Abstract
Objectives
To estimate the number of men who have sex with men and women who are HIV-positive in the United States, and to compare HIV prevalence rates between men who have sex with men and women, men who have sex with men only, and men who have sex with women exclusively.
Methods
Following PRISMA guidelines, we conducted a systematic review and meta-analysis of reports referencing HIV prevalence and men who have sex with men and women. We searched PubMed and Ovid PsycINFO for peer-reviewed, U.S.-based articles reporting on HIV prevalence among men who have sex with men and women. We conducted event rate, effect size, moderation and sensitivity analyses.
Results
We estimate that 1.0% of U.S. males are bisexually-behaving, and that 121,800 bisexually-behaving men are HIV-positive. Men who have sex with men and women are less than half as likely to be HIV-positive as men who have sex with men only (16.9% vs. 33.3%; OR = 0.41, 95% CI: 0.31, 0.54), but more than five times as likely to be HIV-positive as men who have sex with women exclusively (18.3% vs. 3.5%; OR = 5.71, 95% CI: 3.47, 9.39). They are less likely to engage in unprotected receptive anal intercourse than men who have sex with men only (15.9% vs. 35.0%; OR = 0.36, 95% CI: 0.28, 0.46). Men who have sex with men and women in samples with high racial/ethnic minority proportions had significantly higher HIV prevalence than their counterparts in low racial/ethnic minority samples.
Conclusions
This represents the first meta-analysis of HIV prevalence in the U.S. between men who have sex with men and women and men who have sex with men only. Data collection, research, and HIV prevention and care delivery specifically tailored to men who have sex with men and women are necessary to better quantify and ameliorate this population’s HIV burden.
Introduction
Since the beginning of the epidemic, HIV transmission researchers have suggested that men who have sex with men and women (MSMW) are integral viral bridges, responsible for the spread of HIV and other sexually transmitted infections (STI) from a discrete population – men who have sex with men (MSM) – to the general population of heterosexuals [1]–[4]. Studies have indicated that a substantial proportion of HIV/AIDS diagnoses among American women may be attributable to bisexually-behaving male partners, though estimates are widely varied, ranging from one percent to 18% [5]–[7]. Others have calculated that MSMW pose high secondary HIV transmission risks; that sexual transmission of HIV from MSMW may especially elevate HIV prevalence among Black heterosexual women; and that MSMW increase the breadth and density of socio-sexual networks, potentiating the spread of HIV across communities [4], [8]–[11].
Nationally representative population-based surveys have consistently estimated that past-year MSMW comprise 0.3% to 1.6% of U.S. males [12]–[15]. The composition of MSMW in these surveys is somewhat less than the proportion of men who have sex with men only (MSMO), albeit variable according to length of recall window of bisexual behavior: looking through five-year windows, estimated proportions of these two distinct groups of MSM roughly equalize [14], [15]. Researchers have recently estimated that past-year MSM comprise 2.9% of the U.S. male population, and that 580,000 U.S. MSM are living with HIV [16], [17]. To date, however, estimates of HIV infection rates among MSMW are unavailable via the HIV/AIDS Surveillance System, which does not distinguish among MSM, although current federally-promoted HIV Counseling and Testing forms functionally collect bisexual behavior data. Meaningful national estimates of MSMW-specific HIV/AIDS transmission and acquisition are subject to significant recall bias limitations when reliant on secondhand information: knowledge of male partners’ bisexuality may be limited and, therefore, uncertainly reported [6], [18]–[20]. Few studies have attempted to model the number and proportion of HIV acquisitions and transmissions attributable to MSMW via sex with male and female partners. Press accounts sensationalizing bisexual men’s risk to women have, therefore, been under-informed [21]–[25].
To estimate the number of HIV infections among MSMW, it is necessary to estimate the proportion of MSMW in the population and either the proportion of MSMW among HIV- positive MSM or the HIV prevalence of MSMW. To calculate these estimates, we elected to conduct a systematic review and comprehensive meta-analysis. We undertook to answer the following research questions: First, do MSMW in the United States have significantly lower HIV prevalence than men who have sex with men only (MSMO)? Second, do MSMW in the United States have significantly higher HIV prevalence than men who have sex with women exclusively (MSWE)? Third, what moderating factors among MSMW in the United States significantly affect their HIV prevalence effect size compared with MSMO? Fourth, what is the proportion of MSM engaged in bisexual behavior in studies that have assessed HIV prevalence among males, and what factors moderate this? Fifth, what is the proportion of HIV-positive MSMW among HIV-positive MSM, and what factors moderate this? Finally, do MSMW engage in risky sexual behavior in different proportions than MSMO and MSWE that might help explain HIV prevalence effect size differences between these populations? This review estimates comparative rates of HIV infection among males in the United States by gender status of sexual partners and, coincidentally, rates of bisexual behavior and HIV risk behavior among males in the United States recruited into research assessing HIV prevalence.
Methods
Search Strategy
This systematic review and meta-analysis adheres to guidelines established by PRISMA [26]. Systematic literature searches were implemented to identify reports of HIV prevalence among MSMW in the United States. First, in August 2012, two doctoral-level researchers and a health sciences librarian conducted a search of PubMed (January 1946– August 2012). This initial search contained controlled vocabulary terms and free text words representing the concepts of bisexuality and HIV, and search results were limited to English-language journal articles. A revised and more comprehensive PubMed search (January 1946– October 2012) was subsequently developed and completed in October 2012 (Appendix S1). As with the initial search, this final PubMed search was limited to English-language journals.
In addition to PubMed, we searched Ovid PsycINFO (January 1967– October 2012). The PubMed final search string was translated by the health sciences librarian for use in PsycINFO, and the translated search contained both controlled vocabulary and free text terms representing bisexuality and HIV. Finally, articles that presented findings on MSMW and the health conditions of interest were explored for references; citations that met our criteria were then explored for their own references, until no new studies were found meeting our criteria. Articles and reports were then analyzed to see whether findings were presented for MSMW. Studies were included in this review if they were peer-reviewed; published in English; and provided quantitative data on HIV prevalence among behaviorally-identified MSMW in the United States. Studies not meeting these criteria (for instance, those that reported data only for bisexually-identified males or only for AIDS cases) were excluded.
Data Extraction/coding
Bisexuality was operationalized using a definition of male bisexual behavior over any timeframe (behavior recall window) assessed by researchers. Two doctoral-level reviewers independently coded for the following variables: lead author; publication date; dates of data collection; location of data collection; target population of study; sample characteristics; comparison groups (MSMO and/or MSWE); sampling procedures; recall window of bisexual behavior; basis for HIV assessment; numbers of group members who were assessed in each study; numerators and denominators or effect sizes of members of each of the three sexual behavior groups assessed for HIV, STI infection, and HIV risk behavior; and whether each study contained race/ethnicity subgroup data by sexual behavior group in samples as a whole and for each outcome domain. Denominators for HIV testing excluded those whose results were indeterminate/inconclusive/unknown. Disagreements that occurred between researchers during data extraction and coding were resolved through discussion.
When multiple articles based on the same study were identified, the most comprehensive study was chosen for meta-analytic inclusion. When a single study presented data for more than one sample (i.e. cross-sectional HIV testing data in different years), we considered it as more than one study. Codes were conceived of as fitting one of four categories: 1) predictor variables (gender of sexual partners); 2) outcome variables (prevalence of HIV infection; prevalence of bisexual behavior; prevalence of STI infection; prevalence of sexual risk behavior); 3) potential moderator variables (recall window of bisexual behavior; study location; sampling procedure; target population; HIV test basis); and 4) effect size data. Moderators were later dichotomized according to whether they met parameters for target population (more than 90% of participants were Black and/or Latino); sampling strategy (probability-based); data collection date (2000 or after); HIV test basis (serological); recall window for bisexual behavior (one year or more); and location (whether recruitment was conducted in one of the 12-highest HIV/AIDS prevalence metropolitan statistical areas, as defined by CDC) [27]. Additional codes were developed to capture the rates and numbers of total MSM (MSMW+MSMO) and HIV-positive MSM in each study.
