Abstract
High-protein diets have been shown to prevent the development of diet-induced obesity and can improve associated metabolic disorders in mice. Dietary leucine supplementation can partially mimic this effect. However, the molecular mechanisms triggering these preventive effects remain to be satisfactorily explained. Here we review studies showing a connection between high protein or total amino nitrogen intake and obligatory water intake. High amino nitrogen intake may possibly lower lipid storage, and prevent insulin resistance. Suggestions are made for further systematical studies to explore the relationship between water consumption, satiety, and energy expenditure. Moreover, these examinations should better distinguish between leucine-specific and unspecific effects. Research in this field can provide important information to justify dietary recommendations and strategies in promoting long-term weight loss and may help to reduce health problems associated with the comorbidities of obesity.
Keywords: high-protein diet, leucine supplementation, energy intake, water intake, metabolic syndrome, diet-induced obesity
1. Introduction
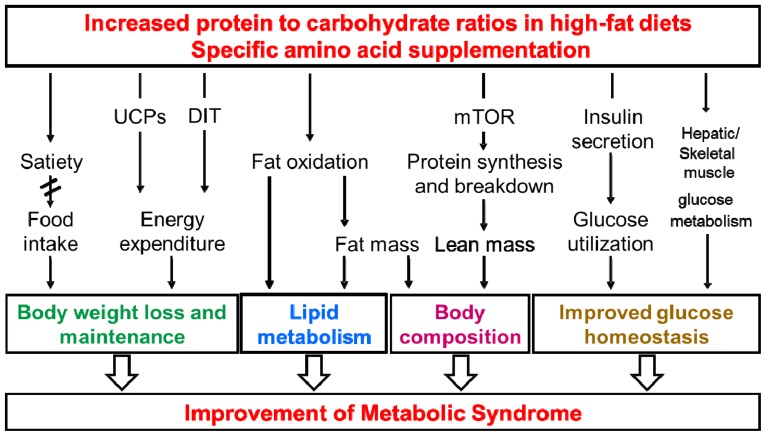
The epidemic dimension of obesity prevalence and related disorders represents an increasing problem in both developed and developing countries [1]. Therefore, it is a challenge to find effective treatments and preventive strategies to reduce the extent of overweight. One of the dietary approaches is the consumption of high-protein diets that can promote weight loss and weight maintenance in animals and humans. Further, high-protein diets could improve glucose homeostasis, increase energy expenditure (EE), may lower blood lipids, can reduce blood pressure, and could preserve lean body mass [2–7]. Similar effects have been demonstrated in mice when the protein to carbohydrate ratio in a high-fat diet was increased [8–11]. In addition, dietary supplementation of functionally different single amino acids including arginine, glutamine, glycine, and leucine may improve glucose and lipid metabolism [12–18]. However, the underlying mechanisms of these beneficial effects are not fully understood and are areas of controversy (summarized in Figure 1).
Figure 1.
Simplified scheme of possible mechanisms of beneficial effects of dietary protein on the metabolic syndrome. UCP, uncoupling protein; DIT, diet-induced thermogenesis; mTOR, mammalian target of rapamycin.
Our own studies [8,19,20] were aimed to investigate the effects of long-term high-whey protein diets containing either a normal or high-fat content on body weight (BW) regulation and EE to clarify the potential role of high-quality protein consumption in the prevention of metabolic syndrome associated traits in mice. It was suggested that the metabolic improvements related to high-protein intake could be mediated by specific amino acids such as the nutritionally indispensable branched-chain amino acid leucine. This suggestion results from several studies that have shown obvious advantageous effects of leucine supplementations on obesity development and/or glucose homeostasis using different rodent models of obesity and diabetes mellitus [18,21–24]. In principle, leucine may have specific functions related to its action on the mTOR pathway in hypothalamus and muscle which could affect food intake and energy homeostasis as well as skeletal muscle protein synthesis or breakdown [25–30]. However, so far it is not confirmed that a long-term leucine supplementation results in a sustained stimulation of protein synthesis and prevention of protein loss [31]. We investigated whether leucine might be responsible for the high-protein mediated effects during short-term and long-term interventions. To this end, we compared high protein (HP) whey diets (50% w/w, HP) with either adequate protein (AP) control (10% w/w, AP) or AP diets supplemented with leucine (AP + L) diets matching the leucine content of HP. Moreover, we investigated the effects of alanine supplementation using an additional control (AP + A). The AP + A diet was equimolar in alanine concentration compared with leucine of the AP + L diet [8,19]. This was done to distinguish leucine specific effects from unspecific amino acid effects. All other studies we are aware of did not include controls of alternative amino acid supplementations in comparison to the leucine supplementations.
2. Amino Acids and Insulin Signaling
It was recognized that mTOR can sense the availability of amino acids which regulate insulin sensitivity and may cause an inhibition of glucose uptake via phosphorylation of downstream factors of insulin signaling cascade by S6 kinase 1 (S6K1) [32,33]. However, the function of leucine in the modulation of glucose tolerance and insulin resistance remains an area of controversy. Whereas an improvement of glucose tolerance and insulin signaling was demonstrated, possibly due to dietary leucine in rodents [18,34,35], animal and human studies have shown that leucine impairs glucose tolerance [36] and can promote insulin resistance [32,33,37–40]. Additional studies showed no effects of leucine on glucose and insulin homeostasis [41–44]. These controversies may be generally due to dose effects, different experimental conditions such as differences in administration forms, and the animal models used [45]. In principle, modulations of glucose homeostasis by dietary leucine can involve different direct and indirect mechanisms such as stimulation of insulin and glucagon secretion, changes of hepatic glucose metabolism, impairment of insulin signaling, and glucose uptake in skeletal muscle [34,36,46]. Amino acids and insulin were suggested to synergistically activate S6K1 and to induce phosphorylation of insulin receptor substrate 1 (IRS-1). This activation may cause insulin resistance by direct inhibition of skeletal muscle glucose transport [32,47,48]. Interestingly, leucine was identified so far as the only amino acid directly interacting with the insulin pathway as a signaling molecule [49]. In contrast, long-term supplementation of leucine did not result in a sustained activation of the mTOR pathway. The insulin-stimulated glucose uptake into skeletal muscle was improved without changes in overall glucose tolerance in old rats [44]. Furthermore, it was suggested that glucose homeostasis can be maintained by an increased recycling of glucose via the glucose-alanine-cycle stimulated by dietary leucine [50,51]. Additionally, leucine and its metabolites were shown to directly activate Sirt1 (a NAD+-dependent deacetylase implicated in metabolic regulation) and Sirt1-dependent pathways of fat oxidation and insulin signaling in a cell-free system [52,53]. Sirt1 activation in liver, brown adipose tissue, and gastrocnemius muscle was shown after leucine supplementation to drinking water, which may contribute to the prevention of metabolic dysfunctions and insulin resistance in high-fat diet fed mice [54]. Taken together, these data demonstrate that the role of leucine in glucose homeostasis and insulin resistance is not completely understood. Moreover, it is not clear whether these effects are leucine-specific or not. Clarification of a causal relationship could contribute to an explanation of the observed diverse effects of high-protein diets on insulin resistance and diabetes risk in animal and human studies [40,55–57]. Therefore, further research is warranted to determine the mechanisms by which dietary interventions such as high-protein intake can improve metabolic health [3,58].
3. Body Weight and Body Composition
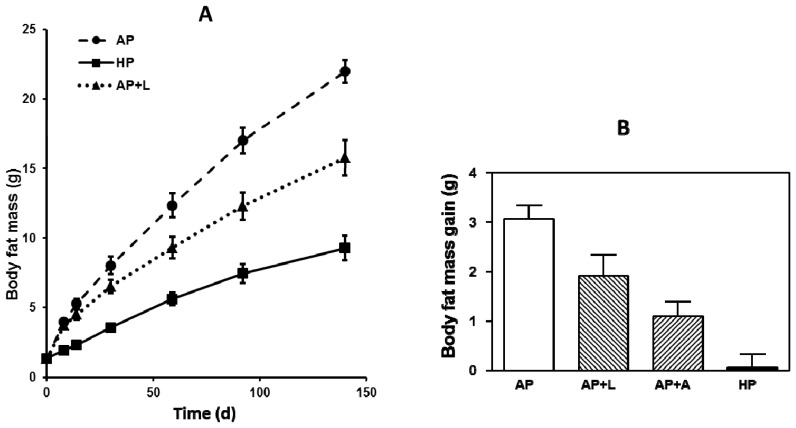
We have shown that a high-fat diet-induced body fat accumulation can be reduced by simultaneous high protein and leucine administration, both in the short and long term (Figure 2). Interestingly, equimolar supplementation with alanine decreased body fat mass gain in a short-term experiment similarly as leucine compared with AP-fed mice, although the metabolic functions of both amino acids are quite different [8,19].
