Abstract
The question of whether cigarette smoking was associated with lung cancer was central to the expansion of epidemiology into the study of chronic diseases in the 1950s. The culmination of this era was the 1964 report of the Advisory Committee to the Surgeon General, a landmark document that included an objective synthesis of the evidence of the health consequences of smoking according to causal criteria. The report concluded that cigarette smoking was a cause of lung cancer in men and sufficient in scope that “remedial action” was warranted at the societal level. The 2014 Surgeon General's report commemorates the 50th anniversary of the 1964 report. The evidence on the health consequences of smoking has been updated many times in Surgeon General's reports since 1964. These have summarized our increasingly greater understanding of the broad spectrum of the deleterious health effects of exposure to tobacco smoke across most major organ systems. In turn, this evidence has been translated into tobacco control strategies implemented to protect the public's health. The Surgeon General report process is an enduring example of evidence-based public health in practice. Substantial progress has been made, but cigarette smoking remains one of the most pressing global health issues of our time.
Keywords: causal inference, cigarette smoking, epidemiology, evidence-based public health, history, lung cancer, research methods, secondhand smoke exposure
The 2014 Surgeon General's report (SGR) entitled “The Health Consequences of Smoking: 50 Years of Progress” (1) was published to coincide with the 50th anniversary of the 1964 publication of “Smoking and Health: Report of the Advisory Committee to the Surgeon General of the Public Health Service” (2). In addition to providing yet another update on the health effects of cigarette smoking, the new report includes a review of the history of cigarette smoking and its deleterious impact on population health. Since the 1964 report, 32 SGRs focused on tobacco have been published (Table 1). Given the enormous toll that cigarette smoke takes on public health, it is indeed fitting that cigarette smoking has been the predominant topic of SGRs issued after 1964.
Table 1.
A Timeline of the Initial Report of the Advisory Committee to the Surgeon General and the 32 Subsequent Reports of the Surgeon General on Topics Related to Cigarette Smoking, Involuntary Smoking, and Tobacco Usea
| Year (Reference No.) | Title |
|---|---|
| 1964 (2) | Smoking and Health: Report of the Advisory Committee to the Surgeon General of the Public Health Service |
| 1967 (35) | The Health Consequences of Smoking: a Public Health Service Review: 1967 |
| 1968 (36) | The Health Consequences of Smoking: 1968 Supplement to the 1967 Public Health Service Review |
| 1969 (37) | The Health Consequences of Smoking: 1969 Supplement to the 1967 Public Health Service Review |
| 1971 (38) | The Health Consequences of Smoking: a Report of the Surgeon General: 1971 |
| 1972 (39) | The Health Consequences of Smoking 1972 |
| 1973 (40) | The Health Consequences of Smoking |
| 1974 (41) | The Health Consequences of Smoking 1974 |
| 1975 (42) | The Health Consequences of Smoking 1975 |
| 1976 (43) | The Health Consequences of Smoking: A Reference Edition |
| 1978 (44) | The Health Consequences of Smoking 1977–1978 |
| 1979 (45) | Smoking and Health |
| 1980 (50) | The Health Consequences of Smoking for Women |
| 1981 (52) | The Health Consequences of Smoking: The Changing Cigarette |
| 1982 (46) | The Health Consequences of Smoking: Cancer |
| 1983 (47) | The Health Consequences of Smoking: Cardiovascular Disease |
| 1984 (48) | The Health Consequences of Smoking: Chronic Obstructive Lung Disease |
| 1985 (49) | The Health Consequences of Smoking: Cancer and Chronic Lung Disease in the Workplace |
| 1986 (53) | The Health Consequences of Involuntary Smoking |
| 1986 (55) | The Health Consequences of Using Smokeless Tobacco |
| 1988 (56) | The Health Consequences of Smoking: Nicotine Addiction |
| 1989 (78) | Reducing the Health Consequences of Smoking: 25 Years of Progress |
| 1990 (57) | The Health Benefits of Smoking Cessation |
| 1992 (79) | Smoking and Health in the Americas |
| 1994 (59) | Preventing Tobacco Use Among Young People |
| 1998 (80) | Tobacco Use Among U.S. Racial/Ethnic Minority Groups—African Americans, American Indians and Alaska Natives, Asian Americans and Pacific Islanders, and Hispanics |
| 2000 (60) | Reducing Tobacco Use |
| 2001 (51) | Women and Smoking |
| 2004 (62) | The Health Consequences of Smoking |
| 2006 (54) | The Health Consequences of Involuntary Exposure to Tobacco Smoke |
| 2010 (58) | How Tobacco Smoke Causes Disease: The Biology and Behavioral Basis for Smoking-Attributable Disease |
| 2012 (61) | Preventing Tobacco Use Among Youth and Young Adults |
| 2014 (1) | The Health Consequences of Smoking: 50 Years of Progress |
a There were a total of 32 independent tobacco-related Surgeon General's reports, including supplements and compendium from other reports (but not excerpts) counted as independent reports. The 1964 report was technically not a Surgeon General's report but rather a nongovernmental report of the Advisory Committee.
The 50th anniversary of the 1964 report provides an opportunity for the community of epidemiologists to reflect upon how closely intertwined the research on smoking and disease has been with the evolution of epidemiology and its role in chronic disease etiology and prevention. It is equally important to embrace the contributions that epidemiologists continued to make to the field after 1964 by carrying out studies that more completely catalogued smoking's health consequences, the ongoing synthesis of this evidence as part of the SGR process, and the translation of this evidence to protect the public's health.
The evidence-based public health framework delineated in Figure 1 is used to organize the discussion of how the events leading up to the 1964 report and the subsequent SGRs helped to shape epidemiology through 1) the development of epidemiologic research methods, 2) evidence synthesis and causal inference, 3) assessment of the risks, benefits, and costs of intervention, and 4) the translation of evidence into public health action. The importance of the ongoing process of the SGRs is then briefly described. Throughout, examples focus on the association between cigarette smoking and lung cancer because of its significance leading up to the 1964 report.
Figure 1.
