Abstract
Background:
Influenza is a major cause of morbidity and mortality in Canada, with up to 7000 influenza-related deaths occurring every year. The elderly and individuals with chronic diseases are at increased risk for influenza-related morbidity and mortality.
Methods:
We conducted a 2-year, community cluster-randomized trial targeting elderly people and at-risk groups to assess the effectiveness of pharmacy-based influenza vaccination clinics on influenza vaccination rates. Small rural communities in interior and northern British Columbia were randomly allocated to the intervention or control. In the intervention communities, pharmacy-based influenza vaccination clinics were held and were promoted to eligible patients using personalized invitations from the pharmacists, invitations distributed opportunistically by a pharmacist to eligible patients presenting to pharmacies during the flu season and community-wide promotion using posters and the local media. The main outcome measure was a difference in the mean influenza vaccination rates. The immunization rates were calculated using the number of immunizations given in each community divided by the population size estimated from the census data.
Results:
Baseline influenza immunization rates in the population ≥65 years of age were the same in the control (n = 10, mean 85.6% [SD 16.6]) and intervention (n = 14, mean 83.8% [SD 16.3]) communities in 2009 (p = 0.79). In 2010, the mean influenza immunization rate was 56.9% (SD 28.0) in the control communities (n = 15) and 80.1% (SD 18.4) in the intervention communities (n = 14) (p = 0.01) for those ≥65 years of age. However, in 2010, for those 2 to 64 years with chronic medical conditions, the immunization rates were lower in the intervention communities (mean 16.3% [SD 7.1]) compared with the control communities (mean 21.2% [SD 5.8]) (p = 0.04).
Conclusion
Clinics were feasible and well attended and they resulted in increased vaccination rates for elderly residents. In contrast, vaccination rates in the younger population with comorbidities remained low and unchanged.
Knowledge into Practice.
The elderly and individuals with chronic diseases are at increased risk for influenza-related morbidity and mortality, and the influenza vaccine is highly recommended for these individuals.
Not all small rural communities have access to a public health office, but they do have access to at least 1 pharmacy.
Pharmacists, who are among the most accessible health care providers, can play a significant role by sending reminder letters to their clients, providing extended service hours, educating clients on risk and benefits of the vaccine and administering vaccinations.
This trial demonstrates that pharmacist-based influenza clinics increased immunization rates for older adults.
Patients supported pharmacists as immunization providers and liked the fact that pharmacies offered extended hours.
Mise En Pratique Des Connaissances.
Les personnes âgées et celles qui souffrent de maladies chroniques ont des risques accrus de morbidité et de mortalité liés à la grippe, c’est pourquoi le vaccin antigrippal est fortement recommandé chez ces personnes.
Toutes les communautés rurales n’ont pas accès à un bureau de santé publique, mais elles ont au moins une pharmacie accessible.
Les pharmaciens, qui font partie des fournisseurs de soins de santé les plus accessibles, peuvent jouer un rôle très important : ils peuvent envoyer des lettres de rappel à leurs clients, offrir des heures d’ouverture prolongées, informer les clients sur les risques et les avantages de la vaccination et administrer les vaccins.
Cette étude démontre que les cliniques antigrippales dans les pharmacies permettent d’accroître les taux de vaccination des personnes âgées.
Les patients soutiennent le rôle du pharmacien dans le domaine de l’immunisation et apprécient les cliniques qui offrent des heures d’ouverture prolongées.
