Abstract
Objective
Smoking and alcohol use are highly related; as such the present study investigated whether alcohol use is associated with failure in tobacco cessation attempts. We first examined the self-reported drinking behavior and smoking over the course of a year at a basic level. Next, we addressed two hypotheses to characterize this relationship at a deeper level: (H1) Alcohol use would be lower for those who attempted to quit smoking (quit for one or more days) during the year compared to those who never quit, and (H2) for those who relapsed to smoking after a quit increases in alcohol consumption would be positively associated with increases in smoking.
Method
Subjects were participants in two smoking cessation programs. One group of participants (N = 139) were part of a smoking cessation study in alcohol dependent smokers in early recovery and the other participants (N = 163) were drawn from a smoking cessation study for HIV positive smokers.
H1 was tested using t-tests. For H2, a time series analysis examined relationships between smoking and alcohol use within person over a one year period. For D1 and for H4, the analyses utilized bivariate time series procedures. Timeline follow-back data allowed for detailed daily reports of both tobacco and alcohol use.
Results
In the overall sample, there was no difference in alcohol use between those who stopped smoking and those who never stopped. However, when broken up by study, a difference was found in the alcohol dependent sample such that mean drinks were higher for those who stopped compared to those who never stopped smoking (H1). The results indicated a high number of positive significant cross-correlations between tobacco and alcohol use such that one substance predicted current, as well as past and future use of the alternate substance. Same-day cross-correlations were the most common, and dissipated with time (H2).
Conclusions
This analysis provided insights into the proximal influence of one substance on the other. Alcohol is related to relapse in smoking cessation attempts. It is important that smoking cessation efforts in alcohol using populations consider alcohol use in treatment.
Keywords: smoking, drinking, timeline follow-back, time series analysis, smoking cessation
1. Introduction
Alcohol and tobacco use are both associated with increased health risks, and there is a high level of co-morbidity for tobacco and alcohol use (Bien & Burge, 1990; D. E. Falk, Yi, & Hiller-Sturmhofel, 2006). Cigarette smokers are more likely to drink alcohol at greater rates than non-smokers (Chiolero, Wietlisbach, Ruffieux, Paccaud, & Cornuz, 2006; Dawson, 2000; D. E. Falk et al., 2006) and smokers are at a greater risk for dangerous levels of drinking (McKee, Falba, O'Malley, Sindelar, & O'Connor, 2007). In spite of the clear risks associated with these behaviors, a large proportion of the United States population continues to use these substances; over 19% describe themselves as smokers (Warner & Méndez, 2012) and 8.5% meet the diagnostic criteria for an alcohol use disorder (D. Falk, Yi, & Hiller-Sturmhöfel, 2008).
Both epidemiological and laboratory studies demonstrate a significant relationship between cigarette smoking and alcohol use (Batel, Pessione, Maitre, & Rueff, 1995), past year drinking frequency is related to smoking initiation (Reed, Wang, Shillington, Clapp, & Lange, 2007) and, among adolescents, some findings suggest that while it is common to drink without smoking, it is very unusual for smokers not to drink (Orlando, Tucker, Ellickson, & Klein, 2005). The National Epidemiological Survey of Alcohol and Related Conditions (NESARC) data show that, even at light and moderate levels of use, alcohol is associated with increased daily tobacco use and dependence in comparison to alcohol abstainers (D. Falk et al., 2008). Cigarette smoking is also related to alcohol use disorders (AUD), such that for those who were nicotine dependent, the 12-month co-morbidity for an AUD was 22.8% compared with the general population at 8.5%. In addition, for those with an AUD, the 12-month co-morbidity for nicotine dependence is 34.5% compared to only 12.8% in the general population (Hasin & Grant, 2004).
Several theories might explain the relationship between smoking and alcohol dependence (Cooney et al., 2007): cross-substance coping response hypothesis (Monti, Rohsenow, Colby, & Abrams, 1995), suggests that smoking might be used to suppress alcohol cravings, just as drinking might be used to suppress cigarette cravings. Another theory, cross substance cue reactivity (Rohsenow et al., 1997), suggests associative learning as well as cognitive or semantic associations between alcohol and cigarette use. It is possible that the two substances are often used in conjunction and that over time each substance becomes a prime for the other substance. This might help to elucidate why alcohol is an obstacle in smoking cessation and might be a cue for relapse (Sayette, Martin, Wertz, Perrott, & Peters, 2005). Lastly, the limited strength model hypothesizes that self-control is a resource that is limited and using this resource consumes strength (Muraven & Baumeister, 2000). As such, it is possible that if an individual “uses up” their self-control for one behavior (e.g. not smoking) it reduces the amount of strength available for subsequent self-control (e.g. abstaining from drinking).
Recent research has examined the effect of alcohol use on smoking treatment failure in smokers (Leeman et al., 2008). Leeman et al. (2008) found that the probability of smoking on heavy drinking days was higher than the probability of smoking on moderate or abstinent drinking days. This study also found that moderate drinkers were less likely than hazardous alcohol users to have relapsed into smoking at 12-weeks post-quit.
We first describe the self-reported drinking behavior of all study participants and smoking relapsers over the course of a year. In addition we characterized the relationship between the amount of alcohol consumed and the mean number of cigarettes smoked per day and investigated differences in the mean cigarettes per day for those who a) drink alcohol compared to those who do not drink alcohol, b) drink daily versus those who do not drink daily, and c) drink heavily versus those who do not drink heavily. Two hypotheses were brought forth: (H1) Alcohol use would be lower for those who attempted to quit smoking (quit for one or more days) during the year compared to those who never quit, and (H2) for those who relapsed to smoking after a quit increases in alcohol consumption would be positively associated with increases in smoking.
