SYNOPSIS
Significant progress has been made in the surgical management of breast cancer. Historically, women with invasive breast cancer underwent a Halsted radical mastectomy; morbid procedure removing the breast, underlying muscle and regional lymph nodes. In contemporary practice, the majority of women diagnosed with early stage invasive breast cancer can now be managed with breast conserving therapy to include a segmental mastectomy followed by radiation. Axillary lymph nodes are routinely assessed by sentinel lymph node biopsy. Axillary lymph node dissection is reserved for patients with documented nodal metastasis, however, here too progress has been made as a population of low risk patients has been identified in whom a complete dissection is not required even in the setting of a positive sentinel lymph node. This chapter details the landmark clinical trials that have guided the surgical management of breast cancer.
Keywords: Breast cancer, clinical trials, breast conserving therapy, sentinel lymph node biopsy
INTRODUCTION
Large cooperative group trials have defined surgical management of breast cancer. Until the late 1890s, breast cancer was a fatal disease. William Stewart Halsted challenged that theory by performing aggressive surgery to achieve local control. [1] Termed the Halsted radical mastectomy, the procedure involved removal of the breast, the underlying pectoralis major and minor muscles, and the regional lymph nodes. This extensive resection addressed Halsted’s premise that cancer spread from the breast to the pectoralis muscles and regional lymph nodes first and then to distant sites. By the late 1960s, however, investigators had begun to question this “contiguous spread” model and suggested instead that breast cancer was a systemic disease. [2–5] Around the same time, interest in using chemotherapy for a variety of malignancies increased. Thus, investigators also started to question the need to routinely perform a procedure as morbid as the radical mastectomy. Subsequently, large randomized clinical trials in the United States and Europe demonstrated that breast cancer could be successfully treated with less radical surgery combined with other modalities including systemic chemotherapy, endocrine therapy, and radiation. Advances from these trials resulted in personalized surgical management of breast cancer. This chapter will review the most recently published data from landmark randomized trials that have guided current practices in surgical management of invasive breast cancer.
FROM RADICAL MASTECTOMY TO BREAST CONSERVING THERAPY
National Surgical Adjuvant Breast and Bowel Project B-04: Radical Mastectomy to Total Mastectomy
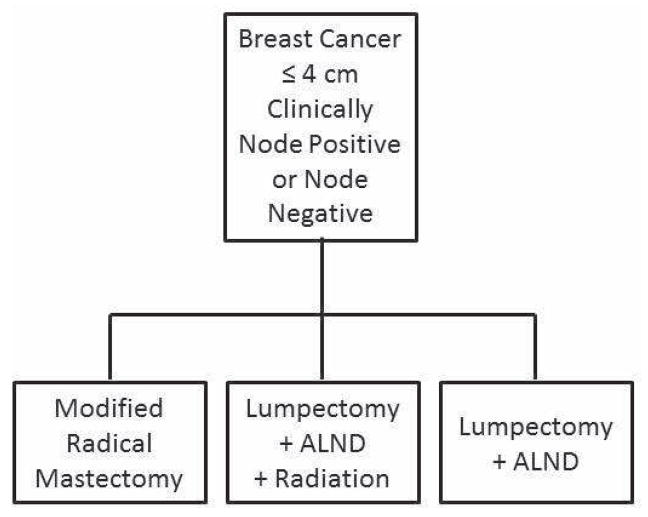
Dissatisfaction with the significant morbidity of radical mastectomy along with new information regarding tumor biology and metastasis led to anecdotal reports of surgeons using less aggressive surgery to treat breast cancer. [2, 6–8] This led investigators from the National Surgical Adjuvant Breast and Bowel Project (NSABP) to conduct the NSABP B-04 trial, which compared radical mastectomy to less extensive surgery. [9] The trial was set up as two parallel trials: one for patients with clinically node-negative disease and one for patients with node-positive disease (Figure 1). Between 1971 and 1974, 1079 patients with clinically node-negative disease were randomized to radical mastectomy (n=362), total mastectomy plus local-regional/axillary radiation (n=352), or total mastectomy alone without axillary treatment (n=365). During the same period, 586 patients with clinically node-positive disease were randomized to radical mastectomy (n=292) or total mastectomy and radiation (n=294). [9] Patients did not receive systemic therapy. The goal was to determine whether patients who received local-regional treatment other than radical mastectomy had similar outcomes to those undergoing radical mastectomy.
Figure 1.
Schema for NSABP B-04 trial.
Initial reports from the NSABP B-04 trial at 3, 5, and 10 years showed no significant differences with respect to disease-free survival (DFS), distant-disease-free survival (DDFS), and overall survival (OS) among the three groups of patients with clinically node-negative disease or the two groups of patients with clinically node-positive disease. [2, 9, 10] The 25-year outcomes from the NSABP B-04 trial reported in 2002 also revealed no significant differences between groups with respect to any endpoint. [11] In the node-negative arm, patients who underwent total mastectomy plus radiation had a lower rate of local-regional recurrence (LRR; 5%) than did those who underwent radical mastectomy (9%) or total mastectomy alone (13%) (p=0.002). In the node-positive arm, the LRR rates were not significantly different: 16% in patients who underwent radical mastectomy versus 14% in patients who underwent total mastectomy plus radiation (p=0.67). When broken down by local versus regional recurrence, the rate of local recurrence was significantly different between those who underwent radical mastectomy (8%) and those who underwent total mastectomy plus radiation (3%); however, no significant differences in regional recurrence rates were found.
Of note, 40% of the patients with clinically node-negative disease who underwent radical mastectomy had lymph node involvement in their surgical specimens. [9] Thus, one can assume that 40% of patients with clinically node-negative disease who underwent total mastectomy also had nodal involvement. However, of the 365 patients with node-negative disease who underwent total mastectomy without radiation, only 68 (19%) subsequently developed nodal disease and underwent axillary lymph node dissection (ALND). [11] The median time from mastectomy to identification of axillary metastases was 15 months (range, 3–135 months), and the majority of cases were identified within 2 years of the initial operation. These patients remained in the total mastectomy cohort for survival analyses, therefore, because there was no significant difference with respect to OS between the arms of the trial, these data suggest that routine ALND for patients with a clinically node negative axilla is unnecessary and omission of this procedure until there is clinically evident disease in the axilla will not have a significant negative impact on OS. This study also did not demonstrate an advantage of adding local-regional radiation to total mastectomy. Most importantly, the trial supported the paradigm shift to less radical surgery for breast cancer.
NSABP B-06: Total Mastectomy versus Breast-Conserving Therapy
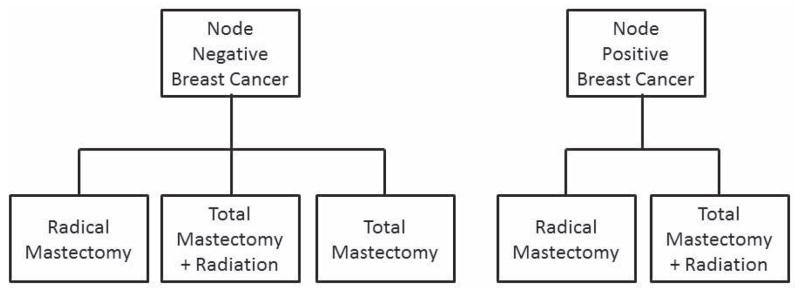
To further minimize the extent of surgery, several investigators evaluated breast-conserving surgery and reported encouraging results in small studies that included patients with small tumors. [12–14] To further evaluate this strategy, NSABP investigators conducted the NSABP B-06 study; a randomized prospective trial comparing lumpectomy and ALND with or without breast irradiation with total mastectomy and ALND (modified radical mastectomy) in patients with tumors 4 cm or less (Figure 2). [15] Patients could enroll regardless of clinical nodal status, and all patients underwent level I and II ALND. Radiation was administered to 50 Gy without a boost to the lumpectomy bed or radiation to the axilla. Patients with positive axillary lymph nodes received adjuvant systemic therapy with fluorouracil and melphalan. The aim of this trial, which enrolled and randomized 2163 patients from 1976 to 1984, was to determine rates of ipsilateral breast cancer recurrence, DFS, DDFS, and OS. Initial reports of the trial at 5, 8, and 12 years included 1843 evaluable patients and showed no significant differences for any endpoint among the groups. [15–17]
Figure 2.