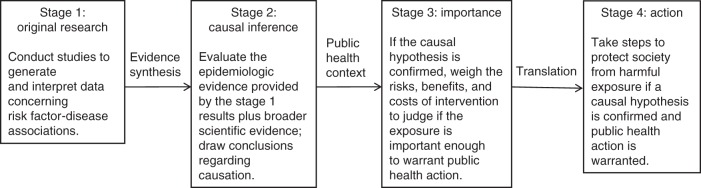
A framework for evidence-based public health.
GENERATING HIGH-QUALITY EPIDEMIOLOGIC EVIDENCE
The attempt to determine the association between cigarette smoking and lung cancer through epidemiologic research, which occurred primarily in the 1950s (with a few earlier studies), has been extensively chronicled (3, 4). A few of the numerous reasons for the historical interest in this topic are as follows: 1) it accelerated a shift from infectious disease to chronic disease epidemiology that began before World War II; 2) observational study designs used to study chronic diseases were refined relative to the pre-World War II experience, leading to important advances in epidemiologic research methods; 3) the study of determinants of chronic diseases motivated the development of a framework for causal inference; 4) the topic had enormous public health implications because smoking was so prevalent at the time; 5) cigarettes were manufactured by an influential and lucrative industry; and 6) the tobacco industry invested heavily to shape the scientific debate surrounding the question of whether there was a causal connection between smoking and disease.
Case-control studies
The steep increase in lung cancer rates that followed the upsurge in cigarette smoking in the first half of the 20th century led to the suspicion that the 2 were linked. This was the leading hypothesis from the outset for Ernst Wynder, a medical student at Washington University who was to be a driving influence in the research on the health effects of smoking throughout the 1950s and beyond. However, other hypothesized explanations for the increase in the rate of lung cancer included increasing industrialization, air pollution from automobile exhaust, and the tarring of roads (the favored a priori hypothesis of Richard Doll (5)). Observational studies were implemented to test these hypotheses (Figure 1, stage 1).
The first studies published were case-control studies. There were studies on the subject in which the case-control approach was used that were published before 1950; however, it was in 1950 that 5 case-control studies (6–10) were published in which investigators observed the consistent finding that cigarette smoking was strongly associated with an increased risk of lung cancer, which stimulated a concerted research focus on this potential relationship. The observation that cigarette smoking was a strong risk factor for lung cancer provoked debate about not only the results but also the validity of the case-control approach. This necessitated rigorous evaluation of the pros and cons of this new methodology. These were rapidly addressed by Jerome Cornfield as he described the odds ratio calculation from case-control data, the value of the odds ratio as an estimate of the relative risk, the rare disease assumption, and the importance of the representativeness of the control group (11). The principles of case-control studies continued to crystallize throughout the decade, as exemplified in the article by Mantel and Haenszel (12). A notable contribution was the conceptualization and calculation of population attributable risk by Morton Levin (13), who was also the lead investigator on one of the early case-control studies in which an association between smoking and lung cancer was demonstrated (8).
Cohort studies
The topic of smoking and lung cancer was also pivotal to establishing the important role of prospective cohort studies to study the etiology of chronic diseases. The need for cohort studies was recognized as researchers began to acknowledge that the case-control approach alone was not going to provide the definitive evidence that would be required to determine whether smoking caused lung cancer. According to the 1964 report, this “led several courageous investigators to undertake the necessarily protracted, expensive, and difficult prospective approach” (2, p. 162). Further, the first prospective cohort studies on this topic, the British Physician's Study (14) and the American Cancer Society Study (15), followed by the Veteran's Cohort Study (16) and others, were also initiated because they could assess additional endpoints, such as other malignancies, cardiovascular disease, and all-cause mortality.
The case-control methodology was validated in practice as cohort studies replicated the findings of the case-control studies. The successful application of case-control and cohort study methodologies to the investigation of smoking and lung cancer documented the value of these approaches, shepherding in the advancement of observational epidemiology to the study of chronic diseases and eventually other health-related outcomes. The emerging body of evidence on smoking and lung cancer was uniformly pointing in the same direction, regardless of study design, which led to discourse about whether this association could be considered causal.
EVIDENCE SYNTHESIS AND CAUSAL INFERENCE
The growing body of evidence from case-control and cohort studies indicated that cigarette smoking was strongly associated with the risk of lung cancer. With respect to methods for evidence synthesis, this association was the topic of what was likely the first ever meta-analysis. In 1956, Cornfield calculated a summary odds ratio for the association between smoking and lung cancer of 7.5 across 14 case-control studies included in his meta-analysis (17).
The association between smoking and lung cancer motivated considerable thought concerning causal inference from observational studies of noninfectious diseases. Cigarette smoking was associated with harm, which precluded the use of experimental studies in humans. In the absence of experimental human data, an important step was the work of Austin Bradford Hill (18) and Cornfield (19), who aimed to show that strong inferences were in fact possible from observational studies. Another key issue was the threat to correct inferences posed by the potential that the link between smoking and lung cancer was indirect and that smoking was merely acting as a marker for the true causal factor. This issue of what was later termed confounding was addressed based on the following sequence of logic: 1) The association between smoking and lung cancer was very strong, 2) any “third” factor would have to be as strongly associated with lung cancer as smoking, and 3) despite scores of studies of smoking and lung cancer, none had yet identified a factor even remotely as strongly associated with lung cancer as smoking (20).
There was also a need to develop a framework for causal inference for the chronic disease research paradigm. The conceptual underpinnings of a causal framework suitable to these circumstances that was premised on the notion of relative rather than absolute causes evolved during the 1950s and early 1960s (21). The transition from the infectious disease model of causality exemplified by the Henle-Koch postulates necessitated a shift to a more flexible causal framework that could allow for multiple causes (not all lung cancer was caused by smoking) and a single agent that could be a cause of multiple outcomes (smoking could cause more than one disease) (22). The criterion of specificity was thus not clearly relevant to this new way of conceiving of a web of disease causation (22). Specificity persisted as a criterion even though its limitations were clearly recognized at the time (e.g., “A universe in which cause and effect always have a one-to-one correspondence with each other would be easier to understand, but it obviously is not the kind we inhabit” (20, p. 196)). Specificity was included as a criterion in the 1964 report, but the discussion of specificity relied heavily on the strength of the association and stressed the limitations of this criterion based on the points noted above (2).
