Abstract
Research focusing on the social determinants of diabetes has focused on individual-level factors such as health behaviors, socio-economic status, and depression. Fewer studies that incorporate a broader consideration of the multiple contexts or organizational levels (e.g. family, health care setting, neighborhood) within which individuals are embedded exist in the mainstream diabetes literature. Such an approach would enhance our understanding of this complex disease, and thus, future avenues of research should consider the following: 1) a life-course approach which examines the influence of early life exposures on the development of diabetes; 2) aiming to understand the biological mechanisms of social determinants of diabetes; and 3) implementing interventions on multiple levels. Integrating this multi-level and life-course approach will require transdisciplinary science which brings together highly specialized expertise from multiple disciplines. Broadening the study of social determinants is a necessary step toward improving the prevention and treatment of type 2 diabetes.
Keywords: Social epidemiology, social determinants, social factors, diabetes, type 2 diabetes, obesity, complications
Introduction
The field of social epidemiology seeks to understand whether and how social, cultural, economic and political factors, sometimes collectively referred to as “social determinants,” influence health and disease in the population (see Table 1 for a list of definitions) [1-5]. While the study of social determinants of health has not been a major emphasis in the field of diabetes, several key papers have attempted to conceptualize and summarize the literature in this area. One of the first manuscripts, developed by Brown and colleagues[6], conceptualized the relationship between socioeconomic status and health for people with diabetes, emphasizing contributors to intermediate diabetes outcomes such as access to health care (i.e. primary care, waiting times), process measures (i.e. HbA1c testing) and health behaviors (i.e. blood glucose monitoring). A second manuscript summarized patient, system, and clinician level interventions to address disparities in diabetes care [7]. Finally, a recent comprehensive review of the literature presented the biological, clinical and non-clinical factors associated with health disparities in endocrine disorders, with diabetes as a major focus [8]. The current manuscript builds on those key papers in the field and summarizes recent evidence on social determinants that influence the development of type 2 diabetes and associated conditions (obesity, diabetes-related complications). Furthermore, this manuscript points to future research directions to broaden and strengthen the literature on the social epidemiology of type 2 diabetes and associated conditions.
Table 1. Key Terms and Definitions for Social Epidemiology.
| Term | Definition |
|---|---|
| Social determinants | Living and working conditions and systems for addressing health and illness that are shaped by social, economic and political structures (World Health Organization. Social determinants of health: key concepts (1). |
| Health disparities | Potentially avoidable health differences across population groups with poorer health outcomes observed among socially disadvantaged groups (2). |
| Multi-level approach | Integration of factors at different levels of organization into studying health outcomes (3). |
| Life-course approach | Study of influences of factors in different stages of life, including those encountered in utero and in childhood on health in later life periods. Factors in prior generations are also sometimes considered in relation to the health of the offspring (4). |
| Social environment | Social factors within groups, neighborhoods, workplaces and other contexts to which individuals belong, including the extent and nature of social connections, social norms and attitudes, social disorder, safety, and other features of the social organization of groups and places(5). |
| Physical environment | Environmental substances and hazards (e.g., air pollution, chemical toxicants) as well as factors related to “man-made built environment”, including buildings, sidewalks, streets, public spaces, physical barriers, and access to healthy food outlets.(5). |
Conceptual Framework
The conceptual framework guiding our summary uses a multi-level social ecological approach (see Figure 1) [9-12]. This framework expands the narrow emphasis on individual-level biomedical and behavioral factors to include a broader consideration of the multiple contexts or organizational levels within which individuals are embedded. These contexts include family/social networks, health care settings/practices, and the physical and social environment, all of which are affected by larger local, state and national policies. Paramount to this conceptual framework is the integration of factors across these inter-connected levels in influencing health outcomes. Furthermore, the framework incorporates a time dimension that extends beyond risk factors and disease processes in adulthood, and suggests that risk factors and development of diabetes are shaped by circumstances throughout the life course, including those encountered in early life [13, 14, 4]. Together, these multilevel and life-course approaches are increasingly recognized as crucial to understanding the social epidemiology of complex chronic diseases such as diabetes. We also acknowledge the importance of race/ethnicity, which is a social construct that strongly impacts many of these “levels.” For example, it impacts how resources are distributed, how health care is delivered and how policies have been developed, historically, and in current times. In this manuscript, our focus is not on racial/ethnic disparities; however, many of the social factors that we discuss are associated with or impacted by race/ethnicity.
Figure 1.
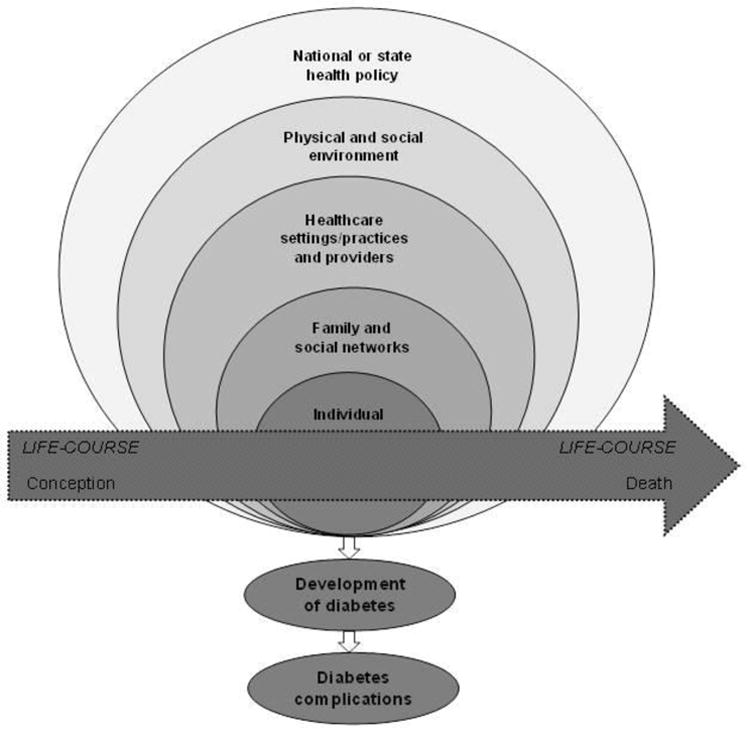
A multilevel framework for social determinants of diabetes incidence and complications.
