Abstract
Purpose
There is literature indicating cognitive ability and depression are related, but few studies have examined the direction of the relationship. This study examined the relationship between depression levels and cognitive abilities from adolescence to early adulthood.
Methods
Using the National Longitudinal Study of Adolescent Health, (n=14,322), this study used path modeling to investigate the relationship between depression and cognitive ability at baseline and again 8 years later.
Results
After controlling for initial levels of depression, cognitive ability, and other covariates, depressive symptoms in adolescence are related to cognitive ability in early adulthood, but adolescent cognitive ability is not related to adult depression levels. Moreover, after controlling for adolescent levels of depression and cognitive ability, the cognitive ability-depression relationship disappears in adulthood.
Conclusions
The cognitive ability-depression relationship appears early in life, and it is likely that the presence of depressive symptoms leads to lower cognitive ability. Thus, intervening at early signs of depression not only can help alleviate depression, but will likely have an effect of cognitive ability as well.
Introduction
Over the past two decades, many studies have been published examining the relationship between cognitive ability and a variety of health outcomes, including both physical and mental health [e.g., 1,2–4]. Most of these types of studies have shown that having lower cognitive ability measured is a strong predictor of multiple psychiatric disorders, including depression [e.g., 5,6,7], or one of its manifestations (e.g., suicide completion. [8,9], suicidal thoughts [10,11]).
This relationship between cognitive ability and depression appears to manifest itself throughout the life cycle, including childhood [12], adulthood [13], or in the elderly[14,9]. More than just a predictor, though, many studies have shown that cognitive ability measured at one time point is related to depression at a later time point [15,16,6,17] indicating that cognitive ability might play a causative role in depression. As depression is problem that many individuals encounter in their life, including adults and children across the age spectrum [18,19], and one with serious potential sequelae [20,21], finding potential risk or causal factors, especially in children and adolescents, could be of much benefit in helping individuals obtain the treatment they need [22].
Problems with Previous Studies
There are two major problems with previous studies that have examined the depression-cognitive ability relationship. One problem is that many of the studies have used either use a cross-sectional design, measuring both cognitive ability and depression concurrently, or a longitudinal design, measuring one variable at one time point and another variable at a later time point. As neither design controls for previous level cognitive ability or depression, they are not able to examine if one variable has a causal connection to the other [23,24].
The second problem with previous studies is that most of them focus on a clinical diagnosis of depression, often marked by severe change in life such as hospitalization or suicide attempt. This metric for depression is faulty for at least two reasons. First, it only captures those at the extreme end of the depressive spectrum and fails to take into account that depression falls onto a continuum [25]. Moreover, this metric only can capture those who are willing (or have friends/family who are willing) and have the means to obtain professional help.
Due in part to their design, most previous studies have not been able to determine if lower cognitive ability puts one at a higher risk for having depressive symptoms, if having depressive symptoms might put one at a higher risk for having lower cognitive ability, or if there might be a third variable that causing the relationship between the variables. Answering the “which comes first” question can be difficult, as it is impossible to assign people to depression/non-depression groups randomly, nor it is possible to assign people certain levels of cognitive ability. Consequently, the answer to the question of if cognitive ability is causatively related to depression (or visa versa) will have be gained through an observational study [26]. While there are a range of different observational methods, one specific type of study that can help answer the cognitive ability-depression question is a longitudinal design where cognitive ability and depression are measured at multiple time points and different potential causal pathways are statistically modeled [27]. The purpose of this current study is to examine the depression-cognitive ability relationship, specifically examining if there might be a causal relationship between the two variables.
Method
Sample
The sample for this study came from the National Longitudinal Study of Adolescent Health (Add Health [13]). Add Health was initiated in 1994, as has been collected in multiple waves, largely through the use of in-home questionnaires. It was designed to be the largest, most comprehensive survey of adolescents ever undertaken to study the health-related behaviors of adolescents and their outcomes in young adulthood. This study used Add Health participants who completed the in-home surveys during Wave I (1994–1995) and Wave III (2001–2002), for a total of 14,322 participants. While there was some attrition between the data collection waves, using the appropriate Add Health sampling weights, which accounts for the attrition, produces unbiased parameter estimates [28]. Demographic information about the sample is given in Table 1.
Table 1.
Descriptive Statistics
| Variable | Mean | Standard Deviation | Range |
|---|---|---|---|
| Age Wave I (years) | 15.98 | 1.42 | 11.42–21.38 |
| Age Wave III (years) | 22.35 | 1.42 | 17.86–28.05 |
| AHPVT Wave I | 100.61 | 14.61 | 10–141 |
| AHPVT Wave III | 102.22 | 13.20 | 11–123 |
| Male | 50.22% | ||
| Race | |||
| Caucasian | 76.31% | ||
| African American | 16.74% | ||
| American Indian | 2.57% | ||
| Asian/Pacific Islander | 4.22% | ||
| Biracial | 0.05% | ||
| Hispanic Origin | 11.83% | ||
Note. All statistics are weighted. AHPVT: Add Health Picture Vocabulary Test. The AHPVT was scaled to have a mean of 100 and standard deviation of 15.
Variables
Cognitive Ability
The measure of cognitive ability used in this study is the Add Health Picture Vocabulary Test (AHPVT), an abridged version of the revised Peabody Picture Vocabulary Test [PPVT-R; 29]. The AHPVT contains half the items from the original PPVT-R and uses the same illustrations, thus there is a strong correlation (.96) between scores on the two instruments. Vocabulary tests are often used as a measure of cognitive ability in health research [30], as vocabulary is consistently found to be one of the strongest measures of overall cognitive ability [31–33]. Moreover, some even advocate its usage over other measures when using a sample of highly diverse individuals [34], and, because measures like the AHPVT require no comprehensive reading skills, it is particularly appropriate for measuring cognitive abilities of people at the lower end of the ability spectrum.
