Abstract
Nigeria is the most populous country in Africa, and its population is expected to double in <25 years (Central Intelligence Agency 2012; Fotso et al. 2011). Over half of the population already lives in an urban area, and by 2050, that proportion will increase to three quarters (United Nations, Department of Economic and Social Affairs, Population Division 2012; Measurement Learning & Evaluation Project, Nigerian Urban Reproductive Health Initiative, National Population Commission 2012). Reducing unwanted and unplanned pregnancies through reliable access to high-quality modern contraceptives, especially among the urban poor, could make a major contribution to moderating population growth and improving the livelihood of urban residents. This study uses facility census data to create and assign aggregate-level family planning (FP) supply index scores to 19 local government areas (LGAs) across six selected cities of Nigeria. It then explores the relationships between public and private sector FP services and determines whether contraceptive access and availability in either sector is correlated with community-level wealth. Data show pronounced variability in contraceptive access and availability across LGAs in both sectors, with a positive correlation between public sector and private sector supply environments and only localized associations between the FP supply environments and poverty. These results will be useful for program planners and policy makers to improve equal access to contraception through the expansion or redistribution of services in focused urban areas.
Keywords: Family planning, Supply environment, Access, Availability, Inequality, Wealth distribution, Urban, Supply, Contraception, Service distribution, Poverty, Nigeria, Public-sector, Private-sector, Community-level
Background/Introduction
Nigeria is the most populous country in Africa. As of 2012, Nigeria was home to approximately 170 million people, and with almost 44 % of the country under 14 years old, that number is expected to double in <25 years.1,2 According to UN estimates (2010), it will be one of six countries that will account for half of the world’s projected population increase by 2100.3
Most of Nigeria’s population growth will occur in its urban areas. As compared to its overall annual growth rate of 2.5 %, Nigeria’s urban growth rate is 3.75 %.1 Over half of the country’s population already lives in an urban area, and by 2050, that proportion will increase to three quarters.4 Due to the rapid urbanization, urban Nigeria increasingly suffers from an acute shortage of social amenities and insufficient infrastructure and services.4 Furthermore, an estimated 63 % of Nigeria’s urban population lives in slums,5 where overcrowding, inadequate sanitation, and poor refuse collection all lead to outbreaks of infectious diseases such as tuberculosis, hepatitis, dengue, pneumonia, cholera, and diarrheal illnesses.6
Research suggests that over 60 % of urban population growth in the developing world, and up to 75 % in Sub-Saharan Africa,7 is a result of fertility rates that have remained high, while mortality rates have decreased.3,8 Indeed, in Nigeria, the overall urban fertility rate has only slowly decreased from 5.1 to 4.7 children per woman since the late 1980s.9 Therefore, in part to slow the growth of the urban population and improve the livelihood of those living there, two of the main objectives of Nigeria’s National Policy on Population (updated 2004) are to increase the prevalence rate of modern contraceptive use—a well-known proximate determinant of fertility10—by at least two percentage points every year and to reduce the country’s overall fertility rate by at least 0.6 children every 5 years.4,11
It has been well established that contraceptive use is typically higher and fertility levels are lower in urban areas, as compared to rural areas;2,12,13 however, these patterns are often not equally distributed among all urban residents. In fact, evidence suggests significant disparities in fertility rates and contraceptive use behaviors among urban wealth quintiles.8,14–19 In Nigeria, for example, the fertility rate is higher overall among the urban poor as compared to the urban rich.2,4,9 Also, knowledge and use of modern contraception increases with greater household wealth.2 Furthermore, women in poorer urban households in Nigeria tend to marry and begin sexual intercourse at earlier ages than women in wealthier urban households, increasing their duration of exposure to the risk of pregnancy and high fertility.2,4,10
The consequences of these inequalities spiral from a higher number of unintended, high-risk pregnancies among the urban poor to a greater need for health service utilization, often decreased opportunity for employment and/or higher education,20 and increased maternal and infant morbidity and mortality9 within the lower wealth quintiles; all of which, in turn, makes it difficult to break the cycle of urban poverty and health inequality.6,20 There are a number of social and political obstacles to consider when determining strategies and frameworks for breaking this cycle, decreasing fertility, and slowing population growth.11 However, on the supply side, one straightforward and cost-effective approach to eliminating unwanted or mistimed pregnancies is to provide easy and reliable access to high-quality contraceptive services for all those who want or need them.4,20–23
In urban areas, both the public and private family planning (FP) sectors are important in ensuring equal access to FP services and availability of modern contraceptives.12,24–28 However, in Nigeria, neither sector has been analyzed in relation to the different subpopulations of wealth status. Therefore, it is unknown whether the two sectors are fully engaged so as to most effectively serve the urban poor. To date, there is no fine-grained description of, or comparison between, Nigeria’s urban private sector FP supply environment and its public sector FP supply environment. Furthermore, studies that have explored these questions have been limited by the fact that few supply side surveys have been collected around the same time as household surveys and/or were not collected in a manner that facilitated strong data linking.29
This study, therefore, fills an important gap in what is known about Nigeria’s contraceptive supply environment. Using survey data from FP service outlets—from here forward referred to as service delivery points (SDPs)—it creates supply index scores (SISs) to measure the aggregate-level public and private sector FP supply environment within and across six purposively selected cities of Nigeria. Specifically, it assesses whether the public and/or private sector FP supply environments are consistent across urban local government areas (LGAs),1 and if not, how they differ. It also explores whether and how services from one sector correlate with and/or compliment services within the other sector. Since there exists no standard measure for quantifying the multidimensional nature of the FP supply environment, this study draws on the commodity security and logistics framework created by the United States Agency for International Development to define supply as product availability and access to services.30 It considers availability as the actual on hand/procurable status of contraceptive commodities at any given SDP and access as the degree to which FP services may be obtained by a large majority of the population.
Finally, by linking aggregate-level SDP data with data collected at the same time from individuals living within corresponding communities, this study explores whether the FP supply environment is correlated with community-level wealth status and is distributed in a way that might mitigate barriers to contraceptive access and availability among the urban poor. A better understanding of these relationships will enable donors, policy makers and program implementers to make informed decisions about limited resource allocation and programming, thereby improving equality in FP access and availability and possibly decreasing overall urban fertility.
Research Design and Methods
This study uses data from the 2010–2011 baseline survey of the Nigerian Urban Reproductive Health Initiative undertaken by the Measurement, Learning & Evaluation (MLE) Project.2 Both individual and SDP data are analyzed from the selected cities of Abuja, Benin City, Ibadan, Ilorin, Kaduna, and Zaria.31
Individual Data
The individual-level data were collected between October 2010 and April 2011 via a two-stage stratified sampling design. First, a random sample of urban enumeration areas, or clusters, was drawn from the 2006 Nigeria Population and Housing Census within the six study cities. The clusters were selected in each city based on probability proportional to their population size. The number of clusters selected per city was based on information from the 2008 Nigeria Demographic Health Survey regarding the number of women per household in urban areas at the state level. The number of clusters per city in the survey ranged from a low of 74 in Zaria to a high of 102 in Ibadan.4
Next, 41 households in each cluster were selected randomly to create an average sample of about 3,000 women in each city. All women, ages 15 to 49, living permanently in the selected households and visitors present on the night before the survey were then asked to participate in a detailed interview with a trained female interviewer following receipt of informed consent.4 The sample was taken from 20 LGAs and included 16,144 married and unmarried women. Of the full sample, this study only analyzed information collected from women who were surveyed within the 19 LGAs from which the sample of SDP-level data, described in the next section, were taken (N = 16,101).
SDP Data
Between February and June 2011, data on FP services and/or commodities were also collected from a sample of SDPs. Four categories of SDPs were surveyed: (1) public sector health facilities (HFs); (2) preferred private HFs; (3) private pharmacies; and (4) private patent medicine stores (PMSs).32 Different selection strategies were used for each SDP type. Public HFs, pharmacies, and PMSs were identified through a compiled list of verified health outlets obtained from relevant Nigerian health agencies3.32 All public HFs were visited; to control survey costs, about 100 pharmacies in the larger cities were randomly sampled, as were about 100 PMSs in all cities. Preferred private HFs were identified from the MLE individual survey; women were asked where they go for child health, maternal health, FP visits, and HIV testing. All mentioned facilities were included in the preferred private facility sample.4 Three different survey tools were used to collect SDP information: one for the pharmacies, one for the PMSs, and a third for the public and preferred private HFs. Table 1 summarizes the sampling approaches.
