Abstract
Background
Little information exists about what primary care physicians (PCPs) and patients experience if patients are invited to read their doctors’ office notes.
Objective
To evaluate the effect on doctors and patients of facilitating patient access to visit notes over secure Internet portals.
Design
Quasi-experimental trial of PCPs and patient volunteers in a year-long program that provided patients with electronic links to their doctors’ notes.
Setting
Primary care practices at Beth Israel Deaconess Medical Center (BIDMC) in Massachusetts, Geisinger Health System (GHS) in Pennsylvania, and Harborview Medical Center (HMC) in Washington.
Participants
105 PCPs and 13 564 of their patients who had at least 1 completed note available during the intervention period.
Measurements
Portal use and electronic messaging by patients and surveys focusing on participants’ perceptions of behaviors, benefits, and negative consequences.
Results
11 797 of 13 564 patients with visit notes available opened at least 1 note (84% at BIDMC, 92% at GHS, and 47% at HMC). Of 5391 patients who opened at least 1 note and completed a postintervention survey, 77% to 87% across the 3 sites reported that open notes helped them feel more in control of their care; 60% to 78% of those taking medications reported increased medication adherence; 26% to 36% had privacy concerns; 1% to 8% reported that the notes caused confusion, worry, or offense; and 20% to 42% reported sharing notes with others. The volume of electronic messages from patients did not change. After the intervention, few doctors reported longer visits (0% to 5%) or more time addressing patients’ questions outside of visits (0% to 8%), with practice size having little effect; 3% to 36% of doctors reported changing documentation content; and 0% to 21% reported taking more time writing notes. Looking ahead, 59% to 62% of patients believed that they should be able to add comments to a doctor’s note. One out of 3 patients believed that they should be able to approve the notes’ contents, but 85% to 96% of doctors did not agree. At the end of the experimental period, 99% of patients wanted open notes to continue and no doctor elected to stop.
Limitations
Only 3 geographic areas were represented, and most participants were experienced in using portals. Doctors volunteering to participate and patients using portals and completing surveys may tend to offer favorable feedback, and the response rate of the patient surveys (41%) may further limit generalizability.
Conclusion
Patients accessed visit notes frequently, a large majority reported clinically relevant benefits and minimal concerns, and virtually all patients wanted the practice to continue. With doctors experiencing no more than a modest effect on their work lives, open notes seem worthy of widespread adoption.
Primary Funding Source
The Robert Wood Johnson Foundation, the Drane Family Fund, the Richard and Florence Koplow Charitable Foundation, and the National Cancer Institute.
Electronic medical records and secure patient portals hold exciting potential for more active patient involvement in care and improved communication between patients and clinicians. These technologies facilitate a potentially disruptive innovation: Doctors can readily invite patients to read and share their visit notes and even contribute to the notes’ formulation. We conducted a quasi-experimental study, OpenNotes, in which more than 100 primary care physicians (PCPs) volunteered to invite more than 20 000 of their patients to review online the notes that the doctors wrote and signed after an office visit (1, 2).
Drawing on existing literature, including small studies of patients with chronic illness (3– 6), we developed 3 principal hypotheses. First, most patients would read the notes, and those who did would report both greater engagement in care and improved management of health and illness. Second, the intervention would have few adverse effects on the doctors’ frenetic work lives. Third, at the end of the approximately 1-year intervention, a large percentage of doctors and patients would choose to continue with open notes.
Before starting the intervention, we queried doctors and patients about their attitudes and expectations about open notes (1). The PCPs who declined to participate expressed considerable worries about disruption of workflow, and many predicted that the notes would confuse or worry their patients. The PCPs who volunteered to participate had fewer worries, with many anticipating improved communication and patient education.
In striking contrast to both groups of doctors, the vast majority of patients were highly enthusiastic, even though they were demographically and geographically diverse. They anticipated many benefits, and few expressed concerns about being worried or confused by the notes. In this article, we report our principal findings from 1 year of experience with the intervention.
Methods
The OpenNotes intervention and results of baseline surveys have been described previously (1, 2). Primary care physicians affiliated with an urban hospital (Beth Israel Deaconess Medical Center [BIDMC] in Boston, Massachusetts), predominantly rural practices (Geisinger Health System [GHS] in Pennsylvania), and an urban safety-net hospital (Harborview Medical Center [HMC] in Seattle, Washington) were invited to offer their patients electronic access to office notes. Patients at BIDMC and GHS had experience with established electronic portals, whereas those at HMC did not. Eligible doctors and their patients were surveyed about expectations before initiation. During the intervention, participating patients were notified electronically when office notes were signed and ready for viewing.
All PCPs were eligible except for housestaff, fellows, and those in BIDMC community practices without portal-compatible records. Participating doctors’ names were posted on the study Web site (7). At BIDMC and GHS, all patients who used portals were invited electronically to participate in the intervention unless specifically excluded by the PCP (158 at BIDMC and 139 at GHS). Patients at HMC were invited individually, excluding 1023 with primarily major mental illness, substance abuse, or both (1, 2).
The names of doctors who left the study were removed from the Web site, and their participating patients were notified through secure messages before access was terminated. Patients of doctors who left the practice were notified according to each site’s policy; access to existing notes was retained at BIDMC and HMC but lost at GHS. At all sites, patient access to notes was terminated immediately on request to withdraw from the study.
