Abstract
Context
Prenatal folic acid supplements reduce the risk of neural tube defects in children, but it has not been determined whether they protect against other neurodevelopmental disorders.
Objective
To examine the association between maternal use of prenatal folic acid supplements and the subsequent risk of autistic disorder in children.
Design, Setting, and Patients
The study sample of 85,176 was derived from the population-based, prospective Norwegian Mother and Child Cohort Study (MoBa). The children were born in 2002–08. By the end of follow-up on March 31st, 2012, the age range was 3.3–10.2 years and the mean age 6.4 years. The exposure of primary interest was use of folic acid from 4 weeks before to 8 weeks after the start of pregnancy. The start of pregnancy was defined as the first day of the last menstrual period before conception. Relative risks of ASD were estimated by odds ratios (ORs) with 95% confidence intervals (CIs) in a logistic regression analysis. Analyses were adjusted for maternal education level, year of birth, and parity.
Main Outcome Measure
Specialist-confirmed diagnosis of autistic disorder.
Results
To date, 114 children in the study sample have been diagnosed with autistic disorder. In children whose mothers took folic acid, 0.10% (64/61,042) had autistic disorder, compared with 0.21% (50/24,134) in those unexposed to folic acid. The adjusted OR for autistic disorder in children of folic acid users was 0.61 (95% CI, 0.41–0.90). Similar analyses for prenatal fish oil supplements showed no such association with autistic disorder, even though fish oil use was associated with the same maternal characteristics as folic acid use.
Conclusion
Prenatal folic acid supplements around the time of conception were associated with a lower risk of autistic disorder in the MoBa cohort.
INTRODUCTION
Supplementation with folic acid around the time of conception reduces the risk of neural tube defects in children1–7. This protective effect has led to mandatory fortification of flour with folic acid in several countries8, and it is generally recommended that women planning to become pregnant take a daily supplement of folic acid from one month before conception8,9.
There is also evidence that maternal folic acid supplementation during pregnancy may be associated with reduced risk of other neurodevelopmental disorders in children. A recent study of 38,954 children in the Norwegian Mother and Child Cohort Study (MoBa) found that maternal intake of folic acid supplements from 4 weeks before to 8 weeks after the start of pregnancy was associated with a lower risk of severe language delay at 3 years of age10. A case-control study of autism spectrum disorder (ASD) from California showed that maternal intake of folic acid and prenatal vitamins during the 3 months prior to pregnancy and the first month of pregnancy was associated with a lower risk of ASD in the offspring, and complementary genetic analyses indicated that the association was modified by gene variants that determine the ability to utilize available folate11,12.
Although ethical considerations preclude placebo-controlled randomized trials that eliminate folic acid, observational studies of mothers who do and do not use supplements may be informative. Here we report the results of such an analysis in MoBa, wherein we investigated the association between the use of maternal folic acid supplements ahead of and in early pregnancy and the subsequent risk of autistic disorder in the offspring.
METHODS
Study Population
The MoBa13 cohort is nationwide and includes 109,000 children born from 1999 to 2009. Mothers were recruited at ultrasound examinations around week 18 of gestation. Cases of ASD in the cohort are identified by a sub-study of autism, the Autism Birth Cohort Study14. The analyses in this study reflect data collected and processed by March 31st, 2012. Participation in MoBa and the Autism Birth Cohort study is based on written informed consent. Both studies are approved by the Regional Committee of Medical Research Ethics for South-Eastern Norway.
Measures of ASD
Cases of ASD are identified through: 1) questionnaire screening of MoBa participants at the ages of 36 months, 5 years and 7 years, 2) professional and parental referrals of participants suspected of having ASD, and 3) linkages to the Norwegian Patient Registry. Referrals are elicited through annual newsletters to MoBa participants and information on the Norwegian Institute of Public Health website. The Norwegian Patient Registry collects data on diagnoses from all hospitals and outpatient clinics in Norway, beginning in the year 2008, thereby capturing all children diagnosed with ASD by Norwegian health services.
When a child with ASD or potential ASD is detected through any of the mechanisms described above, he/she is invited to participate in a clinical assessment that includes the research-standard instruments for diagnosis of ASD, the Autism Diagnostic Interview – Revised (ADI-R)15 and the Autism Diagnostic Observation Schedule (ADOS)16, which have proven high reliability and validity in making diagnoses of ASD in children. Assessments are conducted without knowledge of previous questionnaire responses. Diagnostic conclusions are best-estimate clinical diagnoses derived from test and interview results and from information collected from parents and teachers. Diagnoses are based on DSM-IV criteria, and the case definition includes 299.00 Autistic Disorder, 299.80 Asperger’s Syndrome, and 299.80 Pervasive Developmental Disorder Not Otherwise Specified (PDD-NOS).
The registry contains ICD-10 codes determined by Norwegian specialist health services, and the ASD case definition of the Autism Birth Cohort study includes F84.0 Childhood Autism, F84.1 Atypical Autism, F84.5 Asperger’s Syndrome, F84.8 Other Pervasive Developmental Disorder, and F84.9 Pervasive Developmental Disorder, Unspecified. In this paper, we have used the term autistic disorder for F84.0 and PDD-NOS for F84.1, F84.8, and F84.9.
Measures of Folic Acid Use and Dietary Folate Intake
Since 1998, the Norwegian Directorate of Health has recommended that all women attempting to become pregnant should take a supplement of 400 μg folic acid per day from one month before conception through the first trimester. Folic acid supplements are available over the counter in Norway. There are also multivitamin supplements with folic acid available, but at the time of recruitment to MoBa, all such supplements contained less than 400 μg of folic acid.
In MoBa, detailed information about the mothers’ supplement intake before conception and in early pregnancy was obtained through questionnaire report at week 18 of gestation. No foods were fortified with folic acid at the time when participants were recruited; synthetic supplements thus represented the only source of folate apart from the ordinary diet for the pregnant women. The women were asked to record their intake of vitamins, minerals and other supplements according to the ingredient lists on the supplement containers, within 4-week intervals from before the start of pregnancy. They were not asked to specify the exact amounts, so if folic acid was only taken as part of a multivitamin supplement, the daily dose would be lower than 400 μg.