Summary of the Current Literature
Individual-level social factors
Individual-level factors have been the most investigated determinants of diabetes. There is an expansive literature documenting behavioral factors associated with the development of type 2 diabetes including physical activity, dietary behaviors and smoking. For example, higher levels of physical activity have been consistently associated with lower risk of diabetes [15, 16]. Moreover, many “Western” dietary patterns indicative of high fat, processed and red meat consumption have been associated with higher risk of diabetes [17-19]. In contrast, specific dietary components including higher consumption of fiber, whole grains, omega-3 fatty acids, coffee and alcohol have been associated with lower risk [20-23]. Finally, smoking, an established risk factor for cardiovascular disease, has also been identified as a risk factor for type 2 diabetes in several cohort studies [24, 25]. The conventional research in the area, however, has not focused on how social determinants at multiple levels and across the life-course influence these well-established behavioral risk factors for diabetes. There are many different pathways to achieving these behaviors, which in turn, affect the risk of diabetes and complications. Several individual-level social factors, socio-economic status (SES), cultural and psychosocial, described below, can influence these behaviors.
Socio-economic status (SES)
Lower SES, most frequently measured by education and income, has been associated with increased risk of diabetes [26-30]. In a recent meta-analysis, a 30-40% higher risk of diabetes was associated with lower levels of education, occupational class/status, and income, compared to higher levels of these determinants [28]. Furthermore, poverty has been associated with geographical disparities in obesity [31, 32], higher physical inactivity [33, 34], and sedentary behaviors [35].
Psychosocial factors
An extensive literature has documented a relationship between depression and type 2 diabetes as well as insulin resistance [36]. More severe diabetes complications have been noted among individuals with type 2 diabetes and depression [37]. Other adverse psychosocial factors, such as stressful events, poor social control and stress-prone personality, have also been associated with poor diabetes control [38]. Furthermore, depressive symptomatology, is often manifested in response to stress [39] and evidence supports the theory that stress impacts both psychological and physical well-being for a wide range of diseases, including obesity and diabetes[40, 41]. A few studies have examined this relationship, noting evidence of an association between negative life events in childhood, violence exposure and diabetes [42]. For example, the Adverse Childhood Event (ACE) Study noted a relationship between traumatic childhood experiences and diabetes in adulthood. Furthermore, exposure to specific stressors such as, experiences of discrimination, violence and job stress have been associated with obesity and diabetes [43, 44, 42]. Few studies, however have examined potential mechanisms linking stress both in childhood and adulthood to the development of diabetes.
Cultural factors
The relationship between cultural factors and diabetes has not been fully explored. Acculturation has been shown to influence various health outcomes in different immigrant populations in the US. Defined as “the process by which immigrants adopt the values, customs, beliefs, and behaviors of a new culture,” acculturation has been linked to health behaviors, obesity and diabetes [8]. The results have been mixed with acculturation showing both positive and negative influences on diabetes and associated risk factors. On one hand, lifestyle factors may be negatively influenced for example, by adopting western dietary patterns or more tobacco use. Conversely, increasing levels of acculturation can be associated with more health promoting resources such as higher SES, greater access to health care and more leisure time to engage in healthy behaviors.
It has also been shown that spirituality is seen as a source of emotional support, a coping mechanism for stress, a positive influence on health and a contributor to life satisfaction [45-47]. These studies among persons with type 2 diabetes suggest that a belief in God or spirituality may provide the strength to deal with daily hassles and stresses. Moreover, religious activity might be positively related to a sense of control over health, which, in turn, may help individuals adhere to diabetes self-management behaviors [46]. Some empirical data also suggests that health outcomes such as blood pressure and depressive symptoms are better among those who attended church frequently [48]. Although most aspects of spirituality are considered to have positive influences on health, there could also be the tendency to neglect self-care, with the belief that divine intervention through prayer and/or meditation alone is sufficient to manage health/diabetes. While the role of acculturation and spirituality in understanding self-management has been investigated, more research is needed to tease out the potentially different ways in which they can influence the development of diabetes. Given the essential role that religion and spirituality play in many cultures, it is important to investigate these factors as potential contributors.
Family and social networks
Individuals are nested within social networks of families and friends, and are influenced by the behaviors of members of their networks [49]. Social networks can influence behavior, promoting both positive and negative health behaviors for its members. The relationship between positive social support and better physical and mental health has been well established [7]. In contrast, these networks can also have detrimental effects on individuals if obligations to them entail financial burden, demands on time, criticisms, or caretaking responsibilities [50]. Social networks have furthermore been shown to impact the risk of obesity. Using Framingham Heart Study data, Christakis and colleagues demonstrated that a person's chance of becoming obese increased if he or she had a friend who became obese within a specified time period [51]. With the exception of social support, few studies have examined the relationship between other social network characteristics and diabetes. It has been shown that minority groups rely more heavily on informal social networks to meet disease-management needs and social support has been associated with better glycemic control in a few studies [52].
Healthcare settings/practices
Disease management, educational, and behavioral interventions to improve diabetes care in health care settings have been plentiful [53, 54]. Overall, studies implement a number of different strategies including clinical and patient education, case management, and reminder systems to improve diabetes care. Some of the strategies have health care organizational components such as using electronic patient registries, implementing team changes or ancillary care providers (i.e. nutritionists, nurses), or tackling organizational quality improvement. These disease management interventions are generally effective with an average reduction in HbA1c of 0.42%, which is clinically modest [54, 53]. Incorporating social factors in the management of diabetes has produced better results. For example, interventions targeting ethnic minority groups that were culturally tailored (i.e, having greater community involvement, using community or lay education, using a face-to-face approach) were even more effective than those that were not tailored [55].
Interventions targeting social determinants at the health care systems and organizational-levels (e.g., reducing co-pays, improving healthcare access) have been limited [7]. Recently, “Finding Answers: Disparities Research for Change”, an initiative supported by the Robert Wood Johnson Foundation, created a road map and best practices for organizations to reduce racial/ethnic disparities in health care [56]. Strategies which tackle organizational-level factors such as assessing organizational capacity, implanting interventions into existing infrastructure to improve sustainability, and being flexible and adaptable throughout the implementation process are encouraged. We look forward to the next generation of studies that address organizational-level factors and their impact on diabetes care and prevention.
Physical and social environment
A growing body of literature on neighborhood influences on health has focused on factors capturing the physical and social aspects of the neighborhood environment. Specifically, two pathways have been investigated: (1) a built design pathway affecting diet and physical activity, referred to as the “physical environment”; and (2) a social/stress pathway which can have a direct (i.e., sympathetic nervous system, visceral fat accumulation) and indirect (i.e. unhealthy diet, sedentary behaviors) effect on obesity and diabetes, referred to as the “social environment.”