Depression
Wave I and III of the Add Health study does not measure depression directly, but many of the items in the In-Home surveys ask about symptoms commensurate with a clinical diagnosis of depression [35] and other instruments designed to measure depressive symptoms [e.g., 36]. Consequently, this study formed depression questionnaires for Wave I and Wave III by taking all the items related to depression within each wave and factor analyzing them to develop a single-construct measure of depression [37]. Because the items the In-Home surveys asked in Waves I and III were not the exact same, the questionnaires for the two waves are not identical; however, there was considerable overlap between the instruments (six items), which allowed the scores from both instruments to be equated [38]. The item stems, factor pattern coefficients, and reliability coefficients for the depression instruments’ scores are given in Table 2.
Table 2.
Psychometric Analyses for Depression Instruments
| Variable Name | Wave | Item Stem | Pattern Coefficient | Standard Error |
|---|---|---|---|---|
| H1FS1 | 1 | In the past 7 days, how often were you bothered by things that usually don’t bother you? | 0.65 | 0.02 |
| H1FS2 | 1 | In the past 7 days, how often did you not feel like eating/poor appetite? | 0.50 | 0.02 |
| H1FS3 | 1 | In the past 7 days, how often could you not shake off the blues, even with help from your family and your friends? | 0.80 | 0.01 |
| H1FS5 | 1 | In the past 7 days, how often did you have trouble keeping your mind on what you were doing? | 0.58 | 0.02 |
| H1FS6 | 1 | In the past 7 days, how often were you depressed? | 0.86 | 0.01 |
| H1FS9 | 1 | In the past 7 days, how often did you feel your life had been a failure? | 0.76 | 0.02 |
| H1FS10 | 1 | In the past 7 days, how often did you feel fearful? | 0.60 | 0.02 |
| H1FS13 | 1 | In the past 7 days, how often were you lonely? | 0.75 | 0.01 |
| H1FS16 | 1 | In the past 7 days, how often were you sad? | 0.81 | 0.01 |
| H1FS17 | 1 | In the past 7 days, how often did you feel people disliked you? | 0.60 | 0.02 |
| H1FS19 | 1 | In the past 7 days, how often did you feel your life was not worth living? | 0.76 | 0.02 |
| H3SP2 | 3 | In the past 12 months, how often have you cried a lot? | 0.47 | 0.02 |
| H3SP5 | 3 | In the past 7 days, how often were you bothered by things that usually don’t bother you? | 0.68 | 0.02 |
| H3SP6 | 3 | In the past 7 days, how often could you not shake off the blues, even with help from your family and your friends? | 0.83 | 0.01 |
| H3SP8 | 3 | In the past 7 days, how often did you have trouble keeping your mind on what you were doing? | 0.60 | 0.02 |
| H3SP9 | 3 | In the past 7 days, how often were you depressed? | 0.93 | 0.01 |
| H3SP10 | 3 | In the past 7 days, how often were you too tired to do things? | 0.48 | 0.02 |
| H3SP11 | 3 | In the past 7 days, how often did you enjoy life? | 0.63 | 0.02 |
| H3SP12 | 3 | In the past 7 days, how often were you sad? | 0.84 | 0.01 |
| H3SP13 | 3 | In the past 7 days, how often did you feel people disliked you? | 0.56 | 0.02 |
Note. The correlation between the latent depression scores from Waves I and III was .41. The model fit statistics were: χ2(df=169): 1309.74, Comparative fit index: 0.98, Tucker Lewis index: .98, Root Mean Square Error of Approximation: .02. Reliability estimates were .92 (omega) and .91 (alpha) for Wave I and .89 (omega) and .87 (alpha) for Wave III. Reliability estimates were obtained using non-weighted polychoric correlations [72].
To make sure the instruments were measuring the same construct over time, we tested for measurement invariance of the six items that overlapped both waves’ data [39,40]. Assessing for invariance is a multi-step procedure that examines if items are working the same across different groups[41]. While the groups are often defined by demographic variables, they can also be defined by time (e.g., comparing item performance at Wave I versus Wave III [42]), although when the groups are defined by time the residual variances of the same variables are often modeled to covary [43].
Traditionally, tests of invariance used the change in χ2 values (Δ χ2). If the Δ χ2 values does not “significantly” change as the models grow more restrictive (i.e., more invariance constraints are added), this is taken to indicate that the more restrictive model fits the data as well as the less restrictive model. Thus, the more restrictive (i.e., more parsimonious) model is favored over the less restrictive one. The use of Δ χ2 values has been criticized because of its sensitivity to sample size [44]. Thus, many researchers [45,46] currently suggest using a more practical perspective when examine invariance. Specifically, that the multigroup factor model exhibits an adequate fit to the data and the change in alternative fit indices values from the less restrictive to the more restrictive model is negligible. Cheung and Rensvold [44] and Meade, Johnson, and Braddy [47] have argued that the Comparative Fit Index (CFI) and McDonald’s [48] Noncentrality Index (Mc) are more robust indices to use than the χ2 when examining invariance.
To test invariance, we used three models. First, we fit a baseline model allowing the latent variables and residuals across the six identical items to covary across time, but imposing no parameter constraints. Second, we constrained the six overlapping items to have the same pattern coefficient across time, but allowed the variance of the depression factor at Wave III to be free. Third, we constrained the six identical items’ thresholds to be the same across time, but allowed the mean of the depression factor at Wave III to be free. If the third model fits the data as well as models one and two, this would indicate that that the latent variables are comparable [41]. In all three models, we allowed the residual variances of the same variables across time points to covary.
Covariates
The respondents’ sex and self-reported race and ethnicity were used as covariates. Because the AHPVT used English vocabulary words, we used English language fluency (i.e., if English was the primary language to speak with his/her family or friends) as a covariate. In addition, we used the highest education obtained by the residential parent(s) as a proxy for SES, and used it as a predictor of depression and cognitive ability at both data collection waves.