Schema for NSABP B-06 trial. (ALND = axillary lymph node dissection)
The most recent publication from this trial reported 20-year follow-up data, which also showed no significant differences in DFS, DDFS, or OS among groups. [18] They did however identify differences among the three arms with respect to local control. [18] Chest wall recurrences were reported in 10% of patients who underwent mastectomy. The cumulative incidence of ipsilateral breast tumor recurrence (IBTR) in patients with tumor-free margins was 39% in patients who underwent lumpectomy alone and 14% in patients who underwent lumpectomy and radiation (p<0.001). Patients who received radiation had fewer late recurrences; 73% of recurrences in the lumpectomy plus radiation group were within 5 years while 9% occurred after 10 years compared to the lumpectomy-only group in which 40% of the recurrences were within 5 years and 30% occurred after 10 years. Importantly, patients with positive margins in either lumpectomy group (approximately 10% of patients) who subsequently underwent total mastectomy were followed in their respective lumpectomy group for survival outcome analyses. [18] Similarly, per protocol definition, an IBTR after lumpectomy was not considered an event in the DFS analysis because women who underwent total mastectomy were not at risk. Instead, an IBTR after lumpectomy was considered a cosmetic failure, and such patients who subsequently underwent mastectomy continued in their assigned lumpectomy group for data analyses. [18] The NSABP B-06 trial was critical for establishing the concept of breast-conserving therapy (BCT) and confirmed the importance of radiation as a component of such treatment. These results were confirmed by other randomized clinical trials conducted by others, including the group from the Milan Cancer Institute. [19, 20]
More modern series have reported even lower rates of local-regional failure after BCT. We recently reported our experience at The University of Texas MD Anderson Cancer Center with a cohort of 2331 patients who underwent BCT including lumpectomy and whole-breast irradiation (WBI) between 1987 and 2005. After a median follow-up of 8 years, the 5-year LRR-free rate was 97% (95% confidence interval [CI]: 96%–98%), and the 10-year rate was 94% (95% CI: 93%–95%). [21] These results reflect improvements in imaging and pathologic evaluation; expanding indications for adjuvant therapy including systemic chemotherapy and endocrine therapy, which have been shown to decrease LRR rates in the breast; and improvements in systemic agents. An appreciation for the need to obtain a clearly negative margin at the time of surgery has also increased. [22] Although there is no consensus on the optimal margin width, “no ink on tumor” was considered to be a negative margin in the NSABP B-06 trial.
Cancer and Leukemia Group B 9343: Radiation in Women 70 years and Older
Once studies demonstrated the feasibility of BCT, investigators began questioning whether radiation could be safely omitted in selected patients in whom the absolute risk of recurrence would be predicted to be low. One trial that investigated this was the Cancer and Leukemia Group B (CALGB) 9343, conducted between 1994 and 1999. [23, 24] The trial enrolled 636 women 70 years and older who had undergone lumpectomy for stage I, ER-positive breast cancer. A negative surgical margin, defined as no tumor on the inked margin was required. Patients were randomized to receive tamoxifen (n=319) or tamoxifen and radiation (n=317). ALND was discouraged but was performed in approximately 36% of patients in both groups.[23] The primary endpoints were time to local or regional recurrence, frequency of mastectomy for recurrence, DFS, time to distant metastasis, and OS.
Initial results from the study were published in 2004 after a median follow-up of 5 years. [23] The investigators found no significant differences between the groups in the rates of subsequent mastectomy, distant metastases, or OS. The rate of local or regional recurrence was 1% in the tamoxifen plus radiation group and 4% in the tamoxifen alone group, a difference that was statistically significant (p<0.001). In 2005, following the initial report of the CALGB 9343 results, the National Comprehensive Cancer Network (NCCN) amended their guidelines with a footnote that stated “Breast irradiation may be omitted in those 70 years of age or older with ER-positive, clinically node-negative T1 tumors who receive adjuvant hormonal therapy.” [25] Updated data from this trial were presented in 2010. [24] After a median follow-up of 10.5 years, the LRR rate remained significantly different between the two groups: 9% in the tamoxifen alone group and 2% in the tamoxifen plus radiation group. The difference was driven largely by a difference in IBTR: 8% in the tamoxifen alone group and 2% in the tamoxifen plus radiation group. DDFS, breast cancer-specific survival, OS, and the ability to undergo breast-conserving therapy remained comparable between the two groups. On the basis of these findings, the authors concluded that lumpectomy with endocrine therapy and without radiation is an appropriate treatment option for women 70 years or older with node-negative, ER-positive breast cancer.
Summary and Future Directions: Management of the Primary Breast Tumor
Taken together, the randomized clinical trials discussed above have changed the paradigm of the surgical management of primary tumors of women with invasive breast cancer. As a result of these studies, most patients with early-stage breast cancer undergo BCT that includes segmental resection followed by radiation. Because BCT is now well established, ongoing cooperative group trials are attempting to evaluate other modalities for treating the primary tumor and to minimize radiation. There is interest in managing the primary tumor without surgery using one of several described modalities, including percutaneous ablation, radiofrequency ablation, or cryoablation. [26] For example, the American College of Surgeons Oncology Group (ACOSOG) is conducting the Z1072 trial, a phase II study exploring cryoablation for the treatment of invasive breast cancer less than 2 cm. [27] The trial is currently accruing patients, and the estimated completion date is March 2013.
The previously discussed trials describing BCT all evaluated WBI. Because most IBTRs occur near the lumpectomy cavity, investigators have begun exploring other methods of delivering radiation including accelerated partial-breast irradiation (APBI). APBI is associated with several purported benefits, including a shorter interval for treatment completion, the potential for repeat breastconserving surgery when an in-breast event occurs outside the irradiated cavity, and an alternative for women who are reluctant to undergo WBI. APBI is being evaluated in a large trial by the NSABP and RTOG (NSABP B-39/RTOG 0413). [28] The trial will enroll 4300 women with operable breast cancer treated with lumpectomy. Initial eligibility criteria included stage 0 DCIS or stage I or II invasive cancer that was 3 cm or smaller with fewer than three positive axillary lymph nodes. The trial opened in 2005 and after brisk accrual of low-risk patients (women older than 50 years with DCIS or node-negative and ER-positive invasive tumors), was closed to accrual of patients with these favorable characteristics. The trial continues to accrue higher-risk patients.