Postintervention Questionnaire Design
To permit comparisons between preintervention expectations and actual experiences, the postintervention surveys were based largely on the baseline surveys. To develop additional items for the postintervention surveys, we conducted informal discussions with more than 20 doctors from all 3 sites and solicited suggestions from more than 10 doctors (both participating and nonparticipating) at a BIDMC research conference. To develop items for the patient survey, we used secure e-mail to contact 100 randomly selected BIDMC patients who had opened notes 2 or more times at least 2 months apart and conducted semi-structured phone interviews with the first 25 who responded (interview guide available on request).
Next, we drafted questionnaires and left many questions from the baseline surveys either the same or with verb tenses changed (for example, “I would be better prepared for visits” became “I am better prepared for visits”). Response options similarly changed from level of concern (for example, options for “My visits will take significantly longer” included “not a concern,” “somewhat concerned,” and so forth) to “yes” or “no” assertions of fact after the intervention. Two participating doctors from GHS and 2 from HMC then pretested the doctor survey online and suggested no further revisions. Fourteen BIDMC patients of an investigator, who were therefore excluded from analysis, critiqued the draft postintervention patient survey and offered no further revisions. Each patient interviewed or who participated in the survey pretest received a $10 gift card.
The doctor and patient surveys were designed to take less than 20 minutes to complete. Both included several opportunities for free-text commentary, including what doctors considered the best and most difficult aspects of open notes. Except for questions to patients about demographic characteristics, free-text questions, and skip patterns, all items required a response. Respondents could leave the survey at any time; all responses from completed or partially completed surveys were recorded and included in the analysis (surveys available from the authors on request).
Conducting the Surveys
Participants were surveyed in fall 2011 after 12 to 19 months of experience with open notes, a range reflecting different intervention start dates among the 3 sites. All surveys were done online using SurveyGizmo, version 3.0 (Widgix, Boulder, Colorado). Participating doctors and patients received invitations electronically except for patients who withdrew, died, or had portal accounts deactivated during the intervention period. Survey responses were kept confidential; all analyses used only study identification numbers.
Both patients and doctors at all 3 locations received up to 3 e-mailed reminders. Patients at BIDMC received up to 4 reminders. At HMC, secure messaging was not available, so patients were contacted through personal e-mail addresses to complete the survey, followed by 3 e-mail reminders, up to 3 telephone calls, and in-practice follow-up. In each site, doctors had up to 10 weeks to respond; patients were allowed 12 weeks. Potential participants were offered incentives, such as raffle entries and gift cards, according to individual site policies.
Use Data
Because of differences in portal technologies, data documenting portal use by patients and e-mail messaging from patients to providers varied by site. Both BIDMC and HMC recorded each time a patient clicked the “Notes” tab, but they did not record which note was subsequently opened; GHS captured the date and time that each individual visit note was opened. All 3 sites recorded date and time information when notifications about available notes were sent to patients.
The HMC portal lacked messaging functionality, but BIDMC and GHS collected date and time information about all secure clinical messages from patients in the 12 months before and during the first 12 months of the intervention. All sites opened visit notes, with BIDMC also opening notes documenting letters and phone calls.
Conclusion of the Intervention
After 12 months of the intervention, doctors and patients at BIDMC and GHS were notified that the original study period had ended and that they could stop participating; otherwise, they continued with open notes. At HMC, patient access to the study portal ended at the conclusion of the intervention per the study protocol; however, patients were invited to contact their providers if they were interested in enrolling in a new portal system that was becoming available.
Statistical Analysis
Survey and electronic data from doctors and patients were analyzed by site using descriptive methods. Pre- and postintervention surveys from doctors who completed the intervention and postintervention surveys from patients who opened at least 1 note were included in the analysis. “Agree”/“somewhat agree” and “somewhat disagree”/“disagree” response options on the surveys were pooled for analysis.
To determine whether doctors with larger panels reported greater impacts on their practice from open notes, we compared survey responses from doctors according to panel size (with a cut point of 1000 patients) by using the Cochran–Mantel–Haenszel test (8) adjusted for study site. Analyses using alternate cut points of up to 1800 patients did not differ materially from those presented.
The proportion of patients who opened at least 1 note, regardless of survey participation, was ascertained for each site, and the age and sex of patients who opened at least 1 note were compared with those of patients who opened no notes or had no notes available. To compare the difference in monthly rates of e-mail volume before and during the intervention, we used a regression model with terms for month, period (pre- and postintervention), and the interaction between these 2 terms and accounted for the autocorrelation in the time-series data. Data analyses were performed using SAS software, version 9.3 (SAS Institute, Cary, North Carolina) (9).
The BIDMC was the coordinating center for the project; its institutional review board approved the overall project. The institutional review boards at GHS and the University of Washington approved the implementation at their sites.
Role of the Funding Source
The Robert Wood Johnson Foundation’s Pioneer Portfolio provided the major funding, supplemented by the Drane Family Fund, the Richard and Florence Koplow Charitable Foundation, and the National Cancer Institute. The funding sources had no role in designing or conducting the study, analyzing the data, or preparing the manuscript, or in the decision to submit this manuscript for publication.
Results
PCP and Patient Participation
Of the 113 doctors who started the intervention across all 3 sites, 105 (93%) completed the study (Appendix Figure 1, available at www.annals.org). All but one of those who completed the study submitted postintervention surveys, and 99 submitted both pre- and postintervention surveys. According to their surveys, BIDMC doctors were more likely to dictate notes and at least half of BIDMC and GHS doctors communicated daily by e-mail with patients, compared with 5% of HMC doctors (Table 1).
