Abstract
Excessive food/energy intake is linked to obesity and metabolic disorders, such as diabetes. The hypothalamus in the brain plays a critical role in the control of food intake and peripheral metabolism. The signaling pathways in hypothalamic neurons that regulate food intake and peripheral metabolism need to be better understood for developing pharmacological interventions to manage eating behavior and obesity. Mammalian target of rapamycin (mTOR), a serine/threonine kinase, is a master regulator of cellular metabolism in different cell types. Pharmacological manipulations of mTOR complex 1 (mTORC1) activity in hypothalamic neurons alter food intake and body weight. Our previous study identified Rheb1 (Ras homolog enriched in brain 1) as an essential activator of mTORC1 activity in the brain. Here we examine whether central Rheb1 regulates food intake and peripheral metabolism through mTORC1 signaling. We find that genetic deletion of Rheb1 in the brain causes a reduction in mTORC1 activity and impairs normal food intake. As a result, Rheb1 knockout mice exhibit hypoglycemia and increased lipid mobilization in adipose tissue and ketogenesis in the liver. Our work highlights the importance of central Rheb1 signaling in euglycemia and energy homeostasis in animals.
Keywords: Rheb1, genetic deletion, food intake, hypoglycemia, ketogenesis
1. Introduction
Energy homeostasis is a fundamental mechanism used by multicellular organisms to maintain their survival and body growth [1]. It is tightly linked to food intake [2,3]. How the link between food intake and energy homeostasis is controlled remains incompletely understood. Recent studies show that central mammalian target of rapamycin (mTOR) signaling plays a critical role in the control of food intake and energy homeostasis [4–6]. mTOR, a serine/threonine kinase, is a master regulator of cellular metabolism, including protein and lipid synthesis, and energy production [7–9]. mTOR kinase functions in two distinct protein complexes—mTORC1 (mammalian target of rapamycin complex 1) and mTORC2 (mammalian target of rapamycin complex 2) [10,11]. mTORC1 activity is activated by growth factors (e.g., insulin) and nutrients (e.g., amino acids) [12], and negatively regulated by GTPase activity of the TSC (tuberous sclerosis complex) protein complex encoded by the TSC1 and TSC2 genes [13]. In 2006, a landmark paper showed that altered mTORC1 activity in hypothalamic neurons alters food intake and energy metabolism [4]. Intracerebroventricular injection of leucine in the vicinity of the arcuate (ARC) neurons in hypothalamus activates mTORC1 activity and reduces food intake. Conversely, injection of mTORC1 inhibitor rapamycin increases food intake and blunts leptin-mediated anorectic effect [4]. Subsequently, S6 kinase (S6K), a downstream substrate of mTORC1, is reported to regulate food intake and energy homeostasis [14]. The injection of adenovirus expressing dominant negative (DN) S6K in the mediobasal hypothalamus increases food intake, while expressing constitutively active (CA) S6K decreases food intake [14]. These studies establish the central control of food intake and energy homeostasis through hypothalamic neurons. However, a recent study shows that genetic deletion of TSC1 in hypothalamic POMC (proopiomelanocortin) neurons increases mTORC1 activity, and food intake by TSC1 knockout mice is increased and associated with increased body weight. Also, intracerebral rapamycin infusion was shown to reduce food intake and body weight in aged mice [15]. These results contradict earlier reports showing that increased mTORC1 activity in hypothalamic neurons reduces food intake. Although these studies have demonstrated a critical role of mTORC1 activity in the control of food intake and energy metabolism, most of them are based on pharmacological or viral mediated manipulations of mTORC1 activity in vivo. Therefore, the role of the mTOR signaling pathway in the control of food intake and energy metabolism needs further clarification in genetic models. Our previous study shows that Rheb1 (Ras homolog enriched in brain 1) is required for the activation of mTORC1 activity in the brain [16]. The genetic deletion of Rheb1 in neural stem/progenitor cells of the brain (Rheb1 f/f Nestin-cre, hereafter Rheb1 ko) renders the mTORC1 activity undetectable as shown by the absence of phosphorylation of S6, whereas mTORC2 activity is not impaired [16]. The Rheb1 ko mice show impaired postnatal growth and reduced body weight by 64.7% at 3-week-old, living for about 6 weeks [16]. The reason for the premature death is unknown. Now we show that the Rheb1 ko mouse reduces food intake and develops severe hypoglycemia and peripheral metabolic adaptations to meet the energy demands of the brain.