Analytic Approach
We conducted meta-analyses according to established methods, using NIH-supported software [28], [29]. Four primary meta-analyses were then conducted: (1) comparing HIV prevalence between MSMW, MSMO, and MSWE; (2) comparing sexual risk behavior between MSMO, MSMW, and MSWE; (3) assessing moderators of HIV prevalence within MSMW and within MSMO; and (4) assessing moderators of bisexual behavior and HIV prevalence within MSM. For between-group meta-analyses, odds ratios were used as principal summary measures. For within-group meta-analyses, event rates were used as principal summary measures. Differences in HIV prevalence and bisexual behavior might vary substantially due to methodological issues that could serve to increase heterogeneity and influence pooled outcomes. We assessed heterogeneity by calculating a Q statistic to evaluate how much between-study heterogeneity was due to chance. We used mixed effects models to test differences in pooled prevalence estimates, employing a fixed effect approach across subgroups and a random effects model within subgroups. Weighted mean prevalence (event rates) for outcomes were estimated by computing weighted means, assigning weights to each study that were the inverse of that study’s variance plus an estimate of the variance between studies to account for differing sampling methodologies [28]. For each comparative meta-analytic domain, we conducted sensitivity analyses examining the effect of outliers, using an approach that compared the weighted mean percentage of HIV prevalence between groups with estimates obtained after iterations using k - 1 findings, where k is equal to the number of studies (i.e., removing a finding and re-calculating the weighted mean percentage; then, repeating that process until each finding was separately removed and results re-calculated). To investigate potential publication bias, we utilized Egger’s regression test and examined the symmetry of funnel plots for each comparative meta-analytic domain. For our analysis comparing HIV prevalence between MSMO and MSMW, we conducted an Orwin’s fail-safe n test to estimate how many additional studies would need to be included make effect sizes insignificant.
Finally, we used event rates of HIV prevalence within MSMW, bisexual behavior within MSM, and HIV-positive MSMW within HIV-positive MSM, and paired them with HIV/AIDS surveillance data, standard estimates of proportions of MSM in the United States, and U.S. Census data to estimate population sizes of total MSMW and HIV-positive MSMW, adapting an approach developed by researchers at the Centers for Disease Control and Prevention (CDC) [16].
Results
Search Results
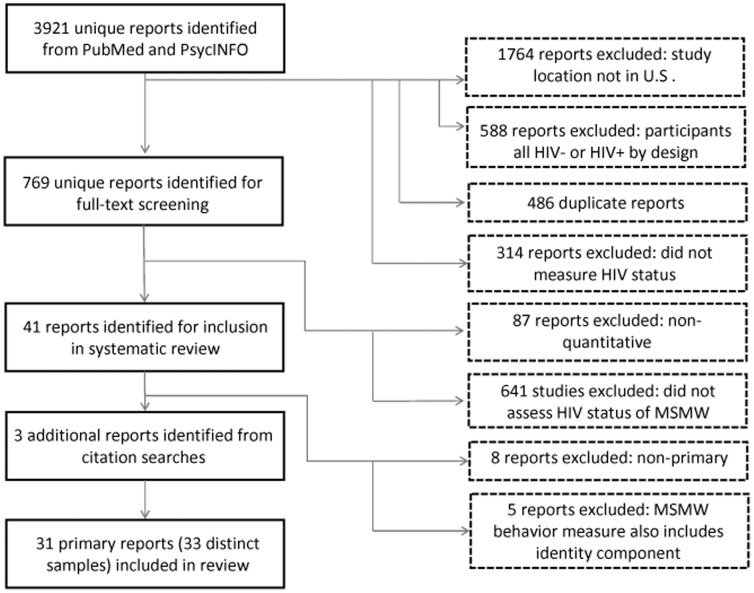
3921 unique reports were initially identified in PubMed and PsycINFO, of which 486 were duplicative. 1764 reports were excluded because they reported on studies outside of the United States. 588 studies were excluded because participants were all HIV negative or HIV-positive by design. 314 reports were excluded because they did not measure HIV status. The 769 reports remaining were subjected to full-text reviews: of these, 87 were excluded because they reflected only qualitative research; and 641 were excluded because they did not report on HIV prevalence among MSMW. Of 41 remaining studies, eight were non-primary reports; and five studies conflated bisexual behavior and identity in a single measure for bisexual males or were ambiguous about their sexuality grouping criteria. Three additional reports were identified through citation searches. A total of 31 unique reports were included in our systematic review and meta-analysis (see Figure 1) [30]–[60].
Figure 1. Flow diagram of included and excluded records.
Two of these articles reported on data collected in different samples and years; these articles were disaggregated. The final dataset for this meta-analysis thus contained 33 distinct samples. Table 1 shows the study characteristics of each of these samples.
Table 1. Study characteristics of 33 samples included in meta-analysis*.
| Lead author, Date | Location | Target population | Recall window | Sampling strategy | MSMW (n) | % MSMW | Age | Race | HIV test basis | % HIV+, MSMW | % HIV+, MSMO | % HIV+, MSWE |
| Bacon, 2006 | San Francisco, CA | YMSM-IDU | D | 3 | 206 | 90.8 | Median age: 23 (16–29). | 80% white, 20% nonwhite. | 1 | 8.7 | 42.9 | – |
| Bowers, 2011 | Los Angeles, CA | Substance-using MSM | n/a | 3 | 310 | 43.5 | MSMW mean age :34.8 | Among MSMW: 51% white, 26% Black, 9% Hispanic, 14% other. | 0 | 18.5 | 39.2 | – |
| Cassels, 2010 | 7 cities | American Indian/Alaskan Native LGBT | D | 2, 3 | 32 | 19.3 | Median age: 45–67. | 100% American Indian/Alaskan Native | 0 | 23.1 | 37.8 | – |
| Catania, 2001 | SF, NY, LA, Chi. | MSM | D | 5 | 385 | 14.7 | Median age: 30–39. | 79% white, 4% AA, 10% Hispanic, 4% Asian, 3% Native American, <1% other. | 1** | 10.1 | 19 | 0 |
| Flores, 2009 | 13 cities | YMSM | A | 1 | 1494 | 14.5 | Mean age: 21.3 | 28% Black, 10% A/PI, 37% Latino, 22% White. | 0 | 0.6 | 1.6 | – |
| Fuller, 2005 | New York, NY | Substance-using MSM | A | 3 | 47 | 49.5 | Median age: 28 (18–40). | 44% Hispanic, 46% Black, 10% white/other. | 1 | 4.3 | 45.8 | – |
| German, 2011a | Baltimore, MD | MSM | B | 1 | 216 | 33.5 | Median age 34 (18–69). | 31% white, 62% African American, 6% other. | 1 | 31.5 | 40.8 | – |