Data Inspection
There were missing data on all variables except for the participant’s sex. As there were no distinguishable patterns in the missing data, and each variable had responses from at least 99% of sample, it is likely that the data are missing at random or completely at random [49].
Determining Model Fit
When comparing statistical models, one needs to have criteria upon which to evaluate them [50]. For overall model fit, we used (a) the root mean square error of approximation (RMSEA), (b) the comparative fit index (CFI), (c) Akaike’s information criterion (AIC), and (d) McDonald’s [51] noncentrality index (Mc). These indices were chosen as they represent a variety of fit criteria and they tend to perform well in evaluating different models [52]. To test the change-in-fit between nested models for invariance, we used the change in CFI and Mc values (Δ CFI and Δ Mc, respectively).
For this study’s criteria of overall model-data fit, we used the following: (a) RMSEA ≤ 0.08 [53,54]; (b) CFI ≥ 0.96 [55]; and (c) Mc ≥ 0.90 [56,57]. AIC values do not indicate how well a model (absolutely) fits the data; rather, they are used in a relative fashion. Models with lower AIC values indicate a better fit than models with higher values, after penalizing each model for its complexity (i.e., number of parameter estimates). While information-based fit measures are typically used with maximum likelihood estimation, the AIC can be estimated using least squares via AIC = χ2 + 2K, where K is the total number of estimated parameters [58].
Cheung and Rensvold [44] and Meade et al. [47] differ on the amount of change needed in the CFI and Mc fit indices to reject invariance, but both would agree than a Δ CFI > 0.01 and a Δ Mc difference > 0.02 in the NCI would indicate a rejection of invariance.
Parameter Estimation
All data analysis was done using Mplus [59], using its robust weighted least squares estimator, which works well with large sample sizes and non-normal data [60].
Consequently, the missing data were handled using Mplus’ 4-step estimation, which is similar to Full Information Maximum Likelihood estimation, in that it uses all the information from the respondents instead of removing those with missing data [61]. The exception is for those individuals missing data on one of the covariates (n=999), which Mplus excluded listwise when using the robust weighted least squares estimator.
Results
Invariance in the Depression Measure
The results from the invariance analysis are given in Table 3. Using the Δ CFI and Δ Mc criteria, it appears as if the overlapping items are essentially acting identically at both waves of data collection. That is, the models that impose constraints on the loadings (I2) and thresholds (I3) do not fit the data any worse than the baseline model that allows the parameters to be freely estimated. Thus, the two depression measures can be considered to be measuring the same construct. Consequently, this analysis used the latent variable formed from the items at each wave as the measure of depression. The odds of having a clinical diagnosis of depression at one standard deviation above the mean on this depression scale versus having a score one standard deviation below the mean is 2.88 for the Wave I measure and 5.38 for the Wave III measure, indicating that the items forming this scale are measuring depression.
Table 3.
Invariance Assessment of Depression Instrument for Overlapping Items
| Model | Model Description | χ2 | df | Δ χ2 | p | CFI | Δ CFI | RMSEA | Mc | Δ Mc |
|---|---|---|---|---|---|---|---|---|---|---|
| I1 | Baseline | 1202.98 | 163 | -- | 0.985 | 0.02 | 0.964 | -- | ||
| I2 | Constrained Factor Structure Coefficients (but free Factor Variance at Wave III) | 1210.08 | 169 | 27.77 | < 0.00 | 0.985 | 0.000 | 0.02 | 0.966 | −0.001 |
| I3 | Constrain Thresholds (but free Factor Mean at Wave III) | 1710.64 | 187 | 530.69 | <0.00 | 0.981 | 0.004 | 0.02 | 0.957 | 0.009 |
Depression and Cognitive Ability Relationship
First, we obtained the correlations between the cognitive ability and depression variables at both waves (results are given in Table 4). As expected, there is a negative relationship between cognitive ability and depression in both data waves. Moreover, there were strong, positive relationships between cognitive ability scores (.69) at Wave I and Wave III and depression scores (.41) across these two waves, this showing the stability of the constructs.
Table 4.
Zero-Order Correlations among Depression and Cognitive Ability Variables
| Cognitive Ability Wave I | Cognitive Ability Wave III | Depression Wave I | |
|---|---|---|---|
| Cognitive Ability Wave III | 0.69 | ||
| Depression Wave I | −0.20 | −0.17 | |
| Depression Wave III | −.011 | −0.12 | 0.40 |
Note. Correlations are model-based estimates.
To test the structural pathways, we initially posited a cross-lagged model where cognitive ability and depression at Wave I predicted cognitive ability and depression at Wave III (Model 1a in Table 5). We subsequently fit two alternative models. First, we constrained the cross-lagged paths in Model 1a to be equal to each other (Model 1b). Second, we removed the paths from Model 1a with weak relationships. (i.e., estimate-to-standard-error ratios < 3), which resulted in removing the direct path from IQ at Wave I to Depression at Wave III (Model 1c). The most parsimonious model (1c) appeared to fit the data no worse than the more complex models (with the AIC indicating it better than the more complex models). The path model (with coefficient values) is shown in Figure 1. The results indicate that after controlling for Wave I scores, cognitive ability at Wave I does not directly relate to depression at Wave III, but depression at Wave I does directly relate to cognitive ability at Wave III, although the relationship is relatively small.
Table 5.
