Abstract
The objective of this study was to determine the conversion rate of human epidermal growth factor receptor 2 (HER2), estrogen receptor (ER) and progesterone receptor (PR) between primary tumors and metastatic lesions in advanced breast cancer. Patients with suspected diagnosis of locally recurrent or metastatic breast cancer, either at first relapse or after successive disease progressions, who had an appropriately preserved sample from a primary tumor and were scheduled for a biopsy of the recurrent lesion, were included. Blinded determinations of receptor status on paired samples were performed by immunohistochemistry and fluorescence in situ hybridization at a central laboratory and compared with those performed locally. Overall, 196 patients were included and 184 patients were considered evaluable. Reasons for non-evaluability included the inability to perform biopsy (n = 4) or biopsy results showing normal tissue (n = 3), benign disease (n = 3) or a second neoplasia (n = 2). Conversion rates determined at local level were higher than those determined centrally (HER2: 16 vs. 3 %, ER: 21 vs. 13 %, PR: 35 vs. 28 %, respectively). There was substantial agreement regarding the expression of HER2 in primary tumors and metastases, and ER at metastases, between local and central laboratories. PR at any site and ER at primary site showed moderate agreement. Oncologists altered their treatment plans in 31 % of patients whose tumor subtype had changed. These results reinforce the recommendation for performing confirmatory biopsies of metastases, not only to avoid misdiagnosis of breast cancer relapse, but also to optimize treatment (clinicaltrials.gov identifier: NCT01377363).
Keywords: Breast neoplasm, Conversion, Hormone receptors, HER2, Tumor markers
Introduction
The status of human epidermal growth factor receptor 2 (HER2) and the hormone receptors (HR), including estrogen receptor (ER) and progesterone receptor (PR), are the most relevant biomarkers for clinical practice, predicting response to anti-HER2 and endocrine therapies, respectively. Recently, the 12th St Gallen International Breast Cancer Conference Expert Panel recommends that the subtype classification of breast cancer, namely ‘HR positive’ (including ‘luminal A’ and ‘luminal B’ tumors), ‘HER2 amplified’ and ‘triple negative,’ should guide the treatment plan for breast cancer patients.
In spite of the relevance of receptor status, the choice of systemic treatment for advanced disease is more often based on the biological characteristics of the primary tumor at the time of initial diagnosis than of the recurrent lesion at the time of relapse. This may be because for many years, it has been assumed that the biomarker status of the primary tumor and its corresponding metastasis was not different. However, several studies have revealed the existence of variable discordances in receptor status between primary tumors and metastatic lesions that may be as high as 40 % for PR, 36 % for ER and 20 % for HER2 [1–3]. Reasons for these discrepancies may include the possibility that the molecular profile of breast cancers evolves over time and that biomarkers are heterogeneously expressed within the tumor [4] and technical inconsistencies in both tissue processing and sample evaluation. No prospective studies have addressed this question [5].
Being aware of the benefits that the correct systemic therapy provides to patients with advanced breast cancer, the Spanish Breast Cancer Research Group (GEICAM) performed a prospective, observational study to determine the conversion rate of receptor status (ER, PR and HER2) between the primary tumor and the recurrent lesion. Blinded determinations in paired samples were carried out at a central laboratory, and results were compared with those performed locally. Lastly, the impact of receptor discordance on the choice of subsequent systemic treatment was assessed.
Materials and methods
Study design
This was a multicenter, prospective, observational study coordinated by GEICAM and performed by the Medical Oncology departments in 31 hospitals. The study protocol was approved by the Institutional Review Board and the Ethics Committee of Hospital Provincial de Castellón (Spain), according to the requirements of the Spanish regulations (GEICAM 2009-03; clinicaltrials.gov identifier: NCT01377363). Study procedures were carried out in accordance with the Declaration of Helsinki, as revised in 2008, and good clinical practice guidelines. Written informed consent was obtained from all patients before enrollment.