FROM AXILLARY LYMPH NODE DISSECTION TO SENTINEL LYMPH NODE DISSECTION
Axillary lymph node involvement has long been considered an important prognostic factor in breast cancer. To determine axillary status for staging purposes, to assist with adjuvant treatment recommendations, and to provide regional control, complete ALND was routinely performed. However, ALND is associated with potential morbidity, including lymphedema, shoulder dysfunction, pain, and paresthesias. [29, 30] In addition, in women presenting with clinically node-negative disease, the rate of nodal metastases is only 20–35%. [31–33] Removing healthy lymph nodes renders no benefit; therefore, sentinel lymph node dissection (SLND), a more selective approach to managing the axilla was developed. The concept of the sentinel lymph node (SLN) as the first draining lymph node was popularized in melanoma in the late 1980s and early 1990s.[34, 35] In 1994, Giuliano and colleagues published findings on the feasibility and accuracy of SLND for early-stage breast cancer in 114 patients and reported a 65% identification rate and 96% accuracy.[36] This report led to the design and conduct of larger trials evaluating SLND as a staging procedure for clinically node negative breast cancer.
Sentinel Lymph Node Dissection for Axillary Staging
NSABP B-32
To determine whether SLND renders the same survival benefit and regional control that ALND does but with fewer side effects in patients with clinically node-negative disease, NSABP investigators conducted the NSABP B-32 trial. Between 1999 and 2004, the trial enrolled 5611 patients and randomized them to undergo SLND plus ALND (group one) or SLND with ALND only if the SLN was positive (group two; Figure 3). The primary endpoints were OS, regional control, and morbidity. The secondary endpoints were accuracy and technical success. [37]
Figure 3.
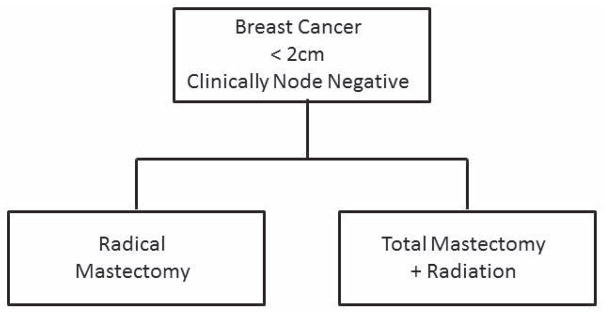
Schema for NSABP B-32 trial.
SLNs were defined as nodes that were radioactive, blue, or hard and highly suspicious for metastatic disease. Radioactive nodes were removed until the count in the axilla was less than 10% of the hottest ex vivo SLN. [31] Pathologic evaluation included sectioning at 2-mm intervals and staining with hematoxylin and eosin (H&E). Routine immunohistochemistry (IHC) was not allowed. The initial publication reported on technical success and accuracy in 5536 patients in whom data were available. [31] A SLN was identified in 5379 (97%). The SLN was positive in 26% of patients in both groups. In group one, the accuracy of SLND was 97%, and the false-negative rate was 9.8%. Factors associated with a higher false-negative rate included tumor location, the type of biopsy performed, and the number of SLNs removed. [31] Patient-reported outcomes and morbidity related to lymphedema, range of motion, sensory deficits, and pain have also been published and for all outcomes, morbidity was greater in patients who underwent ALND. [38, 39]
Data for the primary survival endpoints of the trial were published in 2010. [37] Per protocol, analysis included patients with a pathologically negative SLN in whom follow-up information was available (n=3986). The two groups were well balanced with respect to age, clinical tumor size, and surgical treatment. The use of systemic therapy and radiation was similar between groups. The 5-year Kaplan-Meier estimates for OS were 97% and 95% for groups one and two, respectively, and the 8-year estimates were 92% and 90% respectively (p=0.12). Differences in DFS were also not statistically significant; the 8-year estimates of DFS were 82% in both groups. Rates of regional control were also similar. Eight regional nodal recurrences as first events, including two in the axilla, were reported in group one. Fourteen regional nodal recurrences as first events, including eight in the axilla, were reported in group two. Because the OS, DFS, and regional control rates between the treatment groups were statistically equivalent, the NSABP investigators concluded that when the SLN is negative, SLND alone without further ALND is appropriate for patients with clinically negative lymph nodes.
The findings of the NSABP B-32 trial were confirmed by a single center randomized trial conducted at the European Institute of Oncology. This trial enrolled patients with primary tumors that were 2 cm or smaller who underwent BCT. Patients were randomized to SLND plus ALND (ALND arm; n=257) or SLND and ALND only if the SLN was positive for metastatic disease (SLND arm; n=259). [33, 40, 41] In 2010, the 10-year follow-up data from this trial were published. [41] The ALND and SLND groups were well matched with respect to clinicopathologic characteristics and adjuvant systemic therapy use. After a median follow-up of 102 months, no significant differences in OS were found. Taken together, the NSABP B-32 and EIO trials confirmed that SLND is effective for staging the axilla in patients with clinically node-negative breast cancer and that SLND alone is safe when the SLN is negative.
Role of Completion ALND in the Setting of a Positive SLN
Once SLND was shown to be safe in patients with clinically node-negative disease, omission of ALND in patients with a negative SLN became standard practice. For patients with a positive SLN, most consensus statements, including one from the American Society of Clinical Oncology (ASCO), and NCCN guidelines recommended completion ALND for patients with a positive SLN. [42, 43] However, recalling the results of the NSABP B-04 trial, a study that showed no survival advantage for patients who underwent ALND at the time of their initial surgery, and recognizing improvements in systemic therapy options and radiation delivery, the utility of completion ALND in all patients with a positive SLN was questioned.
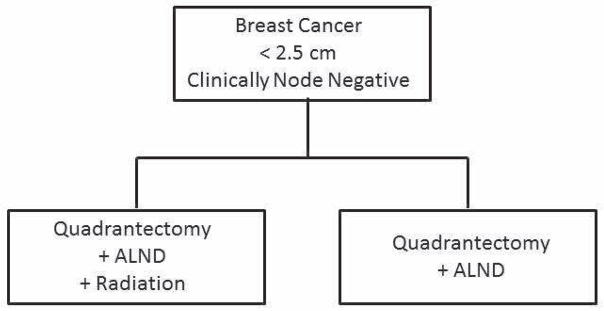
To determine whether all patients with a positive SLN need an ALND, ACOSOG conducted the Z0011 trial which enrolled patients with clinical T1 or T2, N0, M0 breast cancer who underwent BCT and were found to have one or two positive SLNs by H&E evaluation. [44, 45] The patients were randomized to ALND or no further surgery. All patients received WBI (third-field axillary irradiation was not allowed), and recommendations for systemic adjuvant therapy were made at the discretion of the treating oncologist (Figure 4). The primary endpoint was OS and secondary endpoint was DFS. Local-regional control was not a pre-specified endpoint; however, because of concerns that the regional recurrence rates may be high without completion ALND, regional recurrences were monitored.
Figure 4.
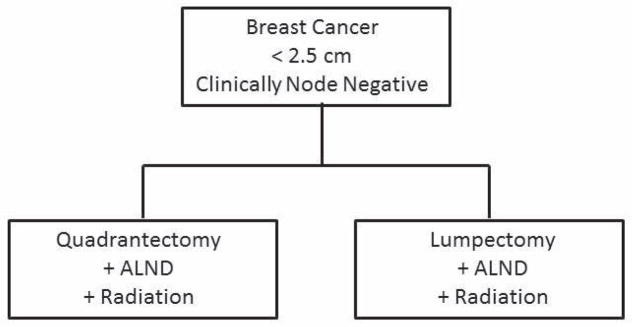
Schema for ACOSOG Z0011 trial.