2. Method
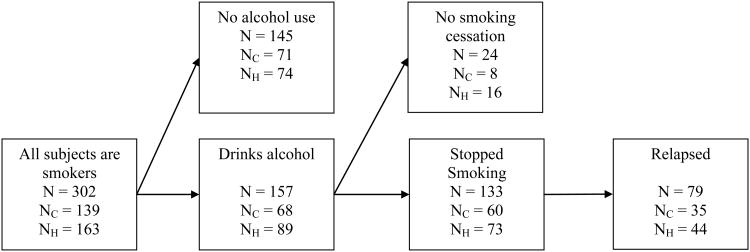
In an effort to help understand these issues, this study examined the temporal relationship between smoking and drinking in two samples seeking smoking cessation treatment: an HIV-positive group and an alcohol dependent group. Both studies used the timeline follow-back method (L. C. Sobell & Sobell, 1996) to obtain self-reports of tobacco and alcohol use covering 90-day periods at 3, 6, 9, and 12 months (Carney, Tennen, Affleck, Del Boca, & Kranzler, 1998). This is a secondary analysis of data from two clinical trials of smoking cessation treatment. Here we provide a brief description of those two trials. Of the 371 total subjects, 26 participants attended only the baseline interview, and 43 did not have TLFB (Timeline Follow-Back) data. Participant flow for this work is displayed in Figure 1.
Figure 1.
Subject Flow.
Note: NC = N for alcohol dependent sample Study, and NH = N for
Study 1. Intensive Intervention for Cigarette Smokers in Alcohol Treatment
The Carmody et al. study (2011) is a two-arm randomized clinical trial, comparing intensive intervention for smoking cessation with usual care among alcohol-dependent smokers in early recovery. The intensive intervention consisted of combination nicotine replacement therapy (i.e., nicotine patches combined with adjuvant nicotine lozenges, gum, inhaler, or nasal spray) and extended cognitive-behavioral counseling conducted over a period of 26 weeks. Usual care involved a referral to a free-standing smoking cessation program. Patients (N = 162) came from the Drug and Alcohol Treatment programs at two Northern California VA Medical Centers and were veterans. Patients were eligible for the study if they were at least 18 years of age, reported alcohol as their primary drug of abuse, were currently smoking at least 5 cigarettes per day, were abstinent from alcohol for at least 7 days and not more than 6 months, and reported an interest in quitting smoking. Exclusion criteria included: any contraindications for nicotine patches or adjuvant nicotine medications (e.g., unstable angina or recent myocardial infarction, skin allergy to the patch, severe cardiovascular disease, lactation, pregnancy by self-report or by positive serum pregnancy test in pre-menopausal women), unstable psychiatric disorder, and severe cognitive impairment. This intensive intervention yielded a higher short-term smoking quit rate compared to the usual care group. Data were collected by trained research assistants using pen and paper surveys.
Study 2. Smoking Treatments in HIV Clinical Care Settings
This study (Humfleet et al., 2009) was a three-arm randomized clinical trial, comparing two targeted smoking treatments to a control: a) HIV-targeted traditional counseling, a six-session individual counseling treatment based on a cognitive-behavioral treatment model, b) Computer-based Intervention which adapted the HIV-targeted counseling condition provided via computer and the Internet, and c) Minimal Contact Control Condition where each participant met with a research staff member who recommended establishing a quit date during Week 2. Patients (N = 209) from two outpatient clinics serving HIV positive persons in San Francisco, California participated in the study. Patients were considered eligible if they were 18 years or older, smoked at least most days of the month, and were registered patients at one of the facilities. Exclusion criteria included: already enrolled in other smoking cessation treatment, or were experiencing significant or severe cognitive impairment or dementia. Baseline data were collected by having participants complete the Composite International Interview (CIDI) and by self-report questionnaires. TLFB data were collected through interview methods. The study found no differences in abstinence rates across groups, but smoking abstinence rates were comparable to those found in other similar treatment studies.
2.1. Measures
Baseline data assessed demographic information: age, years of education, sex, marital status, living situation, ethnicity, employment status, highest degree of education, and sexual orientation. Smoking variables included age at first cigarette, age smoked regularly, prior quit attempts, cigarettes smoked past 24 hours and past 7 days, usual number of cigarettes in the last 24 hours, and breath CO. Alcohol variables included number of days using alcohol in the last 30 days, number of years drinking alcohol, number of days intoxicated in the last 30 days, and number of years with intoxication.
The TLFB method (Linda C Sobell & Sobell, 1992) is an empirically-validated procedure for gathering retrospective self-report information from subjects about smoking, alcohol and other drug use. This approach employs a calendar with specific anchor dates tailored to each subject to identify quantity and frequency of use of substances. Self-reports covering 90-day periods from study intake through 12 months were collected as part of each study's assessment procedures. We estimated the validity of the TLFB data by comparing it to a biologically validated measure, expired carbon monoxide (CO), which was collected at the four follow-up assessments for both studies (3, 6, 9 and 12 months). Self-reported smoking (asking about the last 7 days of use) was used in conjunction with the CO data where both were available for the same time period. Participants were only coded abstinent when they reported no cigarette use, not even a puff, in the last seven days and if their CO level was ≤ 10 ppm. In total, 1202 data points (e.g. participants had multiple data points) had both forms of data and only 6 times did someone have a CO-verified abstinence, yet said they smoked in the last 7 days. Just under 5% (n = 57) of the time someone was coded as smoking via CO when they said in the TLFB they did not smoke.
2.2. Data Analysis
For the preliminary descriptive and characterization work we used simple bivariate correlations and t-tests. For the participants who reported any alcohol consumption and who both smoked, became abstinent (at least 7 days of abstinence), and relapsed back to smoking (relapsers), we examined the correlation of number of drinks with number of cigarettes smoked both before and after the smoking relapse.