Table 1.
Characteristics of 105 PCPs Who Finished the Intervention, by Study Site
| PCP Characteristic | Study Site, %
|
||
|---|---|---|---|
| BIDMC (n = 39) | GHS (n = 24) | HMC (n = 42) | |
| Age at baseline | |||
|
| |||
| 30–39 y | 21 | 22 | 45 |
|
| |||
| 40–49 y | 41 | 22 | 37 |
|
| |||
| 50–59 y | 28 | 52 | 18 |
|
| |||
| ≥60 y | 10 | 4 | 0 |
|
| |||
| No response | 0 | 4 | 10 |
|
| |||
| Women | 49 | 21 | 55 |
| Direct care, n* | |||
|
| |||
| <15 h/wk | 39 | 8 | 81 |
|
| |||
| 15–35 h/wk | 56 | 50 | 19 |
|
| |||
| >36 h/wk | 5 | 38 | 0 |
|
| |||
| No response | 0 | 4 | 0 |
| Way of documenting most notes* | |||
|
| |||
| Dictate | 77 | 4 | 5 |
|
| |||
| Type using templates | 13 | 79 | 43 |
|
| |||
| Type entire note/other | 10 | 13 | 52 |
|
| |||
| No response | 0 | 4 | 0 |
| How often PCPs communicate with patients by e-mail* | |||
|
| |||
| Never | 3 | 0 | 5 |
|
| |||
| Less than once per week | 0 | 0 | 52 |
|
| |||
| At least once per week but not daily | 46 | 17 | 38 |
|
| |||
| At least once daily | 51 | 79 | 5 |
|
| |||
| No response | 0 | 4 | 0 |
|
| |||
| Percentage of entire panel with whom PCPs communicate by e-mail* | |||
| 0–10 | 20 | 8 | 59 |
|
| |||
| 11–25 | 43 | 46 | 19 |
|
| |||
| 26–50 | 26 | 42 | 17 |
|
| |||
| >50 | 8 | 0 | 0 |
|
| |||
| No response | 3 | 4 | 5 |
BIDMC = Beth Israel Deaconess Medical Center; GHS = Geisinger Health System; HMC = Harborview Medical Center; PCP = primary care physician.
Percentages displayed reflect postintervention survey responses.
Before the start of the intervention, 22 703 patients were notified that their doctors planned to participate and would offer them access to their notes (Appendix Figure 2, available at www.annals.org). At BIDMC, the patients notified represented 31% of the doctors’ full panel of patients (ranging from 4% to 88% of individual doctors’ panels); at GHS, they represented 21% of the doctors’ patients (range, 0.4% to 43%). Each HMC doctor had fewer than 20 patients in the study.
Among the 19 371 patients (85% of 22 703) who completed the intervention, 13 564 had at least 1 note available during the intervention period. Overall, 41% of these 13 564 patients completed postintervention surveys, with the highest response rates among patients who opened at least 1 note. At all 3 sites, patients with notes available were older than those with no notes (Appendix Table 1, available at www.annals.org). Patients who opened 1 or more notes had a somewhat greater number of notes than those who did not open notes.
Patient Experiences
Among patients with notes available, 84% at BIDMC, 92% at GHS, and 47% at HMC opened at least 1 note. At BIDMC and GHS, 100% of the signed notes triggered notifications to patients. At GHS, where systems could track each time patients accessed individual notes, 92% of patients with notes opened at least 1 note and 87% opened all of their notes. At BIDMC, 90% of patients with 4 or more notes opened at least 1 note, compared with 74% of those with only 1 note.
Defects in the note-detection system at HMC resulted in only 49% of notes triggering notification e-mails. However, no effect on note viewing was evident: 46% of HMC patients who received at least 1 notification viewed a note versus 48% of those without notifications. In the postintervention survey, the most commonly selected reasons for not reading available notes in all sites were “forgot notes were available online” (33%), “could not find the note online” (23%), and “no reason” (17%).