| German, 2011b | Baltimore, MD | MSM | B | 1 | 109 | 24.3 | Median age 30 (18–72). | 23%% white, 71% African American, 5% other. | 1 | 30.3 | 39.8 | – |
| Gorbach, 2009 | Los Angeles, CA | Substance user or MSM | A | 2 | 461 | 51.7 | Mean age: 42.7. | 19.1% white, 52.8% Black, 22% Hispanic. | 1 | 11.9 | 64 | 4.3 |
| Kalichman, 1998 | Not provided | MSM | B | 3 | 146 | 23.6 | Mean age: 35.1 (18–70). | 82% white, 7% Hispanic, 6% African American, 5% other. | 0 | 3.6 | 19.5 | – |
| Kral, 2005 | San Francisco, CA | MSM-IDU | A | 3 | 157 | 44.0 | Median age>40. | 62% white, 19% African American, 4% Latino, 14% other. | 1 | 19.7 | 36.5 | – |
| Latkin, 2011 | Baltimore, MD | Black MSM | A | 3 | 79 | 33.8 | Mean age: 38. | 100% Black. | 1 | 30.4 | 52.3 | – |
| Lehner 1998 | NYC | Males in STD clinic | D | 4 | 147 | 73.9 | n/a | 41% African American, 54% Hispanic, 4% white. | 1 | 34.7 | 69.2 | 9.6 |
| Levin, 2009 | Seattle, WA | General (18–39 year-olds) | D | 5 | 43 | 59.7 | Mean age: 35 | 34% white, 45% African American, 17% Latino, 4% other (for MSMW). | 1 | 24.4 | 53.8 | 9.2 |
| Lewis, 1994 | San Francisco, CA | Sexually active IDU | D | 3 | 49 | 51.6 | Ages 18–39. | 6% Asian, 7% African American, 79% white, 4% Hispanic, 4% other. | 0 | 7 | 20.7 | 0 |
| McKirnan, 1995 | Chicago, IL | Young MSMW | C | 3 | 536 | * | Mean age: 25 18–30). | 52% Black, 48% white. | 0 | 6.9 | – | – |
| Molitor, 1998 | CA (state) | Sexually active non-IDU | D | 4 | 16,290 | 50.4 | Median age: 20–29. | 56.1% white; 24.6% Latino/a; 10.4% Black; 4.6% API; 50.8% male. | 1 | 5.0 | 6.7 | 0.5 |
| Myers, 1997 | Los Angeles, CA | Black males | B | 3 | 81 | 32.4 | Mean age: 34.5. | 100% Black. | 1 | 58 | 74.6 | 6.8 |
| Operario, 2011 | Oakland, CA | Black MSMW | C | 3 | 68 | * | Median age: 44.6 (21–65). | 100% Black. | 0 | 21.4 | – | – |
| Roffman, 1990 | Seattle, WA | MSM | B | 3 | 32 | 30.2 | Mean age = 38. | MSMW: 94% White, 6% Black; MSMO, 90% White, 10% Black/other. | 0 | 0.0 | 33.3 | – |
| Salazar, 2010 | Atlanta, GA | Male IDU | B | 2 | 38 | – | Mean age: 45 (22–71). | 95% African American, 3.6% white, 1.5% Hispanic. | 0 | 26.3 | – | 7.1 |
| Siegel, 2008 | NYC | MSMW | A | 3 | 46 | * | Mean age 39.6 (20–60). | 41% African American, 35% Hispanic, 22% white, 2% Asian. | 0 | 20.9 | – | – |
| Tieu, 2012 | NYC | Black MSM | A | 3 | 84 | 25.8 | Median age: 41. | 100% Black. | 1 | 50.0 | 66.9 | – |
| Torian, 1996 | NYC | MSM | Not provided | 4 | 79 | 21.6 | Median age: 25–29. | 32% white, 48% AA, 24% Hispanic, 3% other. | 1 | 32.9 | 34.5 | – |
| Torian, 2000 | NYC | Gh+ males in STD clinic | Not provided | 4 | 25 | 36.2 | n/a | n/a | 1 | 44 | 36.4 | 8 |
| Torian, 2002a | NYC | MSM in STD clinic | Not provided | 4 | 145 | 27.6 | n/a | 28% white, 43% African American, 19% Hispanic, 9% mixed/other. | 1 | 43.4 | 47.6 | – |
| Torian, 2002b | NYC | MSM in STD clinic | Not provided | 4 | 133 | 30.5 | n/a | 37% white, 30% African American, 24% Hispanic, 9% other/mixed. | 1 | 14.3 | 19.5 | – |
| Valleroy, 2000 | 7 cities | YMSM | D | 1 | 2117 | 61.4 | Range: 15–22. | 17% African American, 6% Asian, 30% Hispanic, 36% white, 11% mixed/other. | 1 | 7.9 | 6.2 | – |
| Washington, 2010 | Baltimore, MD | Black MSMW-IDU | Not provided | 3 | 105 | * | Mean age: 31.6. | 90% African American; 10% Latino/African American. | 0 | 65.1 | – | – |
| Wheeler, 2008 | NYC; Philadelphia | Black MSM | A | 2 | 226 | 27.5 | Median age: 40–49. | 100% Black. | 1 | 40.7 | 60.1 | – |
| Williams, 2009 | Chicago, IL | Substance user or MSM | A | 2 | 343 | 71.3 | Mean age: 44 (17–70). | 6% white, 80% Black, 13% Hispanic, 1% other. | 1 | 11.4 | 53.6 | 4.7 |
| Wood, 1993 | Seattle, WA | MSM in STD clinic | B | 4 | 494 | 9.0 | n/a | n/a | 1 | 12.3 | 24.1 | – |
| Zule, 2009 | Central North Carolina | Substance user or MSM | C | 2 | 175 | 64.3 | Median age >35. | 77% African American, 20% white. | 1 | 12 | 38.1 | 4.9 |
Table notes: Recall window refers to the recall window of bisexual behavior in each study (A = MSMW ≤6 months; B = MSMW ≤1 year; C = MSMW<3 years; D = MSMW ≥3 years). Sampling strategy refers to recruitment technique (1 = time/location sampling; 2 = respondent-driven sampling; 3 = convenience sampling; 4 = HIV/STI clinic sampling; 5 = population-based sampling). HIV test basis refers to the form of assessment of HIV status (0 = self-report; 1 = serologic).
Refers to studies that focused only on MSMW.
Catania et al inferred the validity of participants’ self-reports by conducting a representative sample of serologic testing.
HIV Prevalence
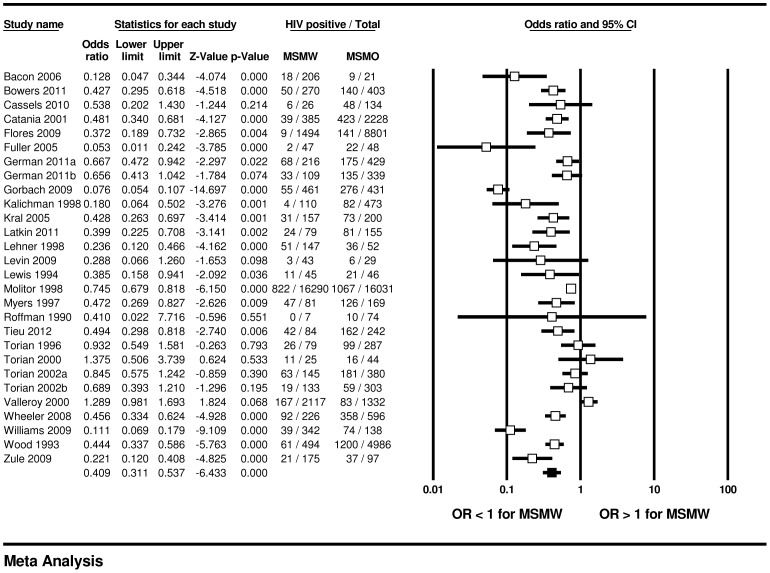
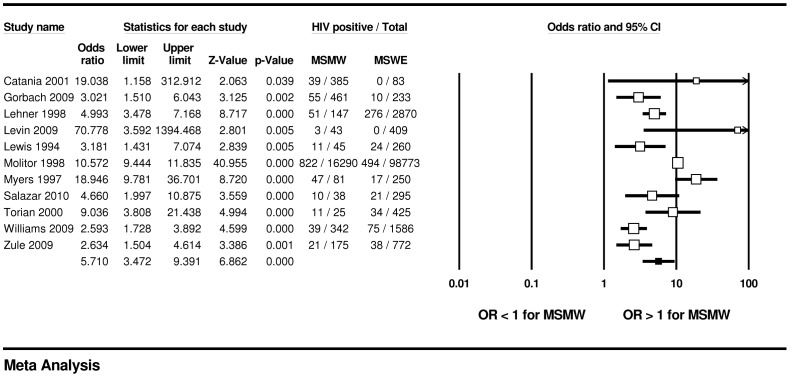
We found significant differences in HIV prevalence by sexual partner gender. Across 28 samples, MSMW were less likely to have HIV compared with MSMO (16.9% vs. 33.3%; OR = 0.41, 95% CI: 0.31, 0.54); across 11 samples, MSMW were more likely to have HIV compared with MSWE (18.3% vs. 3.5%; OR = 5.71, 95% CI: 3.47, 9.39) (see Figures 2–3). Across the 33 samples that included information for MSMW, the weighted mean HIV prevalence rate within MSMW was 17.9% (95% CI: 12.7%, 24.6%). In the 22 samples assessing HIV serologically, the weighted mean HIV prevalence among past-year MSMW was 20.8% (95% CI: 14.0%, 29.8%) (data not shown).
Figure 2. HIV prevalence among MSMW, compared to MSMO, U.S.
