Abstract
Objective
In order to understand the conflicting information on temporomandibular joint (TMJ) pathophysiologic responses after mandibular advancement surgery, an overview of the literature was proposed with a focus on certain risk factors.
Methods
A literature search was carried out in the Cochrane, PubMed, Scopus and Web of Science databases in the period from January 1980 through March 2013. Various combinations of keywords related to TMJ changes [disc displacement, arthralgia, condylar resorption (CR)] and aspects of surgical intervention (fixation technique, amount of advancement) were used. A hand search of these papers was also carried out to identify additional articles.
Results
A total of 148 articles were considered for this overview and, although methodological troubles were common, this review identified relevant findings which the practitioner can take into consideration during treatment planning: 1- Surgery was unable to influence TMJ with preexisting displaced disc and crepitus; 2- Clicking and arthralgia were not predictable after surgery, although there was greater likelihood of improvement rather than deterioration; 3- The amount of mandibular advancement and counterclockwise rotation, and the rigidity of the fixation technique seemed to influence TMJ position and health; 4- The risk of CR increased, especially in identified high-risk cases.
Conclusions
Young adult females with mandibular retrognathism and increased mandibular plane angle are susceptible to painful TMJ, and are subject to less improvement after surgery and prone to CR. Furthermore, thorough evidenced-based studies are required to understand the response of the TMJ after mandibular advancement surgery.
Keywords: Temporomandibular joint, Orthognathic surgery, Mandibular advancement, Bone resorption
INTRODUCTION
Temporomandibular joint (TMJ) response to mandibular advancement surgery is sporadically associated to arthralgia (pain), functional limitations, condylar resorption and skeletal relapse. When the mandible is advanced and fixed, the adjacent tissues are stretched and tend to displace the distal segment back toward its original position46,54,96,97. This response to mandibular advancement is countered bilaterally by the TMJs and may contribute to less stability76.
The adverse effects of mandibular advancement surgery on the TMJs form a pertinent theme well explored in the literature5,7,20,29,56,65,81,99,104,105,134,138,139,142. The TMJ response ranged from adaptive, which included physiological bone remodeling28,34,45, to irreversible complications9,10,55. Undesired TMJ responses to treatments in both short and long-term follow-up periods, such as condyle torque14,138, joint sounds (clicking, popping, crepitus)53, deteriorated discomfort and pain107,141, deviated or limited mouth opening55,96,138, and condylar resorption (CR)29,81,96 have all been reported. However, the limitations and heterogeneity of the studies cannot be overlooked, and because the TMJ response is of multifactorial origin and there is a wide range of individual variability as well as different surgical techniques, there is still controversy as to whether mandible advancement surgery is detrimental to the TMJ. Systematic reviews published in this field found an intermediate degree of evidence and proved inconclusive1,6,76,77. Moreover, for ethical reasons, randomized clinical trial designs involving surgery are limited.
In order to understand the conflicting information on the TMJ response to mandibular advancement surgery and to allow the practitioner to take this into consideration during treatment planning, this overview centered on five risk factors: disk displacement, arthralgia, CR, mandibular fixation techniques, and the amount of mandibular advancement.
METHODS
Criteria for including studies in this review
High-quality research, such as randomized clinical trials, systematic reviews and meta-analysis, is uncommon in the surgical field, despite current high levels of emphasis on evidence-based Dentistry. Hence, intermediate degrees of evidence were found in systematic reviews published on this theme1,6,76,77. Although the issue in this research refers to intervention, the study design pertained to a wider spectrum of studies, which included animal searches, serial cases, updates and observational studies on temporomandibular disorders (TMD), comprising a narrative review (non-systematic review).
Search strategy
Publications were identified through searches of the following databases: Cochrane, PubMed, Scopus and Web of Science in the period from January 1980 through March 2013. Databases were searched for papers published in English. The following search terms were used and combined (AND): "condylar resorption", "mandibular advancement surgery", "rigid internal fixation" (RIF), "sagittal split ramus osteotomy" (SSRO), "temporomandibular disorder" (TMD), and "relapse". In addition, a hand search of the reference lists was carried out to identify additional papers.
Data synthesis
Data was pooled into evidence tables and grouped according to the subjects (1-articular disc displacement, 2- arthralgia, 3- CR, 4- mandibular fixation techniques, and 5- amount of advancement). The study design was identified and a descriptive summary was performed.
RESULTS
This overview comprised a total of 148 articles. Retrospective and prospective clinical studies involving TMJ and mandibular advancement surgery were classified and distributed according to the above-mentioned subjects, and shown in Table 1.
Table 1.
Classification and distribution of retrospective and prospective clinical studies
| Category | Number of papers (n) | References | Percentage (%) |
| 1. Articular disc displacement/Clicking | 6 | 6,56,62,103,106,144 | 7.3 |
| 2. Arthralgia (TMJ pain) | 23 | 1,6,12,20,29,32,33,37,49,62,78,88,101,104,107,108,109,115,120,124,141,142,146 | 28 |
| 3. Condylar remodeling and resorption | 12 | 11,29,68,69,70,72,73,74,79,82,91,134 | 14.6 |
| 4. Mandibular fixation techniques | 14 | 16,18,19,20,22,23,31,49,51,55,62,119,12,138 | 17.1 |
| 5. Amount of mandibular advancement | 9 | 11,18,19,23,29,42,119,135,138 | 11 |
| 6. Others (releapse and condylar position) | 18 | 4,7,14,15,21,28,38,40,64,65,66,78,94,95,9,126,131,140 | 22 |
TMJ=temporomandibular joint
Articular disc displacement
Disc displacement (or internal derangement) is subdivided into disc displacement with and without reduction and the latter is further subdivided into with or without limited mouth opening40. Disc displacement with reduction and no further signs or symptoms is considered not clinically relevant127. Anterior and medial or lateral disc displacement is the most common TMJ disorder in people in general and seems to be more prevalent in patients with dentofacial deformity30,63,88,130,146,147.
Arthralgia is not always followed by disc displacement, but noise (clicking) or restricted mouth opening are the most frequently found clinical signs. Clicking and arthralgia have been proven to fluctuate over time89, and, because of this complex interaction, a wide range (26 to 97%) of disc displacement has been found in asymptomatic patients seeking orthognathic surgery2,30,54,88,147. No association was seen between disc displacement, pain and the type of dentofacial deformity30.
The relationship between disc displacement and degenerative bony changes has still not been fully clarified. There is a consensus that the natural progression of disc displacement with reduction precedes disc displacement without reduction, but the natural progression of the joint disc displacement in CR has not been well defined83. The clinical signs and symptoms of anterior disc displacement without reduction tended to alleviate during the natural course of the condition83,118, except for a quarter of patients who showed no improvement after 2.5 years of follow-up, but there was no deterioration either or change in CR during this period of time83. Disc displacement and CR probably often occur simultaneously, but are considered independent disorders, with CR being trigged by other factors, including age82,83.
Systematic reviews on temporomandibular disorder (TMD) both before and after orthognathic surgery have also reported a heterogeneous study design and controversial results1,6. Hackney, et al.61(1989) did not find any significant difference in the incidence of TM pain or clicking following bilateral sagittal split osteotomy and rigid fixation. But the major evidence with regard to clicking after orthognathic surgery points to the fact that there is greater likelihood of improvement rather than deterioration6,55,67,107,120,146, even if such improvement is temporary89. For these reasons, there is no individual guarantee for the evolution of clicking, in contrast to disc displacement and crepitus which do not seem to be affected by SSRO for mandibular advancement or setback6,80,133, unless a specific surgical intervention is undertaken to recapture the disc in TMJ57.
Arthralgia (TMJ pain)
Temporomandibular arthralgia can be defined as pain and tenderness in the joint capsule and/or the synovial lining of the TMJ due to an inflammatory process40. This localized condition is didactically separated into capsulitis and synovitis. The diagnosis is based on pain during palpation in one or both joint sites (lateral pole and/or posterior attachment), plus one or more self-reports of pain in the region of the joint, during maximum opening and/or during lateral excursion34,88. Arthralgia can lead to a reduction in chewing efficiency and limitation of mouth opening, and can be detected before2,31,79 and/or after54orthognathic surgery. There are doubts about the efficiency of mandibular surgical advancement in mitigating temporomandibular symptoms.
In general, in terms of arthralgia, there is greater likelihood of improvement rather than deterioration after orthognathic surgery, but there is no individual guarantee of its evolution6,31,32,36,67,107,108,115,133,141,142. In the short term, an increase in muscle and TMJ symptoms was normally found after mandibular advancement surgery, and this tended to decline over time, without being considered a risk factor for TMD54. On the other hand, it cannot be overlooked that there is also a risk of asymptomatic patients developing TMD after surgery20,79,115,120,124,142, and the condition of patients with TMJ symptoms worsening after surgery12,103,108,142.
It has been suggested that Class II malocclusions with severe mandibular retrognathism and a hyperdivergent skeletal pattern are risk factors for painful TMD75,93,100, and are subject to lesser improvement after surgery31,36,141.
Studies have concluded that SSRO of the mandible has a favorable effect on TMJ symptoms20,31,55,120,141,142, with better evolution for mandibular prognathism than mandibular retrognathism141,142. More specifically, De Clercq, et al. 31(1995) found significantly fewer post-operative TMJ symptoms in normal/low angle mandibular deficiency deformity, while there was no significant difference in the high angle group.
Condylar remodeling and resorption
In both animal and human studies, condylar and fossa remodeling are common response to treatment involving mandibular advancement surgery. Ellis and Hinton45(1991) have shown remodeling changes occurring in the TMJ of the adult Macaca mulatta monkey. In human tomographic radiographs, superficial change with no major clinical relevance has been detected in the contour of healthy TMJ after surgery28. Changes in joint loading, muscle activity and the new condylar position may contribute to this adaptive occurrence28,46.
On average, a more severe irreversible change in condylar shape can take place in approximately 5% of patients who undergo surgery to advance the mandible, but, in the literature23,33,67,73,81,96,147, a larger range of 1 to 31% was found. Besides the TMJ compression generated by orthognathic surgery, other factors such as autoimmune and connective tissue diseases (rheumatoid arthritis, lupus erythematosis, scleroderma), trauma, infection, hormone imbalance (hyperparathyroidism, extremely irregular menstrual cycles, low 17β-estradiol), nutritional status, drugs (steroid use), repetitive oral habits, age and genetic background, have all been cited as triggering or aggravating this condition9,10,38,49,58-60,84,144.
