Abstract
The mouse-adapted strain of poliovirus type 2 (Lansing) induces fatal poliomyelitis in mice after intracerebral inoculation, whereas mice inoculated with poliovirus type 1 (Mahoney) show no signs of disease. Previous work indicated that the adaptation to mouse virulence is associated with the viral capsid proteins and that mutations in neutralization antigenic site I of poliovirus reduce neurovirulence of the Lansing strain in mice. The role of antigenic site I in mouse neurovirulence was further explored by constructing an antigenic hybrid virus. Six amino acids in antigenic site I of the Mahoney strain were replaced with a sequence specific for the Lansing strain by using a mutagenesis cartridge. The hybrid virus was neutralized by polyclonal antisera elicited by the type 1 and type 2 strains of poliovirus and by neutralizing monoclonal antibodies directed against antigenic site I of type 2 virus. The hybrid virus induced paralytic disease in mice, an observation demonstrating that a short sequence of amino acids in antigenic site I is an important determinant of poliovirus host range. Antigenic site I may be involved in attachment of poliovirus to cells of the mouse central nervous system.
Tissue tropism of viruses and the progression of viral disease in the infected host are determined by several factors. Specific cellular surface molecules that serve as viral receptors play an important role in these events. Another determinant is the genotype of a virus because it affects replication within the cell. Genetic variants of highly virulent viruses whose genomes differ by very few nucleotides may be dramatically attenuated even though adsorption and entry of the variant are not impaired.
Poliovirus, a member of the Picornaviridae, has served as a model system to study the molecular basis of viral pathogenesis, particularly the relationship of genotype and phenotype to neurovirulence and host range (1). Attenuation of poliovirus appears to be caused largely by mutations that impair viral replication within the cell (2, 3). Polioviruses, which occur in three serotypes, are human pathogens that can be propagated only in cultured cells of primate origin because other cell lines do not express a functional receptor molecule (4). Although most poliovirus strains can infect only primates, the Lansing strain of poliovirus type 2 [PV-2(L)] has been adapted to mice (5) and causes fatal paralytic disease when inoculated intracerebrally (6). In contrast, many other poliovirus strains, including type I (Mahoney) [PV-1(M)], although highly neurovirulent in primates including man, are avirulent in mice, even when administered in high doses (7). A molecular genetic analysis of PV-2(L) has revealed that the major determinant or determinants of the mouse-adapted phenotype are contained within the four capsid polypeptides (7). A study of the neurovirulence of neutralization escape mutants of PV-2(L) suggests that the mouse-adapted phenotype is determined by a specific region of VP1 located roughly between amino acids 90 and 105 (8).
The known chemical (9) and three-dimensional (10) structures of poliovirus, the results of analyses with neutralizing monoclonal antibodies (N-mAbs) and neutralization-resistant variants, and the information gained from immunizations with synthetic peptides led to the identification of three neutralization antigenic sites (N-Ag) of the poliovirion (11). One of these sites is a continuous sequence of amino acids (90–105) in VP1 and is identical with the region to which LaMonica et al. (8) had mapped the mouse-adapted phenotype of PV-2(L). We refer to this region as N-AgI. In the crystal structures of human rhinovirus 14 (12) and of PV-1(M) (10), N-AgI occurs as a loop near the apexes of the particle.
The development of infectious poliovirus cDNA clones (13) and transcription vectors that produce unlimited amounts of highly infectious RNA in vitro (14) have made possible the construction of various poliovirus recombinants useful for studying viral replication and pathogenesis. The method of “cartridge mutagenesis,” which facilitates exchange of very small regions of the genome, was adapted for poliovirus (15). To investigate the molecular basis of neutralization and to explore the possibility of developing novel vaccines, we described the construction, via a mutagenesis cartridge, of a viable antigenic hybrid virus consisting of PV-1(M) with the N-AgI of poliovirus type 3 (Leon) [PV-3(Leon)] (16, 17). This PV-1(M)/PV-3(Leon) antigenic hybrid virus is neutralized by type 1– and type 3–specific antisera and elicits, in rabbits and monkeys, a type 1– and type 3–specific neutralizing immune response. Burke et al. (18) also obtained a viable antigenic hybrid virus [PV-1 (Sabin)/PV-3 (Sabin)] by a different route.