With a steadily accruing body of evidence, between 1957 and 1962, a total of 4 review groups in the United States and United Kingdom published evaluations that presaged the 1964 report by assessing the body of scientific evidence regarding the question of whether cigarette smoking was a cause of lung cancer. As summarized in Table 2, all 4 groups (the Medical Research Council (23), the Study Group on Smoking and Health (24), authors of the 1959 Journal of the National Cancer Institute manuscript (20), and the Royal College of Physicians (25)) concluded that cigarette smoking was a cause of lung cancer. This body of work leading up to the 1964 report shared similar approaches of attempting to synthesize all available evidence on the topic and to assess the strength of the evidence against alternative explanations of the data. The evidence considered was broad and cross-cutting, including laboratory evidence of carcinogenicity, the correlation between temporal trends in lung cancer death rates and historic trends in smoking prevalence by sex, and the results of observational studies (including dose-response and smoking cessation). The reports also assessed pathologic evidence that the association was strongest for squamous cell carcinoma and autopsy studies that indicated that smoking was associated with precancerous lung lesions. These reports clearly contained elegant causal thinking and were implicitly using criteria such as strength of the association (including dose-response) and consistency, but they did not explicitly use a framework for causal inference.
Table 2.
Conclusions of 4 United Kingdom–Based and United States–Based Groups That Assessed Whether Cigarette Smoking Was a Cause of Lung Cancer (1957–1962) and the Surgeon General's Advisory Committee on Smoking and Health (1964)
| Year (Reference No.) | Report Name | Contributors | Conclusions |
|---|---|---|---|
| 1957 (23) | Tobacco Smoking and Cancer of the Lung | Medical Research Council | “… [T]he most reasonable interpretation of this evidence is one of cause and effect” (p. 1524). |
| 1958 (24)a | Report of Study Group on Smoking and Health | Richard Bing, R.E. Dyer, Abraham Lilienfeld, Norton Nelson, Michael Shimkin, David Spain, F.M. Strong | “The sum total of scientific evidence establishes beyond reasonable doubt that cigarette smoking is a causative factor in the rapidly increasing incidence of human epidermoid carcinoma of the lung” (p. 60). |
| 1959 (20) | Smoking and Lung Cancer: Recent Evidence and a Discussion of Some Questions | Jerome Cornfield, William Haenszel, E. Cuyler Hammond, Abraham Lilienfeld, Michael Shimkin, Ernst Wynder | “The consistency of all the epidemiologic and experimental evidence also supports the conclusion of a causal relationship (of lung cancer) with cigarette smoking, while there are serious inconsistencies in reconciling the evidence with other hypotheses which have been advanced” (p. 173). |
| 1962 (25) | Smoking and Health: Summary Report of the Royal College of Physicians of London on Smoking in Relation to Cancer of the Lung and Other Diseases | Robert Platt, Aubrey Lewis, J.G. Scadding, R. Bodley Scott, F. Avery Jones, N.C. Oswald, C.M. Fletcher, J.N. Morris, J.A. Scott | “… [S]moking is an important cause of lung cancer” (p. 27). |
| 1964 (2) | Smoking and Health: Report of the Advisory Committee to the Surgeon General of the Public Health Service | Stanhope Bayne-Jones, Walter Burdette, William Cochran, Emmanuel Farber, Louis Fieser, Jacob Furth, John Hickam, Charles LeMaistre, Leonard Schuman, Maurice Seevers | “Cigarette smoking is causally related to lung cancer in men; the magnitude of the effect of cigarette smoking far outweighs all other factors. The data for women, though less extensive, point in the same direction” (p. 196). |
| “On the basis of prolonged study and evaluation of many lines of converging evidence, the Committee makes the following judgment: Cigarette smoking is a health hazard of sufficient importance in the United States to warrant appropriate remedial action” (p. 33). |
a The Study Group on Smoking and Health was sponsored by the National Cancer Institute, National Heart Institute, American Cancer Society, and American Heart Association.
The 1962 Royal College of Physicians report indirectly spurred the 1964 US report. When queried about the 1962 report's conclusion that cigarette smoking caused lung cancer, President John F. Kennedy, unaware of the report, deferred but stated he would provide a future response. Two weeks later, Surgeon General Luther Terry announced that he was establishing a Surgeon General's Advisory Committee (SGAC) of impartial experts to advise him on the matter.
A list was developed among various governmental health agencies, voluntary health organizations, the White House, and tobacco industry representatives to identify 150 potential candidates who had never previously taken a strong public position either for or against the association. From this list, Dr. Peter Hamill, Medical Coordinator to the SGAC, oversaw the SGAC selection process. Dr. Hamill's selection process was guided by criteria that stressed lack of bias, openness to new ideas, ability to critically analyze information, and ability to think across categorical disciplinary lines. The SGAC had to include at least one individual recommended by the tobacco industry (2 were chosen). Ten researchers, including an epidemiologist (Leonard Schuman) and a biostatistician (William Cochran), both of whom were heavy smokers, were appointed to the committee.
The SGAC assembled the relevant evidence, developed criteria for evidence synthesis, and carefully considered alternative hypotheses to causation. The SGAC considered 3 main data sources: 1) animal experiments, 2) clinical and autopsy studies, and 3) epidemiologic studies. Each study was judged according to 1) its validity, 2) the extent to which the inferences were justified based on the data, and 3) its relevance to the committee's conclusions.
Before the evidence review, the SGAC decided upon the causal criteria of consistency of the association, strength of the association, specificity of the association, the temporal relationship of the association, and the coherence of the association (2). The 1964 report entailed synthesizing evidence across scientific disciplines, with epidemiologic studies (29 case-control studies and 7 cohort studies) comprising the bulk of the evidence, but also drawing upon basic science and pathologic research. On the basis of the evidence assessed according to these causal criteria, the Committee concluded that “cigarette smoking is causally related to lung cancer in men … The data for women, though less extensive, point in the same direction” (2, p. 196). Application of the causal framework to assess a body of scientific evidence in this transparent fashion was a novel model of the process of causal inference in public health (26) (Figure 1, stage 2).
