Abstract
Background
The causes of ethnic and caste-based disparities in mental health are poorly understood.
Aim
To identify mediators underlying caste-based disparities in mental health in Nepal.
Subjects and methods
A mixed methods ethnographic and epidemiological study of 307 adults (Dalit/Nepali, n=75; high caste Brahman and Chhetri, n=232) assessed with Nepali versions of Beck Depression (BDI) and Anxiety (BAI) Inventories.
Results
One third (33.7%) of participants were classified as depressed: Dalit/Nepali 50.0%, high caste 28.4%. One quarter (27.7%) of participants were classified as anxious: Dalit/Nepali 50.7%, high caste 20.3%. Ethnographic research identified four potential mediators: stressful life events, owning few livestock, no household income, and lack of social support. The direct effect of caste was 1.08 (95% CI -1.10—3.27) on depression score and 4.76 (95% CI 2.33—7.19) on anxiety score. All four variables had significant indirect (mediation) effects on anxiety, and all but social support had significant indirect effects on depression.
Conclusion
Caste-based disparities in mental health in rural Nepal are statistically mediated by poverty, lack of social support, and stressful life events. Interventions should target these areas to alleviate the excess mental health burden born by Dalit/Nepali women and men.
Keywords: Mental health, ethnicity, multiple mediator models, mixed methods, Nepal
Introduction
One of the major challenges in population health is to understand the mechanisms by which population disparities in mental health arise. There is a tremendous array of mechanisms proposed to explain population differences in mental health. Poverty and livelihood insecurity show tremendous variation across groups, especially between high and low income countries (Das et al. 2007), and this has been associated with disparities in common mental disorders (Hadley and Patil 2006; Hadley and Patil 2008). Moreover, relative poverty in terms of lacking idealized material goods has been associated with depression (Dressler et al. 1998), which may be related to community- or individual-level poverty (Krieger et al. 2005). In addition to these structural inequities, social inequities such as discrimination and social marginalization are another source of poor mental health (Ahmed et al. 2007; Williams et al. 2003). Social support and lack thereof also have been associated with mental health outcomes (Balaji et al. 2007).
Cultural differences may also play a role in population differences in mental health. Culture comprises a “shared system of learned norms, beliefs, values and behaviors that differ across populations defined by region, nationality, ethnicity, or religion,” (Hruschka and Hadley 2008). With cultural groups including such a diversity of social categorizations, it is no surprise that studies of cultural differences in mental health have produced varied results. Prevalence rates of depression in the United States do not consistently differ between African Americans and Americans of European descent (Williams and Williams-Morris 2000). Religion plays a role in prevalence, severity, recidivism, and presentation of mental illness (Koenig 2001). In addition, studies of torture survivors and refugees have shown lower prevalence of psychopathology among Buddhist practitioners compared with members of other religions (Holtz 1998; Mollica et al. 2002; Shrestha et al. 1998). With regard to nationality, the World Health Organization's recent global effort of cross-national research studies have revealed disparate rates between and within world regions (Kessler et al. 2008). And, prevalence rates across nations in these studies do not consistently coincide with poverty, education, physical health morbidity, or other human development indices, despite each of these factors being risks for poor mental health (c.f. Das et al. 2007). Lastly, all of these and the above factors are related to exposure to stressful and traumatic life events, another contributor to group disparities in mental health (Kendler et al. 2004; Williams and Jackson 2005).
All of the above are potential mediators of population disparities in mental health. Mediation refers to “the process by which some variables exert influences on others through intervening or mediator variables,” (Preacher and Hayes 2008). Mediation is central to the issue of cultural disparities in mental health because cultural categories (e.g. African American race, Hispanic ethnicity, Hindu religion, South African nationality, or first generation immigrant status) may be associated with differences in mental health in some context, but these categories in and of themselves are not the causal factors. Rather it is through some mediator such as lack of access to economic opportunities, greater exposure to violence, poorer physical health, or lack of social support that a certain group is at greater risk of mental health problems (c.f. Koenig 2001 for mediators of religion's influence on mental health). However, as one can intuit from the range of possible mediators, it is unlikely that any single factor determines the causal relationship between a ethnic group and mental health outcomes. Instead, it is more realistic to propose that multiple factors mediate population differences.
Multiple mediator models allow for specific testing of pathways through numerous mediators rather than older methods that simply examine reduction in effect estimates with the inclusion of culture-related variables, for example (Lannin et al. 1998). Analytic techniques to explore multiple mediators have advanced rapidly with most standard statistical software packages now able to run such analyses employing user-friendly macros (Preacher and Hayes 2008). However, to date, there has been a dearth of studies exploring population differences in global mental health using tests of multiple mediators.
The unique contribution of this study was to explore the cultural category of “caste” which despite being a central marker of identity in South Asia has received little attention in the global mental health literature. In addition, this study employs tests of multiple mediators to assess simultaneously a range of possible mechanisms underlying caste-based disparities in mental health. Based on a long-running research program in Nepal, the study is unique in its capacity to bring together ethnographic and epidemiologic modes of analyses. This study relies upon ethnographic work to identify potential mediators of caste-based disparities in mental health. The study provides a foundation for future studies of caste and mental health in South Asia, and, more generally, it lays out ethnographically-grounded steps epidemiology approaches to assess multiple pathways by which certain cultural groups may be at greater risk of psychiatric morbidity.
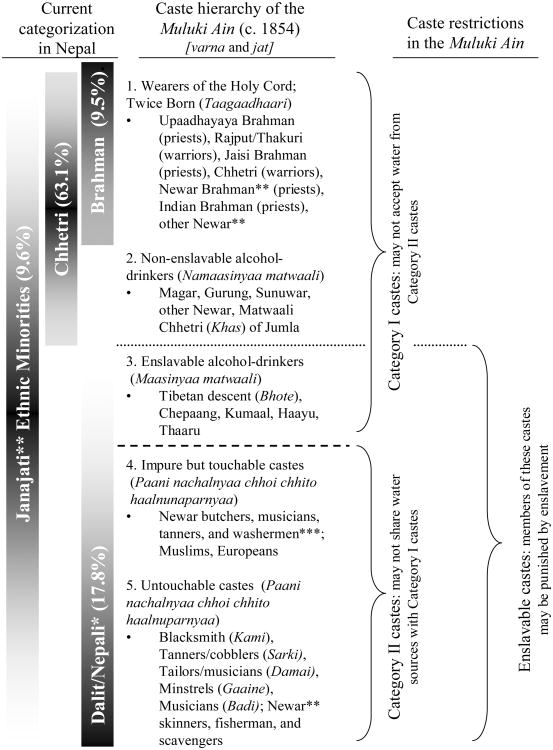
This study took place in Jumla, a mountainous district in northwestern Nepal. The caste system in Nepal is rooted in the India varna system which divides society into social rankings based on ancestral lineages (Höfer 2004). Figure 1 depicts the caste structure in Nepal. The top of the caste system includes two main ‘high caste’ groups Brahman (historically priests) and Chhetri (historically warriors and rulers). At the bottom of the caste system are ‘untouchable’ or Dalit castes. In Nepal, high caste Brahman and Chhetri dominate politics, education, and business while Dalit historically are marginalized from positions of power. In the district of Jumla, where this study took place, the population of 69,226 persons includes 9.5% Brahman, 63.1% Chhetri, and 17.8% Dalit (HMG-CBS 2003).
Figure 1.