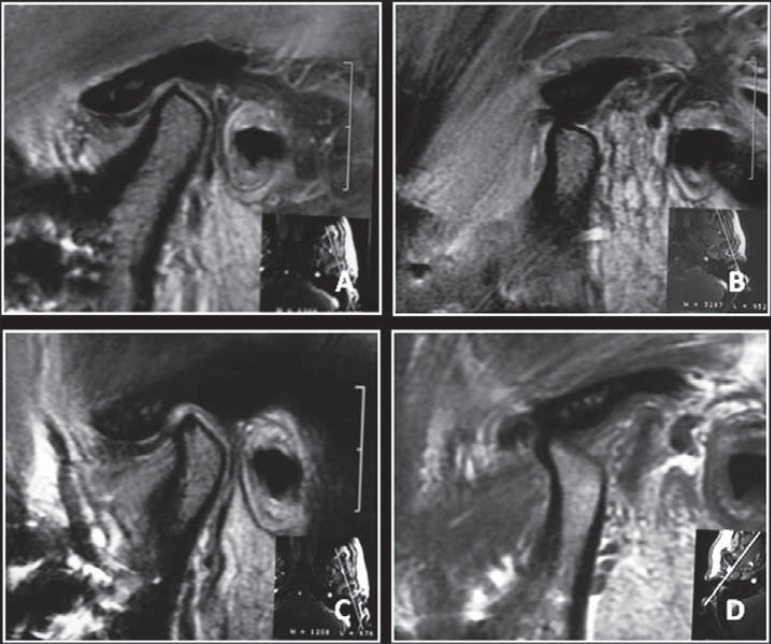
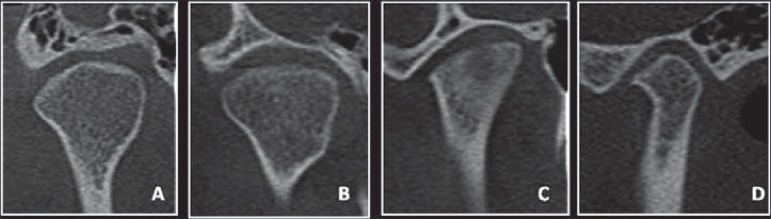
The shape and degree of severity of degenerative bony changes has been detected by CT scans. Such shape changes have been classified as follows147 according to an earlier report: flattening (a flat bony contour deviating from the convex form), erosion (a localized area of decreased density in the cortical condylar surface and adjacent subchondral bone), and osteophyte (a marginal bony overgrowth on the anterior part of the condyle) (Figure 1). Degrees of resorption of the articular surface have varied from superficial changes to complete destruction at advanced stages9,10,26,38(Figure 2).
Figure 1.
Cone-beam computed tomography images of temporomandibular joint showing morphological variation of the mandibular condyle. A- Normal (coronal view); B- Flattening (coronal view); C- Erosion (coronal view); and, D- Osteophyte (sagittal view)
Figure 2.

Cone-beam computed tomography images of temporomandibular joint (coronal view) showing advanced destruction of mandibular condyle
The spectrum of clinical and pathological changes in CR may include disc displacement, perforation and destruction; crepitus; hyperplastic synovial tissue; synovitis; and loss of articular fibrocartilage. In addition, there have been changes in shape and a reduction in the size of condyles69,78,144. Some of the patients affected are asymptomatic, except for joint sounds78,122, while a quarter may develop pain, crepitus, or irregular or limited mouth opening9,33,78,81,128,144. So, symptoms may, or may not, be detected and may vary pre- and post-surgically, and may worsen after surgery. Pain intensity was not correlated with the severity of the CR, except in one study using 3D surface models26.
Localized (non-systemic) inflammatory disease has been called idiopathic CR when individual susceptibility is present and no identified etiologic factor is detected113. This bone loss has also been named condylisis (or condylolysis)38, condylar atrophy 33,78,122, progressive condylar resorption 68,81, or progressive mandibular retrusion 9,10. First described by Sesanna and Raffaini122(1985) and confirmed by others69,81, a progressive, slow irreversible relapse of the mandible develops after mandibular advancement surgery, with a subsequent reduction in the height of the ramus, downward and backward rotation of the mandible, resulting in skeletal Class II malocclusion with an anterior open bite, a steep mandibular plane angle, increased lower facial height, and decreased chin projection. A decrease in the pharyngeal air way space has also been mentioned. Both joints can be symmetrically affected, or just one with minor occurrence, while bilateral involvement with an asymmetric outline is also common56,144. Several studies23,33,68,72,74,78,81,92,94,96have shown that the first signs of postsurgical development were detected 6 months or more after surgery and developed up to 2 years after surgery and was related to a long-term skeletal relapse. On the other hand, idiopathic CR has not been found only after orthognathic surgery, and may be observed during or after active dental restorative, orthodontic or before orthognathic surgery113.
Idiopathic CR is a multifactorial disease, with surgical and non-surgical risk factors23,69,73,74,81. Retrospective23,29,33,67,68,72-74,81,96,121and prospective22,120studies have named some morphological features and outlined some risk factors. From these studies, it was concluded that idiopathic CR primarily affects 16 to 26-year-old females with a mean male/female ratio of 1/8, with skeletal Class II malocclusion due to mandibular retrognathism, and high mandibular plane angles combined with a low posterior facial height. Short condyles with posterior inclination, and/or bone loss before treatment were prone to CR after surgery, and there was a positive correlation with the amount of mandibular advancement and the degree of maxillomandibular counter-clockwise rotation.
Contributing surgical factors have been associated with mechanical overloading and a reduction in vascular supply to the condyle, which may exacerbate the disease in susceptible patients who have undergone mandibular advancement surgery67,96.
Mandibular fixation techniques
Methods of stabilizing the proximal to distal segments at the moment of surgery have progressed from wire fixation to rigid internal fixation (RIF). Wire osteosynthesis was performed in conjunction with a 6 to 8-week period of maxillomandibular fixation (MMF) and was linked, with some exceptions39,135, to postsurgical relapse16,23,37,95,119, due to the weak bone union of the segments which permits proximal segment rotation at the osteotomy sites16. However, in terms of temporomandibular joint pain48,50,101,129 and the mandibular range of motion65, no differences were detected between MMF and RIF.
Spiessl125(1974) introduced RIF in 1974. His method involved using three lag-screws at the osteotomy site (two above the neurovascular bundle, and one below). The advantages of RIF included an early return to normal function, better nutrition support and improved stabilization of the bony segments, which allows for faster bony repair without MMF. Studies on mechanical proprieties and stability at the osteotomy site have attested that RIF is better than wire fixation27,37,95,98,106,110,137. However, the major concern when the mandible is being surgically advanced and rigidly fixed is the risk of damaging the neurovascular bundle and imprecise condylar positioning due to the torque of the rami. In this respect, animal studies45,99have detected a more pronounced effect of the condyle when the rigidity of the fixation method was greater. The intense rigidity brought about by bicortical lag-screws may close the gap between the bone segments and torque the condyle, move it out of the mandibular fossa and cause transverse displacements of the proximal segments14,15,42,140. Consequently, several modifications of RIF patterns have been proposed, varying according to type, number, site, size and placement of screws and miniplates8,24,47,51,52,62,66,76,90,112,117,136.
One way of maintaining the gap while at the same time applying stable fixation is to use positional bicortical screws (non-compressive or non-lag), miniplate systems, or both (hybrid technique)42,103,111. Large gaps between the proximal and distal segments can be minimized by the removal of bone interferences or by using secondary osteotomy before fixation of the mandible42.
Positional bicortical screws have been commonly applied in three linear or L designs66(pattern, backward, inverted, and inverted backward); and inserted at 90º (perpendicular) or 60º angles117,132. One of the advantages of using screws at a 60º angle is the possibility of intrabuccal insertion. Miniplate systems have been used with the technical variant of a horizontal or oblique direction, and fixed with monocortical screws. They also obviate the need for transcutaneous puncture, and its subsequent scarring, reduce time spent in surgery, and pose less risk of nerve damage and condylar torque15. Because the system is less rigid106,117, it is also called semi-rigid fixation99,109. Several hybrid techniques have been cited, such as the miniplate with monocortical screw fixation and positional screws placed bicortically, by means of the plate, or placed separately above or below the plate98,103,107,111.
Retrospective clinical studies18,67have shown that postsurgical stability and condylar changes were not significantly different after using either the miniplate system or positional screws in sagittal split ramus osteotomy. However, in vitro 8,24,62,106,112,117,123,136and finite element27,47,90 studies have shown that miniplate systems provided less mechanical stability in bone segments when compared with different arrangements of bicortical positional screws, and this has been supported by clinical reports that malocclusions developed from a loss of miniplate fixation after mandibular advancement surgery44.
In summary, earlier biomechanical studies compared different designs of mandibular fixation and showed that24,98,106,117,132: 1) three positional screws were equivalent to the hybrid technique with one miniplate fixed with monocortical screws and one positional screw; 2) 2.7 mm screws offered no advantage over 2.0 mm bicortical screws; 3) the angle of insertion of the screw at 90º (percutaneous placement) or 60º (transoral placement) made no significant difference in the resistance of sheep osteotomized mandibles. However, perpendicular insertion (90º) of the screws in inverted-L and linear configurations offered greater laboratory resistance in polyurethane models; and, 4) obliquely placed miniplates offered greater biomechanical stability than those placed horizontally.
Amount of mandibular advancement
The amount of mandibular advancement is another surgical aspect which would appear to contribute towards increasing mechanical loading on TMJ43,45. Elis and Sinn46(1994) demonstrated that the extent of the stretched tissue correlated with the amount of mandibular advancement, suggesting that a larger surgical movement showed a greater tendency towards distal displacement of the surrounding soft tissue in the postsurgical period.
