Abstract
Background
Whereas statins are considered the cornerstone of prevention after acute myocardial infarction (AMI), concerns about worsening depression in association with their use have been raised.
Methods
Using data from 2 prospective AMI registries (PREMIER and TRIUMPH), we examined the change in depressive symptoms from baseline and at 1, 6 and 12 months among statin-naïve patients who were and were not discharged on a statin. Depressive symptoms were assessed with the 8-item Patient Health Questionnaire (PHQ-8). Within-group change in PHQ-8 scores from baseline to each follow-up period was assessed using paired t-tests. A repeated measures propensity-matched analysis examined whether changes in PHQ-8 scores from baseline were different between statin-treated and statin-untreated patients.
Results
Of 3675 patients not previously treated with statins, 3050 (83%) were discharged on a statin and 625 (17%) were not. PHQ-8 scores in the statin group decreased from baseline by a mean (±SD) of 0.9 (±5.1), 1.2 (±5) and 1.1 (±5.1) at 1-, 6-, and 12-months, respectively. Corresponding changes in the non-statin group, were 0.9 (±5.2), 1.3 (±5.1) and 1.5 (±5.8), respectively (P<0.0001 for all comparisons). After propensity-matching 451 patients not discharged on statins with 1240 patients discharged on statins, the mean change in PHQ-8 scores between baseline and the 3 follow-up time points was not significantly different between groups (mean between-group difference at 1-month: −0.13, 95% CI [−0.69 to 0.43], P=0.65; at 6-months: −0.07, 95% CI [−0.66 to 0.52], P=0.82; and at 12-months: −0.05, 95% CI [−0.67 to 0.58], P=0.88).
Conclusions
Initiation of statins after AMI was not associated with worsening depression.
Depression is common among patients with acute myocardial infarction (AMI)1 and is associated with medication non-adherence,2 increased health care costs 3 and diminished quality of life.4, 5 Moreover, depression is associated with higher morbidity and mortality among AMI survivors.6, 7 Therefore, identifying modifiable factors which may influence the development of depressive symptoms in patients with AMI could provide targets for improving patients’ quality of life and survival.
Several non-modifiable factors, such as personality traits, are associated with an increased risk of depression after AMI.8–11 However, it remains unclear if there are modifiable factors—such as medication treatment—which may also increase the risk of depression after AMI. Recently, concerns have been raised about potential deleterious effects of HMG CoA reductase inhibitors (statins) on mood, cognition and other central nervous system functions.12 For example, statins have been implicated in the development of significant affective symptoms in patients with hyperlipidemia.13–16 It has also been postulated that statin use leads to chronic cholesterol depletion, which can impair the function of the serotonin1A receptor.17 Others have reported that the initiation of statin therapy evokes an increase in serotonergic transmission, which may predispose patients to depression or suicide.18 Therefore, an association between statins and depression may be biologically plausible since aberrations of central serotonergic transmission are thought to be vital in the pathogenesis of depression.19
Despite this, two prior studies have not found a consistent association between statin use and depressive symptoms.20, 21 However, these studies are limited by the use of case-control or cross-sectional study designs and by including patients who were already on chronic statin therapy. Therefore, the association between initiation of statin therapy and subsequent development of depression in statin-naïve patients remains unclear but is important to understand, as concerns about causing or exacerbating depressive symptoms with statin use may lead to statin under-treatment by physicians or poor adherence among patients.22 Clarifying this association could therefore reduce such concerns and ensure that AMI patients receive optimal evidence-based care.
Accordingly, we examined the association between the initiation of statin treatment and change in depressive symptoms in a contemporary, prospective cohort of AMI patients not previously treated with statins.
METHODS
Study Population
We used data from two US-based, multi-center, prospective, observational registries of consecutive AMI patients—the TRIUMPH (Translational Research Investigating Underlying Disparities in Acute Myocardial Infarction Patients’ Health Status)23 and PREMIER (Prospective Registry Evaluating Outcomes After Myocardial Infarctions: Events and Recovery)24 registries, which enrolled AMI patients from 2003 through 2008. Both studies employed similar data collection processes and collected similar data elements, enabling pooling of their results.
Patients in both studies were eligible for inclusion if they were 18 years or older, had elevated cardiac enzymes (troponins or creatinine kinase-MB) within 24 hours of hospital admission and had supporting evidence suggestive of AMI, including either prolonged ischemic symptoms or electrocardiographic ST-changes. Exclusion criteria included patients who were incarcerated, refused participation, were unable to provide consent, did not speak English or Spanish, were transferred to the participating hospital from another facility >24 hours after initial admission, or expired prior to being contacted by the investigators. Demographic, social, clinical, health status and psychological data for patients were collected from chart abstraction and baseline interviews by trained staff within 24 to 72 hours of the index AMI admission. All participating patients provided informed consent, and the study protocol was approved by the institutional review board at each participating center.