2. Results and Discussion
2.1. Genetic Deletion of Rheb1 in the Brain Disrupts Food Intake
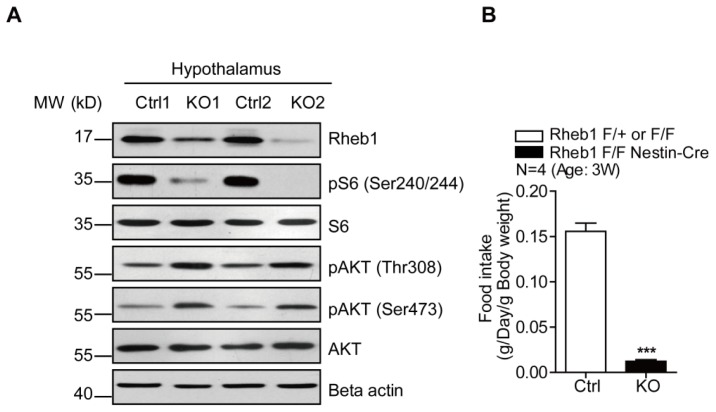
To examine the role of Rheb1/mTORC1 signaling in the regulation of food intake and energy homeostasis, we examined the mTORC1 activity in Rheb1 ko mice (Rheb1 f/f, Nestin-cre) in which Rheb1 was deleted by Cre activity expressed by Nestin promoter [17]. We focused on the hypothalamus, because it is critical in the central control of food intake. The results revealed that mTORC1 activity was dramatically reduced in the hypothalamus of Rheb1 ko, as indicated by pS6 (Ser240/244) (Figure 1A). This finding is consistent with the effect of Rheb1 ko on mTORC1 activity in other brain regions [16]. Given the importance of mTORC1 activity in hypothalamic neurons, particularly in POMC neurons, in the control of food intake, we examined the food intake of 3-week-old Rheb1 ko mice. The results showed that the food intake by Rheb1 ko mice was significantly reduced relative to the control mice (floxed Rheb1 mice without Cre) (N = 4) (Figure 1B). These data indicate that central Rheb1 signaling plays a role in the control of food intake.
Figure 1.
Genetic deletion of Rheb1 in the brain disrupts food intake. (A) Western blotting showing that Rheb1 and pS6 (Ser240/244) protein levels are reduced in Rheb1 ko hypothalamus; (B) Histograms showing the drastic reduction of food intake in Rheb1 ko mice compared to controls (N = 4). Results are averages of four independent animals. Data represent mean ± SEM. *** p < 0.001.
2.2. Genetic Deletion of Rheb1 in the Brain Leads to Hypoglycemia
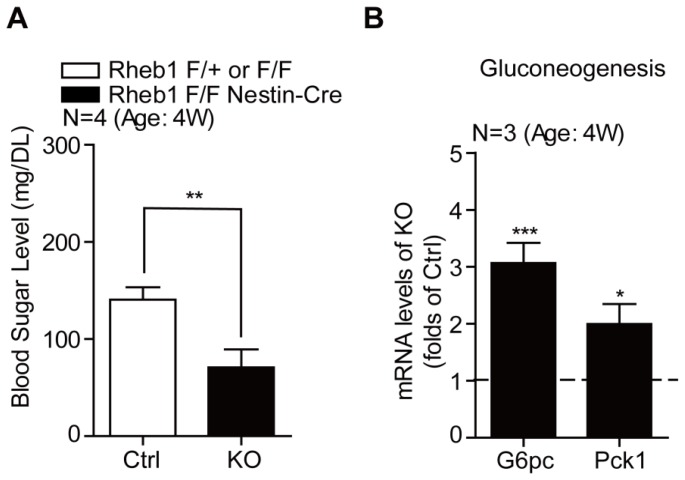
Food intake is critical to maintain blood glucose level and energy homeostasis. We wondered if blood glucose level was altered in Rheb1 ko mice. Blood glucose measurement shows that Rheb1 ko mice had a much lower glucose level (70 mg/DL) than that in their control littermates (150 mg/DL) (N = 4) (Figure 2A). To further examine the effect of Rheb1 ko on energy homeostasis, we examined the gluconeogenesis in the liver where Rheb1/mTORC1 activity in hepatocytes was slightly increased (see below). Real-time PCR analysis revealed that the mRNA levels of two canonical gluconeogenesis genes, G6pc and Pck1 [18], were increased in the liver of Rheb1 ko mice in comparison with those in control livers (Figure 2B). This result suggested that gluconeogenesis was activated in Rheb1 ko mice to synthesize glucose from non-carbohydrate precursors as part of homeostatic adaptation.
Figure 2.
Genetic deletion of Rheb1 in the brain leads to hypoglycemia. (A) Biochemical assays showing the robust reduction of blood glucose level in Rheb1 ko mice compared controls (N = 4). Results are averages of four independent animals. Data represent mean ± SEM. ** p < 0.01; (B) Real-time PCR assays showing the increasing mRNA levels of G6pc and Pck1 in livers of Rheb1 ko mice (N = 3). Results are averages of three independent animals. Data represent mean ± SEM. * p < 0.05, *** p < 0.001.
