Abstract
Background:
Predicting life expectancy is an important component of public health, in that, it may affect policy making in fields such as social security and medical care., To estimate the life expectancy and the average years of life lost (AYLL) of the human immunodeficiency virus (HIV)/acquired immunodeficiency syndrome (AIDS)-infected population, compared with that of the general population, and also to assess the impact of the CD4 count, risk factors of transmission, marital status, and employment status on life expectancy.
Material and Methods:
This study is a population-based cohort study. The sample consisted of HIV/AIDS-infected patients receiving care from 2001-2011. The patients were all adults (20-64 years) who were recruited from the Counseling Center of Behavioral Diseases. Life expectancy was measured based on an abridged life table, according to age-specific mortality rates and average years of life lost (AYLL) during the study period.
Results:
Forty-three of the 205 eligible patients died during 853 person-years follow-up. Compared to the general population, the life expectancy for patients with HIV infection at age 20 is about 36 years less. We have found that out a total of 1597 years of life lost during 2001-2011, compared to an overall AYLL for all HIV/AIDS, the deaths had occurred 36 years earlier than the life expectancy.
Conclusion:
Life expectancy in HIV/AIDS-infected patients is about 38 years less than that of the general population at the exact age of 20. The deaths caused by HIV/AIDS occurred about 36 years before what was expected in the general population at ages 20-64, and many of these years of life lost could be saved if the health care system was implemented against the risk factors of HIV/AIDS.
Keywords: Acquired Immunodeficiency Syndrome (AIDS), HIV, life expectancy, mortality
INTRODUCTION
Predicting life expectancy is an important component of public health, in that, it may affect policy making in fields such as social security and medical care.[1] A valid estimation of life expectancy after human immunodeficiency virus (HIV) diagnosis would be of great value, not only for public health policy-making, but also for the formulation of a clinical guiding principle.[2] Life expectancy and mortality are widely considered as important indicators of health in any population, and relation between HIV prevalence and life expectancy has been shown to be negative.[3] Despite the continuous advances in the fields of medical treatment and prevention, which have been made to improve survival among the infected, HIV remains a major threat to public health.[4] In highly infected countries, HIV/AIDS has reduced life expectancy by more than 20 years and has caused a reduction in production levels more than any other disease has ever done.[5] Clinical trials and observational studies show a significant reduction in mortality and morbidity in patients with HIV, ho have been treated with antiretroviral combination therapy (ARCT).[6,7,8,9,10,11] This reduction in mortality is clearer particularly in industrialized and high income countries where access to health services and antiretroviral treatment is readily available.[12]
Life expectancy in the population varies in different age, sex, and race groups and the fundamental differences between high and low income countries are reflected in the different rates of mortality in people with HIV; also the HIV epidemic patterns vary in different countries.[13] Although there has been a reduction in the number of deaths caused by the acquired immunodeficiency syndrome (AIDS) in both men and women, in all racial/ethnic groups, and all behavioral risk categories, the rate of reduction has not been similar, for example, reduction in the incidence of AIDS and deaths in black women were less than in white men.[4] For the seven sub-Sahara African countries, where the prevalence of HIV in the 15 to 49-year-old population is over 20%, the estimated reduced life expectancy from 2010 to 2015 is about 29.4 years (43.9%) and that is because of the occurrence of most additional deaths caused by AIDS in young age groups (between 25 and 49 years) in these countries.[14] Estimates of life expectancy are important for people who want to plan their lives better as well as for service providers and policy makers. Patients may use this information to make informed decisions about when to start antiretroviral therapy (ART), treatment of comorbidities, starting a family, pension provision or buying a house. Service providers require these estimates to plan the number of patients who will need treatment and the future costs of providing ART. Healthcare policy makers will be interested to show disparities in life expectancy between patients with different characteristics such as race or sex, or between those with early and late initiation of antiretroviral therapy.[13,15]
Therefore, the aims of this study were to estimate the overall and stratified health indicators by the CD4 count, risk factor for transmission, marital status, and employment status, during the calendar time of follow-up. The life expectancy of a person after HIV diagnosis was compared with that of a person in the general population with the same age, in the same calendar year, using the mortality data from the general population. The AYLL after HIV diagnosis was calculated using the mortality data from the general population.