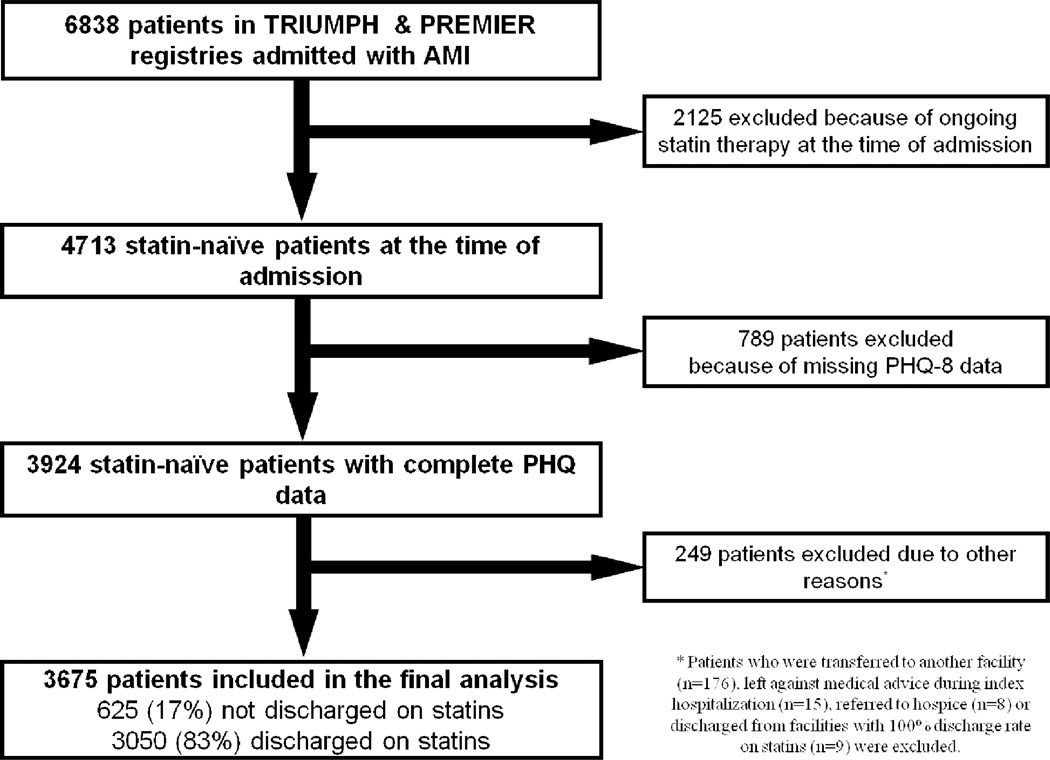
A total of 6838 AMI patients were enrolled in TRIUMPH and PREMIER. Because we were interested in examining the association between initiation of statin therapy and depressive symptoms, we excluded 2125 patients who were on statin therapy prior to the index AMI. Furthermore, we excluded 222 patients without an assessment for depression at baseline and 567 patients without any follow-up assessments of depression. We also excluded 240 patients who expired, were enrolled in hospice, transferred to another facility or left against medical advice during the index hospitalization. Finally, we excluded 9 patients from 1 participating site where 100% of patients were discharged on a statin, as our analyses compared treated and non-treated patients within hospitals. Our final study cohort comprised 3675 AMI patients from 37 centers (Figure 1).
Figure 1.
Flow Chart of Patient Inclusion and Exclusion in the Study
(AMI: Acute myocardial Infarction, PHQ-8: Patient Health Questionnaire-8)
Assessment of Depression and Study Outcome
Quantification of depressive symptoms was performed using the Patient Health Questionnaire (PHQ-8), a validated 8-item tool used for assessing depressive symptoms.25 PHQ-8 scores range from 0 to 24, with higher scores denoting more severe symptoms. A score of 10 or greater defined major depression.25 For this study, we were mainly interested in examining the association between initiation of statin therapy and subsequent change in depressive symptoms. Therefore, the primary endpoint was the change in PHQ-8 scores between the index hospitalization and 1-year follow up. We examined whether initiation of statin therapy was associated with changes in PHQ-8 scores over the first year of therapy, and whether this was different from patients not treated with statins.
Other Study Variables
Demographic variables included age, sex, and race (white, black, and other). We also measured socioeconomic variables, as they are important potential confounders of both treatment and depression. These factors included marital and employment status, educational level (completed high school, college, or graduate school, or did not complete high school), insurance coverage, perceived financial difficulties and social support. Financial difficulties were assessed during the structured interviews by asking patients, whether at the end of a month, they end up with “not enough to make ends meet” and if “healthcare costs created an economic burden for them”. Perceived social support was measured by the 5-item ENRICHD Social Support Inventory (ESSI).26 Based on prior work, low social support was defined as a score of ≤3 on 2 or more items (excluding items on instrumental social support and marital status) and having a sum score of ≤18 on the remaining 5 items.27
In addition, clinical variables were collected and included medical comorbidities (hypercholesterolemia, hypertension, diabetes mellitus, peripheral arterial disease, prior AMI, prior percutaneous coronary intervention [PCI] or coronary artery bypass surgery [CABG], prior stroke, chronic kidney disease, chronic lung disease, chronic heart failure), smoking history, obesity (body mass index ≥30), and current antidepressant treatment. Finally, data on AMI severity were also obtained including type of AMI (ST elevation vs. non-ST elevation), left ventricular ejection fraction <40%, presence of multi-vessel coronary artery disease on coronary angiography and Killip class (class I/II vs. III/IV).