Figure 2.
(A) Long term body fat accumulation. Ten weeks old male C57BL/6 mice were fed for 20 weeks ad libitum with experimental semisynthetic high-fat diets (20% w/w of fat) containing different protein and leucine concentrations. AP, adequate protein (10% w/w of whey protein); HP, high-protein (50% w/w of whey protein); AP + L, AP supplemented with l-leucine corresponding to HP (+6% l-leucine) [8]; (B) Short term body fat mass gain. Ten weeks old male C57BL/6 mice were fed for 7 days ad libitum with experimental semisynthetic high-fat diets (20% w/w of fat) containing different protein and leucine and alanine concentrations. AP, adequate protein (10% w/w of whey protein); HP, high-protein (50% w/w of whey protein); AP + L, AP supplemented with l-leucine corresponding to HP (+6% w/w l-leucine, 0.572 mole); AP + A, AP supplemented with equimolar l-alanine (+4.5% w/w l-alanine, 0.572 mole). Data are means ± SEM, n = 9–10 [19].
Chronic HP exposure also increased lean body mass whereas weights of m. quadriceps were higher in both HP and AP + L long-term experiments. This may be explained through a positive skeletal muscle protein balance. Indeed, we suspected increased rates of skeletal muscle protein synthesis because of higher incorporation of 15N-lysine after long term HP and AP + L exposures [8]. In contrast, other studies did not find an increase in skeletal muscle mass by long-term supplementation of leucine in humans and rats [31,44]. Branched-chain amino acids and particularly leucine are suggested to regulate muscle protein synthesis by activation of the mTOR pathway and thereby to stimulate protein synthesis on the translational level [27,30,59]. However, we did not find any evidence of activation of mTOR or its downstream targets (such as eIF4E-binding protein 1 (4E-BP1) and the ribosomal S6 protein (rS6-P) in skeletal muscle in our experiments ([8,19]). This is in contrast to other publications emphasizing the role of leucine as a potent activator of the mTOR pathway, which could be due to species differences or different experimental set-ups [27,30,60,61].
Consequently, we suggest that alternatively, other mechanism may contribute to the long-term regulation of skeletal muscle mass by dietary protein and leucine. In this context, a depression of protein degradation following leucine supplementation was reported [62–65]. Inhibitions of the ubiquitin-proteasome [66,67] or the autophagy-lysosome systems [68] by leucine were suggested to trigger suppressions of muscle protein breakdown. However, anti-proteolytic functions of leucine are less documented than effects on muscle protein synthesis, which deserves further investigation.
4. Energy and Water Intake
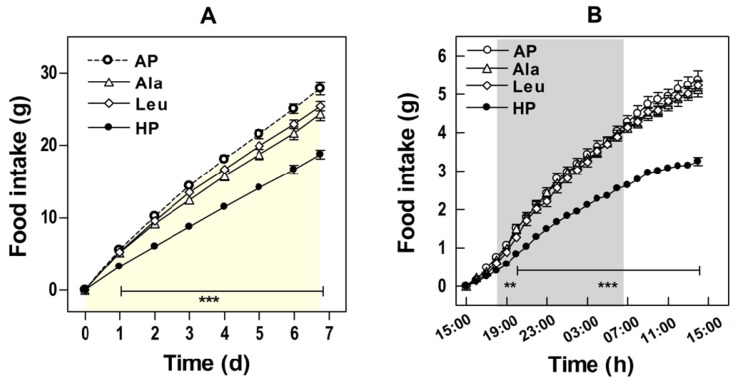
A higher satiating effect of dietary protein was assumed to be the main cause of high-protein diet induced weight loss [7,69]. This is in line with human investigations showing no changes in BW following isoenergetic intakes of high-protein and high-carbohydrate diets [70–73]. Hence, it was assumed that the reduced energy intake and not the macronutrient composition was likely to be crucial for loss of BW following hypo-caloric diets [71,72,74,75]. A higher satiety after high-protein diets might also result in improved weight maintenance because of better acceptance and compliance as compared with low-protein meals [76]. Our experiments with mice were performed under ad libitum conditions and have shown a significantly reduced food intake of HP and AP + L as compared with AP exposed controls with a strong correlation of energy intake with BW gain [8,19]. High-protein diets have also been shown to prevent the initial hyperphagia induced by high-fat feeding and thus can delay the development of obesity [9]. This was confirmed in a short-term study [19] showing that the intake of a high-fat diet was acutely affected by HP supplementation with significant effects apparent as early as five hours after the dietary switch (Figure 3).
Figure 3.
Food intake. Ten weeks old male C57BL/6 mice were fed for seven days ad libitum with experimental semisynthetic high-fat diets (20% w/w of fat) containing different protein and leucine and alanine concentrations. AP, adequate protein (10% w/w of whey protein); HP, high-protein (50% w/w of whey protein); Leu, AP supplemented with l-leucine corresponding to HP (+6% w/w l-leucine, 0.572 mole); Ala, AP supplemented with equimolar l-alanine (+4.5% w/w l-alanine, 0.572 mole). (A) Cumulative food intake during the whole feeding trial; (B) Food intake on the first day of dietary intervention. Values are means ± SEM. The shaded area refers to night (light off) period. Asterisks indicate significant differences from AP (** p < 0.01, *** p < 0.0001) [19].
Interestingly, the supplementation with leucine as well as with alanine led to a reduction in energy intake. However, the extent of this reduction was less compared with HP exposure. Increases in circulating leucine concentrations have been suggested to play a role in hypothalamic regulation of food intake by acting as satiety signal [25,26,28]. As expected, in our study plasma leucine was only increased in the HP and AP + L groups and not in AP + A group [19]. Therefore, changes in circulating leucine concentrations cannot explain the effect on satiety and fat accumulation alone. Furthermore, because alanine supplementation did not alter plasma amino acid levels, it seems unlikely that changes in concentrations of circulating amino acids contribute to the satiety effect we observed [19].
Summarizing, although we could show that food or energy intake is affected by dietary protein and amino acids it seems unlikely that the increase in satiety depends on hypothalamic regulation by leucine. This contrasts with conclusions associating leucine with neural mechanisms [29,77]. However, it is necessary to clearly distinguish the experimental conditions among different studies such as the energy consumed from fat. Furthermore, it became evident that energy intake is responsible to a high degree for changes in BW and body fat in mice exposed to adipogenic high-fat diets.
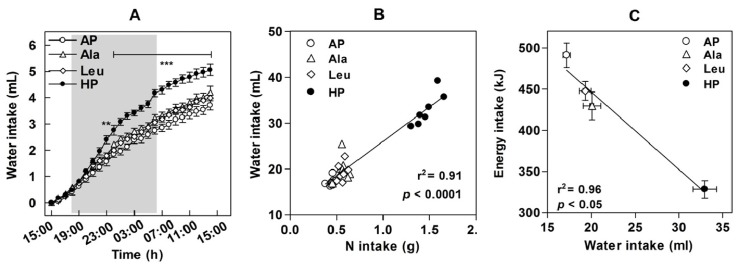
Additionally, we also measured water consumption of mice exposed to the experimental diets during a short-term study [19] (Figure 4) because we suspected a role of water consumption on satiety and BW (for review see: [78]). Human studies demonstrated that drinking of water can increase satiety, reduce energy intake, and induce weight loss [79–81]. We observed an almost doubled water intake of mice fed the HP diet as compared to the AP group [19]. Although the increase in water consumption of the leucine or alanine supplemented groups did not reach statistical significance, overall water intake strongly correlated with dietary amino nitrogen intake and negatively correlated with energy intake in all groups (Figure 4). Similar increases in water intake were observed in high-fat diet fed mice receiving whey protein supplemented in drinking water resulting in 78% greater levels of protein consumption compared to unsupplemented controls [10]. It is possible that this effect is related to urea production, which increases in parallel with the level of ingested protein or amino nitrogen to handle the excess of amino acids consumed [82,83].