2.3. Genetic Deletion of Rheb1 in the Brain Induces Ketogenesis in the Liver
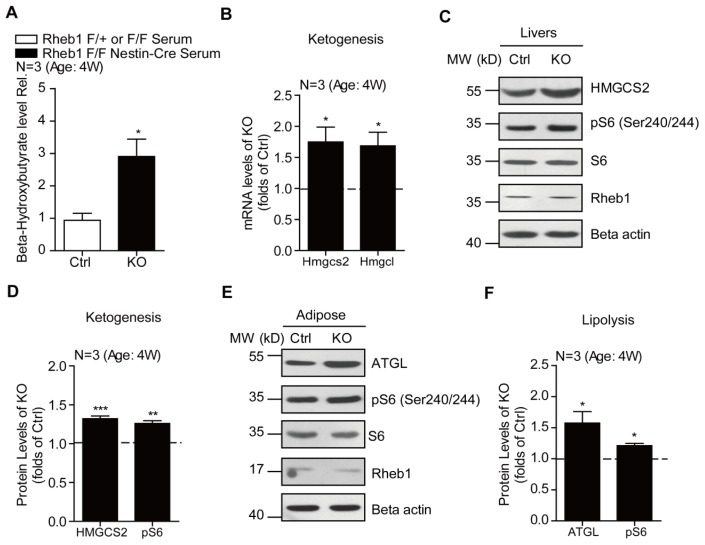
To further examine the adaptive metabolic changes as a result of altered Rheb1/mTORC1 activity in the brain, we assayed the ketogenesis in the liver of Rheb1 ko mice. Ketogenesis is an essential component of metabolic adaptations to meet the energy demand of the brain. We examined ketogenesis in the liver of Rheb1 ko mice and found that the ketogenesis was increased compared to the controls. This was demonstrated through increased levels of beta-hydroxybutyrate in serum of Rheb1 mice (N = 3) (Figure 3A) and increased mRNA levels of hydroxy-methyl-glutaryl coenzyme A synthase 2 (HMG-CoA synthase 2, Hmgcs2) and HMG-CoA lyase (Hmgcl) (N = 3)—enzymes that are critical for ketogenesis in the liver [19,20] (N = 3) (Figure 3B). Consistent with the mRNA increase of Hmgcs2, its protein level was also increased by 32.1% (Figure 3C,D). Increased ketogenesis is normally linked to increased lipid mobilization to provide free fatty acids for biosynthesis of ketone bodies in the liver. The majority of free fatty acids are generated as a consequence of the breakdown of triglycerides in adipose tissue and transferred to the liver through circulation for ketogenesis [21]. Therefore, we assayed the protein level of adipose triglyceride lipase (Atgl) as an indicator of lipolysis. Western blotting revealed a significant increase of ATGL protein level in the adipose tissue of Rheb1 ko mice as compared to the controls (N = 3), suggesting increased lipid mobilization in Rheb1 ko mice. Collectively, our data supports the notion that genetic deletion of Rheb1 in the brain would increase adaptive lipid mobilization and ketogenesis to meet the energy demand of the brain.
Figure 3.
Genetic deletion of Rheb1 in the brain induces ketogenesis in the liver. (A) Biochemical assays showing increased blood ketone levels in 4-week-old Rheb1 ko mice (N = 3). Results are averages of three independent animals. Data represent mean ± SEM. * p < 0.05; (B) Real-time PCR results showing the increasing levels of ketogenesis genes Hmgcs2 and Hmgcl in livers of Rheb1 ko mice (N = 3). Results are averages of three independent animals. Data represent mean ± SEM. * p < 0.05; (C,D) Western blots and histograms showing the increasing of HMGCS2 protein level in livers of Rheb1 ko mice (N = 3). Results are averages of three independent animals. Data represent mean ± SEM. ** p < 0.01, *** p < 0.001; (E,F) Western blots and histograms showing the increasing of ATGL protein level in adipose of Rheb1 ko mice (N = 3). Results are averages of three independent animals. Data represent mean ± SEM. * p < 0.05.
2.4. Genetic Deletion of Rheb1 in the Brain Increases Liver Lipid Droplets and Beta Oxidation
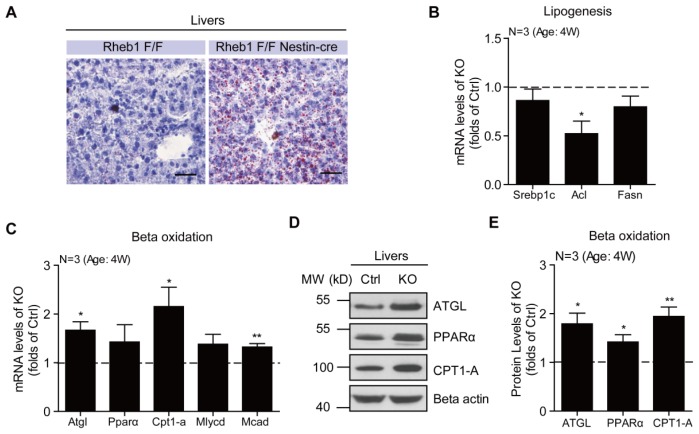
The excessive influx of free fatty acids to the liver as a result of increased lipid mobilization tends to increase the formation of lipid droplets in the liver [22]. In support of this notion, we found that the lipid accumulation in the form of lipid droplets was significantly increased in the liver of Rheb1 ko mice. By oil red O staining, we found a significant increase of lipid droplets in the liver of 4-week-old Rheb1 ko mice relative to controls (Figure 4A). Moreover, real-time PCR results showed that the mRNA levels of genes that were critical for lipogenesis, such as Srebp1c [23], Acl [24] and Fasn [23,24], were not increased in the liver of Rheb1 ko mice (N = 3) (Figure 4B), suggesting that this lipid accumulation was not due to increased de novo lipogenesis in the liver. The fatty acids derived from adipose tissue are utilized by beta-oxidation to generate acetyl-CoA for energy production [25,26]. To investigate whether the beta-oxidation was activated to oxidize the excessive fatty acids in the liver of Rheb1 ko mice, we assayed the mRNA and protein levels of genes that are critical for beta-oxidation. The results showed that the mRNA levels of Atgl [27], Pparα [28], Cpt1-a [29], Mlycd [30] and Mcad [31], were all increased in the liver of Rheb1 ko mice relative to controls (N = 3) (Figure 4C). Consistent with the increases in mRNA levels, protein levels for ATGL, PPARα and CPT1-A were also increased as shown by Western blotting (N = 3) (Figure 4D,E). All these results support the notion that adipose-derived lipids are transferred to the liver for beta-oxidation and subsequent ketogenesis to meet the energy demand of the brain in Rheb1 ko mice.