As revealed by their internal business records, the tobacco industry carefully tracked the emerging scientific evidence. Rather than acknowledge what these records showed they knew to be true, they launched a massive, decades-long public relations campaign challenging the evidence with the deliberate intent to falsely reassure the public, especially current smokers, that the question of whether smoking caused harm was an “open controversy” (27). The tobacco industry attempted to alter the tenor of the scientific debate using various strategies (28), including funding prominent critics of this new epidemiologic causal framework such as R.A. Fisher (29) and Joseph Berkson. Even 20 years after the 1964 report was issued, critics funded by the tobacco industry were still publically questioning the causal framework (30).
FROM EVIDENCE TO ACTION
Epidemiology has important roots in the field of public health. In turn, public health is action-oriented; the identification of a causal association leads to an assessment of the importance of this determination in a public health context that considers the risks, benefits, and costs of intervention (Figure 1, stage 3). In keeping with this framework, the 1964 SGAC was also asked to judge whether the scope of the smoking and health problem warranted remedial action. A critical conclusion of the 1964 report was the finding that, “On the basis of prolonged study and evaluation of many lines of converging evidence, the Committee makes the following judgment: Cigarette smoking is a health hazard of sufficient importance in the United States to warrant appropriate remedial action” (2, p. 33).
The SGAC opted not to provide guidance on what the remedial action should be, but rather left this responsibility to Congress. The 1964 report conclusions were followed by a significant increase in awareness of the harms of cigarette smoking, a shift in public attitudes about smoking (31), and a persistent decline in per capita cigarette consumption after 1964 (32). In the following decade, the remedial action (Figure 1, stage 4) took the form of increasing efforts to regulate the use, sale, and advertising of tobacco products (33), such as placing warning labels on cigarette packs and written advertisements and implementing restrictions on radio/television advertising. By 1991, a comprehensive evidence-based national tobacco control plan was developed that included higher cigarette taxes, smoke-free workplaces, and anti-tobacco marketing in addition to individual-level smoking prevention and cessation interventions (34). The contributions of epidemiologists were not limited to etiologic research. Epidemiologists have contributed to tobacco control efforts in many ways. As it became clear that substantial public health benefits could be achieved by reducing smoking prevalence, some epidemiologists transitioned into the fields of behavioral and social epidemiology to contribute to the effort to control the epidemic of cigarette smoking by, for example, advancing the understanding of the origins of tobacco use and testing tobacco control intervention strategies.
SURGEON GENERAL REPORTS: AN ONGOING PROCESS
The 1964 report was a watershed moment in the history of epidemiology and public health, but it was only the beginning of the effort to apply this evidence-based public health model to the investigation of the health consequences of smoking. The 1964 report was not an official government report, but rather a report from the SGAC to the Surgeon General. However, it was published by the federal government. In fact, it is the only civilian nonmilitary document ever printed with a “top secret” classification. In 1965, Congress passed the federal Cigarette Labeling and Advertising Act, which required warning labels on cigarette packs and also mandated that the Secretary of the Department of Health, Education, and Welfare (now Health and Human Services) report annually to the Congress on current information about the health consequences of smoking. By tradition, these reports came to be known as “US Surgeon General Reports on the Health Consequences of Smoking.” These Congressionally mandated reports continued under the Public Health Cigarette Smoking Act of 1969 until 1998, when new legislation effectively eliminated all congressionally mandated reports, including the SGRs. The Department of Health and Human Services, however, recognized the value of these reports and has maintained the SGR process. Throughout this time span, the SGR process has remained true to the evidence-based public health framework, even though the report-writing procedures have varied over time.
Thus, the 1964 report set in motion a process that, through regular updates of the evidence, continues to more fully characterize what is known about the health effects of exposure to tobacco smoke. Repeatedly, epidemiologists have risen to the occasion to test new hypotheses or refine what is known about the health consequences of smoking and exposure to secondhand smoke (SHS). Consequently, the list of smoking-related health effects continues to grow over time.
SGRs on the health consequences of smoking were published regularly from 1967 through 1978 (35–44), with a 15-year anniversary report issued in 1979 (45) (Table 1). Reflecting the value of publishing focused reports to achieve greater depth of coverage on specific topics, some subsequent SGRs addressed more focused topics, such as smoking as a cause of specific diseases (46–49), smoking in women (50, 51), the changing cigarette (52), involuntary smoking (53, 54), smokeless tobacco use (55), nicotine addiction (56), the health benefits of smoking cessation (57), mechanisms of tobacco-caused pathogenesis (58), and tobacco control (59–61). The reports in 2004 (61) and 2014 (1) followed the format of updating the overall evidence of the health consequences of active smoking within the causal framework.
A notable example of the continual contribution of epidemiologists to advancing what is known about the health effects of exposure to cigarette smoke and the value of the SGRs within the evidence-based public health framework is again provided by the example of smoking and lung cancer, except this time with a focus on exposure to SHS. In 1971, Surgeon General Jesse Steinfeld proposed that “the non-smoker may have untoward effects from the pollution his smoking neighbor forces upon him” and called for a formal review of the evidence on the potential health effects of SHS for the 1972 SGR (34, p. 225). The results emphasized that additional research was needed to assess the potential health consequences of SHS exposure. In 1981, studies were published that described increased lung cancer risk among never-smoking women who were married to smokers (63– 65). Additional evidence rapidly accrued so that by the time the 1986 SGR was published (53), the evidence was judged to be sufficient to conclude that SHS was a cause of lung cancer. The conclusion that SHS exposure caused lung cancer had enormous policy implications. This broadened the population pool of those harmed by tobacco smoke from active smokers to also include nonsmokers who had been exposed to SHS, providing the evidence base to support legislation for smoke-free public places. This example again models the evidence-based public health framework: a new discovery that was then replicated by others in subsequent studies, determined to be causal via evidence synthesis within the causal framework and important enough to warrant intervention, followed by translation into policy change. The evidence on the health effects of SHS exposure posed a new and damaging threat to the tobacco industry, which persisted in contesting the science (66, 67).
WHERE ARE WE NOW?