In consonance with this statement, several studies corroborated a considerable correlation between the amount of mandibular advancement and an increase in condylar displacement4,43,45,139, muscle and TMJ symptoms54, relapse rate11,18,19,21,39,75,137,139and the occurrence of CR29,117,118. However, others failed to demonstrate a tendency towards relapse41,95,114, probably because there were not many patients in the samples with greater mandibular advancement.
A systematic review conducted by Joss and Vassalli76(2009), with regard to surgical stability, pointed out that a ≥7 mm mandibular advancement predisposed towards horizontal relapse. In the literature, surgical technique modifications are used to alleviate stretched tissues and prevent skeletal relapse. Suprahyoid miotomy involved detaching the geniohyoid and anterior digastric muscle in order to reduce stretched tissue at the time of mandibular advancement43. However, clinical studies have not been able to confirm this effect121.
DISCUSSION
Several studies point to mandibular advancement surgery as a potential factor in bringing about TMJ changes, especially in condylar position and shape4,46,63,64,97,126,138,139. A successful functional outcome depends on the final TMJ position and the patient's health, including the remission of preexisting TMD. This study reviewed the response of the TMJ to mandibular advancement surgery by analyzing certain risk factors, which included three TMJ changes (disk displacement, arthralgia, and CR) and two treatment variables (fixation techniques and the amount of advancement). Overall,surgery did not manage to change the presurgical disc position or correct the anterior disc displacement; although it tended to improve preexisting arthralgia without individual guarantees or in a predictable way; and increased the risk of CR, especially in identified high-risk cases. The amount of mandibular advancement81,119,counterclockwise rotation74, and the rigidity of the fixation technique45seemed to influence TMJ position and health. However, the literature frequently presented methodological problems, which limited the final evidence.
Little information was found in the literature to reduce bias and strengthen the evidence6,13,56,82. Certain methodological problems were identified, including: sample size; a lack of defined inclusion criteria; the presence of heterogeneous groups made up of patients who had undergone different types of surgery; the presence of confounding factors; longitudinal studies with short follow-up periods; error analysis method; blinding in measurements;inadequate statistics; extrapolation from animal studies to humans; generalization of in vitro biomechanical results without considering individual variation; little research on the correlation between clinical findings and TMJ images;poor imaging techniques; lack of longitudinal observational and interventional studies; TMD type not always identified; unrecognized TMJ problems before surgery; lack of functional data; different characteristics of the sample with regard to the skeletal relationship, race and age; and lack of internal controls. Although magnetic resonance imaging is the diagnostic "gold standard" for disc displacement, few studies used this methodology before or after orthognathic surgery in a long follow-up period. Nevertheless, relevant data from this overview is useful for clinical comprehension and practice.
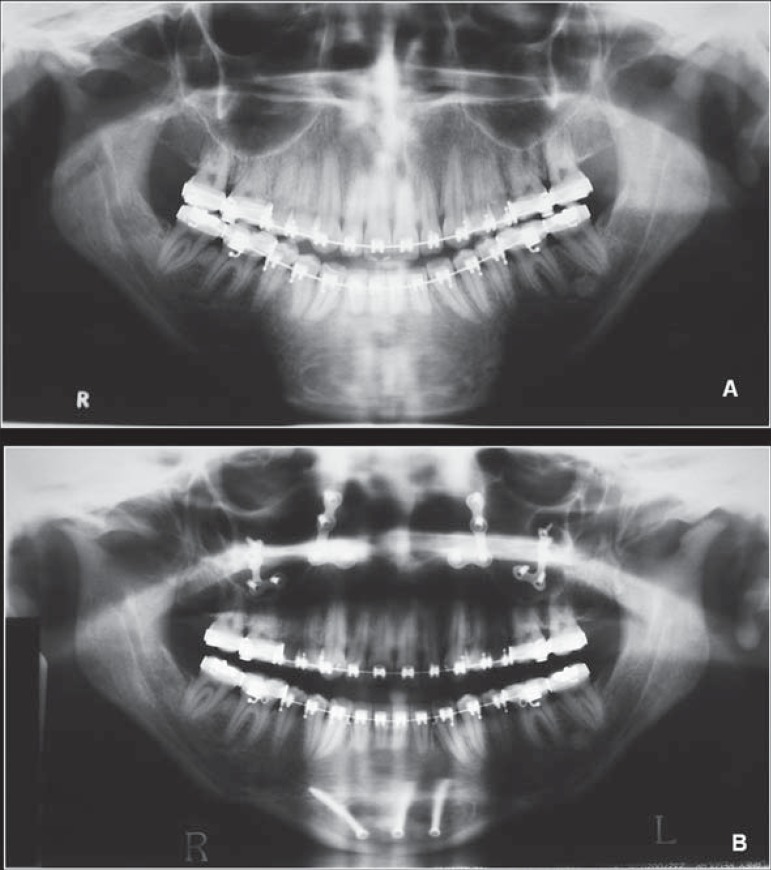
It has been assumed that joints with preexisting displaced discs and crepitus are more likely not to change or improve after mandibular surgery6,55,57,104, unless a specific surgical intervention is undertaken to recapture the disc57,143,144in TMJ. This could be explained by the persistent compression of the condyle against the posterior ligament after surgery. The significance of this persistent disc displacement after surgery is unknown especially in relation to the onset of degenerative disease, as the natural course of the disease could be superimposed on the effects of the treatment and act as a confounding factor (Figure 3).
Figure 3.
Presurgical magnetic resonance of temporomandibular joint showing disc displacement with reduction (A and B), and 10 years after mandibular surgical advancement (C and D) showing the maintenance of the disc status and the onset of condylar degeneration
Most patients present limited or deviated mouth opening shortly after surgery55. This condition can be of muscular or joint origin. When it is of muscular origin, it is attributed to myositis, associated with surgical trauma and can lead to severe functional impairment and disability. But the condition improves post surgically, and most patients regain their full range of movement in the long-term6,65. It is also hypothesized that improvement in self-image after surgery reduces patients' negative feelings, irrespective of the functional outcome108. On the other hand, it cannot be ruled out that persistent orofacial pain after surgery can be modulated by the central nervous system. When of joint origin it is presumed to be temporary54. It would also be associated with disc displacement without reduction, which does not seem to be directly influenced by the surgery6.
It has been considered that minimal condylar and fossa remodeling are unavoidable after mandibular advancement surgery, thus falling within the physiological range of adaptation. An exception is greater condylar destruction, which extrapolates the level of adaptive tolerance and precipitates the development of occlusal and skeletal changes81. According to Proffit114(2000), a loss of more than 2 mm occurred in 10%of patients undergoing mandibular advancement surgery and occlusal instability was foundin half (5%) of these patients. The amount of bone loss in TMJ detected in images extrapolating the level of adaptive tolerance in unknown, but the precise limit can be established in accordance with the development of occlusal and skeletal changes56.
Because idiopathic CR is more common among females, it has been proposed that it may be related to the sex hormone9,58,59. In animal studies102,148, estrogen has been implicated as a mediator of degenerative remodeling of the TMJ, and the increased number of receptors may predispose to an exaggerated response to the loading of the condyle after mandibular advancement surgery. A factor also to be considered in this context isthe higher prevalence of TMJ dysfunction among females89.
The wide range (1 to 31%) of occurrence of CR after orthognathic surgery expressed in the literature may be due to the lack of well-defined diagnostic criteria and the variety of image techniques used. Recent guidelines have recommended computed tomography(CT) as the modality of choice for evaluating TMJ osseous change, as CT images are considered more accurate than panoramic images or cephalograms3. Adequate parameters of FOV and voxel size should be adopted,because they strongly influence the diagnostic efficacy to detect erosions in the TMJ86. Moreover, a refinement in image analysis for accurate visualization through the reconstruction of 2D images in a 3Dsurface-mapping technique using cone-beam CT (CBCT) images might provide the location and quantification of previously unidentified CR25,26.
It is also equally important to consider the idiopathic and rheumatoid CR activity(active or inactive) and the stage of condylar destruction and jaw discrepancy (mild,moderate or severe). This condition has a natural course of evolution and may express a different prognosis. Active resorption has an unpredictable course of duration, but it is known that the idiopathic condition primarily affects young adult females of the age of those most frequently undergoing orthognathic surgeries. It has been presumed that active CR arises out of a loss of cortical bone coverage, typically found at the erosion stage in CT or in magnetic resonance imaging evidencing the lack of cartilaginous integrity of the condylar surface. It is also detected on bone scintigraphy69,113,130. Because false positive and false negative may occur with scintigraphy exam, longitudinal CT images should be recommended to identify presurgical condylar variants and map the stages of disease progression after treatment.
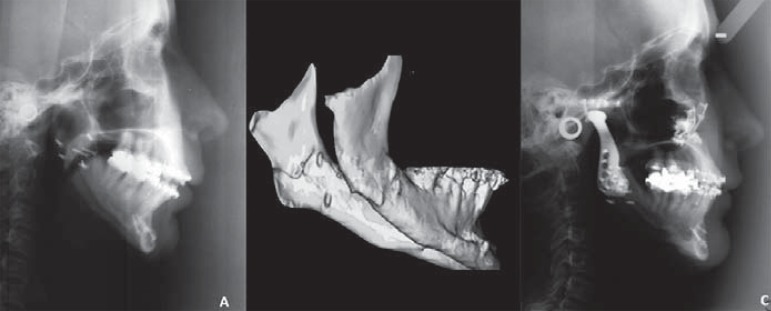
Most studies involving CR have focused on post surgical occurrence and associated long-term relapse33,68,69,94,96. The treatment adopted in cases of relapse has varied from non-surgical (splint therapy, orthodontic camouflage and restorative dentistry) to surgical (re-intervention) approaches17,68,69. However, CR may be present prior to surgery81,84, with onset during adolescence and may be of traumatic, rheumatoid, oridiopathic origin; and related to a secondary and late development of skeletal Class II with open bite malocclusion17,147. It has been well documented that TMJ degeneration does not improve with surgery55, and can lead to unfavorable surgical outcomes because of post surgical mechanical overloading combined with active resorption (Figures 4 and 5). For this reason, in cases of pre existing active CR, doubts arise about the best therapeutic option in terms of preventive management.
Figure 4.