Fit of Different Models Testing the Cognitive Ability and Depression Relationship
| Model | Description | χ2 | df | RMSEA | CFI | Mc | AIC |
|
|
||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1a | Full cross-lagged model without covariates | 1486.30 | 199 | 0.02 | 0.98 | 0.96 | 1680 | 0.48 | 0.16 | ||
| 1b | Model 1a, but cross lagged paths are constrained to be equal | 1491.04 | 200 | 0.02 | 0.98 | 0.96 | 1683 | 0.49 | 0.16 | ||
| 1c | Model 1a, constraining the coefficients for weak relationships to zero | 1465.38 | 200 | 0.02 | 0.98 | 0.96 | 1653 | 0.48 | 0.17 | ||
| 2a | Model 1a with all covariates | 1444.03 | 343 | 0.02 | 0.98 | 0.96 | 1658 | 0.46 | 0.15 | ||
| 2b | Model 1c with all covariates | 1436.81 | 344 | 0.02 | 0.98 | 0.96 | 1649 | 0.46 | 0.15 | ||
| 2c | Model 2b constraining the coefficients for weak relationships to zero | 1430.82 | 345 | 0.02 | 0.98 | 0.96 | 1641 | 0.46 | 0.15 |
Note. CFI: comparative fit index; TLI: Tucker Lewis index; RMSEA: Root mean square error of approximation; Mc; AIC: Akaike information criterion.
Figure 1.
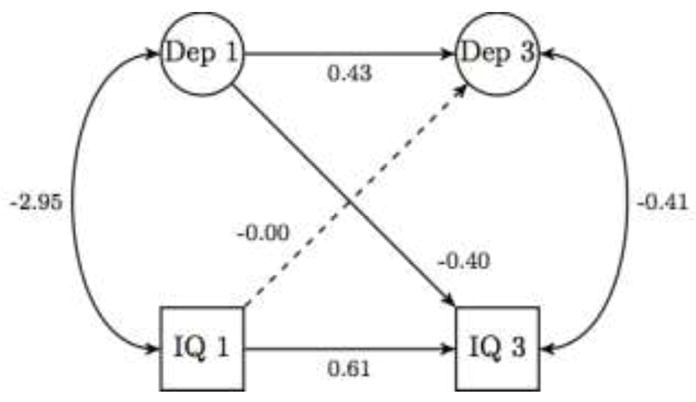
Path Model without Covariates with Unstandardized Coefficients.
Next, we added the covariates to Models 1a and 1c (Models 2a and 2b, respectively, in Table 5). As with Model 1, after controlling for Wave I scores, cognitive ability at Wave I does not directly relate to depression at Wave III, but depression at Wave I does directly relate to cognitive ability at Wave III, although the relationship is still relatively small. There appeared to be a weak relationship between parent education level and the depression score at Wave III, so we removed it and refit the model (Model 2c). This final model appeared to fit the data as well or better than model 2a or 2b. The full model with covariates is shown in Figure 2, with the weak relationships shown using a dashed line. The coefficients associated with model 2c are given in Table 6. Even after controlling for the covariates, depression at Wave I directly relates to cognitive ability at Wave III, albeit with a relatively weak magnitude. Moreover, while parental education does directly relate to cognitive ability at Wave I and III and depression at Wave I, it is not directly related to depression at Wave III.
Figure 2.
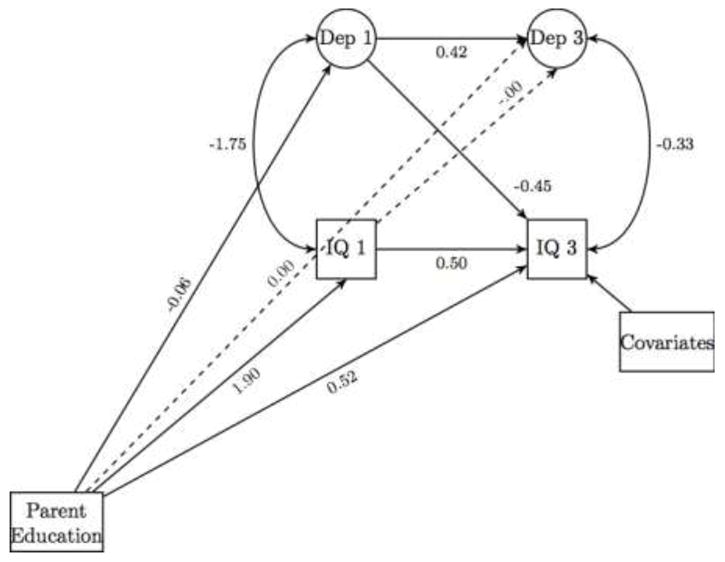
Final Path Model with Covariates with Unstandardized Coefficients.
Table 6.
Unstandardized Coefficients for Model 2c
| From | To | B | SE | B* |
|---|---|---|---|---|
| Depression (Wave I) | Depression (Wave III) | 0.42 | 0.02 | 0.39 |
| Highest Parent Education | Depression (Wave I) | −0.06 | 0.01 | −0.14 |
| Depression (Wave I) | Cognitive Ability (Wave III) | −0.43 | 0.12 | −0.03 |
| Cognitive Ability (Wave I) | Cognitive Ability (Wave III) | 0.5 | 0.01 | 0.53 |
| Highest Parent Education | Cognitive Ability (Wave III) | 0.52 | 0.07 | 0.1 |
| English Fluency | Cognitive Ability (Wave III) | 7.87 | 0.63 | 0.09 |
| Hispanic1 | Cognitive Ability (Wave III) | −2 | 0.52 | −0.05 |
| African American2 | Cognitive Ability (Wave III) | −7.35 | 0.46 | −0.28 |
| American Indian2 | Cognitive Ability (Wave III) | −3.18 | 0.99 | −0.04 |
| Asian2 | Cognitive Ability (Wave III) | −1.10 | 0.79 | −0.02 |
| Other2 | Cognitive Ability (Wave III) | 4.14 | 3.91 | 0.01 |
| Highest Parent Education | Cognitive Ability (Wave I) | 1.90 | 0.12 | 0.33 |
| Depression (Wave I)3 | Cognitive Ability (Wave I) | −1.79 | 0.16 | −0.14 |
| Depression (Wave III)3 | Cognitive Ability (Wave III) | −0.42 | 0.16 | −0.04 |
Note. B: unstandardized path coefficient. SE: Standard error. B*: Standardized path coefficient.