Figure 4.
Water intake. Ten weeks old male C57BL/6 mice were fed for seven days ad libitum with experimental semisynthetic high-fat diets (20% w/w of fat) containing different protein and leucine and alanine concentrations. AP, adequate protein (10% w/w of whey protein); HP, high-protein (50% w/w of whey protein); Leu, AP supplemented with l-leucine corresponding to HP (+6% w/w l-leucine, 0.572 mole); Ala, AP supplemented with equimolar l-alanine (+4.5% w/w l-alanine, 0.572 mole). (A) Water intake on the first day of dietary intervention; (B) Correlations of water intake with nitrogen intake; (C) Correlations of water intake with energy intake. Values in (B) and (C) are means ± SEM (** p < 0.01, *** p < 0.0001) [19].
5. Energy Expenditure (EE)
Additional effects contributing to the leaner phenotype of high-protein diet exposed mice might be an increase in diet-induced thermogenesis (for review see: [7,69]). We could show that both HP diets and leucine supplementation can increase weight specific resting EE to the same extent [8]. This supported the suggested role of HP diets and of leucine in increasing EE [7,51]. EE is predominantly a function of fat free body mass [84–86]. Therefore, our observations are in line with higher m. quadriceps weights of mice following long-term HP or AP + L exposures [8].
Interestingly, differences in water consumption [19] might also have had an impact on EE. It was reported that metabolic rate can increase by about 30% in healthy normal-weight subjects following drinking of 500 mL of water [87]. EE was also enhanced following water intake in overweight and obese subjects [88]. In general, influences of water intake on osmolality, thermogenesis, and on metabolic organ functions have been discussed [88]. However, a connection between water intake induced by dietary protein or amino acids and changes in EE and other metabolic functions is so far only hypothetical and needs to be investigated more systematically.
Previously we also suggested that higher rates of EE might be caused by increased uncoupling protein (UCP) expression following high-protein and leucine intake [18,89]. This suggestion resulted from studies measuring mRNA expressions in rats after long- term or short-term exposures with high-protein diets [89,90]. However, we could not detect any significant changes in the protein expression of UCP homologues in mice in either short-term or long-term experiments which argues against a participation of UCPs in high-protein or leucine-mediated effects on EE [8]. Overall, the data show that diets high in protein or leucine concentration can affect EE. But the extent of its contribution to BW reduction and the mechanisms remains to be elucidated.
6. Lipid Metabolism and NAFLD
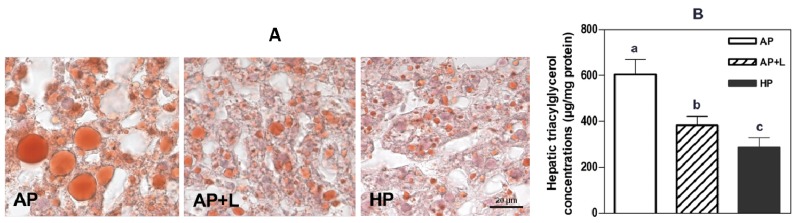
We could show that long-term HP exposure prevents high-fat diet induced fat accumulation in liver which was mimicked to a considerable extent by leucine supplementation (Figure 5, [8]). Significant lower liver triacylglycerol concentrations were also observed in mice after only one week of dietary exposure with the HP diet. In the short term, leucine or alanine supplementations did not (yet) show such significant effects on liver fat [19]. Although, the gain in fat mass was highly correlated with energy intake in these studies, only about 77% of body fat increase could be explained by energy intake. Fewer hepatic fat contents were also found in mice fed with high whey protein containing high-fat diets compared to controls without significant differences in overall energy consumption. [10] Lower feeding efficiency and modifications of energy expenditure and oxygen consumption after high-protein diet exposures can indicate mechanisms resulting in negative energy and fat balance [10,89,90].
Figure 5.
Oil red O staining of livers (A) and hepatic triacylglycerol concentrations (B). Ten weeks old male C57BL/6 mice were fed for 20 weeks ad libitum with experimental semisynthetic high-fat diets (20% w/w of fat) containing different protein and leucine concentrations. AP, adequate protein (10% w/w of whey protein); HP, high-protein (50% w/w of whey protein); AP + L, AP supplemented with l-leucine corresponding to HP (+6% l-leucine). Data are means ± SEM, n = 9–10, “a, b, c” indicates that “p < 0.05” [8].
In general, liver represents a key organ for maintenance of energy homeostasis. Therefore it is very likely that disturbances in hepatic metabolism are linked to events contributing to the metabolic syndrome [91,92]. Several processes leading to a fatty liver phenotype are discussed. These include higher rates of hepatic de novo lipogenesis, reduced lipid oxidation, increased uptake of fatty acids, and defective discharges of lipids. Our gene expression data using adipogenic diets clearly indicated that lower hepatic triacylglycerol concentrations in long-term HP fed mice [8] can be linked to reduced rates of hepatic de novo lipogenesis. In particular, lower mRNA levels of acetyl-CoA-carboxylase alpha (ACCα) were observed in HP diet exposed mice compared with AP controls. However, hepatic mRNA levels of ACCα in leucine supplemented AP + L fed mice were not different from AP controls. This suggests that the HP diet effects on liver lipid metabolism could be rather due to the lower dietary carbohydrate intake with the HP diet and that leucine did not exhibit specific effects [8]. Similarly, mRNA expression of ACCα was also decreased in livers of mice exposed to HP diet for one week while supplementations with alanine or leucine did not reduce ACCα expression significantly (Table 1).
Table 1.
Relative gene expression levels of liver and white adipose tissue proteins from ten weeks old male C57BL/6 mice fed different diets with an adequate (AP), a high (HP) or an adequate protein concentration supplemented with l-alanine (AP + A) or l-leucine (AP + L) for one week [19] 1,2.
| AP | AP + A | AP + L | HP | p < | |
|---|---|---|---|---|---|
| Liver | |||||
| ACCα | 1.00 ± 0.09 a | 0.78 ± 0.12 a | 0.67 ± 0.09 a | 0.35 ± 0.03 b | 0.01 |
| CD36 | 1.00 ± 0.08 | 0.73 ± 0.10 | 0.99 ± 0.10 | 1.04 ± 0.16 | NS |
| FAS | 1.00 ± 0.26 a | 0.55 ± 0.10 b | 0.37 ± 0.05 b | 0.18 ± 0.03 b | 0.05 |
| L-FABP | 1.00 ± 0.14 a | 0.77 ± 0.05 b | 0.59 ± 0.05 b,c | 0.48 ± 0.03 c | 0.05 |
| Epididymal white fat | |||||
| ATGL | 1.00 ± 0.07 a | 1.28 ± 0.15 a | 1.38 ± 0.13 a | 1.86 ± 0.25 b | 0.01 |
| HSL | 1.00 ± 0.05 | 1.10 ± 0.10 | 0.89 ± 0.15 | 1.21 ± 0.08 | NS |
Values are means ± S.E.M., n = 6–8. Within a row, values without a common superscript differ significantly; NS, not significant;
ACCα, acetyl CoA carboxylase; CD36, fatty acid translocase; FAS, fatty acid synthase; L-FABP, liver-type fatty acid binding protein; ATGL, adipose triacylglycerol lipase; HSL, hormone sensitive lipase.
Furthermore, it was shown that an increased fatty acid uptake due to higher expression levels of lipid transport proteins such as fatty acid translocase (CD36) and liver-type fatty acid binding protein (l-FABP) can be more important for deposition of fat in the liver than changes in de novo lipogenesis or fat oxidation [93]. Consequently, the reduced hepatic lipid accumulation in HP and AP + L exposed mice could result from decreased fatty acid uptake due to lower protein levels of CD36. This was observed after long-term feeding of HP as well as of AP + L [8]. In contrast, CD36 protein as well as its mRNA level was not modified in livers of mice fed HP, AP + A, or AP + L diets for only one week (Table 1). Hepatic triacylglycerol concentrations did not differ significantly between amino acid supplemented groups and AP fed controls after one week. However, we cannot exclude an influence of dietary amino acids on hepatic fatty acid uptake because l-FABP mRNA was significantly reduced in all intervention groups compared to AP (Table 1). Interestingly, HP feeding seems to stimulate basal lipolysis in white fat as indicated by increased gene expression of adipose triacylglycerol lipase (ATGL) after one and 20 weeks of high-fat feeding ([8]; Table 1).