MATERIALS AND METHODS
In this single-center, population-based retrospective cohort study, we collected HIV/AIDS surveillance data from the Counseling Center of Behavioral Diseases in Isfahan, Iran. This study, started in 2012, and analyzed the data on people with HIV/AIDS from 2001 through 2011. Only positive HIV-infected patients who had attended the Counseling Center of Behavioral Diseases in Isfahan, Iran, any time from 2001 were included in the study. Based on the data protection policy, all names were removed and replaced by a code derived from the date of the HIV/AIDS diagnosis of the patients. The patients included in this analysis were all HIV/AIDS positive (those with two positive tests, ELISA test and a Western blot test) who had referred to the counseling center in the study period. Records containing laboratory and demographic data such as CD4 count, hemoglobin, age, sex, marital status, education level, drug history (antiretroviral or non-antiretroviral and prophylactic), stage of the HIV infection and AIDS, based on the statement of the World Health Organization (WHO) stage IV HIV disease, Basic counseling information, vital signs, and high-risk behaviors for HIV acquisition were used. We estimated life expectancy using abridged life tables that were constructed from age-specific mortality rates, grouped in five-year age-bands, from the age of 20 to 65. These tables estimate the life expectancy of hypothetical cohorts of people with HIV at a given age by calculating the average additional years that will be lived by a person after that age, according to the cross-sectional age-specific mortality rates for all causes during the study period.[13] We calculated the overall health indicators stratified by CD4 count, risk factor for transmission, marital status, and employment status during the calendar time of follow-up[16] in the Isfahan, Iran, population using the data from 2001-2011. We then compared the life expectancy of a person after HIV diagnosis with that of a person in the general population having the same age, in the same calendar year, using the mortality data from the general population. To estimate the AYLL after HIV diagnosis, we multiplied the numbers of deaths with the numbers of years of expected remaining life according to the life tables in the study period. Overall, the YLL was expressed by Σdi × ei. Then we calculated the average years of life lost (AYLL), which we derived by dividing the total YLL by the number of deaths for each subset (age, CD4 count, hemoglobin, age, sex, marital status, and education level in the same calendar year) of the HIV/AIDS patients.[16] Analyses were done with Stata version 10, SPSS version 20, and Microsoft Excel 2008. A p-value of less than 0.05 was considered as a significant level.
RESULTS
The data set used for the current study contains information on 245 patients with HIV/AIDS in Isfahan, Iran, from 2001 to 2011, from which we excluded 40 (16%) patients from the study, who had incomplete information. Thus, the analyses were based on the data of 205 (84.0%) patients from the Counseling Center for Behavioral Diseases during the follow-up, and 43 deaths (21%) were recorded. Overall, 78% of the individuals were male [Table 1]. Twenty-nine percent had a CD4 count of <200 cells/mm3 after HIV diagnosis, 46% had a CD4 count between 200 and 499 cells/mm3, and 25% had a CD4 count of at least 500 cells/mm3 after diagnosis. The percentage of injection drug users (IDU) and patients having homosexual and/or heterosexual contact were 139/189 (73%) and 115/189 (60.8%), respectively. However, there were 16 patients with missing information about the mentioned risk factors, and 35% had homosexual and/or heterosexual contact and IDU. About 30% of the patients had a diagnosis of AIDS. About 853 person-years of follow-up were accumulated, with a median follow-up per participant of four (interquartile range 1.48-6.70) years. Table 2 shows the health indicators during the period of follow-up. During 2001-2011, for a hypothetical cohort of patients at age 20, with age-specific death rates, the proportion surviving till age 40 would have been 5%. During these years there was a corresponding shift in the distribution of measurements of CD4 counts. Table 3 shows the life expectancy for persons with HIV/AIDS during the study period, and for comparison, the life expectancy of the Isfahan population. Compared with the general Isfahan population, the life expectancy at age 20 was 36 years less for patients with HIV infection. Due to the limited number of HIV diagnoses among females, their life expectancy was not estimated.