The application of causal inference to the evidence via the SGRs has resulted in a lengthy list of diseases and health outcomes determined to be caused by exposure to tobacco smoke. Epidemiologists have repeatedly made major contributions to this knowledge over time by conducting research to address gaps in the evidence so that the presence or absence of causal associations could be more clearly distinguished. The accumulated scientific evidence, usually predominantly epidemiologic evidence, has been judged sufficient to conclude that active cigarette smoking is a cause of 1) 9 types of cancer, 2) cardiovascular disease (e.g., subclinical atherosclerosis, coronary heart disease, stroke), 3) chronic obstructive pulmonary disease, 4) acute respiratory illnesses (e.g., pneumonia), 5) respiratory effects (e.g., wheeze, dyspnea) and adverse impact on lung growth and function, 6) reproductive effects like growth inhibition (e.g., low birth weight), complications of pregnancy, preterm delivery, shortened gestation, and sudden infant death syndrome, and 7) a host of other health effects, such as nuclear cataract, hip fractures, and overall poorer health status even in the absence of clinical disease (61). Further, the evidence has been judged sufficient to conclude that SHS exposure is a cause of coronary heart disease, lung cancer, odor annoyance, and nasal irritation in adults (54). In children, SHS exposure is a cause of sudden infant death syndrome, lower respiratory illnesses, otitis media, middle ear effusion, more severe asthma, and respiratory effects (e.g., wheeze, dyspnea) (54).
What has been the end result of this attempt to curb the epidemic of cigarette smoking? As the deleterious health effects of cigarette smoking were recognized, a major public health accomplishment was the success of tobacco control efforts in curtailing the epidemic. In the United States, the prevalence of current smokers was more than halved between 1965 and 2010, from 42% to 19% (68). This decrease in smoking prevalence since 1964 is estimated to have averted 8 million deaths attributable to smoking in the United States (1). This accomplishment could be celebrated more fully as a public health triumph were it not for the fact that similar estimates indicate that double this number—20 million deaths—were caused by smoking during this same period (1). This latter figure underscores the preeminence of cigarette smoking as a public health threat. The magnitude of this threat is a function of 1) the fact that many of cigarette smoking's numerous deleterious health effects are often fatal and 2) the high prevalence of smoking. In the United States, more than 440,000 deaths per year are attributable to active and passive smoking (69). To reduce the enormous public health burden caused by cigarette smoking, improved and intensified tobacco control efforts are needed to accelerate progress toward reducing what can currently be characterized, alarmingly, as endemic levels of smoking prevalence.
Even with noteworthy tobacco control progress in countries in North America and Western Europe, the sobering news is that formidable challenges remain as tobacco industry strategies continue to evolve. The tobacco industry has proven to be a resource-rich and savvy public health foe. Through aggressive marketing in overseas markets, cigarette smoking continues to grow as a major threat to global public health (70).
In 2008, the number of newly diagnosed lung cancers in developing countries exceeded that in developed countries by 22% (71). The epidemic of tobacco addiction in China illustrates the ongoing trend of a shift in the global lung cancer burden from high-income Western countries to low- and middle-income countries. Because of the increase in the prevalence of current smoking in Chinese males that occurred decades ago, lung cancer mortality rates have already increased 27% between 1990 and 2010 (72), with continued increases projected.
The recent, rapid expansion of the marketplace for tobacco products and devices that deliver nicotine poses new challenges (73–77). Electronic cigarettes (or “e-cigarettes”) are non–tobacco-containing nicotine delivery devices that have experienced a rapid upsurge in use and are now marketed by the major US tobacco companies (73, 74). Monitoring this expansion in products and how the products are used (e.g., product switching, multiple use) and the harms and benefits associated with their use compared with tobacco cigarettes is critical to developing more effective tobacco control strategies.
The initial discovery of the adverse health effects of cigarette smoking was closely intertwined with an important period of development in epidemiologic research methods and framework for causal inference. The substantial body of evidence indicating that smoking was associated with lung cancer risk culminated in the conclusion in the 1964 report that smoking was a cause of lung cancer. Since then, the continual study of the associations between cigarette smoking and health outcomes and the ongoing synthesis of this evidence in subsequent SGRs have led to a long and growing list of smoking-caused deleterious health effects. Despite all that is known about its health consequences, cigarette smoking persists as one of the major global health crises of our time. This remains an evolving story, with the final chapter on the scourge of tobacco upon society yet to be written.
ACKNOWLEDGMENTS
Author affiliations: Hollings Cancer Center, Medical University of South Carolina, Charleston, South Carolina (Anthony J. Alberg, K. Michael Cummings); Department of Public Health Sciences, Medical University of South Carolina, Charleston, South Carolina (Anthony J. Alberg); US Public Health Service, 1962–2001 (retired) (Donald R. Shopland); and Department of Psychiatry and Behavioral Sciences (K. Michael Cummings), Medical University of South Carolina, Charleston, South Carolina.
This work was carried out with funding from the National Institutes of Health (P30 CA138313, UL1 RR029882).
Donald Shopland contributed to the 1964 Report of the Advisory Committee to the Surgeon General and all of the subsequent Surgeon General's reports related to tobacco issued to date.
Conflicts of interest: K. Michael Cummings provides expert testimony on the health effects of smoking and tobacco industry tactics in lawsuits filed against the tobacco industry. The other authors report no conflicts.
