Abstract
Background:
Rotator cuff disease is a common cause of shoulder pain. There are studies about the effectiveness of sodium hyaluronate injection on shoulder and knee pain, but few studies demonstrating the efficacy of sodium hyaluronate ultrasonography guided injection for rotator cuff disease. This study evaluates effectiveness of ultrasonography guided subacromial sodium hyaluronate injection in patients with impingment syndrome without rotator cuff complete tear.
Materials and Methods:
This prospective, double-blind, placebo controlled clinical trial study was performed among 40 patients with subacromial impingement syndrome without complete tear of rotator cuff. Patients randomly injected ultrasonography guided in 2 groups: Case group by 20 mg of sodium hyaluronate (Fermathron™) and control group by 0.9% normal saline. Both groups received 3 weekly injections. The pain score (100 mm visual analogue score [VAS]) was evaluated before first injection and one week after each injection. The constant score was evaluated before first and 12 week after last injection. Data was analyzed statistically by Independent t-test.
Results:
In both groups mean VAS has decreased, but more significantly in case group (P < 0.001). Mean constant score was significantly higher in case group 12 weeks after last injection (P < 0.001). The constant score improved 12 weeks after the last injection in both groups with a significantly better result in case group (P < 0.001).
Conclusion:
Subacromial injections of sodium hyaluronate are effective in treating rotator cuff disease without complete tears.
Keywords: Constant score, rotator cuff disease, sodium hyaluronate, subacromial injections, ultrasonography guided
INTRODUCTION
Shoulder pain accounts for approximately 3 million visits to physicians each year in the United States, and of these, rotator cuff disease is the most common cause of shoulder pain necessitating a visit to a primary care physician.[1] Rotator cuff disease in particular is a common cause of shoulder pain and weakness and comprises a significant proportion of the musculoskeletal complaints presenting to primary care doctors.[2]
Treatments for rotator cuff lesions without complete tears are mainly conservative[3] and surgery should be considered if the patient fails to improve with a progressive non-operative therapy program of 3-6 months.[4] Subacromial injection of anesthetics or corticosteroids is often used to treat patients with persistent symptoms after rehabilitation and use of non-steroidal anti-inflammatory drugs.[5] In patients who have failed conservative treatment, there is evidence that viscosupplementation is beneficial for the treatment of knee pain caused by osteoarthritis.[6] In a study, evaluating rehabilitative and infiltrative treatment with hyaluronic acid in elderly patients with rotator cuff tears found statistically significant results, both for the reduction of pain and for the improvement of range of motion and autonomy in daily life activities.[7] In one large placebo-controlled, randomized trial of 660 patients with moderate to severe shoulder pain caused by osteoarthritis, rotator cuff tear, or adhesive capsulitis, a significant improvement in pain relief was found in all groups up to 13 weeks after viscosupplementation.[6] Another study demonstrated that sodium hyaluronate injection is effective for the treatment of osteoarthritis and persistent shoulder pain that is refractory to other conservative measurements.[8] Thirty patients with symptomatic osteoarthritis of the shoulder who failed conservative treatment and were treated with intraarticular viscosupplementation demonstrated improvement in function and pain levels.[9] Treatment with sodium hyaluronate is emerging as an alternative intraarticular regimen for osteoarthritic knee joints.[10,11] Clinical studies have reported the efficacy of hyaluronate injection in treating shoulder pain.[12,13,14] In a randomized study, sodium hyaluronate was found to be effective for patients with rotator cuff tears.[15]
Ultrasound is a readily available and cheap modality for looking more specifically at the rotator cuff and surrounding structures.[1] More recently, ultrasound guidance has become a commonly employed method to perform diagnostic or therapeutic interventions.[16]
Despite the long history and the fact that this is a common diagnosis made in clinical practice, the exact cause and best treatment for rotator cuff disease still are being explored. Although, there are very few high-quality studies demonstrating the efficacy of sodium hyaluronate injection for rotator cuff disease, this study was performed to examine the effect of ultrasound-guided subacromial sodium hyaluronate injection in patients with impingement syndrome without rotator cuff complete tear.