We have now constructed a similar hybrid virus consisting of PV-1(M) with the N-AgI of PV-2(L) and tested it for expression of the phenotype of mouse neurovirulence. The sequence of the hybrid virus around N-AgI is shown in Fig. 1, and its construction was essentially as previously described (17). Briefly, two complementary PV-2(L)–specific oligodeoxyribonucleotides with a sequence corresponding to amino acids 95–102 (7) were chemically synthesized and inserted into restriction sites of a PV-1(M) cDNA clone especially engineered for this purpose (17). The resulting plasmid contained the poliovirus cDNA preceded by a phage T7 promoter that served as a signal for transcriptional initiation with phage T7 RNA polymerase to generate infectious poliovirus genomic RNA in vitro (14). HeLa cell monolayers were transfected with the synthetic viral RNA, and virus (designated strain W1/2–1D-1) was isolated after a cyto-pathic effect had developed. Nucleotide sequence analyses of the parental plasmid DNAs, of the synthetic transcripts, and of the genomic RNA of the W1/2–1D-1 hybrid virus confirmed the expected heterotypic nucleotide sequence coding for N-AgI. Serological analysis showed that the PV- 2(L)–specific sequence that replaced the N-AgI of PV-1(M) was recognized by a type-specific polyclonal antiserum to PV-2(L), while the other neutralization antigenic sites were recognized by type 1–specific antiserum (Table 1); that is, W1/2–1D-1 was neutralized by hyperimmune sera elicited by PV-1(M) or PV-2(L). Moreover, the hybrid virus was neutralized by monoclonal antibodies specific for N-AgI of PV-2(L) (19) but not by a monoclonal antibody specific for N-AgI of PV-1(M) (20) (Table 2). Thus, the genetically engineered W1/2–1D-1 virus is a true antigenic hybrid virus similar to the PV-1(M)/PV-3(Leon) virus (16, 17).
Fig. 1.
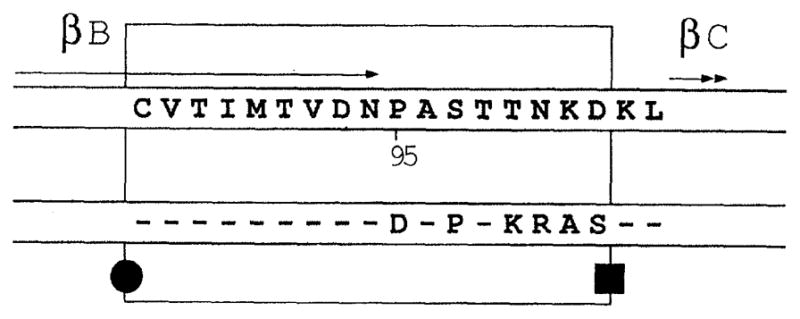
Schematic representation of the poliovirus hybrid showing β sheet B and β sheet C flanking the N-AgI loop (10, 11). Amino acids of PV-1 (M) are shown in the top shaded box and those of W1/2–1D-1 are shown in the bottom box, with the substituted amino acids unshaded. Amino acids identical between PV-1(M) and W1/2– 1D represented by dashes. The mutagenesis cartridge is enclosed in the large box. (●) The naturally occurring Sph I restriction site; (■) the newly generated Hind III restriction site (17). Abbreviations for the amino acid residues are: A, Ala; C, Cys; D, Asp; I, Ile; K, Lys; L, Leu; M, Met; N, Asn; P, Pro; R, Arg; S, Ser; T, Thr; and V, Val.
Table 1.
Serological characterization of the W1/2–1D-1 hybrid virus with neutralizing polyclonal antibodies. TCID50, median tissue culture infectious dose.
| Virus | Dilution of antibody neutralizing 100 TCID50
|
|
|---|---|---|
| Antibody to
| ||
| Type 1 | Type 2 | |
| PV-1(M) | >1:4096 | <1:2 |
| PV-2(L) | <1:2 | 1:2048 |
| W1/2–1D-1 | >1:4096 | 1:64 |
Table 2.
Serological characterization of the W1/2–1D-1 hybrid virus with neutralizing monoclonal antibodies to PV-2(L) N-AgI (22) and PV-1(M) N-AgI (23).
| Virus | Dilution of antibody neutralizing 100 TCID
50 |
|
|---|---|---|
| Antibody to
| ||
| PV-2(L) N-Ag I (mAb 433) | PV-1(M) N-Ag I (mAb 95) | |
| PV-1(M) | <1:4 | 1:32 |
| W1/2–1D-1 | >1:4096 | <1:4 |
| PV-2(L) | 1:1024 | <1:4 |
Tenfold dilutions of the W1/2–1D-1 hybrid virus were injected intracerebrally into 20-day-old mice, and the animals were observed for 21 days as described by LaMonica et al. (8). Median lethal dose (LD50) values were calculated (Table 3). In contrast to PV-1(M), to which mice are completely resistant [at 5 × 108 plaque-forming units (PFU) per inoculation], the W1/2–1D-1 hybrid virus is markedly neurovirulent with an LD50 of 1.4 × 106 PFU. Virus was recovered from the spinal cords of four mice that had become paralyzed at different times after inoculation with different levels of the hybrid virus. Nucleotide sequence analysis of viral RNA indicated that none of the neural isolates contained base changes in the N-AgI region.