Figure 4.
Genetic deletion of Rheb1 in the brain increases liver lipid droplets and beta oxidation. (A) Representative oil red O staining images showing increased number of lipid droplets in livers of Rheb1 ko mice. Bar 25 μm; (B) Real-time PCR assays showing that hepatic lipogenesis genes Srebp1c, Acl and Fasn are not increased in livers of Rheb1 ko mice (N = 3). Results are averages of three independent animals. Data represent mean ± SEM. * p < 0.05; (C) Real-time PCR assays showing the increasing of mRNA levels of beta-oxidation genes, Atgl, Pparα, Cpt1-a, Mlycd and Mcad in livers of Rheb1 ko mice (N = 3). Results are averages of three independent animals. Data represent mean ± SEM. * p < 0.05, ** p < 0.01; (D,E) Western blots and histograms showing the increasing of protein levels of ATGL, PPARα and CPT1-A in livers of Rheb1 ko mice (N = 3). Results are averages of three independent animals. Data represent mean ± SEM. * p < 0.05, ** p < 0.01.
The present study uses genetic approaches to demonstrate a significant role of central Rheb1 in the control of food intake and energy homeostasis. Because mTORC1 activity in hypothalamic neurons is critical for food intake [4,15] and genetic deletion of Rheb1 inhibits mTORC1 activity in hypothalamus (Figure 1A), it is probable that the reduced food intake and hypoglycemia in Rheb1 ko mice is due to reduced mTORC1 activity in hypothalamic neurons. To meet the energy demand of the brain, Rheb1 ko mice develop adaptive changes in peripheral systems, such as lipid mobilization (Figure 3E), ketogenesis (Figure 3A) and gluconeogenesis (Figure 2B).
We noted that the increase in ketogenesis in the liver of Rheb1 ko mice is not due to loss of Rheb1 activity in hepatic cells, because we did not detect any significant change to Rheb1 protein level in livers of Rheb1 ko mice (Figure 3C). This non-cell autonomous effect of Rheb1 is consistent with the report that Nestin is expressed in only hepatic stellate cells that account for only 5% of the total number of cells in the mouse liver [32]. Moreover, we found that mTORC1 activity was slightly increased in hepatic and adipose tissues of Rheb1 ko mice (Figure 3C,E), suggesting that the increased ketogenesis and lipid mobilization in Rheb1 ko mice is a secondary effect of loss of central Rheb1 activity.
Animals develop multiple cellular mechanisms to control food intake to maintain energy homeostasis [1]. How food intake is regulated at the molecular level remains an unresolved question. Recent progress has focused on the importance of hypothalamic neurons in the control of food intake. As a central regulator of metabolisms, mTOR not only controls the lipid and protein biosynthesis, but also manipulates the feeding behaviors. Several studies have showed that mTOR signaling may serve as a negative regulator of food intake. For example, activation of hypothalamic mTORC1 signaling by central administration of leucine decreases food intake and body weight, and inhibition of mTORC1 signaling by rapamycin injection blunts leptin’s anorectic effect [4]. This effect seems to be mediated by S6K, because S6K, which is a major downstream factor of mTORC1, also negatively regulates food intake [14]. However, contradictive evidence points out that activation of mTORC1 by TSC ablation in hypothalamic POMC neurons increases food intake and body weight, while intracerebral rapamycin infusion restores it [15]. These controversial results raise the questions of how the mTOR pathway controls hypothalamic food intake center, anorexigenic or orexigenic. Of note, most of these studies are based on pharmacological or viral-mediated manipulations of mTORC1 activity in vivo. Therefore, studies of genetically modified mouse models are necessary to clarify the role of mTOR signaling in the control of food intake and energy homeostasis. Here, we examined the effect of Rheb1 deletion in the brain on food intake and subsequent alterations to peripheral metabolism. Our results demonstrate that as a result of Rheb1 deletion, mTORC1 activity in the hypothalamus is significantly reduced and the Rheb1 ko mice exhibit significantly reduced food intake and hypoglycemia. To meet the energy demand of the brain, lipid mobilization is activated to increase the biosynthesis of ketone bodies in the liver.