Statistical Analysis
Baseline differences between patients who were and were not initiated on statin treatment during the index hospitalization were compared using Student’s t-test for continuous variables and Chi-square tests for categorical variables.
To determine whether there were changes in depressive symptoms over time in each group, we assessed for changes in PHQ-8 scores from baseline to 1-month, 6-months, and 12-months separately in the statin and non-statin groups, using paired t-tests for each time point comparison. Then, to assess whether initiation of statin therapy was associated with changes in depressive symptoms over time, we compared the mean change in depressive symptoms from baseline to each follow-up time point between the statin treated and untreated groups using a repeated measures analysis. To accomplish this, we first ensured that patients in the statin and non-statin groups were equally matched by developing a propensity score for statin treatment. A non-parsimonious propensity score was generated with a multivariable logistic regression model that included 29 baseline variables to predict treatment with a statin (C-statistic=0.742). These variables included the patient demographic, clinical, and socioeconomic variables described above. Using a caliper width no greater than 0.2 times the standard deviation of the log of the propensity score, each patient who was not initiated on a statin was then matched with up to 3 patients who were initiated on a statin using variable optimal matching (i.e., without replacement) techniques.28 We confirmed that patients treated and not treated with statins were well balanced by ensuring that standardized differences between the 2 groups for each covariate were <10.29
Among patients who were matched by propensity scores, we then compared whether changes in PHQ-8 scores from baseline to each follow-up time point differed between patients treated and not treated with statins using repeated measures models. We additionally examined for significant interactions between changes in depressive symptoms and age (≥65 vs. > 65), gender, race (white vs. other races) and baseline PHQ score (≥10 vs. <10) in the model. Finally, we conducted a sensitivity analysis to control for potential biases in loss to follow-up (i.e., patients who were excluded due to no follow-up PHQ-8 assessments). A second propensity score model was developed to predict the likelihood of follow-up assessments with the PHQ-8. The reciprocal of this probability was used to weight the associations among responders in the repeated measures model. Since results with and without weighting were comparable, the unweighted are presented.30 Finally, to account for all PHQ-8 measurements for each patient, we constructed a repeated measures model to examine if statin treatment was associated with a difference in change in depressive symptoms over time.
At least 1 study covariate was missing in 15% of patients, and 6% were missing more than 2 covariates, with the average number of missing data fields per patient of 0.5. The covariate with the most missing data was the “number of diseased vessels” (n=246, as coronary angiography was not performed in 245 patients) followed by final hematocrit (5.5% of patients). Missing data were imputed using IVEWARE,31 and all covariates that were used in the logistic propensity model were used for imputation. All tests for statistical significance were two-tailed and evaluated at a significance level of 0.05. All analyses were conducted with SAS 9.2 (SAS Institute, Inc, Cary, NC).
RESULTS
Of 3675 AMI patients not previously treated with statins, 3050 patients (83%) were discharged on a statin and 625 (17%) were not. Baseline demographic, social and clinical characteristics of both groups are shown in Table 1. Patients who were not treated with statins were older and more frequently female and African American. In addition, untreated patients had more medical comorbidities and advanced cardiac disease, including hypertension, diabetes, chronic kidney disease, prior MI, prior coronary revascularization, congestive heart failure, peripheral arterial disease, prior stroke and more severe left ventricular systolic dysfunction compared to those who were initiated on statin therapy. Patients who were receiving medications or counseling for depression during index hospitalization or who lived alone were less likely to be discharged on a statin, while those who worked full time or were married were more likely to receive a statin at the time of hospital discharge. Finally, total cholesterol and LDL-C levels were lower and HDL-C levels were higher among patients not treated with statins.
Table 1.