Additional information about supplement use and dietary intake in mid-pregnancy was obtained through a food-frequency questionnaire completed in week 22. In this questionnaire, women were asked to write the name of supplements that they were currently taking (in week 22), and exact amounts of vitamins and minerals were calculated on the basis of this information. The food-frequency questionnaire has been described in a previous paper17 and validated through blood samples and 4-day food records from a subsample of the cohort18.
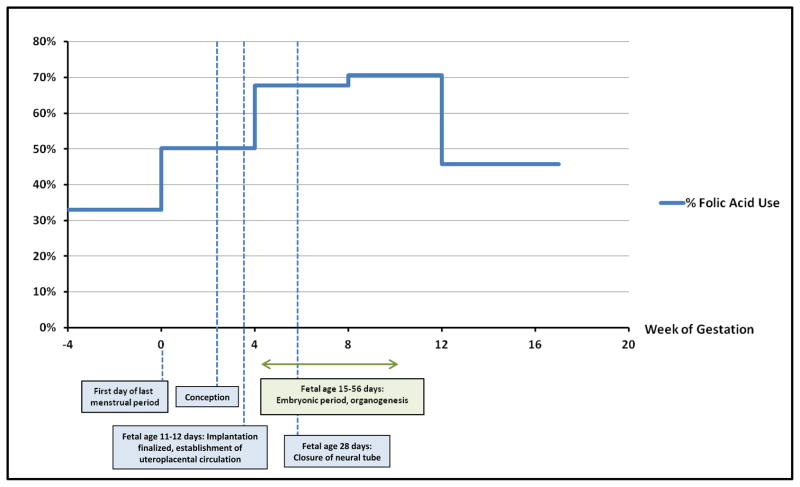
Measures of Timing
For our primary analyses, we examined an interval from 4 weeks before to 8 weeks after the start of pregnancy. The start of pregnancy was defined as the first day of the last menstrual period before conception, in keeping with the standard definition used in the follow-up of pregnant women in Norway. Children of mothers who used folic acid supplements during the entire or parts of the exposure interval were compared to children whose mothers did not use folic acid supplements during the interval. The exposure interval was chosen on the basis of an a priori hypothesis that the effect of folic acid on the development of the central nervous system is most prominent in this period, and it also corresponds to the interval used in the previous study of language delay10. The interval covers or precedes events of critical importance to the fetal brain, such as the closure of the neural tube 28 days after conception (gestational week 6) and the embryonic period with the development of the basic brain structures 15–56 days after conception (gestational week 5–10)19.
Potential Confounders
We explored a number of factors that might influence a potential association between supplement use and ASD risk: parental education, parental age, whether the pregnancy was planned, maternal smoking during pregnancy, maternal body mass index (weight in kilograms divided by height in meters squared), parity, and year of birth.
Statistical Analyses
Analyses were done using SPSS version 19.0 (SPSS Inc., Chicago, Illinois). Odds ratios (ORs), with 95% confidence intervals (CIs), were estimated from logistic regression models. The adjusted models included adjustment for year of birth, maternal education level, and parity, as these were the only covariates that had any influence on the OR estimates. We estimated the power of these analyses for autistic disorder, which was the ASD subtype with the highest number of diagnosed cases in the study sample. The power calculations were based on the observed distributions of the outcome and the exposure, i.e., an overall prevalence of 0.13% of autistic disorder and a proportion of 68% of the study sample exposed to folic acid within the exposure interval. The type I error probability was set at α=0.05 (2-sided). Under these conditions we had a power of 93% to detect an OR of 0.50, 73% for OR 0.60, 45% for OR 0.70, and 18% for OR 0.80.
We conducted a secondary analysis of the association between maternal use of fish oil supplements and the risk of ASD, in order to investigate whether the associations were specific to folic acid or similar across different types of supplements. If they were similar, the associations would more likely be attributable to health-conscious maternal behaviors in general and not the supplements per se20. We also examined the association between folic acid use in week 22 of pregnancy and subsequent risk of ASD, to evaluate whether any associations, if present, were similar in early pregnancy and mid-pregnancy.
The study did not have sufficient power for subgroup analyses, but we have included results of some exploratory analyses for the autistic disorder subtype, as they provide valuable additional information and clues to interactions that could be tested in future studies. We explored the following:
the timing of initiation of folic acid supplementation
maternal use of other vitamins/minerals from 4 weeks before to 8 weeks after the start of pregnancy
maternal total daily intake of folate in week 22 (diet and supplements combined, adjusted for dietary folate equivalents)
stratification of autistic disorder cases by language level at 36 months
stratification of the study sample by year of birth (2002–04 vs. 2005–08)
RESULTS
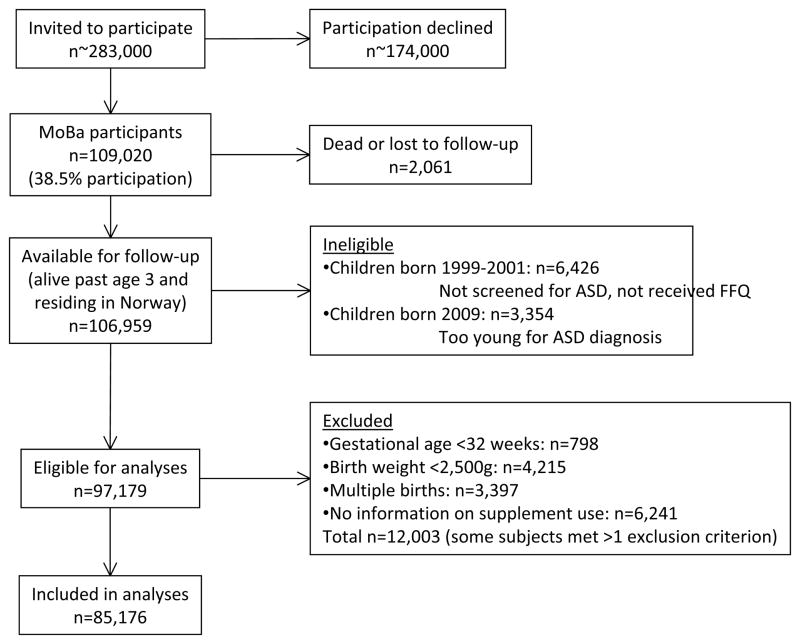
The derivation of the study sample is described in Figure 1. A total of 97,179 cohort participants were eligible for the analyses. To isolate folic acid exposure from other exposure reported to increase the risk of ASD, we excluded children with gestational age <32 weeks at birth, children with birth weight <2,500 g, and multiple births. We also excluded children for whom we did not have data on maternal supplement use before conception and in early pregnancy, and children whose mothers reported supplement use but had not specified the type and duration. In total, 12,003 children were excluded, for one or more reasons. The final study sample included 85,176 children. At the end of follow-up, the age range was 3.3–10.2 years and the mean age 6.4 years.