The features of social and physical neighborhood are generally inter-related. For example, neighborhood poverty has been linked to several features of the built environment, including greater distance to parks and recreational facilities, less walkable areas, poor access to public transportation and higher crime rates, all of which have been associated with lower levels of physical activity. Other aspects of neighborhood design [57] such as greater fast food restaurant density [58, 59], high cost and low quality of healthy foods have been associated with greater body mass index (BMI) [60, 61]. Only a few studies have linked fewer neighborhood resources for physical activity and healthy food to more insulin resistance and to the development of type 2 diabetes [62-64].
Adverse features of the neighborhood environment may also be a direct source of stress. For example, neighborhood crime, lack of safety, poor aesthetic quality, low social support and cohesion can be a source of stress for the residents of the neighborhood [65]. Based on the theory that mixed-income neighborhoods provide a number of material (i.e., more access to healthy food options and places to be physically active) and social (i.e., social norms and networks that promote a healthier lifestyle) resources to low-income families that are not available in areas of concentrated neighborhood poverty, the Moving to Opportunity (MTO) study examined the benefits of using housing vouchers to move families out of public housing projects and into mixed-income housing [66, 67]. A recent follow-up of MTO participants confirmed earlier reports on the benefits of housing voucher use and showed that relocating to low poverty areas reduced diabetes risk [68]. However, the MTO study was unable to characterize the built and social environment in which participants lived, making it difficult to identify mechanisms that could explain why housing relocation to low poverty neighborhoods conferred lower rates of obesity and risk of diabetes.
Summary of social risk factors for diabetes
A summary of the social risk factors for diabetes discussed in this manuscript are presented in Table 2. Overall, many social risk factors have been examined and some are both positively and negatively associated with diabetes, which adds to the complexity of studying them. Moreover, while research is developing on levels higher than the individual (family/social networks, health care settings, environment, and state and local policy), it has not yet reached the volume and precision of the research at the individual-level. Policies on the quality of care and on reimbursements for care in health care settings have received the most attention thus far [8]. More public-health-related policies/programs which integrate the public health and medical care systems are needed. An example of such effort is the New York City Department of Health and Mental Hygiene HbA1c registry, which requires mandatory reporting of HbA1c lab results generated in clinical settings [69]. The HbA1c registry not only allows for surveillance of diabetes control by socio-demographic and neighborhood indicators, which is helpful for allocating public health resources, but it also allows for behavioral/clinical intervention among those in poor control. New York City was the first in the US to mandate this type of program and results of the program have not yet been published for others to absorb or replicate. Thus, given the early stage of research of the social determinants of diabetes at multiple levels, there are many avenues that remain to be pursued.
Table 2. Summary of Social Risk Factors for Diabetes and Associated Conditions.
| Risk Factor of Interest | Main Associationa |
|---|---|
| Individual-level Factors | |
| Physical Activity | − |
| Dietary Patterns | +/− |
| Smoking | + |
| Socio-economic status | − |
| Acculturation | +/− |
| Religion/Spirituality | +/− |
| Depression | + |
| Social Stressors | + |
| Family/Social Networks | |
| Social Networks | − |
| Social Support | +/− |
| Health Care Settings/Practices | |
| Disease Management | − |
| Cultural Tailoring | − |
| Physical Environment | |
| Neighborhood Poverty/SES | + |
| Built Environment | +/− |
| Social Environment | |
| Neighborhood Social Stressors | + |
(+) indicates significance and positive association;
(−) indicates significance and negative association;
Aveneues for Future Research
Thinking earlier for prevention of diabetes and cardiovascular-related outcomes
Over the past decade there has been increasing recognition that many adult diseases begin in childhood. Early life conditions such as prenatal under nutrition, maternal stress and obesity during pregnancy have been associated with increased risk of obesity and diabetes in the offspring [70]. Furthermore, the rise in childhood obesity over the past two decades has led to a dramatic increase in the number of adolescents with diabetes, particularly among minority populations. The American Heart Association has modified its practice guidelines, focusing on the prevention of cardiovascular disease in childhood and adolescence, and emphasizing the need for greater prevention efforts and screening for cardiovascular risk factors including insulin resistance [71]. In addition, the American Diabetes Association recommends screening for diabetes among overweight and obese children who also meet two other risk factors (i.e. family history, high risk race/ethnicity or signs or conditions of insulin resistance) [72].
Given that risk factors and health behaviors known to impact obesity and diabetes track from childhood to adolescence and into adulthood [73, 74], it is prudent that prevention efforts start in childhood. Furthermore, evidence suggests that, the longer a person lives with diabetes the more likely they are to develop cardiovascular disease and diabetes related complications [75]. Little is known, however, about the trajectory of obesity and diabetes from childhood to adulthood. Applying a life course framework to the study of type 2 diabetes would elucidate pathways by which factors in early life, including social conditions, affect the development of diabetes. Integrating a comprehensive life course framework would require longitudinal studies that span various life stages, collect repeated measures of traditional (i.e., diet, physical activity) and non-traditional (i.e., stress, neighborhood conditions) risk factors as well as clinical measures. This wealth of information would allow for the examination of various mechanistic models, for example whether sensitive time periods of exposure exists or a sequence of exposures lead to a final exposure causally related to disease, or whether the accumulation of risk factors across the life course is more detrimental [76]. While no one study could answer all of these questions, longitudinal studies that collect risk factor and outcome data across the life span will be better able to identify critical time periods and mechanistic factors for targeted prevention efforts.
Understanding the biological mechanisms of social determinants of diabetes
The increasing recognition of multi-level models of disease development has brought to attention the importance of social factors, and resulted in a growing body of research on social epidemiology of diabetes. The majority of research, however, has examined social determinants in relation to behavioral factors and clinical outcomes with limited research attempting to elucidate how social factors work their way through biological processes leading to the development of diabetes. Investigating the mechanisms linking social conditions and biological processes is an important, although challenging, area for future research [5]. The results of such research can enhance etiologic research on diabetes, which is primarily focused on pathophysiological levels without much incorporation of higher level social factors. Furthermore, this research can provide essential evidence for implicating social factors in causal pathways to diabetes incidence [77, 13]. While such causal relationships among social conditions and disease processes are often implicitly assumed, they are rarely tested empirically. For example, exposure to individual-level (or family level) social stressors is posited to increase the risk of diabetes through behavioral factors and Hypothalamic-Pituitary-Adrenal (HPA) axis, but few empirical studies have rigorously tested these pathways to the development of diabetes [78]. Two potential pathways linking social stress and diabetes have been proposed. First, it is hypothesized that social stressors affect health behaviors, such as diet, physical activity, smoking and alcohol use, partly accounting for the high rates of obesity and diabetes seen among minority and lower social status populations who largely experience a greater number of stressors than non-minority populations. In a study of adults participating in the National Survey of Midlife in the US (MIDUS), eating more in response to stress partially explained a relationship between history of violence experience and obesity [79]. A second proposed mechanism of the relationship between social stress and obesity/diabetes is a direct stress response through activation of the HPA axis, which in response to chronic stress has been associated with the dysregulation of cortisol [80]. In turn, HPA axis dysfunction has been associated with both obesity and diabetes [39].