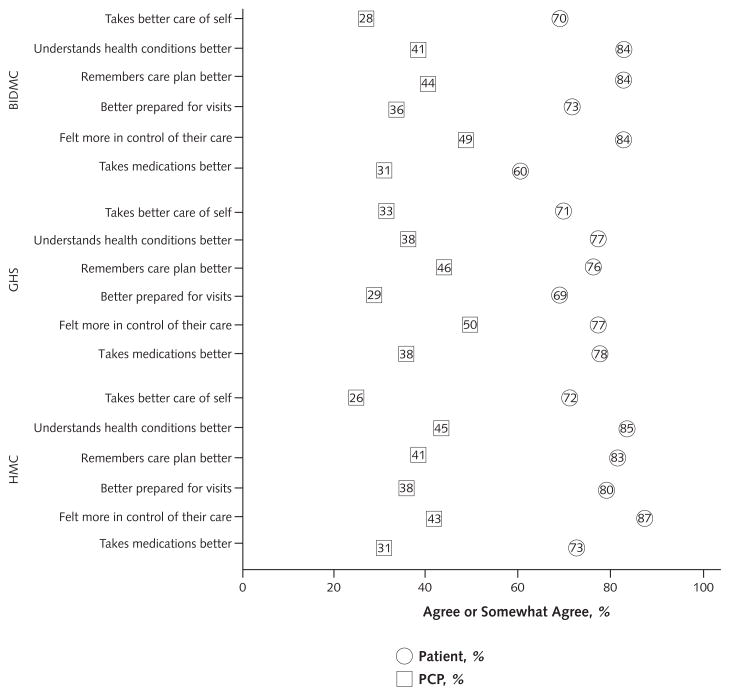
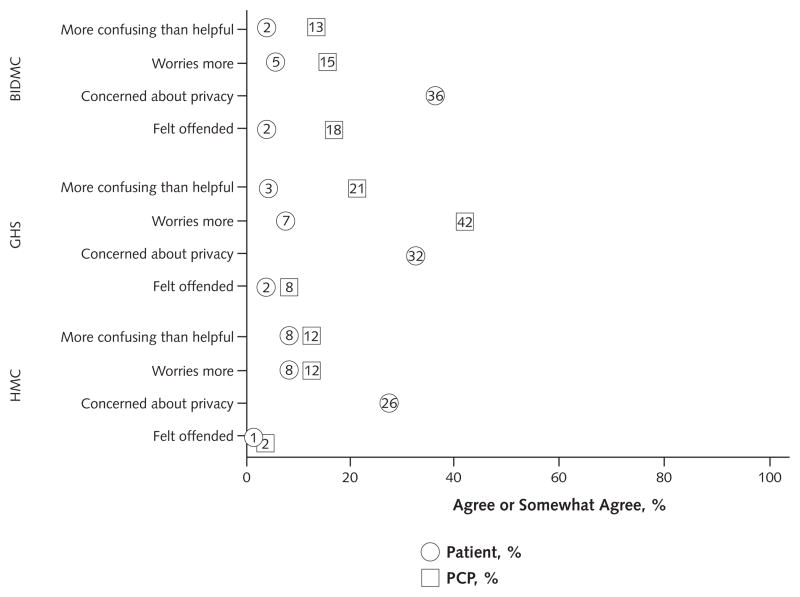
Among patients indicating in the survey that they read at least 1 note, 19% reported that they had mentioned to their doctors that they had read notes online. A large majority of patients perceived benefits, and few reported downsides of open notes; however, one third of patients were concerned about privacy (Figures 1 and 2).
Figure 1. PCPs and patients who “agreed” or “somewhat agreed” with statements about the potential benefits of open notes to patients.
The percentage that responded “don’t know” is not displayed. PCPs who responded “don’t know” ranged from 8% to 26%. Patients who responded “don’t know” ranged from 0% to 12%. BIDMC = Beth Israel Deaconess Medical Center; GHS = Geisinger Health System; HMC = Harborview Medical Center; PCP = primary care physician.
Figure 2. PCPs and patients who “agreed” or “somewhat agreed” with statements about the potential risks of open notes to patients.
The percentage that responded “don’t know” is not displayed. PCPs who responded “don’t know” ranged from 4% to 19%. Patients who responded “don’t know” ranged from 0% to 3%. PCPs were not asked about patients’ privacy concerns. BIDMC = Beth Israel Deaconess Medical Center; GHS = Geisinger Health System; HMC = Harborview Medical Center; PCP = primary care physician.
Twenty percent of patients at BIDMC and GHS and 42% at HMC reported sharing their notes with others, most often family members or relatives. Nearly 99% of patient respondents at BIDMC, GHS, and HMC wanted continued access to their visit notes, and 86% at BIDMC, 87% at GHS, and 89% at HMC agreed that open notes would be a somewhat or very important factor in choosing a future doctor or health plan.
Doctor Experiences
Among doctors who answered the postintervention survey, most estimated that conversations with patients about open notes occurred less than monthly (46% at BIDMC, 67% at GHS, and 73% at HMC). Moreover, 38% at BIDMC, 30% at GHS, and 43% at HMC indicated that they could not estimate the proportion of their patients who read notes because no or very few patients ever mentioned it. On the basis of date and time stamps recorded in the messaging systems, e-mail volume from the 13 564 patients with 1 or more open notes to their doctors (or their representatives) at BIDMC and GHS did not change significantly between the 12 months before the intervention and the next 12 months during the intervention (data not shown).
Before the intervention, both participating and non-participating doctors worried about the effect of open notes on their practices. However, in the postintervention survey, workload concerns of participating doctors had diminished markedly (Table 2). Most individual doctors’ responses did not change between the pre- and postintervention surveys; those whose responses did change most often expected an effect in the preintervention survey and then reported no effect in the postintervention survey (Appendix Tables 2 to 4, available at www.annals.org). A few PCPs reported changing their documentation for open notes (Table 2). At BIDMC, doctors could “monitor” a note, thereby blocking patient access; 3 doctors reported using this option, citing the frequency as “very few,” “occasionally,” or “only once.”
Table 2.