Figure 3. HIV prevalence among MSMW, compared to MSWE, U.S.
Table 2 shows that tests for moderation indicated a significant difference (Q-statistic = 6.8, P<.01) in HIV prevalence effect size between MSMW and MSMO by data collection date: HIV prevalence rates among MSMW and MSMO (15.3% vs. 24.0%, respectively) surveyed before 2000 were significantly more convergent than when groups were surveyed in 2000 or after (19.4% vs. 46.7%). No significant moderation of effect size between MSMW and MSMO was found for recall window of bisexual behavior; target population; locale; HIV test basis; or sampling strategy. Within MSMW, HIV prevalence was significantly moderated by target population: we found higher HIV prevalence in studies with greater than 90% minorities (32.7% vs. 13.2%; Q-statistic = 7.7, P<.01); and by locale: we found higher HIV prevalence in studies undertaken in the 12 CDC-defined high HIV/AIDS incidence locales (20.9% vs. 10.1%; Q-statistic = 5.4, P<.05). Recall window; data collection date; sampling method; and HIV test basis did not significantly moderate HIV prevalence within MSMW. Within MSMO, HIV prevalence rates were significantly moderated by target population: we found higher HIV prevalence in studies with greater than 90% minorities (56.4% vs. 26.4%; Q-statistic = 12.8, P<.001); and by data collection date: participants enrolled prior to 2000 had lower HIV prevalence than participants enrolled in 2000 or after (24.0% vs. 46.7%; Q-statistic = 9.4, P<.01) (data not shown).
Table 2. Mixed effect size moderators of HIV prevalence among MSMW relative to MSMO.
| Moderator variables | Subgroup categories | Number ofstudies | Odds ratio (95% CI) | P-value | Q-statistic(moderator class) | HIV prevalence estimate, MSMW (95% CI) | HIV prevalence estimate, MSMO (95% CI) |
| Date of data collection | Pre-2000 | 15 | 0.58 (0.45, 0.73) | <.001 | 6.8* | 15.3% (9.1%, 24.5%) | 24.0% (15.1%, 36.1%) |
| 2000 and after | 13 | 0.28 (0.17, 0.44) | <.001 | 19.4% (13.3%, 27.4%) | 46.7% (39.4%, 54.1%) | ||
| Study locale | Zone with high HIV/AIDS | 21 | 0.41 (0.29, 0.59) | <.001 | 0.01 | 20.2% (14.0%, 28.4%) | 38.4% (25.4%, 53.4%) |
| Other area | 7 | 0.40 (0.25, 0.64) | <.001 | 8.9% (5.1%, 15.0%) | 20.2% (10.5%, 35.2%) | ||
| Sampling strategy | Convenience | 18 | 0.47 (0.37, 0.60) | <.001 | 0.76 | 20.4% (11.9%, 32.7%) | 36.8% (25.2%, 50.2%) |
| Probability | 10 | 0.35 (0.19, 0.66) | .001 | 11.9% (6.7%, 20.4%) | 27.4% (12.1%, 50.8%) | ||
| Minority-based | <90% minority | 19 | 0.43 (0.30, 0.60) | <.001 | 0.35 | 13.3% (8.7%, 20.0%) | 26.4% (16.4%, 39.7%) |
| ≥90% minority | 7 | 0.31 (0.19, 0.53) | <.001 | 28.4% (15.8%, 45.5%) | 56.4% (46.7%, 64.8%) | ||
| Behavioral recall window | ≤12 months | 15 | 0.31 (0.21, 0.46) | <.001 | 0.12 | 16.3% (10.0%, 25.5%) | 37.5% (23.1%, 54.6%) |
| >12 months | 8 | 0.49 (0.32, 0.73) | <.001 | 12.5% (7.6%, 19.8%) | 25.1% (14.6%, 39.8%) | ||
| Assessment of HIV status | Self-report | 6 | 0.39 (0.29, 0.52) | <.001 | 0.74 | 6.1% (1.4%, 22.7%) | 15.6% (4.0%, 45.3%) |
| Serologic | 22 | 0.41 (0.31, 0.57) | <.001 | 20.8% (14.0%, 29.8%) | 39.4% (28.2%, 51.8%) |
Indicates moderation at p<.01.
In the overall model comparing HIV prevalence among MSMW and MSMO, Egger’s regression test illustrated significant asymmetry (2-tailed P<0.05). However, Orwin’s fail-safe n test indicated that an additional 273 missing studies with a mean odds ratio of 1.0 would need to be uncovered in order for the odds ratio in the overall model comparing MSMW and MSMO to approach non-significance, assuming an OR = 0.95 (95% CI: 0.90, 1.00) overall value and interval for a “trivial” odds ratio. The between-group (mixed effects) Q-statistic was 0.74, which did not indicate significant heterogeneity. Sensitivity analyses conducted with one study removed did not significantly change the overall mixed effects significance.
We found only one paper that presented data that compared HIV infection between MSMW of different races, and only one other paper presented data comparing HIV infection between Hispanic and non-Hispanic MSMW. Only two studies compared risk behavior among MSMW by race/ethnicity. No studies within this meta-analysis reported data comparing STI infection in MSMW by race/ethnicity. Given the lack of subgroup data, we were not able to perform separate meta-analyses on the prevalence of HIV, STI, or risk behavior by race/ethnicity categories.
Prevalence of Bisexual Behavior and Population Estimation
The weighted mean prevalence of bisexual behavior within the larger population of men who have sex with men (MSM) sampled across 28 studies was 38.5% (95% CI: 30.1%, 47.7%). It was 33.8% (95% CI: 23.7%, 45.6%) across 15 studies that assessed bisexual behavior over a time frame of one year or less. Recall window of bisexual behavior (Q-statistic = 4.4, P<.05) was the only significant moderator of the rate of bisexual behavior among MSM: longer recall windows were associated with higher proportions of bisexual behavior (data not shown). We used the estimated proportion of 33.8% for past-year MSMW/MSM with the CDC estimate that 2.9% of the U.S. male population 13 years and older are past-year MSM to calculate that (0.338)*(0.029), or 0.98%, of the U.S. male population is recently bisexually active [16]. Given that there are currently 122,852,862 U.S. males aged 13 or older [16], we calculated that approximately 1,204,204 American males are currently bisexually active, of whom 23.3%, or 280,580 are HIV-positive. We attempted to validate this estimate by calculating the weighted mean proportion of HIV-positive MSMW within HIV-positive MSM. Across the 12 studies assessing HIV serologically among both MSMW and MSMO using a recall window of one year or less for bisexual behavior, the proportion of HIV-positive MSMW among HIV-positive MSM was estimated to be 21.0% (95% CI: 14.7%, 28.9%). We used the CDC estimate that 580,000 MSM were currently living with HIV to predict that 21.0% of those, or 121,800, were past-year MSMW [17]. Although these estimates appear quite different, their 95% confidence intervals overlap – see Table 3.
Table 3. Population estimates of MSMW and HIV-positive MSMW in the United States.
| Data source | Original measure | Estimate (95% CI) | Newly derived measure | Newly derivedestimate (95% CI) |
| A. Purcell et al (2012) | Proportion of past-year MSMamong males ≥13 years old | .029 (.026,.032) | % of U.S. males ≥13 years whoare past-year MSMW (A*D) | 0.98% (0.6%, 1.5%) |
| B. CDC (2011) | No. of MSM living withHIV/AIDS | 580,000 (540,000; 620,000) | No. of past-year MSMWwho are HIV+ (B*E) | 121,800 (79,380; 179,180) |
| C. U.S. Census (2011) | No. of males ≥13 years old | 122,852,862 | No. of past-year MSMWin U.S. (A*C*D) | 1,204,204 (757,019; 1,792,669) |
| D. Meta-analysis | Past-year MSMW/MSM | .338 (.237,.456) | % of HIV+ past-year MSMWof U.S. males >13 years (A*D*F) | 0.23% (0.10%, 0.48%) |
| E. Meta-analysis | Proportion of HIV+ past-yearMSMW/HIV+ MSM | .210 (.147,.289) | – | – |
| F. Meta-analysis | HIV prevalence rate ofpast-year MSMW | .233 (.157,.331) | Number of past-year MSMWwho are HIV+ (A*C*D*F) | 280,580 (118,852; 593,373) |
STI and Sexual Risk Behavior Prevalence
As Table 4 shows, four studies that assessed HIV prevalence among MSMW also assessed STI prevalence among MSMO. Three of these studies [51], [57], [60] assessed STI generally – e.g., “any STI history” – while one study [42] assessed self-reports of several STI non-exclusively: for this study, we included only history of human papillomavirus (HPV). There were no significant differences in STI rates between MSMW and MSMO in these studies (22.0% vs. 26.6%; OR = 0.87, 95% CI: 0.67, 1.13). Three studies examined STI prevalence among both MSMW and MSWE, of which two studies reported on STI generally [49], [60] and one study assessed self-reports of several STI non-exclusively, for which we included only history of HPV [42]. No significant differences were found in STI prevalence between MSMW and MSWE (17.2% vs. 7.3%; OR = 2.64, 95% CI: 0.73, 9.51).