Patient selection
The study included patients over the age of 18 with a suspected diagnosis of locally recurrent or metastatic breast cancer, either at first relapse or after successive disease progressions, between December 2009 and March 2011. Patients were required to have a formalin-fixed paraffin-embedded (FFPE) tissue sample from the primary tumor. Additionally, they had to be scheduled to undergo a biopsy of the recurrent or metastatic lesion within the next 6 weeks according to the routine clinical practice of the hospital. Biopsy could be performed by fine-needle aspiration, drainage of fluid cavities, core biopsy or surgical process. Study participants had to be capable of providing written, informed consent.
Exclusion criteria included in-breast recurrences, as well as second neoplasms, except for appropriately treated in situ cervical cancer and non-melanoma skin cancer.
Study procedures
Registration visit was completed within 6 weeks prior to the previously planned biopsy of the metastatic lesion. For each patient, date of birth, menopausal status, tumor stage, histological grade, receptor status (ER, PR and HER2) of the primary tumor according to local laboratory, type of surgery performed and antitumor treatment, location of the metastatic lesion and whether it was a first relapse or metastatic disease progression were recorded. At this visit, the treating oncologist declared the intended treatment plan for the patient.
Biopsies of the recurrent tumors were analyzed at the local laboratory, and blinded determinations of ER, PR and HER2 were centrally performed at the Pathology Department of Hospital Clinico Universitario de Valencia, (Spain), in paired samples of the primary tumor and the metastatic lesion. Once biopsy results at local level were available, the attending physician assessed the discordances between primary and metastatic tissues and whether the treatment plan should be modified.
Tissue processing
Central laboratory
All primary and metastatic tissues were analyzed at the same time and using the same methodology. For the expression of ER and PR, Benchmark XT instrument and the corresponding CONFIRM® antibodies (Ventana Medical Systems, Inc) were used. Both Allred score and percentage of nuclear staining were determined. Tumors with moderate-to-intense nuclear staining of ≥1 % or an Allred score ≥3 were considered ER positive or PR positive [6, 7]. IHC analysis for the expression of HER2 was conducted using the PATHWAY® anti-HER2 (4B5) monoclonal antibody (Ventana Medical Systems, Inc), considering the expression negative (0, 1+), indeterminate (2+) or positive (3+). When IHC yielded an indeterminate result for HER2 (2+) or when a discordant result between primary tumor and metastasis was observed, FISH was carried out using HER2 FISH PharmDx® kit (Dako Denmark A/S) and results were interpreted according to manufacturer’s instructions [8].
Local laboratory
Pathology report was retrieved from primary tumor diagnosis, and biopsies from metastasis were analyzed at the time of relapse. The methodology used for the analysis of these samples by IHC and FISH at local level was not standardized, and each site used instruments and commercial antibodies according to their own established criteria.
Statistical analysis
The primary objective of this study was to estimate the conversion rate of HER2 status between primary tumors and metastases in patients with advanced breast cancer. Secondary objectives included ER and PR conversion rate, evaluating the impact of the immunohistochemical subtype of the primary tumor on the conversion rate, assessing the concordance between the results obtained locally and centrally and estimating how the conversion rate of receptor status may influence the antitumor treatment. Three immunohistochemical subtypes were previously defined: (1) ‘HR-positive’ tumors (ER positive and/or PR positive and HER2 negative); (2) ‘HER2-amplified’ tumors (HER2 positive/any HR); and (3) ‘triple-negative’ tumors (ER negative, PR negative and HER2 negative).
According to previous studies, the estimated conversion rate of HER2 determined by IHC or FISH was around 10 % (range 4–20 %). Considering that this conversion rate was similar within each molecular subtype, with an alpha error of 0.05 for a bilateral contrast and an accuracy of ±0.09 %, 43 patients would be needed for each molecular subtype, requiring 129 patients. Assuming that 25 % of patients would be lost for analysis due to invalidate biopsies or inconclusive results, 172 patients were required to achieve the main objective of this study. However, in a preliminary analysis after including the first 84 patients, the observed HER2 conversion rate was 3.57 %, so the sample size was re-estimated with the same premises and 222 patients were found to be needed.
All statistical tests were performed against a two-sided, alternative hypothesis using a significance level of 0.05 and a 95 % confidence interval. The variability in the receptor expression results between local and central laboratories was measured using Cohen’s kappa index and interpreted according to Landis and Koch [9]. All these analyses were performed using SPSS statistics software version 17.0 (SPSS Inc, Chicago, Illinois, USA).