The trial, which was designed to enroll 1900 patients, began accrual in 1999. Because of slow accrual and a lower than anticipated event rate, the study was closed early in 2004 after 891 patients were randomized; 446 in the SLND alone arm and 445 in the SLND + ALND arm. Clinicopathologic characteristics were similar between the two groups and overall reflected a population of patients with favorable characteristics (Table 1). [45] Micrometastases were identified in the SLN of 38% of patients in the SLND alone arm and in the SLN of 45% of patients in the ALND arm (p=0.05). Additional positive lymph nodes were identified in 27% of patients in the ALND arm.[44] Adjuvant systemic therapy was administered in 97% of patients in the SLND only arm, including chemotherapy in 58% and hormonal therapy in 47%. In the ALND arm, 96% of patients received adjuvant systemic therapy, including chemotherapy in 58% and hormonal therapy in 46%. [44]
Table 1.
Baseline patient and tumor characteristics of patients enrolled on the American College of Surgeons Oncology Group Z0011 trial. (Data from Giuliano AE, et al. Axillary dissection vs no axillary dissection in women with invasive breast cancer and sentinel node metastasis. JAMA 2011;305:569–75.)
| Characteristic | ALND (n=420) | SLND alone (n=436) |
|---|---|---|
|
| ||
| Age in years, median (range) | 56 (24–92) | 54 (25–90) |
|
| ||
| Clinical T stage | ||
| T1 | 284 (68%) | 303 (71%) |
| T2 | 134 (32%) | 126 (29%) |
| missing | 2 | 7 |
|
| ||
| Tumor size, median (range), cm | 1.7 (0.4–7.0) | 1.6 (0.0–5.0) |
|
| ||
| ER positive | 317 (83%) | 324 (83%) |
|
| ||
| LVI | ||
| Present | 129 (41%) | 113 (35%) |
| Absent | 189 (59%) | 208 (65%) |
| Missing | 102 | 115 |
|
| ||
| Grade* | ||
| 1 | 71 (22%) | 81 (26%) |
| 2 | 158 (49%) | 148 (47%) |
| 3 | 94 (29%) | 87 (27%) |
| Missing | 97 | 120 |
|
| ||
| Histology | ||
| Infiltrating ductal | 344 (83%) | 356 (84%) |
| Infiltrating lobular | 27 (6%) | 36 (8.5%) |
| Other | 45 (11%) | 32 (7.5%) |
| Missing | 4 | 12 |
|
| ||
| Lymph node metastases | ||
| 0 | 4 (1%) | 29 (7%) |
| 1 | 199 (58%) | 295 (71%) |
| 2 | 68 (20%) | 76 (18%) |
| 3 | 25 (7%) | 11 (3%) |
| ≥ 4 | 47 (14%) | 4 (1%) |
| Missing | 77 | 21 |
ER = estrogen receptor
LVI = lymphovascular invasion
ALND = axillary lymph node dissection
SLND = sentinel lymph node dissection
Grade was determined using the modified Bloom-Richardson score
After a median follow-up of 6.3 years, only 29 local-regional recurrences were reported in the entire population. The local recurrence rate was 2% in the SLND arm and 4% in the ALND arm. Ipsilateral axillary recurrences were uncommon, occurring in 4 (0.9%) patients in the SLND arm and 2 (0.5%) patients in the ALND arm. [44] The authors found no differences in DFS or OS between the two groups.[45] On the basis of these results, the ACOSOG investigators concluded that routine use of ALND is not justified and may be safely omitted in selected patients with clinically node-negative disease who have one or two positive SLNs. Importantly, the Z0011 trial did not include patients with T3 tumors or patients who had undergone mastectomy, those receiving neoadjuvant chemotherapy, APBI, or WBI administered in the prone position where the low axilla is not treated. Therefore, the ACOSOG investigators have cautioned against broad extrapolation of the data indicating that, in such patients, ALND remains the standard practice when a positive SLN is identified. [45]
When the Z0011 data were published, several questions were raised regarding the trial and whether the results of the study would change practice. [46] The most significant concern was that the planned sample size was not reached. One reason for early closure was that the increased acceptance of screening mammography and improvements in systemic therapy led to an event rate that was lower than anticipated at the time of study design. In addition, the study was designed to demonstrate the non-inferiority of SLND alone for OS with a p value of 0.008. Because the 95% CIs for the HR did not cross the predefined point at which the treatments would not be considered equal, the results would not be expected to change with a larger sample size. Finally, the endpoints of total local-regional recurrences, DFS, and OS all numerically favored the SLN group. [44–46]
The American Society of Breast Surgeons has issued a consensus statement on axillary management that incorporates the findings from the Z0011 trial. [47] Additionally, in the most recent version of its guidelines, the NCCN has changed their algorithm for the management of clinically node-negative disease in patients with a positive SLN to include the category 1 recommendation to consider no further surgery for patients who meet all of the following criteria: T1 or T2 tumor, one or two positive SLNs, undergoing BCT, planned to receive WBI, and did not receive neoadjuvant chemotherapy. [48] Emerging data confirm that the Z0011 data have been practice changing. [46, 49–51]
The International Breast Cancer Study Group (IBCSG 23–01) trial will provide additional data regarding the necessity of ALND in patients with a positive SLN. This trial enrolled patients with clinically node-negative breast cancer and a primary tumor that was 5 cm or smaller who were found to have a SLN micrometastasis that was 2 mm or smaller. Patients were randomized to ALND or no further axillary surgery. Unlike the Z0011 trial, which required patients to undergo BCT, patients in the IBCSG 23-01 trial could undergo mastectomy. The primary endpoint was DFS, and the secondary endpoints were OS and systemic DFS. The trial was designed to accrue 1960 patients. It opened in 2001 and closed early in 2010 after enrolling 934 patients. Similar to the Z0011 trial, reasons for early closure included slow accrual and a lower than anticipated event rate.
Initial results from this trial were presented in 2011. [52] The mean age of enrolled patients was 54 years (range, 26–81 years), and 56% were postmenopausal. The majority (67%) had tumors that were smaller than 2 cm; 89% had tumors that were ER positive, and 74% had grade 1 or 2 disease. Breast-conserving surgery was performed in 75%. In 85% of patients, one or two SLNs were identified. The SLN metastasis was 1.0 mm or smaller in approximately 70% of patients and 1.1–2.0 mm in approximately 30%. After a median follow-up of 49 months, the investigators reported 88 total DFS events, including 66 that were breast cancer related (8 local, 6 regional, 42 distant, and 10 contralateral breast). The 4-year DFS rate was 91%. The first comparison of outcomes between the two groups will be reported after a median follow-up of 5 years. The overall low event rate in the IBCSG 23-01 trial supports the findings from the Z0011 trial suggesting that ALND can be safely omitted in selected patients with clinically node-negative early-stage breast cancer who have a positive SLN.