Table 4. STI and sexual risk behavior differences between MSMW, MSMO, and MSWE.
| Outcome variables | Comparisongroup | Number of studies | Odds ratio (95% CI) | Effect sizeP- value | Event rate estimate, MSMW (95% CI) | Event rate estimate, comparison (95% CI) |
| STI diagnosis or symptoms* | MSMO | 4 | 0.87 (0.67, 1.13) | .287 | 22.0% (5.2%, 58.6%) | 26.6% (8.8%, 57.7%) |
| MSWE | 3 | 2.64 (0.73, 9.51) | .138 | 17.2% (4.7%, 46.9%) | 7.3% (3.0%, 16.4%) | |
| UAI | MSMO | 4 | 0.91 (0.58, 1.42) | .665 | 32.7% (22.1%, 45.3%) | 33.1% (26.6%, 40.4%) |
| URAI | MSMO | 4 | 0.36 (0.28, 0.46) | <.001 | 15.9% (10.6%, 23.0%) | 35.0% (28.1%, 42.5%) |
| UIAI with male | MSMO | 4 | 1.08 (0.87, 1.34) | .490 | 36.5% (25.0%, 49.9%) | 34.7% (25.1%, 45.8%) |
| UIAI with female | MSWE | 2 | 1.80 (1.29, 2.52) | .001 | 16.6% (10.1%, 26.0%) | 10.4% (8.5%, 12.6%) |
| UVI | MSWE | 4 | 0.61 (0.27, 1.39) | .237 | 43.8% (29.4%, 59.4%) | 55.6% (45.8%, 65.0%) |
All studies included measured any STI rather than individual kinds of STI, except one [42]: for this study, we used data only on human papillomavirus symptoms/diagnosis in these analyses.
MSMW were significantly less likely to engage in unprotected receptive anal intercourse (URAI) than MSMO (15.9% vs. 35.0%; OR = 0.36, 95% CI: 0.28, 0.46), but there were no significant differences between MSMO and MSMW in rates of unprotected anal intercourse (UAI) generally, or of unprotected insertive anal intercourse (UIAI) with men. MSMW were equally as likely as MSWE (43.8% vs. 55.6%; OR = 0.61, 95% CI: 0.27, 1.39) to have reported unprotected vaginal intercourse and more likely to have reported UIAI with women (16.6% vs. 10.4%; OR = 1.80, 95% CI: 1.29, 2.41). Subsidiary tests of moderation on STI and sexual risk behavior were not performed due to the small numbers of relevant studies (four or less per each comparison) reporting these variables (see Table 4).
Discussion
This study, insofar as we are aware, is the first meta-analysis of HIV prevalence among bisexually behaving men in the United States. It provides valuable information about their risk of HIV infection relative to men who have sex exclusively with either men or women. The large effect sizes we report here place MSMW squarely between MSMO and MSWE in HIV prevalence. These results are robust even using conservative mixed effects models, and are not significantly affected by methodological moderator variables except for post-HAART data collection dates. This finding, coupled with our within-group moderation results, suggests that HIV prevalence rates among MSMW are increasing less rapidly than among MSMO, perhaps due to relatively fewer URAI exposures among a pool of MSM whose collective viremia is steadily decreasing. It is not surprising to have found that MSMW have higher rates of HIV compared with MSWE, given that they engage in risk behaviors (URAI) that MSWE do not engage in, and that their male sexual partners have a far higher rate of HIV infection than the female sexual partners of MSWE. It is also not surprising to have found that racial/ethnic minority MSMW experience higher HIV prevalence rates than their counterparts; this mirrors research on MSM in general [61], [62]. It may be surprising, however, to have found MSMW to host such substantially reduced odds of HIV infection compared with MSMO. The literature contains conflicting evidence that MSMW have fewer male sex partners than MSMO [62] or multiple sex partners in general [40], [42], [63]–[66]. Our meta-analysis found that MSMW were significantly less likely to report engaging in URAI than MSMO, which may explain their reduced odds for HIV infection. There is additional evidence beyond the HIV prevalence literature that bisexually behaving men may be less likely to engage in URAI than their exclusively homosexual counterparts [63], [67]–[70]. That MSMW have less HIV and report less URAI than MSMO may be a consequence of their less frequent engagement in receptive anal intercourse in general than men who have sex with men exclusively [58]. On the other hand, we found no significant differences among MSMW and exclusively heterosexual men in unprotected vaginal intercourse; or between MSMW and MSMO engaging in UIAI with men, though MSMW were more likely than MSWE to engage in UIAI with women. Formative research analyzing differences in unprotected insertive intercourse rates among these three groups has been equivocal [71]–[73].
Our findings on prevalence of bisexual behavior within larger populations of MSM aligns closely with previous population-based research in the United States and Europe, in which relative proportions of MSMW and MSMO vary by the timeframe assessed in the recall measure for bisexual behavior: lifetime measures have tended to favor greater proportions of MSMW than MSMO, while past-year measures have tended to favor greater proportions of MSMO than MSMW [12]–[15], [74]. Our estimate that past-year MSMW comprise approximately 1% of the U.S. male population is consistent with previous findings from population-based research.
The extraordinarily high HIV prevalence rates found for MSMW, MSMO, and MSWE in this review should be interpreted with caution; these rates may be inflated as a result of sampling frames that are not nationally representative and were composed of very high-risk men, such as injection drug users and STI clinic attendees living in high HIV/AIDS prevalence cities. Thus, the results we have reported that compare HIV rates and effect sizes between groups are likely more reliable than within-group findings. For this reason, our estimate of the number of MSMW living HIV that derives from the proportion of HIV-positive past-year MSMW within HIV-positive MSM is likely more reliable than our estimate derived from a within-MSMW HIV event rate. This finding – that 121,800 past-year MSMW in the U.S. are living with HIV – suggests two important conclusions. First, bisexually behaving men compose a small but significant proportion of the population of MSM infected with HIV. Little if any research has been conducted that tests how well MSMW have been linked to and retained in care. There is evidence that MSMW have not been effectively reached by existing HIV prevention interventions; may be less likely to disclose same-sex behaviors to health care providers and to have been tested for HIV than their MSMO peers; and may be more likely to be unaware of their HIV positivity and comparatively reluctant to disclose their HIV status to sexual partners, possibly due to greater dissociation from gay communities and higher homonegativity [34], [57], [62], [70], [75], [76]. Given these challenges, HIV-positive MSMW constitute a population that could greatly benefit from dedicated HIV prevention and care interventions. Second, the dominant research trope that examines HIV risk among MSMW within their potential to serve as a bridge population from one community to another (read: the homosexual male community to the heterosexual female community) has likely been overstated. Though our findings suggest that MSMW present potential to both acquire and transmit HIV, heterosexual women appear as likely to encounter an HIV-positive male sexual partner who acquired HIV through injection drug use (IDU) or through heterosexual sex, given CDC estimates that 110,900 heterosexual males and 131,600 heterosexual male IDU are living with HIV/AIDS [17]. Using the same logic, an MSMO would be almost four times as likely to encounter another MSMO who was HIV-positive (458,200) than an HIV-positive MSMW. In view of these comparisons, we suggest that (1) at the population level, MSMW likely present no greater risk of HIV transmission to women than exclusively heterosexual partners; (2) MSMW likely present substantially less risk of HIV transmission to men than MSMO; (3) the dizzyingly disparate HIV rate ratios reported among MSM are likely even higher if measured specifically for MSMO; and (4) the HIV/AIDS risk that MSMW themselves face from each other, from MSMO, and from their female sexual partners is currently under-researched and unmitigated by dedicated intervention development and delivery attuned to bisexually behaving men and their particular needs [16], [21].