Results
Patient characteristics at baseline
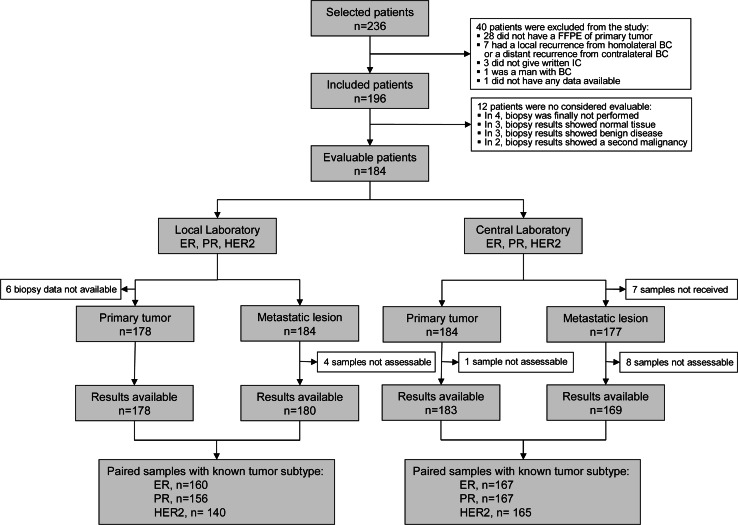
Over 15 months, 236 patients were preselected, 196 patients fulfilled selection criteria, and 184 patients were finally considered evaluable for this study. Twelve out of 196 patients initially included were considered not evaluable because the biopsy was not performed (n = 4) or results obtained showed normal tissue (n = 3), benign disease (n = 3) or a second neoplasm (n = 2) (Fig. 1). A summary of patient characteristics is shown in Table 1.
Fig. 1.
CONSORT diagram of the ConvertHER study
Table 1.
Patient characteristics at study inclusion (n = 196)
| Characteristics | n | % |
|---|---|---|
| Age (years), n = 196 | ||
| Median (range) | 57 (30–92) | |
| Menopausal status, n = 196 | ||
| Pre-/perimenopausal | 60 | 31 |
| Postmenopausal | 136 | 69 |
| Tumor stage at diagnosis, n = 165 | ||
| I | 26 | 16 |
| II | 82 | 50 |
| III | 36 | 22 |
| IV | 21 | 12 |
| Histological grade at diagnosis, n = 163 | ||
| Grade 1 | 25 | 15 |
| Grade 2 | 65 | 40 |
| Grade 3 | 73 | 45 |
| Time from diagnosis until first relapse, n = 194 | ||
| Median (range), years | 3.7 (0.0–19.3) | |
| Time from diagnosis until study inclusion, n = 195 | ||
| Median (range), years | 4.8 (0.0–19.3) | |
| Patient status at study inclusion, n = 196 | ||
| First relapse | 114 | 58 |
| Second or subsequent relapses | 82 | 42 |
| Location of the relapse, n = 191 | ||
| Locoregional lesion | 36 | 19 |
| Thoracic wall | 14 | 7 |
| Lymph nodes | 22 | 12 |
| Distant metastasis | 155 | 81 |
| Visceral metastasis | 65 | 34 |
| Liver | 44 | 23 |
| Lung/pleura | 17 | 9 |
| Other | 4 | 2 |
| Cutaneous and soft tissues | 42 | 22 |
| Bone tissue | 35 | 18 |
| Other | 20 | 11 |
| Treatment strategy, n = 196 | ||
| Primary surgery, n = 186 | ||
| Mastectomy | 106 | 54 |
| Breast conservative therapy | 80 | 41 |
| Neo(-adjuvant) treatment, n = 178 | ||
| Chemotherapy | 158 | 81 |
| Endocrine therapy | 120 | 61 |
| Targeted therapy | 15 | 8 |
| Radiotherapy | 112 | 57 |
| Antitumor treatment for advanced disease, n = 137 | ||
| Chemotherapy | 93 | 47 |
| Endocrine therapy | 81 | 41 |
| Targeted therapy | 59 | 30 |
| Radiotherapy | 50 | 26 |
Conversion rate of receptor status and changes in molecular subtypes between primary tumor and metastasis
Local laboratory
From the 184 evaluable patients, biopsy data were available from all metastatic lesions at local level, but original pathology report from the primary tumor could only be obtained from 178 patients. The conversion rate for HER2 was 16 % (95 % CI 10.7–23.4), similarly distributed in gain (14 patients, 10 %) or loss (9 patients, 6 %) of HER2 overexpression or amplification. Most of the conversions were seen in the HR-positive subtype, while only one patient in the triple-negative subtype and 2 patients in the HER2-amplified subtype changed the HER2 status (Table 2).