Baseline Characteristics of the Study Cohort by Statin Treatment
| Variable | Statin-treated (n=3050) | Statin-untreated (n=625) | P-value |
|---|---|---|---|
| Age, mean (SD) | 57.9 (12.2) | 59.8 (13.4) | <0.001 |
| Women (%) | 936 (30.7) | 256 (41.0) | <0.001 |
| African American (%) | 633 (20.8) | 180 (28.9) | <0.001 |
| Married (%) | 1719 (56.5) | 316 (50.8) | 0.009 |
| Current depression (%)* | 293 (9.6) | 81 (13.0) | 0.01 |
| Low social support (%) | 470 (15.8) | 113 (18.6) | 0.09 |
| Working full time (%) | 1427 (47.1) | 208 (33.5) | <0.001 |
| Coverage for meds | 2154 (71.6) | 443 (71.8) | 0.92 |
| Lives alone (%) | 666 (22.0) | 160 (26.0) | 0.03 |
| Some $ left over (%)† | 1429 (47.8) | 295 (48.4) | 0.77 |
| HTN (%) | 1660 (54.4) | 427 (68.3) | <0.001 |
| DM (%) | 635 (20.8) | 192 (30.7) | <0.001 |
| Hyperlipidemia (%) | 1065 (34.9) | 224 (35.8) | 0.66 |
| CKD (%) | 120 (3.9) | 74 (11.8) | <0.001 |
| Smoking history(%) | 1920 (63.0) | 360 (57.6) | 0.01 |
| STEMI (%) | 1645 (53.9) | 209 (33.4) | <0.001 |
| Cholesterol (mg/dL) | 186.9 ± 49.4 | 175.7 ± 51.2 | <0.001 |
| LDL (mg/dL) | 114.7± 39.1 | 101.8 ± 39.4 | <0.001 |
| HDL (mg/dL) | 42.1 ± 14.1 | 45.2 ± 17.2 | <0.001 |
| BMI | 29.2 ± 6.2 | 29.5 ± 7.4 | 0.33 |
Defined by either taking anti-depressants or receiving depression counseling
Denotes patients with sufficient monetary resources left at the end of each month
(BMI: Body Mass Index, CKD: Chronic Kidney Disease, DM: Diabetes Mellitus, HTN: Hypertension, SD: standard deviation)
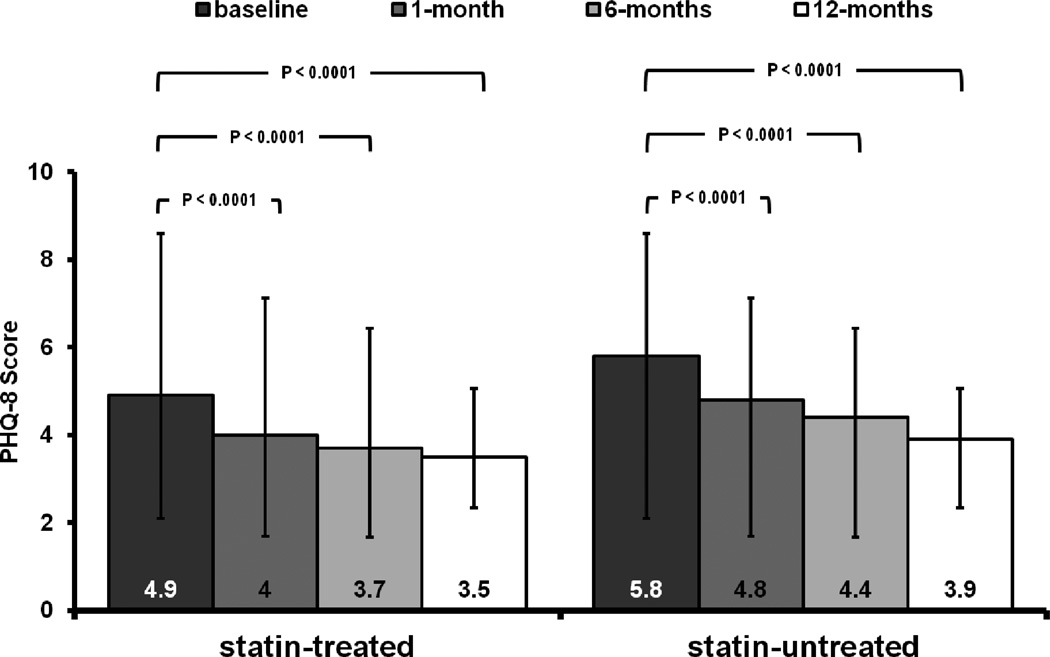
Depressive symptoms significantly decreased over time in both groups (Figure 2). In the statin group, compared with baseline values, mean PHQ-8 scores decreased by 0.9 ± 5.1 (P<0.0001) at 1 month, 1.2 ± 5 (P< 0.0001) at 6 months, and 1.1 ± 5.1 (P< 0.0001) at 12-months. Similarly, compared with baseline values, PHQ-8 scores significantly decreased in the non-statin group by 0.9 ± 5.2 (P< 0.0001), 1.3 ± 5.1 (P< 0.0001) and 1.5 ± 5.8 (P< 0.0001) at 1-, 6- and 12-months, respectively (Table 2).
Figure 2.
Mean PHQ-8 Score in Both Statin Groups at Baseline and at 1-, 6- and 12-months
Table 2.