Table 3.
Mouse neurovirulence of the W1/2–1D-1 hybrid virus relative to PV-1(M) and PV-2(L) viruses. LD50 is the amount of virus (PFU) required to cause paralysis or death in 50% of mice in 21 days. LD50 values for PV-2(L) are from (8) and for PV-1(M) are from (7).
| Virus | LD50 |
|---|---|
| W1/2–1D-1 | 1.4 × 106 |
| PV-2(L) | 5 × 103 to 1 × 105 |
| PV-1(M) | >5 × 108 |
The LD50 value of the antigenic hybrid is about ten times higher than was previously observed for transfection-derived PV-2(L) (Table 3). The reduced neurovirulence of the hybrid virus is not due to changes within N-AgI that might attenuate the virus (8), as demonstrated by sequence analysis of neural isolates. One possibility is that sites other than N-AgI of PV-2(L) are required for the full expression of mouse neurovirulence. However, a similar hybrid constructed by others was reported to be as neurovirulent as PV-2(L) in mice (21). Perhaps the PV-1(M) cDNA clone used in our experiments carries attenuation markers for mouse neurovirulence. We are currently searching for the reason for the reduced neurovirulence of the hybrid virus W1/2–1D-1 relative to PV- 2(L).
Our studies of mouse neurovirulence have led to the conclusion that an exchange of only six amino acids in the N-AgI loop converts PV-1(M) from an avirulent to a highly neurovirulent virus in mice. These data confirm our previous conclusion that the exposed loop formed by amino acids 95–105 in poliovirus is involved in mouse neurovirulence (8). We do not know the molecular basis for the change of host range and the concomitant induction of neurovirulence by the exchange of but a few amino acids in an exposed loop of the poliovirus capsid. Neither the cellular receptor for poliovirus, nor the precise region of the virion that interacts with the receptor has been identified. Rossmann et al. (12) proposed that a canyon surrounding the apex below the exposed loop serves as the receptor attachment site, a suggestion recently corroborated by genetic studies with human rhinovirus 14 (22). It is possible that attachment of poliovirus to the mouse cell receptor, whether or not it is similar to the primate cell receptor, involves amino acids of the N-AgI loop.
Studies of poliovirus neurovirulence in young mice have recently confirmed that the 5′ nontranslated region of poliovirus type 3 (Sabin) confers a strong attenuation phenotype to PV-2(L) (23). In this case, the development of disease is strongly influenced not by surface properties of the particle, but by a specific nucleotide sequence of the viral genome important for replication of the virus. In contrast, the biological properties of the hybrid virus we described are solely the result of surface properties of the virion and therefore are believed to influence steps of virus entry. This conclusion is based on the observation that a recombinant in which the PV-1(M) capsid was exchanged with that of PV-2(L) is as neurovirulent in mice as PV-2(L) and that PV-1(M) RNA replicates efficiently after transfection into cultured mouse cells (24). The W1/2–1D-1 hybrid virus, in addition to an altered antigenic phenotype, also expresses a change of host range. It is likely that multiple amino acid replacements in the highly exposed N-AgI loop have occurred during the evolution of the Picornaviridae. Our results suggest that such subtle changes of the virion capsid may in some cases have led to the emergence of new etiological agents with altered tissue tropism, perhaps explaining in part why human enteroviruses and rhinoviruses cause such a bewildering array of different disease syndromes in humans.
Acknowledgments
We thank A. Kameda for neutralization assays, P. Kissell for synthesis of oligonucleotides, C. Loughran for manuscript preparation, and O. Kew, P. Minor, K. Wiegers, and R. Dernick for antibodies. Supported by a fellowship of the World Health Organization (to X.-F.Y.), by PHS grants AI 20017 (to V.R.R.) and AI 15122 and CA 28146 (to E.W.), and by a Searle Scholars award and an I. T. Hirschl Career Scientist award (to V.R.R.).
Contributor Information
Michael G. Murray, Department of Microbiology, School of Medicine, State University of New York at Stony Brook, Stony Brook, NY 11794
Jonathan Bradley, Department of Microbiology, School of Medicine, State University of New York at Stony Brook, Stony Brook, NY 11794.
Xiao-Feng Yang, Department of Microbiology, School of Medicine, State University of New York at Stony Brook, Stony Brook, NY 11794.
Eckard Wimmer, Department of Microbiology, School of Medicine, State University of New York at Stony Brook, Stony Brook, NY 11794.