Table 1.
Sampling approach by city for each type of SDP
| SDP type | City | Sampling approacha |
|---|---|---|
| Public HFs: government hospitals, health centers, health posts and dispensaries, child welfare clinics, and maternity homes | All | Census |
| Preferred private HFs: faith-based, private or nongovernmental hospitals, clinics, doctor’s offices, and nursing/maternity homes | All | Limited to HFs reported by respondentsb |
| Private pharmacies | Abuja | Random sample of about 100 at the city level |
| Kaduna | Random sample of about 100 at the city level | |
| All others (Benin City, Ibadan, Ilorin, and Zaria) | Census | |
| Private patent medicine stores | All | Random sample of about 100 at the city level |
aThe survey design called for a sample of 100 PMSs and 100 pharmacies in each city. In the cities where there were more than 100 PMSs or pharmacies, a random sample of 100 was selected
bThough the data represent a census of all preferred private HFs mentioned by respondents, they do not include all private sector HFs within each urban LGA sampling frame
SDP data were collected from 25 different LGAs within the six selected cities of Nigeria.4 This study analyzes data from 19 of these LGAs: five LGAs were dropped because there was no information collected from individuals within them and one was excluded because the sampling frame captured too few SDPs to calculate a representative urban LGA-level SIS. Within the remaining 19 LGAs, information was collected from 1,342 SDPs. Eight of these SDPs were dropped because there was no indication of their SDP type and 114 were dropped because they either did not sell FP or the variable indicating whether they sold FP was missing. With the remaining 1,220 SDPs, the FP SIS for each SDP type within each LGA was created.
Supply Environment Measures
Supply Index Score
FP SISs were created to reflect the LGA-level FP supply environment. Four continuous scores were assigned to each LGA: one for public sector FP HFs, one for preferred private FP HFs, one for private FP PMSs, and one for private FP pharmacies. The SISs were created by multiplying two LGA-level variables for each SDP type: (1) FP supply environment strength and (2) FP supply environment size. These two variables were created as follows (see Fig. 1 and Table 2):
-
FP supply environment strength:
This continuous variable was based on seven SDP measures that reflect strength of contraceptive access and availability, including (1) method availability, (2) availability of injectables5, (3) availability of the intrauterine device (IUD)6 (only among public HFs and preferred private HFs, as PMSs and pharmacies do not sell the IUD), (4) stockouts of normally available methods, (5) hours FP services are provided, (6) requirements for partner consent, and (7) availability of socially marketed products (see Table 2 for a summary of measures and the Appendix for a more detailed description of measure creation.)
Using these seven component measures, the variable was created in three steps for each SDP type. First, the values for each of the seven SDP measures were aggregated up to the LGA level. Second, the LGA-level percentage values for each measure were summed within each stratum of SDP type. The range of values for public and private HFs was 0 to 700, and the range for pharmacies and PMSs was 0 to 600. Third, in order to put the final variable on the same 0 to 100 scale for all SDP types, the sum for public and private HFs was divided by 7 and the sum for pharmacies and PMSs was divided by 6.
Case-wise deletion was used to create the seven aggregate-level supply measures. Therefore, due to missing data for some component measures, the range of the number of SDPs included in the final sample for this variable was 1,155 to 1,220. Note that only 376 public and preferred private facilities were included in the LGA-level measure for IUD availability. All PMSs and pharmacies were dropped from this measure, as they do not sell IUDs.
-
FP supply environment size:
This continuous variable measures the FP service density for each SDP type. It was created by dividing the total number of SDPs within the urban areas of each LGA that provide FP by the square kilometer area of the respective urban LGA. The number of FP SDPs used in the numerator for the public HF, preferred private HF, and pharmacy (except in Abuja and Kaduna) density measures were based on the MLE SDP census data. The number of PMSs that sell FP in each urban LGA was estimated by multiplying the ratio of surveyed PMSs that sell FP by the total number of PMSs in the original SDP sample frame obtained prior to sampling. (The same steps were taken to estimate the number of pharmacies that sell FP in Abuja and Kaduna—where a census of pharmacies was not taken.) The urban geographic area of each LGA—the density denominator—was defined as the number of square kilometers within a 5-km buffer zone around the original SDP sample frame. Geographic information system (GIS) shape files of the LGA boundaries and the original SDP sample frame were used.33
Figure 1.
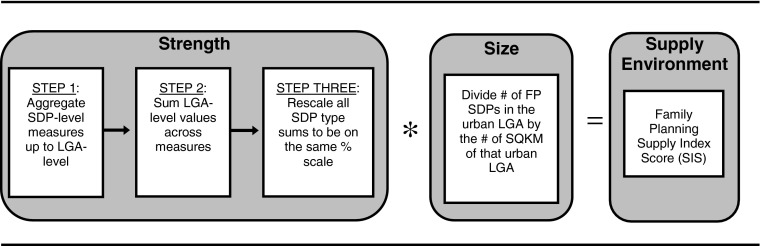
Steps taken to create the FP SIS for each type of FP SDP within each LGA.
Table 2.
Critical measures used to reflect the FP supply environment at the LGA level
| Measure | Definition (within each LGA) | SDPs measured at the LGA level | |
|---|---|---|---|
| Strength | Method availability | Mean percentage of possibly available modern FP methods actually provided across FP SDPs | Public HFs, preferred private HFs, private pharmacies, and private PMSs |
| Availability of injectables | Percentage of FP SDPs that provide an injectable form of contraception | ||
| Availability of IUDa | Percentage of private and public FP HFs that provide IUDs | ||
| Stockout day of interview | Percentage of SDPs with no stockouts of any normally available FP method on day of interview | ||
| Hours FP services are provided | Mean percentage of potential total hours that FP services are actually offered each week across SDPs | ||
| Partner consent | Percentage of SDPs that do not require partner consent to use/access any available form of modern method of contraception | ||
| Socially marketed products | Percentage of SDPs that provide socially marketed products | ||
| Size | FP service density | Number of FP SDPs per square kilometer of urban LGA | |
| Supply environment | FP SIS | Measure of the size and strength of the FP supply environment in each LGA |
aThis measure is only included among public and private HFs because pharmacies and PMSs do not sell the IUD
Community-Level Measures
Two measures of LGA-level poverty were derived using city-specific household wealth quintiles, where Q1 refers to the poorest 20 % of the sample surveyed in each city7:
- Distribution of poorest women. This continuous variable measures the percentage of Q1 that live within each LGA of the city:
- Proportion of LGA in the lowest wealth quintile. This continuous variable measures the percentage of the individual sample within each LGA that falls within Q1:
Analysis
The public and private sector supply environments were evaluated and compared at the LGA level within and across the six selected cities in Nigeria, as well as in relation to measures of community-level wealth status. Descriptive analysis, including calculations of Pearson correlation coefficients, paired t tests, and independent-sample t tests, were used to identify patterns and assess whether and where disparities exist.
Findings
Strength of LGA-Level Public and Private Sector FP Supply Environment
Table 3 presents the scores for the strength of the FP supply environments at the aggregate LGA level for each FP SDP type. Paired t tests were used to compare the mean standardized strength of services between SDP types across LGAs. Results suggest that there is no significant difference between the average strength of public and preferred private FP HFs across LGAs. However, significant differences were found in the average FP supply environment strength of public HFs and pharmacies (t = 3.2, p = 0.01); public HFs and PMSs (t = 6.0, p = 0.00); preferred private HFs and pharmacies (t = 3.1, p = 0.01); preferred private HFs and PMSs (t = 8.7, p = 0.00); and pharmacies and PMSs (t = 4.2, p = 0.00) (see Table 3).
Table 3.
Summary statistics for the strength of the FP supply environment among different types of FP SDPs across LGAs
| FP SDP | Strength of contraceptive access/availability | |||
|---|---|---|---|---|
| Mean (% of total possible points) | Standard deviation | Minimum (% of total possible points) | Maximum (% of total possible points) | |
| Public HFs | 64.0 | 10.38 | 44.9 | 81.1 |
| Preferred private HFs | 62.1 | 7.88 | 48.2 | 82.9 |
| Pharmacies | 55.1 | 7.02 | 41.9 | 70.7 |
| PMSs | 44.5 | 6.72 | 30.0 | 56.1 |
Additionally, Pearson correlation coefficient tests were computed to assess the relationships between the strength of the different SDP FP supply environments across LGAs. Tests showed no statistically significant correlations at the 0.05 level between the strength of the LGA-level public sector and any of the LGA-level private sector supply environments. Further, there was no statistically significant correlation across LGAs between the strength of the preferred private HF and pharmacy supply environments, the preferred private HF and PMS supply environments, or the pharmacy and PMS supply environments.