Sentinel Lymph Node Micrometastases
One purported benefit of SLND is that it allows more rigorous pathologic evaluation of fewer lymph nodes that are at greatest risk for harboring disease. Whereas lymph nodes obtained during ALND are bi-valved and subjected to H&E staining, SLNs routinely undergo serial sectioning with or without IHC. Using these techniques, pathologists can identify small-volume metastases down to the level of isolated tumor cells (ITCs). The clinical relevance of this small-volume disease has been the subject of considerable debate. [53–55]
NSABP B-32
The NSABP B-32 trial, discussed in detail above, provided an opportunity to investigate the clinical significance of occult metastatic disease. Tissue blocks from patients with negative SLNs at the local site were sent for central evaluation. Additional sections deeper in each block were evaluated via H&E staining and IHC to identify occult metastases. [56] For the analysis, patients who underwent SLNB plus ALND and those who underwent SLND alone were grouped together and classified according to whether occult metastasis were detected. The primary outcomes were OS, DFS, and DDFS. [57] Because central analysis results were blinded, no clinical decisions regarding adjuvant therapy were made on the basis of the knowledge of whether occult metastases were present.
Pathologic material was available for 3887 (97%) patients who were determined at local sites to have a negative SLN. Occult metastases were detected in approximately 16%; 11% had ITCs, 4.4% had micrometastases, and 0.4% had macrometastases. The median duration of study enrollment was 95 months. There were significant differences in OS (p=0.03), DFS (p=0.02), and DDFS (p=0.04) between patients with and without occult metastases. The 5-year OS estimates for patients with and without occult metastases were 94.6% and 95.8% respectively. Although occult metastases were associated with a statistically significant detriment in OS, the small degree of absolute difference led investigators to conclude that the additional evaluation of initially negative SLNs using IHC yielded no clinical benefit. [57]
ACOSOG Z0010
The Z0010 trial was designed specifically to evaluate the incidence and significance of SLN and bone marrow micrometastases in patients with early-stage breast cancer who underwent breast-conserving surgery and WBI. [32] Briefly, patients with clinical T1 or T2, N0, M0 breast cancer were enrolled and underwent breast-conserving surgery that included lumpectomy and SLND as well as bilateral anterior iliac crest bone marrow aspiration biopsies (Figure 5). Bone marrow aspiration was initially an optional procedure; however, it was subsequently integrated as a mandatory trial component. Bone marrow aspirates and SLNs that were negative via H&E evaluation at local sites were submitted to a central laboratory for immunocytochemistry (to detect bone marrow micrometasasis) or IHC (to detect SLN micrometastasis). Treating physicians were blinded to the immunochemical status of bone marrow and SLN specimens. The primary endpoint was OS, and the secondary endpoint was DFS.
Figure 5.
Schema for ACOSOG Z0010 trial.
The Z0010 trial began enrolling patients in 1999 with an accrual goal of 5300. The study completed accrual in 2003 with 5538 patients, 5210 of whom were eligible. Of these, 5119 (98%) had a SLN identified, 3904 (76%) of which were negative via H&E staining. Of those that were negative via H&E staining, 3326 (85%) were available to be assessed centrally via IHC, and 349 (11%) of those contained occult metastases. [32] The ages and tumor characteristics of patients with SLNs examined via IHC are shown in Table 2. At a median follow-up of 6.3 years, the investigators found no significant association between IHC-detected occult metastases and OS or DFS. [32] The 5-year OS rates for patients with IHC-positive and negative SLNs were 95% and 96%, respectively (p=0.64). The 5-year DFS rates in these patients were 90% and 92%, respectively (p=.82). IHC-positive SLN metastases were not associated with decreased OS on either univariate or multivariate analysis. Occult metastases were identified in 104 (3%) of 3413 patients who underwent bone marrow biopsy. No concordance between the presence of SLNs and bone marrow occult metastases was found. Bone marrow metastases were associated with decreased OS (unadjusted HR for mortality = 1.94; 95% CI: 1.02 – 3.67, p=0.04); however this association was not significant on multivariate analysis. The only factors found on multivariate analysis to be associated with decreased OS were age greater than 50 years and tumor size larger than 1 cm. Bone marrow metastases were not associated with increased recurrence. [32]
Table 2.
Age and tumor characteristics of patients in the American College of Surgeons Oncology Group Z0010 trial who had a negative SLN via H&E staining that was subsequently evaluated via IHC. (Data from: Giuliano AE, et al. Association of occult metastases in sentinel lymph nodes and bone marrow with survival among women with early-stage invasive breast cancer. JAMA 2011;306:385–93.)
| Variable | Negative via IHC (n=2977) | Positive via IHC (n=349) | P value |
|---|---|---|---|
|
| |||
| Age in years, median (range) | 57 (23–95) | 54 (27–87) | |
|
| |||
| Tumor size, cm | <.001 | ||
| ≤ 1.0 | 1260 (45%) | 101 (31%) | |
| 1.1 – 2.0 | 1202 (43%) | 161 (49%) | |
| > 2.0 | 330 (12%) | 67 (20%) | |
| Missing, number | 185 | 20 | |
|
| |||
| Histology | .002 | ||
| Ductal | 2387 (80%) | 262 (75%) | |
| Lobular | 226 (8%) | 45 (13%) | |
| Both | 77 (2%) | 14 (4%) | |
| Other | 284 (10%) | 28 (8%) | |
| Missing | 3 | 0 | |
|
| |||
| ER status | .3 | ||
| Positive | 2225 (81%) | 268 (84%) | |
| Negative | 518 (19%) | 53 (16%) | |
| Missing | 234 | 28 | |
|
| |||
| LVI | <.001 | ||
| Absent | 1921 (90%) | 217 (83%) | |
| Present | 205 (10%) | 44 (17%) | |
| Missing | 851 | 88 | |
IHC = immunohistochemistry
ER = estrogen receptor
LVI = lymphovascular invasion
The findings from the Z0010 trial therefore support the conclusion that routine use of IHC to detect occult micrometastases in SLNs negative by H&E staining has no clinical benefit. This conclusion is consistent with guidelines from the College of American Pathologists and ASCO, which do not recommend the routine use of IHC for SLN evaluation. [42, 58] Interestingly, the investigators found no correlation between bone marrow metastases and SLN occult metastases, thereby suggesting that the status of the bone marrow may be a distinct prognostic factor. However, the proportion of patients in the ACOSOG Z0010 trial with bone marrow metastases was low; thus, further investigation is needed before consideration can be given to recommending the incorporation of bone marrow aspiration biopsy into practice for patients with early-stage breast cancer.
Summary and Future Directions: Management of the Axilla
Randomized clinical trials have been instrumental in guiding the surgical management of breast cancer to include using SLND to determine the axillary status of patients with clinically node-negative disease. The status of the SLN accurately reflects the status of the entire nodal basin, therefore SLND permits accurate staging of the axilla. For patients with a negative SLN, no further axillary surgery is indicated; therefore, patients without axillary metastases are spared the morbidity of ALND. For patients with a positive SLN, standard practice had been completion ALND; however, data from the recently reported Z0011 trial suggests that ALND may be safely omitted in selected patients undergoing BCT that includes WBI. [44, 45] Data yet to be reported from the IBCSG 23-01 trial will determine whether selected patients who have undergone mastectomy can also avoid ALND after the finding of a micrometastasis in the SLN. Considering early data from that trial and data from the NSABP B-32 and Z0010 trials showing that occult metastases detected via IHC do not have clinical relevance, one would anticipate that the IBCSG 23-01 trial will confirm that ALND can safely be omitted in patients with micrometastasis in their SLN. However, final results of this trial are not yet known and on the basis of currently available data, standard practice for patients with a positive SLN who have undergone mastectomy is completion ALND.