Background:
Influenza virus (A and B) is a major cause of morbidity and mortality in Canada.1,2 Early clinical symptoms of influenza-like illness (ILI) include onset of respiratory illness, fever, cough and 1 or more of the following: sore throat, arthralgia, myalgia or prostration with accompanying gastrointestinal symptoms in children less than 5 years of age.1 Those at highest risk are individuals 65 years and older, accounting for 90% of deaths, as well as individuals with chronic diseases (e.g., diabetes mellitus, cancer, immunodeficiency, immunosuppression, renal disease, anemia, hemoglobinopathies), pregnant women, and children aged 6 to 23 months.3 Annual influenza vaccination (containing inactivated A/H1N1, A/H3N2 and 1 influenza B virus) of individuals at high risk of influenza complications remains the primary strategy for reducing influenza-related morbidity and mortality in community and long-term care settings.3,4
In British Columbia (BC), influenza vaccine is provided free of charge to at-risk groups, as recommended by the National Advisory Committee on Immunization (NACI); however, despite access to free vaccines, adult immunization rates have remained suboptimal (i.e., below the 90% targeted goal set by NACI) and fluctuate considerably both over time and across different regions of the province.4 For example, in 2007, the overall BC influenza vaccine rate was 59% (95% CI 56%-63%) for those 65 years of age and over and 40% (95% CI 39%-42%) for those younger than 65 years with at least 1 chronic medical condition.5,6 The main motivating factor for influenza vaccine uptake is a recommendation from a health care professional, while barriers include lack of knowledge, inconvenience, inaccessibility, allergy to eggs and concerns over adverse events.7,8 Immunization promotion, accessibility and health care provider intervention are believed to be important organizational factors facilitating the uptake of influenza vaccination.7,8
There are approximately 3000 pharmacists practising in BC. Pharmacists are considered among the most easily accessible health care professionals available to the public.9 With an expanding scope of practice moving from product-oriented to patient-centred care, pharmacists are in an ideal position to deliver optimal pharmaceutical care services such as chronic disease management, adapting or writing prescriptions, emergency contraception, and injections, including vaccinations.9 Through regular contact with high-risk individuals, pharmacists have the ability to act as health care interventionists by reminding patients about the benefits of vaccination and taking a proactive, systemic approach in addressing this potential health care need.9
In Canada, the impact of using pharmacy-based vaccination strategies on immunization rates has not been studied. The goal of this study was to determine whether a patient-centred immunization strategy based in community pharmacies could improve vaccination rates in small rural communities. Ethics approval for this study was obtained from the University of British Columbia’s Clinical Research Ethics Board, and consent was obtained from all patients who participated in the intervention arm.
Methods
Community selection and randomization
The 2006 Canadian Census was used to identify 29 communities meeting our inclusion criteria (townships, first nations reserves, amalgamated townships and counties were excluded) of population size between 2000 and 6000 and with no recent geopolitical amalgamation. These communities were located within 2 health authorities in British Columbia—Northern Health and Interior Health Authorities—and each had at least 1 pharmacy in the community. Communities were stratified by size and randomly assigned to the intervention or control arm using a computer-generated randomization sequence. All pharmacies in participating communities were identified using the College of Pharmacists of BC listing of community pharmacies within the province. In addition, participating pharmacists in each community were asked to identify any pharmacies that were missed.
Target population
The target population was those who were at “high risk” of influenza-related adverse outcomes, such as those 65 years and older and those between the ages of 2 and 64 years with at least 1 chronic condition. These 2 groups are eligible to receive free, publicly funded vaccines in the province of British Columbia. These individuals were identified based on prescriptions filled for 1 or more medications for chronic diseases, such as cardiac or pulmonary disorders (e.g., bronchopulmonary dysplasia, cystic fibrosis, asthma, chronic obstructive pulmonary disease), diabetes or other metabolic diseases, cancer, immunodeficiency (including human immunodeficiency virus [HIV] infection), immunosuppression due to underlying disease or therapy (e.g., rheumatoid arthritis requiring immunosuppressive therapies), chronic kidney disease, chronic liver disease, anemia and hemoglobinopathy, and conditions that compromise the management of respiratory secretions and are associated with an increased risk of aspiration (e.g., cognitive dysfunction, spinal cord injury, seizure disorder and neuromuscular disorders).10
Intervention and control communities
All pharmacies in the intervention communities were approached and invited to participate. The strategies provided by pharmacies allocated to the intervention arm included the standardized training of pharmacists on providing injections and the use and safety monitoring of influenza vaccination. All the pharmacists who provided immunizations as part of this study had received training through the accredited “Administration of Injections” course provided by the BC Pharmacy Association. This program is made up of 2 components: an online prestudy called the Immunization Competency Program and an in-person workshop called the Practical Administration of Injections for BC Pharmacists. In addition to participating in this program, pharmacists need to provide valid certificates for cardiopulmonary resuscitation and first aid before being granted the authority to administer injections by the College of Pharmacists of BC.11
The pharmacists generated personalized invitation letters to the eligible clients (based on age or filled prescription for 1 or more medications for a chronic medical condition), which were directed to their clients (target population), inviting them to be vaccinated at the pharmacy clinics. There was also public promotion of the pharmacy-based clinics through advertisements in the media, such as local papers, radio and cable TV, and in pharmacy-based posters. In addition, posters within the pharmacies advertised the influenza vaccination clinics, which included the hours of service and eligibility criteria. Participating pharmacies were encouraged to hold 1 or 2 clinics per week during the influenza vaccination period (October 15 to December 31) and had a dedicated nurse or pharmacist to educate patients on the benefits of vaccination, to vaccinate patients, monitor for potential adverse events and provide education on influenza prevention (e.g., handwashing, lack of effect of antibiotics for influenza).
The strategies described above were not made available to pharmacies in the control communities during the 2 years of the study.