Figure 1.
Derivation of the Study Sample
A total of 270 children (0.32%) in the study sample have been diagnosed with ASD: 114 (0.13%) with autistic disorder, 56 (0.07%) with Asperger’s syndrome, and 100 (0.12%) with PDD-NOS. The distribution of ASD cases by year of birth is shown in eTable 1 of the online supplement. Of the ASD cases, 135 (50.0%) had been clinically assessed through the ABC study. The remaining 135 had specialist-confirmed diagnoses of ASD recorded in the Norwegian Patient Registry. Registry diagnoses have a high validity for ASD as a whole: of the 39 children assessed in the ABC study after being detected through the registry, 38 were found to meet DSM-IV criteria for ASD, generating a positive predictive value (PPV) of 97% (95% CI, 87–100%). PPV estimates are lower for the individual ASD subtype diagnoses: 80% (12/15) for autistic disorder (95% CI, 52–96%), 38% (5/13) for Asperger’s syndrome (95% CI, 14–68%), and 73% (8/11) for PDD-NOS (95% CI, 39–94%). PPV estimates for the subtype diagnoses are preliminary, as the number of cases in each group is still low.
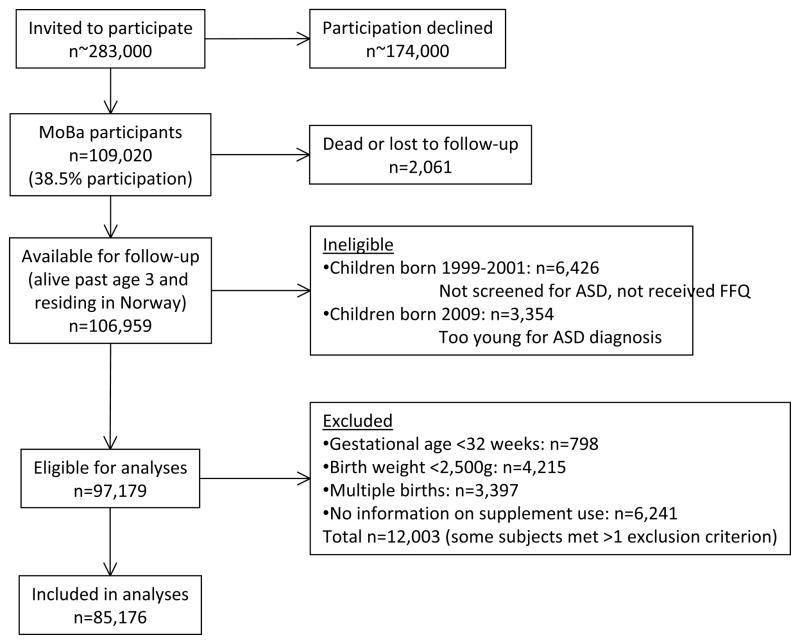
The proportions of mothers reporting folic acid use are shown in Figure 2. In the first interval (weeks 4 to 1 before the start of pregnancy), 32.9% of mothers took folic acid. The proportion increased to 70.7% in week 9–12 and then reverted to 45.8% in week 13–17. The distribution of folic acid use across categories of parent and child characteristics is shown in Table 1. Women who used folic acid within the exposure interval (4 weeks before to 8 weeks after the start of pregnancy) were more likely to have college or university level education, to have planned the pregnancy, to be non-smokers, to have pre-pregnancy BMI below 25, and to be first-time mothers. Folic acid use increased substantially by year of birth, from 43.2% in 2002 to 83.7% in 2008.
Figure 2.
Folic Acid Supplement Use by Pregnancy Interval
Table 1.