Because ALND is associated with significant morbidity in a substantial proportion of patients, ongoing work is focused on investigating alternative strategies for axillary management in patients with a positive SLN. As has been discussed in detail, the Z0011 data support omitting ALND in a select group of patients undergoing BCT that includes WBI. Although WBI is designed to treat the breast, a portion of the lower axilla is naturally included in the treatment field. Therefore, among patients enrolled in the Z0011 trial, WBI likely had a therapeutic effect on a portion of the axilla, although data documenting the amount of the axilla that may have treated are not currently available. This raises the question however of whether axillary radiation is a less invasive alternative to ALND for patients with a positive SLN. In the NSABP B-04 trial, described in detail above, patients with clinically node-negative disease were randomized to radical mastectomy, total mastectomy, or total mastectomy with axillary radiation; the rate of axillary recurrence in the total mastectomy with axillary radiation arm was 4% after 25 years. [11] To further investigate whether axillary radiation is an appropriate alternative to ALND, investigators from the European Organization for Research and Treatment of Cancer are conducting the AMAROS (After Mapping of the Axilla: Radiotherapy or Surgery?) trial. AMAROS is a phase III study comparing ALND with axillary radiation in clinically node negative patients with tumors smaller than 3 cm who have a positive SLN. The primary objective is to prove that axillary radiation yields equivalent locoregional control and reduced morbidity when compared with ALND. Between 2001 and 2010, the trial accrued 4827 patients. [59] An initial publication from this trial reported the technical outcomes for the first 2000 patients. The SLN identification rate was 97%, and the SLN was positive in 647 (34%), including macrometastases in 409 (63%), micrometastases in 161 (25%), and ITCs in 77 (12%). For patients randomized to undergo ALND, additional nodal involvement was identified in 41% of patients with SLN macrometastases, 18% of patients with micrometastases, and 18% of patients with ITCs. [60] Because the extent of nodal involvement may have implications on adjuvant therapy, the investigators also evaluated the administration of adjuvant therapy in these first 2000 patients. In the ALND and axillary radiation arms, 58% and 61% of patients, respectively, received chemotherapy. Multivariate analysis showed that age, tumor grade, multifocality, and SLN metastasis size significantly affected decisions regarding the use of chemotherapy. Treatment arm was not a significant factor in the decision to administer systemic therapy. [61] Primary outcome data from the trial are not yet available.
Future trials will likely investigate whether there are populations of patients in whom any surgical intervention in the axilla, including SLND, can be safely omitted. A trial randomizing patients to SLND or no surgery seems reasonable in a population of patients with very favorable clinicopathologic characteristics, including postmenopausal women with clinical T1 N0, low to intermediate grade, ER-positive tumors. Because of the overall favorable DFS and OS for this population, such a trial may be difficult to conduct in light of the number of patients and length of follow-up time required. Because decisions regarding the use of adjuvant systemic therapy are now made largely on the basis of characteristics other than the nodal status, including patient age and pathologic features of the primary tumor, another potential trial could enroll patients in whom chemotherapy would be administered regardless of nodal status (e.g., patients with triple-negative breast cancer or HER2-positive breast cancer) and randomize them to SLND or no surgery. Such a trial is currently being discussed within the newly established Alliance for Clinical Trials in Oncology cooperative group (personal communication AE Giuliano and KK Hunt).
CONCLUSION
Randomized clinical trials have been critical in guiding the surgical management of breast cancer. Breast cancer is no longer a fatal disease or one that necessitates radical surgery with significant associated morbidity. Today, largely because of the efforts of surgeons conducting these trials, the majority of patients receive personalized surgical management of their disease, including BCT with lumpectomy, SLND, and radiation.
KEY POINTS.
Large randomized trials have demonstrated no OS difference between mastectomy and breast conserving therapy.
SLND has replaced ALND as the recommended procedure for axillary staging of clinically node negative breast cancer patients.
Select patients with 1–2 positive SLNs undergoing BCT can be spared ALND with no impact on local-regional recurrence or OS.
Current cooperative group trials evaluating new radiation approaches, tumor ablative techniques, and systemic treatments along with the development of assays assessing tumor biology will continue to advance personalized local regional treatment plans for individual patients.
Acknowledgments
Funding support: This research is supported in part by the National Institutes of Health through MD Anderson's Cancer Center Support Grant CA016672.
The authors acknowledge that this article only highlights notable trials that have guided the surgical management of breast cancer. Other trials have contributed to the advancement of breast surgical care however due to space limitations, are not included in this review.
Footnotes
Financial Disclosures: The authors have nothing to disclose
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errorsmaybe discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Dalliah M. Black, Email: dmblack@mdanderson.org.
Elizabeth A. Mittendorf, Email: eamitten@mdanderson.org.
References
- 1.Halsted WS. I. A Clinical and Histological Study of certain Adenocarcinomata of the Breast: and a Brief Consideration of the Supraclavicular Operation and of the Results of Operations for Cancer of the Breast from 1889 to 1898 at the Johns Hopkins Hospital. Ann Surg. 1898;28:557–76. [PMC free article] [PubMed] [Google Scholar]
- 2.Fisher B, Redmond C, Fisher ER. The contribution of recent NSABP clinical trials of primary breast cancer therapy to an understanding of tumor biology--an overview of findings. Cancer. 1980;46:1009–25. doi: 10.1002/1097-0142(19800815)46:4+<1009::aid-cncr2820461326>3.0.co;2-h. [DOI] [PubMed] [Google Scholar]
- 3.Fisher B, Fisher ER. Transmigration of lymph nodes by tumor cells. Science. 1966;152:1397–8. doi: 10.1126/science.152.3727.1397. [DOI] [PubMed] [Google Scholar]
- 4.Fisher B, Fisher ER. Experimental evidence in support of the dormant tumor cell. Science. 1959;130:918–9. doi: 10.1126/science.130.3380.918. [DOI] [PubMed] [Google Scholar]
- 5.Fisher B, Fisher ER. The interrelationship of hematogenous and lymphatic tumor cell dissemination. Surg Gynecol Obstet. 1966;122:791–8. [PubMed] [Google Scholar]
- 6.McWhirter R. The value of simple mastectomy and radiotherapy in the treatment of cancer of the breast. Br J Radiol. 1948;21:599–610. doi: 10.1259/0007-1285-21-252-599. [DOI] [PubMed] [Google Scholar]