However, this was not observed in the AP + L and AP + A groups (Table 1), which again might be due to the lower carbohydrate intake of the HP group. Therefore, high-protein exposure and leucine supplementation were able to prevent hepatosteatosis in mice possibly due to different mechanisms. The HP effects on liver lipogenesis and adipose tissue lipolysis could primarily be due to a lower carbohydrate intake while the effects on hepatic fatty acid uptake could also be influenced by single amino acid supplementations.
Alternative mechanisms in prevention of hepatosteatosis are not well-studied so far in particular in the context of the advantageous effects of high-protein diets. Therefore, more detailed studies of alterations in expression and regulation of key enzymes and of transcriptional co-factors controlling hepatic lipid and energy metabolism are required.
7. Specificity of Observed Leucine Effects
Obviously, some of the beneficial effects of high-protein diets in the prevention of disadvantageous effects of adipogenic diets can be mimicked by dietary leucine supplementation [8]. This supports the significance of leucine as a potential nutritional treatment against obesity, insulin resistance, and NAFLD. However, experimental studies did not include additional control groups comparing the effects of alternative amino acids with those of leucine. Therefore, we have compared an additional diet group as control by supplementing alanine in a short-term intervention in mice [19]. Surprisingly, the equimolar substitution of leucine by alanine resulted in comparable effects of both supplementations on BW and body fat mass, food intake, water consumption, and hepatic triacylglycerols [19]. This implies that some or even most changes in energy and substrate metabolism induced by high-protein diets are not specifically related to leucine but seem to be rather a result of increased amino nitrogen consumption. Further long-term experiments are needed to investigate the specificity of leucine effects on metabolic disorders induced by adipogenic diets. It is striking that none of the published studies investigating the effects of leucine supplementation on metabolic syndrome related traits included a control group supplemented with another amino acid or another source of amino nitrogen [18,24,44]. We suggest that this is essential in order to delineate which metabolic effects and mechanisms are amino acid-specific or a result of higher amino nitrogen consumption and its metabolic consequences.
8. Metabolic Consequences of Increased Water Intake in Response to High-Protein Diets
The observed association between increased water intake and lower energy intake led us to suspect that higher amino nitrogen intake resulting in raised urea production could cause the stimulation of obligatory water consumption [19]. It was shown in pigs that the excretion of higher amounts of urea resulted in the need for a higher volume of urine [94]. On the other hand there are some results indicating that higher water consumption may have advantageous metabolic consequences in obesity and diabetes in children and adults [95,96]. Firstly, epidemiological data suggest that water drinkers lower their energy intake. Further, pre-meal water consumption reduces energy intake and daily water intake may facilitate long-term weight loss in older adults [78,97]. It was also observed that a promotion of water drinking can effectively reduce weight gain among school children [98]. Sympathetic activation [99] and increases in metabolic rate [87] were detected following water intake in humans. Secondly, animal studies showed that higher protein concentrations in experimental diets significantly enhanced water intake in mice [100], rats [101–103], and pigs [94] accompanied by higher urine volumes. Interestingly, mice fed high-protein diets exhibited higher liver water contents [91]. Obviously, water drinking can produce intracellular hydration to prevent a hyperosmotic state and alterations in cell volume and hydration are known to regulate metabolism of proteins, glucose, and amino acids, and modify the expression of a wide variety of genes. The increase in amino acid concentrations following their uptake is recognized as one of the signals contributing to liver cell hydration [104,105]. Furthermore, it was shown in a rat study that the inhibition of angiotensin converting enzyme reduced body fat mass and plasma leptin while doubling the intake of water [106]. This suggests that either inhibition of the renin-angiotensin system unblocks fat metabolism or that increased water intake per se can regulate fat metabolism [107]. Moreover, cell dehydration was shown to inactivate mTOR signaling and to decrease insulin-induced glucose uptake [108]. Furthermore, a deficiency of TRPV4 (a transient receptor potential channel regulating cell volume by Ca2+ channeling which is activated by osmolarity) was shown to increase muscle oxidative capacity and resistance to diet-induced obesity in mice [109]. Nevertheless, a transient hypo-osmolarity was shown to increase whole-body lipid turnover in humans [110,111]. Thus, cell hydration should have opposite effects [107]. Consequently, more systematical investigations are needed to delineate the mechanisms of increases in water intake following high-protein diets and its consequences on metabolic syndrome related traits for a better explanation of the efficiency of high-protein diets.
9. Conclusions
We have shown that high-protein diets are able to prevent the development of diet-induced obesity and that they improve associated metabolic disorders in mice. These effects were mimicked by leucine supplementation although less pronounced [8]. Further, all metabolic effects of leucine supplementation seem to be a consequence of the concomitant increase in dietary amino nitrogen at least in the short-term [19]. However, the mechanisms remain to be satisfactorily explained. Long-term intervention studies comparing leucine supplementation with equimolar supplementation of other amino acids should be performed to distinguish between leucine-specific and unspecific effects. Furthermore, the physiological conditions in which leucine can activate mTOR and therefore affect muscle protein synthesis, glucose homeostasis, and food intake have to be elucidated. It seems reasonable to investigate skeletal muscle protein turnover with alternative methods to clarify the underlying mechanisms by which dietary protein and leucine affect body composition. Nevertheless, water intake was found to correlate with amino nitrogen consumption in different experimental groups. Therefore, water consumption was suggested to be related to satiety and EE [19] which should be studied more systematically. Studies in this field can increase our knowledge about the mechanisms of obesity prevention and metabolic syndrome related traits.
Acknowledgments
This work was supported by the Deutsche Forschungsgemeinschaft, Bonn, Germany (contract/grant number: PE 643/7-1). The funders had no role in the decision to publish or in preparation of the manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.World Health Organization. Obesity and overweight. [(accessed on 4 November 2013)]. http://www.who.int/mediacentre/factsheets/fs311/en/#.