MATERIALS AND METHODS
This was a prospective, randomized, double-blind, placebo controlled clinical trial involved 48 patients with subacromial impingement syndrome without a complete tear of rotator cuff. Eight patients were excluded because of protocol violation. The reasons were violation of the selection criteria and refused injection. We included patients between 30 and 80 years old who had shoulder pain, a positive Neer and Hawkins sign, and a positive ultrasonographic diagnosis of rotator cuff pathology without a complete tear, who did not respond to conservative treatments or rehabilitation for at least 6 months and signed the informed consent form. We excluded patients who (1) had any rheumatic disease, glenohumeral osteoarthritis, full-thickness rotator cuff tears, fractures, diabetes mellitus, infections, or tumors, (2) had hypersensitivity to hyaluronate, (3) had participated in any other study within 6 months, (4) had received a subacromial injection within 8 weeks, (5) were pregnant or planned to become pregnant, (6) were at risk of complications of intra-articular injections such as patients who received anti-coagulant drugs. Forty patients randomly allocated in 2 groups: Hyaluronate injection (case group) and normal saline injection (placebo group). According to demographic data gender and age, there were no significant differences between two groups. The test drug was Fermathron™, 20 mg/2 ml of sodium hyaluronate. The placebo was 0.9% normal saline solution, at 2 mL/syringe. Both groups received 3 weekly injections in a same protocol.
All patients screened for complete tear of rotator cuff with ultrasonography and all injections were performed under ultrasonography guidance. Ultrasonography with a high-frequency (7-15 MHz) linear-array probe was performed by one radiologist with a SIEMENS G60 (SIEMENS G 60s, MODEL: 7474922 made in Japan march 2006) device.
Sonographer stood behind the patient, scanning over its shoulder. The long head of biceps tendon was examined within the intertubercular groove, in both the transverse and longitudinal planes, with the patient's arm in a neutral position and the elbow flexed to 90°. The presence of fluid around the tendon was noted, and a search for fluid in the subdeltoid bursa was made. With the shoulder externally rotated, the subscapularis tendon was brought into view and examined in both planes. Then, the patient was asked to rotate the shoulder internally. This movement was achieved either by placing the forearm behind the back with the palm facing posteriorly or by placing the palm on the upper buttock. The supraspinatus and infraspinatus tendons were evaluated in this position in both the transverse and longitudinal planes.
The examination was completed by requesting the patient to place a hand on the contralateral shoulder. This position allowed further assessment of the infraspinatus tendon if required. With ultrasound, the normal tendon was an echoic structure, whereas the cartilage and fluids were hypoechoic. Tendinitis was diagnosed when the tendon lost its echogenicity and became diffusely hypoechoic.[17,18,19] Dynamic evaluation of abduction was performed by observing the supraspinatus tendon and bursa longitudinally as they retract deep to the coracoacromial ligament. Bunching of tissue or buckling of the ligament correlated with impingement.
If ultrasonographic evidence of full-thickness supraspinatus tendon tear was seen, patient excluded from our study. These features included non-visualization of the distal supraspinatus tendon and dipping of the deltoid muscle or abnormal anechoic disruption of the supraspinatus tendon, which extended from the articular to the bursa surface. The diagnosis of a partial rotator cuff tear was made when the hypoechoic or bursal herniation did not cross the full width of the tendon.[17,18,19]
Ultrasound guided injection was done from a lateral approach. We used 21 gage needle for injection of 2cc Fermathron™. As long as the needle was kept in the same axial plane as the probe, it followed accurately until reached the superficial surface of the supraspinatus tendon. A preliminary injection in this location confirmed the correct positioning in the bursa as evident by rapid flow of injected material away from the needle tip. After insurance firm placement within the bursa, injection was completed.
The pain score (100 mm visual analog score [VAS]) was evaluated blindly by the different physiatrists before the first injection and 1 week after each injection. The constant score[20] of shoulder also was evaluated blindly before the first injection and 12 week after last injection. A constant score of 80 points or more or an improvement in the constant score by 10 points or more was considered satisfactory.
Statistical analyses were performed using the SPSS statistical package version 13.0 (SPSS Inc., Chicago, IL, USA). Independent sample t-test or Mann-Whitney U-test, paired t-test or Repeated Measure ANOVA test, and Chi-square test were used to assess the differences between stages, as appropriate. A P < 0.05 was considered significant.