Parent and Child Characteristics by Maternal Folic Acid Use a
| Supplement Use Week (−4) to 8 | ||||||
|---|---|---|---|---|---|---|
|
| ||||||
| Total Study Sample (n=85,176) | No Folic Acid (n=24,134) | Use of Folic Acid (n=61,042) | ||||
|
| ||||||
| n | % | n | % | n | % | |
| Maternal education, y | ||||||
| < 12 | 6,264 | 7.4 % | 3,274 | 13.6 % | 2,990 | 4.9 % |
| 12 | 22,616 | 26.6 % | 8,319 | 34.5 % | 14,297 | 23.4 % |
| 13 – 16 | 34,641 | 40.7 % | 8,298 | 34.4 % | 26,343 | 43.2 % |
| >= 17 | 19,910 | 23.4 % | 3,611 | 15.0 % | 16,299 | 26.7 % |
| Missing data | 1,745 | 2.0 % | 632 | 2.6 % | 1,113 | 1.8 % |
|
| ||||||
| Paternal education, y | ||||||
| < 12 | 9,067 | 10.6 % | 3,915 | 16.2 % | 5,152 | 8.4 % |
| 12 | 32,161 | 37.8 % | 10,434 | 43.2 % | 21,727 | 35.6 % |
| 13 – 16 | 22,476 | 26.4 % | 5,248 | 21.7 % | 17,228 | 28.2 % |
| >= 17 | 18,835 | 22.1 % | 3,541 | 14.7 % | 15,294 | 25.1 % |
| Missing data | 2,637 | 3.1 % | 996 | 4.1 % | 1,641 | 2.7 % |
|
| ||||||
| Maternal age, y | ||||||
| < 25 | 9,384 | 11.0 % | 3,785 | 15.7 % | 5,599 | 9.2 % |
| 25 – 29 | 28,107 | 33.0 % | 7,450 | 30.9 % | 20,657 | 33.8 % |
| 30 – 34 | 32,975 | 38.7 % | 8,551 | 35.4 % | 24,424 | 40.0 % |
| >= 35 | 14,710 | 17.3 % | 4,348 | 18.0 % | 10,362 | 17.0 % |
|
| ||||||
| Paternal age, y | ||||||
| < 25 | 4,041 | 4.7 % | 1,709 | 7.1 % | 2,332 | 3.8 % |
| 25 – 29 | 19,167 | 22.5 % | 5,331 | 22.1 % | 13,836 | 22.7 % |
| 30 – 34 | 33,101 | 38.9 % | 8,629 | 35.8 % | 24,472 | 40.1 % |
| 35 – 39 | 20,231 | 23.8 % | 5,644 | 23.4 % | 14,587 | 23.9 % |
| >= 40 | 8,411 | 9.9 % | 2,734 | 11.3 % | 5,677 | 9.3 % |
| Missing data | 225 | 0.3 % | 87 | 0.4 % | 138 | 0.2 % |
|
| ||||||
| Planned pregnancy | ||||||
| Yes | 68,094 | 79.9 % | 17,394 | 72.1 % | 50,700 | 83.1 % |
| No | 16,061 | 18.9 % | 6,351 | 26.3 % | 9,710 | 15.9 % |
| Missing data | 1,021 | 1.2 % | 389 | 1.6 % | 632 | 1.0 % |
|
| ||||||
| Maternal smoking b | ||||||
| No | 77,845 | 91.4 % | 20,641 | 85.5 % | 57,204 | 93.7 % |
| Yes | 6,740 | 7.9 % | 3,254 | 13.5 % | 3,486 | 5.7 % |
| Missing data | 591 | 0.7 % | 239 | 1.0 % | 352 | 0.6 % |
|
| ||||||
| Maternal pre-pregnancy BMI | ||||||
| < 25 | 56,614 | 66.5 % | 15,150 | 62.8 % | 41,464 | 67.9 % |
| 25 – 29 | 18,332 | 21.5 % | 5,441 | 22.5 % | 12,891 | 21.1 % |
| 30 – 34 | 5,830 | 6.8 % | 1,951 | 8.1 % | 3,879 | 6.4 % |
| >= 35 | 2,158 | 2.5 % | 719 | 3.0 % | 1,439 | 2.4 % |
| Missing data | 2,242 | 2.6 % | 873 | 3.6 % | 1,369 | 2.2 % |
|
| ||||||
|
| ||||||
| Parity c | ||||||
| 0 | 37,946 | 44.6 % | 9,266 | 38.4 % | 28,680 | 47.0 % |
| 1 | 30,674 | 36.0 % | 8,493 | 35.2 % | 22,181 | 36.3 % |
| >= 2 | 16,556 | 19.4 % | 6,375 | 26.4 % | 10,181 | 16.7 % |
| Year of birth | n | Column % | n | Row % | n | Row % |
|---|---|---|---|---|---|---|
| 2002 | 7,377 | 8.7 % | 4,187 | 56.8 % | 3,190 | 43.2 % |
| 2003 | 10,858 | 12.7 % | 5,030 | 46.3 % | 5,828 | 53.7 % |
| 2004 | 11,882 | 13.9 % | 3,682 | 31.0 % | 8,200 | 69.0 % |
| 2005 | 13,711 | 16.1 % | 3,504 | 25.6 % | 10,207 | 74.4 % |
| 2006 | 15,364 | 18.0 % | 3,246 | 21.1 % | 12,118 | 78.9 % |
| 2007 | 14,140 | 16.6 % | 2,552 | 18.0 % | 11,588 | 82.0 % |
| 2008 | 11,844 | 13.9 % | 1,933 | 16.3 % | 9,911 | 83.7 % |
p<0.001 for all variables, 2-sided chi-square test for independence.
Maternal smoking, daily or occasionally, during pregnancy.
Parity including previous miscarriage or abortion after week 22 of gestation.
Women who took folic acid in early pregnancy had a higher response rate to the screening questionnaire completed when the children were 36 months. For the study sample overall, the response rate was 62% in folic acid users and 55% in non-users. For children born in 2005–08, i.e., the youngest children, the difference was somewhat larger, with a response rate of 61% in folic acid users and 50% in non-users. Consequently, ASD children born to women who used folic acid may have had a higher probability of being diagnosed at an early age.
Results of the logistic regression analysis for autistic disorder are displayed in Table 2. There was an inverse association between folic acid use and the subsequent risk of autistic disorder. In children whose mothers took folic acid, 0.10% (64/61,042) had autistic disorder, compared with 0.21% (50/24,134) in children whose mothers did not take folic acid. The adjusted OR of autistic disorder was 0.61 (95% CI, 0.41–0.90) in children of folic acid users.
Table 2.
Risk of Autistic Disorder According to Maternal Folic Acid Use
| Total | Autistic Disorder | Unadjusted | Adjusted a | |||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| n | % | n | % | OR | 95% CI | OR | 95% CI | |
| No folic acid | 24,134 | 28.3 % | 50 | 0.21 % | 1 (ref) | --- | 1 (ref) | --- |
| Use of folic acid | 61,042 | 71.7 % | 64 | 0.10 % | 0.51 | 0.35 – 0.73 | 0.61 | 0.41 – 0.90 |
Adjusted for year of birth, maternal education level, and parity. For maternal education, missing data was included as a separate category in the logistic regression model.