Change in PHQ-8 Scores from Baseline in Each Statin Group
| Statin-treated (n= 3050) | P-value* | Statin-untreated (n=625) | P-value* | |
|---|---|---|---|---|
| Basealine | 4.9 ± 5.1 | N/A | 5.8 ± 5.4 | N/A |
| Baseline to 1-month | −0.9 ± 5.1 | <0.0001 | −0.9 ± 5.2 | <0.0001 |
| Baseline to 6-months | −1.2 ± 5.0 | <0.0001 | −1.3 ± 5.1 | <0.0001 |
| Baseline to 12-months | −1.1 ± 5.1 | <0.0001 | −1.5 ± 5.8 | <0.0001 |
P-value for within-group change in PHQ-8 score compared to baseline
(PHQ: Patient Health Questionnaire)
The proportion of patients with depression by PHQ-8 cut off (score ≥ 10) also decreased over time (Table 3). At baseline, 547 (17.9%) and 146 (23.4%) patients had PHQ-8 scores in the depressed range in the statin-treated and statin-untreated groups, respectively (p-value for between-group difference 0.002). This number fell over time to 313 (12.3%) statin-treated patients vs. 81 (15.8%) statin-untreated patients at 1 month (P=0.03), 282 (12%) vs. 69 (14.1%) at 6-months (P=0.19) and 255 (11%) vs. 61 (13.2%) at 12 months (P=0.18).
Table 3.
Number of Patients with PHQ-8 scores ≥ 10 in each statin group
| Statin-treated (%) | Statin-untreated (%) | P-value | |
|---|---|---|---|
| Baseline | 547 (17.9) | 146 (23.4) | 0.002 |
| 1-month | 313 (12.3) | 81 (15.8) | 0.03 |
| 6-months | 282 (12) | 69 (14.1) | 0.19 |
| 12-months | 255 (11) | 61 (13.2) | 0.18 |
(PHQ: Patient Health Questionnaire)
After propensity matching 451 statin-untreated patients with 1240 statin-treated patients, we found no significant differences in the 1-month change in PHQ-8 scores between the 2 treatment groups (mean difference in 1-month change in PHQ-8 scores between groups: −0.13, 95% CI [−0.69 to 0.43], P=0.65). Similarly, there were no significant differences in change in depressive symptoms between the 2 groups from baseline to 6-months (mean difference in PHQ-8 scores between groups of −0.07, 95% CI [−0.66 to 0.52], P=0.82) and 12-months (mean difference in PHQ-8 scores between groups of − 0.05, 95% CI [−0.67 to 0.58], P=0.88). There were no significant interactions were found between initiation of statin treatment and age, gender, race and baseline PHQ score (P for all interactions >0.05). Finally, when we incorporated all PHQ-8 measurements for each patient in a repeated measures model, we continued to find that statin treatment was not associated with differences in the change in depressive symptoms (P=0.28).
DISCUSSION
In light of potential concerns that statin therapy may be associated with depression, we conducted a detailed comparison of AMI patients’ depressive symptoms and found that initiation of statin therapy during an AMI was not associated with increased depressive symptoms. Instead, we found that depressive symptoms significantly decreased with time in both statin-treated and statin-untreated patients. After adjustment for a number of demographic, clinical, socioeconomic, and psychosocial factors, we found no difference in the mean change in depressive symptoms between the 2 patient groups. Our findings provide reassurance to clinicians that statin treatment is not associated with worsening depressive symptoms in AMI patients despite biologic and physiologic studies that suggest a potential association.
The current study confirms and extends the findings of prior clinical studies evaluating the risk of depression among statin-treated patients. A case-control analysis from an administrative database that included 60 reports of drug-related psychiatric adverse effects among 1323 statin-treated patients showed that psychiatric adverse events (including depression) were not more common with statin use compared to other classes of medications.20 A similar analysis of drug-related adverse events in community-dwelling older individuals (which included 669 patients using statins) also failed to show an association between statins use and depressive symptoms.21 Recently, a third study found that statin use was associated with a lower risk of depressive symptoms in 965 patients with stable coronary artery disease.32 These prior studies, however, were limited by case-control study designs, administrative data sources, self-reporting of adverse events,20, 21 or potential confounding, by including patients who were already on statin therapy at the time of enrollment.32 In contrast, we were able to prospectively collect information on depressive symptoms using a well-validated instrument, examine a large sample of patients who were not on chronic statin therapy, and employ a propensity score analysis to adjust for confounding. Moreover, by restricting our analyses to ‘statin-naïve’ patients to ensure that our findings were not confounded by chronic statin treatment, our study is the first to assess whether initiation of statin therapy was associated with changes in depressive symptoms in the setting of AMI.
Of note, the proportion of patients who met formal criteria for depression (PHQ-8 >10) during the index AMI hospitalization was approximately 20%, and this proportion decreased to about 11% by 1-year. This suggest that, while depression occurred in a substantial minority of patients, the majority with AMI do not meet clinical definitions for depression, although many experience milder depressive symptoms.