The primary analyses used PROC TIMESERIES analysis in SAS 9.2 (SAS, 2008). Within day (synchronous) and across day (lagged) correlations were computed. Univariate time series analysis examines the correlations between observations of a single behavior while bivariate time series analysis, used here, examines the cross-correlations between two behaviors (e.g. smoking and drinking). It is common to statistically remove effects that are not better accounted for by trends and autocorrelations within alcohol and smoking behavior, (i.e.pre-whitening of residuals in univariate time series models) (Fuller et al., 2003). Because PROC ARIMA allows for pre-whitening, we first modeled the data using this procedure both with and without pre-whitening to determine whether the pre-whitening altered the results. As it did not, we used PROC TIMESERIES, which cannot pre-whiten, but has the ability to calculate p-values for the cross-correlations. This analysis estimated both synchronous (within day) and lagged (across day) forecasts between smoking and alcohol use. Analysis was completed for the overall sample and each subsample.
Bivariate time series analysis was used to estimate within person models for synchronous lag (Lag 0) and to examine the relationship between smoking and drinking with day, 7 days of past lags (Lag -1 to Lag -7) to test for the relationship between smoking and drinking when smoking precedes drinking, and 7 days of future lags (Lag 1 to Lag 7) to test for the relationship between smoking and drinking when smoking follows drinking. Each significant correlation (p < .05) was categorized by its sign (positive or negative) indicating its direction. The 7-lag structure was selected to represent a week in either direction, as we believed that was the longest period of time that we could reasonably assume that any real relationship could be justified.
3. Results
3.1. Demographics and alcohol and smoking characteristics (Table 1)
Table 1. Baseline Demographics and Smoking and Drinking Variables (means and percentages).
| All participants (N = 302) | Relapsers (N = 79) | Alcohol dependent sample (N = 35) | HIV sample (N = 44) | |
|---|---|---|---|---|
| Age, M (SD) | 47.8 (8.1) | 46.3 (7. 9) | 49.9 (7.7) | 45.98 (7.8) |
| Years of education, M (SD) | 12.4 (2.4) | 12.1 (1.9) | 13.04 (1.9) | 11.60 (2.8)**** |
| Sex (%) | ||||
| Male | 89.4 | 89.9 | 97.2 | 82.8**** |
| Female | 8.6 | 7.6 | 2.9 | 14.1 |
| Other | 1.7 | 2.5 | 0.0 | 3.1 |
| Marital status (%) | ||||
| Married | 6.7 | 9.2 | 9.4 | 4.4**** |
| Separated, divorced | 32.4 | 27.6 | 5.2 | 15.6 |
| Widowed | 4.3 | 3.9 | 4.3 | 4.4 |
| Never married | 56.6 | 59.2 | 34.5 | 75.6 |
| Live with spouse/partner (% yes) | 15.2 | 15.8 | 10.1 | 20.0** |
| Ethnicity (%) | ||||
| African American | 33.4 | 39.2 | 40.3 | 27.6 |
| Caucasian | 49.7 | 45.6 | 45.3 | 53.4 |
| Other | 16.9 | 15.2 | 14.4 | 19.0 |
| Hispanic (% yes) | 13.8 | 11.5 | 10.8 | 16.5 |
| Employment Status (%) | ||||
| Currently employed | 10.9 | 6.85 | 7.2 | 14.6 |
| Unemployed | 74.2 | 82.19 | 80.6 | 68.1 |
| Retired | 12.0 | 9.59 | 10.8 | 13.2 |
| Homemaker | 1.1 | 1.47 | 0.7 | 1.4 |
| Student | 1.8 | 0.00 | 0.7 | 2.8 |
| Income (%) | ||||
| Less than $10,000 | 50.3 | 53.25 | 57.6 | 43.9 |
| $10,000-$40,999 | 45.4 | 44.16 | 35.9 | 52.9 |
| $41,000-60,999 | 3.0 | 1.30 | 5.0 | 1.3 |
| $61,000 or more | 1.2 | 1.3 | 1.4 | 1.9 |
| Highest degree (%) | ||||
| High school, G.E.D. | 59.7 | 69.7 | 63.5 | 55.9** |
| Some college | 24.1 | 21.2 | 28.6 | 19.7 |
| College graduate, post grad | 16.1 | 9.1 | 7.9 | 24.4 |
| Sexual orientation (%) | ||||
| Heterosexual | 54.5 | 56.58 | 89.8 | 22.9**** |
| Homosexual/gay/lesbian | 40.0 | 42.11 | 8.0 | 68.6 |
| Bisexual | 5.5 | 1.32 | 2.2 | 8.5 |
| Smoking Variables | ||||
| Age 1st tried cigarettes | 14.1 (5.5) | 13.9 (4.9) | 13.8 (4.2) | 14.2 (6.3) |
| Age began smoking regularly, M (SD) | 17.9 (6.5) | 17.4 (5.9) | 18.6 (6.7) | 17.3 (6.2) |
| Prior attempts to quit, M (SD) | 4.0 (6.5) | 4.9 (8.9) | 4.1 (7.3) | 3.9 (5.7) |
| Cigarettes smoked past 24 hours, M (SD) | 15.6 (10.8) | 14.4 (8.4) | 14.4 (10.9) | 16.6 (10.5) |
| Cigarettes smoked last 7 days, M (SD) | 110.8 (71.4) | 109.8 (71.3) | 99.0 (67.8) | 120.8 (73.1)** |
| Cigarettes usual in 24 hours, M (SD) | 18.4 (14.4) | 17.9 (10.3) | 16.8 (10.2) | 19.7 (10.9) |
| Breath CO [ppo], M (SD) | 14.4 (10.1) | 15.2 (11.6) | 10.8 (6.8) | 17.4 (11.2)**** |
| Alcohol Variables | ||||
| Alcohol any use, last 30 days, no. days, M (SD) | 3.9 (7.1) | 4.0 (6.5) | 3.5 (5.8) | 4.3 (8.3) |
| Alcohol any use lifetime, no. years, M (SD) | 23.6 (13.3) | 22.4 (12.2) | 27.9 (11.4) | 19.9 (13.8)**** |
| Alcohol int'xct last 30 days, no. days, M (SD) | 1.8 (4.6) | 1.8 (4.1) | 2.8 (5.2) | .88 (3.7)**** |
| Alcohol int'xct lifetime, no. years, M (SD) | 18.4 (14.1) | 17.3 (13.3) | 23.0 (12.7) | 14.4 (14.1)**** |
Note: Asterix indicate differences between 2 samples;
p<.05,
p<.01,
p<.001,
p<.001
Descriptives and characterizations of the relationship between smoking and alcohol use
The two samples were compared in terms of demographics. The studies did not differ by age, ethnicity, employment status, or income. However, they did differ by gender, education, and by sexual orientation. The studies were also compared by baseline smoking and drinking. The two samples did not differ by age at first cigarette, age became a regular smoker, prior attempts to quit, 24-hour cigarette use, and number of days used alcohol in the last 30 days. For smoking variables, the studies differed by past week cigarettes and by breath CO. They differed by years of lifetime alcohol use, and by number of days intoxicated in the last 30 days. Study 1 was an alcohol treatment sample, and Study 2 had 42.9% alcohol dependent persons.