A 23-year-old woman who had maxillary posterior impaction, mandibular auto rotation and genioplasty for advancement. Relapse of Class II maloclusion was evident at long-term post surgery due to condylar resorption. Facial photos before orthognathic surgery (A); 6 months (B) and 3 years (C) after orthognathic surgery are shown. Patient signed informed consent authorizing the publication of these pictures
Figure 5.
Sequence of figure 6 presenting panoramic images before (A) and after (B) surgery showing the pre-existing juvenile idiopathic arthritis and the deterioration after surgery
Cases of minor jaw discrepancies have been treated by conservative procedures (splint therapy; restorative dentistry; orthodontic treatment with or without skeletal anchorage)85,92,128. However,when major jaw discrepancies are present they are mainly treated by surgical protocols for functional and esthetic recovery17,35,49,144,145. Mandibular advancement surgery in cases of preexisting active CR has been associated with long-term relapse69. Therefore, different protocols have been suggested to help control the advance of condyle resorption or prevent surgical relapse. These include postponing the start of orthodontic-surgical treatment113. More recently, pharmacological control has been recommended both before and during orthodontic surgical treatment in order to stabilize active CR59,84,116. The different options of treatment include condylectomy and reconstruction with costochondral grafting49,69,131; disc repositioning143-145;alloplastic joint reconstruction35,38,91, recommended in cases of advanced condyle destruction (Figure 6).
Figure 6.
Complete destruction of condyle in a patient who had undergone orthognathic surgery, and was re-treated with the aid of temporomandibular joint prostheses. Before surgery (A), 3D image of the mandible showing bilateral absence of condyles (B), and after surgery (C)
Careful attention has been recommended for surgical procedures in high-risk CR patients,including the avoidance of excessive mechanical loading on the TMJ. Transverse rotation of the condyles always accompanies ramus surgery to advance the mandible and is thought to be related to how much TMJ dysfunction has occurred14,142. Biomechanical studies of RIF methods after mandible advancement surgery have tested the parameter of biomechanical stability. Although SSRO is relatively standardized, in the literature there is no agreement about the procedure for RIF, which was selected according to the surgeon's choice. The exception was the lag-screw, which was considered detrimental105. In recent years, the hybridtechnique, defined as varying combinations of the use of positional screw(s) and miniplates24,117, is among the most frequently chosen ostheosynthesis methods. The question that arises is if this same hierarchy of rigidity for fixing the mandibule in the in vitro model is the same as that transmitted to TMJ, in terms of stress generation: Does the rigidity of fixation imply that the more rigid it is, the more stability there is for early functioning, but, on the other hand, the less stress distribution there is, the more susceptible it is to condylar malpositioning (torque),resorption and relapse?
In vivo animal studies investigated the response of the TMJ to mandibular surgical advancement45,87,99. There was a more pronounced effect on the condyle (retrusion, erosion, flattening and osteophyte) when positional screws were used than when mini plates were used, suggesting that this was developed by the higher impact of the screws transmitted to the condyle. However, no evidence with clinical design has been published with respect to the TMJ response to the type of fixation, except studies which showed a greater skeletal long-term relapse rate in patients treated with bicortical screws than with mini plates70,76.
The choice of type and design of mandibular synthesis should be based on the treatment planning rather than on the surgeon's preference. The use of more rigid fixation techniques (positional screws) should be the choice for patients with greater bite force, larger advancements (>7 mm) and no preexisting active CR, while, on the other hand, a less rigid fixation (mini plates) would be a better choice in cases with a risk factor of CR. As is well known, relapse generally occurs with larger mandibular advancement and in response to CR. Before surgery, any signs of CR should also be studied to identify preexisting resorption.
Besides the mechanical aspects of surgical correction, the treatment of Class II malocclusions with severe mandibular retrognathism in association with a hyper divergent skeletal pattern is considered a clinical challenge. This craniofacial morphology is considered a risk factor for disc displacement100, painful TMJ before71,93,100and after73,79surgery, is subject to less painful improvement after surgery33,141,142and is prone to CR before and after surgery23,33, especially if the condylar neck is posteriorly inclined72,74, and results in higher frequency and greater magnitude of horizontal relapse11,94.
CONCLUSIONS
Mandibular advancement surgery maintained the relationship between the articular discand condyle; improved preexisting arthralgia without any individual guarantees or in any predictable manner; and, increased the risk of CR, especially in susceptible cases.
The amount of mandibular advancement, the degree of maxillomandibular counter-clockwise rotation and the increased joint loading due to the greater rigidity of the mandibular fixation technique contributed to influencing TMJ position and health.
Females with skeletal Class II malocclusion and a high mandibular plane angle pattern were subject to less improvement in painful TMD after surgery and were prone to CR before and after surgery, especially in cases associated with a posteriorly inclined condyle, which contributed to greater horizontal relapse.
REFERENCES
- 1.Abrahamsson C, Ekberg E, Henrikson T, Bondemark L. Alterations of temporomandibular disorders before and after orthognathic surgery: a systematic review. Angle Orthod. 2007;77:729–734. doi: 10.2319/052906-215. [DOI] [PubMed] [Google Scholar]
- 2.Abrahamsson C, Ekberg E, Henrikson T, Nilner M, Sunzel B, Bondemark L. TMD in consecutive patients referred for orthognathic surgery. Angle Orthod. 2009;79:621–627. doi: 10.2319/060408-293.1. [DOI] [PubMed] [Google Scholar]
- 3.Ahmad M, Hollender L, Anderson Q, Kartha K, Ohrbach R, Truelove EL, et al. Research diagnostic criteria for temporomandibular disorders (RDC/TMD): development of image analysis criteria and examiner reliability for image analysis. Oral Surg Oral Med Oral Pathol Ora Radiol Endod. 2009;107:844–860. doi: 10.1016/j.tripleo.2009.02.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Alder ME, Deahl ST, Matteson SR, Van Sickels JE, Tiner BD, Rugh JD. Short-term changes of condylar position after sagittal split osteotomy for mandibular advancement. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;87:159–165. doi: 10.1016/s1079-2104(99)70266-0. [DOI] [PubMed] [Google Scholar]
- 5.Alexander G, Stivers M. Control of the proximal segment during application of rigid internal fixation of sagittal split osteotomy of the mandible. J Oral Maxillofac Surg. 2003;61:1113–1114. doi: 10.1016/s0278-2391(03)00329-x. [DOI] [PubMed] [Google Scholar]
- 6.Al-Riyami S, Cunningham SJ, Moles DR. Orthognathic treatment and temporomandibular disorders: a systematic review. Part 2. Signs and symptoms and meta-analyses. Am J Orthod Dentofacial Orthop. 2009;136:626.e1–626.e16. doi: 10.1016/j.ajodo.2009.02.022. [DOI] [PubMed] [Google Scholar]
- 7.Angle AD, Rebellato J, Sheats RD. Transverse displacement of the proximal segment after bilateral sagittal split osteotomy advancement and its effect on relapse. J Oral Maxillofac Surg. 2007;65:50–59. doi: 10.1016/j.joms.2005.11.117. [DOI] [PubMed] [Google Scholar]
- 8.Anucul B, Waite PD, Lemons JE. In vitro strength analysis of sagittal split osteotomy fixation: noncompression monocortical plates versus bicortical position screws. J Oral Maxillofac Surg. 1992;50:1295–1299. doi: 10.1016/0278-2391(92)90230-w. [DOI] [PubMed] [Google Scholar]
- 9.Arnett GW, Milam SB, Gottesman L. Progressive mandibular retrusion - idiopathic condylar resorption. Part I. Am J Orthod Dentofacial Orthop. 1996;110:8–15. doi: 10.1016/s0889-5406(96)70081-1. [DOI] [PubMed] [Google Scholar]
- 10.Arnett GW, Milam SB, Gottesman L. Progressive mandibular retrusion - idiopathic condylar resorption. Part II. Am J Orthod Dentofacial Orthop. 1996;110:117–127. doi: 10.1016/s0889-5406(96)70099-9. [DOI] [PubMed] [Google Scholar]
- 11.Arpornmaeklong P, Shand JM, Heggie AA. Skeletal stability following maxillary impaction and mandibular advancement. Int J Oral Maxillofac Surg. 2004;33:656–663. doi: 10.1016/j.ijom.2004.01.004. [DOI] [PubMed] [Google Scholar]