Effect of Open Visit Notes on PCP Practice
| Statement | PCPs Who Answered “Yes,” by Study Site, %
|
PCPs Who Answered “Yes,” by Study Site, %
|
||||||
|---|---|---|---|---|---|---|---|---|
| BIDMC
|
GHS
|
HMC
|
||||||
| Nonparticipating
|
Participating
|
Nonparticipating
|
Participating*
|
Participating†
|
||||
| Preintervention Survey (n = 12)‡ | Preintervention Survey (n = 39) | Postintervention Survey (n = 39) | Preintervention Survey (n = 51)‡ | Preintervention Survey (n = 22) | Postintervention Survey (n = 22) | Preintervention Survey (n = 38) | Postintervention Survey (n = 38) | |
| Visits will/did take significantly longer | 58 | 23 | 3 | 71 | 32 | 5 | 21 | 0 |
|
| ||||||||
| Will/did spend more time addressing patient questions outside of visits§ (not asked) | 83 (–) | 49 (–) | 8 (38) | 84 (–) | 45 (–) | 0 (32) | 34 (–) | 0 (42) |
|
| ||||||||
| Will/did spend more time writing/dictating/editing my notes | 58 | 46 | 21 | 65 | 36 | 14 | 34 | 0 |
|
| ||||||||
| Will be/was less candid in documentation | 75 | 33 | 28 | 61 | 32 | 9 | 39 | 11 |
|
| ||||||||
| I will/did change the way I address these topics in my notes: | ||||||||
|
| ||||||||
| Cancer/possibility of cancer | 58 | 33 | 26 | 49 | 18 | 18 | 26 | 3 |
|
| ||||||||
| Mental health | 67 | 44 | 36 | 69 | 27 | 27 | 53 | 11 |
|
| ||||||||
| Substance abuse | 75 | 38 | 28 | 59 | 32 | 23 | 42 | 8 |
|
| ||||||||
| Overweight/obesity | 58 | 18 | 33 | 47 | 18 | 5 | 21 | 5 |
|
| ||||||||
| Medical care will be/was delivered more efficiently | 0 | 23 | 20 | 14 | 27 | 32 | 37 | 11 |
|
| ||||||||
| Notes can be useful for patient communication and education|| | 67 | 77 | 82 | 45 | 91 | 91 | 84 | 87 |
BIDMC = Beth Israel Deaconess Medical Center; GHS = Geisinger Health System; HMC = Harborview Medical Center; PCP = primary care physician.
Participating PCPs who did not submit both pre- and postintervention surveys were excluded from analysis (n = 2).
Participating PCPs who did not submit both pre- and postintervention surveys were excluded from analysis (n = 4).
Published previously in reference 1.
Postintervention surveys asked PCPs to estimate how many of their patients read their notes; those responding “none” or “cannot estimate …” were not asked this question.
Represents the percentage of PCPs who agreed or somewhat agreed with the statement (instead of “yes”).
In general, approximately one half as many doctors as patients perceived benefits to patients, but many doctors responded “don’t know” to questions about patient effects (Figure 1). Doctors generally did not perceive negative patient consequences, although 42% of PCPs from GHS reported that patients worried more from reading notes (Figure 2).
Excluding HMC doctors, who individually had few participating patients, we also examined the responses of doctors completing both pre- and postintervention surveys according to their panel size. Despite limited power due to small strata by panel size, we found a significant difference only in the time spent writing or dictating notes. Four of 37 doctors (10.8%) with smaller panels reported spending more time writing or dictating notes, compared with 7 of 24 doctors (29.2%) with panels of 1000 or more patients (P = 0.019).
Among the 73 out of 104 PCPs (70%) who responded with free text to the question, “What was the best thing about opening your notes to patients online?,” doctors most frequently commented about strengthened relationships with some of their patients (including enhanced trust, transparency, communication, and shared decision making) and that participation was easier than expected or seemed to make no difference to their work lives. They often noted that some patients seemed more activated or empowered. Doctors also wrote that shared notes may have improved patient satisfaction, patient safety, the ability to reinforce the office visit, and the opportunity for patient education. A few reported composing “better notes,” and in their comments, some cited increased efficiency.
When asked about the most difficult aspect of open notes, the most common comment among the 77 out of 104 responding PCPs (74%) was that nothing was difficult and that they experienced no changes in their practice. Although several doctors acknowledged fears about additional time burden and offending or worrying patients, they wrote that these concerns did not materialize. Some commented on the extra time needed for writing, editing, or explaining notes to patients. Among them, some framed such efforts as learning “better documentation—a good thing.”
Several doctors struggled with the notion of a one-size-fits-all note, arguing that 1 document cannot address the needs of billing, other doctors, and patients (10). A few changed their own use of the note; for example, eliminating personal reminders about sensitive patient issues, excluding alternate diagnoses to consider for the next visit, restricting note content, or avoiding communication with colleagues through the note. Some PCPs expressed concerns about patient literacy or access to notes, and a few commented on challenges in deciding whether to hide notes from selected patients.
At the conclusion, a large majority of responding PCPs (85% at BIDMC, 91% at GHS, and 88% at HMC) reported that “making visit notes available to patients online is a good idea.” When asked about continuing open notes, a few reported that they would prefer not to continue (26% at BIDMC, 17% at GHS, and 19% at HMC). However, when BIDMC and GHS doctors were offered the option to decline further participation at the end of the 12-month intervention for which they had signed consent, none asked to stop.