The use of fish oil supplements followed similar patterns as folic acid use in the study sample: it was associated with the same parental characteristics (eTable 2), it increased throughout the period of recruitment to the cohort (eTable 2), and it increased from before pregnancy through the first trimester (eFigure 1). Despite these similarities, there was no association between fish oil supplement use and autistic disorder risk, as shown in Table 3. The adjusted OR of autistic disorder was 1.29 (95% CI, 0.88–1.89) in children of mothers who used fish oil supplements.
Table 3.
Secondary Analyses
| Total | Autistic Disorder | Unadjusted | Adjusted a | |||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| n | % | n | % | OR | 95% CI | OR | 95% CI | |
| Fish oil use in week (−4) to 8 b | ||||||||
| No fish oil | 46,314 | 54.4 % | 60 | 0.13 % | 1 (ref) | --- | 1 (ref) | --- |
| Use of fish oil | 38,862 | 45.6 % | 54 | 0.14 % | 1.07 | 0.74 – 1.55 | 1.29 | 0.88 – 1.89 |
|
| ||||||||
| Folic acid use in week 22 c | ||||||||
| No folic acid | 32,064 | 40.4 % | 42 | 0.13 % | 1 (ref) | --- | 1 (ref) | --- |
| 1–399 μg/day | 20,872 | 26.3 % | 26 | 0.12 % | 0.95 | 0.58 – 1.55 | 1.02 | 0.62 – 1.67 |
| ≥ 400 μg/day | 26,467 | 33.3 % | 31 | 0.12 % | 0.89 | 0.56 – 1.42 | 0.96 | 0.60 – 1.55 |
Adjusted for year of birth, maternal education level, and parity. For maternal education, missing data was included as a separate category in the logistic regression model.
Fish oil includes cod liver oil and omega-3 fatty acid supplements.
Analyses includes only responders to the food-frequency questionnaire in week 22 (n=79,403). The food-frequency questionnaire included report of brand names of supplements, enabling exact calculations of the amounts of folic acid ingested per day.
The inverse association found for folic acid use in early pregnancy was absent for folic acid use in mid-pregnancy: the adjusted OR for autistic disorder was 0.96 (95% CI, 0.60–1.55) for those taking ≥400 μg per day in week 22, and 1.02 (95% CI, 0.62–1.67) for those taking less than 400 μg per day at that time.
For Asperger’s syndrome and PDD-NOS, we restricted the analyses to birth years with a cumulative incidence of 0.08% or higher (higher than the lowest level observed for autistic disorder): 2002–04 for Asperger’s syndrome (n=30,117 including 48 cases) and 2002–06 for PDD-NOS (n=59,152 including 91 cases). Our power to detect an OR of similar magnitude to that found for autistic disorder (OR=0.61) was limited: 36% for Asperger’s syndrome, and 61% for PDD-NOS. For Asperger’s syndrome, the proportion of diagnosed cases was 0.12% (21/17,218) in children of folic acid users and 0.21% (27/12,899) in children of non-users, generating an adjusted OR of 0.65 (95% CI, 0.36–1.16). For PDD-NOS, the proportion was 0.15% (58/39,543) in children of folic acid users and 0.17% (33/19,649) in children of non-users, generating an adjusted OR of 1.04 (95% CI, 0.66–1.63).
Results of exploratory analyses are displayed in Table 4. They should be cautiously interpreted, as none of the exploratory analyses had a statistical power of more than 50% to detect an OR of 0.60. There did not seem to be a strong gradient in risk by timing of initiation of folic acid use within the primary exposure interval (Table 4, analysis #1). The use of other vitamins and minerals in addition to folic acid did not appear to affect autistic disorder risk (Table 4, analysis #2). The analyses based on the food-frequency questionnaire data from week 22 did not reveal any apparent association between maternal total daily folate intake in week 22 (diet and supplements combined) and subsequent risk of autistic disorder in children (Table 4, analysis #3). The analysis in which cases were stratified according to language level suggested that the inverse association may be strong in those with severe language delay and weak in those with moderate or no delay (Table 4, analysis #4). The analysis stratified by year of birth suggested that the inverse association may be stronger in the older children (born in 2002–04) than in the younger children (born in 2005–08) (Table 4, analysis #5).
Table 4.