- 12.Athanasiou AE, Yücel-Eroglu E. Short-term consequences on orthognathic surgery on stomatognathic function. Eur J Orthod. 1994;16:491–499. doi: 10.1093/ejo/16.6.491. [DOI] [PubMed] [Google Scholar]
- 13.Atkins D, Eccles M, Flottorp S, Guyatt GH, Henry D, Hill S, et al. Systems for grading the quality of evidence and the strength of recommendations. I: critical appraisal of existing approaches. BMC Health Serv Res. 2004;4:38. doi: 10.1186/1472-6963-4-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Becktor JP, Rebellato J, Becktor KB, Isaksson S, Vickers PD, Keller EE. Transverse displacement of the proximal segment after bilateral sagittal osteotomy. J Oral Maxillofac Surg. 2002;60:395–403. doi: 10.1053/joms.2002.31227. [DOI] [PubMed] [Google Scholar]
- 15.Becktor JP, Rebellato J, Sollenius O, Vedtofte P, Isaksson S. Transverse displacement of the proximal segment after bilateral sagittal osteotomy: a comparison of lag screw fixation versus miniplates with monocortical screw technique. J Oral Maxillofac Surg. 2008;66:104–111. doi: 10.1016/j.joms.2006.06.275. [DOI] [PubMed] [Google Scholar]
- 16.Berger JL, Pangrazio-Kulbersh V, Bacchus SN, Kaczynski R. Stability of bilateral sagittal ramus osteotomy: rigid fixation versus transosseous wiring. Am J Orthod Dentofacial Orthop. 2000;118:397–403. doi: 10.1067/mod.2000.108781. [DOI] [PubMed] [Google Scholar]
- 17.Bilodeau JE. Retreatment of a patient who presented with condylar resorption. Am J Orthod Dentofacial Orthop. 2007;131:89–97. doi: 10.1016/j.ajodo.2004.11.040. [DOI] [PubMed] [Google Scholar]
- 18.Blomqvist JE, Ahlborg G, Isaksson S, Svartz K. A comparison of skeletal stability after mandibular advancement and use of two rigid internal fixation techniques. J Oral Maxillofac Surg. 1997;55:568–574. doi: 10.1016/s0278-2391(97)90486-9. [DOI] [PubMed] [Google Scholar]
- 19.Blomqvist JE, Isaksson S. Skeletal stability after mandibular advancement: a comparison of two rigid internal fixation techniques. J Oral Maxillofac Surg. 1994;52:1133–1137. doi: 10.1016/0278-2391(94)90529-0. [DOI] [PubMed] [Google Scholar]
- 20.Borstlap WA, Stoelinga PJ, Hoppenreijs TJ, van't Hof MA. Stabilization of sagittal split advancement osteotomies with miniplates: a prospective, multicentre study with two-year follow-up. Part I. Clinical parameters. Int J Oral Maxillofac Surg. 2004;33:433–441. doi: 10.1016/j.ijom.2004.02.003. [DOI] [PubMed] [Google Scholar]
- 21.Borstlap WA, Stoelinga PJ, Hoppenreijs TJ, van't Hof MA. Stabilisation of sagittal split advancement osteotomies with miniplates: a prospective, multicentre study with two-year follow up. Part II. Radiograph parameters. Int J Oral Maxillofac Surg. 2004;33:535–542. doi: 10.1016/j.ijom.2004.01.015. [DOI] [PubMed] [Google Scholar]
- 22.Borstlap WA, Stoelinga PJ, Hoppenreijs TJ, van't Hof MA. Stabilisation of sagittal split advancement osteotomies with miniplates: a prospective, multicentre study with two-year follow-up. Part III. Condylar remodeling and resorption. Int J Oral Maxillofac Surg. 2004;33:649–655. doi: 10.1016/j.ijom.2004.01.018. [DOI] [PubMed] [Google Scholar]
- 23.Bouwman JP, Kerstens HC, Tuinzing DB. Condylar resorption in orthognathic surgery: the role of intermaxillary fixation. Oral Surg Oral Med Oral Pathol. 1994;78:138–141. doi: 10.1016/0030-4220(94)90135-x. [DOI] [PubMed] [Google Scholar]
- 24.Brasileiro BF, Grempel RG, Ambrosano GM, Passeri LA. An in vitro evaluation of rigid internal fixation techniques for sagittal split ramus osteotomies: advancement surgery. J Oral Maxillofac Surg. 2000;67:809–817. doi: 10.1016/j.joms.2008.11.009. [DOI] [PubMed] [Google Scholar]
- 25.Cevidanes LH, Bailey LJ, Tucker GR, Jr, Styner MA, Mol A, Philips CL, et al. Superimposition of 3D cone-beam CT models of orthognathic surgery patients. Dentomaxillofac Radiol. 2005;34:369–375. doi: 10.1259/dmfr/17102411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cevidanes LH, Hajati AK, Paniagua B, Lim PF, Walker DG, Palconet G, et al. Quantification of condylar resorption in temporomandibular joint osteoarthritis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;110:110–117. doi: 10.1016/j.tripleo.2010.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chuong CJ, Borotikar B, Schwartz-Dabney C, Sinn DP. Mechanical characteristics of the mandible after bilateral sagittal split ramus osteotomy: comparing 2 different fixation techniques. J Oral Maxillofac Surg. 2005;63:68–76. doi: 10.1016/j.joms.2003.12.045. [DOI] [PubMed] [Google Scholar]
- 28.Cottrell DA, Suguimoto RM, Wolford LW, Sachdeva R, Guo IY. Condylar change after upward and forward rotation of the maxillomandibular complex. Am J Orthod Dentofac Orthop. 1997;111:156–162. doi: 10.1016/s0889-5406(97)70211-7. [DOI] [PubMed] [Google Scholar]
- 29.Cutbirth M, Van Sickels JE, Thrash WJ. Condylar resorption after bicortical screw fixation of mandibular advancement. J Oral Maxillofac Surg. 1998;56:178–182. doi: 10.1016/s0278-2391(98)90863-1. [DOI] [PubMed] [Google Scholar]
- 30.Dahlberg G, Petersson A, Westesson PL, Eriksson L. Disk displacement and temporomandibular joint symptoms in orthognathic surgery patients. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995;79:273–277. doi: 10.1016/s1079-2104(05)80219-7. [DOI] [PubMed] [Google Scholar]
- 31.De Clercq CA, Abeloos JS, Mommaerts MY, Neyt LF. Temporomandibular joint symptoms in an orthognathic surgery population. J Craniomaxillofac Surg. 1995;23:195–199. doi: 10.1016/s1010-5182(05)80010-1. [DOI] [PubMed] [Google Scholar]
- 32.De Clercq CA, Neyt LF, Mommaerts MY, Abeloos JV. Orthognathic surgery: patients' subjective findings with focus on the temporomandibular joint. J Craniomaxillofac Surg. 1998;26:29–34. doi: 10.1016/s1010-5182(98)80032-2. [DOI] [PubMed] [Google Scholar]
- 33.De Clercq CA, Neyt LF, Mommaerts MY, Abeloos JV, De Mot BM. Condylar resorption in orthognathic surgery: a retrospective study. Int J Adult Orthodon Orthognath Surg. 1994;9:233–240. [PubMed] [Google Scholar]
- 34.De Leeuw R. American Academy of Orofacial Pain guidelines for assessment, diagnosis, and management. 4th ed. Chicago: Quintessence; 2008. [Google Scholar]
- 35.Dela Coleta KE, Wolford LM, Gonçalves JR, Pinto AS, Pinto LP, Cassano DS. Maxillo-mandibular counter-clockwise rotation and mandibular advancement with TMJ Concepts total joint prostheses: part I - skeletal and dental stability. Int J Oral Maxillofac Surg. 2009;38:126–138. doi: 10.1016/j.ijom.2008.11.024. [DOI] [PubMed] [Google Scholar]
- 36.Dervis E, Tuncer E. Long-term evaluations of temporomandibular disorders in patients undergoing orthognatic surgery compared with a control group. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;94:554–560. doi: 10.1067/moe.2002.128021. [DOI] [PubMed] [Google Scholar]
- 37.Dolce C, Van Sickels JE, Bays RE, Rugh JD. Skeletal stability after mandibular advancement with rigid versus wire fixation. J Oral Maxillofac Surg. 2000;58:1219–1227. doi: 10.1053/joms.2000.16617. [DOI] [PubMed] [Google Scholar]
- 38.Doucet JC, Morrison AD. Bilateral mandibular condylysis from systemic sclerosis: case report of surgical correction with bilateral total temporomandibular joint replacement. Craniomaxillofac Trauma Reconstr. 2011;4:11–18. doi: 10.1055/s-0031-1272904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Douma E, Kuftinec MM, Moshiri F. A comparative study of stability after mandibular advancement surgery. Am J Orthod Dentofacial Orthop. 1991;100:141–155. doi: 10.1016/S0889-5406(05)81521-5. [DOI] [PubMed] [Google Scholar]
- 40.Dworkin SF, LeResche L. Research diagnostic criteria for temporomandibular disorders: review, criteria, examinations, and specifications critique. J Craniomandib Disord. 1992;6:301–355. [PubMed] [Google Scholar]
- 41.Eggensperger N, Smolka K, Luder J, Iizuka T. Short- and longterm skeletal relapse after mandibular advancement surgery. Int J Oral Maxillofac Surg. 2006;35:36–42. doi: 10.1016/j.ijom.2005.04.008. [DOI] [PubMed] [Google Scholar]
- 42.Ellis E 3rd. A method to passively align the sagittal ramus osteotomy segments. J Oral Maxillofacial Surg. 2007;65:2125–2130. doi: 10.1016/j.joms.2007.02.005. [DOI] [PubMed] [Google Scholar]
- 43.Ellis E, 3rd, Carlson DS. Stability two years after mandibular advancement with and without suprahyoid myotomy: an experimental study. J Oral Maxillofac Surg. 1983;41:426–437. doi: 10.1016/0278-2391(83)90127-1. [DOI] [PubMed] [Google Scholar]
- 44.Ellis E, 3rd, Esmail N. Malocclusions resulting from loss of fixation after sagittal split ramus osteotomies. J Oral Maxillofac Surg. 2009;67:2528–2533. doi: 10.1016/j.joms.2009.06.022. [DOI] [PubMed] [Google Scholar]
- 45.Ellis E, 3rd, Hinton RJ. Histological examination of the temporomandibular joint after mandibular advancement with and without rigid fixation: an experimental investigation in adult Macaca mulatta. J Oral Maxilofac Surg. 1991;49:1316–1327. doi: 10.1016/0278-2391(91)90311-9. [DOI] [PubMed] [Google Scholar]