In addition, all demographic and alcohol and smoking characteristics were analyzed for both the entire sample of participants and for the relapsers separately. Table 1 summarizes the demographic characteristics of all study participants, relapsers only, and each study separately. Table 2 displays summary statistics for reported alcohol consumption and number of cigarettes smoked based on the TLFB data, as well as number of days with data. As not all participants filled in information for all days, the number of days covered varies by participant.
Table 2.
Summary of self-reported alcohol consumption and smoking.
| All participants (N = 302) | Relapsers (N = 79) | Alcohol dependent sample (N = 35) | HIV sample (N = 44) | |
|---|---|---|---|---|
| Mean number of days with data (min and max days) | 299.8 (69, 365) | 322.6 (161, 365) | 322.9 (161, 365) | 322.3 (164, 365) |
| Reporting any days drinking (%) | 51.9 | 100.0 | 62.9 | 45.5 |
| % who drank daily (smoker/drinkers) | 1.3 | 0.00 | 10.7 (18.3) | 12.6 (22.4) |
| % reporting heavy drinking* (smoker/drinkers) | 26.5 | 53.2 | 16.3 (21.3) | 21.39 (29.6) |
| Mean % days drinking (smoker/drinkers), M (SD) | 20.1 (28.1) | 11.8 (20.6) | - | - |
| Mean % days drinking (smoker/heavy drinkers), M (SD) | 25.1 (27.9) | 18.7 (25.4) | - | - |
| Mean % heavy drinking days among drinking days (smoker/heavy drinkers), M (SD) | 60.4 (38.8) | 61.5 (39.2) | 64.64 (39.1) | 58.01 (40.2) |
| Mean cigarettes per day, M (SD) | 8.7 (7.1) | 7.3 (6.1) | 7.82 (5.5) | 6.94 (6.6) |
Note: Heavy drinking defined as 5+ drinks per day for men, 4+ per day for women. Heavy drinker Ns: All=80, Relapsers = 42.
3.2. Relationships between Alcohol and Cigarettes
Number of cigarettes smoked per day and total number of alcoholic beverages consumed over the year was significantly correlated in the overall sample (r = .22, p < .0001), in each study (alcohol dependent sample: r = .21, p < .05, HIV sample r = .25, p < .01) and in relapsers (r = .24, p < .05).
In the full sample, there was no difference in cigarettes smoked per day in those who drank alcohol compared to those who did not (t(300) = 0.10, p = .92) nor was there in each sample (alcohol dependent sample: t(137) = 0.98, p = .33, HIV sample t(167) = 0.87, p = .38). There was also no difference in mean cigarettes smoked per day for those who drank alcohol daily compared to those who did not (overall: t(300) = 1.01, p =.32; HIV sample: t(161) = 0.86, p =.39). There was, however, a significant difference in cigarettes smoked per day among those who drank heavily compared to those who did not in the full sample (t(300) = 3.07, p < .01) and in relapsers (t(77) = 2.71, p < .01), such that heavy drinkers smoked more cigarettes on average per day (full sample: M = 8.77, SD = 6.7; relapsers: M = 7.92, SD = 5.7) than those who were not heavy drinkers (full sample: M = 6.39, SD = 5.63; relapsers: M = 4.72, SD = 4.60). However by sample, only one sample found this effect (alcohol dependent sample: t(137) = 0.20, p = .83, HIV sample: t(161) = 4.11, p < .0001).
Hypothesis 1. Differences in alcohol use between those who stopped smoking and those who never stopped
In the overall sample, there was no difference in alcohol use between those who stopped smoking (even for one day) and those who never stopped (t(300) = 0.08, p = .93). When broken up by study though there was a significant difference in one group (alcohol dependent sample: t(137) = 2.88, p < .0001, HIV sample: t(161) = 1.42, p = .16); in the alcohol dependent sample, for those who had stopped, the mean number of drinks was 29.76 (SD = 90.9) and for those who did not stop the mean was 131.7 (SD = 324.5). It should be noted that 5 % of the full sample quit for just one day.