REFERENCES
- 1.US Department of Health and Human Services. The Health Consequences of Smoking: 50 Years of Progress: a Report of the Surgeon General. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2014. [PubMed] [Google Scholar]
- 2.US Department of Health, Education, and Welfare. Smoking and Health: Report of the Advisory Committee to the Surgeon General of the Public Health Service. Washington, DC: US Department of Health, Education, and Welfare, Public Health Service; 1964. (Public Health Service Publication No. 1103) [Google Scholar]
- 3.Kluger R. Ashes to Ashes: America's Hundred-year Cigarette War, the Public Health, and the Unabashed Triumph of Philip Morris. New York, NY: Vintage Books; 1997. [Google Scholar]
- 4.Proctor RN. The history of the discovery of the cigarette-lung cancer link: evidentiary traditions, corporate denial, global toll. Tob Control. 2012;21(2):87–91. doi: 10.1136/tobaccocontrol-2011-050338. [DOI] [PubMed] [Google Scholar]
- 5.Doll R. Conversation with Sir Richard Doll. Br J Addict. 1991;86(4):365–377. doi: 10.1111/j.1360-0443.1991.tb03410.x. [DOI] [PubMed] [Google Scholar]
- 6.Doll R, Hill AB. Smoking and carcinoma of the lung; preliminary report. Br Med J. 1950;2(4682):739–748. doi: 10.1136/bmj.2.4682.739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wynder EL, Graham EA. Tobacco smoking as a possible etiologic factor in bronchiogenic carcinoma; a study of 684 proved cases. J Am Med Assoc. 1950;143(4):329–336. doi: 10.1001/jama.1950.02910390001001. [DOI] [PubMed] [Google Scholar]
- 8.Levin ML, Goldstein H, Gerhardt PR. Cancer and tobacco smoking; a preliminary report. J Am Med Assoc. 1950;143(4):336–338. doi: 10.1001/jama.1950.02910390008002. [DOI] [PubMed] [Google Scholar]
- 9.Mills CA, Porter MM. Tobacco smoking habits and cancer of the mouth and respiratory system. Cancer Res. 1950;10(9):539–542. [PubMed] [Google Scholar]
- 10.Schrek R, Baker CH, Ballard GP, et al. Tobacco smoking as an etiologic factor in disease; cancer. Cancer Res. 1950;10(1):49–58. [PubMed] [Google Scholar]
- 11.Cornfield J. A method of estimating comparative rates from clinical data. Applications to cancer of the lung, breast, and cervix. J Natl Cancer Inst. 1951;11(6):1269–1275. [PubMed] [Google Scholar]
- 12.Mantel N, Haenszel W. Statistical aspects of the analysis of data from retrospective studies of disease. J Natl Cancer Inst. 1959;22(4):719–748. [PubMed] [Google Scholar]
- 13.Levin ML. The occurrence of lung cancer in man. Acta Unio Int Contra Cancrum. 1953;9(3):531–541. [PubMed] [Google Scholar]
- 14.Doll R, Hill AB. The mortality of doctors in relation to their smoking habits: a preliminary report. Br Med J. 1954;4877(1):1451–1455. doi: 10.1136/bmj.1.4877.1451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hammond EC, Horn D. Smoking and death rates: report on forty-four months of follow-up of 187,783 men. 2. Death rates by cause. J Am Med Assoc. 1958;166(11):1294–1308. doi: 10.1001/jama.1958.02990110030007. [DOI] [PubMed] [Google Scholar]
- 16.Dorn HF. Tobacco consumption and mortality from cancer and other diseases. Public Health Rep. 1959;74(7):581–593. [PMC free article] [PubMed] [Google Scholar]
- 17.Cornfield J. A statistical problem arising from retrospective studies. In: Neyman J, editor. Proceedings of the 3rd Berkeley Symposium on Mathematical Statistics and Probability. Vol. IV. Biology and Problems of Health. Berkeley, CA: University of California Press; 1956. pp. 135–148. [Google Scholar]
- 18.Hill AB. Observation and experiment. N Engl J Med. 1953;248(24):995–1001. doi: 10.1056/NEJM195306112482401. [DOI] [PubMed] [Google Scholar]
- 19.Cornfield J. Statistical relationships and proof in medicine. Am Stat. 1954;8(5):19–21. [Google Scholar]
- 20.Cornfield J, Haenszel, Hammond EC, et al. Smoking and lung cancer: recent evidence and a discussion of some questions. J Natl Cancer Inst. 1959;22(1):173–203. [PubMed] [Google Scholar]
- 21.Blackburn H, Labarthe D. Stories from the evolution of guidelines for causal inference in epidemiologic associations: 1953–1965. Am J Epidemiol. 2012;176(12):1071–1077. doi: 10.1093/aje/kws374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Evans AS. Causation and disease: the Henle-Koch postulates revisited. Yale J Biol Med. 1976;49(2):175–195. [PMC free article] [PubMed] [Google Scholar]
- 23.Medical Research Council. Tobacco smoking and cancer of the lung. Statement by the Medical Research Council. Br Med J. 1957;1(5034):1523–1524. [Google Scholar]
- 24.Report of study group on smoking and health: section on lung cancer. CA Cancer J Clin. 1958;8(2):57–61. doi: 10.3322/canjclin.8.2.57. [DOI] [PubMed] [Google Scholar]
- 25.Royal College of Physicians. Smoking and Health: Summary Report of the Royal College of Physicians of London on Smoking in Relation to Cancer of the Lung and Other Diseases. London, UK: Pitman Publishing Co.; 1962. [PubMed] [Google Scholar]
- 26.Parascandola M, Weed DL, Dasgupta A. Two Surgeon General's reports on smoking and cancer: a historical investigation of the practice of causal inference. Emerg Themes Epidemiol. 2006;3:1. doi: 10.1186/1742-7622-3-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cummings KM, Brown A, O'Connor R. The cigarette controversy. Cancer Epidemiol Biomarkers Prev. 2007;16(6):1070–1076. doi: 10.1158/1055-9965.EPI-06-0912. [DOI] [PubMed] [Google Scholar]
- 28.Bero LA. Tobacco industry manipulation of research. Public Health Rep. 2005;120(2):200–208. doi: 10.1177/003335490512000215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Stolley PD. When genius errs: R.A. Fisher and the lung cancer controversy. Am J Epidemiol. 1991;133(5):416–425. doi: 10.1093/oxfordjournals.aje.a115904. [DOI] [PubMed] [Google Scholar]
- 30.Burch PRJ. The Surgeon General's “epidemiologic criteria for causality.” A critique. J Chronic Dis. 1983;36(12):821–836. doi: 10.1016/0021-9681(83)90003-6. [DOI] [PubMed] [Google Scholar]