- 46.Ellis E, 3rd, Sinn DS. Connective tissue forces from mandibular advancement. J Oral Maxillofacial Surg. 1994;52:1160–1163. doi: 10.1016/0278-2391(94)90534-7. [DOI] [PubMed] [Google Scholar]
- 47.Erkmen E, Simsek B, Yücel E, Kurt A. Comparison of different fixation methods following sagittal split ramus osteotomies using three-dimensional finite elements analysis. Part 1: advancement surgery - posterior loading. Int J Oral Maxillofac Surg. 2005;34:551–558. doi: 10.1016/j.ijom.2004.10.009. [DOI] [PubMed] [Google Scholar]
- 48.Feinerman DM, Piecuch JF. Long-term effects of orthognathic surgery on the temporomandibular joint: comparison of rigid and nonrigid fixation methods. Int J Oral Maxillofac Surg. 1995;4:268–272. doi: 10.1016/s0901-5027(95)80026-3. [DOI] [PubMed] [Google Scholar]
- 49.Ferguson JW, Luyk NH, Parr NC. A potential role for costochondral grafting in adults with mandibular condylar destruction secondary to rheumatoid arthritis - a case report. J Craniomaxillofac Surg. 1993;21:15–18. doi: 10.1016/s1010-5182(05)80525-6. [DOI] [PubMed] [Google Scholar]
- 50.Flynn B, Brown DT, Lapp TH, Bussard DA, Roberts WE. A comparative study of temporomandibular symptoms following mandibular advancement by bilateral sagittal split osteotomies: rigid versus nonrigid fixation. Oral Surg Oral Med Oral Pathol. 1990;70:372–380. doi: 10.1016/0030-4220(90)90163-m. [DOI] [PubMed] [Google Scholar]
- 51.Foley WL, Beckman TW. In vitro comparison of screw versus plate fixation in the sagittal split osteotomy. Int J Adult Orthodon Orthognath Surg. 1992;7:147–151. [PubMed] [Google Scholar]
- 52.Foley WL, Frost DE, Paulin WB, Tucker MR. Internal screw fixation: comparison of placement pattern and rigidity. J Oral Maxillofac Surg. 1989;47:720–723. doi: 10.1016/s0278-2391(89)80013-8. [DOI] [PubMed] [Google Scholar]
- 53.Freihofer HP, Jr, Petresevic D. Late results after advancing the mandible by sagittal splitting of the rami. J Maxillofac Surg. 1975;3:250–257. doi: 10.1016/s0301-0503(75)80051-8. [DOI] [PubMed] [Google Scholar]
- 54.Frey DR, Hatch JP, Van Sickels JE, Dolce C, Rugh JD. Effects of surgical mandibular advancement and rotation on signs and symptoms of temporomandibular disorder: a 2-year follow-up study. Am J Orthod Dentofacial Orthop. 2008;133:490.e1–490.e8. doi: 10.1016/j.ajodo.2007.10.033. [DOI] [PubMed] [Google Scholar]
- 55.Gaggl A, Schultes G, Santler G, Kärcher H, Simbrunner J. Clinical and magnetic resonance findings in the temporomandibular joints of patients before and after orthognatic surgery. Br J Oral Maxillofac Surg. 1999;37:41–45. doi: 10.1054/bjom.1998.0387. [DOI] [PubMed] [Google Scholar]
- 56.Gill DS, El Maaytah M, Naini FB. Risk factors for postorthognathic condylar resorption: a review. World J Orthod. 2008;9:21–25. [PubMed] [Google Scholar]
- 57.Gonçalves JR, Cassano DS, Wolford LM, Santos-Pinto A, Márquez IM. Postsurgical stability of counterclockwise maxillomandibular advancement surgery: effect of articular disc repositioning. J Oral Maxillofac Surg. 2008;66:724–738. doi: 10.1016/j.joms.2007.11.007. [DOI] [PubMed] [Google Scholar]
- 58.Gunson MJ, Arnett GW, Formby B, Falzone C, Mathur R, Alexander C. Oral contraceptive pill use and abnormal menstrual cycles in women with severe condylar resorption: a case for low serum 17beta-estradiol as a major factor in progressive condylar resorption. Am J Orthod Dentofacial Orthop. 2009;136:772–779. doi: 10.1016/j.ajodo.2009.07.011. [DOI] [PubMed] [Google Scholar]
- 59.Gunson MJ, Arnett GW, Milam SB. Pathophysiology and pharmacologic control of osseous mandibular condylar resorption. J Oral Maxillofac Surg. 2012;70:1918–1934. doi: 10.1016/j.joms.2011.07.018. [DOI] [PubMed] [Google Scholar]
- 60.Gynther GW, Tronje G, Holmlund AB. Radiographic changes in the temporomandibular joint in patients with generalized osteoarthritis and rheumatoid arthritis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996;81:613–618. doi: 10.1016/s1079-2104(96)80058-8. [DOI] [PubMed] [Google Scholar]
- 61.Hackney FL, Van Sickels JE, Nummikoski PV. Condylar displacement and temporomandibular joint dysfunction following bilateral sagittal split osteotomy and rigid fixation. J Oral Maxillofac Surg. 1989;47:223–227. doi: 10.1016/0278-2391(89)90221-8. [DOI] [PubMed] [Google Scholar]
- 62.Hammer B, Ettlin D, Rahn B, Prein J. Stabilization of the short sagittal split osteotomy: in vitro testing of different plate and screw configurations. J Craniomaxillofac Surg. 1995;23:321–324. doi: 10.1016/s1010-5182(05)80164-7. [DOI] [PubMed] [Google Scholar]
- 63.Harper RP. Analysis of temporomandibular joint function after orthognathic surgery using condylar path tracings. Am J Orthod Dentofacial Orthop. 1990;97:480–488. doi: 10.1016/S0889-5406(05)80028-9. [DOI] [PubMed] [Google Scholar]
- 64.Harris MD, Van Sickels JE, Alder M. Factors influencing condylar position after the bilateral sagittal split osteotomy fixed with bicortical screws. J Oral Maxillofac Surg. 1999;57:650–654. doi: 10.1016/s0278-2391(99)90422-6. [DOI] [PubMed] [Google Scholar]
- 65.Hatch JP, Van Sickels JE, Rugh JD, Dolce C, Bays RA, Sakai S. Mandibular range of motion after bilateral sagittal split ramus osteotomy with wire osteosynthesis or rigid fixation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;91:274–280. doi: 10.1067/moe.2001.112685. [DOI] [PubMed] [Google Scholar]
- 66.Haug RH, Barber E, Punjabi AP. An in vitro comparison of the effect of number and pattern of positional screws on load resistance. J Oral Maxillofac Surg. 1999;57:300–308. doi: 10.1016/s0278-2391(99)90677-8. [DOI] [PubMed] [Google Scholar]
- 67.Hoppenreijs TJ, Freihofer HP, Stoelinga PJ, Tuinzing DB, van't Hof MA. Condylar remodeling and resorption after Le Fort I and bimaxillary osteotomies in patients with anterior open bite. A clinical and radiological study. Int J Oral Maxillofac Surg. 1998;27:81–91. doi: 10.1016/s0901-5027(98)80301-9. [DOI] [PubMed] [Google Scholar]
- 68.Hoppenreijs TJ, Stoelinga PJ, Grace KL, Robben CM. Longterm evaluation of patients with progressive condylar resorption following orthognathic surgery. Int J Oral Maxillofac Surg. 1999;28:411–418. [PubMed] [Google Scholar]
- 69.Huang YL, Pogrel MA, Kaban LB. Diagnosis and management of condylar resorption. J Oral Maxillofac Surg. 1997;55:114–119. doi: 10.1016/s0278-2391(97)90222-6. [DOI] [PubMed] [Google Scholar]
- 70.Hughes R. Relapse following bilateral sagittal split osteotomy with rigid internal fixation. Evid Based Dent. 2009;10:81–82. doi: 10.1038/sj.ebd.6400671. [DOI] [PubMed] [Google Scholar]
- 71.Hwang CJ, Sung SJ, Kim SJ. Lateral cephalometric characteristics of malocclusion patients with temporomandibular joint disorder symptoms. Am J Orthod Dentofacial Orthop. 2006;129:497–503. doi: 10.1016/j.ajodo.2004.12.019. [DOI] [PubMed] [Google Scholar]
- 72.Hwang SJ, Haers PE, Sailer HF. The role of a posteriorly inclined condylar neck in condylar resorption after orthognathic surgery. J Craniomaxillofac Surg. 2000;28:85–90. doi: 10.1054/jcms.2000.0129. [DOI] [PubMed] [Google Scholar]
- 73.Hwang SJ, Haers PE, Seifert B, Sailer HF. Non-surgical risk factors for condylar resorption after orthognathic surgery. J Craniomaxillofac Surg. 2004;32:103–111. doi: 10.1016/j.jcms.2003.09.007. [DOI] [PubMed] [Google Scholar]
- 74.Hwang SJ, Haers PE, Zimmermann A, Oechslin C, Seifert B, Sailer HF. Surgical risk factors for condylar resorption after orthognathic surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;89:542–552. doi: 10.1067/moe.2000.105239. [DOI] [PubMed] [Google Scholar]
- 75.Joss CU, Thüer UW. Stability of the hard and soft tissue profile after mandibular advancement surgery in saggital split osteotomies: a longitudinal and long-term follow-up study. Eur J Orthod. 2008;30:16–23. doi: 10.1093/ejo/cjm080. [DOI] [PubMed] [Google Scholar]
- 76.Joss CU, Vassalli IM. Stability after bilateral sagittal split osteotomy advancement surgery with rigid internal fixation: a systematic review. J Oral Maxillafac Surg. 2009;67:301–313. doi: 10.1016/j.joms.2008.06.060. [DOI] [PubMed] [Google Scholar]
- 77.Kersey ML, Nebbe B, Major PW. Temporomandibular joint morphology changes with mandibular advancement surgery and rigid internal fixation: a systematic literature review. Angle Orthod. 2003;73:79–85. doi: 10.1043/0003-3219(2003)073<0079:TJMCWM>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 78.Kerstens HC, Tuinzing DB, Golding RP, van der Kwast WA. Condylar atrophy and osteoarthrosis after bimaxillary surgery. Oral Surg Oral Med Oral Pathol. 1990;69:274–280. doi: 10.1016/0030-4220(90)90286-2. [DOI] [PubMed] [Google Scholar]