Hispanic origin was coded as a separate variable than race.
The race variable was coded using weighted effects with White being the reference group.
No causal directionality was specified, so this is a covariance estimate.
Discussion
This study investigated the relationship between depression and cognitive ability. While many previous studies have been able to show that the two constructs are related to each other, there has been no answer to the question of if there is a causal relationship. To help answer that question, this study used data from the National Longitudinal Study of Adolescent Health [Add Health; 62], examining cognitive ability and depression at Wave I and Wave III (approximately 8 years apart).
As with most other studies examining cognitive ability and depression, this study found that cognitive ability and depression were negatively related to each other at both Wave I and Wave III. Moreover, depression at Wave I was related to depression at Wave III, and likewise for cognitive ability, which shows the stability of both constructs through a very tumultuous time in development [63]. When looking specifically at the cognitive ability-depression relationships, we found that depression and cognitive ability at Wave I were related to cognitive ability and depression, respectively, at Wave III. When modeling a relationship between the Wave I and Wave III variables, we found that depression at Wave I had a small, negative relationship with cognitive ability at Wave III, but cognitive ability at Wave I did not have a relationship with depression at Wave III that was statistically different than zero. Moreover, after controlling for depression and cognitive ability at Wave I, the relationship between depression and cognitive ability at Wave III was not statistically different than zero. This relationship pattern held even after controlling for parental education, and the respondents’ sex, race, and English language proficiency.
The results from this study are important for multiple reasons. First, it confirmed the stability of depression and cognitive ability during adolescence and young adulthood, a very tumultuous time of development. Second, it went beyond showing that cognitive ability and depression were related to each other to showing that depression levels in adolescence possibly have a causal relationship to cognitive ability levels in early adulthood. The direction of the effects align themselves with other studies that have shown depression to have an effect on various aspects of cognitive ability [64,65,16], and some going so far as to state that the effect of depression of cognition is similar to having moderately severe traumatic brain injury [66].
Third, and perhaps the most interesting finding, this study showed that after controlling for early measures of cognitive ability and depression in adolescence, the depression-cognitive ability relationship in early adulthood disappeared. Likely, this indicates that the relationship that depression and cognitive ability have on each other develops in childhood/adolescence, but does not necessarily grow as adolescents move into adulthood. There are likely multiple reasons for this effect, but one probable agent is parental influence. As parental education was related to both depressive symptoms and cognitive ability at Wave I, but only slightly related to cognitive ability at Wave III, this could be an indication that parental influence, at least for these constructs, is most potent when the children are at the age where they are living with them. As the respondents move into adulthood, genetic [67], and other influences [68] become more important, while the effects of parents’ ability begins to wan [69].
Limitations
There were a few limitations with the study. First, the time between Wave I and Wave III measures was approximately eight years. While these eight years span one of the most tumultuous time periods in development, perhaps a longer time span would show a relationships of different magnitudes. Second, while measure of depression used in this study had sound psychometric properties, it was developed from items in the Add Health In-Home questionnaire and not a standardized measure of depressive symptoms. While the items used were typical of depression questionnaires, more validity evidence should be gathered on it. Third, this study did not examine possible moderating events (e.g., social support, school or family problems) that may affect the risk of depression. Future studies should examine if the depression-cognitive ability relationship is moderated by such environmental factors.
Clinical Implications
This results from this study show the importance of addressing depressive symptoms during childhood/adolescence. Depressive symptoms are occurring in childhood and adolescence more frequently now than before [70], and the results from this study indicate that this time in development is likely when depressive symptoms become associated with cognitive ability. Thus, while early intervention is important to treating depression [71], such intervention could likely have a positive influence on later cognitive ability, as well.
Acknowledgments
First and Second Author were supported by Award Number XXXXXXXX from the Eunice Kennedy Shriver National Institute Of Child Health & Human Development. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Eunice Kennedy Shriver National Institute Of Child Health & Human Development or the National Institutes of Health.
This research uses data from Add Health, a program project designed by J. Richard Udry, Peter S. Bearman, and Kathleen Mullan Harris, and funded by a grant P01-HD31921 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, with cooperative funding from 17 other agencies. Special acknowledgment is due Ronald R. Rindfuss and Barbara Entwisle for assistance in the original design. Persons interested in obtaining data files from Add Health should contact Add Health, Carolina Population Center, 123 W. Franklin Street, Chapel Hill, NC 27516-2524 (addhealth@unc.edu). No direct support was received from grant P01-HD31921 for this analysis.
Footnotes
The authors declare they have no conflict of interest.