The central regulation of food intake is an immensely complex process involving the coordinated activities of multiple cerebral loci, such as the limbic system [33] and the cerebral cortex [34]. The neuronal processes from these loci project onto hypothalamic neurons and regulate appetite. Recent imaging studies indicate the awareness of hunger involves cortical functions [35]. Since the mTORC1 activity in the cortex is also affected in Rheb1 ko mice, presumably, the awareness of hunger is also altered by Rheb1 deletion. Although Rheb1 has been widely accepted as a key activator of mTORC1 signaling in vitro and in vivo, there may be additional mTORC1-independent effects of Rheb1. Because genetic deletion of Rheb1 in the brain increases AKT activity by the mTORC1-S6K1-IRS feedback pathway, future studies will address whether increased AKT activity contributes to the reduced food intake in Rheb1 ko mice. Again, genetic deletion of mTOR kinase or raptor may also help to further clarify whether the effect of Rheb1 on food intake is mediated by mTORC1 signaling.
3. Experimental Section
3.1. Reagents and Antibodies
The biochemical kit of beta-hydroxybutyrate was purchased from Biovision (Milpitas, CA, USA). The following antibodies, ATGL and pS6 (S240/244), were from Cell Signaling Technology (Danvers, MA, USA). Anti-β-actin was purchased from Millipore (Billerica, MA, USA). And CPT1-A antibody was from Abcam (Cambridge, UK). PPARα was from Thermo Scientific (Rockford, IL, USA), and HMGCS2 from LifeSpan BioScience (Seattle, WA, USA). Anti-Rheb1 antibody has been described previously [16].
3.2. Animals
Rheb1 ko mice were generated by breeding floxed Rheb1 mice with Nestin-cre deleter mice, and genotyped as previously described [16]. Both the Rheb1 ko and control littermates were housed in environmentally controlled conditions with a 12-hour light/dark cycle, and fed normal chow. All mouse work was done in accordance with the Animal Care and Use Committee guidelines of Sichuan University West-China Hospital.
3.3. Blood Glucose Measurement
Blood glucose levels were measured in a drop of blood obtained from tails of 4-week-old Rheb1 ko mice and control littermates at 10:00 a.m. in the fed state. The blood glucose analysis was performed using the Roche Accu-Chek Active System (Roche Diagnostics, Mannheim, Germany).
3.4. Western Blotting
Mouse adipose, liver and hypothalamus extracts were made with lysis buffer (2% SDS with protease and phosphatase inhibitors). Same amounts of proteins were loaded into SDS-PAGE gels and blotted with various antibodies, according to standard Western blotting procedures.
3.5. RNA Extraction and Real-Time PCR Assay
Total RNAs were extracted from tissues using Trizol reagent (Invitrogen, Carlsbad, CA, USA). RNA was subjected to reverse transcription with reverse transcriptase according to the manufacturer’s instructions (Fermentas, Glen Burnie, MD, USA). Quantitative real-time PCR was performed using the Bio-Rad iQ5 system (Bio-Rad, Hercules, CA, USA), and the relative gene expression was normalized to internal control as beta-actin. Primer sequences for SYBR Green probes of target genes were as follows:
G6pc: 5′-GTGTCCGTGATCGCAGACC-3′ and 5′-GACGAGGTTGAGCCAGTCTC-3′;
Pck1: 5′-T TGAGAAAGCGTTCAATGCCA-3′ and 5′-CACGTAGGGTGAATCCGTCAG-3′;
Hmgcs2: 5′-ATA CCACCAACGCCTGTTATGG-3′ and 5′-CAATGTCACCACAGACCACCAG-3′;
Hmgcl: 5′-ACTA CCCAGTCCTGACTCCAA-3′ and 5′-TAGAGCAGTTCGCGTTCTTCC-3′;
Srebp1c: 5′-GGAGCC ATGGATTGCACATT-3′ and 5′-GCTTCCAGAGAGGAGGCCAG-3′;
Acl: 5′-GAAGCTGACCTT GCTGAACC-3′ and 5′-CTGCCTCCAATGATGAGGAT-3′;
Fasn: 5′-TGGGTTCTAGCCAGCAGA GT-3′ and 5′-ACCACCAGAGACCGTTATGC-3′;
Atgl: 5′-TGTGGCCTCATTCCTCCTAC-3′ and 5′-TGCTGGATGTTGGTGGAGCT-3′;
Pparα: 5′-TGTTTGTGGCTGCTATAATTTGC-3′ and 5′-GCAACTTCTCAATGTAGCCTATGTTT-3′;
Cpt1-a: 5′-GGAGAGAATTTCATCCACTTCCA-3′ and 5′-CTTCCCAAAGCGGTGTGAGT-3′;
Mlycd: 5′-GCACGTCCGGGAAATG AAC-3′ and 5′-GCCTCACACTCGCTGATCTT-3′;
Mcad: 5′-TTTCGAAGACGTCAGAGTGC-3′ and 5′-TGCGACTGTAGGTCTGGTTC-3′;
Beta-actin: 5′-GAGACCTTCAACACCCCAGC-3′ and 5′-ATGTCACGCACGATTTCCC-3′.