- 79.Kerstens HC, Tuinzing DB, van der Kwast WA. Temporomandibular joint symptoms in orthognathic surgery. J Craniomaxillofac Surg. 1989;17:215–218. doi: 10.1016/s1010-5182(89)80071-x. [DOI] [PubMed] [Google Scholar]
- 80.Kim YK, Yun PY, Ahn JY, Kim JW, Kim SG. Changes in the temporomandibular joint disc position after orthognathic surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;108:15–21. doi: 10.1016/j.tripleo.2009.02.005. [DOI] [PubMed] [Google Scholar]
- 81.Kobayashi T, Izumi N, Kojima T, Sakagami N, Saito I, Saito C. Progressive condylar resorption after mandibular advancement. Br J Oral Maxillofac Surg. 2012;50:176–180. doi: 10.1016/j.bjoms.2011.02.006. [DOI] [PubMed] [Google Scholar]
- 82.Kurita H, Uehara S, Yokochi M, Nakatsuka A, Kobayashi H, Kurashina K. A long-term follow-up study of radiographically evident degenerative changes in the temporomandibular joint with different conditions of disk displacement. Int J Oral Maxillofac Surg. 2006;35:49–54. doi: 10.1016/j.ijom.2005.04.004. [DOI] [PubMed] [Google Scholar]
- 83.Kurita K, Westesson PL, Yuasa H, Toyama M, Machida J, Ogi N. Natural course of untreated symptomatic temporomandibular joint disc displacement without reduction. J Dent Res. 1998;77:361–365. doi: 10.1177/00220345980770020401. [DOI] [PubMed] [Google Scholar]
- 84.Kuroda S, Kuroda Y, Tomita Y, Tanaka E. Long-term stability of conservative orthodontic treatment in a patient with rheumathoid arthritis and severe condylar resorption. Am J Orthod Dentofacial Orthop. 2012;141:352–362. doi: 10.1016/j.ajodo.2010.04.036. [DOI] [PubMed] [Google Scholar]
- 85.Kuroda S, Sakai Y, Tamamura N, Deguchi T, Takano-Yamamoto T. Treatment of severe anterior open bite with skeletal anchorage in adults: comparison with orthognathic surgery outcome. Am J Orthod Dentofacial Orthop. 2007;132:599–605. doi: 10.1016/j.ajodo.2005.11.046. [DOI] [PubMed] [Google Scholar]
- 86.Librizzi ZT, Tadinada AS, Valiyaparambil JV, Lurie AG, Mallya SM. Cone-beam computed tomography to detect erosions of the temporomandibular joint: effect of field of view and voxel size on diagnostic efficacy and effective dose. Am J Orthod Dentofacial Orthop. 2011;140:e25–e30. doi: 10.1016/j.ajodo.2011.03.012. [DOI] [PubMed] [Google Scholar]
- 87.Lima Navarro R, Oltramari PV, Sant' Ana E, Henriques JF, Taga R, Cestari TM, et al. Histological and molecular temporomandibular joint analyses after mandibular advancement surgery: study in minipigs. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106:331–338. doi: 10.1016/j.tripleo.2008.01.026. [DOI] [PubMed] [Google Scholar]
- 88.Link JJ, Nickerson JW., Jr Temporomandibular joint internal derangements in an orthognathic surgery population. Int J Adult Orthodon Orthognath Surg. 1992;7:161–169. [PubMed] [Google Scholar]
- 89.Magnusson T, Egermark I, Carlsson GE. A longitudinal epidemiologic study of signs and symptoms of temporomandibular disorders from 15 to 35 years of age. J Orofac Pain. 2000;14:310–319. [PubMed] [Google Scholar]
- 90.Maurer P, Knoll WD, Schubert J. Comparative evaluation of two osteosynthesis methods on stability following sagittal split osteotomy. J Craniomaxillofac Surg. 2003;31:284–289. doi: 10.1016/s1010-5182(03)00073-8. [DOI] [PubMed] [Google Scholar]
- 91.Mercuri LG. Osteoarthritis, osteoarthrosis, and idiopathic condylar resorption. Oral Maxillofac Surg Clin North Am. 2008;20:169–183. doi: 10.1016/j.coms.2007.12.007. [DOI] [PubMed] [Google Scholar]
- 92.Merkx MA, Van Damme PA. Condylar resorption after orthognathic surgery. Evaluation of treatment in 8 patients. J Craniomaxillofac Surg. 1994;22:53–58. doi: 10.1016/s1010-5182(05)80297-5. [DOI] [PubMed] [Google Scholar]
- 93.Miller JR, Mancl L, Critchlow C. Severe retrognathia as a risk factor for recent onset painfull TMJ disorders among adult females. J Orthod. 2005;32:249–256. doi: 10.1179/146531205225021222. [DOI] [PubMed] [Google Scholar]
- 94.Mobarak KA, Espeland L, Krogstad O, Lyberg T. Mandibular advancement surgery in high-angle and low-angle Class II patients: different long-term skeletal responses. Am J Orthod Dentofacial Orthop. 2001;119:368–381. doi: 10.1067/mod.2001.110983. [DOI] [PubMed] [Google Scholar]
- 95.Moenning JE, Bussard DA, Lapp TH, Garrison BT. A comparison of relapse in bilateral sagittal split osteotomies for mandibular advancement: rigid internal fixation (screws) versus inferior border wiring with anterior skeletal fixation. Int J Adult Orthod Orthognath Surg. 1990;5:175–182. [PubMed] [Google Scholar]
- 96.Moore KE, Gooris PJ, Stoelinga PJ. The contributing role of condylar resorption to skeletal relapse following mandibular advancement surgery: report of five cases. J Oral Maxillofac Surg. 1991;49:448–460. doi: 10.1016/0278-2391(91)90166-j. [DOI] [PubMed] [Google Scholar]
- 97.Motta AT, Cevidanes LH, Carvalho FA, Almeida MA, Phillips C. Three-dimensional regional displacements after mandibular advancement surgery: one year of follow-up. J Oral Maxillofac Surg. 2011;69:1447–1457. doi: 10.1016/j.joms.2010.07.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Murphy MT, Haug RH, Barber JE. An in vitro comparison of the mechanical characteristics of three sagittal ramus osteotomy fixation techniques. J Oral Maxillofac Surg. 1997;55:489–494. doi: 10.1016/s0278-2391(97)90699-6. [DOI] [PubMed] [Google Scholar]
- 99.Navarro RL, Oltramari-Navarro PV, Sant' Ana E, Henriques JF, Taga R, Cestari TM, et al. Histologic and tomographic analyses of the temporomandibular joint after mandibular advancement surgery: study in mini pigs. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107:477–484. doi: 10.1016/j.tripleo.2008.10.006. [DOI] [PubMed] [Google Scholar]
- 100.Nebbe B, Major PW, Prasad NG. Adolescent female craniofacial morphology associated with advanced bilateral TMJ disc displacement. Eur J Orthod. 1998;20:701–712. doi: 10.1093/ejo/20.6.701. [DOI] [PubMed] [Google Scholar]
- 101.Nemeth DZ, Rodrigues-Garcia RC, Sakai S, Hatch JP, Van Sickels JE, Bays RA, et al. Bilateral sagittal split osteotomy and temporomandibular disorders: rigid fixation versus wire fixation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;89:29–34. doi: 10.1016/s1079-2104(00)80010-4. [DOI] [PubMed] [Google Scholar]
- 102.Okuda T, Yasuoka T, Nakashima M, Oka N. The effect of ovariectomy on the temporomandibular joints of growing rats. J Oral Maxillofac Surg. 1996;54:1201–1210. doi: 10.1016/s0278-2391(96)90352-3. [DOI] [PubMed] [Google Scholar]
- 103.Oliveira LB, Sant'Ana E, Manzato AJ, Guerra FL, Arnett GW. Biomechanical in vitro evaluation of three stable internal fixation techniques used in sagittal osteotomy of the mandibular ramus: a study in sheep mandibles. J Appl Oral Sci. 2012;20:419–426. doi: 10.1590/S1678-77572012000400006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Onizawa K, Schmelzeisen R, Vogt S. Alteration of temporomandibular joint symptoms after orthognathic surgery: comparison with healthy volunteers. J Oral Maxillofac Surg. 1995;3:117–121. doi: 10.1016/0278-2391(95)90383-6. [DOI] [PubMed] [Google Scholar]
- 105.O'Ryan F, Epker BN. Surgical orthodontic and the temporomandibular joint. II. Mandibular advancement via modified sagittal split ramus osteotomies. Am J Orthod. 1983;83:418–427. doi: 10.1016/0002-9416(83)90325-1. [DOI] [PubMed] [Google Scholar]
- 106.Özden B, Alkan A, Arici S, Erdem E. In vitro comparison of biomechanical characteristics of sagittal split osteotomy fixation techniques. Int J Oral Maxillofac Surg. 2006;35:837–841. doi: 10.1016/j.ijom.2006.03.001. [DOI] [PubMed] [Google Scholar]
- 107.Pahkala R, Heino J. Effects of sagittal split ramus osteotomy on temporomandibular disorders in seventy-two patients. Acta Odontol Scand. 2004;62:238–244. doi: 10.1080/00016350410001667. [DOI] [PubMed] [Google Scholar]
- 108.Pahkala RH, Kellokoski JK. Surgical-orthodontic treatment and patients' functional and psychosocial well-being. Am J Orthod Dentofacial Orthop. 2007;132:158–164. doi: 10.1016/j.ajodo.2005.09.033. [DOI] [PubMed] [Google Scholar]
- 109.Panula K, Somppi M, Finne K, Oikarinen K. Effects of orthognathic surgery on temporomandibular joint dysfunction. A controlled prospective 4-year follow-up study. Int J Oral Maxillofac Surg. 2000;29:183–187. [PubMed] [Google Scholar]
- 110.Paulus GW. Semirigid bone fixation: a new concept in orthognathic surgery. J Craniofac Surg. 1991;2:146–151. [PubMed] [Google Scholar]
- 111.Pereira FL, Janson M, Sant'Ana E. Hybrid fixation in the bilateral sagittal split osteotomy for lower jaw advancement. J Appl Oral Sci. 2010;18:92–99. doi: 10.1590/S1678-77572010000100015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Peterson GP, Haug RH, Van Sickels JE. A biomechanical evaluation of bilateral sagittal ramus osteotomy fixation techniques. J Oral Maxillofac Surg. 2005;63:1317–1324. doi: 10.1016/j.joms.2005.05.301. [DOI] [PubMed] [Google Scholar]