Table 2.
Conversion rates of receptor status between primary tumor and metastasis at local and central laboratories
| At local laboratory | Overall | HR positive | HER2 amplified | Triple negative | ||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | |
| ER, n = 160 | ||||||||
| No conversion | 126 | 79 | 94 | 82 | 18 | 60 | 14 | 93 |
| From positive to negative | 14 | 9 | 7 | 6 | 6 | 20 | 1 | 7 |
| From negative to positive | 20 | 12 | 14 | 12 | 6 | 20 | 0 | 0 |
| Fisher’s exact test | p = 0.032 | |||||||
| PR, n = 156 | ||||||||
| No conversion | 102 | 65 | 66 | 59 | 21 | 72 | 15 | 100 |
| From positive to negative | 34 | 22 | 28 | 25 | 6 | 21 | 0 | 0 |
| From negative to positive | 20 | 13 | 18 | 16 | 2 | 7 | 0 | 0 |
| Fisher’s exact test | p = 0.021 | |||||||
| HER2, n = 140 | ||||||||
| No conversion | 117 | 84 | 78 | 80 | 26 | 93 | 13 | 93 |
| From positive to negative | 9 | 6 | 8 | 8 | 0 | 0 | 1 | 7 |
| From negative to positive | 14 | 10 | 12 | 12 | 2 | 7 | 0 | 0 |
| Fisher’s exact test | p = 0.322 | |||||||
| At central laboratoy ER, n = 167 | ||||||||
| No conversion | 146 | 87 | 108 | 92 | 22 | 71 | 16 | 89 |
| From positive to negative | 16 | 10 | 10 | 8 | 6 | 19 | 0 | 0 |
| From negative to positive | 5 | 3 | 0 | 0 | 3 | 10 | 2 | 11 |
| Fisher’s exact test | p < 0.05 | |||||||
| PR, n = 167 | ||||||||
| No conversion | 120 | 72 | 86 | 73 | 18 | 58 | 16 | 89 |
| From positive to negative | 34 | 20 | 24 | 20 | 10 | 32 | 0 | 0 |
| From negative to positive | 13 | 8 | 8 | 7 | 3 | 10 | 2 | 11 |
| Fisher’s exact test | p = 0.042 | |||||||
| HER2, n = 165 | ||||||||
| No conversion | 160 | 97 | 113 | 97 | 31 | 100 | 16 | 94 |
| From positive to negative | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| From negative to positive | 5 | 3 | 4 | 3 | 0 | 0 | 1 | 6 |
| Fisher’s exact test | p = 0.443 | |||||||
ER estrogen receptor, HER2 human epidermal growth factor receptor 2, HR hormone receptor, PR progesterone receptor
For ER, the conversion rate was 21 % (95 % CI 15.7–28.9): a switch from ER positive to ER negative was identified in 14 patients (9 %) and from ER negative to ER positive in 20 patients (12 %). The conversion rate for PR was 35 % (95 % CI 27.5–42.8): a switch from PR positive to PR negative in 34 patients (22 %) and from PR negative to PR positive in 20 patients (13 %). Overall, the conversion rate for HR was 15 % (95 % CI 10.2–22.0), equally distributed from positive to negative and the reverse (12 patients each). Hormone receptor discordance was observed in only one out of 15 patients (7 %) with triple-negative subtype.
In 36 (26 %) tumors, the immunohistochemical subtype between the primary tumor and the metastatic lesion had changed. The most frequent change observed was from a HR-positive to a HER2-amplified tumors (12 patients, 9 %), followed by the change in the opposite direction (8 patients, 6 %). Other frequent changes were from HR-positive to triple-negative tumors (7 patients, 5 %) and the reverse (6 patients, 4 %). Changes between triple-negative and HER2-amplified tumors in either direction were rarely observed (Table 3).