This systematic review and meta-analysis has several important limitations. First, our primary eligibility criterion of HIV prevalence assessment excluded several articles that solely presented secondary findings, such as STI and risky sexual behavior, of import to this analysis. Search strategies that target STI among MSMW, or risky sexual behavior among MSMW, may lead to different results in these domains. The paucity of existing research, as we have noted above, did not allow for subgroup analyses of HIV prevalence by race/ethnicity both within MSMW and compared to their peers. Our comparison of MSMW and MSWE may constitute a highly conservative (though still robust and highly significant) effect size: the majority of studies that included MSWE in our review and meta-analysis did so using very high-risk samples, such as street-based illicit substance users and their sexual partners or STI clinic attendees [37], [41], [54], [58], [60]. We did not code for sexual identity, because it is an imperfect corollary of sexual behavior, but it may have proven an important moderator of HIV risk among MSMW [39], [46], [65], [72], [77]–[82]. Most important, though we attempted to be as inclusive as possible, our PubMed and Ovid PsycINFO searches may have excluded relevant studies from this systematic review and meta-analysis, for instance those that report HIV rates among gay men or MSM but that also contain relevant tabular data referencing bisexual behavior, or health department reports and/or conference abstracts that may meet this review’s criteria but were not peer-reviewed articles. A strategy to include such grey literature may have reduced the indication of publication bias within this meta-analysis. While we acknowledge these limitations, we suggest that the robustness of our results, their internal consistency, and their external congruence with other studies indicate their validity and generalizability.
Our findings have important implications for HIV prevention and care planning, priority-setting, and intervention development. Local and state HIV care and prevention planning groups rely on national data to constitute HIV prevention and care plans; to set priority populations; and to recommend intervention placement and training to service providers. Exclusion of MSMW as a specified risk category in HIV/AIDS surveillance reports creates an environment wherein bisexually behaving men are more easily ignored by organizations receiving funding to provide HIV prevention and care, and wherein HIV rates specific to MSMO are likely diluted. There are currently no HIV prevention interventions that target bisexually behaving men in the CDC’s Diffusion of Effective Behavioral Interventions portfolio, which has been the gold standard for intervention diffusion and deployment for the last several years, though promising intervention designs for racial/ethnic minority MSMW are being evaluated, representing a long-overdue development that may provide models for reaching other MSMW effectively [82], [83]. Our results suggest a need to collect and report bisexual behavior in our local, state, and national HIV/AIDS and STI surveillance systems and within HIV intervention design, development, and delivery. Further formative research on HIV risk (such as synergistic epidemics, or syndemics) and protective factors (such as resiliencies) particular to MSMW is necessary to intervention development, as are meta-analyses specific to risky sexual behavior, mental health, and STI among MSMW and longitudinal research into bisexual men’s physical and psychosocial health over time. At present, while research is emerging lately, data are insufficient to estimate HIV prevalence differences between MSMW of specific races and ethnicities or to assess HIV incidence among MSMW. Nonetheless, our findings indicate that MSMW who are racial/ethnic minorities suffer disparate HIV burden and deserve particular attention in prevention and care research and delivery.
Though our literature search uncovered hundreds of articles purporting to assess HIV risk among “gay and bisexual” men, only a small fraction of these effectively differentiated those populations. Our results show that, in terms of HIV prevalence and risk behavior, MSMW and MSMO are quite distinct. Those few researchers studying HIV among MSMW have for years recommended more precise data collection and intervention design specific to MSMW [3], [25], [44], [84]. It is past time to heed their calls. Only a combination of MSMW-targeted research and improved data collection and reporting will allow our national, state, and local HIV prevention and care planning groups to effectively address the acquisition and transmission risks of bisexually behaving men in the United States.
Supporting Information
Electronic Search Strategy (PubMed Database).
(DOCX)
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Checklist.
(DOC)
Acknowledgments
The lead author thanks Nathaniel Soltesz for his assistance with graphics production, and Mike Marshal for informal meta-analysis training.
Funding Statement
Funding support was limited to a grant from the University of Pittsburgh Graduate School of Public Health (Dean’s Office) to the University of Pittsburgh Center for LGBT Health Research, which enabled the purchase of meta-analysis software and open access publication. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Morse EV, Simon PM, Osofsky HJ, Balson PM, Gaumer HR (1991) The male street prostitute: a vector for transmission of HIV infection into the heterosexual world. Soc Sci Med 32: 535–539. [DOI] [PubMed] [Google Scholar]
- 2. Ekstrand ML, Coates TJ, Guydish JR, Hauck WW, Collette L, et al. (1994) Are bisexually identified men in San Francisco a common vector for spreading HIV infection to women? Am J Public Health 84: 915–919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Doll LS, Beeker C (1996) Male bisexual behavior and HIV risk in the United States: synthesis of research with implications for behavioral interventions. AIDS Educ Prev 8: 205–225. [PubMed] [Google Scholar]
- 4. O’Leary A, Jones KT (2006) Bisexual men and heterosexual women: how big is the bridge? How can we know? Sex Transm Dis 33: 594–595. [DOI] [PubMed] [Google Scholar]
- 5. Chu SY, Peterman TA, Doll LS, Buehler JW, Curran JW (1992) AIDS in bisexual men in the United States: epidemiology and transmission to women. Am J Public Health 82: 220–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Montgomery J, Mokotoff E, Gentry A, Blair J (2003) The extent of bisexual behaviour in HIV-infected men and implications for transmission to their female sex partners. AIDS Care 15: 829–837. [DOI] [PubMed] [Google Scholar]
- 7. Kahn JG, Gurvey J, Pollack LM, Binson D, Catania JA (1997) How many HIV infections cross the bisexual bridge? An estimate from the United States. AIDS 11: 1031–1037. [DOI] [PubMed] [Google Scholar]
- 8. Pinkerton SD, Abramson PR, Kalichman SC, Catz SL, Johnson-Masotti AP (2000) Secondary HIV transmission rates in a mixed-gender sample. Int J STD AIDS 11: 38–44. [DOI] [PubMed] [Google Scholar]
- 9. Prabhu R, Owen CL, Folger K, McFarland W (2004) The bisexual bridge revisited: sexual risk behavior among men who have sex with men and women, San Francisco, 1998–2003. AIDS 18: 1604–1606. [DOI] [PubMed] [Google Scholar]
- 10. Adimora AA, Fullilove RE (2006) Men who have sex with men and women: pieces of the U.S. HIV epidemic puzzle. Sex Transm Dis 33: 596–598. [DOI] [PubMed] [Google Scholar]
- 11. Hightow LB, Leone PA, Macdonald PD, McCoy SI, Sampson LA, et al. (2006) Men who have sex with men and women: a unique risk group for HIV transmission on North Carolina College campuses. Sex Transm Dis 33: 585–593. [DOI] [PubMed] [Google Scholar]
- 12. Jeffries WLt, Dodge B (2007) Male bisexuality and condom use at last sexual encounter: results from a national survey. J Sex Res 44: 278–289. [DOI] [PubMed] [Google Scholar]
- 13. Rogers SM, Turner CF (1991) Male-male sexual contact in the USA: Findings from five sample surveys, 1970–1990. Journal of Sex Research 28: 491–519. [Google Scholar]
- 14. Smith TW (2006) Sexual behavior in the United States. Sex and sexuality 1: 104–132. [Google Scholar]
- 15.Laumann EO, Gagnon JH, Michael RT, Michaels S (1994) The social organization of sexuality: Sexual practices in the United States: University of Chicago Press.