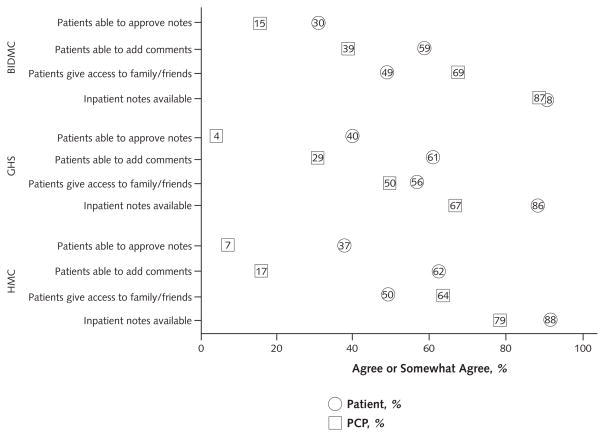
Future of Notes
When asked to consider the future, approximately 3 out of 5 patients and approximately one third of doctors agreed that patients should be able to add comments to doctors’ notes. Few PCPs believed that patients should be able to approve the content of notes; however, approximately one third of patients agreed that they should be able to do so. Most patients and doctors agreed that patients should have the option to grant caregivers access to notes and that inpatient notes should be made available on the portals (Figure 3).
Figure 3. PCPs and patients who “agreed” or “somewhat agreed” with statements about the future of open notes.
The percentage that responded “no opinion” is not displayed. PCPs who responded “no opinion” ranged from 0% to 13%. Patients who responded “no opinion” ranged from 6% to 19%. BIDMC = Beth Israel Deaconess Medical Center; GHS = Geisinger Health System; HMC = Harborview Medical Center; PCP = primary care physician.
Discussion
Patients were enthusiastic about open access to PCP visit notes; 99% of those who completed surveys recommended that this transparency continue. Overall, a large majority opened some or all of their notes, and almost 90% believed that open notes would affect their decisions when seeking care in the future. The vast majority reported an increased sense of control, greater understanding of their medical issues, improved recall of their plans for care, and better preparation for future visits. Perhaps most important clinically, a remarkable number reported becoming more likely to take medications as prescribed. In contrast to the fears of many doctors, few patients reported being confused, worried, or offended by what they read.
These benefits were achieved with far less impact on the work life of doctors and their staffs than anticipated. Few PCPs reported requiring longer encounters, taking more time with visits, or addressing more questions outside of visits, and none opted to discontinue open notes at the end of the year-long intervention period. Although a sizable minority reported changing the way that their notes addressed substance abuse, mental health issues, cancer, and obesity, few spent more time preparing their notes. E-mail traffic from patients was unchanged; many doctors reported that they did not know whether their patients were reading the notes; and hallway conversations, focus groups, and free-text survey comments suggested that many doctors were astonished by how little effect the intervention had on their practices. Several wondered whether the intervention had been implemented. One comment may best summarize their collective experience: “My fears: Longer notes, more questions, and messages from patients. In reality, it was not a big deal.”
Why was there so little impact on the lives of the doctors? Our findings are consistent with small studies focusing on patients with chronic illnesses and with the experience of M.D. Anderson Cancer Center, a large hospital that offers open notes to the patients of all of its doctors (4, 11, 12). Perhaps for every patient who engendered more activity from the staff or doctor, another may have read the doctor’s notes and found his or her questions answered. We also suspect that patients are both respectful of doctors’ time and resourceful in addressing questions that notes raise, perhaps more so than many doctors might assume.
We did not examine individual notes, and a recent study suggests that doctors may not change documentation markedly in the presence of open notes (13). However, from our previous interviews, focus groups, and preintervention surveys, we expected some doctors to report changing documentation, in particular when addressing potentially sensitive issues. A substantial minority reported doing so, but we cannot judge the clinical effect of such changes, including their reported change in “candor.” For example, some doctors reported using “body mass index” in place of “obesity,” fearing that patients would find the latter pejorative. However, patient responses may differ from doctors’ expectations. One patient’s comment reflected that of several others: “In his notes, the doctor called me ‘mildly obese.’ This prompted my immediate enrollment in Weight Watchers and daily exercise. I didn’t think I had gained that much weight. I’m determined to reverse that comment by my next check-up.” In a similar way, although many doctors at HMC excluded patients with substance abuse from the study (1), several PCPs commented that some of these patients both communicated better and had improved outcomes after seeing their doctors’ concerns in writing.
Patients in this study received e-mails when a doctor’s note was signed and posted to their portal, but whether to open the note was up to the patient. A remarkable majority of existing portal users at GHS and BIDMC (approximately 90%) opened all or some of their notes. At HMC, the number was smaller (47%). Although the notification system was inconsistent there, we found no evidence that it contributed to the lower proportion of patients opening notes, and this finding may reflect that HMC patients had been personally invited to participate in the intervention and were new to using a portal, compared with self-selected and experienced portal users at the other sites. Further, the HMC population may have had limited Internet and computer access because many did not have their own computers. Regardless of where they lived, virtually all patients indicated that they should have the option to read notes, an opinion consistent with a patient’s comment before the study began: “I don’t know if I want to read (my entire medical record), but I want to have it.” (14).
In striking contrast to the doctors’ predictions, few patients reported being worried, confused, or offended by notes they read. We suspect that fear or uncertainty of what is in the doctor’s “black box” may engender far more anxiety than what is actually written, and patients who are especially likely to react negatively to notes may self-select not to read them. Nevertheless, we anticipate that some may be disturbed in the short term by reading their notes, and doctors will need to work with patients to prevent such harms, ideally by talking frankly with them or agreeing proactively that some things are, at times, best left unread. An option to block selected notes from a patient’s view may also be helpful as both clinicians and patients tailor care in the future.