Size of Supply Environment: FP Service Density
A strong contraceptive supply environment is based not only on the strength of its FP SDPs but also on the number and geographic distribution of FP SDPs that exist. Therefore, in addition to LGA-level strength of contraceptive access and availability, this study also considered the size of the environment in terms of LGA FP service density.
More variation was found in the density of FP SDP types within and across LGAs than in the strength of the different SDP supply environments. Specifically, the density of PMSs that carry contraceptives varied dramatically across LGAs, with the minimum number of FP PMSs per 100 km2 being 13 and the maximum being 498 (see Table 4).
Table 4.
Summary statistics of the FP service density among different types of SDPs across LGAs
| FP SDPs | FP service density (number of FP SDPs/100 km2) | |||
|---|---|---|---|---|
| Mean | Standard deviation | Minimum | Maximum | |
| Public HFs | 12.4 | 13.26 | 1.0 | 51.0 |
| Preferred private HFs | 13.2 | 11.87 | 1.0 | 47.0 |
| Pharmacies | 33.4 | 31.63 | 3.0 | 99.0 |
| PMSs | 178.0 | 158.51 | 13.0 | 498.0 |
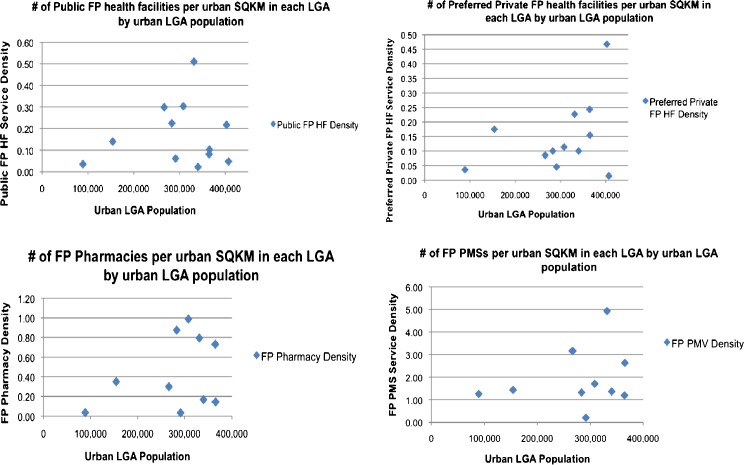
The variation in the geographic density of SDPs may be related to the size of the LGA population. A larger population might result in higher demand for services and, therefore, higher service density. However, within the urban LGAs of Nigeria—for which population estimates were available34—there were no significant correlations at the 0.05 level between the density of any FP SDP type and the size of the urban LGA population (see Fig. 2 and Table 5).
Figure 2.
FP service density by size of urban LGA population in each LGA34.
Table 5.
FP service density by urban area (in square kilometers) and size of urban population
| City | LGA | Populationa | Urban area (km2) | Public HFs | Preferred private HFs | Pharmacies | PMSs | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| No. sell FP | Density (no./km2) | No. sell FP | Density (no./km2) | No. sell FP | Density (no./km2) | Proxyb no. sell FP | Density (no./km2) | ||||
| Zaria | Sabon Gari | 291,358 | 243.22 | 15 | 0.06 | 11 | 0.05 | 8 | 0.03 | 50 | 0.21 |
| Zaria | 406,990 | 272.39 | 13 | 0.05 | 4 | 0.01 | 11 | 0.04 | 52 | 0.19 | |
| Kaduna | Chikun | 512.66 | 6 | 0.01 | 9 | 0.02 | 31 | 0.06 | 262 | 0.51 | |
| Kaduna N | 364,575 | 86.15 | 7 | 0.08 | 21 | 0.24 | 63 | 0.73 | 103 | 1.20 | |
| Kaduna S | 402,731 | 59.87 | 13 | 0.22 | 28 | 0.47 | 25 | 0.42 | 298 | 4.98 | |
| Abuja | AMAC | 918.28 | 13 | 0.01 | 24 | 0.03 | 200 | 0.22 | 117 | 0.13 | |
| Bwari | 385.49 | 5 | 0.01 | 2 | 0.01 | 30 | 0.08 | 72 | 0.19 | ||
| Ilorin | Ilorin E | 106.53 | 4 | 0.04 | 8 | 0.08 | 22 | 0.21 | 16 | 0.15 | |
| Ilorin S | 36.64 | 5 | 0.14 | 10 | 0.27 | 8 | 0.22 | 120 | 3.28 | ||
| Ilorin W | 365,221 | 97.30 | 10 | 0.10 | 15 | 0.15 | 14 | 0.14 | 256 | 2.63 | |
| Offa | 88,975 | 84.77 | 3 | 0.04 | 3 | 0.04 | 3 | 0.04 | 107 | 1.26 | |
| Ibadan | Ibadan N | 308,119 | 26.33 | 8 | 0.30 | 3 | 0.11 | 26 | 0.99 | 45 | 1.71 |
| Ibadan NE | 331,444 | 17.64 | 9 | 0.51 | 4 | 0.23 | 14 | 0.79 | 87 | 4.93 | |
| Ibadan NW | 154,029 | 28.56 | 4 | 0.14 | 5 | 0.18 | 10 | 0.35 | 41 | 1.44 | |
| Ibadan SE | 266,457 | 23.40 | 7 | 0.30 | 2 | 0.09 | 7 | 0.30 | 74 | 3.16 | |
| Ibadan SW | 283,098 | 40.03 | 9 | 0.22 | 4 | 0.10 | 35 | 0.87 | 53 | 1.32 | |
| Benin | Egor | 340,287 | 89.92 | 2 | 0.02 | 9 | 0.10 | 15 | 0.17 | 123 | 1.37 |
| Ikpoba-Okha | 194.13 | 5 | 0.03 | 12 | 0.06 | 6 | 0.03 | 251 | 1.29 | ||
| Oredo | 91.44 | 7 | 0.08 | 24 | 0.26 | 60 | 0.66 | 353 | 3.86 | ||
aSource: http://www.citypopulation.de/php/nigeria-admin.php. Population census data are only available at the full LGA level; urban areas are not delineated from nonurban areas. Therefore, for the purposes of this study, population estimates were only included for LGAs that are almost entirely urban. An LGA was considered to be almost entirely urban if the entire square kilometer area of the LGA minus the square kilometer area from which the SDP sample frame was taken within that LGA was <30 km2
bThe number of FP SDPs is based on SDP census data in the original SDP sample frame. The number of FP PMSs was estimated by multiplying the ratio of surveyed PMSs that sell FP by the total number of PMSs in the original SDP sample frame for each city. The same method was used to estimate the number of pharmacies that sell FP in Abuja and Kaduna
The density of FP services within an LGA may also vary in conjunction with the strength of services within that LGA. However, there were no significant correlations at the 0.05 level between urban LGA-level strength and density of FP services, regardless of the SDP type.
Finally, the density of one type of FP SDP has the potential to drive and/or curb the density of another in and across LGAs. In Nigeria, the density of different FP SDP types were only positively significantly correlated between PMSs and preferred private HFs (r = 0.82, p < 0.001); PMSs and public HFs (r = 0.70, p < 0.001); and pharmacies and public HFs (r = 0.70, p < 0.001). There was no statistically significant correlation between the FP service densities of preferred private HFs and public HFs, preferred private HFs and pharmacies, or PMSs and pharmacies.8
Overall Supply Index Scores
Table 6 presents the overall SISs for each SDP type within each LGA. Because there was only moderate variation in the LGA-level strength measures for the different SDP types, the SISs were predominantly driven by the number of FP facilities per square kilometer in each LGA. Pearson correlation coefficient tests showed that the density of each SDP type was strongly correlated at the 0.01 level with the SIS of their respective SDP type.
Table 6.