Table 1.
Demographic characteristics of persons (20-64 years) with HIV/AIDS, Isfahan, Iran, 2001-2011
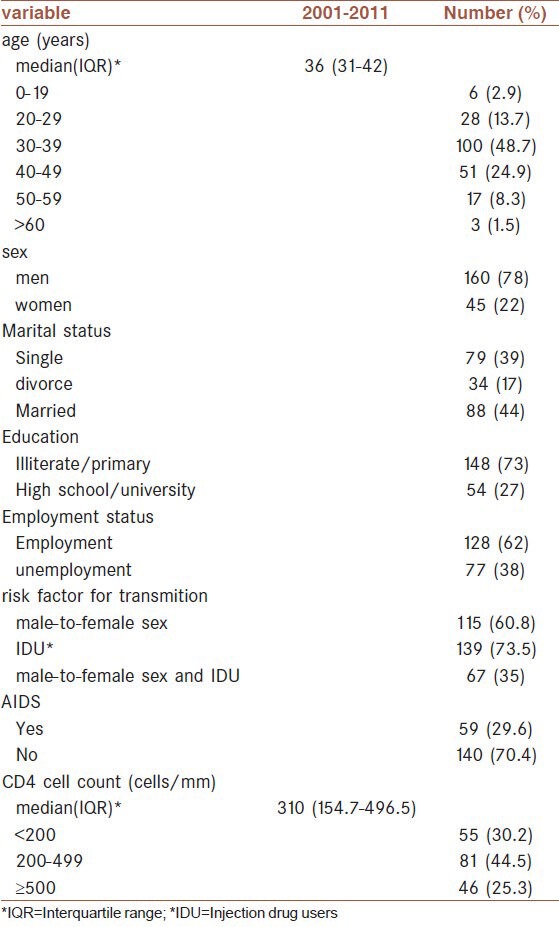
Table 2.
Health indicators for HIV/AIDS patients (20-64 years) stratified by demographic variables, Isfahan, Iran, 2001-2011
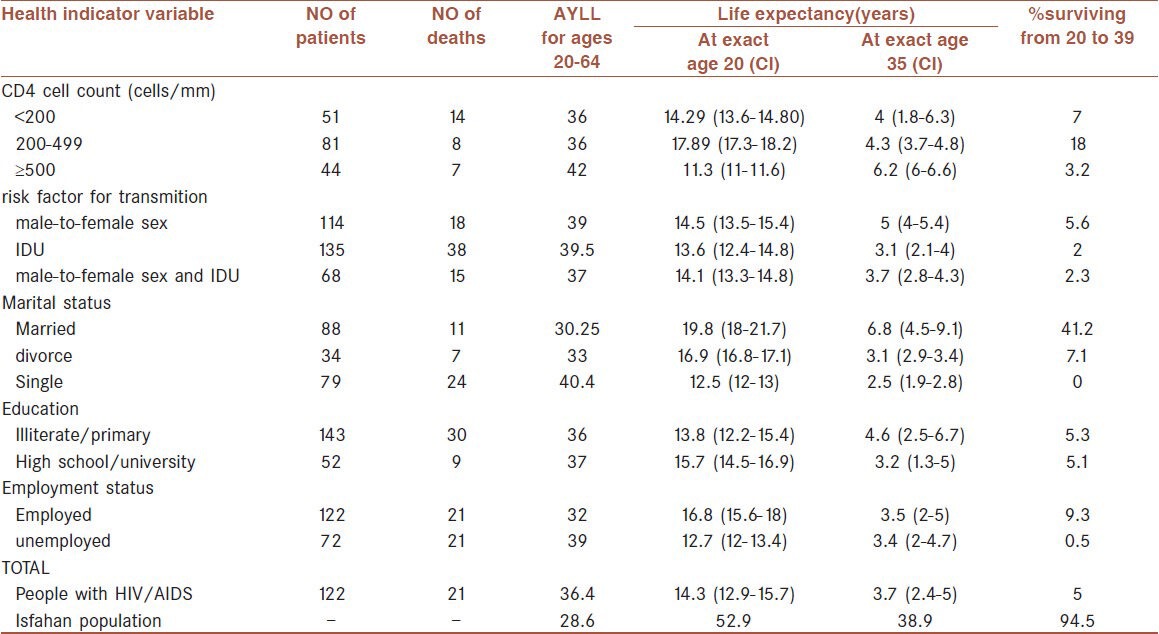
Table 3.