Caste hierarchy in Nepal according to current categorization and codified at the time of the Muluki Ain (1854). Notes: Percentages in parentheses refer to Jumla district population percentage per 2001 census. *Persons from Dalit/Nepali castes in Jumla preferred to be identified as ‘Nepali’. **Newar as a whole are considered a Janajati (ethnic minority) group; however, there is a caste system within Newar subclassifying them at different levels of the Hindu hierarchy. ***Newar in the fourth level of the caste hierarchy are treated comparably to Dalit/Nepali in level five, however, they also are considered Janajati. (Figure adapted from Höfer 2004:9-10)
Ethnography
Ethnographic methods
We chose ethnographic methods to determine how caste was locally defined and the perceived relationship of caste with mental health. Additionally, we identified factors that differed among castes and were perceived to be associated with psychological distress. The factors that met these criteria were then evaluated in the multiple mediation models.
Ethnography comprised participant observation in Jumla which included attendance at rituals and festivals, traditional healing ceremonies, political meetings, and summer migration to highland pastures, combined with unstructured community observation conducted over a yearlong period in 2000. At that time a subset of participants (n=65) were selected to complete semi-structured interviews assessing mental and physical health, life stressors, and the influence of caste on wellbeing. Medical histories and physical evaluations were conducted to indentify the influence of physical factors on mental health presentation (Kohrt et al. 2005). Additional participant observation was conducted in 2007 including work at the district hospital, health camps, and community outreach. Two of the authors, natives of Jumla, reviewed the ethnographic results and hypotheses to be tested in the epidemiological analysis.
Ethnographic results
Identification of caste differences
One of the ethnographic goals was to determine the local salience and categorization of caste. When asked about caste classification in Jumla, most respondents described four groups: Brahman, Chhetri, Janajati (ethnic minority groups many of whom are not Hindu), and Dalit. There was consensus among groups in identifying and labeling members of Brahman and Chhetri castes, e.g. individuals who self-identified as Brahman were also labeled by members of other castes as Brahman. However, Brahman and Chhetri residents referred to Dalit as Dom (a local label for low caste laborers), Dalit, or by their specific jat (descent group) such as Kami or Saarki. Dalit did not use the word Dalit to self-identify but rather labeled themselves by their specific jat. Many also used the term Nepali which denotes low caste. The term Nepali included the same groups as those identified as Dalit by others. Therefore, we use the term Dalit/Nepali to describe this group as it incorporates both the preferred self-labeling of the group and the label commonly used by activists and dominant castes. Janajati were excluded as group because of their small sample in this study.
Gender as confounder/independent risk factor
We found that three major themes for the vulnerability of women to mental health problems. (1) The first issue was abuse of alcohol by male relatives. Both high caste and Dalit/Nepali groups reported male relatives' abuse of alcohol. Many Dalit/Nepali women reported that their husband's alcohol dependence led to domestic violence, marital rape, and losing the little income families earned from labor. Although alcohol consumption is prohibited in the Brahman caste, upper caste women also suffered domestic violence related to alcoholic husbands and sons. (2) The second theme was related to child-bearing with the competing pressures of having to produce a great number of children and then struggle with co-wives over resources for these offspring. Both Dalit/Nepali and upper caste women described reproductive health stresses associated with mental health problems. Women described being forced to bear many children to increase their labor resources. Women emphasized the stress of polygamy. Wealthy men married multiple wives, and these wives competed for resources. (3) The third theme was related to the stress of emphases on child marriage and restrictions on widows, both of which were interpreted in relation to Hindu purity. Girls were married at early ages to assure their virginal status. These women described being married as early as nine years old and suffering marital rape before puberty. This resulted in elderly men having wives ranging in age from ten to fifty years old. Upper caste widows could not remarry. The combination of early age of marriage for girls and large disparities in age between husbands and wives led to upper caste girls being widowed as early as ten years old and then being treated as childless burdens on surviving family members. These themes, taken together, suggested that female gender was associated with increased stress. We hypothesized that gender would have an independent risk factor for poor mental health as both Dalit/Nepali women and high caste women reported greater distress than men in their caste groups.
Age as confounder/independent risk factor
Age also appeared to be an independent risk factor as elderly members of both Dalit/Nepali and high castes described greater life distress compared with younger groups. Self-worth was strongly connected with productivity and once older men and women could not work in the fields or do other labor, younger family members regarded them as “useless mouths to feed.” Elderly adults in Jumla, which some considered being older than 40 years old, reported feeling that they were worthless burdens on their children and they were just waiting to die. Moreover, elderly respondents described the suffering from physical health problems accumulated over a lifetime of physical labor and lack of medical care.
Livelihood insecurity as mediator
Poverty and livelihood insecurity appeared to differ among castes and relate with psychological distress. Dalit/Nepali reported lower economic status and more insecurity compared with high caste participants. The vocations of Dalit/Nepali place them in a position of livelihood insecurity. The Dalit/Nepali vocations of blacksmith, tailor, cobbler, washer, and musician require exchange of services with other castes for food. They are more insecure than upper castes with land and livestock. “We have no property so we have to work for Brahman. Then Brahman eat our labor,” a Dalit/Nepali explained. Markers of poverty most commonly described were availability of cash household income and number of livestock. More high caste participants described having a member of the household who was an officeholder and received cash salary. Household cash income was necessary to access healthcare, education, and purchase basic necessities in case of food shortage and crop failure. Cash income also allowed for social status displays such as hosting festivals, extravagant weddings, and other public presentations of wealth. Livestock were identified as an important social marker and source of livelihood stability from historical times through the present. Livestock provided dairy products, meat, and labor such as ploughing. Because of these factors, we selected monthly household cash and number of livestock as potential mediators of the relationship of caste with mental health.
Social support as mediator
Social support was another factor related to mental health. People described the importance of social networks for access to labor during harvest seasons, care for children, obtaining financial loans, providing care or transport when a family member was ill, and loaning or repairing household and farming goods. Social support networks were also extremely important in traveling to bazaars and urban centers and bringing back needed items. Because individuals traveled rarely outside of Jumla, it was very useful to have social supports who journeyed to urban centers to procure household goods and medicines. High caste persons described having a wide diversity of social supports in terms of aphno manchhe—people who were considered to be reliable and ready to assist whenever called upon. They described how the providing of social support to other high caste individuals increased one's social status. In contrast, providing social assistance to Dalit/Nepali persons was not seen as beneficial because it was a one-way path; Dalit/Nepali persons did not have the resources to return the favor at a later date. Dalit/Nepali also said that there was a lack of support among Dalit/Nepali castes because of stratification within the Dalit/Nepali groups. Based on these findings, we selected material social support as a potential mediator of the relationship between caste and mental health. Another issue was that the common migration of Dalit/Nepali men to India for work decreased the material social support available to others in their extended family. Migrating for work meant that fewer men were available to assist others in the Jumla. Numerous older Dalit/Nepali men described concern over their emigrated adult children, “I will have to work until my last breath if my son does not return.” Another man reported that all six of his sons were working in India, but he rarely received money.
Stressful life events as mediator
Based on the descriptions above, it is not surprising that caste groups differed in reports of exposure to stressful life events and that these events were associated with psychological distress. Dalit/Nepali reported that they were more vulnerable to injury because of their work in manual labor, and they complained of greater health problems. They also described losing their parents to illness when they were children. Dalit/Nepali participants reported that they felt more vulnerable to stressful political and security events. They felt the police, army, and political officials could exploit and persecute Dalit/Nepali persons with impunity. High caste participants echoed some of the stressors related to poverty reported by Dalit/Nepali but to a lesser degree. Thus, we included exposure to stressful life events as a potential mediator.