FP environment strength, size, and SIS for each type of SDP within each LGA
| City | LGA name | Public FP HFs | Private FP HFs | FP Pharmacies | FP PMSs | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Strength | Size | SIS | Strength | Size | SIS | Strength | Size | SIS | Strength | Size | SIS | ||
| Zaria | Sabon Gari | 45.00 | 0.06 | 2.70 | 59.39 | 0.05 | 2.97 | 65.20 | 0.03 | 1.96 | 43.18 | 0.21 | 9.07 |
| Zaria | 44.91 | 0.05 | 2.25 | 60.98 | 0.01 | 0.61 | 49.99 | 0.04 | 2.00 | 48.53 | 0.19 | 9.22 | |
| Kaduna | Chikun | 56.60 | 0.01 | 0.57 | 62.22 | 0.02 | 1.24 | 58.69 | 0.06 | 3.52 | 50.47 | 0.51 | 25.74 |
| Kaduna N | 64.27 | 0.08 | 5.14 | 68.78 | 0.24 | 16.51 | 54.22 | 0.73 | 39.58 | 56.06 | 1.20 | 67.27 | |
| Kaduna S | 56.06 | 0.22 | 12.33 | 58.64 | 0.47 | 27.56 | 58.94 | 0.42 | 24.75 | 48.99 | 4.98 | 243.95 | |
| Abuja | AMAC | 67.53 | 0.01 | 0.68 | 67.95 | 0.03 | 2.04 | 52.07 | 0.22 | 11.46 | 43.12 | 0.13 | 5.61 |
| Bwari | 76.16 | 0.01 | 0.76 | 65.00 | 0.01 | 0.65 | 53.62 | 0.08 | 4.29 | 45.73 | 0.19 | 8.69 | |
| Ilorin | Ilorin E | 81.12 | 0.04 | 3.24 | 59.12 | 0.08 | 4.73 | 61.03 | 0.21 | 12.82 | 29.96 | 0.15 | 4.49 |
| Ilorin S | 76.90 | 0.14 | 10.77 | 57.35 | 0.27 | 15.48 | 70.71 | 0.22 | 15.56 | 37.57 | 3.28 | 123.22 | |
| Ilorin W | 68.51 | 0.10 | 6.85 | 63.25 | 0.15 | 9.49 | 61.76 | 0.14 | 8.65 | 43.98 | 2.63 | 115.66 | |
| Offa | 60.75 | 0.04 | 2.43 | 62.93 | 0.04 | 2.52 | 54.23 | 0.04 | 2.17 | 32.07 | 1.26 | 40.40 | |
| Ibadan | Ibadan N | 61.74 | 0.30 | 18.52 | 71.43 | 0.11 | 7.86 | 55.29 | 0.99 | 54.74 | 47.79 | 1.71 | 81.73 |
| Ibadan NE | 65.86 | 0.51 | 33.59 | 67.91 | 0.23 | 15.62 | 46.05 | 0.79 | 36.38 | 44.50 | 4.93 | 219.40 | |
| Ibadan NW | 59.55 | 0.14 | 8.34 | 49.50 | 0.18 | 8.91 | 50.03 | 0.35 | 17.51 | 47.04 | 1.44 | 67.74 | |
| Ibadan SE | 64.26 | 0.30 | 19.28 | 48.20 | 0.09 | 4.34 | 41.94 | 0.30 | 12.58 | 51.18 | 3.16 | 161.73 | |
| Ibadan SW | 69.61 | 0.22 | 15.31 | 82.91 | 0.10 | 8.29 | 56.31 | 0.87 | 48.99 | 53.21 | 1.32 | 70.24 | |
| Benin | Egor | 81.09 | 0.02 | 1.62 | 56.72 | 0.10 | 5.67 | 47.37 | 0.17 | 8.05 | 39.21 | 1.37 | 53.72 |
| Ikpoba-Okha | 54.57 | 0.03 | 1.64 | 55.58 | 0.06 | 3.33 | 49.87 | 0.03 | 1.50 | 40.56 | 1.29 | 52.33 | |
| Oredo | 62.04 | 0.08 | 4.96 | 62.59 | 0.26 | 16.27 | 60.27 | 0.66 | 39.78 | 41.92 | 3.86 | 161.82 | |
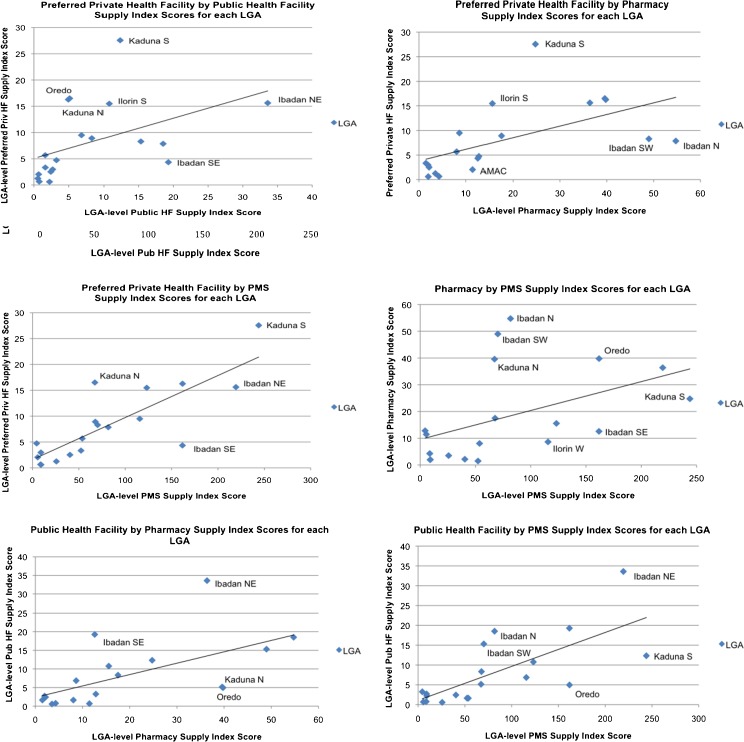
That said, including the strength of the service environment in the overall SIS resulted in significant correlations between all FP SDP type supply environments. The LGA-level SISs for public FP HFs were significantly and positively correlated with preferred private FP HFs (r = 0.46, p = 0.05), FP pharmacies (r = 0.61, p = 0.01), and FP PMSs (r = 0.72, p = 0.00). Additionally, the LGA-level SISs for each private sector FP SDP type were positively correlated with one another: preferred private HFs were correlated with pharmacies (r = 0.57, p = 0.01); preferred private HFs were correlated with PMSs (r = 0.82, p = 0.00); and pharmacies were correlated with PMSs (r = 0.46, p = 0.05). The graphs in Fig. 3 demonstrate that the distribution of scores among each SDP type is skewed to the low end of the respective SDP SIS range. In fact, there seems to be a cluster of nine LGAs with scores for all SDP types that fall below the corresponding SDP type median: Chikun, AMAC, Bwari, Ikpoba-Okha, Egor, Zaria, Offa, Sabon Gari, and Ilorin East. Wider dispersion exists among LGAs with higher scores.
Figure 3.
Significant positive correlations between LGA SISs by type of FP SDP.
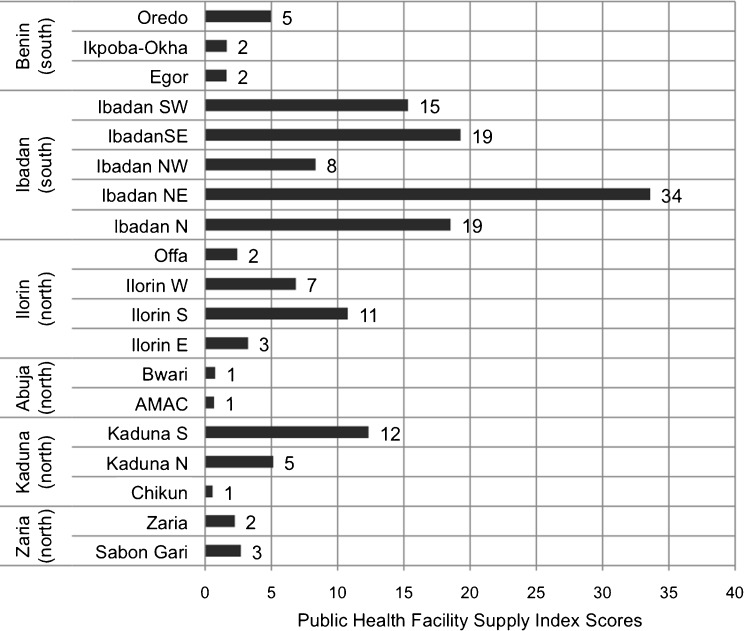
Public and Private Supply Environment: Regional Differences
Broad historical, political, and religious differences exist between the north and south of Nigeria, warranting a comparison of the FP supply environments between the two regions. Therefore, an independent-samples t test was conducted to compare the SISs of the different FP SDP types in the LGAs located in the north (in the cities of Abuja, Ilorin, Kaduna, and Zaria) versus those in the south (in the cities of Ibadan and Benin City). Results suggest that the public sector HF supply environment is significantly better in the south (M = 12.9, SD = 11.0) as compared to the north (M = 4.3, SD = 4.1; t(2.4) = 17, p = 0.03). In fact, even without considering the outlier, Ibadan NE, the average SIS for LGAs in the south is almost 2.5 times higher than the average LGA score in the north. Furthermore, the public sector HF environment appears to be strongest in Ibadan, with four LGA-level SISs that are at least five times greater than almost half (47 %) of all of the urban LGAs included in this study (see Fig. 4).
