analysis of possible predictors of flow-mediated dilation
DISCUSSION
Evidences have shown the association of psychological factors such as anxiety/depression and stress with endothelial dysfunction and increased risk of CVD.[15,16] According to a new meta-analysis, including studies on healthy subjects and also patients with CVD, mood disorders have been associated with endothelial dysfunction measured by FMD (an early marker of CVD)[17] Also, using antidepressant medication in patients with CVD who were depressed was associated with improved FMD[18,19] However, the responsible mechanisms for this association are not clear yet.[15] The effects of psychological factors on the immune system have been considered and reviewed for long. Many studies also showed the reciprocal interaction of the immune system and behavior/emotion.[20,21,22] On the contrary, a systemic inflammatory state is known as a risk factor for CVD.[23,24,25] Consequently, it is possible that at least part of the effect of psychological factors on the increased risk of CVD is due to the increased systemic inflammatory and pre-inflammatory factors.[16] In our study, the relationship of these symptoms of anxiety/depression with serum levels of hs-CRP (a marker of systemic inflammation) with the percentage of FMD (indicating endothelial function) in employees of an industrial company were investigated. According to the results, no relationship was found between anxiety/depression and endothelial dysfunction or systemic inflammation, though increased depression was associated with reduced FMD in diabetic patients.
Evidences concerning the relationship between depression/anxiety and serum CRP level have indicated different results. Several studies have been conducted on the general population and also on patients with specific diseases. Results of a meta-analysis suggest that in normal population and depressed patients, there is a direct relationship between the severity of depression and serum levels of CRP, IL-1, and IL-6, while BMI is a meditative factor in this regard. Three general routes are suggested in this regard; the effect of depression on inflammation; the effect inflammation on depression; and also the bidirectional relationship.[1] The studies on patients with coronary artery disease,[26] dialysis patients[27,28] and patients with fibromyalgia,[29] have indicated a relationship between anxiety/depression severity and serum levels of CRP. In patients with symptoms of obstructive sleep apnea, serum level of CRP has been significantly associated with anxiety and depression severity, and patients with combined mood disorder had the highest CRP levels.[30] Interestingly, according to a meta-analysis, the treatment of depression with antidepressants reduces inflammatory markers such as IL-6 and CRP.[31] A cohort study in general population also showed that anxiety symptoms increase the hs-CRP level of more than 3.0 mg/L with 2.19 times, while anxiety symptoms combined with depression increases this level by 1.7 times.[32] Another study on healthy subjects showed that depression is independently associated with abnormal changes in heart rate, systemic inflammation, and endothelial function.[33]
In contrast, certain other studies on diabetic patients,[34] patients with acute coronary syndrome,[35] and patients with cancer,[36] did not show the relationship between anxiety/depression and serum levels of CRP. In the study on adults with and without clinical anxiety, the results showed a relationship between anxiety and IL-6 (preinflammatory According cytokines), while anxiety had no correlation with CRP level.[37] other study by Bjerkes et al.,[38] on a large sample from normal population, the association of CRP and depression was influenced by confounding factors such as chronic illness, smoking, and BMI > 30, as the odds ratio was reduced from 1.28-1.08 by controlling these factors.[38] Also, in a cohort study with 5-year follow-upon patients with coronary artery disease, mood disorder significantly predicted the level of IL-6 and CRP, but inflammatory markers were not predictive for depression symptoms in the follow-up. However, according to the analyses by controlling the health behaviors associated with depression such as physical activity, smoking, and BMI, we found no association between depression and systemic inflammation. These results show that health behaviors are among the mediators of the effect of depression on the inflammatory response and subsequent coronary disease.[39] However, the results of our analysis in diabetic patients showed that by controlling the factors such as BMI and smoking the effect of depression on FMD percentage is still remained.
Although most previous studies have shown the effects of anxiety/depression on endothelial dysfunction (decreased percent FMD), the role of systemic inflammation as part of the mechanism of this relationship has not been confirmed by all studies. We found no relationship between anxiety/depression and FMD that could be influenced by several factors. As a limitation of our study, the instrument used to measure anxiety and depression (HADS) mostly assesses the current situation (2 weeks) of persons, while in some studies the instrument examined the trait of anxiety (in contrast with the anxiety state).[4,26] Also, the duration of mood disorder, for which we had no information, may be an effective factor on the impact of mood disorders on endothelial function. In one study on healthy older adults, anxiety disorders has been associated with sympathetic activity and endothelial dysfunction (reduced FMD)[40] ; however, this relationship has not been seen in the younger individuals.[4] This finding indicates that the periods of exposure may be an important factor in the impact of mood disorders on endothelial function. Finally, it seems that more investigations especially cohort studies are needed regarding the relationship between mood symptoms and endothelial function with the assessment of duration of mood disorder.