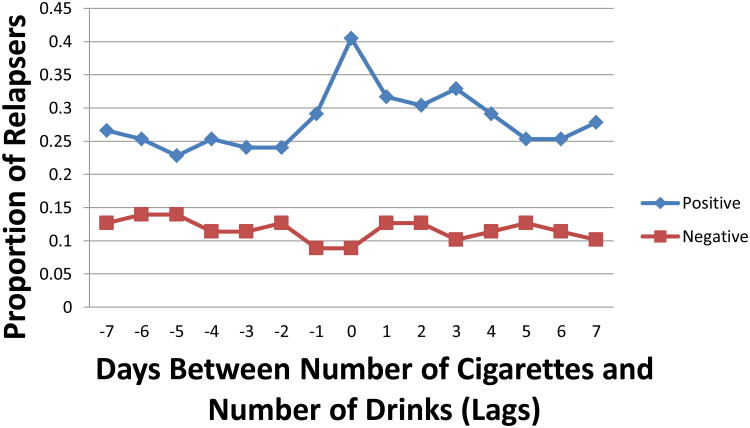
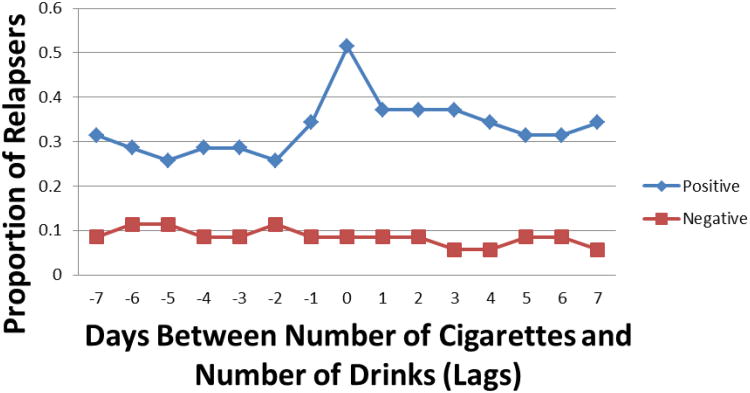
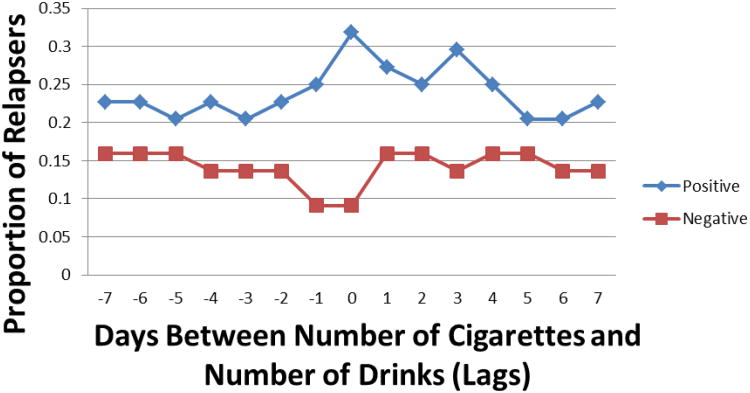
Hypothesis 2: For those who relapsed to smoking after a quit are increases in alcohol consumption associated with increases in smoking? What is the direction of this relationship?
Figure 2 (a-c) presents the proportion of participants at each of the 15 lags (Lag -7 to Lag 7) who had significant cross-correlations between smoking and alcohol use by direction of the relationship (positive or negative) for the overall sample and each study. Overall, positive cross-correlations were more common than negative cross-correlations. Specifically, higher levels of smoking or drinking predicted higher levels of the alternate behavior within day and on past and future days, whereas lower levels of smoking or drinking predicted lower levels of the alternative behavior. This pattern appears the most clearly at Lag 0 (i.e. level of drinking and smoking on the same day), with 40.5% (alcohol dependent sample: 51.4%, HIV sample: 31.2%) of the sample of relapsers showing positive significant cross-correlations between alcohol and smoking on the same day. There was also a strong demonstration of this effect at Lag 1 and Lag -1, such that between 29.1% (alcohol dependent sample: 34.3%, HIV sample: 25.0%) (Lag -1) and 31.6% (alcohol dependent sample: 37.1%, HIV sample: 27.3%) (Lag 1) of relapsers had positive significant cross-correlations. The number of significant positive cross-correlations decreased with increasing time lag.
Figure 2.
Figure 2a. Proportion of subjects with significant alcohol × smoking cross lags by temporal direction and behavioral direction (overall, Alcohol dependent sample Study, HIV sample Study).
Figure 2b. Proportion of subjects with significant alcohol × smoking cross lags by temporal direction and behavioral direction (Alcohol dependent sample Study).
Figure 2c. Proportion of subjects with significant alcohol × smoking cross lags by temporal direction and behavioral direction (HIV sample Study).
Note: Negative lags indicate when smoking preceded drinking, while positive lags indicate when smoking followed drinking
An examination of the within-person cross-correlations revealed that 49 (62.0% overall, alcohol dependent sample: 62.9%, HIV sample: 59.1%) of the relapsers exhibited a statistically significant cross-correlation at one or more lag (past or future). This indicates a clear relationship between smoking and drinking either when smoking follows or precedes drinking. The results were also examined by direction of lag, such that 40 participants (50.6% of relapsers, alcohol dependent sample: 48.6%, HIV sample: 52.3%) showed significant future (positive lags) cross-correlations. Twenty-nine (36.7%, alcohol dependent sample: 42.9%, HIV sample: 31.8%) of relapsers had positive cross-correlations at future lags (Lag 1 to Lag 7), 11 (13.9%, alcohol dependent sample: 11.4%, HIV sample: 15.9%) relapsers showed negative cross-correlations at the positive lags. Thirty-four of the relapsers (43.0%, alcohol dependent sample: 45.7%, HIV sample: 40.9%) had statistically significant cross-correlations at negative (past) lags. Thirty-five relapsers (44.3%, alcohol dependent sample: 42.9%, HIV sample: 45.5%) showed positive past cross-correlations, but did not show positive future lag cross-correlations indicating that smoking predicted drinking across time. Thirty-nine (49.4%, alcohol dependent sample: 51.4%, HIV sample: 47.7%) of relapsers had positive future cross-correlations, but no past lag positive cross-correlations, indicating that drinking predicted smoking. These results suggest that drinking predicted future smoking.
4. Discussion
While most researchers believe that alcohol use negatively influences smoking quit rates (Agudo et al., 2004; Leeman et al., 2008; Zimmerman, Warheit, Ulbrich, & Auth, 1990), there is a paucity of research on the influence of present drinking on smoking cessation rates, and alcohol use has been noted as a precipitant for smoking relapse (Shiffman, 1986), even after a long period of smoking abstinence (Krall, Garvey, & Garcia, 2002).