Exploratory Analyses
| Total | Autistic Disorder | Unadjusted | Adjusted a | |||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| n | % | n | % | OR | 95% CI | OR | 95% CI | |
| 1. Initiation of folic acid | ||||||||
| No folic acid | 14,721 | 17.3 % | 32 | 0.22 % | 1 (ref) | --- | 1 (ref) | --- |
| Initiation week (−4) to (−1) | 28,061 | 32.9 % | 32 | 0.11 % | 0.52 | 0.32 – 0.86 | 0.67 | 0.40 – 1.14 |
| Initiation week 0 to 4 | 16,797 | 19.7 % | 18 | 0.11 % | 0.49 | 0.28 – 0.88 | 0.58 | 0.32 – 1.05 |
| Initiation week 5 to 8 | 16,184 | 19.0 % | 14 | 0.09 % | 0.40 | 0.21 – 0.75 | 0.44 | 0.23 – 0.83 |
| Initiation week 9 to 17 | 9,395 | 11.0 % | 18 | 0.19 % | 0.88 | 0.49 – 1.57 | 0.87 | 0.49 – 1.57 |
|
| ||||||||
| 2. Use of other vitamins and minerals in week (−4) to 8 | ||||||||
| No vitamins/minerals | 21,106 | 24.8 % | 44 | 0.21 % | 1 (ref) | --- | 1 (ref) | --- |
| Other vitamins/minerals, no folic acid | 3,028 | 3.6 % | 6 | 0.20 % | 0.95 | 0.41 – 2.23 | 0.93 | 0.40 – 2.19 |
| Folic acid only | 29,075 | 34.1 % | 31 | 0.11 % | 0.51 | 0.32 – 0.81 | 0.62 | 0.38 – 1.00 |
| Folic acid plus other vitamins/minerals | 31,967 | 37.5 % | 33 | 0.10 % | 0.50 | 0.32 – 0.78 | 0.58 | 0.36 – 0.94 |
|
| ||||||||
| 3. Total daily folate intake in week 22 (μg) b | ||||||||
| Quartile 1 (mean 209, range 62–272) | 19,611 | 24.7 % | 26 | 0.13 % | 1 (ref) | --- | 1 (ref) | --- |
| Quartile 2 (mean 345, range 272–434) | 19,634 | 24.7 % | 22 | 0.11 % | 0.85 | 0.48 – 1.49 | 0.88 | 0.50 – 1.55 |
| Quartile 3 (mean 560, range 434–667) | 19,485 | 24.5 % | 26 | 0.13 % | 1.01 | 0.58 – 1.73 | 1.08 | 0.62 – 1.87 |
| Quartile 4 (mean 874, range 667–5,673) | 19,429 | 24.5 % | 23 | 0.12 % | 0.89 | 0.51 – 1.57 | 0.97 | 0.55 – 1.72 |
| Intake not quantified c | 1,244 | 1.6 % | 2 | 0.16 % | 1.21 | 0.29 – 5.12 | 1.01 | 0.24 – 4.27 |
|
| ||||||||
| 4. Autistic disorder cases stratified by language level at 36 months d | ||||||||
| Severe language delay | ||||||||
| No folic acid | 24,134 | 28.3 % | 18 | 0.07 % | 1 (ref) | --- | 1 (ref) | --- |
| Use of folic acid | 61,042 | 71.7 % | 18 | 0.03 % | 0.40 | 0.21 – 0.76 | 0.49 | 0.25 – 0.99 |
| Moderate or no language delay | ||||||||
| No folic acid | 24,134 | 28.3 % | 13 | 0.05 % | 1 (ref) | --- | 1 (ref) | --- |
| Use of folic acid | 61,042 | 71.7 % | 29 | 0.05 % | 0.88 | 0.46 – 1.70 | 0.91 | 0.46 – 1.81 |
| Missing data | ||||||||
| No folic acid | 24,134 | 28.3 % | 19 | 0.08 % | 1 (ref) | --- | 1 (ref) | --- |
| Use of folic acid | 61,042 | 71.7 % | 17 | 0.03 % | 0.35 | 0.18 – 0.68 | 0.48 | 0.24 – 0.96 |
|
| ||||||||
| 5. Study sample stratified by year of birth | ||||||||
| 2002–04 | ||||||||
| No folic acid | 12,899 | 42.8 % | 37 | 0.29 % | 1 (ref) | --- | 1 (ref) | --- |
| Use of folic acid | 17,218 | 57.2 % | 21 | 0.12 % | 0.42 | 0.25 – 0.73 | 0.45 | 0.26 – 0.79 |
| 2005–08 | ||||||||
| No folic acid | 11,235 | 20.4 % | 13 | 0.12 % | 1 (ref) | --- | 1 (ref) | --- |
| Use of folic acid | 43,824 | 79.6 % | 43 | 0.10 % | 0.85 | 0.46 – 1.58 | 0.84 | 0.45 – 1.59 |
Adjusted for year of birth, maternal education level, and parity. For maternal education, missing data was included as a separate category in the logistic regression models. The analysis stratified by year of birth was adjusted for maternal education level and parity.
Analyses includes only responders to the food-frequency questionnaire in week 22 (n=79,403). The food-frequency questionnaire included report of brand names of supplements, enabling exact calculations of the amounts of folic acid ingested per day. Dietary intake was adjusted for dietary folate equivalents (DFEs) when total intake was calculated.
Not quantified because reported daily energy intake was outside of the valid range, i.e., <4,500 kJ/day or >20,000 kJ/day.
Information on language skills was obtained from the MoBa 36-month questionnaire, and data were missing for autistic disorder cases whose mothers had not responded to that questionnaire (n=36).
COMMENT
The study found that maternal folic acid supplementation from 4 weeks before to 8 weeks after the start of pregnancy was associated with a lower risk of autistic disorder – the most severe form of ASD – in children. If the observed inverse association represents a causal relationship, the finding indicates that a deficiency of folate around conception and early pregnancy, or a reduced ability to utilize available folate, are important causes of autistic disorder. If so, this finding creates opportunities for highly effective preventive measures.
Use of folic acid supplements was associated with higher socio-economic status and more health-conscious maternal behavior patterns in the study sample. We cannot exclude the possibility that some portion of the inverse association represents residual, unmeasured confounding. However, if residual confounding was substantial, we would have expected to find a lowering of risk associated with fish oil supplement use as well, since the use of fish oil was associated with exactly the same parental characteristics in the study sample. No such lowering of risk was observed. We would also have expected the inverse association between folic acid use and autistic disorder risk to persist in mid-pregnancy (week 22), which it did not.
To further assess the possibility of residual confounding, we explored whether maternal illness and medication use during pregnancy had any effect on the inverse association. Information about maternal illness and medication use was obtained from the questionnaire completed in week 18 and from the Medical Birth Registry. We adjusted the logistic regression models for the presence of anxiety, depression, epilepsy, preeclampsia, and diabetes during pregnancy (separately for each disorder). We also made separate adjustments for use of medications for anxiety, depression, and epilepsy, and for the use of hormone treatment and in vitro fertilization to become pregnant. None of the adjustments made any difference, which might reflect the fact that the pregnant women in the cohort were generally healthy and had low proportions of medication use during pregnancy. We did not have data on more rare psychiatric disorders, but we believe that such disorders are unlikely to have had any significant influence.
Our findings indicate that the inverse association may be largely driven by the autistic disorder cases with severe language delay at 36 months, who were presumably the more severely affected children. It is also worth noting that the OR estimate for those with missing data on language level (non-responders to the screening questionnaire) was similar to those with severe language delay. This suggests that mothers with severely affected children may have had lower response rates, and that an ascertainment bias may have been present. The possibility of such bias, combined with the small numbers in each stratum, warrants caution in the interpretation of these findings.