3.6. β-Hydroxybutyrate Assay
Serum samples from Rheb1 ko or control mice (fed normally) were collected into a 96-well plate by retroorbital bleeding according to standard procedure. The procedure was performed at approximately same time on the days when the blood glucose assay was carried out. Beta-hydroxybutyrate levels were measured using a commercial diagnostic kit of Biovision (Catalog. #K632-100, Milpitas, CA, USA) according to the manufacturer’s instruction.
3.7. Oil Red O Staining
Standard Oil Red O staining was performed on frozen liver sections to evaluate tissue lipid content. After sacrifice, fresh livers were frozen immediately and subsequently cut into 10 μm sections by Cryostat Microtome. The staining solution was prepared by dissolving 0.5 g oil-red-O (Sigma, St. Louis, MO, USA) in 100 mL of isopropanol; 60 mL of this solution was mixed with 40 mL of distilled water. After 1 h at room temperature the staining solution was filtered and added to liver slices for 15 min. The staining solution was then removed and liver slices were washed twice with distilled water.
3.8. Food Intake Assay
For food intake experiments, three-week-old Rheb1 ko mice and control littermates were separated and each mouse was raised with chow (10 g/day) in a single cage. After 24 h, all the remainder food was collected and quantified. The experiments lasted for five days. Then the mass of intake food was normalized to mouse body weight for statistical analysis.
3.9. Statistical Analysis
All results of Western blotting, real-time PCR, and food intake across time were presented as mean ± SEM from a minimum of three or four independent experiments. Data from Western-blots were analyzed by ImageJ software (U.S. National Institutes of Health (NIH), Bethesda, MD, USA). P values were calculated using the Student’s t test for normally distributed data, and the value 0.05 (*), 0.01 (**) and 0.001 (***) was assumed as the level of significance for the statistic tests carried out.
4. Conclusions
In conclusion, our work highlights an important role of central Rheb1 in euglycemia and energy homeostasis in animals, which is mostly likely mediated by mTORC1 signaling. Our study sets the stage to examine how Rheb1/mTORC1 activity in hypothalamic neurons controls food intake and alters peripheral metabolism.
Acknowledgments
This study was supported by the grant from National 973 Basic Research Program of China (2009CB941400) and Sichuan Science and Technology Support Program of China (2012SZ0152).
Abbreviations
- mTOR
mammalian target of rapamycin
- mTORC1
mammalian target of rapamycin complex 1
- mTORC2
mammalian target of rapamycin complex 2
- Rheb1
Ras homolog enriched in brain 1
- ARC
arcuate
- POMC
proopiomelanocortin
- DN
dominant negative
- CA
constitutively active
- Rheb1 ko
Rheb1 f/f Nestin-cre
- HMG-CoA
hydroxy-methyl-glutaryl coenzyme A
- HMGCS2
HMG-CoA synthase 2
- HMGCL
HMG-CoA lyase
- ATGL
adipose triglyceride lipase
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Coupe B., Grit I., Hulin P., Randuineau G., Parnet P. Postnatal growth after intrauterine growth restriction alters central leptin signal and energy homeostasis. PLoS One. 2012;7:e30616. doi: 10.1371/journal.pone.0030616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hardie D.G., Ross F.A., Hawley S.A. AMPK: A nutrient and energy sensor that maintains energy homeostasis. Nat. Rev. Mol. Cell Biol. 2012;13:251–262. doi: 10.1038/nrm3311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pimentel G.D., Ropelle E.R., Rocha G.Z., Carvalheira J.B. The role of neuronal AMPK as a mediator of nutritional regulation of food intake and energy homeostasis. Metab. Clin. Exp. 2013;62:171–178. doi: 10.1016/j.metabol.2012.07.001. [DOI] [PubMed] [Google Scholar]
- 4.Cota D., Proulx K., Smith K.A., Kozma S.C., Thomas G., Woods S.C., Seeley R.J. Hypothalamic mTOR signaling regulates food intake. Science. 2006;312:927–930. doi: 10.1126/science.1124147. [DOI] [PubMed] [Google Scholar]
- 5.Wiczer B.M., Thomas G. The role of the mTOR pathway in regulating food intake. Curr. Opin. Drug Discov. Dev. 2010;13:604–612. [PubMed] [Google Scholar]