Inflammation and oxidative stress are thought to play a role in the development of depression after stroke and de novo.33–35 In addition, a small study of 193 patients who underwent cardiac intervention showed that statins use was associated with a lower risk of subsequent depression, which the authors attributed to the anti-oxidant and anti-inflammatory properties of statins.36 Therefore, statins may actually have a protective effect against depression via their potential anti-inflammatory and antioxidant properties, thus possibly conferring biologic plausibility to our findings, although post AMI depression may have different underlying mechanisms compared to other depression syndromes‥ We were unable in this analysis to confirm the hypothesis that statin initiation is associated with less depressive symptoms after AMI and we observed instead a similar change in depressive symptoms in both treatment groups.
Clinical Implications
Statin under-treatment remains a problem in contemporary practice. A recent report from the American College of Cardiology’s PINNACLE cardiac outpatient registry found that the rate of statin non-treatment in patients with prior AMI or coronary revascularization was 15.7%, even after excluding patients with an allergy or intolerance to statin therapy.37 Similarly, the REduction of Atherothrombosis for Continued Health (REACH) Registry found that 17% of patients with known atherosclerosis in the outpatient setting did not receive statin therapy.38 Although it is unclear why eligible patients were not treated with statins despite current treatment guidelines, our study provides further evidence that concerns about depression should not be a reason for withholding statin treatment in these settings.
Limitations and Strengths
Our study should be interpreted in the context of the following limitations. First, despite our use of a robust propensity score analysis to account for a wide array of clinical and psychosocial variables, our findings may still be subject to residual confounding. However, as the crude differences in 12-month change in depressive symptoms were not meaningfully different, the presence of significant residual confounding is unlikely. Second, the current study design does not allow for confirming actual patient adherence to statin treatment. Finally, we did not have data on the actual prescribed statin or dose; therefore, we were unable to assess whether our findings were consistent across different types of statin medications and potencies.
In contrast to these potential limitations, this study has several strengths. The assessment of depressive symptoms was performed prospectively using a well-validated tool. In addition, data on other potential and important confounders of the study’s endpoint were collected systematically by trained study coordinators using standardized definitions. Lastly, to our knowledge, this is the first study to address the association between initiation of statins and subsequent depressive symptoms after AMI in a statin-naïve cohort.
CONCLUSIONS
Treatment with statins in patients after AMI was not associated with worsening depressive symptoms. Given the established benefits of statin treatment in patients after AMI, withholding statin therapy because of concerns of worsening depression appears to be unjustified and could lead to underuse of evidence-based therapies for patients with AMI.
References
- 1.Thombs BD, Bass EB, Ford DE, Stewart KJ, Tsilidis KK, Patel U, et al. Prevalence of depression in survivors of acute myocardial infarction. J Gen Intern Med. 2006;21(1):30–38. doi: 10.1111/j.1525-1497.2005.00269.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gehi A, Haas D, Pipkin S, Whooley MA. Depression and medication adherence in outpatients with coronary heart disease: findings from the Heart and Soul Study. Arch Intern Med. 2005;165(21):2508–2513. doi: 10.1001/archinte.165.21.2508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Frasure-Smith N, Lesperance F, Gravel G, Masson A, Juneau M, Talajic M, et al. Depression and health-care costs during the first year following myocardial infarction. J Psychosom Res. 2000;48(4–5):471–478. doi: 10.1016/s0022-3999(99)00088-4. [DOI] [PubMed] [Google Scholar]
- 4.Swenson JR. Quality of life in patients with coronary artery disease and the impact of depression. Curr Psychiatry Rep. 2004;6(6):438–445. doi: 10.1007/s11920-004-0008-x. [DOI] [PubMed] [Google Scholar]
- 5.Ruo B, Rumsfeld JS, Hlatky MA, Liu H, Browner WS, Whooley MA. Depressive symptoms and health-related quality of life: the Heart and Soul Study. JAMA. 2003;290(2):215–221. doi: 10.1001/jama.290.2.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Barth J, Schumacher M, Herrmann-Lingen C. Depression as a risk factor for mortality in patients with coronary heart disease: a meta-analysis. Psychosomatic medicine. 2004;66(6):802–813. doi: 10.1097/01.psy.0000146332.53619.b2. [DOI] [PubMed] [Google Scholar]