The participation rate among women invited to participate in MoBa was 38.5%, and the cohort is not fully representative of the Norwegian population. Comparisons to nationwide registry data have demonstrated that the mothers in the cohort were more likely to be first-time mothers and that they had higher levels of education, a higher mean age, and lower levels of smoking than other pregnant women21. The proportions of single mothers and mothers with an immigrant background were very low (unpublished data). We tested the generalizability of our findings by replicating the analyses in a nationwide data file containing data from the Medical Birth Registry of Norway, the Norwegian Patient Registry, and Statistics Norway. We included children born in 1999–2007 and applied the same inclusion criteria as for the MoBa-based analyses. The replication sample included 473,095 children, of whom 822 (0.17%) had autistic disorder diagnoses recorded by Norwegian specialist health services. Folic acid use is substantially underreported in the Medical Birth Registry; our comparisons with the MoBa questionnaire data found that half of the mothers reported to be non-users in the registry actually had reported folic acid use in the questionnaires. This underreporting is a major limitation and will bias association measures towards the null. Despite this, we did find a significant inverse association in the nationwide sample: mothers with reported folic acid use had an adjusted OR of 0.83 (95% CI, 0.71–0.97) for autistic disorder in their children. When the MoBa participants were analysed using the registry-based folic acid variable, the adjusted OR was 0.75 (95% CI, 0.46–0.96). The similarity between MoBa participants and non-participants indicate that our MoBa-based analyses have not been significantly affected by selection bias.
The strengths of the study were the cohort design, large sample size, population-based recruitment of cohort participants, prospective data collection, and the combination of screening, referrals and registry linkage for detection of ASD cases. The richness of the exposure data allowed for differentiations between different supplements, and between the various stages of pregnancy. Our ability to compare the study sample with a nationwide sample was also an advantage. The main limitation was the incomplete ascertainment of ASD cases in the cohort. The prevalence of diagnosed ASD was lower than what has been reported from the United Kingdom and the United States22,23, although that discrepancy is not merely due to underscertainment, because the nationwide ASD prevalence is also lower in Norway24. For the country as a whole, the prevalence is estimated to be 0.8% in 12-year-olds24, which is not very different from the 0.66% prevalence observed for children born in 2002 and 2003 in the MoBa cohort (eTable 1). Underascertainment was less of a problem for autistic disorder than for the other ASD subtypes, but it was still reassuring that the inverse association for autistic disorder was stronger in the older children (born in 2002–04), for whom case ascertainment was closer to completion. The relative weakness of the inverse association among the younger children (born in 2005–08) may have resulted from the fact that mothers who took prenatal folic acid supplements had higher questionnaire response rates, causing the ASD cases among their children to be identified earlier. As mentioned previously, there was also the possibility of ascertainment bias arising from lower response rates among parents of the more severely affected autistic disorder cases. If such bias was present, the OR estimate for the younger children would be biased towards the null..
Another limitation of the study was the reliance on subtype diagnoses of ASD. These have not been found to have high reliability across assessment sites in studies in the United States, and may be removed altogether from the upcoming DSM-V classification system25. Our own validation of registry diagnoses indicated that subtype diagnoses were less reliable than for ASD as a whole, but there was still a high level of agreement (PPV=80%) for autistic disorder diagnoses, which was the outcome of primary interest.
Our main finding was that maternal use of folic acid supplements around the time of conception was associated with a lower risk of autistic disorder. This finding does not establish a causal relation between folic acid use and autistic disorder, but provides a rationale for replicating the analyses in other study samples and further investigating genetic factors and other biological mechanisms that may explain the inverse association.
Supplementary Material
Acknowledgments
The Norwegian Mother and Child Cohort is supported by the Norwegian Ministry of Health and Care Services, the Norwegian Ministry of Education and Research, the Research Council of Norway/FUGE (grant 151918), the National Institute of Neurological Disorders and Stroke (NIH/NINDS), Bethesda, MD, USA (grant NS47537 [Lipkin]), and the National Institute of Environmental Health Sciences (NIH/NIEHS), Research Triangle Park, NC, USA (contract NO-ES-75558). The Autism Birth Cohort study is funded by the NINDS (grant NS47537 [Lipkin]). Pål Surén’s salary is funded by the Research Council of Norway (grants 185476 and 190694). We are grateful to all the families in Norway who take part in these ongoing studies. Camilla Stoltenberg and Ezra Susser declare that they had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Deborah Hirtz, the Scientific Program Officer for the Autism Birth Cohort study at NINDS, participated in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, and approval of the manuscript.