Figure 4.
Public HF SISs by region.
Among private sector SISs, independent-sample t tests only revealed a significant difference between the pharmacy scores of the south (M = 27.4, SD = 20.0) and the north (M = 11.5, SD = 11.7; t(17) = 2.2, p = 0.04). These results suggest that there is better FP access and availability among pharmacies in the south than in the north; however, there are no significant regional differences among preferred private HFs and PMSs.
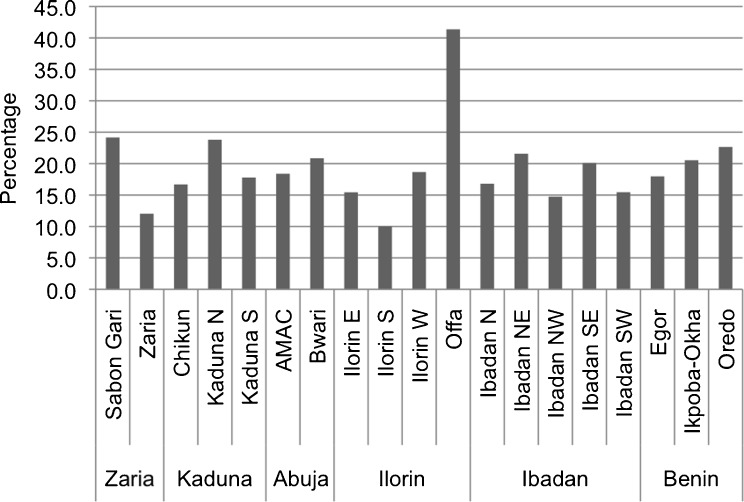
Supply Environment and Poverty
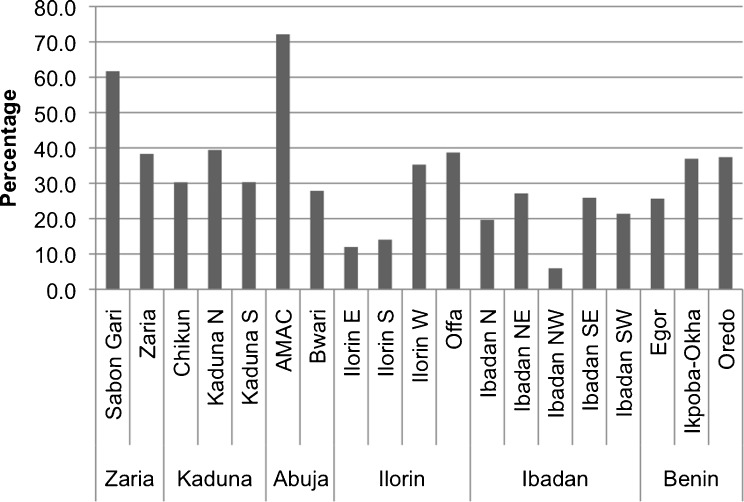
Addressing poverty-related inequalities in FP behavior and fertility outcomes may require targeted interventions that improve contraceptive access and availability for the urban poor. In order to assess what, if anything, needs to be done, it is important to not only identify possible gaps and inequalities in the supply environment but also to define the target population and identify where they live.17 If wealth was evenly distributed across each city, we would expect that, by definition, approximately 20 % of the sample in each LGA would fall within Q1.9 Instead, as seen in Fig. 5, it seems that some LGAs are slightly better off than others; the observed percentage of Q1 in each LGA sample varies across LGAs by a standard deviation of 6.50 from the mean, 19.4 % (min = 10.0 %, max = 41.4 %).
Figure 5.
Percentage of sample in each LGA that falls within Q 1.
LGAs that are disproportionately poor are not necessarily the same LGAs where most of the urban poor live. Concentration of poverty is a function of both the distribution of the poor, as well as the distribution of the total population across LGAs. Where Fig. 5 shows the proportion of each LGA that is in Q1, Fig. 6 demonstrates where most of each city’s Q1 can be found.
Figure 6.
Percentage of city’s total Q 1 who live within each urban LGA.
Despite the disparities in wealth distribution and SISs across LGAs, Pearson correlation coefficient tests showed no significant correlation between the SIS of any SDP type and the percentage of each LGA that are in Q1. Furthermore, there is no clear pattern between the SISs and the distribution of Q1 across each city. For example, the concentration of Q1 in Oredo is not appreciably different from that in Ikpoba-Okha; however, the two LGAs have markedly different SISs across SDP types. Also, Oreda in Benin City is the only LGA that contains both the highest percentage of Q1 and the highest LGA-level SIS for each SDP type (see Table 7).
Table 7.
Distribution of city’s poorest women across LGAs compared to private and public FP SIS
| City | LGA | Urban LGA populationa | Percentage of city’s poorest women in each LGA | Public HF SIS | Private HF SIS | Pharmacy SIS | PMS SIS |
|---|---|---|---|---|---|---|---|
| Zaria | Sabon Gari | 291,358 | 61.69 | 2.7 | 3.0 | 2.0 | 9.1 |
| Zaria | 406,990 | 38.31 | 2.3 | 0.6 | 2.0 | 9.2 | |
| Kaduna | Chikun | 30.26 | 0.6 | 1.2 | 3.5 | 25.7 | |
| Kaduna N | 364,575 | 39.44 | 5.1 | 16.5 | 39.6 | 67.3 | |
| Kaduna S | 402,731 | 30.30 | 12.3 | 27.6 | 24.8 | 244.0 | |
| Abuja | AMAC | 72.14 | 0.7 | 2.0 | 11.5 | 5.6 | |
| Bwari | 27.86 | 0.8 | 0.7 | 4.3 | 8.7 | ||
| Ilorin | Ilorin E | 11.98 | 3.2 | 4.7 | 12.8 | 4.5 | |
| Ilorin S | 14.05 | 10.8 | 15.5 | 15.6 | 123.2 | ||
| Ilorin W | 365,221 | 35.27 | 6.9 | 9.5 | 8.7 | 115.7 | |
| Offa | 88,975 | 38.70 | 2.4 | 2.5 | 2.2 | 40.4 | |
| Ibadan | Ibadan N | 308,119 | 19.65 | 18.5 | 7.9 | 54.7 | 81.7 |
| Ibadan NE | 331,444 | 27.13 | 33.6 | 15.6 | 36.4 | 219.4 | |
| Ibadan NW | 154,029 | 5.94 | 8.3 | 8.9 | 17.5 | 67.7 | |
| Ibadan SE | 266,457 | 25.91 | 19.3 | 4.3 | 12.6 | 161.7 | |
| Ibadan SW | 283,098 | 21.37 | 15.3 | 8.3 | 49.0 | 70.2 | |
| Benin | Egor | 340,287 | 25.66 | 1.6 | 5.7 | 8.1 | 53.7 |
| Ikpoba-Okha | 36.94 | 1.6 | 3.3 | 1.5 | 52.3 | ||
| Oredo | 37.40 | 5.0 | 16.3 | 39.8 | 161.8 |
Bold and Italicized values show the LGAs that contain the highest percentage of each city’s poorest women, as well as the LGAs that have the highest SIS for each SDP type within each city
aSource: http://www.citypopulation.de/php/nigeria-admin.php. Population census data are only available at the full LGA level; urban areas are not delineated from nonurban areas. Therefore, for the purposes of this study, population estimates were only included for LGAs that are almost entirely urban. An LGA was considered to be almost entirely urban if the entire square kilometer area of the LGA minus the square kilometer area from which the SDP sample frame was taken within that LGA was <30 km2
Discussion
Over 50 % of the world’s population lives in an urban area. Due in large part to high levels of fertility in urban areas of the developing world, that number is projected to increase to two thirds by 2050.1 Over time, there will be more people seeking employment, housing, and other limited resources in urban areas, further exacerbating already depleted living conditions and overall poor health.14,35 As a result, governments and donor organizations have become increasingly vigilant of poverty-related inequalities in urban fertility, as well as in urban contraceptive use behaviors and service utilization.4,14,35 At the same time, inequalities in the urban FP supply environment have become an area of interest for FP program and policy makers.24,36,37
As the most populous country in Africa, with an urban growth rate that indicates continued rapid population growth and urbanization, Nigeria is an opportune setting in which to explore inequalities in the urban FP supply environment. This study aimed to identify how the public and private sector FP supply environments vary and interact within and across urban LGAs. It also explored whether Nigeria’s urban FP supply environment is correlated with community-level wealth, so as to mitigate obstacles related to contraceptive access and availability among the urban poor.