Table 3.
Change in immunohistochemical subtypes between primary tumor and metastasis at local and central laboratories
| Primary tumor | Metastatic lesion | |||||
|---|---|---|---|---|---|---|
| HR positive/HER2 negative n = 69 |
HER2 amplified n = 43 |
Triple negative n = 27 |
||||
| n | % | n | % | n | % | |
| At local laboratory, n = 139 | ||||||
| HR positive/HER2 negative, n = 74 | 55 | 74 | 12 | 16 | 7 | 10 |
| HER2 amplified, n = 38 | 8 | 21 | 29 | 76 | 1 | 3 |
| Triple negative, n = 27 | 6 | 22 | 2 | 7 | 19 | 71 |
| HR positive/HER2 negative n = 108 |
HER2 amplified n = 36 |
Triple negative n = 21 |
||||
|---|---|---|---|---|---|---|
| At central laboratory, n = 165 | ||||||
| HR positive/HER2 negative, n = 117 | 105 | 90 | 4 | 3 | 8 | 7 |
| HER2 amplified, n = 31 | 0 | 0 | 31 | 100 | 0 | 0 |
| Triple negative, 17 | 3 | 18 | 1 | 6 | 13 | 76 |
HER2 human epidermal growth factor receptor 2, HR hormonal receptor
Central laboratory
The status of HER2 was again the most stable, with a conversion rate of 3 % (95 % CI 1.1–7.2). All the changes (5 patients) were from negative to positive status. Most of the conversions (4 patients) were seen in the HR-positive subtype, with only one change in the triple-negative subtype (Table 2).
The conversion rate for ER was 13 % (95 % CI 8.6–19.4): A switch from ER positive to ER negative was identified in 17 patients (10 %) and from ER negative to ER positive in 5 patients (3 %). The conversion rate for PR was 28 % (95 % CI 21.9–35.9): a switch from PR positive to PR negative in 34 patients (20 %) and from PR negative to PR positive in 13 patients (8 %). Overall, the conversion rate for HR was 12 % (95 % CI 7.6–18), 14 of 20 patients (8 %) from positive to negative and 6 of 20 patients (4 %) the reverse.
In 16 (10 %) tumors, the immunohistochemical subtype changed between the primary tumor and the metastasis. The most frequent change observed was from HR positive to triple negative (8 patients, 5 %) and to HER2 amplified (4 patients, 2 %). Changes from triple negative to HR positive were also observed (3 patients, 2 %), whereas in only one patient was there a change from a triple-negative tumor to a HER2-amplified tumor (1 %) (Table 3).
Variability in the receptor expression between local and central laboratories
There was substantial agreement for HER2 status in both primary tumor and metastasis between local and central determinations. There was also a substantial concordance for ER expression at metastasis (kappa index = 0.794). By contrast, the highest variability was detected in the PR expression, in both primary tumor and metastasis (kappa index [k] = 0.555) (Table 4).
Table 4.
Variability in the receptor expression results between local and central laboratories in primary tumor and metastatic samples
| At local laboratory | At central laboratory | |||
|---|---|---|---|---|
| Primary tumor | Metastasis | |||
| ER positive | ER negative | ER positive | ER negative | |
| ER positive | 120 | 2 | 109 | 5 |
| ER negative | 25 | 29 | 8 | 37 |
| Kappa index | 0.591 | 0.794 | ||
| P value | <0.001 | <0.001 | ||
| PR positive | PR negative | PR positive | PR negative | |
|---|---|---|---|---|
| PR positive | 88 | 7 | 62 | 10 |
| PR negative | 30 | 51 | 25 | 59 |
| Kappa index | 0.568 | 0.555 | ||
| P value | <0.001 | <0.001 | ||
| HER2 positive | HER2 negative | HER2 positive | HER2 negative | |
|---|---|---|---|---|
| HER2 positive | 27 | 16 | 31 | 15 |
| HER2 negative | 4 | 112 | 5 | 100 |
| Kappa index | 0.651 | 0.667 | ||
| P value | <0.001 | <0.001 | ||
ER estrogen receptor, HER2 human epidermal growth factor receptor 2, PR progesterone receptor
Influence of previous treatment and biopsy site on conversion rate
There was no significant difference in conversion rate of HER2, ER and PR (centrally assessed) with respect to the previously received treatment. When compared to the changes in receptor status between locoregional recurrences and distant metastases, there was no significant difference for HER2, although we found a higher conversion rate for ER (26 vs. 10 %; p = 0.019) and a non-significant trend for PR (41 vs. 25 %; p = 0.088) in the locoregional recurrences.