- 2.Hodgson J.M., Burke V., Beilin L.J., Puddey I.B. Partial substitution of carbohydrate intake with protein intake from lean red meat lowers blood pressure in hypertensive persons. Am. J. Clin. Nutr. 2006;83:780–787. doi: 10.1093/ajcn/83.4.780. [DOI] [PubMed] [Google Scholar]
- 3.Johnstone A.M. Safety and efficacy of high-protein diets for weight loss. Proc. Nutr. Soc. 2012;71:339–349. doi: 10.1017/S0029665112000122. [DOI] [PubMed] [Google Scholar]
- 4.Krieger J.W., Sitren H.S., Daniels M.J., Langkamp-Henken B. Effects of variation in protein and carbohydrate intake on body mass and composition during energy restriction: A meta-regression 1. Am. J. Clin. Nutr. 2006;83:260–274. doi: 10.1093/ajcn/83.2.260. [DOI] [PubMed] [Google Scholar]
- 5.Layman D.K., Evans E.M., Erickson D., Seyler J., Weber J., Bagshaw D., Griel A., Psota T., Kris-Etherton P. A moderate-protein diet produces sustained weight loss and long-term changes in body composition and blood lipids in obese adults. J. Nutr. 2009;139:514–521. doi: 10.3945/jn.108.099440. [DOI] [PubMed] [Google Scholar]
- 6.Westerterp-Plantenga M.S. Protein intake and energy balance. Regul. Pept. 2008;149:67–69. doi: 10.1016/j.regpep.2007.08.026. [DOI] [PubMed] [Google Scholar]
- 7.Westerterp-Plantenga M.S., Nieuwenhuizen A., Tomé D., Soenen S., Westerterp K.R. Dietary protein, weight loss, and weight maintenance. Annu. Rev. Nutr. 2009;29:21–41. doi: 10.1146/annurev-nutr-080508-141056. [DOI] [PubMed] [Google Scholar]
- 8.Freudenberg A., Petzke K.J., Klaus S. Comparison of high-protein diets and leucine supplementation in the prevention of metabolic syndrome and related disorders in mice. J. Nutr. Biochem. 2012;23:1524–1530. doi: 10.1016/j.jnutbio.2011.10.005. [DOI] [PubMed] [Google Scholar]
- 9.Klaus S. Increasing the protein: Carbohydrate ratio in a high-fat diet delays the development of adiposity and improves glucose homeostasis in mice. J. Nutr. 2005;135:1854–1858. doi: 10.1093/jn/135.8.1854. [DOI] [PubMed] [Google Scholar]
- 10.Shertzer H.G., Woods S.E., Krishan M., Genter M.B., Pearson K.J. Dietary whey protein lowers the risk for metabolic disease in mice fed a high-fat diet. J. Nutr. 2011;141:582–587. doi: 10.3945/jn.110.133736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sorensen A., Mayntz D., Raubenheimer D., Simpson S.J. Protein-leverage in mice: The geometry of macronutrient balancing and consequences for fat deposition. Obesity (Silver Spring) 2008;16:566–571. doi: 10.1038/oby.2007.58. [DOI] [PubMed] [Google Scholar]
- 12.Alam M.A., Kauter K., Withers K., Sernia C., Brown L. Chronic l-arginine treatment improves metabolic, cardiovascular and liver complications in diet-induced obesity in rats. Food Funct. 2013;4:83–91. doi: 10.1039/c2fo30096f. [DOI] [PubMed] [Google Scholar]
- 13.Alvarado-Vasquez N., Zamudio P., Ceron E., Vanda B., Zenteno E., Carvajal-Sandoval G. Effect of glycine in streptozotocin-induced diabetic rats. Comp. Biochem. Physiol. C. 2003;134:521–527. doi: 10.1016/s1532-0456(03)00046-2. [DOI] [PubMed] [Google Scholar]
- 14.El Hafidi M., Perez I., Zamora J., Soto V., Carvajal-Sandoval G., Banos G. Glycine intake decreases plasma free fatty acids, adipose cell size, and blood pressure in sucrose-fed rats. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2004;287:R1387–R1393. doi: 10.1152/ajpregu.00159.2004. [DOI] [PubMed] [Google Scholar]
- 15.Fu W.J., Haynes T.E., Kohli R., Hu J., Shi W., Spencer T.E., Carroll R.J., Meininger C.J., Wu G. Dietary l-arginine supplementation reduces fat mass in Zucker diabetic fatty rats. J. Nutr. 2005;135:714–721. doi: 10.1093/jn/135.4.714. [DOI] [PubMed] [Google Scholar]
- 16.Jobgen W., Meininger C.J., Jobgen S.C., Li P., Lee M.J., Smith S.B., Spencer T.E., Fried S.K., Wu G. Dietary l-arginine supplementation reduces white fat gain and enhances skeletal muscle and brown fat masses in diet-induced obese rats. J. Nutr. 2009;139:230–237. doi: 10.3945/jn.108.096362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Opara E.C., Petro A., Tevrizian A., Feinglos M.N., Surwit R.S. l-glutamine supplementation of a high fat diet reduces body weight and attenuates hyperglycemia and hyperinsulinemia in C57BL/6J mice. J. Nutr. 1996;126:273–279. doi: 10.1093/jn/126.1.273. [DOI] [PubMed] [Google Scholar]
- 18.Zhang Y., Guo K., LeBlanc R.E., Loh D., Schwartz G.J., Yu Y.H. Increasing dietary leucine intake reduces diet-induced obesity and improves glucose and cholesterol metabolism in mice via multimechanisms. Diabetes. 2007;56:1647–1654. doi: 10.2337/db07-0123. [DOI] [PubMed] [Google Scholar]
- 19.Freudenberg A., Petzke K.J., Klaus S. Dietary l-leucine and l-alanine supplementation have similar acute effects in the prevention of high-fat diet-induced obesity. Amino Acids. 2013;44:519–528. doi: 10.1007/s00726-012-1363-2. [DOI] [PubMed] [Google Scholar]
- 20.Noatsch A., Petzke K.J., Millrose M.K., Klaus S. Body weight and energy homeostasis was not affected in C57BL/6 mice fed high whey protein or leucine-supplemented low-fat diets. Eur. J. Nutr. 2011;50:479–488. doi: 10.1007/s00394-010-0155-2. [DOI] [PubMed] [Google Scholar]
- 21.Arakawa M., Masaki T., Nishimura J., Seike M., Yoshimatsu H. The effects of branched-chain amino acid granules on the accumulation of tissue triglycerides and uncoupling proteins in diet-induced obese mice. Endocr. J. 2011;58:161–170. doi: 10.1507/endocrj.k10e-221. [DOI] [PubMed] [Google Scholar]
- 22.Eller L.K., Saha D.C., Shearer J., Reimer R.A. Dietary leucine improves whole-body insulin sensitivity independent of body fat in diet-induced obese Sprague-Dawley rats. J. Nutr. Biochem. 2013;24:1285–1294. doi: 10.1016/j.jnutbio.2012.10.004. [DOI] [PubMed] [Google Scholar]
- 23.Guo K., Yu Y.H., Hou J., Zhang Y. Chronic leucine supplementation improves glycemic control in etiologically distinct mouse models of obesity and diabetes mellitus. Nutr. Metab. (Lond.) 2010;7:57. doi: 10.1186/1743-7075-7-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Macotela Y., Emanuelli B., Bang A.M., Espinoza D.O., Boucher J., Beebe K., Gall W., Kahn C.R. Dietary leucine—An environmental modifier of insulin resistance acting on multiple levels of metabolism. PLoS One. 2011;6:e21187. doi: 10.1371/journal.pone.0021187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cota D. Mammalian target of rapamycin complex 1 (mTORC1) signaling in energy balance and obesity. Physiol. Behav. 2009;97:520–524. doi: 10.1016/j.physbeh.2009.03.006. [DOI] [PubMed] [Google Scholar]
- 26.Cota D., Proulx K., Smith K.A., Kozma S.C., Thomas G., Woods S.C., Seeley R.J. Hypothalamic mTOR signaling regulates food intake. Science. 2006;312:927–930. doi: 10.1126/science.1124147. [DOI] [PubMed] [Google Scholar]
- 27.Drummond M.J., Rasmussen B.B. Leucine-enriched nutrients and the regulation of mammalian target of rapamycin signalling and human skeletal muscle protein synthesis. Curr. Opin. Clin. Nutr. Metab. Care. 2008;11:222–226. doi: 10.1097/MCO.0b013e3282fa17fb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Potier M., Darcel N., Tome D. Protein, amino acids and the control of food intake. Curr. Opin. Clin. Nutr. Metab. Care. 2009;12:54–58. doi: 10.1097/MCO.0b013e32831b9e01. [DOI] [PubMed] [Google Scholar]
- 29.Ropelle E.R., Pauli J.R., Fernandes M.F., Rocco S.A., Marin R.M., Morari J., Souza K.K., Dias M.M., Gomes-Marcondes M.C., Gontijo J.A., et al. A central role for neuronal AMP-activated protein kinase (AMPK) and mammalian target of rapamycin (mTOR) in high-protein diet-induced weight loss. Diabetes. 2008;57:594–605. doi: 10.2337/db07-0573. [DOI] [PubMed] [Google Scholar]