Measurement of outcomes
The primary outcome was the difference in the mean influenza vaccination rates in the intervention and control communities in 2009 and 2010. Data on influenza immunization rates were obtained at the community level for the entire population of residents 65 years and older and those between 2 to 64 years with at least 1 chronic medical condition. To estimate the number of patients with chronic medical conditions in each community, we used CIHI and CCHS data, which indicate that approximately 30% of individuals aged 2 to 64 years have at least 1 chronic illness.12
Data on the number of vaccinations given to individuals in our 2 study populations were obtained from the 2 health authorities. The data from the health authorities on influenza vaccinations are collected from all immunizers in the community (i.e., physician offices, pharmacies, public health units) in aggregate format by each health unit during each influenza season.
All participants at the pharmacy-based influenza clinics were asked to complete a short questionnaire during both years in which the intervention occurred. Questions regarding demographics, socioeconomic status, medical status, vaccination history and reasons for attending the pharmacy-based clinics were analyzed as secondary outcomes.
Analysis
The main analysis used the intention-to-treat approach and was based on a 2-sample independent t test comparing mean immuni-zation rates in each cluster aggregated across the 2 allocation arms. None of the randomized communities were excluded, and the patients were analyzed according to the randomization scheme. The results were reported as estimates of the differences between arms, 95% confidence interval and associated p values. For all tests, we used alpha = 0.05 level of significance. All analyses were performed using SAS version 9.2 (Cary, North Carolina).
Results
Study implementation and demographics
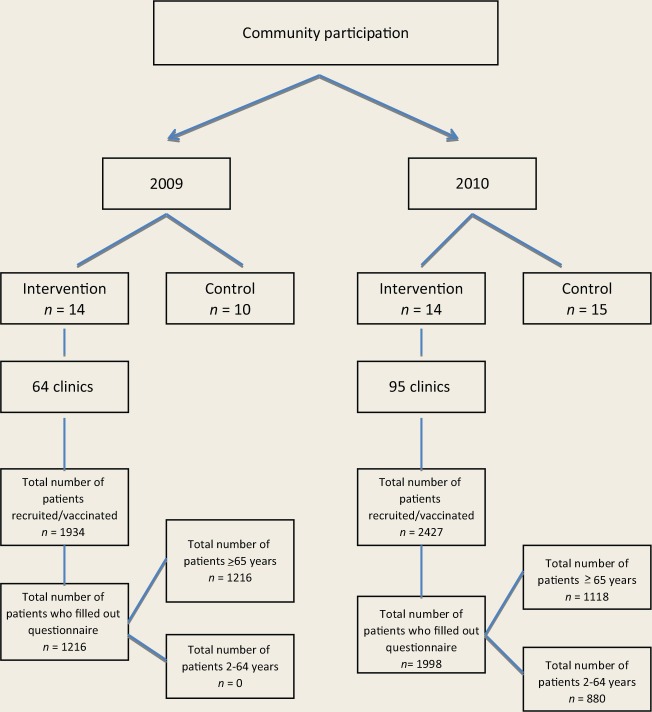
Figure 1 shows the trial profile. In 2009, of the 29 eligible communities, only 24 elected to participate. The communities that did not participate had only 1 pharmacy in the community and were too short-staffed to arrange for influenza vaccination clinics within the pharmacy. In the 24 included communities, the mean number of residents aged 65 years and over was 632 (min = 100, max = 1605; SD = 526) in the 14 intervention communities and 597 (min = 240, max = 1110; SD = 266) in the 10 control communities. The mean number of residents 2 to 64 years of age was 3028 (min = 1387, max = 5776; SD = 1268) in the 14 intervention communities and 3043 (min = 1662, max = 5810; SD = 1089) in the 15 control communities in 2010. All 14 intervention communities successfully implemented the strategy in 2009. A total of 15 pharmacies were recruited, and they held 64 clinics during the influenza season (October 15, 2009, to November 15, 2009). In 2010, the same 14 intervention communities with 19 pharmacies held a total of 95 clinics during the influenza campaign (October 15, 2010, to March 31, 2011). Overall, 2400 personalized invitation letters were sent to eligible patients: 800 letters in 2009 and 1600 letters in 2010. Within the intervention communities, 4361 residents received influenza vaccination in pharmacy-based sessions: 1934 residents during the 2009 influenza season and 2427 residents during the 2010 season. Not all patients recruited completed the questionnaire after receiving their influenza vaccination. Thus, a total of 1216 (in 2009) and 1998 (in 2010) questionnaires were completed by the vaccinated patients. The demographics of these patients are shown in Table 1.
Figure 1.
Trial profile
Table 1.