- 16. Purcell DW, Johnson CH, Lansky A, Prejean J, Stein R, et al. (2012) Estimating the Population Size of Men Who Have Sex with Men in the United States to Obtain HIV and Syphilis Rates. Open AIDS Journal 6: 98–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Centers for Disease Control and Prevention (2011) HIV surveillance–United States, 1981–2008. MMWR Morb Mortal Wkly Rep 60: 689–693. [PubMed] [Google Scholar]
- 18. Satcher AJ, Durant T, Hu X, Dean HD (2007) AIDS cases among women who reported sex with a bisexual man, 2000–2004–United States. Women Health 46: 23–40. [DOI] [PubMed] [Google Scholar]
- 19. Cunningham S, Olthoff G, Burnett P, Rompalo A, Ellen J (2006) Evidence of heterosexual bridging among syphilis-positive men who have sex with men. Sexually transmitted infections 82: 444–445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kennamer JD, Honnold J, Bradford J, Hendricks M (2000) Differences in disclosure of sexuality among African American and White gay/bisexual men: implications for HIV/AIDS prevention. AIDS Educ Prev 12: 519–531. [PubMed] [Google Scholar]
- 21. Millett G, Malebranche D, Mason B, Spikes P (2005) Focusing “down low”: bisexual black men, HIV risk and heterosexual transmission. J Natl Med Assoc 97: 52S–59S. [PMC free article] [PubMed] [Google Scholar]
- 22. Malebranche DJ (2008) Bisexually active Black men in the United States and HIV: acknowledging more than the “Down Low”. Arch Sex Behav 37: 810–816. [DOI] [PubMed] [Google Scholar]
- 23. Saleh LD, Operario D (2009) Moving beyond “the down low”: a critical analysis of terminology guiding HIV prevention efforts for African American men who have secretive sex with men. Soc Sci Med 68: 390–395. [DOI] [PubMed] [Google Scholar]
- 24. Worth H (2011) Is the myth of the bisexual infector still a myth? Reflections on HIV risk and men who have sex with men and women. Journal of Bisexuality 11: 488–492. [Google Scholar]
- 25.Rust PC (2000) Bisexuality in the United States: A social science reader: Columbia University Press.
- 26. Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS medicine 6: e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Morin SF, Kelly JA, Charlebois ED, Remien RH, Rotheram-Borus MJ, et al. (2011) Responding to the National HIV/AIDS Strategy–Setting the Research Agenda. Journal of acquired immune deficiency syndromes (1999) 57: 175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Borenstein M, Hedges LV, Higgins JP, Rothstein HR (2011) Introduction to meta-analysis: Wiley.
- 29.Borenstein M, Hedges L, Higgins J, Rothstein H (2005) Comprehensive meta-analysis version 2. Englewood, NJ: Biostat.
- 30. Bacon O, Lum P, Hahn J, Evans J, Davidson P, et al. (2006) Commercial sex work and risk of HIV infection among young drug-injecting men who have sex with men in San Francisco. Sex Transm Dis 33: 228–234. [DOI] [PubMed] [Google Scholar]
- 31. Bowers JR, Branson CM, Fletcher J, Reback CJ (2011) Differences in substance use and sexual partnering between men who have sex with men, men who have sex with men and women and transgender women. Cult Health Sex 13: 629–642. [DOI] [PubMed] [Google Scholar]
- 32. Cassels S, Pearson CR, Walters K, Simoni JM, Morris M (2010) Sexual partner concurrency and sexual risk among gay, lesbian, bisexual, and transgender american indian/alaska natives. Sex Transm Dis 37: 272–278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Catania JA, Osmond D, Stall RD, Pollack L, Paul JP, et al. (2001) The continuing HIV epidemic among men who have sex with men. American Journal of Public Health 91: 907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Flores SA, Bakeman R, Millett GA, Peterson JL (2009) HIV risk among bisexually and homosexually active racially diverse young men. Sex Transm Dis 36: 325–329. [DOI] [PubMed] [Google Scholar]
- 35. Fuller CM, Absalon J, Ompad DC, Nash D, Koblin B, et al. (2005) A comparison of HIV seropositive and seronegative young adult heroin- and cocaine-using men who have sex with men in New York City, 2000–2003. J Urban Health 82: i51–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. German D, Sifakis F, Maulsby C, Towe VL, Flynn CP, et al. (2011) Persistently high prevalence and unrecognized HIV infection among men who have sex with men in Baltimore: the BESURE Study. JAIDS Journal of Acquired Immune Deficiency Syndromes 57: 77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Gorbach PM, Murphy R, Weiss RE, Hucks-Ortiz C, Shoptaw S (2009) Bridging sexual boundaries: men who have sex with men and women in a street-based sample in Los Angeles. J Urban Health 86 Suppl 163–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Kalichman SC, Roffman RA, Picciano JF, Bolan M (1998) Risk for HIV infection among bisexual men seeking HIV-prevention services and risks posed to their female partners. Health Psychol 17: 320–327. [PubMed] [Google Scholar]
- 39. Kral AH, Lorvick J, Ciccarone D, Wenger L, Gee L, et al. (2005) HIV prevalence and risk behaviors among men who have sex with men and inject drugs in San Francisco. J Urban Health 82: i43–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Latkin C, Yang C, Tobin K, Penniman T, Patterson J, et al. (2011) Differences in the social networks of African American men who have sex with men only and those who have sex with men and women. Am J Public Health 101: e18–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Lehner T, Chiasson MA (1998) Seroprevalence of human immunodeficiency virus type 1 and sexual behaviors in bisexual African-American and Hispanic men visiting a sexually transmitted disease clinic in New York City. Am J Epidemiol 147: 269–272. [DOI] [PubMed] [Google Scholar]
- 42. Levin EM, Koopman JS, Aral SO, Holmes KK, Foxman B (2009) Characteristics of men who have sex with men and women and women who have sex with women and men: results from the 2003 Seattle sex survey. Sex Transm Dis 36: 541–546. [DOI] [PubMed] [Google Scholar]
- 43. Lewis DK, Watters JK (1994) Sexual behavior and sexual identity in male injection drug users. J Acquir Immune Defic Syndr 7: 190–198. [PubMed] [Google Scholar]
- 44. McKirnan DJ, Stokes JP, Doll L, Burzette RG (1995) Bisexually active men: Social characteristics and sexual behavior. Journal of Sex Research 32: 65–76. [Google Scholar]
- 45. Molitor F, Truax SR, Ruiz JD, Sun RK (1998) Association of methamphetamine use during sex with risky sexual behaviors and HIV infection among non-injection drug users. West J Med 168: 93–97. [PMC free article] [PubMed] [Google Scholar]
- 46. Myers HF, Satz P, Miller BE, Bing EG, Evans G, et al. (1997) The African-American Health Project (AAHP): study overview and select findings on high risk behaviors and psychiatric disorders in African American men. Ethn Health 2: 183–196. [DOI] [PubMed] [Google Scholar]
- 47. Operario D, Smith CD, Arnold E, Kegeles S (2011) Sexual risk and substance use behaviors among African American men who have sex with men and women. AIDS Behav 15: 576–583. [DOI] [PubMed] [Google Scholar]
- 48. Roffman RA, Gillmore MR, Gilchrist LD, Mathias SA, Krueger L (1990) Continuing unsafe sex: assessing the need for AIDS prevention counseling. Public Health Rep 105: 202–208. [PMC free article] [PubMed] [Google Scholar]
- 49. Salazar L, Crosby R, Head S, Siegler A (2010) Male injecting drug users in the Deep South: Bisexual behaviour is a marker for elevated HIV risk. International Journal of STD & AIDS 21: 691–696. [DOI] [PubMed] [Google Scholar]
- 50. Siegel K, Schrimshaw EW, Lekas HM, Parsons JT (2008) Sexual behaviors of non-gay identified non-disclosing men who have sex with men and women. Arch Sex Behav 37: 720–735. [DOI] [PubMed] [Google Scholar]
- 51. Tieu HV, Spikes P, Patterson J, Bonner S, Egan JE, et al. (2012) Sociodemographic and risk behavior characteristics associated with unprotected sex with women among black men who have sex with men and women in New York City. AIDS Care 24: 1111–1119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Torian LV, Weisfuse IB, Makki HA, Benson DA, DiCamillo LM, et al. (1996) Trends in HIV seroprevalence in men who have sex with men: New York City Department of Health sexually transmitted disease clinics, 1988–1993. AIDS 10: 187–192. [DOI] [PubMed] [Google Scholar]