- 7.Carney RM, Freedland KE, Steinmeyer B, Blumenthal JA, Berkman LF, Watkins LL, et al. Depression and five year survival following acute myocardial infarction: a prospective study. J Affect Disord. 2008;109(1–2):133–138. doi: 10.1016/j.jad.2007.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schrader G, Cheok F, Hordacre AL, Marker J. Predictors of depression 12 months after cardiac hospitalization: the Identifying Depression as a Comorbid Condition study. The Australian and New Zealand journal of psychiatry. 2006;40(11–12):1025–1030. doi: 10.1080/j.1440-1614.2006.01927.x. [DOI] [PubMed] [Google Scholar]
- 9.Naqvi TZ, Rafique AM, Andreas V, Rahban M, Mirocha J, Naqvi SS. Predictors of depressive symptoms post-acute coronary syndrome. Gend Med. 2007;4(4):339–351. doi: 10.1016/s1550-8579(07)80063-5. [DOI] [PubMed] [Google Scholar]
- 10.Mols F, Martens EJ, Denollet J. Type D personality and depressive symptoms are independent predictors of impaired health status following acute myocardial infarction. Heart (British Cardiac Society) 96(1):30–35. doi: 10.1136/hrt.2009.170357. [DOI] [PubMed] [Google Scholar]
- 11.Martens EJ, Smith OR, Winter J, Denollet J, Pedersen SS. Cardiac history, prior depression and personality predict course of depressive symptoms after myocardial infarction. Psychological medicine. 2008;38(2):257–264. doi: 10.1017/S0033291707001377. [DOI] [PubMed] [Google Scholar]
- 12.Golomb BA, Criqui MH, White H, Dimsdale JE. Conceptual foundations of the UCSD Statin Study: a randomized controlled trial assessing the impact of statins on cognition, behavior, and biochemistry. Arch Intern Med. 2004;164(2):153–162. doi: 10.1001/archinte.164.2.153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tatley M, Savage R. Psychiatric adverse reactions with statins, fibrates and ezetimibe: implications for the use of lipid-lowering agents. Drug Saf. 2007;30(3):195–201. doi: 10.2165/00002018-200730030-00003. [DOI] [PubMed] [Google Scholar]
- 14.Morales K, Wittink M, Datto C, DiFilippo S, Cary M, TenHave T, et al. Simvastatin causes changes in affective processes in elderly volunteers. J Am Geriatr Soc. 2006;54(1):70–76. doi: 10.1111/j.1532-5415.2005.00542.x. [DOI] [PubMed] [Google Scholar]
- 15.Hyyppa MT, Kronholm E, Virtanen A, Leino A, Jula A. Does simvastatin affect mood and steroid hormone levels in hypercholesterolemic men? A randomized double-blind trial. Psychoneuroendocrinology. 2003;28(2):181–194. doi: 10.1016/s0306-4530(02)00014-8. [DOI] [PubMed] [Google Scholar]
- 16.Buajordet I, Madsen S, Olsen H. Statins--the pattern of adverse effects with empahsis on mental reactions. Data from a national and an international database. Tidsskr Nor Laegeforen. 1997;117(22):3210–3213. [PubMed] [Google Scholar]
- 17.Shrivastava S, Pucadyil TJ, Paila YD, Ganguly S, Chattopadhyay A. Chronic cholesterol depletion using statin impairs the function and dynamics of human serotonin(1A) receptors. Biochemistry. 2010;49(26):5426–5435. doi: 10.1021/bi100276b. [DOI] [PubMed] [Google Scholar]
- 18.Vevera J, Fisar Z, Kvasnicka T, Zdenek H, Starkova L, Ceska R, et al. Cholesterol-lowering therapy evokes time-limited changes in serotonergic transmission. Psychiatry research. 2005;133(2–3):197–203. doi: 10.1016/j.psychres.2004.11.005. [DOI] [PubMed] [Google Scholar]
- 19.Haenisch B, Linsel K, Bruss M, Gilsbach R, Propping P, Nothen MM, et al. Association of major depression with rare functional variants in norepinephrine transporter and serotonin1A receptor genes. American journal of medical genetics Part B, Neuropsychiatric genetics : the official publication of the International Society of Psychiatric Genetics. 2009;150B(7):1013–1016. doi: 10.1002/ajmg.b.30912. [DOI] [PubMed] [Google Scholar]
- 20.Tuccori M, Lapi F, Testi A, Coli D, Moretti U, Vannacci A, et al. Statin-associated psychiatric adverse events: a case/non-case evaluation of an Italian database of spontaneous adverse drug reaction reporting. Drug Saf. 2008;31(12):1115–1123. doi: 10.2165/0002018-200831120-00007. [DOI] [PubMed] [Google Scholar]
- 21.Feng L, Tan CH, Merchant RA, Ng TP. Association between depressive symptoms and use of HMG-CoA reductase inhibitors (statins), corticosteroids and histamine H(2) receptor antagonists in community-dwelling older persons: cross-sectional analysis of a population-based cohort. Drugs Aging. 2008;25(9):795–805. doi: 10.2165/00002512-200825090-00005. [DOI] [PubMed] [Google Scholar]
- 22.Allen LaPointe NM, Ou FS, Calvert SB, Melloni C, Stafford JA, Harding T, et al. Changes in beliefs about medications during long-term care for ischemic heart disease. American heart journal. 2010;159(4):561–569. doi: 10.1016/j.ahj.2009.12.025. [DOI] [PubMed] [Google Scholar]