Demographics of the population vaccinated in the pharmacy-based sessions in the intervention communities in 2009 and 2010
| Characteristic | 2009 | 2010 |
|---|---|---|
| n = 1216 (100%)* | n = 1998 (100%)* | |
| Mean age (SD), years | 74.43 (7.03) | 63.19 (15.52) |
| Gender | ||
| Male | 602 (49.6) | 940 (47.3) |
| Marital status | ||
| Married/common law | 831 (69.3) | 1374 (69.7) |
| Single | 43 (3.6) | 206 (10.6) |
| Separated/divorced | 79 (6.6) | 127 (6.6) |
| Widowed | 247 (20.5) | 257 (13.0) |
| Education level | ||
| Elementary school | 196 (16.5) | 169 (8.7) |
| High school | 614 (51.6) | 1091 (56.2) |
| College or university | 378 (31.7) | 655 (33.8) |
| Currently a student | 3 (0.2) | 25 (1.3) |
| Employment | ||
| Yes | 79 (6.7) | 504 (33.7) |
| Total household income | ||
| <$14,999 | 113 (10.8) | 226 (15.3) |
| $15,000-$29,999 | 317 (30.4) | 372 (25.2) |
| $30,000-$44,999 | 199 (19.1) | 300 (20.3) |
| $45,000-$59,999 | 151 (14.5) | 230 (15.6) |
| $60,000-$79,999 | 89 (8.5) | 164 (11.1) |
| $80,000-$99,999 | 51 (4.89) | 104 (7.0) |
| ≥$100,000 | 37 (3.6) | 83 (5.5) |
| Average number of persons in household (SD) | 1.9 (2.1) | 2.1 (2.2) |
| Length of time at present address | ||
| <1 year | 54 (4.5) | 127 (6.5) |
| 1-5 years | 252 (21.1) | 495 (25.2) |
| ≥5 years | 886 (74.4) | 1339 (68.3) |
| Home ownership | ||
| Owned | 683 (86.6) | 1293 (84.7) |
| Rented | 106 (13.4) | 233 (15.3) |
| Work settings | ||
| Health care facility | 53 (3.1) | |
| Long-term care facility or community home | 50 (3.0) | |
| Providing childcare services to children <24 months | 9 (0.4) | |
| Working in closed setting (e.g., cruise ships) | 10 (0.5) | |
| Essential community services (e.g., firefighter) | 10 (0.6) | |
| None selected | 1854 (92.2) | |
| Chronic medical conditions (multiple)† | ||
| Diabetes | 170 (40.8) | 308 (37.4) |
| Renal disease | 14 (3.4) | 21 (2.6) |
| Liver disease | 9 (2.2) | 40 (4.9) |
| Respiratory disease | 119 (28.5) | 219 (26.6) |
| Cardiovascular disease | 95 (22.8) | 181 (21.9) |
| Solid organ or bone marrow transplant | 2 (0.5) | 3 (0.4) |
| Immunosuppressant related to disease or therapy | 8 (1.9) | 51 (6.2) |
Missing data not included in the analysis.
Participants were allowed to select multiple conditions.
Immunization rates
Table 2 shows the impact of using pharmacy-based vaccination strategies on immunization rates for the year 2009 (we used these as our baseline rates). Because this was the pandemic year, 2 influenza vaccination programs were rolled out across Canada—the seasonal influenza campaign with the trivalent vaccine and the pandemic H1N1 vaccine campaign. For British Columbia, the trivalent seasonal vaccine campaign was offered in 2 phases; the first phase was for individuals 65 years of age or older, beginning mid-October, while the second phase, beginning mid-November, was for those at high risk of influenza complications. In reality, only those patients 65 years of age or older were immunized with the seasonal vaccine, as the H1N1 vaccine was rolled out to the entire population as soon as it became available in mid-November.13 The mean rate of immunization in the 14 intervention communities was 83.8% (SD 16.3) compared with 85.6% (SD 16.6) in the 10 control communities, p = 0.79 (difference of 1.8%, 95% CI −12.3% to 15.9%). In 2010, there was a significant difference in influenza immunization rates in the 14 intervention communities compared with the 15 control communities in the population 65 years and over (80.1% [SD 18.4] vs 56.9% [SD 28]), p = 0.01 (difference of 23.8%, 95% CI −41.4% to −5.0%) but a lower rate for those between 2 and 64 years of age in the intervention (54.0% [SD 22.9]) compared with control communities (70.8% [SD 19.2]), p = 0.04 (difference of 16.8%, 95% CI −14.36% to −0.655%) (Table 3).
Table 2.