Education excluded from mediator list
We also asked about education in relation to caste and mental health. It did not have a clear association with castes. Dalit/Nepali participants described not being able to attend school because of discrimination by other groups, although they suggest that this has improved for the current generation. There were also restrictions upon upper castes for access to education. Young adult Brahman women described distress from not being able to obtain an education because it was seen as spoiling women before marriage. One Brahman man described not attending school because his grandfather would not allow him to study where Dalit/Nepali children also studied. Based on this finding, the meaningfulness of education as a descriptor was questionable, and education was not selected as a potential mediator.
Epidemiology
Epidemiology study design and population
This was a cross-sectional study with random sampling of one adult per household. The sample was recruited for a psychiatric epidemiology study of depression and somatization from February through August 2000 (Kohrt et al. 2005). It is important to note that this study was conducted prior to mass Maoist violence in the area, which began in late 2001. Prior to the study, there had been no major attacks by Maoists in the study area. The study location included a bazaar (semi-urban) region and contiguous rural areas of Jumla. All participants were 18 years of age or older and were read a consent form. Consent was recorded with a signature for literate or a thumbprint for illiterate participants. The Department of Psychiatry at Tribhuvan University Teaching Hospital/Institute of Medicine in Kathmandu provided consultation prior to and during the assessment and gave final approval for the study. Caste was assessed through self identification. The main exposure variable was caste and the outcome variables were depression and anxiety.
Study instruments
Beck Depression Inventory (BDI) and Beck Anxiety Inventory (BAI)
These 21-item scales were used to assess depression and anxiety symptoms over the prior two weeks. Items are scored 0-3 with an instrument range of 0 to 62. Both scales have been validated for use in Nepal (Kohrt et al. 2002; Kohrt et al. 2003): area under the curve (AUC), which captures the amount of correctly classified persons in this case for moderate depression or anxiety, was 0.919 (95% CI 0.878—0.960) for the BDI and 0.847 (95% CI 0.789—0.906) for the BAI; internal reliability was also high, BDI Cronbach's α=0.90 and BAI α=0.90. Based on clinical validation of the BDI in Nepal, a score of 20 or higher suggests moderate depression with the need for mental health intervention (sensitivity=0.73, specificity=0.91). On the BAI, a score of 17 or higher indicates moderate anxiety with the need for intervention (sensitivity=0.77, specificity=0.81). Two-week test-retest reliability Spearman-Brown coefficients for the BDI were 0.84 and for the BAI were 0.88.
Stressful Life Events Rating Scale for Cross Cultural Research (SLERS)
Individuals reported both the frequency (number of times an event occurred in the past 12 months) of stressful life events with the SLERS (Zheng and Lin 1994). This instrument consists of nine subscales: academic events (3 items, e.g. failed exam, left school), intimate partner events (8 items, e.g. got married, fighting with spouse, spouse ran away, extramarital affair), health events (11 items, e.g. spouse death, child death, severe illness, pregnancy, miscarriage), family events (9 items, e.g. child cannot find work, child eloped, fighting with relatives, parents fighting), work events (5 items, e.g. cannot find work, not satisfied with work, fired from work), financial events (9 items, e.g. salary decreased, lost property, took a mortgage, lost livestock, crop shortage), social relationship events (7 items, e.g. disgraced in public, broken relationship with friend, criticized by others), environmental events (5 items, e.g. natural disaster, village more polluted), and political events (7 items, e.g. took part in political activities, lost job from political affiliation). Greater frequency of stressful life events (SLEs) as assessed by the SLERS is associated significantly with locally-defined psychosomatic complaints in Nepal (Kohrt et al. 2005).
Social support was assessed with nine question assessing if support was available in the following areas: care when sick, going to the bazaar or store, providing basic necessities, lending money or other financial assistance, fixing broken equipment and maintenance (e.g. kitchenware, ploughs, radio), domestic chores and work, getting advice, preparing and cooking food, and child care. These items were summed to provide a score of 0 to 9, with 9 indicating support available in all of the areas. Internal reliability, as assessed by Cronbach's alpha, was 0.87.
Demographics assessed included self-reports of gender, age, monthly household income (recorded in Nepali rupiyaa; at the time of the study US$1=70 rupiyaa), and number of livestock (e.g. water buffalo, cows, and goats).
Analytic strategy
The ethnographic study identified caste differences in psychological distress. Moreover, prior analyses with this sample revealed caste differences in prevalence of psychosomatic complaints (Kohrt et al. 2005), and other studies in Nepal have shown caste differences in mental health (Thapa and Hauff 2005). Based on the ethnographic work, it was suggested that the observed caste differences could be the result of less access to financial and livelihood resources, less diversity of social support, and greater exposure to stressful life events among members of Dalit/Nepali castes compared with persons in the Brahman and Chhetri high castes.
Our two analytic goals were: (i) to quantify the relationship of caste and the mental health outcomes (BDI and BAI); and (ii) to evaluate the possible roles of household income, number of livestock, social support, and SLEs as mediators of the relationship between caste and mental health. Odds ratios with 95% confidence intervals were used to assess the strength and statistical significance of association for caste with other categorical variables. Simple linear regression was used to assess the strength and statistical significance of associations for covariates (including caste) and the two mental health outcomes.
Covariate roles
We considered two possible roles for variables included in the analysis: mediator and confounder. We defined a possible confounder as a variable that (a) is associated with the exposure (caste) either in the data or in theory, but for which the exposure is not a plausible cause (we could not identify how any of the variables here could cause caste status), and (b) is theoretically a causal risk factor for the outcome. We considered a strong association between the variable and the outcome in the unexposed (i.e. high caste group) as data-based support for (b). If failure to control for such a variable distorted the effect estimate for caste, then the variable was considered to be a confounder. For example, in our models gender and age are confounders because age and gender do not cause caste. However, both gender and age influence the mental health outcomes. Therefore, they are included as confounds.
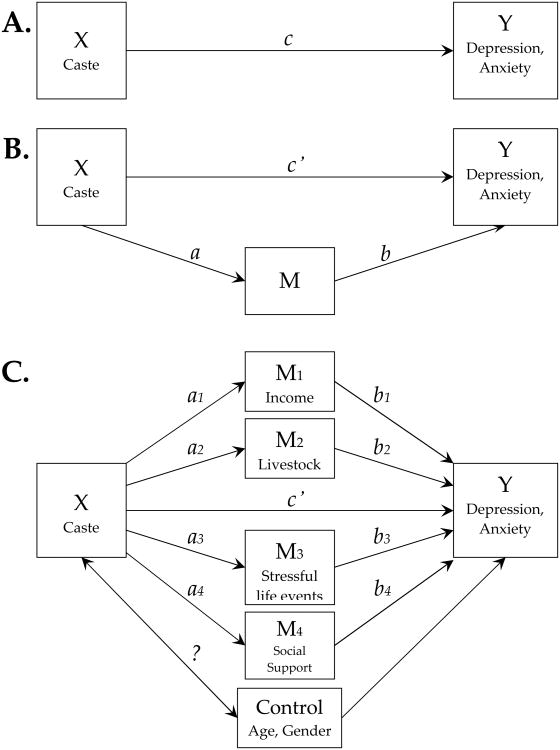
We defined a possible mediator as a variable that theoretically lies in the causal pathway from the exposure (Dalit/Nepali caste) to the mental health outcome. Figure 2A shows a diagram of a causal association between an exposure (X) and outcome (Y). In this diagram, c represents the “total effect” of X, or the effect of X when not accounting for mediation. Figure 2B shows a simple mediation model, in which one mediator (M) lies on the causal pathway from X to Y. The “direct effect,” represented by c′, is the effect of the exposure that is not explained by M. The “indirect effect,” or the effect of the exposure that is explained by the mediator, the product of the effect of X on M (represented by a) and the effect of M on Y (represented by b). We will also call the effect of M on Y (represented by b) a “direct effect” if it has no mediator in the models being considered. The indirect effect also can be conceptualized as the difference between the total effect and the direct effect (c – c′).