Access to FP is contingent on the consistent and convenient availability of contraceptive methods. Therefore, two important components of contraceptive access and availability were used to define the aggregate-level FP supply environment: the overall strength of FP supply among the SDPs within each LGA and the density of SDPs that provide FP within each LGA.
Of note, the variable measuring average strength of each SDP type supply environment was low relative to the highest possible score that could have been given. These results imply that there is a substantial percentage of facilities in each LGA that either do not offer all of the methods that should normally be available in each SDP type, including important marker methods such as injectables and IUDs; experience commodity stockouts; are not open for the maximum number of hours per week; do not offer socially marketed products; and/or require partner consent in order to obtain at least one available method (not including forms of sterilization). Using paired t tests to compare the means of these component measures, it seems that, among public and preferred private sector FP HFs, the measures that increased the LGA strength scores were the number of hours that the SDPs were open, the percentage that sold IUDs, and the percentage that sold injectables. On the other hand, the overall strength scores for public and private HFs were brought down mostly due to the fact there was a large percentage of them in each LGA that required partner consent for reversible modern contraceptive methods. On average, 60.4 % of public and 76.1 % of preferred private FP HFs of them in each LGA required partner consent for at least one available method. Among pharmacies and PMSs, the component scores are highly correlated. However, 71.9 % of pharmacies offered the injectable form of modern contraception, which brought its overall mean strength score up, and only 17.5 % of PMSs offered the injectable, which pulled its overall mean strength score down.
Though one might have expected their scores to be even higher than was observed, it comes as little surprise that the highest standardized LGA-level strength scores were given to public and preferred private FP HFs. Public HFs more often follow government standards of service provision and are more easily monitored and regulated. Also, the private HFs used in this analysis were identified as preferred providers, which in and of itself might introduce positive bias to the results. Furthermore, pharmacies and PMSs are significantly less likely to provide socially marketed products or injectables than public and private HFs, and they are not open for as many hours.
On the other hand, although there was no discernible pattern for variation across LGAs, the average density of pharmacies and PMSs far outweighed those of the public and private FP HFs. Partly due to their sheer numbers, pharmacies and PMSs serve as crucial points for contraceptive commodity provision; as such, they are a good starting point for improving the FP supply environment in urban Nigeria.2,4,9
When comparing the calculated SISs for each SDP type, data showed wide variability in the public and private sectors across urban LGAs. Where there was a good public FP supply environment, there was increased likelihood that there was also a good private sector FP supply environment. This outcome could reflect greater demand for all health services and, thus, more providers within those LGAs. However, according to the analysis, the density of providers was not significantly correlated to urban LGA population size. Another interpretation of this outcome is that neither sector is working to fill service gaps where the other sector is lacking.23 Modern contraception may be more accessible if the government increased public FP HFs in areas that lack private SDPs.
Finally, there is no evidence of significant correlation between the public or private sector supply environments and the percentage of the population in each LGA that falls within the lowest wealth quintile. Furthermore, data suggest that the level of public and private sector contraceptive access and availability is not correlated with how the poorest women are distributed within each city. These results likely reflect the fact that the FP service environment answers to and/or serves needs that are not wealth-based. It also suggests that people who are poor are just as likely to live in a good FP supply environment as those who are wealthy, depending on the city in which they live. In order to better target the urban poor, efforts to improve FP access and availability may need to be focused, therefore, on urban LGAs, such as AMAC, Sabon Gari, and Offa, where the proportion of each city’s population of poorest women is highest.
Limitations
This study gives insight into Nigeria’s urban FP supply environment, highlighting possible gaps in public and private sector contraceptive access and availability; however, there are certain limitations to the study. Inherent to any secondary data analysis, the data used in this study lacked certain information needed to better fit its aims. For example, to reflect the strength of the supply environment, it might have been beneficial to also include measures such as distance between individuals/clusters and service outlets38 and location of SDPs in relation to highly traveled areas, such as markets, public transportation, etc.39 Also, measures to reflect cost of contraceptives and medical barriers, including FP restrictions based on age and parity, were collected, however, not in a manner that fit the methodology of this study. Therefore, though they are important indicators of access and availability, they were not used in analysis.
Additionally, the definition of “urban geographic area” varies widely from country to country. In this study, the unit of analysis was the urban portion of each LGA that falls within six selected Nigerian cities. However, though LGA boundaries have been defined, there are no official boundaries to geographically delineate their urban portions; and in some cases, the LGAs might be considered largely rural. Therefore, though GIS tools were used to make careful approximations of the urban areas within each LGA, calculations of service density may be overestimated or underestimated.
Because of the prohibitive cost of obtaining information from all SDPs, one sampling limitation was that there was not a census taken of pharmacies (in two cities) or PMSs (in any city). Instead, these SDPs were randomly sampled at the city level. Because the random sample was not stratified by LGA, there is no guarantee of proportionate SDP representation across LGAs due to sampling error. Also, the sampling frame of private HFs was designed as a census of private facilities reportedly used by surveyed individuals. The intention was to allow for individual linking of women to their preferred HFs. However, for the purposes of this study, it would have been beneficial to have a census or random sample of all private HFs, in order to assess and generalize the findings to the overarching private sector HF universe. Therefore, the degree to which this limitation is a problem for this study depends on the extent to which preferred private HFs represent the actual private HF frame. This information, however, is unknown.
Finally, one aim of this study was to obtain a better understanding of intracity distribution of public and private sector contraceptive access and availability. For that reason, data were analyzed at the LGA level instead of at the city level. However, the small number of urban LGAs included in the analysis limited the findings. To improve the statistical power of the results, future research would benefit from including more urban LGAs within Nigeria, which would require collecting data from more Nigerian cities.
Concluding Remarks and Recommendations
An outstanding question that is beyond the scope of this study is whether the geographic distribution of access and availability of contraceptives affects individual contraceptive use in urban areas. Unlike in most rural areas, services in urban areas are denser and travel between communities is easier. While rural populations tend to frequent SDPs based on proximity to residence and affordability, urban populations are exposed to a greater choice and number of SDPs and, therefore, demonstrate more complex patterns for accessing health care.4 Hence, further research should be conducted to analyze the relationship between a woman's immediate supply environment and demand-side factors, such as her use of contraception.
As it is, however, this study provides sound baseline measures of the strength and size of the private and public FP supply environments in urban Nigeria and documents for the first time spatial relationships between them. It identifies LGAs that have a weaker supply environment than others and compares those areas with those in which the urban poor can be found. Though no systematic pattern was identified between the private and public FP supply environment and urban poverty, program planners and policy makers can still use this information to identify localized areas in which efforts can be made to improve equal access to contraception. More specifically, it can be used as a gauge to determine possible windows for encouraging private sector expansion and/or redistribution of public services in highly concentrated poor areas that also suffer from poor FP access and availability.
Acknowledgments
The data for this research were made possible by the support from the Bill & Melinda Gates Foundation (BMGF) under the terms of the Measurement, Learning & Evaluation for the Urban Reproductive Health Project (MLE). The author’s views expressed in this publication do not necessarily reflect the views of BMGF or the MLE project. The authors would also like to thank Meghan Corroon for her insights into the data collection and analysis process, as well as Karen Foreit, Ph.D., and Herbert Peterson, M.D., for their review of earlier versions of the paper.
Appendix
Table 8.