Studies can also be designed to elucidate the possibility that biological changes exert influences on behaviors and social resources relevant to the development of diabetes and complications. Improving our understanding of how social factors affect biology (sometimes referred to as getting “under the skin”) also discourages the arbitrary dichotomies between social vs. biological causes of disease, and provides a more useful conceptual and pragmatic approach to addressing the burden of diabetes.
Recently epigenetic modifications, heritable and potentially modifiable markers that regulate gene expression without changing the underlying DNA sequence, have emerged as a promising area for investigating biological mechanisms underlying social determinants of health [81-83]. Epigenetic markers are responsive to non-biological and environmental exposures, particularly those encountered in early life, and are being increasingly associated with a number of chronic diseases and associated risk factors [84-86]. A number of studies have recently provided supportive evidence for involvement of epigenetic mechanisms in the associations between indicators of fetal nutrition and growth, childhood body adiposity, impaired glucose tolerance and lower DNA methylation of imprinted IGF2 genes in mid to late adulthood [87-89]. A small but growing body of research has also begun to study social conditions in relation to epigenetic factors including socioeconomic circumstances and global and genome-wide DNA methylation [90-93]. While epigenetic epidemiology remains in its early stages, with anticipated advances in technological capabilities and conceptual clarity, this type of research will be an important avenue for understanding the role of multiple and complex risk factors, including social factors, in the development of diabetes.
In addition to providing a more complete knowledge of the etiology of diabetes, understanding pathways underlying associations across levels can inform translational and intervention research. For example, understanding how social environment combines with pathophysiological mechanisms and pathways to diabetes, can help to identify targets for change in intervention studies (e.g., decreasing social stressors at individual or neighborhood levels) or identify points for interventions (e.g., improving healthcare resources for individuals or neighborhoods experiencing high levels of social stressors).
Implementing Interventions on multiple levels
Ultimately, the goal would be to target these social determinants at multiple levels as we describe in our framework (see Figure 1) and incorporate them into interventions to reduce obesity, diabetes, and associated complications. This is no easy task as each level of influence is fraught with its own set of methodological, research, and implementation challenges.
A good example of a national debate on prevention at multiple levels including government, clinical and community strategies to improve lifestyle behaviors is the case of the Diabetes Prevention Program (DPP) [94-96]. In 2002, the DPP showed that intensive lifestyle interventions targeting diet and exercise, primarily in individuals at high risk, may prevent or delay the onset of type 2 diabetes by up to 58% [97]. Furthermore, the long-term effects of this intervention have been proven to be beneficial [98]. This program has become the gold standard in the field; however, the feasibility of conducting these lifestyle interventions in non-trial settings remains potentially limiting for widespread implementation.
A recent meta-analysis summarized the effectiveness of the DPP in real-world settings and therefore provides a preliminary guide for the development of future tailored interventions [99]. The studies were implemented in various community and clinic settings and were delivered by clinically trained professionals, ancillary care providers, and lay educators. Thus, the translation of these programs is feasible and appropriate. Recently, the Centers for Disease Control and Prevention (CDC) convened a working group to provide recommendations for implementing diabetes prevention strategies with an approach that integrates community organizations, medical practice, and policy [100]. The committee called for steps toward immediate action (e.g. training of work force to deliver proven programs), strategic action (e.g. advocate for insurers to pay for proven prevention programs), and research (investigate ways to increase sustainability and reach of effective prevention programs) for health care and public health settings. This example should prompt incorporation of new social factors into intervention methods and further exploration of integrative approaches to tackling the epidemic of diabetes.
Conclusion
Integrating our knowledge of social and environmental influences with downstream biological pathways to disease requires varied and highly specialized expertise from multiple disciplines, including social and molecular epidemiologists, basic scientists, clinical and behavioral researchers, and biostatisticians. Transdisciplinary science, which brings together multiple disciplinary perspectives and expertise to work on a shared conceptual and empirical framework, is best suited for tackling complex cells-to-society research questions [101, 102].
Acknowledgments
This project was funded by grants from the National Institutes of Health. Funding was provided by NHLBI to Dr. Gary-Webb (K01-HL084700) and Dr. Suglia (K01-HL103199) and by NCI to Dr. Tehranifar (K07-CA151777).
Footnotes
Compliance with Ethics Guidelines: Conflict of Interest: Tiffany L. Gary-Webb, Shakira F. Suglia, and Parisa Tehranifar declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent: This article does not contain any studies with human or animal subjects performed by any of the authors.
References
- 1.Organization WH. Social Determinants of Health: Key Concepts. 2013 http://www.who.int/social_determinants/thecommission/finalreport/key_concepts/en/index.html.