Figure 2.
Illustration of multiple mediation design with 4 mediators and 2 controls. (A) Unmediated model: X (caste) affects Y (mental health outcome). (B) Simple mediator model: X affects Y and M is the a single mediator. (C) Multiple mediators: X is hypothesized to exert indirect effects on Y through M1 (income), M2 (livestock), M3 (stressful life events), and M4 (social support). Path ai represents the effect of X on the proposed mediator Mi. Path bi is the effect of Mi on Y. Specific indirect effects are ai * bi. Total indirect effects represent the sum of specific indirect effects and equals (c – c′). Adapted from Preacher and Hayes, 2008.
The distinction between a confounder and a mediator is based solely on theoretical knowledge of causal relationships. Assumptions about causal relationships were based on our own ethnographic research and literature review. We considered an independent predictor to be a covariate associated with the outcome but not a confounder or mediator, and we did not include any variables that were believed a priori to be independent predictors. We did this to ground the analyses in the ethnographic data rather than test every possible association which may have shown spurious associations and required the need to account for multiple testing. We did not require statistically significant crude exposure-covariate or covariate-outcome associations in order for a variable to be considered a possible confounder or mediator, again because we employed the ethnographic data as our foundation for inclusion and exclusion. Figure 2C shows the causal diagram including all possible confounders and mediators. For our models, we did not assess interactions such as gender by caste because of the small sample size.
Evaluation of confounding
We used a backwards elimination strategy for assessment of confounding (c.f. Frazier et al. 2004; Kleinbaum et al. 1982). Each potential confounder (age and gender) was removed individually from a model with the exposure and all potential confounders as independent variables. If the point estimate for caste effect changed by more than ten percent, the variable was considered to be a confounder (c.f. Kleinbaum et al. 1982). For each outcome, the regression model including caste and confounders was used as the “base model” for mediation analysis. Age and gender were found to be confounders for depression and not for anxiety; however, we retained the variables for both outcomes to keep the “base models” for mediation analysis similar.
Evaluation of mediation
We used a regression-based approach to mediation analysis with bootstrap estimation of indirect effects. Many mediation studies use regression-based approaches (MacKinnon et al. 2002), and we explored using a regression-based method that addresses some drawbacks of traditional regression-based approaches. Bootstrapping is a non-parametric technique for obtaining parameter estimates by numerous resamplings of the data. We used Preacher and Hayes' indirect macro for SPSS, which calculates bootstrap estimates of indirect effect for models with one or more mediators (Preacher and Hayes, 2008, see http://www.comm.ohio-state.edu/ahayes/macros.htm for macro). The macro also can include covariates that are not considered to be mediators. Execution of the indirect macro provides bootstrap confidence intervals for the total indirect effect, the indirect effect of specific mediators (or the “specific indirect effect”), and comparisons (contrasts) between the specific indirect effects of mediators. Direct effects for caste and other covariates (including confounders, mediators, and independent predictors) are estimated by OLS regression. For further reading on mediation analysis, we recommend a recent review by MacKinnon and colleagues (2007).
Preacher and Hayes' indirect macro for the bootstrap estimation of multiple mediation effects has several strengths. First, simulation studies have shown that bootstrap estimation compares favorably with distribution-based estimation or significance tests for simple mediation models (i.e. one mediator), especially for small sample sizes or when the mediator is a binary variable (MacKinnon et al. 2004; Shrout and Bolger 2002). Bootstrapping also has been advocated for when a regression-based approach is used to evaluate multiple mediators (MacKinnon et al. 2007; Preacher and Hayes 2008). Another strength of the INDIRECT macro is that it allows for the inclusion of control variables. In the presence of confounding, a model that does not control for the confounder gives a biased estimate of the exposure effect. Therefore, it is desirable to control for confounders when assessing mediation of the exposure. In our study, mediation analyses that excluded the confounders yielded different estimates of indirect effect from the analyses controlling for confounders. A third strength of the INDIRECT macro is its ability to estimate indirect effects in a multiple mediator model. One of the popular regression-based mediation analysis approaches, the “causal steps” method (Baron and Kenny 1986) is not applicable to multiple mediation models. Other regression-based approaches for multiple mediator analysis have been described but, in the view of these authors, are more difficult to implement and also are based on distribution assumptions that may not be met. Lastly, the macro is available for use in common statistical analysis software (SAS and SPSS).
All statistical analyses were performed in SPSS v.16.0 (SPSS Inc. 2007).
Epidemiologic results
A total of 316 persons participated: 79 Brahman, 153 Chhetri, 9 Janajati, and 75 Dalit/Nepali. The sample included 186 men (60.6%). All Janajati individuals were women. Due to the small sample size and gender-bias of the Janajati group, they were excluded from analyses. Demographics of the sample are provided in Table I. From herein, all caste comparisons are between Dalit/Nepali and high caste (which includes Brahman and Chhetri castes).
Table I.
Crude associations of caste, covariates and mental health outcomes (n=307).
| Covariate association with caste | Covariate association with mental health outcomes | |||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Dalit/Nepali (n=75) | High Caste1 (n=232) | Dalit/Nepali vs. High Caste | Depression (BDI) | Anxiety (BAI) | ||||
| No. (%) | No. (%) | OR (95% CI)2 | p-value | β (95% CI) 3 | p-value | β (95% CI) 3 | p-value | |
| Gender | ||||||||
| Female | 17 (22.7) | 104 (44.8) | 0.36 (0.20—0.66) | .001 | 3.15 (1.09—5.20) | .003 | 4.21 (1.99—6.42) | <.001 |
| Male | 58 (77.3) | 127 (55.2) | 1 [Ref.] | [Ref.] | [Ref.] | |||
| SLEs | ||||||||
| 0-9 events | 11 (14.7) | 63 (27.2) | 1 [Ref.] | [Ref.] | [Ref.] | |||
| 10-14 events | 24 (32.0) | 94 (40.5) | 1.46 (0.67—3.20) | .34 | 2.11 (-0.422—4.64) | 0.10 | 2.41 (-0.24—5.07) | .08 |
| 15-20 events | 19 (25.3) | 53 (22.8) | 2.05 (0.90—4.70) | .09 | 4.67 (1.84—7.50) | .001 | 6.84 (3.88—9.81) | <.001 |
| 21+ events | 21 (28.8) | 22 (9.5) | 5.47 (2.28—13.13) | <.001 | 8.56 (5.29—1.84) | <.001 | 11.75 (8.31—15.18) | <.001 |
| Income | ||||||||
| No income | 49 (65.3) | 91 (39.2) | 2.92 (1.70—5.03) | <.001 | 5.47 (3.51—7.42) | <.001 | 5.87 (3.74—7.99) | <.001 |
| Any income | 26 (34.7) | 141 (60.8) | 1 [Ref.] | [Ref.] | [Ref.] | |||
| Livestock | ||||||||
| 0-6 animals | 66 (88.0) | 127 (54.7) | 6.06 (2.88—12.74) | <.001 | 3.75 (1.68—5.81) | <.001 | 3.52 (1.26—5.78) | .002 |
| 7+ animals | 9 (12.0) | 105 (45.3) | 1 [Ref.] | [Ref.] | [Ref.] | |||
| Social Support | ||||||||
| 4 or less types | 21 (28.0) | 31 (13.4) | 2.52 (1.34—4.74) | .004 | 2.67 (-0.03—5.37) | .05 | 4.47 (1.54—7.38) | .003 |
| 5 or greater types | 54 (72.0) | 201 (86.6) | 1 [Ref.] | [Ref.] | [Ref.] | |||
High caste includes Brahman and Chhetri castes.