Steps for creating LGA-level variables that were used to measure FP supply environment “strength” for each SDP type
| Variable | Survey question | SDP level | LGA level |
|---|---|---|---|
| Method choice: This continuous variable reflects FP availability and choice. It measures the mean. Percentage of possibly available modern contraceptives that are actually offered across FP SDPs within the LGA | “Does this SDP provide ‘X modern’ family planning method?”a | Created a dichotomous variable indicating whether each method was provided: yes = 1 and no = 0 | Averaged the no. of methods provided among each FP SDP type in the LGA |
| Added the total no. of methods available at each FP SPD | Divided that no. by the no. of methods that the respective FP SDP type could be offering, if they offered all possible contraceptive choices (10 for public and private HFs and 6 for PMSs and pharmacies) | ||
| The range was from 0 to 10 among public and private HFs and from 0 to 6 among private pharmacies and PMSs | Divided the final ratio by 100 | ||
| Availability of injectables: This variable is a marker of the availability of a commonly used form of modern FP in Nigeria. It measures the percentage of FP SDPs that provide an injectable form of contraception | “Does this SDP provide injectable contraceptives?” | Created a dichotomous variable indicating whether the SDP provides the method: yes = 1 and no = 0 | Summed the total no. of FP SDPs that provided injectables |
| Divided that no. by the total no. of FP SDPs within the LGA | |||
| Multiplied the final ratio by 100 | |||
| Availability of IUD: This variable is a marker of superior method choice. It measures the percentage of private and preferred public FP HFs that provides an IUD within the LGA | “Does this SDP provide the IUD?” | Created a dichotomous variable indicating whether the SDP provides the method: yes = 1 and no = 0 | Summed the total no. of FP SDPs that provided IUDs |
| Divided that no. by the total no. of FP SDPs within the LGA | |||
| Multiplied the final ratio by 100 | |||
| Stockouts: This variable is an indicator of stockout frequency. It measures the percentage of FP SDPs that had all normally available FP methods/brands in stock on the day of the interview | “Is X modern method currently available?”b | Created a dichotomous variable indicating current method availability: yes = 0 and no = 1 (“don’t know” was marked as missing) | Summed the no. of FP SDPs that had a stockout of at least 1 modern FP method |
| If the SDP did not carry a certain method, then the answer was not applicable | Divided that no. by the total no. of FP SDPs in the LGA | ||
| Summed the no. of normally available methods/brands that were not available on the day of the interview | To put the measure on the same percentage scale as the other measures, subtracted the ratio from one and multiplied it by 100 | ||
| If the sum was greater than “0” (e.g., that SDP had at least 1 method out of stock), then that SDP was marked as “1”; otherwise the SDP was marked as “0” | Example: [(total no. of SDPs at least one stockout on the day of the interview / total no. of FP SDPs) − 1] × 100 | ||
| Hours provide FP services: This continuous variable is an indicator of physical access. It measures the average percentage of potential total hours (168 h in a week = 24 h × 7 days) that FP services/commodities are actually offered each week across SDPs | PMSs and pharmacies: “On average, how many hours per day is this (SDP) open?; and on average, how many days per week is this (SDP) open?” | PMSs and pharmacies: Multiplied the average no. of hrs the SDP was open by the average no. of days the SDP was open each week | Averaged the no. of hours that each SDP type was open in a week across the LGA (the range was 0 to 168 h) |
| Made the assumption that if a pharmacy or PMS offers FP, then they do so at all times that the facility is open | Divided that no. by the maximum no. of hours that each SDP could be and/or are known, in cases, to be open (168 h/week = 24 h × 7 days) | ||
| Public and private HFs: “What time does the facility typically open?; what time does the facility typically close?; and how many days per week is FP counseling and services available?” | Public and private HFs: Subtracted the time open from the time closed and multiplied that no. by the no. of days FP is offered in the week | ||
| Divided the final ratio by 100 | |||
| For all data sets, the response “don’t know” was recoded as missing and “open 24 h” were recoded as 24 | |||
| Partner consent: This variable is an indicator of administrative accessibility. It measures the percentage of FP SDPs in each LGA that require partner consent for at least one available modern method of contraception | “Do you require a partner’s consent before you will provide X modern method?” | Created dichotomous variable indicating partner requirement for each method: yes = 1 and no = 0 | Summed the no. of FP SDPs that were marked “1” |
| Summed the answers within each SDP | Divided that no. by the total no. of FP SDPs in the LGA | ||
| If the sum was >“0” (e.g., that SDP required partner consent for at least one available FP method), then the SDP was marked as “1”; otherwise, it was “0” | Multiplied the final ratio by 100 | ||
| Socially marketed contraceptives: This variable is an indicator of economic accessibility. It measures the percentage of FP SDPs that provide socially marketed contraceptives (contraceptives that are often sold at a lower price than commercial brands) within each LGA | “Does this SDP have socially marketed contraceptive products in stock?” | Created a dichotomous variable indicating whether the SDP provides at least one socially marketed brand: yes = 1 and no = 0 | Summed the total no. of FP SDPs that provide socially marketed contraceptives within the LGA |
| Divided that no. by the total no. of FP SDPs in the LGA. | |||
| Multiplied the final ratio by 100 |
aModern methods included (1) combined oral contraceptive pill, (2) progesterone-only pill, (3) emergency contraception, (4) male condom, (5) female condom, (6) injectables, (7) implants, (8) IUD, (9) female sterilization, and (10) male sterilization. The pharmacies and PMSs were not asked about forms of sterilization, the IUD, or implants
bThese methods included (1) combined oral contraceptive pill, (2) progesterone-only pill, (3) emergency contraception, (4) male condom, (5) female condom, (6) injectables, (7) implants, (8) IUD. Forms of sterilization were not included
Footnotes
Nigeria is subdivided into states, which are further subdivided into LGAs. This study looks at the urban portions of the LGAs that lie within six cities of Nigeria. Please see the “Research Design and Methods” section for more details.
The MLE project was funded by the Bill & Melinda Gates Foundation to conduct a rigorous impact evaluation of their Urban Reproductive Health Initiative (URHI). The URHI aims to promote innovative FP programs in urban areas of four countries: Uttar Pradesh, India; Nigeria; Kenya; and Senegal. The goal of the MLE is to identify the most effective and cost-efficient programmatic approaches to increase access to, demand for, and use of high-quality FP among the urban poor in each of the URHI intervention sites.
The agencies included the National Bureau of Statistics, Federal Ministry of Health (MoH), National Primary Health Care Development Agency, State MoH offices, Guild of Medical Directors, Association of General Private Medical Practitioners, Association of Private Nurse Practitioners, Association of Community Pharmacists, Association of Proprietary and Patent Medicine Dealers, and a list of registered pharmacies.
In Ibadan, due to the large number of facilities, only the health facility most commonly mentioned by women in the same cluster was considered to be the preferred facility.32
This measure is being used to reflect the availability of a marker method. According to representative data collected by MLE in 2010, the most commonly used or ever-used modern contraceptive methods among women in union, living in urban areas of Nigeria is the male condom or injectable.2
It is more difficult to obtain an IUD in Nigeria than other reversible modern methods, and yet, it is one of the more effective contraceptive choices for preventing pregnancy.2 Therefore, this measure is being used as a high-level marker of method choice. Note that pharmacies and PMSs do not sell the IUD, so it is only included for public and private health facilities.
MLE calculated household wealth scores using principal component analysis and assigned those scores to the respective household members. They then ranked the individuals living in the same city from poorest to least poor and divided the resulting data into quintiles.
These correlations were not quite statistically significance at the 5 % level.
Reminder: The sample was designed to produce estimates with acceptable precision at the city level not the LGA level; therefore, there will be potentially large sampling error at the LGA level.
References
- 1.Central Intelligence Agency. The world factbook. https://www.cia.gov/library/publications/the-world-factbook/geos/ni.html (2012). Accessed March 2012.
- 2.Fotso JC, Ajayi JO, Idoko EE, et al. Family planning and reproductive health in urban Nigeria: levels trends and differentials. MLE Technical Working Paper 2-2010. Measure, Learning & Evaluation Project; 2011.
- 3.United Nations, Department of Economic and Social Affairs, Population Division. World population prospects: the 2010 revision, highlights and advance tables. http://www.un.org/esa/population/unpop.htm (2011). Accessed February 2012.