Influence of the change in molecular subtype on treatment plans
The intended treatment plan was modified in 15 patients (8 % of the evaluable population) after the biopsy: in 11 of the 36 patients (31 %) whose tumor subtype changed in the metastatic lesion according to the local assessments and in 4 of the 103 patients (4 %) who did not change (p < 0.001).
Discussion
To the best of our knowledge, ConvertHER is the largest prospective study that evaluates the conversion rate of the receptor status (HER2, ER and PR) between the primary tumor and a recurrent lesion in a population of advanced breast cancer patients. Moreover, it is the only study that has compared the expression status determined at 31 local laboratories with those obtained at a single central laboratory. Our results showed that the expression of HER2 was the most stable, while the receptor that showed the highest conversion rate was PR, followed by ER. Conversion rates determined centrally were lower than those determined at local level (HER2: 3 vs. 16 %, ER: 13 vs. 21 %, PR: 28 vs. 35 %, respectively), suggesting that the discrepancies in receptor status can only be partially explained by laboratory artifacts.
Substantial agreement was found in the expression of HER2 between local and central laboratories, as well as in the expression of ER at the metastasis. The expression of PR at any site and that of ER at the primary site showed a lower agreement. Probably, the fact that ER at the primary site was determined at different time intervals in central and local laboratories may have influenced these results. Oncologists modified treatment plans in 31 % of patients whose tumor subtype had changed according to local laboratories.
Our results are in line with those reported previously by two prospective trials [10, 11]. The DESTINY study reported data from 121 patients in a single center who underwent biopsy, showing a conversion rate of 10, 16 and 40 % for HER2, ER and PR, respectively [10]. Out of 44 patients who showed a discordance in one or more receptors, 17 (39 %) modified antitumor treatment from that planned before biopsy. The Breast Recurrence in Tissues Study (BRITS) analyzed paired samples from 137 patients with advanced breast cancer in 20 hospitals and reported a conversion rate of 3 % for HER2, 10 % for ER and 25 % for PR [11]. Of 54 patients with discordances of any receptor, subsequent treatment was modified in 24 (46 %). A meta-analysis using individual patient data from these two studies showed conversion rates of 6, 13 and 31 % for HER2, ER and PR, respectively [12]. Interestingly, the results obtained centrally from our study were almost identical to those obtained by the BRITS, probably because in that study, samples from both the primary tumor and the recurrence were sent to a central specialist pathologist to be analyzed. In contrast, results obtained locally in our study are more similar to those obtained in the DESTINY study. The fact that samples from primary tumors were not systematically reanalyzed in the DESTINY study when relapses occurred may explain the higher conversion rates observed.
Overall, according to results obtained centrally, most changes in HR status tended to be loss of expression (50/68, 74 %) as opposed to gain of expression (18/68, 26 %). In contrast, all changes in HER2 status were to acquire the expression (5/5, 100 %). These results may reflect the clonal evolution to more aggressive phenotypes [3, 10, 11, 13]. A more profound examination of the molecular differences not only at the receptor level but also at the functional pathway level between the primary tumor and its corresponding metastases could contribute to elucidate whether these receptor discordances are the result of a gradual evolution of the cancer in the metastatic site.
The percentage of modifications in subsequent treatment observed in our study (8 %) seems slightly lower than those observed in the BRITS (17 %) and the DESTINY (14 %) studies. Moreover, it is surprising that after performing a confirmatory biopsy with its consequent risks, physicians still only tailor treatment accordingly in such a low percentage of patients. This probably reflects the fact that when clinicians observe a change in receptor status, they are still uncertain as to whether it is due to a biological change in the tumor or due to a methodological inconsistency. Consequently, clinicians feel more confident adding the corresponding antitumor treatment when a gain of receptor expression is detected, rather than removing an effective and not excessively toxic treatment like endocrine therapy or anti-HER2 monoclonal antibody even though the receptor expression is lost [14]. Additionally, almost half of the changes observed in our study were related to PR, which rarely influences the treatment plan.