Abbreviations
- ASD
Autism spectrum disorder
- CI
Confidence interval
- MoBa
The Norwegian Mother and Child Cohort Study
- OR
Odds ratio
- PDD-NOS
Pervasive developmental disorder not otherwise specified
- PPV
Positive predictive value
References
- 1.Czeizel AE, Dudas I. Prevention of the first occurrence of neural-tube defects by periconceptional vitamin supplementation. N Engl J Med. 1992 Dec 24;327(26):1832–1835. doi: 10.1056/NEJM199212243272602. [DOI] [PubMed] [Google Scholar]
- 2.Werler MM, Shapiro S, Mitchell AA. Periconceptional folic acid exposure and risk of occurrent neural tube defects. JAMA. 1993 Mar 10;269(10):1257–1261. [PubMed] [Google Scholar]
- 3.Daly LE, Kirke PN, Molloy A, Weir DG, Scott JM. Folate levels and neural tube defects. Implications for prevention. JAMA. 1995 Dec 6;274(21):1698–1702. doi: 10.1001/jama.1995.03530210052030. [DOI] [PubMed] [Google Scholar]
- 4.Shaw GM, Schaffer D, Velie EM, Morland K, Harris JA. Periconceptional vitamin use, dietary folate, and the occurrence of neural tube defects. Epidemiology. 1995 May;6(3):219–226. doi: 10.1097/00001648-199505000-00005. [DOI] [PubMed] [Google Scholar]
- 5.Berry RJ, Li Z, Erickson JD, et al. Prevention of neural-tube defects with folic acid in China. China-U.S. Collaborative Project for Neural Tube Defect Prevention. N Engl J Med. 1999 Nov 11;341(20):1485–1490. doi: 10.1056/NEJM199911113412001. [DOI] [PubMed] [Google Scholar]
- 6.Milunsky A, Jick H, Jick SS, et al. Multivitamin/folic acid supplementation in early pregnancy reduces the prevalence of neural tube defects. JAMA. 1989 Nov 24;262(20):2847–2852. doi: 10.1001/jama.262.20.2847. [DOI] [PubMed] [Google Scholar]
- 7.Prevention of neural tube defects: results of the Medical Research Council Vitamin Study. MRC Vitamin Study Research Group. Lancet. 1991 Jul 20;338(8760):131–137. [PubMed] [Google Scholar]
- 8.Centers for Disease C, Prevention. CDC Grand Rounds: additional opportunities to prevent neural tube defects with folic acid fortification. MMWR Morbidity and mortality weekly report. 2010 Aug 13;59(31):980–984. [PubMed] [Google Scholar]
- 9.Scientific Advisory Committee on Nutrition. London, United Kingdom: 2006. Folate and Disease Prevention. [Google Scholar]
- 10.Roth C, Magnus P, Schjolberg S, et al. Folic acid supplements in pregnancy and severe language delay in children. JAMA. 2011 Oct 12;306(14):1566–1573. doi: 10.1001/jama.2011.1433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schmidt RJ, Hansen RL, Hartiala J, et al. Prenatal vitamins, one-carbon metabolism gene variants, and risk for autism. Epidemiology. 2011 Jul;22(4):476–485. doi: 10.1097/EDE.0b013e31821d0e30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schmidt RJ, Tancredi DJ, Ozonoff S, et al. Maternal periconceptional folic acid intake and risk of autism spectrum disorders and developmental delay in the CHARGE (CHildhood Autism Risks from Genetics and Environment) case-control study. The American journal of clinical nutrition. 2012 Jul;96(1):80–89. doi: 10.3945/ajcn.110.004416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Magnus P, Irgens LM, Haug K, Nystad W, Skjaerven R, Stoltenberg C. Cohort profile: the Norwegian Mother and Child Cohort Study (MoBa) Int J Epidemiol. 2006 Oct;35(5):1146–1150. doi: 10.1093/ije/dyl170. [DOI] [PubMed] [Google Scholar]
- 14.Stoltenberg C, Schjolberg S, Bresnahan M, et al. The Autism Birth Cohort: a paradigm for gene-environment-timing research. Mol Psychiatry. 2010 Jul;15(7):676–680. doi: 10.1038/mp.2009.143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lord C, Rutter M, Le Couteur A. Autism Diagnostic Interview-Revised: a revised version of a diagnostic interview for caregivers of individuals with possible pervasive developmental disorders. J Autism Dev Disord. 1994 Oct;24(5):659–685. doi: 10.1007/BF02172145. [DOI] [PubMed] [Google Scholar]
- 16.Lord C, Risi S, Lambrecht L, et al. The autism diagnostic observation schedule-generic: a standard measure of social and communication deficits associated with the spectrum of autism. J Autism Dev Disord. 2000 Jun;30(3):205–223. [PubMed] [Google Scholar]
- 17.Meltzer HM, Brantsaeter AL, Ydersbond TA, Alexander J, Haugen M. Methodological challenges when monitoring the diet of pregnant women in a large study: experiences from the Norwegian Mother and Child Cohort Study (MoBa) Matern Child Nutr. 2008 Jan;4(1):14–27. doi: 10.1111/j.1740-8709.2007.00104.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Brantsaeter AL, Haugen M, Alexander J, Meltzer HM. Validity of a new food frequency questionnaire for pregnant women in the Norwegian Mother and Child Cohort Study (MoBa) Matern Child Nutr. 2008 Jan;4(1):28–43. doi: 10.1111/j.1740-8709.2007.00103.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sadler TW. Langman’s Medical Embryology. Baltimore, MD: Lippincott Williams & Wilkins; 2010. [Google Scholar]
- 20.Smith GD. Assessing intrauterine influences on offspring health outcomes: can epidemiological studies yield robust findings? Basic & clinical pharmacology & toxicology. 2008 Feb;102(2):245–256. doi: 10.1111/j.1742-7843.2007.00191.x. [DOI] [PubMed] [Google Scholar]
- 21.Nilsen RM, Vollset SE, Gjessing HK, et al. Self-selection and bias in a large prospective pregnancy cohort in Norway. Paediatric and perinatal epidemiology. 2009 Nov;23(6):597–608. doi: 10.1111/j.1365-3016.2009.01062.x. [DOI] [PubMed] [Google Scholar]
- 22.Baird G, Simonoff E, Pickles A, et al. Prevalence of disorders of the autism spectrum in a population cohort of children in South Thames: the Special Needs and Autism Project (SNAP) Lancet. 2006 Jul 15;368(9531):210–215. doi: 10.1016/S0140-6736(06)69041-7. [DOI] [PubMed] [Google Scholar]
- 23.Prevalence of autism spectrum disorders--Autism and Developmental Disabilities Monitoring Network, 14 sites, United States, 2008. MMWR Surveill Summ. 2012 Mar 30;61(3):1–19. [PubMed] [Google Scholar]
- 24.Suren P, Bakken IJ, Aase H, et al. Autism spectrum disorder, ADHD, epilepsy, and cerebral palsy in Norwegian children. Pediatrics. 2012 Jul;130(1):e152–158. doi: 10.1542/peds.2011-3217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lord C, Petkova E, Hus V, et al. A multisite study of the clinical diagnosis of different autism spectrum disorders. Arch Gen Psychiatry. 2012 Mar;69(3):306–313. doi: 10.1001/archgenpsychiatry.2011.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.