- 6.Woods S.C., Seeley R.J., Cota D. Regulation of food intake through hypothalamic signaling networks involving mTOR. Ann. Rev. Nutr. 2008;28:295–311. doi: 10.1146/annurev.nutr.28.061807.155505. [DOI] [PubMed] [Google Scholar]
- 7.Laplante M., Sabatini D.M. An emerging role of mTOR in lipid biosynthesis. Curr. Biol. 2009;19:R1046–R1052. doi: 10.1016/j.cub.2009.09.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yecies J.L., Manning B.D. Transcriptional control of cellular metabolism by mTOR signaling. Cancer Res. 2011;71:2815–2820. doi: 10.1158/0008-5472.CAN-10-4158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Braun S., Bitton-Worms K., LeRoith D. The link between the metabolic syndrome and cancer. Int. J. Biol. Sci. 2011;7:1003–1015. doi: 10.7150/ijbs.7.1003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jacinto E., Facchinetti V., Liu D., Soto N., Wei S., Jung S.Y., Huang Q., Qin J., Su B. SIN1/MIP1 maintains rictor-mTOR complex integrity and regulates Akt phosphorylation and substrate specificity. Cell. 2006;127:125–137. doi: 10.1016/j.cell.2006.08.033. [DOI] [PubMed] [Google Scholar]
- 11.Sarbassov D.D., Guertin D.A., Ali S.M., Sabatini D.M. Phosphorylation and regulation of Akt/PKB by the rictor-mTOR complex. Science. 2005;307:1098–1101. doi: 10.1126/science.1106148. [DOI] [PubMed] [Google Scholar]
- 12.Nobukuni T., Joaquin M., Roccio M., Dann S.G., Kim S.Y., Gulati P., Byfield M.P., Backer J.M., Natt F., Bos J.L., et al. Amino acids mediate mTOR/raptor signaling through activation of class 3 phosphatidylinositol 3OH-kinase. Proc. Natl. Acad. Sci. USA. 2005;102:14238–14243. doi: 10.1073/pnas.0506925102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Garami A., Zwartkruis F.J., Nobukuni T., Joaquin M., Roccio M., Stocker H., Kozma S.C., Hafen E., Bos J.L., Thomas G. Insulin activation of Rheb, a mediator of mTOR/S6K/4E-BP signaling, is inhibited by TSC1 and 2. Mol.Cell. 2003;11:1457–1466. doi: 10.1016/s1097-2765(03)00220-x. [DOI] [PubMed] [Google Scholar]
- 14.Blouet C., Ono H., Schwartz G.J. Mediobasal hypothalamic p70 S6 kinase 1 modulates the control of energy homeostasis. Cell Metab. 2008;8:459–467. doi: 10.1016/j.cmet.2008.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yang S.B., Tien A.C., Boddupalli G., Xu A.W., Jan Y.N., Jan L.Y. Rapamycin ameliorates age-dependent obesity associated with increased mTOR signaling in hypothalamic POMC neurons. Neuron. 2012;75:425–436. doi: 10.1016/j.neuron.2012.03.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zou J., Zhou L., Du X.X., Ji Y., Xu J., Tian J., Jiang W., Zou Y., Yu S., Gan L., et al. Rheb1 is required for mTORC1 and myelination in postnatal brain development. Dev. Cell. 2011;20:97–108. doi: 10.1016/j.devcel.2010.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tronche F., Kellendonk C., Kretz O., Gass P., Anlag K., Orban P.C., Bock R., Klein R., Schutz G. Disruption of the glucocorticoid receptor gene in the nervous system results in reduced anxiety. Nat. Genet. 1999;23:99–103. doi: 10.1038/12703. [DOI] [PubMed] [Google Scholar]
- 18.Ozcan L., Wong C.C., Li G., Xu T., Pajvani U., Park S.K., Wronska A., Chen B.X., Marks A.R., Fukamizu A., et al. Calcium signaling through CaMKII regulates hepatic glucose production in fasting and obesity. Cell Metab. 2012;15:739–751. doi: 10.1016/j.cmet.2012.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kostiuk M.A., Keller B.O., Berthiaume L.G. Palmitoylation of ketogenic enzyme HMGCS2 enhances its interaction with PPARalpha and transcription at the Hmgcs2 PPRE. FASEB J. 2010;24:1914–1924. doi: 10.1096/fj.09-149765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pie J., Lopez-Vinas E., Puisac B., Menao S., Pie A., Casale C., Ramos F.J., Hegardt F.G., Gomez-Puertas P., Casals N. Molecular genetics of HMG-CoA lyase deficiency. Mol. Genet. Metab. 2007;92:198–209. doi: 10.1016/j.ymgme.2007.06.020. [DOI] [PubMed] [Google Scholar]
- 21.Kolditz C.I., Langin D. Adipose tissue lipolysis. Curr. Opin. Clin. Nutr. Metab. Care. 2010;13:377–381. doi: 10.1097/MCO.0b013e32833bed6a. [DOI] [PubMed] [Google Scholar]