We consider that our results strengthen the need to obtain biopsies from metastatic lesions at the time of relapse in breast cancer patients. This is not only due to the conversion rates observed in receptor expression but also due to the need to confirm disease recurrence. On this point, an interesting finding of our study was the observation that 8 (4 %) of 196 patients initially included had a clinical misdiagnosis of relapsed breast cancer. This percentage is lower than the 10 % previously reported, but still remarkable, and underscores the importance of the biopsy, particularly at first relapse [11, 15]. Lastly, our results showed that biopsy of metastatic lesions is technically feasible and that receptor expression can be determined from most biopsies as previously reported [10]. This is an important issue, since novel early-phase clinical trials require biomarker assessment of the most recent disease for patient selection.
We recognize that the design and implementation of our study may have certain methodological limitations. Although the same procedures for sample testing were followed at the central laboratory, the methodologies used within the 31 participating sites probably varied widely because they were not standardized and may have evolved over time. An important question is whether the conversion of the receptor status and management changes would ultimately lead to improvements in patient quality of life and survival. Although intuitively the actual information about the receptor status of the metastases and the according systemic treatment should improve outcomes, this belief has to be proven in clinical trials.
In conclusion, the results of the ConvertHER study reinforce the recommendation to perform confirmatory biopsies of metastasis when relapse of breast cancer patient is suspected. Reasons for supporting this recommendation include not only avoiding the misdiagnosis of breast cancer relapse, but also tailoring more accurately anticancer treatment according to tumor evolution.
Acknowledgments
This study was sponsored by the Spanish Breast Cancer Research Group (GEICAM). Statistical analysis was performed by Laura Casas of Dynamic Solutions (Madrid, Spain) and the medical writing services by Beatriz Gil-Alberdi of HealthCo (Madrid, Spain). This study was financially supported by an unrestricted grant from Roche.
Conflict of interest
The authors have stated that they do not have any conflict of interest that may inappropriately influence this work.
Ethical standards
The study protocol was approved by the Institutional Review Board and the Ethics Committee of Hospital Provincial de Castellón (Spain), according to the requirements of the Spanish regulations (GEICAM 2009-03; clinicaltrials.gov identifier: NCT01377363). Study procedures were carried out in accordance with the Declaration of Helsinki, as revised in 2008, and good clinical practice guidelines. Written informed consent was obtained from all patients before enrollment.
References
- 1.Edgerton SM, Moore D, 2nd, Merkel D, Thor AD. erbB-2 (HER-2) and breast cancer progression. Appl Immunohistochem Mol Morphol. 2003;11:214–221. doi: 10.1097/00129039-200309000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Liedtke C, Hatzis C, Symmans WF, Desmedt C, Haibe-Kains B, Valero V, Kuerer H, Hortobagyi GN, Piccart-Gebhart M, Sotiriou C, Pusztai L. Genomic grade index is associated with response to chemotherapy in patients with breast cancer. J Clin Oncol. 2009;27:3185–3191. doi: 10.1200/JCO.2008.18.5934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sari E, Guler G, Hayran M, Gullu I, Altundag K, Ozisik Y. Comparative study of the immunohistochemical detection of hormone receptor status and HER-2 expression in primary and paired recurrent/metastatic lesions of patients with breast cancer. Med Oncol. 2011;28:57–63. doi: 10.1007/s12032-010-9418-2. [DOI] [PubMed] [Google Scholar]