CONCLUSION
According to the results, in the studied population there was no relationship between anxiety/depression and systemic inflammation or endothelial dysfunction, while in individuals with diabetes, depression was associated with endothelial dysfunction. In this regard, more cohort studies with evaluation for the duration of mood disorder are recommended.
ACKNOWLEDGMENTS
This study was conducted with financial support of the Isfahan University of Medical Sciences. Authors are thankful to Mrs. Hassanzadeh, Dr. Tarahomi, and Dr. Gashnizjani who helped us conducting this study. Also, we are thankful to Dr. Gholamrezaei who helped us in data analyses and editing this report.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Sararoodi BR. Type D penonality. J Res Behav Sci. 2009;7:75–86. [Google Scholar]
- 2.Lin TK, Weng CY, Wang WC, Chen CC, Lin IM, Lin CL. Hostility trait and vascular dilatory functions in healthy Taiwanese. J Behav Med. 2008;31:517–24. doi: 10.1007/s10865-008-9177-0. [DOI] [PubMed] [Google Scholar]
- 3.Harris KF, Matthews KA, Sutton-Tyrrell K, Kuller LH. Associations between psychological traits and endothelial function in postmenopausal women. Psychosom Med. 2003;65:402–9. doi: 10.1097/01.psy.0000035720.08842.9f. [DOI] [PubMed] [Google Scholar]
- 4.Narita K, Murata T, Hamada T, Takahashi T, Kosaka H, Yoshida H, et al. Association between trait anxiety and endothelial function observed in elderly males but not in young males. Int Psychogeriatr. 2007;19:947–54. doi: 10.1017/S1041610206004571. [DOI] [PubMed] [Google Scholar]
- 5.Howren MB, Lamkin DM, Suls J. Associations of depression with C-reactive protein, IL-1, and IL-6: A meta-analysis. Psychosom Med. 2009;71:171–86. doi: 10.1097/PSY.0b013e3181907c1b. [DOI] [PubMed] [Google Scholar]
- 6.Clearfield MB. C-reactive protein: A new risk assessment tool for cardiovascular disease. J Am Osteopath Assoc. 2005;105:409–16. [PubMed] [Google Scholar]
- 7.Paul A, Ko KW, Li L, Yechoor V, McCrory MA, Szalai AJ, et al. C-reactive protein accelerates the progression of atherosclerosis in apolipoprotein E-deficient mice. Circulation. 2004;109:647–55. doi: 10.1161/01.CIR.0000114526.50618.24. [DOI] [PubMed] [Google Scholar]
- 8.Pearson TA, Mensah GA, Alexander RW, Anderson JL, Cannon RO, 3rd, Criqui M, et al. Centers for Disease Control and Prevention; American Heart Association. Markers of inflammation and cardiovascular disease: Application to clinical and public health practice: A statement for healthcare professionals from the Centers for Disease Control and Prevention and the American Heart Association. Circulation. 2003;107:499–511. doi: 10.1161/01.cir.0000052939.59093.45. [DOI] [PubMed] [Google Scholar]
- 9.Torzewski J, Torzewski M, Bowyer DE, Fröhlich M, Koenig W, Waltenberger J, et al. C-reactive protein frequently colocalizes with the terminal complement complex in the intima of early atherosclerotic lesions of human coronary arteries. Arterioscler Thromb Vasc Biol. 1998;18:1386–92. doi: 10.1161/01.atv.18.9.1386. [DOI] [PubMed] [Google Scholar]
- 10.Godbout JP, Glaser R. Stress-induced immune dysregulation: Implications for wound healing, infectious disease and cancer. J Neuroimmune Pharmacol. 2006;1:421–7. doi: 10.1007/s11481-006-9036-0. [DOI] [PubMed] [Google Scholar]
- 11.Eklund CM. Proinflammatory cytokines in CRP baseline regulation. Adv Clin Chem. 2009;48:111–36. doi: 10.1016/s0065-2423(09)48005-3. [DOI] [PubMed] [Google Scholar]
- 12.Teper E, O’Brien JT. Vascular factors and depression. Int J Geriatr Psychiatry. 2008;23:993–1000. doi: 10.1002/gps.2020. [DOI] [PubMed] [Google Scholar]