Immunization rates for people ≥65 years of age in the intervention and control communities in 2009
| Number of patients immunized | Population in community* | Rate of immunization† | |
|---|---|---|---|
| Intervention communities | |||
| 1 | 367 | 445 | 82.5 |
| 2 | 500 | 670 | 74.6 |
| 3 | 738 | 680 | 108.5 |
| 4 | 1186 | 950 | 124.8 |
| 5 | 1151 | 1405 | 81.9 |
| 6 | 1743 | 1435 | 121.5 |
| 7 | 807 | 1605 | 50.3 |
| 8 | 110 | 145 | 75.9 |
| 9 | 74 | 120 | 61.7 |
| 10 | 104 | 100 | 104.0 |
| 11 | 509 | 525 | 96.9 |
| 12 | 150 | 215 | 69.8 |
| 13 | 149 | 120 | 124.2 |
| 14 | 343 | 430 | 79.8 |
| Mean = 83.8 (SD 16.3)‡ | |||
| Control communities | |||
| 1 | 224 | 240 | 93.3 |
| 2 | 439 | 688 | 63.8 |
| 3 | 306 | 340 | 90.0 |
| 4 | 360 | 370 | 97.3 |
| 5 | 778 | 400 | 194.5 |
| 6 | 411 | 742 | 55.4 |
| 7 | 671 | 610 | 110.0 |
| 8 | 444 | 635 | 69.9 |
| 9 | 908 | 835 | 108.7 |
| 10 | 960 | 1110 | 86.5 |
| Mean = 85.6 (SD 16.6)‡ |
Determined from the 2006 Census data.
Clients immunized in a community/population in that community.
Assuming the communities with greater than 100% immunization rates had a maximum of 100% immunization.
Table 3.
Immunization rates in the intervention and control communities in 2010
| Population ≥65 years | Population 2-64 years with chronic medical conditions | |||||
|---|---|---|---|---|---|---|
| Number of patients immunized | Population in community* | Rate of immunization† | Number of patients immunized | Population in community‡ | Rate of immunization† | |
| Intervention communities | ||||||
| 1 | 325 | 540 | 60.2 | 235 | 1622 | 48.3 |
| 2 | 513 | 575 | 89.2 | 895 | 3642 | 81.9 |
| 3 | 589 | 795 | 74.1 | 253 | 2386 | 35.4 |
| 4 | 1119 | 1015 | 110.3 | 558 | 3021 | 61.6 |
| 5 | 1718 | 1545 | 111.2 | 894 | 2825 | 105.5 |
| 6 | 1702 | 1620 | 105.1 | 543 | 2876 | 62.9 |
| 7 | 1306 | 1755 | 74.4 | 631 | 2997 | 70.2 |
| 8 | 152 | 195 | 77.9 | 264 | 2438 | 36.1 |
| 9 | 185 | 165 | 112.1 | 387 | 4708 | 27.4 |
| 10 | 187 | 280 | 66.8 | 128 | 2174 | 19.6 |
| 11 | 570 | 670 | 85.1 | 698 | 4647 | 50.1 |
| 12 | 202 | 275 | 73.5 | 445 | 1889 | 78.5 |
| 13 | 79 | 150 | 52.7 | 200 | 1387 | 48.1 |
| 14 | 443 | 810 | 54.7 | 632 | 5776 | 36.5 |
| Mean = 80.1 (SD 18.4)** | Mean = 54.0 (SD 22.9)** | |||||
| Control communities | ||||||
| 1 | 134 | 290 | 46.2 | 209 | 1662 | 41.9 |
| 2 | 444 | 3360 | 13.2 | 1121 | 3892 | 96.0 |
| 3 | 277 | 395 | 70.1 | 423 | 3223 | 43.8 |
| 4 | 103 | 380 | 27.1 | 567 | 2898 | 65.2 |
| 5 | 858 | 480 | 178.8 | 601 | 2522 | 79.4 |
| 6 | 393 | 425 | 92.5 | 619 | 3386 | 60.9 |
| 7 | 653 | 695 | 93.9 | 534 | 1982 | 89.8 |
| 8 | 410 | 655 | 62.6 | 351 | 2021 | 57.8 |
| 9 | 860 | 910 | 94.5 | 480 | 3331 | 48.0 |
| 10 | 763 | 1220 | 62.5 | 694 | 3663 | 63.2 |
| 11 | 2009 | 4800 | 41.9 | 998 | 5810 | 57.3 |
| 12 | 275 | 625 | 44.0 | 529 | 2009 | 87.8 |
| 13 | 987 | 2568 | 38.4 | 745 | 2765 | 89.8 |
| 14 | 659 | 1766 | 37.3 | 567 | 2232 | 84.7 |
| 15 | 988 | 3446 | 28.7 | 1221 | 4245 | 95.9 |
| Mean = 56.9 (SD 28.0)** | Mean = 70.8 (SD 19.2)** | |||||
Determined from the 2006 Census data.