- 31.Cummings KM, Proctor RN. The changing public image of smoking in the United States: 1964–2014. Cancer Epidemiol Biomarkers Prev. 2014;23(1):32–36. doi: 10.1158/1055-9965.EPI-13-0798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Warner KE, Sexton DW, Gillespie BW, et al. Impact of tobacco control on adult per capita cigarette consumption in the United States. Am J Public Health. 2014;104(1):83–89. doi: 10.2105/AJPH.2013.301591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Warner KE. Effects of the antismoking campaign: an update. Am J Public Health. 1989;79(2):144–151. doi: 10.2105/ajph.79.2.144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.US Department of Health and Human Services. Bethesda, MD: US Department of Health and Human Services; 1991. Strategies to Control Tobacco Use in the United States: a Blueprint for Public Health Action in the 1990s. (NIH Pub. No. 92-3316) [Google Scholar]
- 35.US Department of Health, Education, and Welfare. The Health Consequences of Smoking: a Public Health Service Review: 1967. Washington, DC: US Department of Health, Education, and Welfare, Public Health Service; 1967. (Public Health Service Publication No. 1696) [Google Scholar]
- 36.US Department of Health, Education, and Welfare. The Health Consequences of Smoking: 1968 Supplement to the 1967 Public Health Service Review. Washington, DC: US Department of Health, Education, and Welfare, Public Health Service; 1968. (Public Health Service Publication No. 1696-1) [Google Scholar]
- 37.US Department of Health, Education, and Welfare. The Health Consequences of Smoking: 1969 Supplement to the 1967 Public Health Service Review. Washington, DC: US Department of Health, Education, and Welfare, Public Health Service; 1969. (Public Health Service Publication No. 1696-2) [Google Scholar]
- 38.US Department of Health, Education, and Welfare. The Health Consequences of Smoking: a Report of the Surgeon General: 1971. Washington, DC: US Department of Health, Education, and Welfare, Public Health Service; 1971. (DHEW Publication No. (HSM) 71-7513) [Google Scholar]
- 39.US Department of Health, Education, and Welfare. The Health Consequences of Smoking 1972. Washington, DC: US Department of Health, Education, and Welfare, Public Health Service, Health Services and Mental Health Association; 1972. (DHEW Publication No. (HSM) 72-7516) [Google Scholar]
- 40.US Department of Health, Education, and Welfare. The Health Consequences of Smoking. Washington, DC: US Department of Health, Education, and Welfare, Public Health Service, Health Services and Mental Health Administration; 1973. (DHEW Publication No. (HSM) 73-8704) [Google Scholar]
- 41.US Department of Health, Education, and Welfare. The Health Consequences of Smoking 1974. Washington, DC: US Department of Health, Education, and Welfare, Public Health Service; 1974. (DHEW Publication No. (CDC) 74-8704) [Google Scholar]
- 42.US Department of Health, Education, and Welfare. The Health Consequences of Smoking 1975. Atlanta, GA: US Department of Health, Education, and Welfare, Public Health Service, Centers for Disease Control; 1975. (DHEW Publication No. (CDC) 76-8704) [Google Scholar]
- 43.US Department of Health, Education, and Welfare. The Health Consequences of Smoking: a Reference Edition. Atlanta, GA: US Department of Health, Education, and Welfare, Public Health Service, Centers for Disease Control; 1976. (HEW Publication No. (CDC) 78-8357) [Google Scholar]
- 44.US Department of Health, Education, and Welfare. The Health Consequences of Smoking 1977–1978. Rockville, MD: US Department of Health, Education, and Welfare, Public Health Service, Office of the Assistant Secretary for Health, Office on Smoking and Health; 1978. (DHEW Publication No. (PHS) 79-50065) [Google Scholar]
- 45.US Department of Health, Education, and Welfare. Smoking and Health: a Report of the Surgeon General. Washington, DC: US Department of Health, Education, and Welfare, Public Health Service, Office of the Assistant Secretary for Health, Office on Smoking and Health; 1979. (DHEW Publication No. (PHS) 79-50066) [Google Scholar]
- 46.US Department of Health and Human Services. The Health Consequences of Smoking: Cancer: a Report of the Surgeon General. Rockville, MD: US Department of Health and Human Services, Public Health Service, Office on Smoking and Health; 1982. (DHHS Publication No. (PHS) 82-50179) [Google Scholar]
- 47.US Department of Health and Human Services. The Health Consequences of Smoking: Cardiovascular Disease: a Report of the Surgeon General. Rockville, MD: US Department of Health and Human Services, Public Health Service, Office on Smoking and Health; 1983. (DHHS Publication No. (PHS) 84-50204) [Google Scholar]
- 48.US Department of Health and Human Services. The Health Consequences of Smoking: Chronic Obstructive Lung Disease: a Report of the Surgeon General. Rockville, MD: US Department of Health and Human Services, Public Health Service, Office on Smoking and Health; 1984. [Google Scholar]
- 49.US Department of Health and Human Services. The Health Consequences of Smoking: Cancer and Chronic Lung Disease in the Workplace: a Report of the Surgeon General. Rockville, MD: US Department of Health and Human Services, Public Health Service, Office on Smoking and Health; 1985. (DHHS Publication No. (PHS) 85-50207) [Google Scholar]
- 50.US Department of Health and Human Services. The Health Consequences of Smoking for Women: a Report of the Surgeon General. Rockville, MD: US Department of Health and Human Services, Public Health Service, Office on Smoking and Health; 1980. [Google Scholar]
- 51.US Department of Health and Human Services. Women and Smoking: a Report of the Surgeon General. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention, Office on Smoking and Health; 2001. [Google Scholar]
- 52.US Department of Health and Human Services. The Health Consequences of Smoking: The Changing Cigarette: a Report of the Surgeon General. Rockville, MD: US Department of Health and Human Services, Public Health Service, Office on Smoking and Health; 1981. (DHSS Publication No. (PHS) 81-50156) [Google Scholar]
- 53.US Department of Health and Human Services. The Health Consequences of Involuntary Smoking: a Report of the Surgeon General. Rockville, MD: US Department of Health and Human Services, Public Health Service, Centers for Disease Control, Center for Health Promotion and Education, Office on Smoking and Health; 1986. (DHHS Publication No. (CDC) 87-8398) [Google Scholar]
- 54.US Department of Health and Human Services. The Health Consequences of Involuntary Exposure to Tobacco Smoke: a Report of the Surgeon General. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention, Office on Smoking and Health; 2006. [Google Scholar]