- 23.Arnold S, Chan P, Jones P, Decker C, Buchanan D, Krumholz H, et al. Translational Research Investigating Underlying disparities in acute Myocardial infarction Patient's Health status (TRIUMPH): Design and Rationale of Prospective Multicenter Registry. Circ Cardiovasc Qual Outcomes. doi: 10.1161/CIRCOUTCOMES.110.960468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Spertus JA, Peterson E, Rumsfeld JS, Jones PG, Decker C, Krumholz H. The Prospective Registry Evaluating Myocardial Infarction: Events and Recovery (PREMIER)--evaluating the impact of myocardial infarction on patient outcomes. American heart journal. 2006;151(3):589–597. doi: 10.1016/j.ahj.2005.05.026. [DOI] [PubMed] [Google Scholar]
- 25.Kroenke K, Strine TW, Spitzer RL, Williams JB, Berry JT, Mokdad AH. The PHQ-8 as a measure of current depression in the general population. J Affect Disord. 2009;114(1–3):163–173. doi: 10.1016/j.jad.2008.06.026. [DOI] [PubMed] [Google Scholar]
- 26.Mitchell PH, Powell L, Blumenthal J, Norten J, Ironson G, Pitula CR, et al. A short social support measure for patients recovering from myocardial infarction: the ENRICHD Social Support Inventory. Journal of cardiopulmonary rehabilitation. 2003;23(6):398–403. doi: 10.1097/00008483-200311000-00001. [DOI] [PubMed] [Google Scholar]
- 27.Enhancing recovery in coronary heart disease patients (ENRICHD): study design and methods. The ENRICHD investigators. American heart journal. 2000;139(1 Pt 1):1–9. doi: 10.1016/s0002-8703(00)90301-6. [DOI] [PubMed] [Google Scholar]
- 28.Paul Rosenbaum DR. Constructing a Control Group Using Multivariate Matched Sampling Methods That Incorporate the Propensity Score. The American Statistician. 1985;39(1):33–38. [Google Scholar]
- 29.Normand ST, Landrum MB, Guadagnoli E, Ayanian JZ, Ryan TJ, Cleary PD, et al. Validating recommendations for coronary angiography following acute myocardial infarction in the elderly: a matched analysis using propensity scores. J Clin Epidemiol. 2001;54(4):387–398. doi: 10.1016/s0895-4356(00)00321-8. [DOI] [PubMed] [Google Scholar]
- 30.Lunceford JK, Davidian M. Stratification and weighting via the propensity score in estimation of causal treatment effects: a comparative study. Stat Med. 2004;23(19):2937–2960. doi: 10.1002/sim.1903. [DOI] [PubMed] [Google Scholar]
- 31.Raghunathan TESP, Van Hoewyk J. IVEware: Imputation and Variance Estimation Software - User Guide. Michigan: Survey Research Center, Institute for Social Research University of Michigan; 2002. [Google Scholar]
- 32.Otte C, Zhao S, Whooley MA. Statin use and risk of depression in patients with coronary heart disease: longitudinal data from the heart and soul study. J Clin Psychiatry. 2012;73(5):610–615. doi: 10.4088/JCP.11m07038. [DOI] [PubMed] [Google Scholar]
- 33.Bilici M, Efe H, Koroglu MA, Uydu HA, Bekaroglu M, Deger O. Antioxidative enzyme activities and lipid peroxidation in major depression: alterations by antidepressant treatments. J Affect Disord. 2001;64(1):43–51. doi: 10.1016/s0165-0327(00)00199-3. [DOI] [PubMed] [Google Scholar]
- 34.Pasco JA, Nicholson GC, Williams LJ, Jacka FN, Henry MJ, Kotowicz MA, et al. Association of high-sensitivity C-reactive protein with de novo major depression. Br J Psychiatry. 2010;197(5):372–377. doi: 10.1192/bjp.bp.109.076430. [DOI] [PubMed] [Google Scholar]
- 35.Pascoe MC, Crewther SG, Carey LM, Crewther DP. Inflammation and depression: why poststroke depression may be the norm and not the exception. Int J Stroke. 2011;6(2):128–135. doi: 10.1111/j.1747-4949.2010.00565.x. [DOI] [PubMed] [Google Scholar]
- 36.Stafford L, Berk M. The use of statins after a cardiac intervention is associated with reduced risk of subsequent depression: proof of concept for the inflammatory and oxidative hypotheses of depression? J Clin Psychiatry. 2011;72(9):1229–1235. doi: 10.4088/JCP.09m05825blu. [DOI] [PubMed] [Google Scholar]
- 37.Chan PS, Oetgen WJ, Buchanan D, Mitchell K, Fiocchi FF, Tang F, et al. Cardiac performance measure compliance in outpatients: the American College of Cardiology and National Cardiovascular Data Registry's PINNACLE (Practice Innovation And Clinical Excellence) program. Journal of the American College of Cardiology. 2010;56(1):8–14. doi: 10.1016/j.jacc.2010.03.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kumar A, Fonarow GC, Eagle KA, Hirsch AT, Califf RM, Alberts MJ, et al. Regional and practice variation in adherence to guideline recommendations for secondary and primary prevention among outpatients with atherothrombosis or risk factors in the United States: a report from the REACH Registry. Crit Pathw Cardiol. 2009;8(3):104–111. doi: 10.1097/HPC.0b013e3181b8395d. [DOI] [PubMed] [Google Scholar]