References
- 1.Deary IJ, Weiss A, Batty GD. Intelligence and personality as predictors of illness and death. Psychological Science in the Public Interest. 2010;11(2):53–79. doi: 10.1177/1529100610387081. [DOI] [PubMed] [Google Scholar]
- 2.Emerson E, Einfeld S, Stancliffe R. The mental health of young children with intellectual disabilities or borderline intellectual functioning. Social Psychiatry Psychiatric Epidemiology. 2010;45(5):579–587. doi: 10.1007/s00127-009-0100-y. [DOI] [PubMed] [Google Scholar]
- 3.Chong S, Subramaniam M, Lee IM, Pek E, Cheok C, Verma S, Wong J. Academic attainment: a predictor of psychiatric disorders? Social Psychiatry Psychiatric Epidemiology. 2009;44(11):999–1004. doi: 10.1007/s00127-009-0027-3. [DOI] [PubMed] [Google Scholar]
- 4.Jansson J-Å, Eklund M. How the inner world is reflected in relation to perceived ward atmosphere among patients with psychosis. Social Psychiatry and Psychiatriac Epidemiology. 2002;37(11):519–526. doi: 10.1007/s00127-002-0584-1. [DOI] [PubMed] [Google Scholar]
- 5.Der G, Batty GD, Deary IJ. The association between IQ in adolescence and a range of health outcomes at 40 in the 1979 US National Longitudinal Study of Youth. Intelligence. 2009;37(6):573–580. doi: 10.1016/j.intell.2008.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Koenen KC, Moffitt TE, Roberts AL, Martin LT, Kubzansky L, Harrington H, Poulton R, Caspi A. Childhood IQ and adult mental disorders: A test of the cognitive reserve hypothesis. American Journal of Psychiatry. 2009;166:50–57. doi: 10.1176/appi.ajp.2008.08030343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Upmark M, Lundberg I, Sadigh J, Allebeck P, Bigert C. Psychosocial characteristics in young men as predictors of early disability pension with a psychiatric diagnosis. Social psychiatry and psychiatric epidemiology. 1999;34(10):533–540. doi: 10.1007/s001270050172. [DOI] [PubMed] [Google Scholar]
- 8.Fergusson DM, Horwood LJ, Ridder EM. Show me the child at seven II: childhood intelligence and later outcomes in adolescence and young adulthood. Journal of Child Psychology and Psychiatry. 2005;46(8):850–858. doi: 10.1111/j.1469-7610.2005.01472.x. [DOI] [PubMed] [Google Scholar]
- 9.Kunik ME, Champagne L, Harper RG, Chacko RC. Cognitive functioning in elderly depressed patients with and without psychosis. International Journal of Geriatric Psychiatry. 1994;9(11):871–874. doi: 10.1002/gps.930091103. [DOI] [Google Scholar]
- 10.Andersson L, Allebeck P, Gustafsson JE, Gunnell D. Association of IQ scores and school achievement with suicide in a 40-year follow-up of a Swedish cohort. Acta Psychiatrica Scandinavica. 2008;118(2):99–105. doi: 10.1111/j.1600-0447.2008.01171.x. [DOI] [PubMed] [Google Scholar]
- 11.Gunnell D, Harbord R, Singleton N, Jenkins R, Lewis G. Is low IQ associated with an increased risk of developing suicidal thoughts? Social psychiatry and psychiatric epidemiology. 2009;44(1):34–38. doi: 10.1007/s00127-008-0404-3. [DOI] [PubMed] [Google Scholar]
- 12.Horowitz JL, Garber J. Relation of intelligence and religiosity to depressive disorders in offspring of depressed and nondepressed mothers. Journal of the American Academy of Child and Adolescent Psychiatry. 2003;42(5):578–586. doi: 10.1097/01.chi.0000046831.09750.03. [DOI] [PubMed] [Google Scholar]
- 13.Bain GH, Lemmon H, Teunisse S, Starr JM, Fox HC, Deary IJ, Whalley LJ. Quality of life in healthy old age: relationships with childhood IQ, minor psychological symptoms and optimism. Social Psychiatry and Psychiatriac Epidemiology. 2003;38(11):632–636-636. doi: 10.1007/s00127-003-0685-5. [DOI] [PubMed] [Google Scholar]
- 14.Chi I, Chou KL. Depression predicts cognitive decline in Hong Kong Chinese older adults. Aging & Mental Health. 2000;4(2):148–157. doi: 10.1080/13607860050008673. [DOI] [Google Scholar]
- 15.David AS, Zammit S, Lewis G, Dalman C, Allebeck P. Impairments in cognition across the spectrum of psychiatric disorders: Evidence from a Swedish conscript cohort. Schizophrenia Bulletin. 2008;34(6):1035–1041. doi: 10.1093/schbul/sbn028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hammars?rdal G. Cognitive functioning in major depression - A summary. Frontiers in Human Neuroscience. 2009:3. doi: 10.3389/neuro.09.026.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zammit S, Allebeck P, David AS, Dalman C, Hemmingsson T, Lundberg I, Lewis G. A longitudinal study of premorbid IQ score and risk of developing schizophrenia, bipolar disorder, severe depression, and other nonaffective psychoses. Archives of general psychiatry. 2004;61(4):354–360. doi: 10.1001/archpsyc.61.4.354. [DOI] [PubMed] [Google Scholar]
- 18.Furniss T, Beyer T, Guggenmos J. Prevalence of behavioural and emotional problems among six-years-old preschool children. Social Psychiatry and Psychiatriac Epidemiology. 2006;41(5):394–399. doi: 10.1007/s00127-006-0045-3. [DOI] [PubMed] [Google Scholar]
- 19.Haarasilta L, Marttunen M, Kaprio J, Aro H. Major depressive episode and health care use among adolescents and young adults. Social Psychiatry and Psychiatriac Epidemiology. 2003;38(7):366–372. doi: 10.1007/s00127-003-0644-1. [DOI] [PubMed] [Google Scholar]
- 20.Mattila V, Pelkonen M, Henriksson M, Marttunen M. Injury risk in young psychiatric outpatients. Social Psychiatry and Psychiatriac Epidemiology. 2008;43(8):627–634. doi: 10.1007/s00127-008-0343-z. [DOI] [PubMed] [Google Scholar]