- 7.Handley RS. The Technic and Results of Conservative Radical Mastectomy (Patey's Operation) Prog Clin Cancer. 1965;10:462–70. [PubMed] [Google Scholar]
- 8.Fisher B. Laboratory and clinical research in breast cancer--a personal adventure: the David A. Karnofsky memorial lecture. Cancer Res. 1980;40:3863–74. [PubMed] [Google Scholar]
- 9.Fisher B, Montague E, Redmond C, et al. Comparison of radical mastectomy with alternative treatments for primary breast cancer. A first report of results from a prospective randomized clinical trial. Cancer. 1977;39:2827–39. doi: 10.1002/1097-0142(197706)39:6<2827::aid-cncr2820390671>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- 10.Fisher B, Redmond C, Fisher ER, et al. Ten-year results of a randomized clinical trial comparing radical mastectomy and total mastectomy with or without radiation. N Engl J Med. 1985;312:674–81. doi: 10.1056/NEJM198503143121102. [DOI] [PubMed] [Google Scholar]
- 11.Fisher B, Jeong JH, Anderson S, et al. Twenty-five-year follow-up of a randomized trial comparing radical mastectomy, total mastectomy, and total mastectomy followed by irradiation. N Engl J Med. 2002;347:567–75. doi: 10.1056/NEJMoa020128. [DOI] [PubMed] [Google Scholar]
- 12.Crile G., Jr Treatment of Breast Cancer by Local Excision. Am J Surg. 1965;109:400–3. doi: 10.1016/s0002-9610(65)80161-1. [DOI] [PubMed] [Google Scholar]
- 13.Montague ED, Gutierrez AE, Barker JL, et al. Conservation surgery and irradiation for the treatment of favorable breast cancer. Cancer. 1979;43:1058–61. doi: 10.1002/1097-0142(197903)43:3<1058::aid-cncr2820430341>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- 14.Peters MV. Carcinoma of the breast. Stage II--radiation range. Wedge resection and irradiation. An effective treatment in early breast cancer. JAMA. 1967;200:134–5. doi: 10.1001/jama.200.2.134. [DOI] [PubMed] [Google Scholar]
- 15.Fisher B, Bauer M, Margolese R, et al. Five-year results of a randomized clinical trial comparing total mastectomy and segmental mastectomy with or without radiation in the treatment of breast cancer. N Engl J Med. 1985;312:665–73. doi: 10.1056/NEJM198503143121101. [DOI] [PubMed] [Google Scholar]
- 16.Fisher B, Redmond C, Poisson R, et al. Eight-year results of a randomized clinical trial comparing total mastectomy and lumpectomy with or without irradiation in the treatment of breast cancer. N Engl J Med. 1989;320:822–8. doi: 10.1056/NEJM198903303201302. [DOI] [PubMed] [Google Scholar]
- 17.Fisher B, Anderson S, Redmond CK, et al. Reanalysis and results after 12 years of follow-up in a randomized clinical trial comparing total mastectomy with lumpectomy with or without irradiation in the treatment of breast cancer. N Engl J Med. 1995;333:1456–61. doi: 10.1056/NEJM199511303332203. [DOI] [PubMed] [Google Scholar]
- 18.Fisher B, Anderson S, Bryant J, et al. Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. N Engl J Med. 2002;347:1233–41. doi: 10.1056/NEJMoa022152. [DOI] [PubMed] [Google Scholar]
- 19.Veronesi U, Cascinelli N, Mariani L, et al. Twenty-year follow-up of a randomized study comparing breast-conserving surgery with radical mastectomy for early breast cancer. N Engl J Med. 2002;347:1227–32. doi: 10.1056/NEJMoa020989. [DOI] [PubMed] [Google Scholar]
- 20.Effects of radiotherapy and surgery in early breast cancer. An overview of the randomized trials. Early Breast Cancer Trialists' Collaborative Group. N Engl J Med. 1995;333:1444–55. doi: 10.1056/NEJM199511303332202. [DOI] [PubMed] [Google Scholar]
- 21.Mittendorf EA, Buchholz TA, Tucker SL, Meric-Bernstam F, Kuerer HM, Gonzalez-Angulo AM, Bedrosian I, Babiera GV, Hoffman KE, Yi M, Ros MI, Hortobagyi GN, Hunt KK. Impact of chemotherapy sequencing on local-regional failure risk in breast cancer patients undergoing breast conserving therapy. Ann Surg. 2012 doi: 10.1097/SLA.0b013e3182805c4a. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Houssami N, Macaskill P, Marinovich ML, et al. Meta-analysis of the impact of surgical margins on local recurrence in women with early-stage invasive breast cancer treated with breast-conserving therapy. Eur J Cancer. 2010;46:3219–32. doi: 10.1016/j.ejca.2010.07.043. [DOI] [PubMed] [Google Scholar]
- 23.Hughes KS, Schnaper LA, Berry D, et al. Lumpectomy plus tamoxifen with or without irradiation in women 70 years of age or older with early breast cancer. N Engl J Med. 2004;351:971–7. doi: 10.1056/NEJMoa040587. [DOI] [PubMed] [Google Scholar]
- 24.Hughes KS, Schnaper LA, Cirrincione C, et al. Lumpectomy plus tamoxifen with or without irradiation in women age 70 or older with early breast cancer. J Clin Oncol. 2010;28:15s. doi: 10.1200/JCO.2012.45.2615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Network NCC. Clinical Practice Guidelines in Oncology: Breast. 2005 [Google Scholar]
- 26.Mamounas E, Wickerham DL. Kuerer's Textbook of Breast Surgical Oncology. In: Kuerer HM, editor. The NSABP Experience. 1. United States: McGraw-Hill; 2010. p. 627. [Google Scholar]
- 27.National Institutes of Health. Cryoablation Therapy in Treating Patients With Invasive Ductal Breast Cancer. 2012 http://www.clinicaltrials.gov/ct2/show/NCT00723294.
- 28.National Institutes of Health. Radiation Therapy in Treating Women Who Have Undergone Surgery For Ductal Carcinoma In Situ or Stage I or Stage II Breast Cancer. 2012 http://www.clinicaltrials.gov/ct2/show/NCT00103181?term=NCT00103181&rank=1.
- 29.Fleissig A, Fallowfield LJ, Langridge CI, et al. Post-operative arm morbidity and quality of life. Results of the ALMANAC randomised trial comparing sentinel node biopsy with standard axillary treatment in the management of patients with early breast cancer. Breast Cancer Res Treat. 2006;95:279–93. doi: 10.1007/s10549-005-9025-7. [DOI] [PubMed] [Google Scholar]
- 30.Lucci A, McCall LM, Beitsch PD, et al. Surgical complications associated with sentinel lymph node dissection (SLND) plus axillary lymph node dissection compared with SLND alone in the American College of Surgeons Oncology Group Trial Z0011. J Clin Oncol. 2007;25:3657–63. doi: 10.1200/JCO.2006.07.4062. [DOI] [PubMed] [Google Scholar]
- 31.Krag DN, Anderson SJ, Julian TB, et al. Technical outcomes of sentinel-lymph-node resection and conventional axillary-lymph-node dissection in patients with clinically node-negative breast cancer: results from the NSABP B-32 randomised phase III trial. Lancet Oncol. 2007;8:881–8. doi: 10.1016/S1470-2045(07)70278-4. [DOI] [PubMed] [Google Scholar]
- 32.Giuliano AE, Hawes D, Ballman KV, et al. Association of occult metastases in sentinel lymph nodes and bone marrow with survival among women with early-stage invasive breast cancer. JAMA. 2011;306:385–93. doi: 10.1001/jama.2011.1034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Veronesi U, Paganelli G, Viale G, et al. A randomized comparison of sentinel-node biopsy with routine axillary dissection in breast cancer. N Engl J Med. 2003;349:546–53. doi: 10.1056/NEJMoa012782. [DOI] [PubMed] [Google Scholar]