- 30.Escobar J., Frank J.W., Suryawan A., Nguyen H.V., Van Horn C.G., Hutson S.M., Davis T.A. Leucine and alpha-ketoisocaproic acid, but not norleucine, stimulate skeletal muscle protein synthesis in neonatal pigs. J. Nutr. 2010;140:1418–1424. doi: 10.3945/jn.110.123042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Balage M., Dardevet D. Long-term effects of leucine supplementation on body composition. Curr. Opin. Clin. Nutr. Metab. Care. 2010;13:265–270. doi: 10.1097/MCO.0b013e328336f6b8. [DOI] [PubMed] [Google Scholar]
- 32.Tremblay F., Krebs M., Dombrowski L., Brehm A., Bernroider E., Roth E., Nowotny P., Waldhausl W., Marette A., Roden M. Overactivation of S6 kinase 1 as a cause of human insulin resistance during increased amino acid availability. Diabetes. 2005;54:2674–2684. doi: 10.2337/diabetes.54.9.2674. [DOI] [PubMed] [Google Scholar]
- 33.Um S.H., D'Alessio D., Thomas G. Nutrient overload, insulin resistance, and ribosomal protein S6 kinase 1, S6K1. Cell Metab. 2006;3:393–402. doi: 10.1016/j.cmet.2006.05.003. [DOI] [PubMed] [Google Scholar]
- 34.Bernard J.R., Liao Y.H., Ding Z., Hara D., Kleinert M., Nelson J.L., Ivy J.L. An amino acid mixture improves glucose tolerance and lowers insulin resistance in the obese Zucker rat. Amino Acids. 2013;45:191–203. doi: 10.1007/s00726-013-1488-y. [DOI] [PubMed] [Google Scholar]
- 35.Bernard J.R., Liao Y.H., Hara D., Ding Z., Chen C.Y., Nelson J.L., Ivy J.L. An amino acid mixture improves glucose tolerance and insulin signaling in Sprague-Dawley rats. Am. J. Physiol. Endocrinol. Metab. 2011;300:E752–E760. doi: 10.1152/ajpendo.00643.2010. [DOI] [PubMed] [Google Scholar]
- 36.Balage M., Dupont J., Mothe-Satney I., Tesseraud S., Mosoni L., Dardevet D. Leucine supplementation in rats induced a delay in muscle IR/PI3K signaling pathway associated with overall impaired glucose tolerance. J. Nutr. Biochem. 2011;22:219–226. doi: 10.1016/j.jnutbio.2010.02.001. [DOI] [PubMed] [Google Scholar]
- 37.Krebs M., Roden M. Nutrient-induced insulin resistance in human skeletal muscle. Curr. Med. Chem. 2004;11:901–908. doi: 10.2174/0929867043455620. [DOI] [PubMed] [Google Scholar]
- 38.Newgard C.B., An J., Bain J.R., Muehlbauer M.J., Stevens R.D., Lien L.F., Haqq A.M., Shah S.H., Arlotto M., Slentz C.A., et al. A branched-chain amino acid-related metabolic signature that differentiates obese and lean humans and contributes to insulin resistance. Cell Metab. 2009;9:311–326. doi: 10.1016/j.cmet.2009.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Promintzer M., Krebs M. Effects of dietary protein on glucose homeostasis. Curr. Opin. Clin. Nutr. Metab. Care. 2006;9:463–468. doi: 10.1097/01.mco.0000232909.84483.a9. [DOI] [PubMed] [Google Scholar]
- 40.Tremblay F., Lavigne C., Jacques H., Marette A. Role of dietary proteins and amino acids in the pathogenesis of insulin resistance. Annu. Rev. Nutr. 2007;27:293–310. doi: 10.1146/annurev.nutr.25.050304.092545. [DOI] [PubMed] [Google Scholar]
- 41.Lynch C.J., Hutson S.M., Patson B.J., Vaval A., Vary T.C. Tissue-specific effects of chronic dietary leucine and norleucine supplementation on protein synthesis in rats. Am. J. Physiol. Endocrinol. Metab. 2002;283:E824–E835. doi: 10.1152/ajpendo.00085.2002. [DOI] [PubMed] [Google Scholar]
- 42.Nairizi A., She P., Vary T.C., Lynch C.J. Leucine supplementation of drinking water does not alter susceptibility to diet-induced obesity in mice. J. Nutr. 2009;139:715–719. doi: 10.3945/jn.108.100081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Torres-Leal F.L., Fonseca-Alaniz M.H., Teodoro G.F., de Capitani M.D., Vianna D., Pantaleao L.C., Matos-Neto E.M., Rogero M.M., Donato J., Jr., Tirapegui J. Leucine supplementation improves adiponectin and total cholesterol concentrations despite the lack of changes in adiposity or glucose homeostasis in rats previously exposed to a high-fat diet. Nutr. Metab. (Lond.) 2011;8:62. doi: 10.1186/1743-7075-8-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zeanandin G., Balage M., Schneider S.M., Dupont J., Hebuterne X., Mothe-Satney I., Dardevet D. Differential effect of long-term leucine supplementation on skeletal muscle and adipose tissue in old rats: An insulin signaling pathway approach. Age (Dordr.) 2012;34:371–387. doi: 10.1007/s11357-011-9246-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zanchi N.E., Guimaraes-Ferreira L., de Siqueira-Filho M.A., Felitti V., Nicastro H., Bueno C., Lira F.S., Naimo M.A., Campos-Ferraz P., Nunes M.T., et al. Dose and latency effects of leucine supplementation in modulating glucose homeostasis: Opposite effects in healthy and glucocorticoid-induced insulin-resistance states. Nutrients. 2012;4:1851–1867. doi: 10.3390/nu4121851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kalogeropoulou D., Lafave L., Schweim K., Gannon M.C., Nuttall F.Q. Leucine, when ingested with glucose, synergistically stimulates insulin secretion and lowers blood glucose. Metabolism. 2008;57:1747–1752. doi: 10.1016/j.metabol.2008.09.001. [DOI] [PubMed] [Google Scholar]
- 47.Krebs M., Krssak M., Bernroider E., Anderwald C., Brehm A., Meyerspeer M., Nowotny P., Roth E., Waldhausl W., Roden M. Mechanism of amino acid-induced skeletal muscle insulin resistance in humans. Diabetes. 2002;51:599–605. doi: 10.2337/diabetes.51.3.599. [DOI] [PubMed] [Google Scholar]
- 48.Tremblay F., Marette A. Amino acid and insulin signaling via the mTOR/p70 S6 kinase pathway. A negative feedback mechanism leading to insulin resistance in skeletal muscle cells. J. Biol. Chem. 2001;276:38052–38060. doi: 10.1074/jbc.M106703200. [DOI] [PubMed] [Google Scholar]
- 49.Devkota S., Layman D.K. Protein metabolic roles in treatment of obesity. Curr. Opin. Clin. Nutr. Metab. Care. 2010;13:403–407. doi: 10.1097/MCO.0b013e32833a7737. [DOI] [PubMed] [Google Scholar]
- 50.Layman D.K., Boileau R.A., Erickson D.J., Painter J.E., Shiue H., Sather C., Christou D.D. A reduced ratio of dietary carbohydrate to protein improves body composition and blood lipid profiles during weight loss in adult women. J. Nutr. 2003;133:411–417. doi: 10.1093/jn/133.2.411. [DOI] [PubMed] [Google Scholar]
- 51.Layman D.K., Walker D.A. Potential importance of leucine in treatment of obesity and the metabolic syndrome. J. Nutr. 2006;136:319S–323S. doi: 10.1093/jn/136.1.319S. [DOI] [PubMed] [Google Scholar]
- 52.Bruckbauer A., Zemel M.B. Effects of dairy consumption on SIRT1 and mitochondrial biogenesis in adipocytes and muscle cells. Nutr. Metab. (Lond.) 2011;8:91. doi: 10.1186/1743-7075-8-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Bruckbauer A., Zemel M.B., Thorpe T., Akula M.R., Stuckey A.C., Osborne D., Martin E.B., Kennel S., Wall J.S. Synergistic effects of leucine and resveratrol on insulin sensitivity and fat metabolism in adipocytes and mice. Nutr. Metab. (Lond.) 2012;9:77. doi: 10.1186/1743-7075-9-77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Li H., Xu M., Lee J., He C., Xie Z. Leucine supplementation increases SIRT1 expression and prevents mitochondrial dysfunction and metabolic disorders in high-fat diet-induced obese mice. Am. J. Physiol. Endocrinol. Metab. 2012;303:E1234–E1244. doi: 10.1152/ajpendo.00198.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Metges C.C., Barth C.A. Metabolic consequences of a high dietary-protein intake in adulthood: Assessment of the available evidence. J. Nutr. 2000;130:886–889. doi: 10.1093/jn/130.4.886. [DOI] [PubMed] [Google Scholar]