Logistic regression used to assess crude association of caste with covariates. High Caste is reference group.
Simple linear regression coefficients (β) of covariates for mental health outcome scores (treated as continuous variables).
Descriptives
Dalit/Nepali were less likely than high castes to be female (OR=0.36, 95% CI = 0.20, 0.66). Dalits were more likely than high castes to have 21 or more SLEs (OR=5.47, 95% CI 2.28, 13.13), with a reference of 0 to 9 events. Dalits were also more likely to have no income (OR=2.92, 95% CI 1.70, 5.03), less livestock (0 to 6 animals) (OR = 6.06, 95% CI 2.88, 12.74), and four or less types of social support (OR = 2.52, 95% CI 1.34, 4.74). All potential confounders and mediators were associated significantly with depression and anxiety outcomes, see Table I. Women had higher scores compared with men for depression (β=3.15, 95% CI 1.09, 5.20) and anxiety (β=4.21, 95% CI 1.99—6.42). Similarly, greater SLEs, less income, and fewer livestock were associated with depression and anxiety (p<.05). Less diversity of social support were associated with anxiety (p=.003) but not with depression (p=.05).
Crude association between caste and mental health
Our first analytic goal was to quantify the relationship of caste and the mental health outcomes. Dalit/Nepali participants had a greater burden of depression and anxiety compared with high caste participants, see Table II. The mean total BDI and BAI scores were greater for the Dalit/Nepali group when assessing continuous outcomes (BDI: Dalit/Nepali mean=19.98, SD=9.71, high caste mean=15.03, SD=8.51; BAI: Dalit/Nepali mean=18.11, SD=11.39, high caste mean=10.69, SD=8.57).
Table II.
Depression and anxiety by caste (n=307).
| Mental health continuous outcomes | Mental health categorical outcomes | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| Mean total score (95% CI) | t-statistic1 | p-value | No. (%) above cutoff2 | Odds Ratio (95% CI)3 | p-value | |
| Depression (BDI) | ||||||
| High Caste4 (n=232) | 15.03 (13.93—16.13) | 4.23 | <.001 | 66 (28.4) | 1.00 [Ref.] | .001 |
| Dalit/Nepali (n=75) | 19.98 (17.75—22.22) | 37 (50.0) | 2.51 (1.47—4.31) | |||
| Total sample (N=307) | 16.24 (15.23—17.25) | 103 (33.7) | ||||
| Anxiety (BAI) | ||||||
| High Caste4 (n=232) | 10.69 (9.58—11.80) | 5.18 | <.001 | 47 (20.3) | 1.00 [Ref.] | <.001 |
| Dalit/Nepali (n=75) | 18.11 (15.49—20.73) | 38 (50.7) | 4.04 (2.32—7.04) | |||
| Total sample (N=307) | 12.50 (11.39—13.61) | 85 (27.7) | ||||
Independent t-tests were used to compare continuous scale mean scores between High Caste and Dalit/Nepali caste.
Validated Nepali cutoff scores indicating moderate or severe distress and need for mental health intervention are 20 or greater for the BDI (Kohrt et al. 2002) and 17 or greater for the BAI (Kohrt et al. 2003).
Mantel-Haenszel odds ratio estimate and Wald confidence intervals with High Caste as the referent group.
High Caste includes Brahman and Chhetri castes.
We also assessed binary outcomes (depressed vs. not and anxious vs. not) using validated Nepali cutoff scores. Dalit/Nepali participants were more likely than high caste participants to be above the BDI cutoff score for depression intervention (OR=2.51, 95% CI 1.47, 4.31) and above the BAI cutoff score for anxiety intervention (OR=4.04, 95% CI 2.32, 7.04). When stratifying by gender, 75.0% of Dalit/Nepali women compared with 40.4% of high caste women were above the depression cutoff. For men, 43.1% of Dalit/Nepali was above the depression cutoff compared with 18.8% of high caste men. For anxiety, 70.6% of Dalit/Nepali women were above the cutoff compared with 33.7% of high caste women. And, 44.8% of Dalit/Nepali men were above the anxiety cutoff compared with 9.4% of high caste men. We present the binary outcomes only to allow comparison of prevalence rates with other settings; for all subsequent analyses in this paper we employ the continuous outcomes.
Exposure to specific categories of stressful life events varied by caste, with Dalit/Nepali participants reporting more health, family, financial, environmental, and political stressful life events (see Table III). In contrast, high caste participants reported more academic stressful events. All of the stress categories except work events were associated with depression. All of the stress categories were associated with anxiety except social relationship stressors.
Table III.
Crude associations of number of stressful life events (SLEs) by category with caste and mental health outcomes (n=307).
| Covariate association with caste | Covariate association with mental health outcomes | |||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Dalit/Nepali (n=75) | High Caste1 (n=232) | Dalit/Nepali vs. High Caste2 | Depression (BDI) | Anxiety (BAI) | ||||
| Mean (SD) | Mean (SD) | Mean difference (95% CI) | p-value | β (95% CI) 3 | p-value | β (95% CI) 3 | p-value | |
| Stressful life events | ||||||||
| Academic events | 0.08 (0.35) | 0.17 (0.34) | -0.08 (-0.17—0.02) | .09 | -5.53 (-8.41— -2.66) | <.001 | -3.30 (-6.44— -0.15) | <.001 |
| Romantic relationships | 0.20 (0.36) | 0.14 (0.21) | 0.06 (-0.02—0.15) | .15 | 9.15 (5.22—13.07) | <.001 | 12.91 (8.79—17.04) | <.001 |
| Health events | 0.25 (0.31) | 0.14 (0.21) | 0.12 (0.04—0.19) | .003 | 9.59 (5.56—13.61) | <.001 | 15.54 (11.40—19.68) | <.001 |
| Family events | 0.51 (0.47) | 0.31 (0.21) | 0.20 (0.09—0.31) | .001 | 6.72 (4.06—9.39) | <.001 | 8.71 (5.89—11.53) | <.001 |
| Work events | 0.31 (0.59) | 0.19 (0.29) | 0.07 (-0.02—0.26) | .09 | 2.30 (-0.33—4.92) | .09 | 4.58 (1.78—7.38) | .001 |
| Financial events | 0.39 (0.35) | 0.27 (0.29) | 0.04 (0.04—0.20) | .003 | 6.56 (3.37—9.74) | <.001 | 8.41 (5.02—11.80) | <.001 |
| Social relationships | 0.19 (0.25) | 0.16 (0.27) | 0.03 (-0.04—0.09) | .46 | 4.28 (0.37—8.19) | .03 | 1.94 (-2.30—6.17) | .37 |
| Environmental events | 0.73 (0.61) | 0.55 (0.28) | 0.18 (0.03—0.32) | .02 | 3.14 (0.60—5.67) | .02 | 3.50 (0.77—6.23) | .01 |
| Political events | 0.23 (0.25) | 0.15 (0.27) | 0.09 (0.02—0.15) | .02 | 5.15 (1.39—8.91) | .007 | 9.38 (5.79—13.69) | <.001 |
High caste includes Brahman and Chhetri castes.