RESULTS
In this study, there were 20 patients in each group, in case group there were 8 male (40%) and 12 females (60%) and the placebo group contained 6 males (30%) and 14 females (70%). Chi-square test showed that they did not differ significantly in gender.
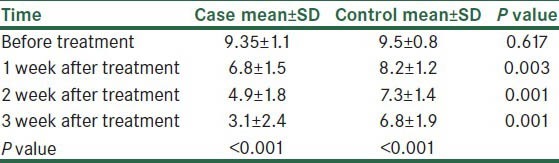
Using Independent t-test, revealed that mean VAS scores did not differ significantly before treatment (P = 0.617) but 1 week after the first, second and third injection (W1, W2 and W3) mean VAS was significantly lower in case group (P < 0.05). In both groups mean VAS has decreased every week during the treatment but this decrement significantly was more in case group (P < 0.001) [Table 1].
Table 1.
Comparison of visual analog scores before and after treatment within and between the two groups
Although, it showed that there were no significant differences between 2 groups in mean constant score before treatment (P = 0.4) but mean constant score was significantly higher in case group 12 weeks after the last injection (P < 0.001). The constant score improved at the 12 weeks after the last injection in both groups, although the independent t-test revealed significantly better results in case group (P < 0.001) [Table 2].
Table 2.
Comparison of constant scores before and after treatment within and between the two groups

No complications such as flare reaction, infection, hemarthrosis and synovitis were reported by the patients in either group. Of the patients in the placebo group 15 had additional sodium hyaluronate injections and 6 were unavailable for follow-up. The remaining patients were satisfied with their results so hadn’t any additional procedures.
Of the patients in the case group, 2 had additional injections 6 months after the last injection, 8 were lost to follow-up and the remaining satisfied with their results.
DISCUSSION
The literature on the efficacy of intraarticular viscosupplementation is primarily focused on the knee, with limited studies of other joints. Although, the literature covering visco supplementation for knee osteoarthritis has been conflicting and has a known publication bias,[21,22] meta-analyses suggest an improvement in pain compared with placebo.[22] In patients who have failed conservative treatment, there is evidence that visco supplementation is beneficial for the treatment of knee pain caused by osteoarthritis.[21,22]
The clinical effects of sodium hyaluronate on pain associated with osteoarthritis of the knee are probably mediated by several factors. In vitro and in vivo studies indicate that sodium hyaluronate can enhance prostaglandin synthesis and prevent its release from the cell matrix. Regarding inflammation, sodium hyaluronate suppresses the production and activity of pro-inflammatory mediators and proteases as well as altering the function of certain immune cells. Histological evidence shows that sodium hyaluronate prevents the degradation of cartilage and may promote its regeneration.[23]
Chou et al. performed a randomized, double-blind, placebo-controlled study of sodium hyaluronate (ARTZ Dispo) treatment in 51 patients with rotator cuff lesions without complete tears. They had injections of 25 mg/wk. of sodium hyaluronate into the subacromial bursa for 5 consecutive weeks in case group and 2.5 ml of normal saline with the same injection protocol for control group.[24] We performed the study with patients and all the injections were performed ultrasound guided. Additionally, instead of 5 injections, we treated our patients with 3 injections of sodium hyaluronate. The results were the same.
A recent study assessed the hypothesis that injection of high-molecular weight hyaluronate in the treatment of subacromial impingement syndrome is effective and sodium hyaluronate, compared with corticosteroid injection in the shoulder joint. They found that subacromial hyaluronate injection to treat impingement syndrome produces similar pain and functional improvement to corticosteroid at a short-term follow-up.[25]
The probable mechanism of action of sodium hyaluronate is an autocrine stimulation of its own synthesis in a positive feedback manner in synoviocytes that has been shown in vitro.[26,27]
In our study, the case group had significantly better constant scores than the placebo group at the 12th week after the last injection and improvement of VAS scores each week after the injections. It shows that although the injection of normal saline solution into the subacromial bursa may relieve the symptoms of impingement syndrome but the results are not constant. Furthermore, we know that signs and symptoms of rotator cuff disease may relieve gradually if extrinsic and intrinsic factors are stabilized by resting or modification of activity.[28] It may be the cause of some degree of improvement after placebo injection. Another theory is removing inflammatory mediators by normal saline. Sodium hyaluronate may have inhibitory effect on the function of inflammatory cells and it may account for the deactivation of pain receptors.