- 13.Montazeri A, Vahdaninia M, Ebrahimi M, Jarvandi S. The Hospital Anxiety and Depression Scale (HADS): Translation and validation study of the Iranian version. Health Qual Life Outcomes. 2003;1:14. doi: 10.1186/1477-7525-1-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J Psychosom Res. 2002;52:69–77. doi: 10.1016/s0022-3999(01)00296-3. [DOI] [PubMed] [Google Scholar]
- 15.Steiner M. Serotonin, depression, and cardiovascular disease: Sex-specific issues. Acta Physiol (Oxf) 2011;203:253–8. doi: 10.1111/j.1748-1716.2010.02236.x. [DOI] [PubMed] [Google Scholar]
- 16.Player MS, Peterson LE. Anxiety disorders, hypertension, and cardiovascular risk: A review. Int J Psychiatry Med. 2011;41:365–77. doi: 10.2190/PM.41.4.f. [DOI] [PubMed] [Google Scholar]
- 17.Cooper DC, Tomfohr LM, Milic MS, Natarajan L, Bardwell WA, Ziegler MG, et al. Depressed mood and flow-mediated dilation: A systematic review and meta-analysis. Psychosom Med. 2011;73:360–9. doi: 10.1097/PSY.0b013e31821db79a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pizzi C, Mancini S, Angeloni L, Fontana F, Manzoli L, Costa GM. Effects of selective serotonin reuptake inhibitor therapy on endothelial function and inflammatory markers in patients with coronary heart disease. Clin Pharmacol Ther. 2009;86:527–32. doi: 10.1038/clpt.2009.121. [DOI] [PubMed] [Google Scholar]
- 19.Sherwood A, Hinderliter AL, Watkins LL, Waugh RA, Blumenthal JA. Impaired endothelial function in coronary heart disease patients with depressive symptomatology. J Am Coll Cardiol. 2005;46:656–9. doi: 10.1016/j.jacc.2005.05.041. [DOI] [PubMed] [Google Scholar]
- 20.Blume J, Douglas SD, Evans DL. Immune suppression and immune activation in depression. Brain Behav Immun. 2011;25:221–9. doi: 10.1016/j.bbi.2010.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ho RC, Neo LF, Chua AN, Cheak AA, Mak A. Research on psychoneuroimmunology: Does stress influence immunity and cause coronary artery disease? Ann Acad Med Singapore. 2010;39:191–6. [PubMed] [Google Scholar]
- 22.Anisman H, Merali Z. Cytokines, stress and depressive illness: Brain-immune interactions. Ann Med. 2003;35:2–11. doi: 10.1080/07853890310004075. [DOI] [PubMed] [Google Scholar]
- 23.Pfutzner A, Schondorf T, Hanefeld M, Forst T. High-sensitivity C-reactive protein predicts cardiovascular risk in diabetic and nondiabetic patients: Effects of insulin-sensitizing treatment with pioglitazone. J Diabetes Sci Technol. 2010;4:706–16. doi: 10.1177/193229681000400326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lavie CJ, Milani RV, Verma A, O’Keefe JH. C-reactive protein and cardiovascular diseases--is it ready for primetime? Am J Med Sci. 2009;338:486–92. doi: 10.1097/MAJ.0b013e3181c61b66. [DOI] [PubMed] [Google Scholar]
- 25.Osman R, L’Allier PL, Elgharib N, Tardif JC. Critical appraisal of C-reactive protein throughout the spectrum of cardiovascular disease. Vasc Health Risk Manag. 2006;2:221–37. doi: 10.2147/vhrm.2006.2.3.221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gegenava T, Gegenava M, Kavtaradze G. C-reactive protein level correlation with depression and anxiety among patients with coronary artery disease. Georgian Med News. 2011:34–7. [PubMed] [Google Scholar]
- 27.Dogan E, Erkoc R, Eryonucu B, Sayarlioglu H, Agargun MY. Relation between depression, some laboratory parameters, and quality of life in hemodialysis patients. Ren Fail. 2005;27:695–9. doi: 10.1080/08860220500242728. [DOI] [PubMed] [Google Scholar]