Eric G. Moss, Department of Microbiology, Columbia University College of Physicians and Surgeons, New York, NY 10032
Vincent R. Racaniello, Department of Microbiology, Columbia University College of Physicians and Surgeons, New York, NY 10032
REFERENCES AND NOTES
- 1.Nomoto A, Wimmer E. In: Molecular Basis of Virus Disease. Russell WC, Almond JW, editors. Vol. 40. Cambridge Univ. Press; New York: 1987. pp. 107–134. [Google Scholar]; Racaniello VR. Adv Virus Res. 1988;34:217. doi: 10.1016/s0065-3527(08)60519-9. [DOI] [PubMed] [Google Scholar]
- 2.Omata T, et al. J Virol. 1986;58:348. doi: 10.1128/jvi.58.2.348-358.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Westrop GD, et al. In: The Molecular Biology of the Positive Strand Viruses. Rowlands JD, Mayo MA, Mahy BWJ, editors. Academic Press; London: 1987. pp. 53–60. [Google Scholar]
- 4.Crowell RL, Landau BJ. In: Comprehensive Virology. Fraenkel-Conrat H, Wagner RR, editors. Vol. 18. Plenum; New York: 1983. pp. 1–42. [Google Scholar]
- 5.Armstrong C. Public Health Rep. 1939;54:2302. [Google Scholar]
- 6.Jubelt B, Gallez-Hawkins B, Narayan O, Johnson RT. J Neuropathol Exp Neurol. 1980;39:738. doi: 10.1097/00005072-198003000-00003. [DOI] [PubMed] [Google Scholar]
- 7.LaMonica N, Meriam C, Racaniello VR. J Virol. 1986;57:515. doi: 10.1128/jvi.57.2.515-525.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.LaMonica N, Kupsky W, Racaniello VR. Virology. 1987;161:429. doi: 10.1016/0042-6822(87)90136-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kitamura N, et al. Nature. 1981;291:547. doi: 10.1038/291547a0. [DOI] [PubMed] [Google Scholar]; Racaniello VR, Baltimore D. Proc Natl Acad Sci USA. 1981;78:4887. doi: 10.1073/pnas.78.8.4887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hogle JM, Chow M, Filman DJ. Science. 1985;229:1358. doi: 10.1126/science.2994218. [DOI] [PubMed] [Google Scholar]
- 11.Wimmer E, Emini EA, Diamond DC. In: Concepts in Viral Pathogenesis II. Notkins AL, Oldstone MBA, editors. Springer-Verlag; New York: 1986. pp. 159–173. [Google Scholar]; Minor PD, et al. In: Brinton MA, Rueckert RR, editors. Positive Strand RNA Viruses; UCLA Symposium; Keystone, CO. 1986; New York: Liss; 1987. pp. 539–553. [Google Scholar]
- 12.Rossmann MG, et al. Nature. 1985;317:145. doi: 10.1038/317145a0. [DOI] [PubMed] [Google Scholar]
- 13.Racaniello VR, Baltimore D. Science. 1980;214:916. doi: 10.1126/science.6272391. [DOI] [PubMed] [Google Scholar]; Semler BL, Dorner AJ, Wimmer E. Nucleic Acids Res. 1984;12:5123. doi: 10.1093/nar/12.12.5123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.van der Werf S, et al. Proc Natl Acad Sci USA. 1986;83:2330. doi: 10.1073/pnas.83.8.2330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kuhn RJ, et al. ibid. 1988;85:519. [Google Scholar]
- 16.Murray MG, Kuhn RJ, Wimmer E. Abstract, 7th International Congress of Virology, Edmonton, Alberta, Canada (1987) In: Lerner RA, Chanock RM, Brown F, Ginsberg H, editors. Vaccines ‘88. Cold Spring Harbor Laboratory; Cold Spring Harbor, NY: 1988. pp. 197–204. [Google Scholar]
- 17.Murray MG, et al. Proc Natl Acad Sci USA. 1988;85:3203. doi: 10.1073/pnas.85.9.3203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Burke KL, Dunn G, Ferguson M, Minor PD, Almond JW. Nature. 1988;332:81. doi: 10.1038/332081a0. [DOI] [PubMed] [Google Scholar]
- 19.Minor PD, Ferguson M, Evans DMA, Almond JW, Icenogle JP. J Gen Virol. 1986;67:1283. doi: 10.1099/0022-1317-67-7-1283. [DOI] [PubMed] [Google Scholar]
- 20.Wiegers KJ, Dernick R. Virology. 1987;157:248. doi: 10.1016/0042-6822(87)90337-0. [DOI] [PubMed] [Google Scholar]
- 21.Martin A, et al. EMBO J. in press. [Google Scholar]
- 22.Colonno RJ, et al. Proc Natl Acad Sci USA. in press. [Google Scholar]
- 23.LaMonica N, Almond JW, Racaniello VR. J Virol. 1987;61:2917. doi: 10.1128/jvi.61.9.2917-2920.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Detjen BM, Lucas J, Wimmer E. J Virol. 1978;27:582. doi: 10.1128/jvi.27.3.582-586.1978. [DOI] [PMC free article] [PubMed] [Google Scholar]