- 22.Foretz M., Ancellin N., Andreelli F., Saintillan Y., Grondin P., Kahn A., Thorens B., Vaulont S., Viollet B. Short-term overexpression of a constitutively active form of AMP-activated protein kinase in the liver leads to mild hypoglycemia and fatty liver. Diabetes. 2005;54:1331–1339. doi: 10.2337/diabetes.54.5.1331. [DOI] [PubMed] [Google Scholar]
- 23.Porstmann T., Santos C.R., Griffiths B., Cully M., Wu M., Leevers S., Griffiths J.R., Chung Y.L., Schulze A. SREBP activity is regulated by mTORC1 and contributes to Akt-dependent cell growth. Cell Metab. 2008;8:224–236. doi: 10.1016/j.cmet.2008.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bobrovnikova-Marjon E., Hatzivassiliou G., Grigoriadou C., Romero M., Cavener D.R., Thompson C.B., Diehl J.A. PERK-dependent regulation of lipogenesis during mouse mammary gland development and adipocyte differentiation. Proc. Natl. Acad. Sci. USA. 2008;105:16314–16319. doi: 10.1073/pnas.0808517105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lopes-Cardozo M., van den Bergh S.G. Ketogenesis in isolated rat liver mitochondria. III. Relationship with the rate of beta-oxidation. Biochim. Biophys. Acta. 1974;357:53–62. doi: 10.1016/0005-2728(74)90111-x. [DOI] [PubMed] [Google Scholar]
- 26.Serviddio G., Giudetti A.M., Bellanti F., Priore P., Rollo T., Tamborra R., Siculella L., Vendemiale G., Altomare E., Gnoni G.V. Oxidation of hepatic carnitine palmitoyl transferase-I (CPT-I) impairs fatty acid beta-oxidation in rats fed a methionine-choline deficient diet. PLoS One. 2011;6:e24084. doi: 10.1371/journal.pone.0024084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chakrabarti P., Kandror K.V. Adipose triglyceride lipase: A new target in the regulation of lipolysis by insulin. Curr. Diabetes Rev. 2011;7:270–277. doi: 10.2174/157339911796397866. [DOI] [PubMed] [Google Scholar]
- 28.El Kebbaj Z., Andreoletti P., Mountassif D., Kabine M., Schohn H., Dauca M., Latruffe N., El Kebbaj M.S., Cherkaoui-Malki M. Differential regulation of peroxisome proliferator-activated receptor (PPAR)-alpha1 and truncated PPARalpha2 as an adaptive response to fasting in the control of hepatic peroxisomal fatty acid beta-oxidation in the hibernating mammal. Endocrinology. 2009;150:1192–1201. doi: 10.1210/en.2008-1394. [DOI] [PubMed] [Google Scholar]
- 29.Gaidhu M.P., Fediuc S., Ceddia R.B. 5-Aminoimidazole-4-carboxamide-1-β-d-ribofuranosideinduced AMP-activated protein kinase phosphorylation inhibits basal and insulin-stimulated glucose uptake, lipid synthesis, and fatty acid oxidation in isolated rat adipocytes. J. Biol. Chem. 2006;281:25956–25964. doi: 10.1074/jbc.M602992200. [DOI] [PubMed] [Google Scholar]
- 30.Derdak Z., Villegas K.A., Harb R., Wu A.M., Sousa A., Wands J.R. Inhibition of p53 attenuates steatosis and liver injury in a mouse model of non-alcoholic fatty liver disease. J. Hepatol. 2012;58:785–791. doi: 10.1016/j.jhep.2012.11.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hanley P.J., Gopalan K.V., Lareau R.A., Srivastava D.K., von Meltzer M., Daut J. β-Oxidation of 5-hydroxydecanoate, a putative blocker of mitochondrial ATP-sensitive potassium channels. J. Physiol. 2003;547:387–393. doi: 10.1113/jphysiol.2002.037044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Niki T., Pekny M., Hellemans K., Bleser P.D., Berg K.V., Vaeyens F., Quartier E., Schuit F., Geerts A. Class VI intermediate filament protein nestin is induced during activation of rat hepatic stellate cells. Hepatology. 1999;29:520–527. doi: 10.1002/hep.510290232. [DOI] [PubMed] [Google Scholar]
- 33.Fukamauchi F., Aihara O., Kusakabe M. Reduced mRNA expression of neuropeptide Y in the limbic system of tenascin gene disrupted mouse brain. Neuropeptides. 1998;32:265–268. doi: 10.1016/s0143-4179(98)90046-4. [DOI] [PubMed] [Google Scholar]
- 34.Tacconi M.T., Lligona L., Salmona M., Pitsikas N., Algeri S. Aging and food restriction: Effect on lipids of cerebral cortex. Neurobiol. Aging. 1991;12:55–59. doi: 10.1016/0197-4580(91)90039-m. [DOI] [PubMed] [Google Scholar]
- 35.Lassman D.J., McKie S., Gregory L.J., Lal S., D’Amato M., Steele I., Varro A., Dockray G.J., Williams S.C., Thompson D.G. Defining the role of cholecystokinin in the lipid-induced human brain activation matrix. Gastroenterology. 2010;138:1514–1524. doi: 10.1053/j.gastro.2009.12.060. [DOI] [PubMed] [Google Scholar]