Clients immunized in a community/population in that community.
Clients immunized in a community/population with chronic conditions in that community (assumed to be 30%).
Assuming the communities with greater than 100% immunization rates had a maximum of 100% immunization.
Reasons for attending pharmacy-based clinics
Most participants had received an influenza vaccination the year prior to the influenza season, with the majority of the participants receiving their vaccination at a public health clinic (Table 4). As was expected, there was a high association between the respondents having the influenza vaccination in previous years with those coming in for influenza vaccination the current year. Approximately one-third of the participants heard of the influenza vaccination clinic at the pharmacy from the local newspaper, and just over 20% came to the pharmacy because of a personalized letter from their pharmacist. The most common reason provided by the participants for coming to the influenza clinic was because of the expanded hours associated with pharmacies.
Table 4.
Influenza vaccination information
| Question | 2009 | 2010 |
|---|---|---|
| n = 1216 (100%)* | n = 1998 (100%)* | |
| Did participant receive an influenza vaccination last year? | ||
| Yes | 991 (91.0) | 1641 (90.0) |
| No | 98 (9.0) | 183 (10.0) |
| If vaccinated last year, where did participant receive influenza vaccination? | ||
| Pharmacy clinic | 26 (2.7) | 200 (11.9) |
| Public health clinic | 507 (52.0) | 926 (54.1) |
| Family physician office | 98 (10.1) | 115 (6.8) |
| Walk-in clinic | 96 (9.9) | 151 (8.9) |
| At work | 4 (0.4) | 28 (1.7) |
| Seniors centre/hall/complex | 158 (16.3) | 106 (6.3) |
| Other | 83 (8.6) | 149 (8.9) |
| Hospital | 0 (0) | 25 (1.4) |
| Did participant receive influenza vaccination 2 years ago? | ||
| Yes | 655 (87.3) | 1128 (86.5) |
| No | 78 (12.7) | 176 (13.5) |
| How did the participant learn about the pharmacy-based clinic?† | ||
| Invitation letter from my pharmacist in mail | 317 (28.4) | 427 (23.4) |
| Flyer/sticker from pharmacist | 76 (6.8) | 191 (10.5) |
| Flyer/poster in the community | 83 (7.4) | 138 (7.6) |
| Local newspaper | 504 (45.2) | 584 (32.1) |
| Told by friend, family, neighbor | 117 (10.5) | 367 (20.2) |
| Walk-in | 46 (4.1) | 241 (13.2) |
| What brought participant to influenza vaccination clinic?† | ||
| Picking up medications | 282 (32.5) | 756 (41.2) |
| Free parking | 141 (16.2) | 115 (6.3) |
| Expanded opening hours | 356 (40.9) | 1183 (64.5) |
| Picking up nonmedicine items at store | 248 (28.5) | 704 (38.4) |
| Other | 62 (6.3) | 6 (0.33) |
Missing data not included in the analysis.
Participants were allowed to pick multiple answers.
Discussion
We demonstrated that a pharmacist-based intervention improved immunization rates in the elderly (those ≥65 years) within small rural communities. However, our study did not observe a difference in those between the ages of 2 and 64 years with a chronic medical condition. Implemented strategies that largely contributed to improvements in vaccination rates were newspaper advertisements and personalized mail-out invitation letters from the pharmacist.
This outcome is supported by a systematic review by Ompad et al.,14 who showed that advertising and patient mailings, along with telephone calls and patient/staff education, are interventions that enabled practitioners to meet the Healthy People 2010 targets (i.e., 90% vaccination for noninstitutionalized patients ≥65 years). Similarly, a systematic review conducted by the Cochrane Collaboration noted that any form of patient reminder, including letters and advertisements, did improve immunization rates, regardless of patient age or type of setting.15 Intervention strategies that were found to be the most effective often contained an element of personalization or increased exposure to the general community. Strategies such as personalized invitations, local newspaper advertisements, walk-in capability and word of mouth (by friends or family) showed greater value in increasing awareness of pharmacy-based influenza clinic immunization opportunities in comparison to general flyers from the pharmacy or in the community. Other studies have also shown that increasing the frequency and degree of personalization in advertising is effective in increasing immunization rates. In addition, multiple intervention strategies likely contribute to increasing vaccination rates—in other words, a combination of interventions is better than 1 specific intervention at increasing vaccination rates.16-18
Our survey showed that a large proportion of participation in a pharmacy-based influenza clinic was due to convenience (i.e., participants could pick up other items from store, or opening hours were extended). A survey conducted in Nova Scotia by Corsten et al.19 also revealed that 80% of participants preferred pharmacy-based clinic immunization due to convenience. Therefore, involvement of qualified pharmacists, who are highly accessible in rural communities, as vaccinators may be the key in developing a multicomponent immunization approach.