Life expectancy of persons with HIV/AIDS (20-64 years) by demographic characteristics, Iran, Isfahan, 2001-2011
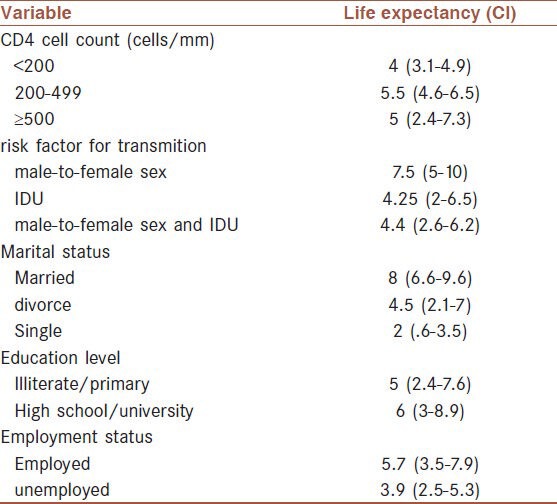
During the 11-year period, the category of male and female intercourse had the longest life expectancy among the transmission categories [7.5 (95% CI: 5 to10) years], but there was no significant difference in the life expectancy between the transmission categories IDU [4.25 (95% CI: 2 to 6.5) years] and male-to-female sex and IDU [4.4 (95% CI: 2.6.6 to 6.2) years] [Table 2]. Injection drug users had the worst life expectancy among all transmission categories, in the 11-year period.
On the basis of the CD4 count, persons with a CD4 count of < 200 cells/mm3 had the worst life expectancy among all CD4 count categories, and there was no significant difference in the life expectancy between CD4 count categories 200-499 cells/mm3 [5.5 (95% CI: 4.6 to 6.5) years] and ≥500 [5 (95% CI: 2.4 to 7.3) years] [Table 2]. Among all the patients, life expectancy was longer for married patients [8 (95% CI: 6.6 to 9.6) years] compared to single [2 (95% CI: .6 to 3.5) and divorced patients [4.5 (95% CI: 2.1 to 7) years]; and for employed patients [5.7 (95% CI: 3.5.6 to 7.9) years] when compared with unemployed patients [3.9 (95% CI: 2.5.6 to 5.3) years], but there was no significant difference in the life expectancy between the education level categories illiterate/primary [5 (95% CI: 2.4 to 7.6) years] and high school/university [6 (95% CI: 3 to 8.9) years] [Table 3].
Overall we observed a total number of 1597 years of life lost from 2001-2011, which were related to an overall AYLL for all HIV/AIDS deaths, 36 years earlier than life expectancy. If we compare this with the Isfahan population estimates shown in Table 3, the average years of life lost at age 64 is about 36, 36, and 42, for those with CD4 counts of < 200, 200-499, and > 500 cells/mm3, respectively [Figure 1]. Among the transmission categories, AYLL was 39, 39.5, and 37 for male-to-female sex, IDU, and male-to-female sex and IDU at age 64 years [Figure 2]. On the basis of marital status, married patients had the fewest AYLL compared to single and divorced patients at 64 years [30 years (married); 33 years (divorce); and 40 years (single)] [Figure 3], and in this period AYLL was 20 and 21 for the employed and unemployed patients [Figure 4].