In summary, Sodium hyaluronate may contribute to healing and pain reduction in rotator cuff disease. Further studies are required to find the exact mechanisms of action of this drug.
ACKNOWLEDGMENT
It has been registered in www.clinicaltrials.gov. The identifier is NCT01735058.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Praemer AF, Rice D. Vol. 2. Rosemont, IL: American Academy of Orthopaedic Surgeons; 1999. Musculoskeletal conditions in the United States; pp. 27–33. [Google Scholar]
- 2.Lin JC, Weintraub N, Aragaki DR. Nonsurgical treatment for rotator cuff injury in the elderly. J Am Med Dir Assoc. 2008;9:626–32. doi: 10.1016/j.jamda.2008.05.003. [DOI] [PubMed] [Google Scholar]
- 3.Andrews JR. Diagnosis and treatment of chronic painful shoulder: Review of nonsurgical interventions. Arthroscopy. 2005;21:333–47. doi: 10.1016/j.arthro.2004.11.003. [DOI] [PubMed] [Google Scholar]
- 4.Frontera WR, Silver JK, Rizzo TD. 2nd ed. Philadelphia: Saunders; 2008. Rotator cuff tendinitis. Essentials of Physical Medicine and Rehabilitation; p. 75. [Google Scholar]
- 5.Meloni F, Milia F, Cavazzuti M, Doria C, Lisai P, Profili S, et al. Clinical evaluation of sodium hyaluronate in the treatment of patients with sopraspinatus tendinosis under echographic guide: Experimental study of periarticular injections. Eur J Radiol. 2008;68:170–3. doi: 10.1016/j.ejrad.2007.11.001. [DOI] [PubMed] [Google Scholar]
- 6.Braddom RL. Physical Medicine and Rehabilitation. 4th ed. Philadelphia: Saunders; 2011. Peripheral joint and soft tissue injection techniques; p. 520. [Google Scholar]
- 7.Costantino C, Olvirri S. Rehabilitative and infiltrative treatment with hyaluronic acid in elderly patients with rotator cuff tears. Acta Biomed. 2009;80:225–9. [PubMed] [Google Scholar]
- 8.Blaine T, Moskowitz R, Udell J, Skyhar M, Levin R, Friedlander J, et al. Treatment of persistent shoulder pain with sodium hyaluronate: A randomized, controlled trial. A multicenter study. J Bone Joint Surg Am. 2008;90:970–9. doi: 10.2106/JBJS.F.01116. [DOI] [PubMed] [Google Scholar]
- 9.Silverstein E, Leger R, Shea KP. The use of intra-articular hylan G-F 20 in the treatment of symptomatic osteoarthritis of the shoulder: A preliminary study. Am J Sports Med. 2007;35:979–85. doi: 10.1177/0363546507300256. [DOI] [PubMed] [Google Scholar]
- 10.Wu JJ, Shih LY, Hsu HC, Chen TH. The double-blind test of sodium hyaluronate (ARTZ) on osteoarthritis knee. Zhonghua Yi Xue Za Zhi (Taipei) 1997;59:99–106. [PubMed] [Google Scholar]
- 11.Dahl LB, Dahl IM, Engström-Laurent A, Granath K. Concentration and molecular weight of sodium hyaluronate in synovial fluid from patients with rheumatoid arthritis and other arthropathies. Ann Rheum Dis. 1985;44:817–22. doi: 10.1136/ard.44.12.817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Itokazu M, Matsunaga T. Clinical evaluation of high-molecular-weight sodium hyaluronate for the treatment of patients with periarthritis of the shoulder. Clin Ther. 1995;17:946–55. doi: 10.1016/0149-2918(95)80072-7. [DOI] [PubMed] [Google Scholar]
- 13.Takagishi N, Minamikawa H, Iwamoto H, Kida H, Okuyama S, Tanaka M, et al. Clinical evaluation of SPH (high molecular weight sodium hyaluronate) on periarthritis of the shoulder. Jpn J Pharmacol Ther. 1998;16:3553–67. [Google Scholar]