- 2.Diez Roux AV. Conceptual approaches to the study of health disparities. Annual review of public health. 2012;33:41–58. doi: 10.1146/annurev-publhealth-031811-124534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Diez Roux AV. A glossary for multilevel analysis. J Epidemiol Community Health. 2002;56(8):588–94. doi: 10.1136/jech.56.8.588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Power C, Kuh D, Morton S. From developmental origins of adult disease to life course research on adult disease and aging: insights from birth cohort studies. Annual review of public health. 2013;34:7–28. doi: 10.1146/annurev-publhealth-031912-114423. [DOI] [PubMed] [Google Scholar]
- 5.Diez Roux AV, Mair C. Neighborhoods and health. Annals of the New York Academy of Sciences. 2010;1186:125–45. doi: 10.1111/j.1749-6632.2009.05333.x. [DOI] [PubMed] [Google Scholar]
- 6.Brown AF, Ettner SL, Piette J, Weinberger M, Gregg E, Shapiro MF, et al. Socioeconomic position and health among persons with diabetes mellitus: a conceptual framework and review of the literature. Epidemiologic reviews. 2004;26:63–77. doi: 10.1093/epirev/mxh002. [DOI] [PubMed] [Google Scholar]
- 7.Brown AF. Patient, system and clinician level interventions to address disparities in diabetes care. Curr Diabetes Rev. 2007;3(4):244–8. doi: 10.2174/157339907782329988. [DOI] [PubMed] [Google Scholar]
- 8•.Golden SH, Brown A, Cauley JA, Chin MH, Gary-Webb TL, Kim C, et al. Health disparities in endocrine disorders: biological, clinical, and nonclinical factors--an Endocrine Society scientific statement. J Clin Endocrinol Metab. 2012;97(9):E1579–639. doi: 10.1210/jc.2012-2043. This article summarized the literature for health disparities in diabetes and associated conditions and attempted to understand the multiple contributors to these disparities including biological, clinical, and nonclincal influences. It also brought together a multidisciplinary team to think about these issues. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bronfenbrenner U. In: Measuring environment across the life span: Emerging methods and conepts. Friedman SL, Wachs TD, editors. Washington, DC: American Psychological Association Press.; 1999. [Google Scholar]
- 10.McLeroy KR, Bibeau D, Steckler A, Glanz K. An ecological perspective on health promotion programs. Health education quarterly. 1988;15(4):351–77. doi: 10.1177/109019818801500401. [DOI] [PubMed] [Google Scholar]
- 11.Glickman D, Parker L, Sim LJ, Del Valle Cook H, Miller EA. Accelerating progress in obesity prevention: solving the weight of the nation: Institute of Medicine. 2012. [PubMed] [Google Scholar]
- 12.Taplin SH, Anhang Price R, Edwards HM, Foster MK, Breslau ES, Chollette V, et al. Introduction: Understanding and influencing multilevel factors across the cancer care continuum. Journal of the National Cancer Institute Monographs. 2012;2012(44):2–10. doi: 10.1093/jncimonographs/lgs008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Glass TA, McAtee MJ. Behavioral science at the crossroads in public health: extending horizons, envisioning the future. Social science & medicine. 2006;62(7):1650–71. doi: 10.1016/j.socscimed.2005.08.044. [DOI] [PubMed] [Google Scholar]
- 14.Morrissey JP, Lich KH, Price RA, Mandelblatt J. Computational modeling and multilevel cancer control interventions. Journal of the National Cancer Institute Monographs. 2012;2012(44):56–66. doi: 10.1093/jncimonographs/lgs014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jeon CY, Lokken RP, Hu FB, van Dam RM. Physical activity of moderate intensity and risk of type 2 diabetes: a systematic review. Diabetes Care. 2007;30(3):744–52. doi: 10.2337/dc06-1842. [DOI] [PubMed] [Google Scholar]
- 16.Thomas DE, Elliott EJ, Naughton GA. Exercise for type 2 diabetes mellitus. Cochrane database of systematic reviews. 2006;(3):CD002968. doi: 10.1002/14651858.CD002968.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hu EA, Pan A, Malik V, Sun Q. White rice consumption and risk of type 2 diabetes: meta-analysis and systematic review. Bmj. 2012;344:e1454. doi: 10.1136/bmj.e1454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pan A, Sun Q, Bernstein AM, Schulze MB, Manson JE, Willett WC, et al. Red meat consumption and risk of type 2 diabetes: 3 cohorts of US adults and an updated meta-analysis. The American journal of clinical nutrition. 2011;94(4):1088–96. doi: 10.3945/ajcn.111.018978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.de Koning L, Malik VS, Rimm EB, Willett WC, Hu FB. Sugar-sweetened and artificially sweetened beverage consumption and risk of type 2 diabetes in men. The American journal of clinical nutrition. 2011;93(6):1321–7. doi: 10.3945/ajcn.110.007922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pan A, Sun Q, Manson JE, Willett WC, Hu FB. Walnut consumption is associated with lower risk of type 2 diabetes in women. The Journal of nutrition. 2013;143(4):512–8. doi: 10.3945/jn.112.172171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bhupathiraju SN, Pan A, Malik VS, Manson JE, Willett WC, van Dam RM, et al. Caffeinated and caffeine-free beverages and risk of type 2 diabetes. The American journal of clinical nutrition. 2013;97(1):155–66. doi: 10.3945/ajcn.112.048603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wu JH, Micha R, Imamura F, Pan A, Biggs ML, Ajaz O, et al. Omega-3 fatty acids and incident type 2 diabetes: a systematic review and meta-analysis. The British journal of nutrition. 2012;107(2):S214–27. doi: 10.1017/S0007114512001602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wedick NM, Pan A, Cassidy A, Rimm EB, Sampson L, Rosner B, et al. Dietary flavonoid intakes and risk of type 2 diabetes in US men and women. The American journal of clinical nutrition. 2012;95(4):925–33. doi: 10.3945/ajcn.111.028894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yeh HC, Duncan BB, Schmidt MI, Wang NY, Brancati FL. Smoking, smoking cessation, and risk for type 2 diabetes mellitus: a cohort study. Annals of internal medicine. 2010;152(1):10–7. doi: 10.1059/0003-4819-152-1-201001050-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Willi C, Bodenmann P, Ghali WA, Faris PD, Cornuz J. Active smoking and the risk of type 2 diabetes: a systematic review and meta-analysis. JAMA : the journal of the American Medical Association. 2007;298(22):2654–64. doi: 10.1001/jama.298.22.2654. [DOI] [PubMed] [Google Scholar]