- 113.Posnick JC, Fantuzzo JJ. Idiopathic condylar resorption: current clinical perspectives. J Oral Maxillofac Surg. 2007;65:1617–1623. doi: 10.1016/j.joms.2007.03.026. [DOI] [PubMed] [Google Scholar]
- 114.Proffit WR. Contemporary orthodontics. St Louis: Mosby Elsevier; 2007. p. 716. [Google Scholar]
- 115.Rubens BC, Stoelinga PJ, Blijdorp PA, Schoenaers JH, Politis C. Skeletal stability following sagittal split osteotomy using monocortical miniplate internal fixation. Int J Oral Maxillofac Surg. 1988;17:371–376. doi: 10.1016/s0901-5027(88)80066-3. [DOI] [PubMed] [Google Scholar]
- 116.Sasaguri K, Ishizaki-Takeuchi R, Kuramae S, Tanaka EM, Sakurai T, Sato S. The temporomandibular joint in a rheumatoid arthritis patient after orthodontic treatment. Angle Orthod. 2009;79:804–811. doi: 10.2319/040708-201.1. [DOI] [PubMed] [Google Scholar]
- 117.Sato FR, Asprino L, Consani S, Moraes M. Comparative biomechanical and photoelastic evaluation of different fixation techniques of sagittal split ramus osteotomy in mandibular advancement. J Oral Maxillofac Surg. 2010;68:160–166. doi: 10.1016/j.joms.2009.09.004. [DOI] [PubMed] [Google Scholar]
- 118.Sato S, Kawamura H, Nagasaka H, Motegi K. The natural course of anterior disc displacement without reduction in the temporomandibular joint: follow-up at 6, 12, and 18 months. J Oral Maxillofac Surg. 1997;55:234–238. doi: 10.1016/s0278-2391(97)90531-0. [DOI] [PubMed] [Google Scholar]
- 119.Satrom KD, Sinclair PM, Wolford LM. The stability of double jaw surgery: a comparison of rigid versus wire fixation. Am J Orthod Dentofacial Orthop. 1991;99:550–563. doi: 10.1016/S0889-5406(05)81632-4. [DOI] [PubMed] [Google Scholar]
- 120.Scheerlinck JP, Stoelinga PJ, Blijdorp PA, Brouns JJ, Nijs ML. Sagittal split advancement osteotomies stabilized with miniplates: a 2-5 year follow-up. Int J Oral Maxillofac Surg. 1994;23:127–131. doi: 10.1016/s0901-5027(05)80285-1. [DOI] [PubMed] [Google Scholar]
- 121.Schendel SA, Epker BN. Results after mandibular advancement surgery: an analysis of 87 cases. J Oral Surg. 1980;38:265–282. [PubMed] [Google Scholar]
- 122.Sesenna E, Raffaini M. Bilateral condylar atrophy after combined osteotomy for correction of mandibular retrusion. A case report. J Maxillofac Surg. 1985;13:263–266. doi: 10.1016/s0301-0503(85)80061-8. [DOI] [PubMed] [Google Scholar]
- 123.Shetty V, Freymiller E, McBrearty D, Caputo AA. Experimental analysis of functional stability of saggital split ramus osteotomies secured by miniplates and position screws. J Oral Maxillofac Surg. 1996;54:1317–1324. doi: 10.1016/s0278-2391(96)90490-5. [DOI] [PubMed] [Google Scholar]
- 124.Smith V, Williams B, Stapleford R. Rigid internal fixation and the effects on the temporomandibular joint and masticatory system: a prospective study. Am J Orthod Dentofacial Orthop. 1992;102:491–500. doi: 10.1016/0889-5406(92)70065-I. [DOI] [PubMed] [Google Scholar]
- 125.Spiessl B. Osteosynthesis in sagittal osteotomy using the Obwegeser-Dal Pont method. Fortschr Kiefer Gesichtschir. 1974;18:145–148. [PubMed] [Google Scholar]
- 126.Sund G, Eckerdal O, Astrand P. Changes in the temporomandibular joint after oblique sliding osteotomy of the mandibular rami. A longitudinal radiological study. J Maxillofac Surg. 1983;11:87–91. doi: 10.1016/s0301-0503(83)80021-6. [DOI] [PubMed] [Google Scholar]
- 127.Tallents RH, Katzberg RW, Murphy W, Proskin H. Magnetic resonance imaging findings in asymptomatic volunteers and symptomatic patients with temporomandibular disorders. J Prosthet Dent. 1996;75:529–533. doi: 10.1016/s0022-3913(96)90458-8. [DOI] [PubMed] [Google Scholar]
- 128.Tanaka E, Kikuchi K, Sasaki A, Tanne K. An adult case of TMJ osteoarthrosis treated with splint therapy and the subsequent orthodontic occlusal reconstruction: adaptive change of the condyle during the treatment. Am J Orthod Dentofacial Orthop. 2000;118:566–571. doi: 10.1067/mod.2000.93966. [DOI] [PubMed] [Google Scholar]
- 129.Timmis DP, Aragon SB, Van Sickels JE. Masticatory dysfunction with rigid and nonrigid osteosynthesis of sagittal split osteotomies. Oral Surg Oral Med Oral Pathol. 1986;62:119–123. doi: 10.1016/0030-4220(86)90027-7. [DOI] [PubMed] [Google Scholar]
- 130.Toll DE, Popovic N, Drinkuth N. The use of MRI diagnostics in orthognathic surgery: prevalence of TMJ pathologies in Angle Class I, II III patients. J Orofac Orthop. 2010;71:68–80. doi: 10.1007/s00056-010-0903-1. [DOI] [PubMed] [Google Scholar]
- 131.Troulis MJ, Tayebaty FT, Papadaki M, Williams WB, Kaban LB. Condylectomy and costochondral graft reconstruction for treatment of active idiopathic condylar resorption. J Oral Maxillofac Surg. 2008;66:65–72. doi: 10.1016/j.joms.2007.08.030. [DOI] [PubMed] [Google Scholar]
- 132.Uckan S, Schwimmer A, Kummer F, Greenberg AM. Effect of the angle of the screw on the stability of the mandibular sagittal split ramus osteotomy: a study in sheep mandibles. Br J Oral Maxillofac Surg. 2001;39:266–268. doi: 10.1054/bjom.2000.0580. [DOI] [PubMed] [Google Scholar]
- 133.Ueki K, Marukawa K, Shimada M, Hashiba Y, Nakgawa K, Yamamoto E. Condylar and disc positions after sagittal split ramus osteotomy with and without Le Fort I osteotomy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103:342–348. doi: 10.1016/j.tripleo.2006.05.024. [DOI] [PubMed] [Google Scholar]
- 134.Van Damme PA, Merkx MA. Condylar resorption in orthognathic surgery. Oral Surg Oral Pathol Oral Radiol Endod. 1995;79:265–266. doi: 10.1016/s1079-2104(05)80212-4. [DOI] [PubMed] [Google Scholar]
- 135.Van Sickels JE, Dolce C, Keeling S, Tiner BD, Clark GM, Rugh JD. Technical factors accounting for stability of bilateral sagittal split osteotomy advancement: wire osteosynthesis versus rigid fixation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;89:19–23. doi: 10.1016/s1079-2104(00)80008-6. [DOI] [PubMed] [Google Scholar]
- 136.Van Sickels JE, Peterson GP, Holms S, Haug RH. An in vitro comparison of an adjustable bone fixation system. J Oral Maxillofac Surg. 2005;63:1620–1625. doi: 10.1016/j.joms.2005.06.008. [DOI] [PubMed] [Google Scholar]
- 137.Van Sickels JE, Larsen AJ, Thrash WJ. Relapse after rigid fixation of mandibular advancement. J Oral Maxillofac Surg. 1986;44:698–702. [PubMed] [Google Scholar]
- 138.Van Sickels JE, Tiner BD, Alder ME. Condylar torque as a possible cause of hypomobility after sagittal split osteotomy: report of three cases. J Oral Maxillofac Surg. 1997;55:398–402. doi: 10.1016/s0278-2391(97)90134-8. [DOI] [PubMed] [Google Scholar]
- 139.Van Sickels JE, Tiner BD, Keeling SD, Clark GM, Bays R, Rugh J. Condylar position with rigid fixation versus wire osteosynthesis of a sagittal split advancement. J Oral Maxillofac Surg. 1999;57:31–34. doi: 10.1016/s0278-2391(99)90627-4. [DOI] [PubMed] [Google Scholar]
- 140.Watzke IM, Tucker MR, Turvey TA. Lag screw versus position screw techniques for rigid internal fixation of sagittal osteotomies: a comparison of stability. Int J Adult Orthodon Orthognath Surg. 1991;6:19–27. [PubMed] [Google Scholar]
- 141.Westermark A, Shayeghi F, Thor A. Temporomandibular dysfunction in 1,516 patients before and after orthognathic surgery. Int J Adult Orthodon Orthognath Surg. 2001;16:145–151. [PubMed] [Google Scholar]
- 142.White CS, Dolwick MF. Prevalence and variance of temporomandibular dysfunction in orthognathic surgery patients. Int J Adult Orthod Orthognath Surg. 1992;7:7–14. [PubMed] [Google Scholar]
- 143.Wolford LM. Concomitant temporomandibular joint and orthognathic surgery. J Oral Maxillofac Surg. 2003;61:1198–1204. doi: 10.1016/s0278-2391(03)00682-7. [DOI] [PubMed] [Google Scholar]
- 144.Wolford LM, Cardenas L. Idiopathic condylar resorption: diagnosis, treatment protocol, and outcomes. Am J Orthod Dentofacial Orthop. 1999;116:667–677. doi: 10.1016/s0889-5406(99)70203-9. [DOI] [PubMed] [Google Scholar]
- 145.Wolford LM, Mehra P. Simultaneous temporomandibular joint and mandibular reconstruction in an immunocompromised patient with rheumatoid arthritis: a case report with 7-year follow-up. J Oral Maxillofac Surg. 2001;59:345–350. doi: 10.1053/joms.2001.21011. [DOI] [PubMed] [Google Scholar]
- 146.Wolford LM, Reiche-Fischel O, Mehra P. Changes in temporomandibular joint dysfunction after orthogantic surgery. J Oral Maxillofac Surg. 2003;61:655–660. doi: 10.1053/joms.2003.50131. [DOI] [PubMed] [Google Scholar]
- 147.Yamada K, Hanada K, Hayashi T, Ito J. Condylar bony change, disk displacement and signs and symptoms of TMJ disorders in orthognathic surgery patients. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;91:603–610. doi: 10.1067/moe.2001.112153. [DOI] [PubMed] [Google Scholar]
- 148.Yasuoka T, Nakashima M, Okuda T, Tatematsu N. Effect of estrogen replacement on temporomandibular joint remodeling in ovariectomized rats. J Oral Maxillofac Surg. 2000;58:189–196. doi: 10.1016/s0278-2391(00)90337-9. [DOI] [PubMed] [Google Scholar]