Our study had a number of limitations, with the largest being that its first year coincided with the H1N1 pandemic.20,21 As a result, seasonal vaccine was only indicated for those 65 years and older in that year, which meant that we could not draw conclusions from those 2 to 64 years of age with chronic medical conditions. Given our findings for the year 2010, where we did not see a significant increase in immunization rates within the 2 to 64 years of age cohort but did for the elderly, it would have been important to include this group in the first year of our study as well. In addition, it is not clear how the H1N1 pandemic affected the following year’s influenza vaccination rates. Another difference between 2009 and 2010 influenza seasons was that in the first year of our study, most of the pharmacy-based clinics were led by nurses and were by appointment only or had limited scheduled times, as the pharmacists were not yet certified to give injections and therefore needed to hire a nurse to run their clinics. By 2010, the majority of the clinics were run by pharmacists and so hours of operation and number of clinics offered were greater. This aspect may have contributed to the effect seen in 2010 but not in 2009 for those over 65 years of age and older.
Another limitation of our study was lack of accurate denominator data. This posed 2 problems for us—one was that the numerator sometimes exceeded the denominator, which gave us vaccination rates of over 100%. While these rates were set to 100% in our calculations of the immunization rates, this is clearly a limitation. However, we believe this was likely the result of a significant number of people driving from adjacent areas and receiving their vaccinations in the study communities. Accurate data are lacking regarding the number of patients with chronic medical conditions in each community, so we had to estimate the proportion of patients with a chronic medical condition within the chosen communities based on CIHI and CCHS data, which suggest that approximately 30% of individuals aged 2 to 64 years have a chronic illness. Although 2028 surveys were assigned participant ID numbers, only 1998 were completed. Of the completed questionnaires, some had missing data that could have biased the results. In addition, like all questionnaires, a certain degree of subjectivity is always present. Participant honesty, memory and motivation to complete the survey are all variables that could have skewed the results. A further limitation would be the representativeness of the sample given that the data are self-reported. Although participants chosen to complete the surveys were randomly sampled, errors due to no response may exist; people who chose to respond to the survey may have been different from those who did not, thus leading to a biased response rate as a result of confounding variables.
Pharmacists, with their expanding scope of practice, are among the most accessible health care professionals available to the general public and can be at the forefront of public health initiatives. Pharmacists are in an ideal place to act as public health care interventionists through proactive identification and engagement with patients. As a result of legislation that allows a pharmacist to immunize, the convenient locations of pharmacies, extended opening hours and overall accessibility, the lack of availability of public health clinics in small rural locations means that the establishment of pharmacy-based clinics in rural areas can aid in achieving higher rates of vaccination. The results of this study suggest that by promoting immunization programs publicly and improving access to immunization services as a result, communities can increase immunization coverage rates—leading to predictable outcomes such as improvement in patient quality of life through reduced morbidity and mortality and a reduction in health care cost.
Conclusion
In a cluster-randomized trial of pharmacist intervention to improve influenza vaccination rates, we demonstrated an improvement in vaccination in patients 65 years of age and older. Given these findings, we suggest that the use of multiple strategies to increase education of the provider, increase community demand and decrease barriers for vaccinations can result in higher vaccination rates. ■
Acknowledgments
We thank the communicable disease control public health nursing managers, medical health officers and pharmacists within the Interior Health Authority and Northern Health Authority for supporting this initiative. The study could not have taken place without the tireless work of Ms. Elissa Murru and Ms. Louise Gastonguay for obtaining ethics approval, recruiting the pharmacists and collecting the data. Finally, we thank the BC Pharmacy Association and Canadian Pharmacists Association for printing posters and their support in kind.
Footnotes
Financial acknowledgements:This study was funded by the Partners in Health Grant through the Canadian Institutes of Health Research (CIHR), Michael Smith Foundation for Health Research (MSFHR), Pharmaceutical Services Division within the Ministry of Health and Safety.