- 26.Dray-Spira R, Gary-Webb TL, Brancati FL. Educational disparities in mortality among adults with diabetes in the U.S. Diabetes Care. 2010;33(6):1200–5. doi: 10.2337/dc09-2094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Robbins JM, Vaccarino V, Zhang H, Kasl SV. Socioeconomic status and diagnosed diabetes incidence. Diabetes Res Clin Pract. 2005;68(3):230–6. doi: 10.1016/j.diabres.2004.09.007. [DOI] [PubMed] [Google Scholar]
- 28.Agardh E, Allebeck P, Hallqvist J, Moradi T, Sidorchuk A. Type 2 diabetes incidence and socio-economic position: a systematic review and meta-analysis. Int J Epidemiol. 2011;40(3):804–18. doi: 10.1093/ije/dyr029. [DOI] [PubMed] [Google Scholar]
- 29.Dray-Spira R, Gary TL, Brancati FL. Socioeconomic position and cardiovascular disease in adults with and without diabetes: United States trends, 1997-2005. J Gen Intern Med. 2008;23(10):1634–41. doi: 10.1007/s11606-008-0727-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Maty SC, Everson-Rose SA, Haan MN, Raghunathan TE, Kaplan GA. Education, income, occupation, and the 34-year incidence (1965-99) of Type 2 diabetes in the Alameda County Study. Int J Epidemiol. 2005;34(6):1274–81. doi: 10.1093/ije/dyi167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Singh GK, Kogan MD, van Dyck PC. A multilevel analysis of state and regional disparities in childhood and adolescent obesity in the United States. J Community Health. 2008;33(2):90–102. doi: 10.1007/s10900-007-9071-7. 10.1007/s10900-007-9071-7 [doi] [DOI] [PubMed] [Google Scholar]
- 32.McLaren L. Socioeconomic status and obesity. Epidemiol Rev. 2007;29:29–48. doi: 10.1093/epirev/mxm001. [DOI] [PubMed] [Google Scholar]
- 33.Crespo CJ, Ainsworth BE, Keteyian SJ, Heath GW, Smit E. Prevalence of physical inactivity and its relation to social class in U.S. adults: results from the Third National Health and Nutrition Examination Survey, 1988-1994. Med Sci Sports Exerc. 1999;31(12):1821–7. doi: 10.1097/00005768-199912000-00019. [DOI] [PubMed] [Google Scholar]
- 34.Giles-Corti B, Donovan RJ. Socioeconomic status differences in recreational physical activity levels and real and perceived access to a supportive physical environment. Prev Med. 2002;35(6):601–11. doi: 10.1006/pmed.2002.1115. [DOI] [PubMed] [Google Scholar]
- 35.Bowman SA. Television-viewing characteristics of adults: correlations to eating practices and overweight and health status. Preventing chronic disease. 2006;3(2):A38. [PMC free article] [PubMed] [Google Scholar]
- 36.Kan C, Silva N, Golden SH, Rajala U, Timonen M, Stahl D, et al. A systematic review and meta-analysis of the association between depression and insulin resistance. Diabetes Care. 2013;36(2):480–9. doi: 10.2337/dc12-1442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Katon WJ, Rutter C, Simon G, Lin EH, Ludman E, Ciechanowski P, et al. The association of comorbid depression with mortality in patients with type 2 diabetes. Diabetes Care. 2005;28(11):2668–72. doi: 10.2337/diacare.28.11.2668. [DOI] [PubMed] [Google Scholar]
- 38.Chida Y, Hamer M. An association of adverse psychosocial factors with diabetes mellitus: a meta-analytic review of longitudinal cohort studies. Diabetologia. 2008;51(12):2168–78. doi: 10.1007/s00125-008-1154-1. [DOI] [PubMed] [Google Scholar]
- 39.Golden SH. A review of the evidence for a neuroendocrine link between stress, depression and diabetes mellitus. Curr Diabetes Rev. 2007;3(4):252–9. doi: 10.2174/157339907782330021. [DOI] [PubMed] [Google Scholar]
- 40.Kiecolt-Glaser JK, McGuire L, Robles TF, Glaser R. Psychoneuroimmunology: Pscyhological influences on immune function and health. Journal of Consulting & Clinical Psychology. 2002;70(3):537–47. doi: 10.1037//0022-006x.70.3.537. [DOI] [PubMed] [Google Scholar]
- 41.Miller G, Chen E, Cole SW. Health Psychology: Developing Biologically Plausible Models Linking the Social World and Physical Health. Annual Revew of Psychology. 2009;60:501–24. doi: 10.1146/annurev.psych.60.110707.163551. [DOI] [PubMed] [Google Scholar]
- 42.Rich-Edwards JW, Spiegelman D, Lividoti Hibert EN, Jun HJ, Todd TJ, Kawachi I, et al. Abuse in childhood and adolescence as a predictor of type 2 diabetes in adult women. Am J Prev Med. 2010;39(6):529–36. doi: 10.1016/j.amepre.2010.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mason SM, Wright RJ, Hibert EN, Spiegelman D, Jun HJ, Hu FB, et al. Intimate partner violence and incidence of type 2 diabetes in women. Diabetes Care. 2013;36(5):1159–65. doi: 10.2337/dc12-1082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Chambers EC, Tull ES, Fraser HS, Mutunhu NR, Sobers N, Niles E. The relationship of internalized racism to body fat distribution and insulin resistance among African adolescent youth. J Natl Med Assoc. 2004;96(12):1594–8. [PMC free article] [PubMed] [Google Scholar]
- 45.Samuel-Hodge CD, Headen SW, Skelly AH, Ingram AF, Keyserling TC, Jackson EJ, et al. Influences on day-to-day self-management of type 2 diabetes among African-American women: spirituality, the multi-caregiver role, and other social context factors. Diabetes Care. 2000;23(7):928–33. doi: 10.2337/diacare.23.7.928. [DOI] [PubMed] [Google Scholar]
- 46.Quinn MT, Cook S, Nash K, Chin MH. Addressing religion and spirituality in African Americans with diabetes. Diabetes Educ. 2001;27(5):643–4. 7–8, 55. doi: 10.1177/014572170102700505. [DOI] [PubMed] [Google Scholar]
- 47.Reeves RR, Adams CE, Dubbert PM, Hickson DA, Wyatt SB. Are Religiosity and Spirituality Associated with Obesity Among African Americans in the Southeastern United States (the Jackson Heart Study)? J Relig Health. 2012;51(1):32–48. doi: 10.1007/s10943-011-9552-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Polzer R, Miles MS. Spirituality and self-management of diabetes in African Americans. Journal of holistic nursing : official journal of the American Holistic Nurses' Association. 2005;23(2):230–50. doi: 10.1177/0898010105276179. discussion 51-4; quiz 26-7. [DOI] [PubMed] [Google Scholar]
- 49.Berkman L, Kawachi I. Social Epidemiology. Oxford University Press; 2000. [Google Scholar]
- 50.Brown AF, Karter AJ, Schillinger D. Impact of Ethnic and Socioeconomic Factors on Diabetes-Related Health and Management. In: Venkat Narayan DW, Gregg Edward W, Cowie Catherine C, editors. Diabetes Public Health: From Data to Policy. Oxford University Press; 2010. [Google Scholar]
- 51.Christakis NA, Fowler JH. The spread of obesity in a large social network over 32 years. N Engl J Med. 2007;357(4):370–9. doi: 10.1056/NEJMsa066082. [DOI] [PubMed] [Google Scholar]
- 52.Ford ME, Tilley BC, McDonald PE. Social support among African-American adults with diabetes, Part 2: A review. J Natl Med Assoc. 1998;90(7):425–32. [PMC free article] [PubMed] [Google Scholar]