Mean cigarettes per day and past year total number of alcoholic beverages consumed were positively correlated. This supports the literature where similar relationships have been observed (Batel et al., 1995). No difference was found in cigarettes per day among those who drank alcohol at any level compared to alcohol abstainers; however, there was a significant difference in total cigarettes per day smoked for those who drank heavily compared to those who did not drink heavily such that heavy drinkers smoked more cigarettes per year only in relapsers. It is possible that comparing people who drank at any level to those who did not drink at all showed no difference because those who drank at any level might have such low use that the relationship with cigarettes was not discernible.
No difference in alcohol use was found between those who stopped smoking (even for one day) and those who never quit smoking in the overall sample (and the HIV sample sample), but differences were found in one study. For the alcohol dependent sample, the mean number of drinks was significantly higher for those who never quit compared to those who did quit. It is possible that no difference was found in the overall sample and in the HIV sample study because “quitting” for one day or even several days is not substantial enough to find any differences between groups on alcohol use when examining alcohol use over the course of the year (e.g. not specific within person correlations in a small time period).
This analysis used TLFB methods to assess daily smoking and drinking behaviors; while studies have examined daily reports of smoking or drinking, only one prior study has examined cross-correlations of these behaviors (Dierker et al., 2006). Positive cross-correlations, indicating that higher levels of one of the behaviors is related to higher levels of the other behavior; were more common than negative cross-correlations, indicating that lower levels of one behavior are correlated with greater levels of the other behavior. Greater levels of smoking or drinking predicted higher levels of the alternate behavior within-day and on past and future days, just as lower levels of smoking or drinking predicted lower levels of smoking or drinking same day or on past or future days. Results for the two samples were very similar and so results for the combined data are presented next.
At Lag 0 (within-day) we see the strong relationship between alcohol use and smoking most visibly; 40% of the relapsers exhibited statistically significant positive cross-correlations between alcohol and smoking behaviors on the same day. This finding supports previous research indicating that smoking and alcohol behaviors are highly correlated on the same day. At Lag 1 and Lag -1 (i.e., when smoking on Day t is related to drinking on Day t+1 and vice a versa) we also saw this same pattern of results. For approximately 30% of the sample of relapsers past day drinking or smoking predicted next day smoking or drinking in the same direction, as well as the reverse. The strength of the relationship decreased as the time separation increased which would indicate that any relationship is confined to within a few days at most.
Within-person cross-correlations indicated that 62% of the sample demonstrated a strong relationship between smoking and drinking either when smoking follows or precedes alcohol use. Direction of lag was also examined and it was found that for approximately 50% of relapsers alcohol predicted smoking), for approximately 40% of relapsers alcohol predicted more future smoking, for 15% alcohol predicted less future smoking, and 40% of relapsers showed that smoking predicted alcohol use. In addition, for approximately 50% smoking positively predicted alcohol use but alcohol did not predict smoking; indicative that smoking predicted drinking across time. Conversely, for approximately half of all relapsers alcohol predicted more smoking s without smoking predicting increased future alcohol use, indicating that alcohol use also predicted smoking. It is difficult to tease apart whether the relationship between alcohol and smoking is bi-directional as no causality can be directly inferred (i.e. alcohol use predicts cigarette use and/or vice versa) from these results. Indeed drinking predicted future smoking and may to be the most theoretically plausible interpretation. Alternatively, it is possible there are different subpopulations, such that one population is more likely to smoke after having consumed alcohol while another expresses the reverse relationship. This interpretation is based on the finding that 45% of the relapsers showed only that smoking predicted alcohol and 50% showed that alcohol predicted smoking only.
In non-experimental settings it is difficult to disentangle cause and effect from simple relationships. The pattern visible in this data clearly indicates that alcohol use and smoking are related; however the specific nature of this relationship is not clearly discernible. It is possible that some third variable or set of variables are responsible for this relationship. For this reason the strict reliance on theory is imperative.
The cross-substance response hypothesis (Monti et al., 1995) was not supported by our findings. This theory postulates that smoking is used to suppress cravings for alcohol and vice versa. Our findings suggest that there might be an increased alcohol urge after cigarette use (or cigarette use after alcohol). Smoking (or drinking) does not appear to be an effective way to cope with cravings. However, an alternative theory, the cross substance cue reactivity theory (Rohsenow et al., 1997) suggests that, based on classical conditioning principles, alcohol and tobacco are often consumed together and as such the repeated pairings create smoking cues when drinking (and vice versa) as a conditioned stimuli. Accordingly, smoking might elicit urges to drink and drinking might elicit urges to smoke. This theory appears to be supported by the data. Note that the cross-substance coping theory and the cross substance cue reactivity theory produce opposite predictions for alcohol using populations who are concurrently treated for smoking. Lastly, the limited strength model (Muraven & Baumeister, 2000) purports that self-control is a limited resource such that exerting self-control “consumes” self-control strength and it can essentially be “used up.” Practically, this might mean that if an individual suppresses urges to smoke, that individual might not be able to suppress urges to drink. This theory has important implications for treating alcohol dependent smokers and appears to be supported by the data (but was not directly tested).
Most models regarding the co-morbidity of alcohol and smoking indicate that there is a shared vulnerability common to both addictions and a reciprocal influence between the two behaviors (Little, 2000; Rohsenow et al., 1997; Sher, Gotham, Erickson, & Wood, 1996). Shared susceptibility to alcohol and smoking can be related to a wide range of constructs including genetic predisposition (Grucza & Bierut, 2006), psychological variables such as depression (Epstein, Induni, & Wilson, 2009), and environmental effects (von der Pahlen et al., 2008). It is also likely that one substance primes use of the reciprocal substance (Leeman et al., 2008). Rohsenow et al. (Rohsenow et al., 1997) suggested associative learning as well as cognitive or semantic associations between alcohol and cigarette use. It is possible that the two substances are used in conjunction for a number of reasons and that over time each substance becomes a prime for the other substance. This might help to elucidate why alcohol is an obstacle in smoking cessation and might be a cue for relapse.