References
- 1. Reyes F, Aziz S, Macey JF, et al. Influenza in Canada: 2006-2007 season update. Canada Communicable Diseases Report 2007;33(9):85-92 [PubMed] [Google Scholar]
- 2. Public Health Agency of Canada Flu watch: definitions for the 2013-2014 season. Ottawa (ON): PHAC; 2013. Available: http://www.phac-aspc.gc.ca/fluwatch/13-14/def13-14-eng.php (accessed November 19, 2013). [Google Scholar]
- 3. National Advisory Committee on Immunization (NACI) Statement on seasonal Trivalent Inactivated Influenza Vaccine (TIV) for 2010-2011. Available: www.phac-aspc.gc.ca/publicat/ccdr-rmtc/10vol36/acs-6/index-eng.php#toc1 (accessed November 15, 2011). [DOI] [PMC free article] [PubMed]
- 4. BC Center for Disease Control Immunization in British Columbia, 2008. Available: www.bccdc.ca (accessed November 16, 2011).
- 5. Canadian Community Health Survey Influenza immunization for community-based populations aged 65 years and older for 2003, 2005 and 2007. Available: www.bccdc.org (accessed April 8, 2013).
- 6. Canadian Community Health Survey Influenza immunization for select high-risk groups under 65 years of age for 2003, 2005 and 2007. Available: www.bccdc.org (accessed April 8, 2013).
- 7. Noula M. Evaluation of elderly immunization coverage against flu. Review of Clinical Pharmacology and Pharmacokinetics International Edition 2007;21(3):279-84 [Google Scholar]
- 8. Zimmerman RK, Nowalk MP, Bardella IJ, et al. Physician and practice factors related to influenza vaccination among the elderly. Am J Prev Med 2004:26(1):1-10 [DOI] [PubMed] [Google Scholar]
- 9. Canadian Pharmacists Association Summary of pharmacists’ expanded scope of practice activities across Canada. Ottawa (ON): Canadian Pharmacists Association; 2013. Available: http://blueprintforpharmacy.ca/docs/kt-tools/pharmacists’-expanded-scope_summary-chart—cpha—october-2013.pdf (accessed November 19, 2013). [Google Scholar]
- 10. BCCDC Communicable Disease Manual Immunization. Available: www.bccdc.ca/NR/rdonlyres/9C32CA14-634C-46DE-9538-4FC168E10D8D/0/Section_VII_Biological_ProductsNovember212012FINAL.pdf (accessed November 23, 2011).
- 11. College of Pharmacists of BC Medication management (administering injections). Available: www.bcpharmacists.org/about_us/key_initiatives/index/articles/70.php (accessed April 27, 2013).
- 12. Canadian Institute for Health Information Primary health care. Figure 2: percentage of adults who reported having at least 1 of 11 chronic conditions, by age group, Canada. Available>: www.cihi.ca/CIHI-ext-portal/internet/en/document/types+of+care/primary+health/release_27jan11_fig2 (accessed March 12, 2012).
- 13. BC Centre for Disease Control Immunization program. Available: www.bccdc.ca/NR/rdonlyres/649FA900-F6DF-481F-A52D-C61673470908/0/ac_2009_18_Influenza.pdf (accessed October 31, 2013).
- 14. Ompad DC, Galea S, Vlahov D. Distribution of influenza vaccine to high risk groups. Epidemiol Rev 2006;28:54-70 [DOI] [PubMed] [Google Scholar]
- 15. Jacobson Vann J, Szilagyi P. Patient reminder and patient recall systems to improve immunization rates: a review. Cochrane Database Syst Rev 2005;(3):CD003941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Ndiaye SM, Hopkins DP, Shefer AM, et al. Interventions to improve influenza, pneumococcal polysaccharide, and hepatitis B vaccination coverage among high-risk adults. Am J Prev Med 2005;28(5 Suppl):248-77 [DOI] [PubMed] [Google Scholar]
- 17. Baker AM, McCarthy B, Gurley VF, Yood MU. Influenza immunization in a managed care organization. J Gen Intern Med 1998;13:469-75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Zimmerman RK, Nowalk MP, Raymund M, et al. Tailored interventions to increase influenza vaccination in neighbourhood health centers serving the disadvantaged. Am J Public Health 2003;93:1699-705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Corsten E, Bowles SK, Power B, McNeil S. Pharmacists as immunizers: key determinants of community pharmacists’ willingness to administer immunizations to adults (abstract). Can J Infect Dis Med Microbiol 2006;17:372 [Google Scholar]
- 20. Louie JK, Acosta M, Winter K, et al. ; California Pandemic (H1N1) Working Group Factors associated with death or hospitalization due to pandemic 2009 influenza A(H1N1) infection in California. JAMA 2009;302:1896-902 [DOI] [PubMed] [Google Scholar]
- 21. Jain S, Kamimoto L, Bramley AM, et al. ; 2009. Pandemic Influenza A (H1N1) Virus Hospitalizations Investigation Team Hospitalized patients with 2009 H1N1 influenza in the United States, April-June 2009. N Engl J Med 2009;361:1935-44 [DOI] [PubMed] [Google Scholar]