Independent samples t-tests used to assess crude association of stressful life events with caste.
Simple linear regression coefficients (β) of stressful life events category with mental health outcome scores.
Total, direct, and indirect effects of caste
Adjusting for age and gender, the total effect of Dalit/Nepali caste on depression score was 4.33 (95% CI 2.21, 6.45) (Model 1, Table IV). The total effect of Dalit/Nepali caste on anxiety was 7.86 (95% CI 5.48, 10.23). Adjusting for age, gender, and potential mediators (SLEs, livestock, income, and social support), the direct effect of Dalit/Nepali caste on depression was 1.08 (95% CI -1.10, 3.27) and 4.76 (95% CI 2.33, 7.19) on anxiety.
Table IV.
Direct and indirect effects for Dalit/Nepali caste versus High Caste on depression and anxiety scales (n=307).
| Depression (BDI total score) | Anxiety (BAI total score) | |
|---|---|---|
|
| ||
| Effect3 (95% CI) | Effect3 (95% CI) | |
| Model 11:total caste effect (without mediators) | ||
| Caste (Dalit/Nepali vs. High Caste [ref]) | 4.33 (2.21—6.45)3 | 7.86 (5.48—10.23)3 |
| Gender (Female vs. Male [ref]) | 4.51 (2.67—6.35) | 5.88 (3.83—7.94) |
| Age (year increase) | 0.29 (0.22—0.36) | 0.15 (0.07—0.23) |
| Model 22:direct effects | ||
| Direct effects of caste and covariates/potential confounders | ||
| Caste4 (Dalit/Nepali vs. High Caste [ref]) | 1.08 (-1.10—3.27) | 4.76 (2.33—7.19) |
| Gender (Female vs. Male [ref]) | 3.93 (2.20—5.66) | 5.45 (3.53—7.38) |
| Age (year increase) | 0.30 (0.23—0.36) | 0.15 (0.07—0.22) |
| Direct effects of potential mediators | ||
| SLEs (4 ordinal levels vs. lowest SLEs [ref]) | 1.43 (0.52—2.35) | 2.67 (1.66—3.69) |
| Livestock (0 thru 6 animals vs. 7 or more animals [ref]) | 3.90 (2.09—5.70) | 2.14 (0.13—4.15) |
| Income (no income vs. any income [ref]) | 2.85 (1.02—4.67) | 1.83 (-0.20—3.85) |
| Social support (0 thru 4 types vs. 5 or more types [ref]) | 1.97 (-0.28—4.21) | 3.09 (0.59—5.59) |
| Model 22:indirect (mediation) effects | ||
| Total indirect effect | 3.25 (2.13—4.49)5 | 3.10 (1.83—4.71)5 |
| Specific indirect effects5 | ||
| SLEs (4 ordinal levels vs. lowest SLEs [ref]) | 0.72 (0.24—1.48) | 1.35 (0.60—2.37) |
| Livestock (0 thru 6 animals vs. 7 or more animals [ref]) | 1.47 (0.75—2.36) | 0.81 (0.10—1.61) |
| Income (no income vs. any income [ref]) | 0.77 (0.26—1.64) | 0.49 (0.01—1.25) |
| Social support (0 thru 4 types vs. 5 or more types [ref]) | 0.29 (-0.03—1.00) | 0.45 (0.07—1.21) |
Model 1: Covariates/independent variables are caste, age, Gender.
Model 2: Covariates/independent variables are caste, age, Gender, and the potential mediators (stressful life events, livestock, income, and social support).
Effects for Model 1 and for direct effects in Model 2 are OLS linear regression coefficients with Wald confidence intervals.
This is the “direct effect” of caste, or the effect of caste not attributable to the mediators that are included in the model.
Indirect effects for Model 2 are bootstrap point estimates with 2.5th and 97.5th percentile confidence intervals, analogous to 95% confidence intervals. Number of boostrap resamples=5000.
Our second analytic goal was to evaluate the possible roles of household income, number of livestock, social support, and SLEs as mediators of the relationship between caste and mental health. The total indirect effect of the four mediators considered, which was the sum of the specific indirect effects for the four mediators, was 3.25 (95% CI 2.13, 4.49) on depression and 3.10 (95% CI 1.83, 4.71) on anxiety. SLEs had a significant specific indirect effect on depression (0.72, 95% CI 0.24, 1.48) and anxiety (3.10, 95% CI1.83, 4.71). Number of livestock had a significant specific indirect effect for depression (1.47, 95% CI 0.75, 2.36) and anxiety (0.81, 95% CI 0.10, 1.61). Level of income had a significant specific indirect effect on depression (0.77, 95% CI 0.26, 1.64) and anxiety (0.49, 95% CI 0.01, 1.25). Social support had a significant specific indirect effect on anxiety (0.45, 95% CI 0.07, 1.21). There were no significant contrasts between the mediators, meaning that no mediator had a significantly greater indirect effect than any other mediator for either depression or anxiety. All presented indirect effect estimates are bootstrap-based with percentile confidence intervals that are analogous to 95% confidence intervals.
These results indicate that the effect of Dalit/Nepali caste on both depression and anxiety is partially mediated by the mediators that were considered. Each of the mediators considered had a significant specific indirect effect, meaning that each was a statistically significant mediator when including the other three mediators in the model.
Direct effects of covariates
In the models with caste, gender, and age (Model 1, Table IV), female gender was associated with higher BDI (β=4.51, 95% CI 2.67, 6.35) and higher BAI (β=5.88, 95% CI 3.83, 7.94). This association remained in the full models (Model 2, Table IV), with effects of 3.93 (95% CI 2.20, 5.66) and 5.45 (95% CI 3.53, 7.38) for depression and anxiety, respectively. In the full models, increasing category of SLEs was associated with higher depression score (β=1.43, 95% CI 0.52, 2.35) and higher anxiety score (β=2.67, 95% CI 1.66, 3.69). Similarly, livestock had statistically significant direct effects on depression or anxiety in the full models. Income only had a statistically significant direct effect for depression, and social support only had a statistically significant direct effect for anxiety.
Discussion
This study examined possible mechanisms underlying caste differences in mental health outcomes. Dalit/Nepali castes have considerably greater prevalence of depression and anxiety when compared with high castes. The association of caste with depression was mediated by exposure to stressful life events, number of livestock, and household income. When considering these mediators, the direct effect of caste on depression was not significant. This suggests that much of the caste disparity in depression can be explained by the processes of poverty and livelihood insecurity, as measured by low income and lack of livestock, and greater exposure to stressful life events. The relationship of these risk factors with depression is not novel (Desjarlais et al. 1995; Kessler et al. 2008). However, what is surprising is that these mediators alone were able explain the majority of the association of Dalit/Nepali caste with depression.