4.1. Limitations
The findings in this study should be interpreted with certain limitations in mind. There is some concern for Type I error as a p < .05 was used to determine statistical significance for all cross-correlations. It is also important to note that all data were retrospective self-reported data and while CO reports were used to validate part of the TLFB data, they cannot be used to assume that the full 90 day recall periods were accurate. Both of the samples studied were composed of treatment seeking smokers, as such the results are not generalizeable to non-treatment seeking smokers, however this increases the validity of the conclusions relative to the smoking cessation literature. While one of the samples was comprised of veterans the generalizability of these findings might be limited, but the results appear to be robust as they were paralleled in the other non-veteran sample. In addition, one of the samples (Carmody et al., 2011) were in smoking cessation program for alcohol dependent individuals.
4.2. Conclusion
Overall, there is a paucity of research on the specific temporal relationship between alcohol use and smoking relapse. We found a positive relationship between the amount of alcohol consumed and the number of cigarettes smoked. Time series analysis revealed that positive cross-correlations were more common than negative cross-correlations; indicating that higher (or lower) levels alcohol or cigarettes were related to higher (or lower) levels of the other substance. This pattern was most apparent within day and for predictions of one day to the following day, but dissipates with increasing days between behaviors. There appears to be a relationship between smoking and drinking both when smoking follows and precedes drinking. It appears that treatment programs for smoking cessation should not ignore the perils of alcohol on smoking relapse and thus must have a dual focus on both cigarettes and alcohol in order to enhance efficacy. Future research is needed to further distinguish the specific mechanisms that underlie this complex relationship.
Highlights.
Two smoking cessation trials samples were examined.
Time series analysis used to examine the relationship between smoking and alcohol use.
High number of positive cross-correlations between substances, particularly on the same day.
Alcohol plays a significant role in relapse in smoking cessation attempts.
Acknowledgments
Research supported by NIDA TRC Center Grant (P50 DA09253) and NIDA Training Grant (T32 DA 007250).
Footnotes
Author Disclosures: The authors have nothing to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Agudo A, Pera G, Rodriguez M, Quiros JR, Navarro C, Martinez C, et al. Chirlaque MD. Changes in smoking habits in adults: results from a prospective study in Spain. Annals of epidemiology. 2004;14(4):235–243. doi: 10.1016/S1047-2797(03)00245-X. [DOI] [PubMed] [Google Scholar]
- Batel P, Pessione F, Maitre C, Rueff B. Relationship between alcohol and tobacco dependencies among alcoholics who smoke. Addiction. 1995;90(7):977–980. doi: 10.1046/j.1360-0443.1995.90797711.x. [DOI] [PubMed] [Google Scholar]
- Bien TH, Burge R. Smoking and drinking - a review of the literature. International Journal of the Addictions. 1990;25(12):1429–1454. doi: 10.3109/10826089009056229. [DOI] [PubMed] [Google Scholar]
- Carmody TP, Delucchi K, Duncan CL, Banys P, Simon JA, Solkowitz SN, et al. Hall SM. Intensive intervention for alcohol-dependent smokers in early recovery: A randomized trial. Drug and alcohol dependence. 2011 doi: 10.1016/j.drugalcdep.2011.09.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carney MA, Tennen H, Affleck G, Del Boca FK, Kranzler HR. Levels and patterns of alcohol consumption using timeline follow-back, daily diaries and real-time “electronic interviews”. Journal Of Studies On Alcohol. 1998;59(4):447–454. doi: 10.15288/jsa.1998.59.447. [DOI] [PubMed] [Google Scholar]
- Chiolero A, Wietlisbach V, Ruffieux C, Paccaud F, Cornuz J. Clustering of risk behaviors with cigarette consumption: A population-based survey. Preventive Medicine. 2006;42(5):348–353. doi: 10.1016/j.ypmed.2006.01.011. [DOI] [PubMed] [Google Scholar]
- Cooney NL, Litt MD, Cooney JL, Pilkey DT, Steinburg HR, Oncken CA. Alcohol and tobacco cessation in alcohol-dependent smokers: Analysis of realtime reports. Psychology of Addictive Behaviors. 2007;21(3):277. doi: 10.1037/0893-164X.21.3.277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson DA. Drinking as a risk factor for sustained smoking. Drug and Alcohol Dependence. 2000;59(3):235–249. doi: 10.1016/s0376-8716(99)00130-1. [DOI] [PubMed] [Google Scholar]
- Dierker L, Lloyd-Richardson E, Stolar M, Flay B, Tiffany S, Collins L, et al. Tern The proximal association between smoking and alcohol use among first year college students. Drug and Alcohol Dependence. 2006;81(1):1–9. doi: 10.1016/j.drugalcdep.2005.05.012. [DOI] [PubMed] [Google Scholar]
- Epstein JF, Induni M, Wilson T. Peer Reviewed: Patterns of Clinically Significant Symptoms of Depression Among Heavy Users of Alcohol and Cigarettes. Preventing chronic disease. 2009;6(1) [PMC free article] [PubMed] [Google Scholar]
- Falk D, Yi H, Hiller-Sturmhöfel S. An epidemiologic analysis of co-occurring alcohol and drug use and disorders. Alcohol Res Health. 2008;31:100–110. [PMC free article] [PubMed] [Google Scholar]
- Falk DE, Yi HY, Hiller-Sturmhofel S. An epidemiologic analysis of co-occurring alcohol and tobacco use and disorders - Findings from the National Epidemiologic Survey on Alcohol and Related Conditions. Alcohol Research & Health. 2006;29(3):162–171. [PMC free article] [PubMed] [Google Scholar]