- 4.Measurement Learning & Evaluation Project, Nigerian Urban Reproductive Health Initiative, National Population Commission. 2010–2011 Nigeria baseline survey for the Urban Reproductive Health Initiative. http://www.nurhi.org/sites/nurhi.k4health.org/files/2011_Nigeria_Urban_Reproductive_Health_Survey_FINAL.pdf (2012). Accessed March 2012.
- 5.United Nations Statistics Division, Department of Economic and Social Affairs, United Nations. Millennium development goals indicators: the official United Nations site for the MDG indicators. http://mdgs.un.org/unsd/mdg/SeriesDetail.aspx?srid=710&crid=566 (2012). Accessed February 2013.
- 6.World Health Organization Centre for Health Development UNHSP. Hidden cities: unmasking and overcoming health inequities in urban settings. http://www.hiddencities.org/report.html (2010). Accessed February 2013.
- 7.Brockerhoff MA. An urbanizing world. Popul Bull. 2000;55(3):1–44. [Google Scholar]
- 8.Ezech AC, Kodzi I, Emina J. Reaching the urban poor with family planning services. Stud Fam Plan. 2010;41(2):109–116. doi: 10.1111/j.1728-4465.2010.00231.x. [DOI] [PubMed] [Google Scholar]
- 9.National Population Commission (NPC) [Nigeria] and ICF Macro. Nigeria demographic and health survey 2008. Abuja, Nigeria: National Population Commission and ICF Macro; 2009.
- 10.Bongaarts J. A framework for analyzing the proximate determinants of fertility. Popul Dev Rev. 1978;4(11):104–132. [Google Scholar]
- 11.Nigeria National Population Commission. Population policy and action. http://www.population.gov.ng/index.php/population-programmes/population-policy (2012). Accessed January 2013.
- 12.Winfrey W, Heaton L, Fox T, Adamchak S. Factors influencing the growth of the commercial sector family planning service provision. The POLICY Project Working Paper No. 6. Washington, DC: The Futures Group International; 2000.
- 13.Khan S, Mishra V, Arnold F, Abderrahim N. Contraceptive trends in developing countries. DHS Comparative Reports No. 16. Calverton, MD: Macro International; 2007.
- 14.Speizer IS, Nanda P, Achyut P, Pillai G, Guilkey DK. Family planning use among urban poor women from six cities of Uttar Pradesh, India. J Urban Health. 2012 doi: 10.1007/s11524-011-9667-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stephenson R, Hennink M. Barriers to family planning service use among the urban poor in Pakistan. Opportunities and Choices Working Paper No. 2; 2004.
- 16.Kongsri S, Limwattananon S, Sirilak S, Prakongsai P, Tangcharoensathien V. Equity of access to and utilization of reproductive health services in Thailand: national Reproductive Health Survey data, 2006 and 2009. Reprod Health Matters. 2011;19(37):86–97. doi: 10.1016/S0968-8080(11)37569-6. [DOI] [PubMed] [Google Scholar]
- 17.Foreit K. Addressing poverty: a guide for considering poverty-related and other inequities in health. USAID and MEASURE evaluation. http://www.cpc.unc.edu/measure/publications/ms-08-27:70 (2012).
- 18.Sedgh G, Hussain R, Bankole A, Singh S. Women with an unmet need for contraception in developing countries and their reasons for not using a method. Occasional Report No. 37. New York: Guttmacher Institute; June 2007.
- 19.Gillespie D, Ahmed S, Tsui A, Radloff S. Unwanted fertility among the poor: an inequity? Bull World Health Organ. 2007;85:100–107. doi: 10.2471/BLT.06.033829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Federal Government of Nigeria. Health policy project. RAPID: the change we seek, Nigeria. http://www.healthpolicyproject.com/pubs/37_FINALRAPIDNigeriaFertilityMCHNovFORWEfinal.pdf (2011). Accessed January 2013.
- 21.Guengant J-P, May J. Proximate determinants of fertility in sub-Saharan Africa and their possible use in fertility projections. United Nations, Department of Economic and Social Affairs, Expert Paper No. 2011/13. Paper presented at the United Nations Expert Group Meeting on Completing the Fertility Transition, New York; 2011.
- 22.Ogbaje E, Igharo E. Contraceptive security in Nigeria: assessing strengths and weaknesses. USAID | DELIVER PROJECT, Task Order 1. Arlington, MD: USAID; 2009.
- 23.SHOPS Project, USAID. Nigeria private health sector assessment. Brief. Strengthening Health Outcomes through the Private Sector Project, Abt Associates. Bethesda: USAID; 2012.
- 24.Sharma S, Dayaratna V. Creating conditions for greater private sector participation in achieving contraceptive security. Health Policy. 2005;71:347–357. doi: 10.1016/j.healthpol.2004.09.010. [DOI] [PubMed] [Google Scholar]
- 25.Peters DH, Mirchandani GG, Hansen PM. Strategies for engaging the private sector in sexual and reproductive health: how effective are they? Health Policy Plan. 2004;19(Suppl. 1):i5–i21. doi: 10.1093/heapol/czh041. [DOI] [PubMed] [Google Scholar]
- 26.Berman P, Rose L. The role of private providers in maternal and child health and family planning services in developing countries. Health Policy Plan. 1996;11(2):142–155. doi: 10.1093/heapol/11.2.142. [DOI] [PubMed] [Google Scholar]
- 27.Patouillard E, Goodman CA, Hanson KG, Mills AJ. Can working with the private for-profit sector improve utilization of quality health services by the poor? A systematic review of the literature. Int J Equity Health. 2007;6:17. [DOI] [PMC free article] [PubMed]
- 28.Montagu D, Prata N, Campbell MM, Walsh J, Orero S. Kenya: reaching the poor through the private sector—a network model for expanding access to reproductive health services. Washington, DC: The International Bank for Reconstruction and Development/The World Bank; 2005. [Google Scholar]
- 29.Gage A, Zomahoun D. Influence of the service delivery environment on family planning outcomes in Nigeria. USAID and MEASURE Evaluation; 2011.
- 30.MEASURE Evaluation PRH. Commodity security and logistics. http://www.cpc.unc.edu/measure/prh/rh_indicators/crosscutting/commodity-security-and-logistics-1 (2011). Accessed December 2011.
- 31.Guilkey D, Speizer I, Lance P. Study design for the Measurement, Learning & Evaluation Project. Technical Working Paper: Measurement, Learning & Evaluation Project for the Urban Reproductive Health Initiative; 2009.
- 32.Measurement Learning & Evaluation Project, Nigerian Urban Reproductive Health Initiative, National Population Commission. 2010–2011 Baseline facility survey for the Nigerian urban reproductive health initiative. http://www.urbanreproductivehealth.org/sites/mle/files/nurhi_baseline_facility_report_23feb12_final.pdf (2012). Accessed March 2012.
- 33.Consultative Group on International Agricultural Research. Poverty mapping: income poverty, vitamin A and iodine in Nigeria. http://gisweb.ciat.cgiar.org/povertymapping/ (2006). Accessed January 2012.
- 34.City Population States and local government areas: the population of the states and local government areas of Nigeria. http://www.citypopulation.de/php/nigeria-admin.php (2012). Accessed October 2012.
- 35.Hanson K, Kumaranayake L, Thomas I. Ends versus means: the role of markets in expanding access to contraceptives. Health Policy Plan. 2001;16(2):125–136. doi: 10.1093/heapol/16.2.125. [DOI] [PubMed] [Google Scholar]
- 36.USAID | DELIVER PROJECT, Task Order 4. Nigeria: Contraceptive logistics management system assessment report. http://deliver.jsi.com/dhome/resources/publications/allpubs/pubsforcountry?p_persp=PERSP_DLVR_CNTRY_NG (2011). Accessed January 2012.
- 37.DELIVER and Task Order 1 of the USAID/Health Policy Initiative. Contraceptive security index 2006: a tool for priority setting and planning. Arlington: DELIVER, for the US Agency for International Development; December 2006.
- 38.Entwisle B, Hermalin A, Kamnuansilpa P, Chamratrithirong A. A multi-level model of family planning availability and contraceptive use in rural Thailand. Demography. 1984;21(4):559–574. doi: 10.2307/2060915. [DOI] [PubMed] [Google Scholar]
- 39.Tsui AO, Hogan DP, Teachman JD, Chanes CW. Community availability of contraceptives and family limitation. Demography. 1981;18(4):615–625. doi: 10.2307/2060950. [DOI] [PubMed] [Google Scholar]