Figure 1.
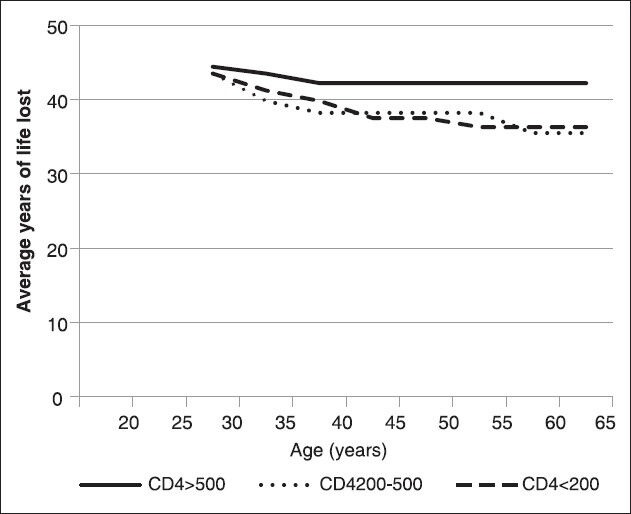
Estimated AYLL of HIV/AIDS patients by CD4 count (Isfahan, Iran, 2001-2011)
Figure 2.
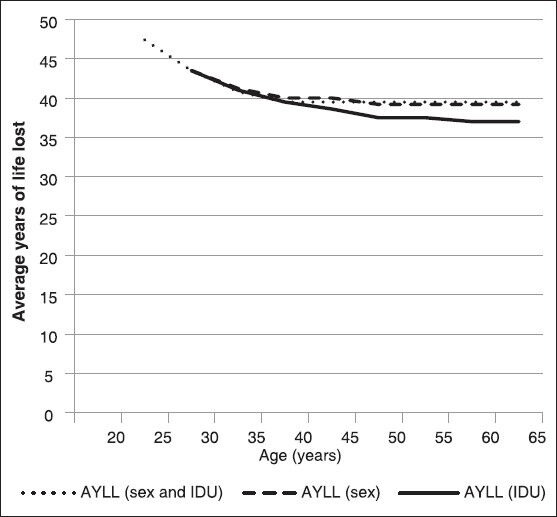
Estimated AYLL of HIV/AIDS patients by transmission category (Isfahan, Iran, 2001-2011)
Figure 3.
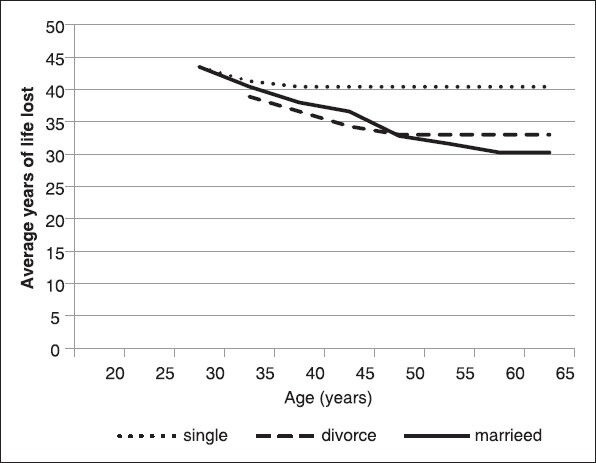
Estimated AYLL of HIV/AIDS patients by marital status (Isfahan, Iran, 2001-2011)
Figure 4.