- 56.Stepien M., Gaudichon C., Fromentin G., Even P., Tome D., Azzout-Marniche D. Increasing protein at the expense of carbohydrate in the diet down-regulates glucose utilization as glucose sparing effect in rats. PLoS One. 2011;6:e14664. doi: 10.1371/journal.pone.0014664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Weickert M.O., Roden M., Isken F., Hoffmann D., Nowotny P., Osterhoff M., Blaut M., Alpert C., Gogebakan O., Bumke-Vogt C., et al. Effects of supplemented isoenergetic diets differing in cereal fiber and protein content on insulin sensitivity in overweight humans. Am. J. Clin. Nutr. 2011;94:459–471. doi: 10.3945/ajcn.110.004374. [DOI] [PubMed] [Google Scholar]
- 58.Adams S.H. Emerging perspectives on essential amino acid metabolism in obesity and the insulin-resistant state. Adv. Nutr. 2011;2:445–456. doi: 10.3945/an.111.000737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Murgas Torrazza R., Suryawan A., Gazzaneo M.C., Orellana R.A., Frank J.W., Nguyen H.V., Fiorotto M.L., El-Kadi S., Davis T.A. Leucine supplementation of a low-protein meal increases skeletal muscle and visceral tissue protein synthesis in neonatal pigs by stimulating mTOR-dependent translation initiation. J. Nutr. 2010;140:2145–2152. doi: 10.3945/jn.110.128421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Lang C.H., Frost R.A., Bronson S.K., Lynch C.J., Vary T.C. Skeletal muscle protein balance in mTOR heterozygous mice in response to inflammation and leucine. Am. J. Physiol. Endocrinol. Metab. 2010;298:E1283–E1294. doi: 10.1152/ajpendo.00676.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Wilson F.A., Suryawan A., Gazzaneo M.C., Orellana R.A., Nguyen H.V., Davis T.A. Stimulation of muscle protein synthesis by prolonged parenteral infusion of leucine is dependent on amino acid availability in neonatal pigs. J. Nutr. 2010;140:264–270. doi: 10.3945/jn.109.113621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Buse M.G., Reid S.S. Leucine. A possible regulator of protein turnover in muscle. J. Clin. Invest. 1975;56:1250–1261. doi: 10.1172/JCI108201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Matthews D.E. Observations of branched-chain amino acid administration in humans. J. Nutr. 2005;135:1580S–1584S. doi: 10.1093/jn/135.6.1580S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.May M.E., Buse M.G. Effects of branched-chain amino acids on protein turnover. Diabetes Metab. Rev. 1989;5:227–245. doi: 10.1002/dmr.5610050303. [DOI] [PubMed] [Google Scholar]
- 65.Zanchi N.E., Nicastro H., Lancha A.H., Jr. Potential antiproteolytic effects of l-leucine: Observations of in vitro and in vivo studies. Nutr. Metab. (Lond.) 2008;5:20. doi: 10.1186/1743-7075-5-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Hamel F.G., Upward J.L., Siford G.L., Duckworth W.C. Inhibition of proteasome activity by selected amino acids. Metabolism. 2003;52:810–814. doi: 10.1016/s0026-0495(03)00094-5. [DOI] [PubMed] [Google Scholar]
- 67.Nakashima K., Ishida A., Yamazaki M., Abe H. Leucine suppresses myofibrillar proteolysis by down-regulating ubiquitin-proteasome pathway in chick skeletal muscles. Biochem. Biophys. Res. Commun. 2005;336:660–666. doi: 10.1016/j.bbrc.2005.08.138. [DOI] [PubMed] [Google Scholar]
- 68.Sugawara T., Ito Y., Nishizawa N., Nagasawa T. Regulation of muscle protein degradation, not synthesis, by dietary leucine in rats fed a protein-deficient diet. Amino Acids. 2009;37:609–616. doi: 10.1007/s00726-008-0180-0. [DOI] [PubMed] [Google Scholar]
- 69.Halton T.L., Hu F.B. The effects of high protein diets on thermogenesis, satiety and weight loss: A critical review. J. Am. Coll. Nutr. 2004;23:373–385. doi: 10.1080/07315724.2004.10719381. [DOI] [PubMed] [Google Scholar]
- 70.Gannon M.C., Nuttall F.Q., Saeed A., Jordan K., Hoover H. An increase in dietary protein improves the blood glucose response in persons with type 2 diabetes. Am. J. Clin. Nutr. 2003;78:734–741. doi: 10.1093/ajcn/78.4.734. [DOI] [PubMed] [Google Scholar]
- 71.Luscombe N.D., Clifton P.M., Noakes M., Parker B., Wittert G. Effects of energy-restricted diets containing increased protein on weight loss, resting energy expenditure, and the thermic effect of feeding in type 2 diabetes. Diabetes Care. 2002;25:652–665. doi: 10.2337/diacare.25.4.652. [DOI] [PubMed] [Google Scholar]
- 72.Sacks F.M., Bray G.A., Carey V.J., Smith S.R., Ryan D.H., Anton S.D., McManus K., Champagne C.M., Bishop L.M., Laranjo N., et al. Comparison of weight-loss diets with different compositions of fat, protein, and carbohydrates. N. Engl. J. Med. 2009;360:859–873. doi: 10.1056/NEJMoa0804748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Sargrad K.R., Homko C., Mozzoli M., Boden G. Effect of high protein vs high carbohydrate intake on insulin sensitivity, body weight, hemoglobin A1c, and blood pressure in patients with type 2 diabetes mellitus. J. Am. Diet. Assoc. 2005;105:573–580. doi: 10.1016/j.jada.2005.01.009. [DOI] [PubMed] [Google Scholar]
- 74.Golay A., Allaz A.F., Morel Y., de Tonnac N., Tankova S., Reaven G. Similar weight loss with low- or high-carbohydrate diets. Am. J. Clin. Nutr. 1996;63:174–178. doi: 10.1093/ajcn/63.2.174. [DOI] [PubMed] [Google Scholar]
- 75.Lean M.E., Han T.S., Prvan T., Richmond P.R., Avenell A. Weight loss with high and low carbohydrate 1200 kcal diets in free living women. Eur. J. Clin. Nutr. 1997;51:243–248. doi: 10.1038/sj.ejcn.1600391. [DOI] [PubMed] [Google Scholar]
- 76.Clifton P. High-protein and low-glycaemic diets improve dietary compliance and maintenance of weight loss in overweight adults who have lost weight on a low-calorie diet. Evid. Based Med. 2011;16:112–113. doi: 10.1136/ebm1197. [DOI] [PubMed] [Google Scholar]
- 77.Fromentin G., Darcel N., Chaumontet C., Marsset-Baglieri A., Nadkarni N., Tome D. Peripheral and central mechanisms involved in the control of food intake by dietary amino acids and proteins. Nutr. Res. Rev. 2012;25:29–39. doi: 10.1017/S0954422411000175. [DOI] [PubMed] [Google Scholar]
- 78.Dennis E.A., Flack K.D., Davy B.M. Beverage consumption and adult weight management: A review. Eat. Behav. 2009;10:237–246. doi: 10.1016/j.eatbeh.2009.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Davy B.M., Dennis E.A., Dengo A.L., Wilson K.L., Davy K.P. Water consumption reduces energy intake at a breakfast meal in obese older adults. J. Am. Diet. Assoc. 2008;108:1236–1239. doi: 10.1016/j.jada.2008.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Popkin B.M., Armstrong L.E., Bray G.M., Caballero B., Frei B., Willett W.C. A new proposed guidance system for beverage consumption in the United States. Am. J. Clin. Nutr. 2006;83:529–542. doi: 10.1093/ajcn.83.3.529. [DOI] [PubMed] [Google Scholar]
- 81.Stookey J.D., Constant F., Popkin B.M., Gardner C.D. Drinking water is associated with weight loss in overweight dieting women independent of diet and activity. Obesity (Silver Spring) 2008;16:2481–2488. doi: 10.1038/oby.2008.409. [DOI] [PubMed] [Google Scholar]
- 82.Forslund A.H., Hambraeus L., Olsson R.M., El-Khoury A.E., Yu Y.M., Young V.R. The 24-h whole body leucine and urea kinetics at normal and high protein intakes with exercise in healthy adults. Am. J. Physiol. 1998;275:E310–E320. doi: 10.1152/ajpendo.1998.275.2.E310. [DOI] [PubMed] [Google Scholar]