- 55.US Department of Health and Human Services. The Health Consequences of Using Smokeless Tobacco: a Report of the Advisory Committee to the Surgeon General. Bethesda, MD: US Department of Health and Human Services, Public Health Service; 1986. (NIH Publication No. 86-2874) [Google Scholar]
- 56.US Department of Health and Human Services. The Health Consequences of Smoking: Nicotine Addiction: a Report of the Surgeon General. Rockville, MD: US Department of Health and Human Services, Public Health Service, Centers for Disease Control, Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 1988. (DHHS Publication No. (CDC) 88-8406) [Google Scholar]
- 57.US Department of Health and Human Services. The Health Benefits of Smoking Cessation: a Report of the Surgeon General. Atlanta, GA: US Department of Health and Human Services, Public Health Service, Centers for Disease Control, Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 1990. (DHHS Publication No. (CDC) 90-8416) [Google Scholar]
- 58.US Department of Health and Human Services. How Tobacco Smoke Causes Disease: The Biology and Behavioral Basis for Smoking-Attributable Disease: A Report of the Surgeon General. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention, Office on Smoking and Health; 2010. [Google Scholar]
- 59.Centers for Disease Control and Prevention. Preventing Tobacco Use Among Young People: a Report of the Surgeon General. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 1994. [Google Scholar]
- 60.US Department of Health and Human Services. Reducing Tobacco Use: a Report of the Surgeon General. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2000. [Google Scholar]
- 61.US Department of Health and Human Services. Preventing Tobacco Use Among Youth and Young Adults: a Report of the Surgeon General. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention, Office on Smoking and Health; 2012. [Google Scholar]
- 62.US Department of Health and Human Services. The Health Consequences of Smoking: a Report of the Surgeon General. Atlanta, GA: Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2004. [Google Scholar]
- 63.Hirayama T. Non-smoking wives of heavy smokers have a higher risk of lung cancer: a study from Japan. Br Med J (Clin Res Ed) 1981;282(6259):183–185. doi: 10.1136/bmj.282.6259.183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Trichopoulos D, Kalandidi A, Sparros L, et al. Lung cancer and passive smoking. Int J Cancer. 1981;27(1):1–4. doi: 10.1002/ijc.2910270102. [DOI] [PubMed] [Google Scholar]
- 65.Garfinkel L. Time trends in lung cancer mortality among nonsmokers and a note on passive smoking. J Natl Cancer Inst. 1981;66(6):1061–1066. doi: 10.1093/jnci/66.6.1061. [DOI] [PubMed] [Google Scholar]
- 66.Muggli ME, Hurt RD, Repace J. The tobacco industry's political efforts to derail the EPA report on ETS. Am J Prev Med. 2004;26(2):167–177. doi: 10.1016/j.amepre.2003.10.015. [DOI] [PubMed] [Google Scholar]
- 67.De Camargo KR., Jr How to identify science being bent: the tobacco industry's fight to deny second-hand smoking health hazards as an example. Soc Sci Med. 2012;75(7):1230–1235. doi: 10.1016/j.socscimed.2012.03.057. [DOI] [PubMed] [Google Scholar]
- 68.National Center for Health Statistics. Hyattsville, MD: US Department of Health and Human Services; 2011. Health, United States, 2010: With Special Feature on Death and Dying. [PubMed] [Google Scholar]
- 69.Centers for Disease Control and Prevention (CDC) Smoking-attributable mortality, years of potential life lost, and productivity losses—United States, 2000–2004. MMWR Morb Mortal Wkly Rep. 2008;57(45):1226–1228. [PubMed] [Google Scholar]
- 70.Bartecchi CE, MacKenzie TD, Schrier RW. The global tobacco epidemic. Sci Am. 1995;272(5):44–51. doi: 10.1038/scientificamerican0595-44. [DOI] [PubMed] [Google Scholar]
- 71.Jemal A, Bray F, Center MM, et al. Global cancer statistics. CA Cancer J Clin. 2011;61(2):69–90. doi: 10.3322/caac.20107. [DOI] [PubMed] [Google Scholar]
- 72.Yang G, Wang Y, Zeng Y, et al. Rapid health transition in China, 1990–2010: findings from the Global Burden of Disease Study 2010. Lancet. 2013;381(9882):1987–2015. doi: 10.1016/S0140-6736(13)61097-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Popova L, Ling PM. Alternative tobacco product use and smoking cessation: a national study. Am J Public Health. 2013;103(5):923–930. doi: 10.2105/AJPH.2012.301070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Kamerow D. Big Tobacco lights up e-cigarettes. BMJ. 2013;346:f3418. doi: 10.1136/bmj.f3418. [DOI] [PubMed] [Google Scholar]
- 75.Schuster RM, Hertel AW, Mermelstein R. Cigar, cigarillo, and little cigar use among current cigarette-smoking adolescents. Nicotine Tob Res. 2013;15(5):925–931. doi: 10.1093/ntr/nts222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Jawad M, McEwen A, McNeill A, et al. To what extent should waterpipe tobacco smoking become a public health priority? Addiction. 2013;108(11):1873–1884. doi: 10.1111/add.12265. [DOI] [PubMed] [Google Scholar]
- 77.Centers for Disease Control and Prevention (CDC) Consumption of cigarettes and combustible tobacco—United States, 2000–2011. MMWR Morb Mortal Wkly Rep. 2012;61(30):565–569. [PubMed] [Google Scholar]
- 78.US Department of Health and Human Services. Reducing the Health Consequences of Smoking: 25 Years of Progress: a Report of the Surgeon General. Rockville, MD: US Department of Health and Human Services, Public Health Service, Centers for Disease Control, Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 1989. (DHHS Publication No. (CDC) 89-8411) [Google Scholar]
- 79.US Department of Health and Human Services. Smoking and Health in the Americas: a 1992 Report of the Surgeon General, in Collaboration With the Pan American Health Organization. Atlanta, GA: US Department of Health and Human Services, Public Health Service, Centers for Disease Control, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 1992. (DHHS Publication No. (CDC) 92-8419) [Google Scholar]
- 80.US Department of Health and Human Services. Tobacco Use Among U.S. Racial/Ethnic Minority Groups—African Americans, American Indians and Alaska Natives, Asian Americans and Pacific Islanders, and Hispanics: a Report of the Surgeon General. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 1998. [Google Scholar]