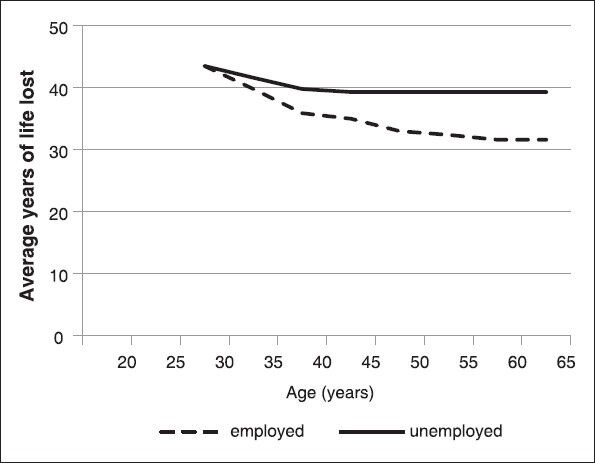
Estimated AYLL of HIV/AIDS patient by employment status (Isfahan, Iran, 2001-2011)
DISCUSSION
On the basis of the data from the Counseling Center for Behavioral Diseases, life expectancy after an HIV diagnosis was seen to be much lower than that of the Isfahan population. Life expectancy was worse for persons diagnosed at a later stage of disease (CD4 count of <200 cells/mm3) compared to all HIV-diagnosed persons. Patients who were diagnosed late or deferred treatment until their CD4 count fell to below 200 cells/mm3, were estimated at age 20 to have a life expectancy that was at least four years less than those who had a CD4 count of 200-499 cells/mm3. Furthermore, the clear impact of a low CD4 count on life expectancy implies that it is particularly important to diagnose HIV infection at an early stage. This would benefit both the patients and the healthcare systems, as the patient would experience increased life expectancy and the healthcare system a reduction in the costs associated with lower CD4 count at diagnosis, including hospital treatment or admission, or both. Late diagnoses may be due to poor access to testing or rapid progression of the disease. Persons who know that they are infected with HIV report fewer behavioral risk factors; therefore, prevention efforts aimed at increased testing and diagnosis should be augmented, and support for effective proven interventions should continue.
Injection drug users had a lower life expectancy in concurrence with their higher risk of death, which may be due not only to access to adherence obstacles, but also may be related to substance abuse and co-infections, in this population.[17,18] In addition to infection, the patient may also differ from the general population in behavioral risk factors and socioeconomic factors, both of which can impact life expectancy and AYLL.[16] HIV-infected persons that were single, and/or unemployed had higher rates than the general population. AYLL is a measure that reflects early death. It reflects how many years before what is anticipated the person dies. Unlike the mortality rate, which is generally higher in aged persons, AYLL gives greater weight to diseases that affect younger patients and less to those affecting the aged.[19] AYLL can be used in combination with other measures of HIV disease burden, for example, mortality and survival rates, to provide policy makers, clinicians, and patients with a more comprehensive picture of the burden to the HIV-infected individual. Programs intended to raise access to care for HIV-infected persons may increase the proportion of persons being treated and thus stretch survival.[16]
In the present study, we provided a picture of premature mortality by HIV/AIDS. In single patients, for instance, AYLL with HIV/AIDS was 40 years, while that of the divorced and married was 33 and 30 years, respectively, reflecting the fact that single patients are younger than other patients. In the CD4 cell count category, HIV/AIDS, for instance, tended to affect younger patients, who died more than 42 years earlier than expected. A shortening of AYLL may generally reflect an improvement in the effectiveness of treatment for HIV/AIDS. In the present study, the overall AYLL from HIV/AIDS in sex workers was similar to that in IDU (39 years vs. 39.5 years in this period). The postponement of these deaths may have benefited, at least in part, from improvements in medical health care or appropriate prevention. It is possible that public health management will benefit from the deliberation of these measures for premature mortality. Many of these premature deaths might have been avoided or postponed by proper involvement, such as primary prevention. Nevertheless, IDU remains the major risk factor for HIV/AIDS. Public health programs against IDU and sex workers contribute to reducing HIV/AIDS and may reduce the AYLL accordingly.