Improving adherence to medical regimens has long been an enormous stumbling block in medical practice, and the recent increase in out-of-pocket costs for medications compounds the challenge (15). We were excited to see that more than half of patients who received medications reported improved adherence, consistent with findings about general adherence from another open-records study (12). Although self-reports fall short of objective data, open notes may prove to be a simple intervention that has an important effect on medication adherence. Comments in focus groups, individual patient interviews, and free-text survey commentary gave credence to the striking data in Figure 1. As a patient stated, “Having it written down, it’s almost like there’s another person telling you to take your meds.”
Our study has limitations, several of which we detailed in an earlier report on the baseline survey (1). For many reasons, our results may not be generalizable to all U.S. practices. Participants were limited to 3 regions and included only practices with both electronic medical records and patient portals. Many of the doctors were either in a large, integrated health system or in academic group practices with small panels, and those who participated volunteered to do so. Limited numbers of each doctor’s patients used the portals. Response rates from patient surveys were not optimal, although they were similar to response rates in Web-based surveys of patients (16). Respondents to surveys tend to be more upbeat than nonrespondents, and patients’ general endorsement of positive statements, such as, “I take better care of myself,” may reflect confirmation bias. In general, compared with the nonrespondents, survey respondents were somewhat more likely to be older and female, as is typical of patients seen in primary care. Finally, the survey questions were designed specifically for our project, and although they had face validity, they were not developed with formal psychometric testing.
The study findings suggest that open notes may be a powerful intervention for improving the health of patients and point to many avenues for future elaboration and inquiry. Will open notes improve patient adherence to medications and care plans, facilitate the management and course of chronic disease, or decrease the incidence of medical errors? Might open notes improve the effectiveness of informal caregivers and even reduce their own stress and consequent associated illness? (17–19) How should we share notes with patients who lack access or experience with computer technologies? And, could open notes evolve into jointly generated contracts between patients and clinicians, with associated measures that become compelling markers of quality? (10, 20)
In response to a relatively simple intervention, the patients in this large-scale trial reported striking benefits and presented a clear mandate to continue open notes. The doctors encountered few problems, and we hope that the problems that exist can be overcome with further analysis, education, and experimentation. Since reviewing their individual results as documented in this report, the 3 participating institutions have each decided to broaden patient access to their clinicians’ notes. Despite important limitations in our study and the need for much more exploration, our findings suggest that expanding such transparency is the right thing to do.
Supplementary Material
Context
Electronic portals are increasingly used to provide patients with access to their medical records and to interact with the health care system.
Contribution
In this study of doctors and patients who participated in a 1-year pilot program, most patients reported that the ability to read their doctors’ office notes was beneficial and wanted the program to continue. Most doctors reported little or no impact on daily workload or patient anxiety or confusion.
Caution
The survey was completed by those who chose to participate in the program.
Implication
Providing patients with electronic access to their doctors’ notes may have benefits without increasing doctors’ workload.
—The Editors
Acknowledgments
The authors thank Elaine Bianco, BSN; Carolyn Conti, BS; Christopher Dries, BA; James I. Hoath, PhC; Margaret Jeddry; Jing Ji, MS; J. Andrew Markiel, PhD; Lawrence Markson, MD, MPH; Natalia Oster, MPH; Lisa M. Reich, PhD; Joan Topper, BS; Qiang Wang, MD; and Clara De La Cruz Watral, MBA, for invaluable contributions to this project. They also thank the many patients and doctors who both took a chance and participated actively in OpenNotes.
Grant Support: All investigators were supported by The Robert Wood Johnson Foundation’s Pioneer Portfolio grant 65921. Dr. Delbanco and Ms. Walker were also supported by the Drane Family Fund and the Richard and Florence Koplow Charitable Foundation. Dr. Elmore was also supported by the National Cancer Institute (K05 CA 104699).
Footnotes
Potential Conflicts of Interest: Disclosures can be viewed at www.acponline.org/authors/icmje/ConflictOfInterestForms.do?msNum=M12-0737.
Reproducible Research Statement: Study protocol, statistical code, and data set: Not available.
Current author addresses and author contributions are available at www.annals.org.
Author Contributions: Conception and design: T. Delbanco, J. Walker, J.D. Darer, J.G. Elmore, H.J. Feldman, J.D. Ralston, S.E. Ross, S.G. Leveille.
Analysis and interpretation of the data: T. Delbanco, J. Walker, S.K. Bell, J.G. Elmore, R. Mejilla, L. Ngo, J.D. Ralston, S.E. Ross, S.G. Leveille.
Drafting of the article: T. Delbanco, J. Walker, S.G. Leveille.
Critical revision of the article for important intellectual content: T. Delbanco, J. Walker, S.K. Bell, J.G. Elmore, R. Mejilla, L. Ngo, J.D. Ralston, S.E. Ross, S.G. Leveille.
Final approval of the article: T. Delbanco, J. Walker, S.K. Bell, J.D. Darer, J.G. Elmore, N. Farag, H.J. Feldman, R. Mejilla, L. Ngo, J.D. Ralston, S.E. Ross, N. Trivedi, E. Vodicka, S.G. Leveille.
Provision of study materials or patients: T. Delbanco, J. Walker, S.K. Bell, J.D. Darer, J.G. Elmore, N. Farag, L. Ngo, J.D. Ralston, S.E. Ross, N. Trivedi, E. Vodicka, S.G. Leveille.