- Fuller JA, Stanton JM, Fisher GG, Spitzmüller C, Russell SS, Smith PC. A lengthy look at the daily grind: time series analysis of events, mood, stress, and satisfaction. Journal of Applied Psychology. 2003;88(6):1019. doi: 10.1037/0021-9010.88.6.1019. [DOI] [PubMed] [Google Scholar]
- Grucza R, Bierut L. Co-occurring risk factors for alcohol dependence and habitual smoking: update on findings from the Collaborative Study on the Genetics of Alcoholism. Alcohol research & health: the journal of the National Institute on Alcohol Abuse and Alcoholism. 2006;29(3):172. [PMC free article] [PubMed] [Google Scholar]
- Hasin D, Grant B. The co-occurrence of DSM-IV alcohol abuse in DSM-IV alcohol dependence: results of the National Epidemiologic Survey on Alcohol and Related Conditions on heterogeneity that differ by population subgroup. Archives of General Psychiatry. 2004;61(9):891. doi: 10.1001/archpsyc.61.9.891. [DOI] [PubMed] [Google Scholar]
- Humfleet GL, Delucchi K, Kelley K, Hall SM, Dilley J, Harrison G. Characteristics of HIV-positive cigarette smokers: a sample of smokers facing multiple challenges. AIDS education and prevention: official publication of the International Society for AIDS Education. 2009;21(3 Suppl):54. doi: 10.1521/aeap.2009.21.3_supp.54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krall EA, Garvey AJ, Garcia RI. Smoking relapse after 2 years of abstinence: findings from the VA Normative Aging Study. Nicotine & Tobacco Research. 2002;4(1):95–100. doi: 10.1080/14622200110098428. [DOI] [PubMed] [Google Scholar]
- Leeman RF, McKee SA, Toll BA, Krishnan-Sarin S, Cooney JL, Makuch RW, O'Malley SS. Risk factors for treatment failure in smokers: Relationship to alcohol use and to lifetime history of an alcohol use disorder. Nicotine & Tobacco Research. 2008;10(12):1793–1809. doi: 10.1080/14622200802443742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Little HJ. Behavioral mechanisms underlying the link between smoking and drinking. Alcohol Research & Health. 2000 [PMC free article] [PubMed] [Google Scholar]
- McKee SA, Falba T, O'Malley SS, Sindelar J, O'Connor PG. Smoking status as a clinical indicator for alcohol misuse in US adults. Archives of Internal Medicine. 2007;167(7):716–721. doi: 10.1001/archinte.167.7.716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monti PM, Rohsenow DJ, Colby SM, Abrams DB. Smoking among alcoholics during and after treatment: Implications for models, treatment strategies, and policy. Alcohol and tobacco: From basic science to clinical practice. 1995:187–206. [Google Scholar]
- Muraven M, Baumeister RF. Self-regulation and depletion of limited resources: Does self-control resemble a muscle? Psychological bulletin. 2000;126(2):247. doi: 10.1037/0033-2909.126.2.247. [DOI] [PubMed] [Google Scholar]
- Orlando M, Tucker JS, Ellickson PL, Klein DJ. Concurrent use of alcohol and cigarettes from adolescence to young adulthood: An examination of developmental trajectories and outcomes. Substance use & misuse. 2005;40(8):1051–1069. doi: 10.1081/JA-200030789. [DOI] [PubMed] [Google Scholar]
- Reed MB, Wang R, Shillington AM, Clapp JD, Lange JE. The relationship between alcohol use and cigarette smoking in a sample of undergraduate college students. Addictive Behaviors. 2007;32(3):449–464. doi: 10.1016/j.addbeh.2006.05.016. [DOI] [PubMed] [Google Scholar]
- Rohsenow DJ, Monti PM, Colby SM, Gulliver SB, Sirota AD, Niaura RS, Abrams DB. Effects of alcohol cues on smoking urges and topography among alcoholic men. Alcoholism: Clinical and Experimental Research. 1997;21(1):101–107. [PubMed] [Google Scholar]
- SAS. SAS/STAT® 9.2 User's Guide 2008 [Google Scholar]
- Sayette MA, Martin CS, Wertz JM, Perrott MA, Peters AR. The effects of alcohol on cigarette craving in heavy smokers and tobacco chippers. Psychology of addictive behaviors: journal of the Society of Psychologists in Addictive Behaviors. 2005;19(3):263. doi: 10.1037/0893-164X.19.3.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sher KJ, Gotham HJ, Erickson DJ, Wood PK. A Prospective, High-Risk Study of the Relationship between Tobacco Dependence and Alcohol Use Disorders. Alcoholism: Clinical and Experimental Research. 1996;20(3):485–492. doi: 10.1111/j.1530-0277.1996.tb01079.x. [DOI] [PubMed] [Google Scholar]
- Shiffman S. A cluster-analytic classification of smoking relapse episodes. Addictive behaviors. 1986;11(3):295–307. doi: 10.1016/0306-4603(86)90057-2. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Measuring alcohol consumption. Springer; 1992. Timeline follow-back; pp. 41–72. [Google Scholar]
- Sobell LC, Sobell MB. Alcohol timeline followback (TLFB) users' manual. Toronto: Addiction Research Foundation; 1996. [Google Scholar]
- von der Pahlen B, Santtila P, Johansson A, Varjonen M, Jern P, Witting K, Kenneth Sandnabba N. Do the same genetic and environmental effects underlie the covariation of alcohol dependence, smoking, and aggressive behaviour? Biological psychology. 2008;78(3):269–277. doi: 10.1016/j.biopsycho.2008.03.013. [DOI] [PubMed] [Google Scholar]
- Warner KE, Méndez D. Accuracy and Importance of Projections From a Dynamic Simulation Model of Smoking Prevalence in the United States. American Journal of Public Health. 2012;(0):1–3. doi: 10.2105/AJPH.2012.300771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimmerman RS, Warheit GJ, Ulbrich PM, Auth JB. The relationship between alcohol use and attempts and success at smoking cessation. Addictive Behaviors. 1990;15(3):197–207. doi: 10.1016/0306-4603(90)90063-4. [DOI] [PubMed] [Google Scholar]