Direct comparison with previous estimates of life expectancy compared with the general population was done, and we found that the previous studies reported AYLL to be significant.[17] Furthermore, at older ages, the AYLL is lower. For example, Harrison et al.[16] has reported that at the age of 60 years, AYLL is 11 years and at age 70 it is eight years. Our populations are HIV/AIDS patients in care and estimates based on patients in care likely overestimate (more than ours do) life expectancy and survival in the general HIV-infected population,[13,16,17] but other studies that compared an HIV-infected population with the general population have reported better life expectancy and survival[13,16,20,21] than we have reported here. This reduction may be due to late diagnosis and treatment initiation among them, or factors related to the therapy adherence.[16]
In summary, deaths due to HIV/AIDS occurred about 36 years prior to that expected in the general population at age 20-64 years, and many of these years of life lost might have been saved if programs against risk factors of HIV/AIDS were implemented. To our knowledge, these estimates have not been previously provided in Iran. These results can direct clinician announcement to patients about their life expectancies after HIV diagnosis and policy makers to estimate expenses and allocate funds. They also can be helpful for patients planning and establishing general expectations.
ACKNOWLEDGMENT
The authors would like to thank the Deputy Head of Research at the School of Health, Vice-Chancellor of Research at the Isfahan University of Medical Sciences for grant number 391267, Dr. Namdari from the Center of Behavioral Diseases in the Ministry of Health, Treatment, and Medical Education, and also the staff in Counseling Center for Behavioral Diseases in Isfahan.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Olshansky SJ, Passaro DJ, Hershow RC, Layden J, Carnes BA, Brody J, et al. A Potential Decline in Life Expectancy in the United States in the 21st Century. N Engl J Med. 2005;352:1138–45. doi: 10.1056/NEJMsr043743. [DOI] [PubMed] [Google Scholar]
- 2.Welch HG, Albertsen PC, Nease RF, Bubolz TA, Wasson JH. Estimating treatment benefits for the elderly: The effect of competing risks. Ann Intern Med. 1996;124:577–84. doi: 10.7326/0003-4819-124-6-199603150-00007. [DOI] [PubMed] [Google Scholar]
- 3.McGuire A, Barer J, Montaner J, Hogg R. There and back again: The impact of adult HIV prevalence on national life expectancies. HIV Med. 2005;6:57–8. doi: 10.1111/j.1468-1293.2005.00266.x. [DOI] [PubMed] [Google Scholar]
- 4.Fleming P, Wortley P, Karon J, DeCock K, Janssen R. Tracking the HIV epidemic: Current issues, future challenges. Am J Public Health. 2000;90:1037–41. doi: 10.2105/ajph.90.7.1037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organization; 2009. HIV/AIDS. JUNPo. 2008 Report on the global AIDS epidemic. [Google Scholar]
- 6.Chiasson MA, Berenson L, Li W, Schwartz S, Singh T, Forlenza S, et al. Declining HIV/AIDS mortality in New York city. J Acquir Immune Defic Syndr. 1999;21:59–64. doi: 10.1097/00126334-199905010-00008. [DOI] [PubMed] [Google Scholar]
- 7.Detels R, Muñoz A, McFarlane G, Kingsley LA, Margolick JB, Giorgi J, et al. Effectiveness of potent antiretroviral therapy on time to AIDS and death in men with known HIV infection duration. JAMA. 1998;280:1497–503. doi: 10.1001/jama.280.17.1497. [DOI] [PubMed] [Google Scholar]