Stressful life events, number of livestock, household income, and social support were mediators of the association between caste and anxiety. In contrast to depression, the direct effect of caste on anxiety (i.e., the effect when controlling for mediators) was statistically significant and of a clinically meaningful magnitude. This suggests that there was a large amount of influence of caste on anxiety not explained by these mediators, which raises the question: What are the other possible mediators for the relationship between caste and anxiety? Two possible mediators are acute discrimination and history of economic status; the former we did not assess, and we only assessed current economic status rather livelihood stability over time. Ultimately, the different findings for depression and anxiety support the continued exploration of them as independent—although often comorbid—disorders, despite claims that the distinction between these disorders in international settings is “not clinically valid” (Patel 2001).
There also may be caste-differences in the meaning and endorsement of symptoms. For example, Cole has shown that Brahman children learn to differentially endorse anger symptoms compared with Tibeto-Burman language speaking children in Nepal and compared with children in the United States (Cole et al. 2006). Ethnographic research should explore whether Chhetri endorse depression and anxiety symptoms less because of the group's history as rulers and protectors of their communities, whereas Dalit/Nepali and Brahman may endorse these complaints more readily due to of the importance of suffering (Nepali dukha) in expressing religious devotion.
One of the dramatic findings was the high prevalence rate of depression (33.7%) and anxiety (27.7%) in the sample as a whole. Psychiatric epidemiology in Nepal has been extremely limited; one other study found a prevalence rate of 18.4% of any mental disorder in a rural community (Subedi et al. 2004; Tausig et al. 2004). This was a Janajati (not caste-Hindu) group on a motorable road in a tourist region with a greater human development index than Jumla. Our prevalence rates are also higher than the 12-month prevalence rates observed in the WHO World Mental Health Surveys (Kessler et al. 2008), for example, depression and anxiety rates: South Africa (9.8%, 15.8%), Nigeria (1.1%, 4.2%), and Columbia (6.9%, 13.5%). However, these studies showed regional variation with some areas having a third greater prevalence rates of depression and anxiety. Given that Nepal ranks considerable lower than these countries on human development indices, and that Jumla is in the area of Nepal that ranks the lowest in the country, our prevalence rates may reasonably estimate levels of moderate depression and anxiety.
A unique contribution of this research was the use of ethnographically informed multiple mediator models to test and explore the association of caste with mental health. We also note that we used a confounding assessment method that is commonly used in epidemiological studies (the “change-in-estimate” criteria), and a mediation analysis approach that is popular in the social sciences literature (estimation of the indirect effect). These approaches are similar in that both are based on changes in the magnitude of the exposure effect that occur when including a possible confounder or mediator in the model. As we have noted, decisions about whether or not a variable should be considered a possible confounder or a possible mediator should be based on theory of causal pathways. Some social science researchers suggest using the same analytical method to assess both confounding and mediation (MacKinnon et al. 2000; Preacher and Hayes 2008), and this issue should be explored in the future.
An alternative mediation analysis method for handling multiple mediators is structural equation modeling (SEM). SEM would have several advantages over the method we employed: the capability to model latent variables or measurement error, and the capability to compare models using global fit tests. We feel that a regression-based approach is easier to interpret for readers not well-versed in mediation analysis, but SEM may be useful analytic tool for future studies.
In addition to our main analyses of interest, this study also revealed that caste is just one of a number of risk factors for poor mental health in rural Nepal. Female gender was a strong predictor of poor mental health. Women described experiences of domestic violence and stressful events related to intimate partners. This is consistent with global mental health research which shows women at greater risk of psychological distress across cultures and world regions (Das et al. 2007; Desjarlais et al. 1995). In addition to gender, age was a strong independent risk factor for anxiety and depression. Subedi and collaborators (2004) also have identified aging as a important risk factor for mental illness in Nepal; as well as in other low income settings across the world (Das et al. 2007). One of the surprising findings was the inverse association of academic stressful events with depression and anxiety. This is most likely a result of academic stress events being more common among younger participants, those pursuing higher education, and those with better financial standing—all factors that likely contribute to better mental health. Our failure to find ethnographic support for education as a potential causal factor for poor mental health also has been observed in Bosnia, Indonesia, Mexico, and India (Das et al. 2007).
An important caveat for the interpretation of these results is the possibility of reverse causation, or the situation in which the dependent variable, in this case mental health status, may affect the independent variables. It is possible that mental health status can affect economic status, exposure to stressful events, and amount of social support, in which case we cannot make the assumptions of causality that are necessary for the consideration of these variables as mediators. In our ongoing work with this population, we will be exploring this issue through longitudinal studies, which provide temporal sequence and thus more information for inferences regarding causality.
Ultimately, we are left with the challenge of how to improve the mental health in Nepal, especially for Dalit/Nepali women and men. From a mental health perspective, we would argue that concrete actions could be taken to address the mediators of poor mental health. This could be done through income generation and microcredit programs especially for Dalit/Nepali women, through promoting inclusion of Dalit/Nepali women and men in civil service and government jobs, through making healthcare available locally and providing economic support for transport to medical care in urban centers, and through harm reduction in migratory labor with mechanisms developed for earnings out of the country to benefit relatives in Jumla. In addition, the damaging effects of caste-based social inequity should encourage the United Nations and other bodies developing global human rights policy to eradicate caste discrimination and its mediating sequelae. However, this study also demonstrates the need to address the overall high rate of depression and anxiety in rural Nepali communities by providing support to other risk groups such as the elderly and women. Reduction of depression and anxiety in rural Nepal requires multisectoral interventions that address social marginalization, structural support, and mental health services.
Acknowledgments
The first author was funded by a Fulbright Fellowship, NIHM NRSA F31, the Wenner-Gren Foundation, and the Graduate School of Arts and Sciences and the Department of Anthropology at Emory University. The authors thank the research staff and participants from Jumla, Nepal, especially Ganesh Rokaya and Indra Subba. Thanks to the Fulbright program in Nepal including Michael Gill and Peter Moran. Special thanks to Christina Chan, Michael Cipra, and Nathan Eagle for their support and assistance during the research period. Peter Brown, Craig Hadley, and Daniel Hruschka provided invaluable feedback during the drafting of this manuscript.