- 4.Tolles J, Bai Y, Baquero M, Harris LN, Rimm DL, Molinaro AM. Optimal tumor sampling for immunostaining of biomarkers in breast carcinoma. Breast Cancer Res. 2011;13:R51. doi: 10.1186/bcr2882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Arslan C, Sari E, Aksoy S, Altundag K. Variation in hormone receptor and HER-2 status between primary and metastatic breast cancer: review of the literature. Expert Opin Ther Targets. 2011;15:21–30. doi: 10.1517/14656566.2011.537260. [DOI] [PubMed] [Google Scholar]
- 6.Allred DC, Harvey JM, Berardo M, Clark GM. Prognostic and predictive factors in breast cancer by immunohistochemical analysis. Mod Pathol. 1998;11:155–168. [PubMed] [Google Scholar]
- 7.Hammond ME, Hayes DF, Dowsett M, Allred DC, Hagerty KL, Badve S, Fitzgibbons PL, Francis G, Goldstein NS, Hayes M, Hicks DG, Lester S, Love R, Mangu PB, McShane L, Miller K, Osborne CK, Paik S, Perlmutter J, Rhodes A, Sasano H, Schwartz JN, Sweep FC, Taube S, Torlakovic EE, Valenstein P, Viale G, Visscher D, Wheeler T, Williams RB, Wittliff JL, Wolff AC. American Society of Clinical Oncology/College of American Pathologists guideline recommendations for immunohistochemical testing of estrogen and progesterone receptors in breast cancer. J Clin Oncol. 2010;28:2784–2795. doi: 10.1200/JCO.2009.25.6529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wolff AC, Hammond ME, Schwartz JN, Hagerty KL, Allred DC, Cote RJ, Dowsett M, Fitzgibbons PL, Hanna WM, Langer A, McShane LM, Paik S, Pegram MD, Perez EA, Press MF, Rhodes A, Sturgeon C, Taube SE, Tubbs R, Vance GH, van de Vijver M, Wheeler TM, Hayes DF. American Society of Clinical Oncology/College of American Pathologists guideline recommendations for human epidermal growth factor receptor 2 testing in breast cancer. J Clin Oncol. 2007;25:118–145. doi: 10.1200/JCO.2006.09.2775. [DOI] [PubMed] [Google Scholar]
- 9.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–174. doi: 10.2307/2529310. [DOI] [PubMed] [Google Scholar]
- 10.Amir E, Miller N, Geddie W, Freedman O, Kassam F, Simmons C, Oldfield M, Dranitsaris G, Tomlinson G, Laupacis A, Tannock IF, Clemons M. Prospective study evaluating the impact of tissue confirmation of metastatic disease in patients with breast cancer. J Clin Oncol. 2012;30:587–592. doi: 10.1200/JCO.2010.33.5232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Thompson AM, Jordan LB, Quinlan P, Anderson E, Skene A, Dewar JA, Purdie CA. Prospective comparison of switches in biomarker status between primary and recurrent breast cancer: the Breast Recurrence In Tissues Study (BRITS) Breast Cancer Res. 2010;12:R92. doi: 10.1186/bcr2771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Amir E, Clemons M, Purdie CA, Miller N, Quinlan P, Geddie W, Coleman RE, Freedman OC, Jordan LB, Thompson AM. Tissue confirmation of disease recurrence in breast cancer patients: pooled analysis of multi-centre, multi-disciplinary prospective studies. Cancer Treat Rev. 2012;38:708–714. doi: 10.1016/j.ctrv.2011.11.006. [DOI] [PubMed] [Google Scholar]
- 13.Tapia C, Savic S, Wagner U, Schonegg R, Novotny H, Grilli B, Herzog M, Barascud AD, Zlobec I, Cathomas G, Terracciano L, Feichter G, Bubendorf L. HER2 gene status in primary breast cancers and matched distant metastases. Breast Cancer Res. 2007;9:R31. doi: 10.1186/bcr1676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Amir E, Clemons M. Should a biopsy be recommended to confirm metastatic disease in women with breast cancer? Lancet Oncol. 2009;10:933–935. doi: 10.1016/S1470-2045(09)70295-5. [DOI] [PubMed] [Google Scholar]
- 15.Simmons C, Miller N, Geddie W, Gianfelice D, Oldfield M, Dranitsaris G, Clemons MJ. Does confirmatory tumor biopsy alter the management of breast cancer patients with distant metastases? Ann Oncol. 2009;20:1499–1504. doi: 10.1093/annonc/mdp028. [DOI] [PMC free article] [PubMed] [Google Scholar]