- 21.Thompson A. Younger onset of depression is associated with greater suicidal intent. Social Psychiatry and Psychiatriac Epidemiology. 2008;43(7):538–544. doi: 10.1007/s00127-008-0329-x. [DOI] [PubMed] [Google Scholar]
- 22.Duhoux A, Fournier L, Nguyen C, Roberge P, Beveridge R. Guideline concordance of treatment for depressive disorders in Canada. Social Psychiatry and Psychiatriac Epidemiology. 2009;44(5):385–392. doi: 10.1007/s00127-008-0444-8. [DOI] [PubMed] [Google Scholar]
- 23.Willett JB, Singer JD, Martin NC. The design and analysis of longitudinal studies of development and psychopathology in context: Statistical models and methodological recommendations. Development and Psychopathology. 1998;10 (02):395–426. doi: 10.1017/s0954579498001667. [DOI] [PubMed] [Google Scholar]
- 24.Murnane RJ, Willett JB. Methods matter: Improving causal inference in educational and social science research. Oxford University Press; New York, NY: 2011. [Google Scholar]
- 25.Angst J, Merikangas K. The depressive spectrum: Diagnostic classification and course. Journal of Affective Disorders. 1997;45(1–2):31–40. doi: 10.1016/s0165-0327(97)00057-8. [DOI] [PubMed] [Google Scholar]
- 26.Rosenbaum PR. Observational study. In: Everitt BS, Howell DC, editors. Encyclopedia of Statistics in Behavioral Science. Vol. 3. Wiley; Chichester, West Sussex, UK: 2005. pp. 1451–1462. [Google Scholar]
- 27.Shadish WR, Cook TD, Campbell DT. Experimental and quasi-experimental designs for generalized causal inference. Houghton Mifflin; Boston: 2002. vol Book, Whole. [Google Scholar]
- 28.Chantala K, Kalsbeek WD, Andraca E. Non-response in Wave III of the Add Health study. 2004. [Google Scholar]
- 29.Dunn LM, Dunn LM. Peabody picture vocabulary test. American Guidance Service; Circle Pines, MN: 1981. [Google Scholar]
- 30.Gottfredson LS. Intelligence: Is It the Epidemiologists’ Elusive “Fundamental Cause” of Social Class Inequalities in Health? Journal of Personality and Social Psychology. 2004;86:174–199. doi: 10.1037/0022-3514.86.1.174. [DOI] [PubMed] [Google Scholar]
- 31.Jensen AR. The g factor: The science of mental ability. Praeger; Westport, CN: 1998. [Google Scholar]
- 32.Jensen AR. Vocabulary and general intelligence. Behavioral and Brain Science. 2001;24:1109–1110. doi: 10.1017/S0140525X01280133. [DOI] [PubMed] [Google Scholar]
- 33.Williams KT, Wang JJ. Technical reference to the Peabody Picture Vocabulary Test-Third Edition. American Guidance Service; Circle Pines, MN: 1997. [Google Scholar]
- 34.Manly JJ, Touradji P, Tang M-X, Stern Y. Literacy and memory decline among ethnically diverse elders. Journal of clinical and experimental neuropsychology. 2003;25(5):680– 690. doi: 10.1076/jcen.25.5.680.14579. [DOI] [PubMed] [Google Scholar]
- 35.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Author; Washington, D.C: 2000. Revised. [Google Scholar]
- 36.Beck AT, Steer RA, Brown GK. Beck depression inventory. The Psychological Corporation; San Antonio, TX: 1996. [Google Scholar]
- 37.Floyd FJ, Widaman KF. Factor analysis in the development and refinement of clinical assessment instruments. Psychological Assessment. 1995;7(3):286–299. doi: 10.1037/1040-3590.7.3.286. [DOI] [Google Scholar]
- 38.Kolen MJ, Brennan RL. Test equating, scaling, and linking: Methods and practices. 2. Springer-Verlag; New York: 2004. vol Book, Whole. [Google Scholar]
- 39.Teresi JA. Overview of quantitative measurement methods: Equivalence, invariance, and differential item functioning in health applications. Medical Care. 2006;44(11):S39–S49. doi: 10.1097/1001.mlr.0000245452.0000248613.0000245445. [DOI] [PubMed] [Google Scholar]
- 40.Vandenberg RJ, Lance CE. A review and synthesis of the measurement invariance literature: Suggestions, practices, and recommendations for organizational research. Organizational Research Methods. 2000;3(1):4–70. doi: 10.1177/109442810031002. [DOI] [Google Scholar]
- 41.Millsap RE. Statistical approaches to measurement invariance. Routledge; New York: 2011. [Google Scholar]
- 42.Bontempo DE, Hofer SM. Assessing factorial invariance in cross-sectional and longitudinal studies. In: Ong AD, van Dulmen M, editors. Handbook of methods in positive psychology. Oxford University Press; New York: 2007. pp. 153–175. [Google Scholar]
- 43.McArdle JJ. Latent variable modeling of differences and changes with longitudinal data. Annual Review of Psychology. 2009;60(1):577–605. doi: 10.1146/annurev.psych.60.110707.163612. [DOI] [PubMed] [Google Scholar]
- 44.Cheung GW, Rensvold RB. Evaluating goodness-of-fit indexes for testing measurement invariance. Structural Equation Modeling: A Multidisciplinary Journal. 2002;9(2):233– 255. doi: 10.1207/S15328007SEM0902_5. [DOI] [Google Scholar]
- 45.Little TD. Mean and covariance structures (MACS) analyses of cross-cultural data: Practical and theoretical issues. Multivariate Behavioral Research. 1997;32(1):53–76. doi: 10.1207/s15327906mbr3201_3. [DOI] [PubMed] [Google Scholar]
- 46.Byrne BM, Stewart SM. The MACS approach to testing for multigroup invariance of a second-order structure: A walk through the process. Structural Equation Modeling. 2006;13(2):287–321. doi: 10.1207/s15328007sem1302_7. [DOI] [Google Scholar]