- 8.Hogg RS, Heath KV, Yip B, Craib KJ, O’Shaughnessy MV, Schechter MT, et al. Improved survival among HIV-infected individuals following initiation of antiretroviral therapy. JAMA. 1998;279:450–4. doi: 10.1001/jama.279.6.450. [DOI] [PubMed] [Google Scholar]
- 9.Mocroft A, Vella S, Benfield T, Chiesi A, Miller V, Gargalianos P, et al. Changing patterns of mortality across Europe in patients infected with HIV-1. Lancet. 1998;352:1725–30. doi: 10.1016/s0140-6736(98)03201-2. [DOI] [PubMed] [Google Scholar]
- 10.Moore RD, Chaisson RE. Natural history of HIV infection in the era of combination antiretroviral therapy. AIDS. 1999;13:1933–42. doi: 10.1097/00002030-199910010-00017. [DOI] [PubMed] [Google Scholar]
- 11.Wong KH, Chan KC, Lee SS. Delayed progression to death and to AIDS in a Hong Kong cohort of patients with advanced HIV type 1 disease during the era of highly active antiretroviral therapy. Clin Infect Dis. 2004;39:853–60. doi: 10.1086/423183. [DOI] [PubMed] [Google Scholar]
- 12.Prince JD, Akincigil A, Kalay E, Walkup JT, Hoover DR, Lucas J, et al. Psychiatric rehospitalization among elderly persons in the United States. Psychiatr Serv. 2008;59:1038–45. doi: 10.1176/ps.2008.59.9.1038. [DOI] [PubMed] [Google Scholar]
- 13.May M, Gompels M, Delpech V, Porter K, Post F, Johnson M, et al. Impact of late diagnosis and treatment on life expectancy in people with HIV-1: UK Collaborative HIV Cohort (UK CHIC) Study. BMJ. 2011;343:d6016. doi: 10.1136/bmj.d6016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Neumayer E. HIV/AIDS and its impact on convergence in life expectancy, infant and child survival rates. HEW. 2004 [Google Scholar]
- 15.Cooper DA. Life and death in the cART era. Lancet. 2008;372:266–7. doi: 10.1016/S0140-6736(08)61086-7. [DOI] [PubMed] [Google Scholar]
- 16.Harrison KM, Song R, Zhang X. Life expectancy after HIV diagnosis based on national HIV surveillance data from 25 states, United States. J Acquir Immune Defic Syndr. 2010;53:124–30. doi: 10.1097/QAI.0b013e3181b563e7. [DOI] [PubMed] [Google Scholar]
- 17.Bhaskaran K, Hamouda O, Sannes M, Boufassa F, Johnson AM, Lambert PC, et al. Changes in the risk of death after HIV seroconversion compared with mortality in the general population. JAMA. 2008;300:51–9. doi: 10.1001/jama.300.1.51. [DOI] [PubMed] [Google Scholar]
- 18.Chander G, Himelhoch S, Moore RD. Substance abuse and psychiatric disorders in HIV-positive patients: Epidemiology and impact on antiretroviral therapy. Drugs. 2006;66:769–89. doi: 10.2165/00003495-200666060-00004. [DOI] [PubMed] [Google Scholar]
- 19.Ibayashi H, Pham TM, Fujino Y, Kubo T, Ozasa K, Matsuda S, et al. Estimation of premature mortality from oral cancer in Japan, 1995 and 2005. Cancer Epidemiol. 2011;35:342–4. doi: 10.1016/j.canep.2011.01.010. [DOI] [PubMed] [Google Scholar]
- 20.Bhaskaran K, Hamouda O, Sannes M, Boufassa F, Johnson AM, Lambert PC, et al. Changes in the risk of death after HIV seroconversion compared with mortality in the general population. JAMA. 2008;300:51–9. doi: 10.1001/jama.300.1.51. [DOI] [PubMed] [Google Scholar]
- 21.Jaggy C, von Overbeck J, Ledergerber B, Schwarz C, Egger M, Rickenbach M, et al. Mortality in the Swiss HIV Cohort Study (SHCS) and the Swiss general population. Lancet. 2003;362:877–8. doi: 10.1016/S0140-6736(03)14307-3. [DOI] [PubMed] [Google Scholar]