- 83.Young V.R., El-Khoury A.E., Raguso C.A., Forslund A.H., Hambraeus L. Rates of urea production and hydrolysis and leucine oxidation change linearly over widely varying protein intakes in healthy adults. J. Nutr. 2000;130:761–766. doi: 10.1093/jn/130.4.761. [DOI] [PubMed] [Google Scholar]
- 84.Speakman J.R., Selman C. Physical activity and resting metabolic rate. Proc. Nutr. Soc. 2003;62:621–634. doi: 10.1079/PNS2003282. [DOI] [PubMed] [Google Scholar]
- 85.Weyer C., Walford R.L., Harper I.T., Milner M., MacCallum T., Tataranni P.A., Ravussin E. Energy metabolism after 2 y of energy restriction: The biosphere 2 experiment. Am. J. Clin. Nutr. 2000;72:946–953. doi: 10.1093/ajcn/72.4.946. [DOI] [PubMed] [Google Scholar]
- 86.Zhang K., Sun M., Werner P., Kovera A.J., Albu J., Pi-Sunyer F.X., Boozer C.N. Sleeping metabolic rate in relation to body mass index and body composition. Int. J. Obes. Relat. Metab. Disord. 2002;26:376–383. doi: 10.1038/sj.ijo.0801922. [DOI] [PubMed] [Google Scholar]
- 87.Boschmann M., Steiniger J., Hille U., Tank J., Adams F., Sharma A.M., Klaus S., Luft F.C., Jordan J. Water-induced thermogenesis. J. Clin. Endocrinol. Metab. 2003;88:6015–6019. doi: 10.1210/jc.2003-030780. [DOI] [PubMed] [Google Scholar]
- 88.Boschmann M., Steiniger J., Franke G., Birkenfeld A.L., Luft F.C., Jordan J. Water drinking induces thermogenesis through osmosensitive mechanisms. J. Clin. Endocrinol. Metab. 2007;92:3334–3337. doi: 10.1210/jc.2006-1438. [DOI] [PubMed] [Google Scholar]
- 89.Petzke K.J., Friedrich M., Metges C.C., Klaus S. Long-term dietary high protein intake up-regulates tissue specific gene expression of uncoupling proteins 1 and 2 in rats. Eur. J. Nutr. 2005;44:414–421. doi: 10.1007/s00394-004-0545-4. [DOI] [PubMed] [Google Scholar]
- 90.Petzke K.J., Riese C., Klaus S. Short-term, increasing dietary protein and fat moderately affect energy expenditure, substrate oxidation and uncoupling protein gene expression in rats. J. Nutr. Biochem. 2007;18:400–407. doi: 10.1016/j.jnutbio.2006.07.005. [DOI] [PubMed] [Google Scholar]
- 91.Schwarz J., Tome D., Baars A., Hooiveld G.J., Muller M. Dietary protein affects gene expression and prevents lipid accumulation in the liver in mice. PLoS One. 2012;7:e47303. doi: 10.1371/journal.pone.0047303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Sommerfeld A., Krones-Herzig A., Herzig S. Transcriptional co-factors and hepatic energy metabolism. Mol. Cell. Endocrinol. 2011;332:21–31. doi: 10.1016/j.mce.2010.11.020. [DOI] [PubMed] [Google Scholar]
- 93.Zhu L., Baker S.S., Liu W., Tao M.H., Patel R., Nowak N.J., Baker R.D. Lipid in the livers of adolescents with nonalcoholic steatohepatitis: Combined effects of pathways on steatosis. Metabolism. 2011;60:1001–1011. doi: 10.1016/j.metabol.2010.10.003. [DOI] [PubMed] [Google Scholar]
- 94.Pfeiffer A., Henkel H., Verstegen M.W.A., Philipczyk I. The influence of protein intake on water balance, flow rate and apparent digestibilty of nutrients at the distal ileum in growing pigs. Livestock Prod. Sci. 1995;44:179–187. [Google Scholar]
- 95.Daniels M.C., Popkin B.M. Impact of water intake on energy intake and weight status: A systematic review. Nutr. Rev. 2010;68:505–521. doi: 10.1111/j.1753-4887.2010.00311.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Muckelbauer R., Sarganas G., Gruneis A., Muller-Nordhorn J. Association between water consumption and body weight outcomes: A systematic review. Am. J. Clin. Nutr. 2013;98:282–299. doi: 10.3945/ajcn.112.055061. [DOI] [PubMed] [Google Scholar]
- 97.Dennis E.A., Dengo A.L., Comber D.L., Flack K.D., Savla J., Davy K.P., Davy B.M. Water consumption increases weight loss during a hypocaloric diet intervention in middle-aged and older adults. Obesity (Silver Spring) 2010;18:300–307. doi: 10.1038/oby.2009.235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Muckelbauer R., Libuda L., Clausen K., Reinehr T., Kersting M. A simple dietary intervention in the school setting decreased incidence of overweight in children. Obes. Facts. 2009;2:282–285. doi: 10.1159/000229783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.May M., Gueler F., Barg-Hock H., Heiringhoff K.H., Engeli S., Heusser K., Diedrich A., Brandt A., Strassburg C.P., Tank J., et al. Liver afferents contribute to water drinking-induced sympathetic activation in human subjects: A clinical trial. PLoS One. 2011;6:e25898. doi: 10.1371/journal.pone.0025898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Frey I.M., Rubio-Aliaga I., Klempt M., Wolf E., Daniel H. Phenotype analysis of mice deficient in the peptide transporter PEPT2 in response to alterations in dietary protein intake. Pflugers Arch. 2006;452:300–306. doi: 10.1007/s00424-005-0042-5. [DOI] [PubMed] [Google Scholar]
- 101.Bouby N., Trinh-Trang-Tan M.M., Coutaud C., Bankir L. Vasopressin is involved in renal effects of high-protein diet: Study in homozygous Brattleboro rats. Am. J. Physiol. 1991;260:F96–F100. doi: 10.1152/ajprenal.1991.260.1.F96. [DOI] [PubMed] [Google Scholar]
- 102.Chan K.C., Lou P.P., Hargrove J.L. High casein-lactalbumin diet accelerates blood coagulation in rats. J. Nutr. 1993;123:1010–1016. doi: 10.1093/jn/123.6.1010. [DOI] [PubMed] [Google Scholar]
- 103.Jorda A., Zaragoza R., Portoles M., Baguena-Cervellera R., Renau-Piqueras J. Long-term high-protein diet induces biochemical and ultrastructural changes in rat liver mitochondria. Arch. Biochem. Biophys. 1988;265:241–248. doi: 10.1016/0003-9861(88)90124-5. [DOI] [PubMed] [Google Scholar]
- 104.Haussinger D., Reinehr R., Schliess F. The hepatocyte integrin system and cell volume sensing. Acta Physiol. (Oxf.) 2006;187:249–255. doi: 10.1111/j.1748-1716.2006.01542.x. [DOI] [PubMed] [Google Scholar]
- 105.Lang F. Effect of cell hydration on metabolism. Nestle Nutr. Inst. Workshop Ser. 2011;69:115–126. doi: 10.1159/000329290. discussion 126–130. [DOI] [PubMed] [Google Scholar]
- 106.Mathai M.L., Naik S., Sinclair A.J., Weisinger H.S., Weisinger R.S. Selective reduction in body fat mass and plasma leptin induced by angiotensin-converting enzyme inhibition in rats. Int. J. Obes. (Lond.) 2008;32:1576–1584. doi: 10.1038/ijo.2008.126. [DOI] [PubMed] [Google Scholar]
- 107.Thornton S.N., Even P.C., van Dijk G. Hydration increases cell metabolism. Int. J. Obes. (Lond.) 2009;33:385. doi: 10.1038/ijo.2008.264. author reply 386. [DOI] [PubMed] [Google Scholar]
- 108.Schliess F., Richter L., vom Dahl S., Haussinger D. Cell hydration and mTOR-dependent signalling. Acta Physiol. (Oxf.) 2006;187:223–229. doi: 10.1111/j.1748-1716.2006.01547.x. [DOI] [PubMed] [Google Scholar]
- 109.Kusudo T., Wang Z., Mizuno A., Suzuki M., Yamashita H. TRPV4 deficiency increases skeletal muscle metabolic capacity and resistance against diet-induced obesity. J. Appl. Physiol. 2012;112:1223–1232. doi: 10.1152/japplphysiol.01070.2011. [DOI] [PubMed] [Google Scholar]
- 110.Bilz S., Ninnis R., Keller U. Effects of hypoosmolality on whole-body lipolysis in man. Metabolism. 1999;48:472–476. doi: 10.1016/s0026-0495(99)90106-3. [DOI] [PubMed] [Google Scholar]
- 111.Keller U., Szinnai G., Bilz S., Berneis K. Effects of changes in hydration on protein, glucose and lipid metabolism in man: Impact on health. Eur. J. Clin. Nutr. 2003;57:S69–S74. doi: 10.1038/sj.ejcn.1601904. [DOI] [PubMed] [Google Scholar]