- 47.Meade AW, Johnson EC, Braddy PW. Power and sensitivity of alternative fit indices in tests of measurement invariance. Journal of Applied Psychology. 2008;93(3):568–592. doi: 10.1037/0021-9010.93.3.568. [DOI] [PubMed] [Google Scholar]
- 48.McDonald RP. An index of goodness-of-fit based on noncentrality. Journal of Classification. 1989;6(1):97–103. doi: 10.1007/bf01908590. [DOI] [Google Scholar]
- 49.Little RJA, Rubin DB. Statistical analysis with missing data. 2. John Wiley; Hoboken, NJ: 2002. vol Book, Whole. [Google Scholar]
- 50.Hu L-T, Bentler PM. Evaluating model fit. In: Hoyle RH, editor. Structural equation modeling: Concepts, issues, and applications. Sage Publications Inc; Thousand Oaks, CA: 1995. pp. 76–99. [Google Scholar]
- 51.McDonald RP. An index of goodness-of-fit based on noncentrality. Journal of Classification. 1989;6:97–103. [Google Scholar]
- 52.Marsh HW, Hau K-T, Grayson D. Goodness of fit in structural equation models. In: Maydeu-Olivares A, McArdle JJ, editors. Contemporary psychometrics: A festschrift for Roderick P McDonald. Lawrence Erlbaum; Mahwah, NJ: 2005. pp. 275–340. [Google Scholar]
- 53.Browne MW, Cudeck R. Alternative ways of assessing model fit. In: Bollen KA, Long JS, editors. Testing structural equation models. Sage; Newbury Park, CA: 1993. pp. 136–162. [Google Scholar]
- 54.Hu L, Bentler PM. Cutoff criteria for fit indices in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- 55.Yu C-Y. Evaluating cutoff criteria of model fit indices for latent variable models with binary and continuous outcomes. 2002. [Google Scholar]
- 56.Marsh HW, Hau K-T, Wen Z. In search of golden rules: Comment on hypothesis testing approaches to setting cutoff values for fit indexes and dangers in overgeneralizing Hu and Bentler’s (1999) findings. Structural Equation Modeling. 2004;11(3):320–341. doi: 10.1207/s15328007sem1103_2. [DOI] [Google Scholar]
- 57.Sivo SA, Xitao F, Witta EL, Willse JT. The search for “optimal” cutoff properties: Fit index criteria in structural equation modeling. Journal of Experimental Education. 2006;74(3):267–288. doi: 10.3200/JEXE.74.3.267-288. [DOI] [Google Scholar]
- 58.Burnham KP, Anderson DR. Model selection and multi-model inference: a practical information-theoretic approach. Springer; New York, NY: 2002. [Google Scholar]
- 59.Muthen LK, Muthen BO. Mplus (version 6) [Computer software] Muthén and Muthén; Los Angeles, CA: 2010. 6.12 (Mac) edn. [Google Scholar]
- 60.Flora DB, Curran PJ. An empirical evaluation of alternative methods of estimation for confirmatory factor analysis with ordinal data. Psychological Methods. 2004;9(4):466–491. doi: 10.1037/1082-989X.9.4.466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Allison PD. Missing data. Sage; Thousand Oaks, CA: 2011. [Google Scholar]
- 62.Udry JR, Bearman PS. New methods for new research on adolescent sexual behavior. In: Jessor R, editor. New perspectives on adolescent risk behavior. Cambridge University Press; Cambridge, UK: 1998. pp. 241–269. [Google Scholar]
- 63.Petersen AC. Adolescent development. Annual Review of Psychology. 1988;39(1):583–607. doi: 10.1146/annurev.ps.39.020188.003055. [DOI] [PubMed] [Google Scholar]
- 64.Strömgren LS. The influence of depression on memory. Acta Psychiatrica Scandinavica. 1977;56(2):109–128. doi: 10.1111/j.1600-0447.1977.tb06670.x. [DOI] [PubMed] [Google Scholar]
- 65.Fann JR, Uomoto JM, Katon WJ. Cognitive improvement with treatment of depression following mild traumatic brain injury. Psychosomatics. 2001;42(1):48–54. doi: 10.1176/appi.psy.42.1.48. [DOI] [PubMed] [Google Scholar]
- 66.Veiel HOF. A preliminary profile of neuropsychological deficits associated with major depression. Journal of clinical and experimental neuropsychology. 1997;19(4):587–603. doi: 10.1080/01688639708403745. [DOI] [PubMed] [Google Scholar]
- 67.Rice F, Harold G, Thapar A. The genetic aetiology of childhood depression: A review. Journal of Child Psychology and Psychiatry. 2002;43(1):65–79. doi: 10.1111/1469-7610.00004. [DOI] [PubMed] [Google Scholar]
- 68.Dunn J, Plomin R. Separate lives: Why siblings sre so different. Wiley; New York: 1992. [Google Scholar]
- 69.Harris JR. Where is the child’s environment? A group socialization theory of development. Psychological Review. 1995;102(3):458–489. doi: 10.1037/0033-295x.102.3.458. [DOI] [Google Scholar]
- 70.Birmaher B, Ryan ND, Williamson DE, Brent DA, Kaufman J, Dahl RE, Perel J, Nelson B. Childhood and adolescent depression: A review of the past 10 years. Part I. Journal of the American Academy of Child and Adolescent Psychiatry. 1996;35(11):1427–1439. doi: 10.1097/00004583-199611000-00011. [DOI] [PubMed] [Google Scholar]
- 71.Koivumaa-Honkanen H, Tuovinen T, Honkalampi K, Antikainen R, Hintikka J, Haatainen K, Viinamäki H. Mental health and well-being in a 6-year follow-up of patients with depression. Social psychiatry and psychiatric epidemiology. 2008;43(9):688–696. doi: 10.1007/s00127-008-0353-x. [DOI] [PubMed] [Google Scholar]
- 72.Gadermann AM, Guhn M, Zumbo BD. Estimating ordinal reliability for Likert-type and ordinal item response data: A conceptual, empirical, and practical guide. Practical Assessment, Research & Evaluation. 2012;17 (3):1–13. [Google Scholar]
- 73.Asparouhov T, Muthen BO. Robust chi square difference testing with mean and variance adjusted test statistics. Los Angeles, CA: 2006. [Google Scholar]