- 34.Cabanas RM. An approach for the treatment of penile carcinoma. Cancer. 1977;39:456–66. doi: 10.1002/1097-0142(197702)39:2<456::aid-cncr2820390214>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- 35.Morton DL, Wen DR, Wong JH, et al. Technical details of intraoperative lymphatic mapping for early stage melanoma. Arch Surg. 1992;127:392–9. doi: 10.1001/archsurg.1992.01420040034005. [DOI] [PubMed] [Google Scholar]
- 36.Giuliano AE, Kirgan DM, Guenther JM, et al. Lymphatic mapping and sentinel lymphadenectomy for breast cancer. Ann Surg. 1994;220:391–8. doi: 10.1097/00000658-199409000-00015. discussion 98–401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Krag DN, Anderson SJ, Julian TB, et al. Sentinel-lymph-node resection compared with conventional axillary-lymph-node dissection in clinically node-negative patients with breast cancer: overall survival findings from the NSABP B-32 randomised phase 3 trial. Lancet Oncol. 2010;11:927–33. doi: 10.1016/S1470-2045(10)70207-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ashikaga T, Krag DN, Land SR, et al. Morbidity results from the NSABP B-32 trial comparing sentinel lymph node dissection versus axillary dissection. J Surg Oncol. 2010;102:111–8. doi: 10.1002/jso.21535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Land SR, Kopec JA, Julian TB, et al. Patient-reported outcomes in sentinel node-negative adjuvant breast cancer patients receiving sentinel-node biopsy or axillary dissection: National Surgical Adjuvant Breast and Bowel Project phase III protocol B-32. J Clin Oncol. 2010;28:3929–36. doi: 10.1200/JCO.2010.28.2491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Veronesi U, Paganelli G, Viale G, et al. Sentinel-lymph-node biopsy as a staging procedure in breast cancer: update of a randomised controlled study. Lancet Oncol. 2006;7:983–90. doi: 10.1016/S1470-2045(06)70947-0. [DOI] [PubMed] [Google Scholar]
- 41.Veronesi U, Viale G, Paganelli G, et al. Sentinel lymph node biopsy in breast cancer: ten-year results of a randomized controlled study. Ann Surg. 2010;251:595–600. doi: 10.1097/SLA.0b013e3181c0e92a. [DOI] [PubMed] [Google Scholar]
- 42.Lyman GH, Giuliano AE, Somerfield MR, et al. American Society of Clinical Oncology guideline recommendations for sentinel lymph node biopsy in early-stage breast cancer. J Clin Oncol. 2005;23:7703–20. doi: 10.1200/JCO.2005.08.001. [DOI] [PubMed] [Google Scholar]
- 43.National Comprehensive Cancer Network. Clinical Practice Guidelines in Oncology: Breast. 2008 Version 2. [Google Scholar]
- 44.Giuliano AE, McCall L, Beitsch P, et al. Locoregional recurrence after sentinel lymph node dissection with or without axillary dissection in patients with sentinel lymph node metastases: the American College of Surgeons Oncology Group Z0011 randomized trial. Ann Surg. 2010;252:426–32. doi: 10.1097/SLA.0b013e3181f08f32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Giuliano AE, Hunt KK, Ballman KV, et al. Axillary dissection vs no axillary dissection in women with invasive breast cancer and sentinel node metastasis: a randomized clinical trial. JAMA. 2011;305:569–75. doi: 10.1001/jama.2011.90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Morrow M, Giuliano AE. To cut is to cure: can we really apply Z11 in practice? Ann Surg Oncol. 2011;18:2413–5. doi: 10.1245/s10434-011-1857-2. [DOI] [PubMed] [Google Scholar]
- 47.American Society of Breast Surgeons. Position Statement on Management of the Axilla In Patients with Invasive Breast Cancer. 2012 www.breastsurgeons.org.
- 48.National Comprehensive Cancer Network. Clinical Practice Guidelines in Oncology: Breast. 2012;12 doi: 10.6004/jnccn.2003.0016. [DOI] [PubMed] [Google Scholar]
- 49.Caudle AS, Hunt KK, Kuerer HM, et al. Multidisciplinary considerations in the implementation of the findings from the American College of Surgeons Oncology Group (ACOSOG) Z0011 study: a practice-changing trial. Ann Surg Oncol. 2011;18:2407–12. doi: 10.1245/s10434-011-1593-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Gainer SMHK, Beitsch P. Changing behavior in clinical practice in response to the ACOSOG Z0011 trial: A survey of the American Society of Breast Surgeons. Ann Surg Oncol. 2012 Jul 21; doi: 10.1245/s10434-012-2523-z. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 51.Caudle AS, Hunt KK, Tucker SL, et al. American College of Surgeons (ACOSOG) Z0011: Impact on surgeon practice patterns. Ann Surg Oncol. 2012 Jul 31; doi: 10.1245/s10434-012-2531-z. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Galimberti VCB, Zurrida S, Viale G, Luini A, Veronesi P, Baratella P, Chifu C, Sargenti M, Intra M, Gentilini O, Massarut S, Garbay J-R, Zgajnar J, Galatius H, Recalcati A, Littlejohn D, Banert M, Price KN, Goldhirsch A, Gelber RD, Veronesi U International Breast Cancer Study Group Trial 23- 01 Investigators. Update of International Breast Cnacer Study Group Trial 23-01 to compare axillary dissection versus no axillary dissection in patients with clinically node negative breast cancer and micrometastases in the sentinel node. Cancer Res. 2011;71:102s. [Google Scholar]
- 53.Dowlatshahi K, Fan M, Snider HC, et al. Lymph node micrometastases from breast carcinoma: reviewing the dilemma. Cancer. 1997;80:1188–97. doi: 10.1002/(sici)1097-0142(19971001)80:7<1188::aid-cncr2>3.0.co;2-h. [DOI] [PubMed] [Google Scholar]
- 54.de Boer M, van Dijck JA, Bult P, et al. Breast cancer prognosis and occult lymph node metastases, isolated tumor cells, and micrometastases. J Natl Cancer Inst. 2010;102:410–25. doi: 10.1093/jnci/djq008. [DOI] [PubMed] [Google Scholar]
- 55.Weaver DL. Sentinel lymph nodes and breast carcinoma: which micrometastases are clinically significant? Am J Surg Pathol. 2003;27:842–5. doi: 10.1097/00000478-200306000-00018. [DOI] [PubMed] [Google Scholar]
- 56.Weaver DL, Le UP, Dupuis SL, et al. Metastasis detection in sentinel lymph nodes: comparison of a limited widely spaced (NSABP protocol B-32) and a comprehensive narrowly spaced paraffin block sectioning strategy. Am J Surg Pathol. 2009;33:1583–9. doi: 10.1097/PAS.0b013e3181b274e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Weaver DL, Ashikaga T, Krag DN, et al. Effect of occult metastases on survival in node-negative breast cancer. N Engl J Med. 2011;364:412–21. doi: 10.1056/NEJMoa1008108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Fitzgibbons PL, Page DL, Weaver D, et al. Prognostic factors in breast cancer. College of American Pathologists Consensus Statement 1999. Arch Pathol Lab Med. 2000;124:966–78. doi: 10.5858/2000-124-0966-PFIBC. [DOI] [PubMed] [Google Scholar]
- 59.EORTC 10981-22023 AMAROS trial website. Cancer E O f R a T o. 2010 http://research.nki.nl/amaros/
- 60.Straver ME, Meijnen P, van Tienhoven G, et al. Sentinel node identification rate and nodal involvement in the EORTC 10981-22023 AMAROS trial. Ann Surg Oncol. 2010;17:1854–61. doi: 10.1245/s10434-010-0945-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Straver ME, Meijnen P, van Tienhoven G, et al. Role of axillary clearance after a tumor-positive sentinel node in the administration of adjuvant therapy in early breast cancer. J Clin Oncol. 2010;28:731–7. doi: 10.1200/JCO.2008.21.7554. [DOI] [PMC free article] [PubMed] [Google Scholar]