- 14.Yamamoto R, Namiki O, Iwata H, Shinmei M, Mikasa M, Ogawa N. Randomized cooperative study of sodium hyaluronate (SPH) on perarthritis scapulohumeralis. Jpn J Pharmacol Ther. 1988;19:713–33. [Google Scholar]
- 15.Shibata Y, Midorikawa K, Emoto G, Naito M. Clinical evaluation of sodium hyaluronate for the treatment of patients with rotator cuff tear. J Shoulder Elbow Surg. 2001;10:209–16. doi: 10.1067/mse.2001.113501. [DOI] [PubMed] [Google Scholar]
- 16.Adler RS, Sofka CM. Percutaneous ultrasound-guided injections in the musculoskeletal system. Ultrasound Q. 2003;19:3–12. doi: 10.1097/00013644-200303000-00002. [DOI] [PubMed] [Google Scholar]
- 17.Kluger R, Mayrhofer R, Kröner A, Pabinger C, Pärtan G, Hruby W, et al. Sonographic versus magnetic resonance arthrographic evaluation of full-thickness rotator cuff tears in millimeters. J Shoulder Elbow Surg. 2003;12:110–6. doi: 10.1067/mse.2003.10. [DOI] [PubMed] [Google Scholar]
- 18.Kim HA, Kim SH, Seo YI. Ultrasonographic findings of painful shoulders and correlation between physical examination and ultrasonographic rotator cuff tear. Mod Rheumatol. 2007;17:213–9. doi: 10.1007/s10165-007-0577-8. [DOI] [PubMed] [Google Scholar]
- 19.Teefey SA, Petersen B, Prather H. Shoulder Ultrasound vs MRI for rotator cuff pathology. PM R. 2009;1:490–5. doi: 10.1016/j.pmrj.2009.03.013. [DOI] [PubMed] [Google Scholar]
- 20.Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987;214:160–4. [PubMed] [Google Scholar]
- 21.Bellamy N, Campbell J, Robinson V, Gee T, Bourne R, Wells G. Viscosupplementation for the treatment of osteoarthritis of the knee. Cochrane Database Syst Rev. 2006;19:CD005321. doi: 10.1002/14651858.CD005321.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lo GH, LaValley M, McAlindon T, Felson DT. Intra-articular hyaluronic acid in treatment of knee osteoarthritis: A meta-analysis. JAMA. 2003;290:3115–21. doi: 10.1001/jama.290.23.3115. [DOI] [PubMed] [Google Scholar]
- 23.Moreland LW. Intra-articular hyaluronan (hyaluronic acid) and hylans for the treatment of osteoarthritis: Mechanisms of action. Arthritis Res Ther. 2003;5:54–67. doi: 10.1186/ar623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chou WY, Ko JY, Wang FS, Huang CC, Wong T, Wang CJ, et al. Effect of sodium hyaluronate treatment on rotator cuff lesions without complete tears: A randomized, double-blind, placebo-controlled study. J Shoulder Elbow Surg. 2010;19:557–63. doi: 10.1016/j.jse.2009.08.006. [DOI] [PubMed] [Google Scholar]
- 25.Kim YS, Park JY, Lee CS, Lee SJ. Does hyaluronate injection work in shoulder disease in early stage? A multicenter, randomized, single blind and open comparative clinical study. J Shoulder Elbow Surg. 2012;21:722–7. doi: 10.1016/j.jse.2011.11.009. [DOI] [PubMed] [Google Scholar]
- 26.Ghosh P. The role of hyaluronic acid (hyaluronan) in health and disease: Interactions with cells, cartilage and components of synovial fluid. Clin Exp Rheumatol. 1994;12:75–82. [PubMed] [Google Scholar]
- 27.Rosier RN, O’Keefe RJ. Hyaluronic acid therapy. Instr Course Lect. 2000;49:495–502. [PubMed] [Google Scholar]
- 28.Ko JY, Huang CC, Chen WJ, Chen CE, Chen SH, Wang CJ. Pathogenesis of partial tear of the rotator cuff: A clinical and pathologic study. J Shoulder Elbow Surg. 2006;15:271–8. doi: 10.1016/j.jse.2005.10.013. [DOI] [PubMed] [Google Scholar]