Statistical expertise: R. Mejilla, L. Ngo, S.G. Leveille.
Obtaining of funding: T. Delbanco, J. Walker.
Administrative, technical, or logistic support: N. Farag, H.J. Feldman, N. Trivedi, E. Vodicka.
Collection and assembly of data: J. Walker, N. Farag, H.J. Feldman, R. Mejilla, N. Trivedi, E. Vodicka, S.G. Leveille.
References
- 1.Walker J, Leveille SG, Ngo L, Vodicka E, Darer JD, Dhanireddy S, et al. Inviting patients to read their doctors’ notes: patients and doctors look ahead: patient and physician surveys. Ann Intern Med. 2011;155:811–9. doi: 10.7326/0003-4819-155-12-201112200-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Leveille SG, Walker J, Ralston JD, Ross SE, Elmore JG, Delbanco T. Evaluating the impact of patients’ online access to doctors’ visit notes: designing and executing the OpenNotes project. BMC Med Inform Decis Mak. 2012;12:32. doi: 10.1186/1472-6947-12-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ralston JD, Hirsch IB, Hoath J, Mullen M, Cheadle A, Goldberg HI. Web-based collaborative care for type 2 diabetes: a pilot randomized trial. Diabetes Care. 2009;32:234–9. doi: 10.2337/dc08-1220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Earnest MA, Ross SE, Wittevrongel L, Moore LA, Lin CT. Use of a patient-accessible electronic medical record in a practice for congestive heart failure: patient and physician experiences. J Am Med Inform Assoc. 2004;11:410–7. doi: 10.1197/jamia.M1479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ralston JD, Revere D, Robins LS, Goldberg HI. Patients’ experience with a diabetes support programme based on an interactive electronic medical record: qualitative study. BMJ. 2004;328:1159. doi: 10.1136/bmj.328.7449.1159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ross SE, Lin CT. The effects of promoting patient access to medical records: a review. J Am Med Inform Assoc. 2003;10:129–38. doi: 10.1197/jamia.M1147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.OpenNotes. [8 August 2012];2010 Accessed at www.myopennotes.org on.
- 8.Stokes ME, Davis CS, Koch GG. Categorical Data Analysis Using the SAS System. 2. Cary, NC: SAS Inst; 2000. [Google Scholar]
- 9.SAS/STAT User’s Guide, Version 8. Cary, NC: SAS Inst; 2000. [Google Scholar]
- 10.Delbanco T, Walker J, Darer JD, Elmore JG, Feldman HJ, Leveille SG, et al. Open notes: doctors and patients signing on. Ann Intern Med. 2010;153:121–5. doi: 10.7326/0003-4819-153-2-201007200-00008. [DOI] [PubMed] [Google Scholar]
- 11.Feeley TW, Shine KI. Access to the medical record for patients and involved providers: transparency through electronic tools [Editorial] Ann Intern Med. 2011;155:853–4. doi: 10.7326/0003-4819-155-12-201112200-00010. [DOI] [PubMed] [Google Scholar]
- 12.Ross SE, Moore LA, Earnest MA, Wittevrongel L, Lin CT. Providing a web-based online medical record with electronic communication capabilities to patients with congestive heart failure: randomized trial. J Med Internet Res. 2004;6:e12. doi: 10.2196/jmir.6.2.e12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kind EA, Fowles JB, Craft CE, Kind AC, Richter SA. No change in physician dictation patterns when visit notes are made available online for patients. Mayo Clin Proc. 2011;86:397–405. doi: 10.4065/mcp.2010.0785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Walker J, Ahern DK, Le LX, Delbanco T. Insights for internists: “I want the computer to know who I am ”. J Gen Intern Med. 2009;24:727–32. doi: 10.1007/s11606-009-0973-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Auerbach DI, Kellermann AL. A decade of health care cost growth has wiped out real income gains for an average US family. Health Aff (Millwood) 2011;30:1630–6. doi: 10.1377/hlthaff.2011.0585. [DOI] [PubMed] [Google Scholar]
- 16.Hassol A, Walker JM, Kidder D, Rokita K, Young D, Pierdon S, et al. Patient experiences and attitudes about access to a patient electronic health care record and linked web messaging. J Am Med Inform Assoc. 2004;11:505–13. doi: 10.1197/jamia.M1593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Grunfeld E, Coyle D, Whelan T, Clinch J, Reyno L, Earle CC, et al. Family caregiver burden: results of a longitudinal study of breast cancer patients and their principal caregivers. CMAJ. 2004;170:1795–801. doi: 10.1503/cmaj.1031205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bevans M, Sternberg EM. Caregiving burden, stress, and health effects among family caregivers of adult cancer patients. JAMA. 2012;307:398–403. doi: 10.1001/jama.2012.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rodrigue JR, Dimitri N, Reed A, Antonellis T, Pavlakis M, Johnson SR, et al. Spouse caregivers of kidney transplant patients: quality of life and psychosocial outcomes. Prog Transplant. 2010;20:335–42. doi: 10.1177/152692481002000406. [DOI] [PubMed] [Google Scholar]
- 20.Delbanco T, Berwick DM, Boufford JI, Edgman-Levitan S, Ollenschläger G, Plamping D, et al. Healthcare in a land called PeoplePower: nothing about me without me. Health Expect. 2001;4:144–50. doi: 10.1046/j.1369-6513.2001.00145.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.