References
- Ahmed AT, Mohammed SA, Williams DR. Racial discrimination & health: pathways & evidence. Indian Journal of Medical Research. 2007;126:318–27. [PubMed] [Google Scholar]
- Balaji AB, Claussen AH, Smith DC, Visser SN, Morales MJ, Perou R. Social support networks and maternal mental health and well-being. J Womens Health (Larchmt) 2007;16(10):1386–1396. doi: 10.1089/jwh.2007.CDC10. [DOI] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. Journal of Personality & Social Psychology. 1986;51(6):1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Cole PM, Walker AR, Lama-Tamang MS. Emotional Aspects of Peer Relations Among Children in Rural Nepal. In: Chen Xinyin, French Doran C, Schneider Barry H., editors. Peer relationships in cultural context. 2006. [Google Scholar]
- Das J, Do QT, Friedman J, McKenzie D, Scott K. Mental health and poverty in developing countries: revisiting the relationship. Social Science & Medicine. 2007;65(3):467–480. doi: 10.1016/j.socscimed.2007.02.037. [DOI] [PubMed] [Google Scholar]
- Desjarlais RR, Eisenberg L, Good B, Kleinman AM. World mental health: problems and priorities in lowincome countries. New York: Oxford University Press; 1995. p. 382. [Google Scholar]
- Dressler WW, Balieiro MC, dos Santos JE. Culture, socioeconomic status, and physical and mental health in Brazil. Medical Anthropology Quarterly. 1998;12(4):424–446. doi: 10.1525/maq.1998.12.4.424. [DOI] [PubMed] [Google Scholar]
- Frazier PA, Tix AP, Barron KE. Testing Moderator and Mediator Effects in Counseling Psychology Research. Journal of Counseling Psychology. 2004;51:115–134. [Google Scholar]
- Hadley C, Patil CL. Food insecurity in rural Tanzania is associated with maternal anxiety and depression. American Journal of Human Biology. 2006;18:359–68. doi: 10.1002/ajhb.20505. [DOI] [PubMed] [Google Scholar]
- Hadley C, Patil CL. Seasonal changes in household food insecurity and symptoms of anxiety and depression. American Journal of Physical Anthropology. 2008;135:225–32. doi: 10.1002/ajpa.20724. [DOI] [PubMed] [Google Scholar]
- HMG-CBS. Census Results-2001. His Majesty's Goverment Central Bureau of Statistics; Kathmandu, Nepal: 2003. [Google Scholar]
- Höfer A. The caste hierarchy and the state in Nepal: a study of the Muluki Ain of 1854. Lalitpur: Himal Books; 2004. p. xxxvii.p. 238. [Google Scholar]
- Holtz TH. Refugee trauma versus torture trauma: a retrospective controlled cohort study of Tibetan refugees. Journal of Nervous & Mental Disease. 1998;186(1):24–34. doi: 10.1097/00005053-199801000-00005. [DOI] [PubMed] [Google Scholar]
- Hruschka DJ, Hadley C. A glossary of culture in epidemiology. Journal of Epidemiology & Community Health. 2008;62(11):947–951. doi: 10.1136/jech.2008.076729. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Kuhn J, Prescott CA. The interrelationship of neuroticism, sex, and stressful life events in the prediction of episodes of major depression. American Journal of Psychiatry. 2004;161(4):631–636. doi: 10.1176/appi.ajp.161.4.631. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Üstün TB World Health Organization. The WHO World Mental Health Surveys: global perspectives on the epidemiology of mental disorders. Cambridge; New York; Geneva: Cambridge University Press; 2008. p. xviii.p. 580. Published in collaboration with the World Health Organization. [Google Scholar]
- Kleinbaum DG, Kupper LL, Morgenstern H. Epidemiologic research: principles and quantitative methods. Belmont, Calif: Lifetime Learning Publications; 1982. p. xix.p. 529. [Google Scholar]
- Koenig HG. Religion and medicine II: religion, mental health, and related behaviors. International Journal of Psychiatry in Medicine. 2001;31(1):97–109. doi: 10.2190/BK1B-18TR-X1NN-36GG. [DOI] [PubMed] [Google Scholar]
- Kohrt BA, Kunz RD, Baldwin JL, Koirala NR, Sharma VD, Nepal MK. “Somatization” and “Comorbidity”: A Study of Jhum-Jhum and Depression in Rural Nepal. Ethos. 2005;33(1):125–147. [Google Scholar]
- Kohrt BA, Kunz RD, Koirala NR, Sharma VD, Nepal MK. Validation of a Nepali version of the Beck Depression Inventory. Nepalese Journal of Psychiatry. 2002;2(4):123–130. [Google Scholar]
- Kohrt BA, Kunz RD, Koirala NR, Sharma VD, Nepal MK. Validation of the Nepali Version of the Beck Anxiety Inventory. Journal of the Institute of Medicine. 2003;25(1):1–4. [Google Scholar]
- Krieger N. Stormy weather: race, gene expression, and the science of health disparities. American Journal of Public Health. 2005;95:2155–60. doi: 10.2105/AJPH.2005.067108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lannin DR, Mathews HF, Mitchell J, Swanson MS, Swanson FH, Edwards MS. Influence of socioeconomic and cultural factors on racial differences in late-stage presentation of breast cancer. JAMA. 1998;279:180–1 7. doi: 10.1001/jama.279.22.1801. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP, Fairchild AJ, Fritz MS. Mediation analysis. Annual Review of Psychology. 2007;58:593–614. doi: 10.1146/annurev.psych.58.110405.085542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychol Methods. 2002;7(1):83–104. doi: 10.1037/1082-989x.7.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Krull JL, Lockwood CM. Equivalence of the mediation, confounding and suppression effect. Prevention Science. 2000;1:173–81. doi: 10.1023/a:1026595011371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, Williams J. Confidence limits for the indirect effect: Distribution of the product and resampling methods. Multivariate Behavioral Research. 2004;39:99–128. doi: 10.1207/s15327906mbr3901_4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mollica RF, Cui X, McInnes K, Massagli MP. Science-based policy for psychosocial interventions in refugee camps: a Cambodian example. Journal of Nervous & Mental Disease. 2002;190(3):158–166. doi: 10.1097/00005053-200203000-00004. [DOI] [PubMed] [Google Scholar]
- Patel V. Cultural factors and international epidemiology. British Medical Bulletin. 2001;57:33–45. doi: 10.1093/bmb/57.1.33. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav Res Methods. 2008;40(3):879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- Shrestha NM, Sharma B, Van Ommeren M, Regmi S, Makaju R, Komproe I, Shrestha GB, de Jong JT. Impact of torture on refugees displaced within the developing world: symptomatology among Bhutanese refugees in Nepal. Jama. 1998;280(5):443–448. doi: 10.1001/jama.280.5.443. [DOI] [PubMed] [Google Scholar]
- Shrout PE, Bolger N. Mediation in experimental and nonexperimental studies: new procedures and recommendations. Psychological Methods. 2002;7:422–45. [PubMed] [Google Scholar]
- SPSS Inc. SPSS Version 16 Version 16.0. Chicago: SPSS Inc; 2007. [Google Scholar]
- Subedi S, Tausig M, Subedi J, Broughton CL, Williams-Blangero S. Mental illness and disability among elders in developing countries: the case of Nepal. Journal of Aging & Health. 2004;16(1):71–87. doi: 10.1177/0898264303260446. [DOI] [PubMed] [Google Scholar]
- Thapa SB, Hauff E. Psychological distress among displaced persons during an armed conflict in Nepal. Social Psychiatry and Psychiatric Epidemiology. 2005;40(8):672–679. doi: 10.1007/s00127-005-0943-9. [DOI] [PubMed] [Google Scholar]
- Williams DR, Jackson PB. Social sources of racial disparities in health. Health Aff (Millwood) 2005;24(2):325–334. doi: 10.1377/hlthaff.24.2.325. [DOI] [PubMed] [Google Scholar]
- Williams DR, Williams-Morris R. Racism and mental health: the African American experience. Ethnicity & Health. 2000;5(3-4):243–268. doi: 10.1080/713667453. [DOI] [PubMed] [Google Scholar]
- Williams DR. Racial discrimination & health: pathways & evidence. Indian Journal of Medical Research. 2007;126:318–27. [PubMed] [Google Scholar]
- Williams DR, Neighbors HW, Jackson JS. Racial/ethnic discrimination and health: findings from community studies. American Journal of Public Health. 2003;93:200–8. doi: 10.2105/ajph.93.2.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng YP, Lin KM. A nationwide study of stressful life events in Mainland China. Psychosomatic Medicine. 1994;56(4):296–305. doi: 10.1097/00006842-199407000-00004. [DOI] [PubMed] [Google Scholar]