- 28.Preljevic VT, Osthus TB, Sandvik L, Bringager CB, Opjordsmoen S, Nordhus IH, et al. Psychiatric disorders, body mass index and C-reactive protein in dialysis patients. Gen Hosp Psychiatry. 2011;33:454–61. doi: 10.1016/j.genhosppsych.2011.06.010. [DOI] [PubMed] [Google Scholar]
- 29.Menzies V, Lyon DE, Elswick RK, Jr, Montpetit AJ, McCain NL. Psychoneuroimmunological relationships in women with fibromyalgia. Biol Res Nurs. 2013;15:219–25. doi: 10.1177/1099800411424204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Einvik G, Hrubos-Strom H, Randby A, Nordhus IH, Somers VK, Omland T, et al. Major depressive disorder, anxiety disorders, and cardiac biomarkers in subjects at high risk of obstructive sleep apnea. Psychosom Med. 2011;73:378–84. doi: 10.1097/PSY.0b013e318219e64e. [DOI] [PubMed] [Google Scholar]
- 31.Hiles SA, Baker AL, de Malmanche T, Attia J. Interleukin-6, C-reactive protein and interleukin-10 after antidepressant treatment in people with depression: A meta-analysis. Psychol Med. 2012;42:2015–26. doi: 10.1017/S0033291712000128. [DOI] [PubMed] [Google Scholar]
- 32.Liukkonen T, Rasanen P, Jokelainen J, Leinonen M, Järvelin MR, Meyer-Rochow VB, et al. The association between anxiety and C-reactive protein (CRP) levels: Results from the Northern Finland 1966 birth cohort study. Eur Psychiatry. 2011;26:363–9. doi: 10.1016/j.eurpsy.2011.02.001. [DOI] [PubMed] [Google Scholar]
- 33.Pizzi C, Manzoli L, Mancini S, Costa GM. Analysis of potential predictors of depression among coronary heart disease risk factors including heart rate variability, markers of inflammation, and endothelial function. Eur Heart J. 2008;29:1110–7. doi: 10.1093/eurheartj/ehn137. [DOI] [PubMed] [Google Scholar]
- 34.Al-Maskari M, Al-Shukaili A, Al-Mammari A. Pro-inflammatory cytokines in Omani type 2 diabetic patients presenting anxiety and depression. Iran J Immunol. 2010;7:124–9. [PubMed] [Google Scholar]
- 35.Zhang JM, Ma WL, Xu Y, Li MJ, Zhao MZ, Xing Y, et al. The relation between post-acute coronary syndrome anxiety and serum levels of inflammatory factors. Zhonghua Nei Ke Za Zhi. 2007;46:1022–4. [PubMed] [Google Scholar]
- 36.Orre IJ, Reinertsen KV, Aukrust P, Dahl AA, Fossa SD, Ueland T, et al. Higher levels of fatigue are associated with higher CRP levels in disease-free breast cancer survivors. J Psychosom Res. 2011;71:136–41. doi: 10.1016/j.jpsychores.2011.04.003. [DOI] [PubMed] [Google Scholar]
- 37.O’Donovan A, Hughes BM, Slavich GM, Lynch L, Cronin MT, O’Farrelly C, et al. Clinical anxiety, cortisol and interleukin-6: Evidence for specificity in emotion-biology relationships. Brain Behav Immun. 2010;24:1074–7. doi: 10.1016/j.bbi.2010.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bjerkeset O, Romild U, Smith GD, Hveem K. The associations of high levels of C-reactive protein with depression and myocardial infarction in 9258 women and men from the HUNT population study. Psychol Med. 2011;41:345–52. doi: 10.1017/S0033291710000887. [DOI] [PubMed] [Google Scholar]
- 39.Duivis HE, de Jonge P, Penninx BW, Na BY, Cohen BE, Whooley MA. Depressive symptoms, health behaviors, and subsequent inflammation in patients with coronary heart disease: Prospective findings from the heart and soul study. Am J Psychiatry. 2011;168:913–20. doi: 10.1176/appi.ajp.2011.10081163. [DOI] [PubMed] [Google Scholar]
- 40.Narita K, Murata T, Hamada T, Takahashi T, Omori M, Suganuma N, et al. Interactions among higher trait anxiety, sympathetic activity, and endothelial function in the elderly. J Psychiatr Res. 2007;41:418–27. doi: 10.1016/j.jpsychires.2006.01.003. [DOI] [PubMed] [Google Scholar]