- 53.Shojania KG, Ranji SR, McDonald KM, Grimshaw JM, Sundaram V, Rushakoff RJ, et al. Effects of quality improvement strategies for type 2 diabetes on glycemic control: a meta-regression analysis. JAMA : the journal of the American Medical Association. 2006;296(4):427–40. doi: 10.1001/jama.296.4.427. [DOI] [PubMed] [Google Scholar]
- 54.Pimouguet C, Le Goff M, Thiebaut R, Dartigues JF, Helmer C. Effectiveness of disease-management programs for improving diabetes care: a meta-analysis. CMAJ : Canadian Medical Association journal = journal de l'Association medicale canadienne. 2011;183(2):E115–27. doi: 10.1503/cmaj.091786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Hawthorne K, Robles Y, Cannings-John R, Edwards AG. Culturally appropriate health education for Type 2 diabetes in ethnic minority groups: a systematic and narrative review of randomized controlled trials. Diabetic medicine : a journal of the British Diabetic Association. 2010;27(6):613–23. doi: 10.1111/j.1464-5491.2010.02954.x. [DOI] [PubMed] [Google Scholar]
- 56.Chin MH, Clarke AR, Nocon RS, Casey AA, Goddu AP, Keesecker NM, et al. A roadmap and best practices for organizations to reduce racial and ethnic disparities in health care. J Gen Intern Med. 2012;27(8):992–1000. doi: 10.1007/s11606-012-2082-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Frank LD, Andresen MA, Schmid TL. Obesity relationships with community design, physical activity, and time spent in cars. Am J Prev Med. 2004;27(2):87–96. doi: 10.1016/j.amepre.2004.04.011. [DOI] [PubMed] [Google Scholar]
- 58.Austin SB, Melly SJ, Sanchez BN, Patel A, Buka S, Gortmaker SL. Clustering of fast-food restaurants around schools: a novel application of spatial statistics to the study of food environments. Am J Public Health. 2005;95(9):1575–81. doi: 10.2105/AJPH.2004.056341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lewis L, Sloane DC, Nascimento LM, et al. African American's access to health food options in South Los Angeles restaurants. Am J Public Health. 2005;95(4):668–73. doi: 10.2105/AJPH.2004.050260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Sturm R, Datar A. Body mass index in elementary school children, metropolitan area food prices and food outlet density. Public Health. 2005;119(12):1059–68. doi: 10.1016/j.puhe.2005.05.007. [DOI] [PubMed] [Google Scholar]
- 61.Kipke MD, Iverson E, Moore D, Booker C, Ruelas V, Peters AL, et al. Food and park environments: neighborhood-level risks for childhood obesity in east Los Angeles. J Adolesc Health. 2007;40(4):325–33. doi: 10.1016/j.jadohealth.2006.10.021. [DOI] [PubMed] [Google Scholar]
- 62.Auchincloss AH, Diez Roux AV, Brown DG, O'Meara ES, Raghunathan TE. Association of insulin resistance with distance to wealthy areas: the multi-ethnic study of atherosclerosis. Am J Epidemiol. 2007;165(4):389–97. doi: 10.1093/aje/kwk028. [DOI] [PubMed] [Google Scholar]
- 63.Auchincloss AH, Diez Roux AV, Brown DG, Erdmann CA, Bertoni AG. Neighborhood resources for physical activity and healthy foods and their association with insulin resistance. Epidemiology. 2008;19(1):146–57. doi: 10.1097/EDE.0b013e31815c480. [DOI] [PubMed] [Google Scholar]
- 64.Auchincloss AH, Diez Roux AV, Mujahid MS, Shen M, Bertoni AG, Carnethon MR. Neighborhood resources for physical activity and healthy foods and incidence of type 2 diabetes mellitus: the MultiEthnic study of Atherosclerosis. Archives of internal medicine. 2009;169(18):1698–704. doi: 10.1001/archinternmed.2009.302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Elliott M. The stress process in neighborhood context. Health Place. 2000;6(4):287–99. doi: 10.1016/s1353-8292(00)00010-1. S1353829200000101 [pii] [DOI] [PubMed] [Google Scholar]
- 66.Kling J, Liebman J, Klatz L. Experimental Analysis of Neighborhood Effect. Econometrica. 2007;75(1):83–119. [Google Scholar]
- 67.Development DoHaU. Expanding housing choices for HUD-assisted families. Washington, DC: 1996. [Google Scholar]
- 68.Ludwig J, Sanbonmatsu L, Gennetian L, Adam E, Duncan GJ, Katz LF, et al. Neighborhoods, obesity, and diabetes--a randomized social experiment. N Engl J Med. 2011;365(16):1509–19. doi: 10.1056/NEJMsa1103216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Chamany S, Silver LD, Bassett MT, Driver CR, Berger DK, Neuhaus CE, et al. Tracking diabetes: New York City's A1C Registry. The Milbank quarterly. 2009;87(3):547–70. doi: 10.1111/j.1468-0009.2009.00568.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Berends LM, Ozanne SE. Early determinants of type-2 diabetes. Best Pract Res Clin Endocrinol Metab. 2012;26(5):569–80. doi: 10.1016/j.beem.2012.03.002. [DOI] [PubMed] [Google Scholar]
- 71.Kavey RE, Daniels SR, Lauer RM, Atkins DL, Hayman LL, Taubert K. American Heart Association guidelines for primary prevention of atherosclerotic cardiovascular disease beginning in childhood. Circulation. 2003;107(11):1562–6. doi: 10.1161/01.cir.0000061521.15730.6e. [DOI] [PubMed] [Google Scholar]
- 72.Association AD. Standards of Medical Care- 2013. Diabetes Care. 2013;36(Supplement 1):S11–S66. doi: 10.2337/dc13-S011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Kelder SH, Perry CL, Klepp KI, Lytle LL. Longitudinal tracking of adolescent smoking, physical activity, and food choice behaviors. Am J Public Health. 1994;84(7):1121–6. doi: 10.2105/ajph.84.7.1121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Telama R. Tracking of physical activity from childhood to adulthood: a review. Obesity facts. 2009;2(3):187–95. doi: 10.1159/000222244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Banerjee C, Moon YP, Paik MC, Rundek T, Mora-McLaughlin C, Vieira JR, et al. Duration of diabetes and risk of ischemic stroke: the Northern Manhattan Study. Stroke. 2012;43(5):1212–7. doi: 10.1161/STROKEAHA.111.641381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76•.Power C, Kuh D, Morton S. From developmental origins of adult disease to life course research on adult disease and aging: insights from birth cohort studies. Annu Rev Public Health. 2013;34:7–28. doi: 10.1146/annurev-publhealth-031912-114423. This article provides the conceptual frameworks guiding life course research of adult diseases, and reviews evidence on the influence of socioeconomic conditions across generations and lifecourse on adult health outcomes. [DOI] [PubMed] [Google Scholar]