- 53. Torian LV, Makki HA, Menzies IB, Murrill CS, Benson DA, et al. (2000) High HIV seroprevalence associated with gonorrhea: New York City Department of Health, sexually transmitted disease clinics, 1990–1997. AIDS 14: 189–195. [DOI] [PubMed] [Google Scholar]
- 54. Torian LV, Makki HA, Menzies IB, Murrill CS, Weisfuse IB (2002) HIV infection in men who have sex with men, New York City Department of Health sexually transmitted disease clinics, 1990–1999: a decade of serosurveillance finds that racial disparities and associations between HIV and gonorrhea persist. Sex Transm Dis 29: 73–78. [DOI] [PubMed] [Google Scholar]
- 55. Valleroy LA, MacKellar DA, Karon JM, Rosen DH, McFarland W, et al. (2000) HIV prevalence and associated risks in young men who have sex with men. JAMA: the journal of the American Medical Association 284: 198–204. [DOI] [PubMed] [Google Scholar]
- 56. Washington TA, Thomas C (2010) Exploring the use of web-based HIV prevention for injection-drug-using black men who have sex with both men and women: A feasibility study. Journal of Gay & Lesbian Social Services: Issues in Practice, Policy & Research 22: 432–445. [Google Scholar]
- 57. Wheeler DP, Lauby JL, Liu KL, Van Sluytman LG, Murrill C (2008) A comparative analysis of sexual risk characteristics of Black men who have sex with men or with men and women. Arch Sex Behav 37: 697–707. [DOI] [PubMed] [Google Scholar]
- 58. Williams CT, Mackesy-Amiti ME, McKirnan DJ, Ouellet LJ (2009) Differences in sexual identity, risk practices, and sex partners between bisexual men and other men among a low-income drug-using sample. J Urban Health 86 Suppl 193–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Wood RW, Krueger LE, Pearlman TC, Goldbaum G (1993) HIV transmission: Women’s risk from bisexual men. Am J Public Health 83: 1757–1759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Zule WA, Bobashev GV, Wechsberg WM, Costenbader EC, Coomes CM (2009) Behaviorally bisexual men and their risk behaviors with men and women. J Urban Health 86 Suppl 148–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Millett GA, Peterson JL, Wolitski RJ, Stall R (2006) Greater risk for HIV infection of black men who have sex with men: a critical literature review. Journal Information 96. [DOI] [PMC free article] [PubMed]
- 62. Munoz-Laboy M, Dodge B (2007) Bisexual Latino men and HIV and sexually transmitted infections risk: an exploratory analysis. Am J Public Health 97: 1102–1106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Knight KR, Shade SB, Purcell DW, Rose CD, Metsch LR, et al. (2007) Sexual transmission risk behavior reported among behaviorally bisexual HIV-positive injection drug-using men. J Acquir Immune Defic Syndr 46 Suppl 2S80–87. [DOI] [PubMed] [Google Scholar]
- 64. Jeffries WLIV (2011) The number of recent sex partners among bisexual men in the United States. Perspectives on Sexual and Reproductive Health 43: 151–157. [DOI] [PubMed] [Google Scholar]
- 65. Goodenow C, Netherland J, Szalacha L (2002) AIDS-related risk among adolescent males who have sex with males, females, or both: evidence from a statewide survey. Am J Public Health 92: 203–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Spikes PS, Purcell DW, Williams KM, Chen Y, Ding H, et al. (2009) Sexual risk behaviors among HIV-positive black men who have sex with women, with men, or with men and women: implications for intervention development. Am J Public Health 99: 1072–1078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Nakamura N, Semple SJ, Strathdee SA, Patterson TL (2011) HIV risk profiles among HIV-positive, methamphetamine-using men who have sex with both men and women. Arch Sex Behav 40: 793–801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Agronick G, O’Donnell L, Stueve A, Doval AS, Duran R, et al. (2004) Sexual behaviors and risks among bisexually- and gay-identified young Latino men. AIDS Behav 8: 185–197. [DOI] [PubMed] [Google Scholar]
- 69. Wold C, Seage GR III, Lenderking WR, Mayer KH, Cai B, et al. (1998) Unsafe sex in men who have sex with both men and women. J Acquir Immune Defic Syndr Hum Retrovirol 17: 361–367. [DOI] [PubMed] [Google Scholar]
- 70. Hays RB, Paul J, Ekstrand M, Kegeles SM, Stall R, et al. (1997) Actual versus perceived HIV status, sexual behaviors and predictors of unprotected sex among young gay and bisexual men who identify as HIV-negative, HIV-positive and untested. AIDS 11: 1495–1502. [DOI] [PubMed] [Google Scholar]
- 71. Crepaz N, Marks G (2003) Serostatus disclosure, sexual communication and safer sex in HIV-positive men. AIDS Care 15: 379–387. [DOI] [PubMed] [Google Scholar]
- 72. Pathela P, Schillinger JA (2010) Sexual behaviors and sexual violence: adolescents with opposite-, same-, or both-sex partners. Pediatrics 126: 879–886. [DOI] [PubMed] [Google Scholar]
- 73. Zellner JA, Martinez-Donate AP, Sanudo F, Fernandez-Cerdeno A, Sipan CL, et al. (2009) The interaction of sexual identity with sexual behavior and its influence on HIV risk among latino men: results of a community survey in northern San Diego County, California. Am J Public Health 99: 125–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Sandfort T (1998) Homosexual and bisexual behaviour in European countries. Sexual behaviour and HIV/AIDS in Europe: 68–105.
- 75. Shoptaw S, Weiss RE, Munjas B, Hucks-Ortiz C, Young SD, et al. (2009) Homonegativity, substance use, sexual risk behaviors, and HIV status in poor and ethnic men who have sex with men in Los Angeles. J Urban Health 86 Suppl 177–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Bernstein KT, Liu KL, Begier EM, Koblin B, Karpati A, et al. (2008) Same-sex attraction disclosure to health care providers among New York City men who have sex with men: implications for HIV testing approaches. Arch Intern Med 168: 1458–1464. [DOI] [PubMed] [Google Scholar]
- 77. Cochran SD, Mays VM (2007) Physical health complaints among lesbians, gay men, and bisexual and homosexually experienced heterosexual individuals: results from the California Quality of Life Survey. Am J Public Health 97: 2048–2055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Deren S, Stark M, Rhodes F, Siegal H, Cottler L, et al. (2001) Drug-using men who have sex with men: Sexual behaviours and sexual identities. Culture, Health & Sexuality 3: 329–338. [Google Scholar]
- 79. Ross MW, Essien EJ, Williams ML, Fernandez-Esquer ME (2003) Concordance between sexual behavior and sexual identity in street outreach samples of four racial/ethnic groups. Sex Transm Dis 30: 110–113. [DOI] [PubMed] [Google Scholar]
- 80. Xia Q, Osmond DH, Tholandi M, Pollack LM, Zhou W, et al. (2006) HIV prevalence and sexual risk behaviors among men who have sex with men: results from a statewide population-based survey in California. J Acquir Immune Defic Syndr 41: 238–245. [DOI] [PubMed] [Google Scholar]
- 81.Aggleton P (1996) Bisexualities and AIDS: International perspectives: Taylor & Francis.
- 82. Martinez-Donate AP, Zellner JA, Sanudo F, Fernandez-Cerdeno A, Hovell MF, et al. (2010) Hombres Sanos: evaluation of a social marketing campaign for heterosexually identified Latino men who have sex with men and women. Am J Public Health 100: 2532–2540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Operario D, Smith CD, Arnold E, Kegeles S (2010) The Bruthas Project: Evaluation of community-based HIV prevention intervention for African American men who have sex with men and women. AIDS Education and Prevention 22: 37–48. [DOI] [PubMed] [Google Scholar]
- 84. Mimiaga MJ, Reisner SL, Cranston K, Isenberg D, Bright D, et al. (2009) Sexual mixing patterns and partner characteristics of black MSM in Massachusetts at increased risk for HIV infection and transmission. J Urban Health 86: 602–623. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Electronic Search Strategy (PubMed Database).
(DOCX)
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Checklist.
(DOC)