- 77.Galea S, Link BG. Six paths for the future of social epidemiology. Am J Epidemiol. doi: 10.1093/aje/kwt148. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Golden SH. A review of the evidence for a neuroendocrine link between stress, depression and diabetes mellitus. Current diabetes reviews. 2007;3(4):252–9. doi: 10.2174/157339907782330021. [DOI] [PubMed] [Google Scholar]
- 79.Greenfield EA, Marks NF. Violence from parents in childhood and obesity in adulthood: using food in response to stress as a mediator of risk. Social Science and Medicine. 2009;68(5):791–8. doi: 10.1016/j.socscimed.2008.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Suglia SF, Staudenmayer J, Cohen S, Enlow MB, Rich-Edwards JW, Wright RJ. Cumulative Stress and Cortisol Disruption among Black and Hispanic Pregnant Women in an Urban Cohort. Psychol Trauma. 2010;2(4):326–34. doi: 10.1037/a0018953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Kuzawa CW, Sweet E. Epigenetics and the embodiment of race: developmental origins of US racial disparities in cardiovascular health. American journal of human biology : the official journal of the Human Biology Council. 2009;21(1):2–15. doi: 10.1002/ajhb.20822. [DOI] [PubMed] [Google Scholar]
- 82.McEwen BS. Brain on stress: how the social environment gets under the skin. Proceedings of the National Academy of Sciences of the United States of America; 2012; pp. 17180–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Szyf M, McGowan P, Meaney MJ. The social environment and the epigenome. Environmental and molecular mutagenesis. 2008;49(1):46–60. doi: 10.1002/em.20357. [DOI] [PubMed] [Google Scholar]
- 84.Terry MB, Delgado-Cruzata L, Vin-Raviv N, Wu HC, Santella RM. DNA methylation in white blood cells: association with risk factors in epidemiologic studies. Epigenetics : official journal of the DNA Methylation Society. 2011;6(7):828–37. doi: 10.4161/epi.6.7.16500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Waki H, Yamauchi T, Kadowaki T. The epigenome and its role in diabetes. Current diabetes reports. 2012;12(6):673–85. doi: 10.1007/s11892-012-0328-x. [DOI] [PubMed] [Google Scholar]
- 86.Slomko H, Heo HJ, Einstein FH. Minireview: Epigenetics of obesity and diabetes in humans. Endocrinology. 2012;153(3):1025–30. doi: 10.1210/en.2011-1759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Heijmans BT, Tobi EW, Stein AD, Putter H, Blauw GJ, Susser ES, et al. Persistent epigenetic differences associated with prenatal exposure to famine in humans. Proceedings of the National Academy of Sciences of the United States of America; 2008; pp. 17046–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Godfrey KM, Sheppard A, Gluckman PD, Lillycrop KA, Burdge GC, McLean C, et al. Epigenetic gene promoter methylation at birth is associated with child's later adiposity. Diabetes. 2011;60(5):1528–34. doi: 10.2337/db10-0979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Toperoff G, Aran D, Kark JD, Rosenberg M, Dubnikov T, Nissan B, et al. Genome-wide survey reveals predisposing diabetes type 2-related DNA methylation variations in human peripheral blood. Human molecular genetics. 2012;21(2):371–83. doi: 10.1093/hmg/ddr472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Borghol N, Suderman M, McArdle W, Racine A, Hallett M, Pembrey M, et al. Associations with early-life socio-economic position in adult DNA methylation. Int J Epidemiol. 2012;41(1):62–74. doi: 10.1093/ije/dyr147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91•.Tehranifar P, Wu HC, Fan X, Flom JD, Ferris JS, Cho YH, et al. Early life socioeconomic factors and genomic DNA methylation in mid-life. Epigenetics : official journal of the DNA Methylation Society. 2013;8(1):23–7. doi: 10.4161/epi.22989. This article attempts to link social factors from a lifecourse perspective to epigenetic modifications (DNA methylation) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Subramanyam MA, Diez-Roux AV, Pilsner JR, Villamor E, Donohue KM, Liu Y, et al. Social factors and leukocyte DNA methylation of repetitive sequences: the multi-ethnic study of atherosclerosis. PloS one. 2013;8(1):e54018. doi: 10.1371/journal.pone.0054018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.McGuinness D, McGlynn LM, Johnson PC, MacIntyre A, Batty GD, Burns H, et al. Socio-economic status is associated with epigenetic differences in the pSoBid cohort. Int J Epidemiol. 2012;41(1):151–60. doi: 10.1093/ije/dyr215. [DOI] [PubMed] [Google Scholar]
- 94.Engelgau MM, Geiss LS, Saaddine JB, Boyle JP, Benjamin SM, Gregg EW, et al. The evolving diabetes burden in the United States. Annals of internal medicine. 2004;140(11):945–50. doi: 10.7326/0003-4819-140-11-200406010-00035. [DOI] [PubMed] [Google Scholar]
- 95.Narayan KM, Bowman BA, Engelgau ME. Prevention of type 2 diabetes. Bmj. 2001;323(7304):63–4. doi: 10.1136/bmj.323.7304.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999-2010. JAMA : the journal of the American Medical Association. 2012;307(5):491–7. doi: 10.1001/jama.2012.39. [DOI] [PubMed] [Google Scholar]
- 97.Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346(6):393–403. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Diabetes Prevention Program Research Group. Knowler WC, Fowler SE, Hamman RF, Christophi CA, Hoffman HJ, et al. 10-year follow-up of diabetes incidence and weight loss in the Diabetes Prevention Program Outcomes Study. Lancet. 2009;374(9702):1677–86. doi: 10.1016/S0140-6736(09)61457-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Ali MK, Echouffo-Tcheugui J, Williamson DF. How effective were lifestyle interventions in real-world settings that were modeled on the Diabetes Prevention Program? Health affairs. 2012;31(1):67–75. doi: 10.1377/hlthaff.2011.1009. [DOI] [PubMed] [Google Scholar]
- 100.Green LW, Brancati FL, Albright A Primary Prevention of Diabetes Working G. Primary prevention of type 2 diabetes: integrative public health and primary care opportunities, challenges and strategies. Family practice. 2012;29(1):i13–23. doi: 10.1093/fampra/cmr126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Hernandez LM, Blazer DG. Genes, Behavior, and the Social Environment: Moving Beyond the Nature/Nurture Debate. The National Academies Collection: Reports funded by National Institutes of Health; Washington (DC): 2006. [PubMed] [Google Scholar]
- 102.Warnecke RB, Oh A, Breen N, Gehlert S, Paskett E, Tucker KL, et al. Approaching health disparities from a population perspective: the National Institutes of Health Centers for Population Health and Health Disparities. Am J Public Health. 2008;98(9):1608–15. doi: 10.2105/AJPH.2006.102525. [DOI] [PMC free article] [PubMed] [Google Scholar]


