Abstract
Prostate cancer is the second-leading cause of cancer-related mortality in men in Western societies. Androgen receptor (AR) signaling is a critical survival pathway for prostate cancer cells, and androgen-deprivation therapy (ADT) remains the principal treatment for patients with locally advanced and metastatic disease. While a majority of patients initially respond to ADT, most will eventually develop castrate-resistance, defined as disease progression despite serum testosterone levels of less than 20ng/dL. The recent discovery that AR signaling persists during systemic castration via intratumoral production of androgens led to the development of novel anti-androgen therapies including abiraterone acetate and enzalutamide. While these agents effectively palliate symptoms and prolong life, metastatic castration-resistant prostate cancer (mCRPC) remains incurable. An increased understanding of the mechanisms that underlie the pathogenesis of castrate-resistance is therefore needed to develop novel therapeutic approaches for this disease. The aim of this review is to summarize the current literature on the biology and treatment of castrate-resistant prostate cancer.
Keywords: castrate-resistant prostate cancer, ADT, alternative pathways
INTRODUCTION
The mainstay of therapy for patients with locally advanced prostate cancer, metastatic prostate cancer, and biochemically recurrent disease after failure of localized treatments is androgen-deprivation therapy (ADT) with gonadropin-releasing hormone (GnRH) analogs and anti-androgens.1 GnRH analogs like leuprolide cause continuous stimulation of the pituitary gland, leading to `chemical castration' with suppression of testosterone production from the testes, whereas anti-androgens directly inhibit the androgen receptor (AR).
ADT is known to provide remission of the disease, best evidenced by a decline of prostate-specific antigen (PSA) in about 90% of patients.2 After a mean time of 2–3 years, however, the disease progresses despite continuous hormonal manipulation. This type of cancer is known as castrate-resistant prostate cancer (CRPC).2 Metastatic castration-resistant prostate cancer (mCPRC) is associated with a poor prognosis and mean survival time of only 16–18 months.3
Docetaxel and cabazitaxel are the only FDA (United States Food and Drug Administration)-approved chemotherapies for the treatment of mCRPC. These tubulin-binding taxanes have been proven to decrease PSA levels and palliate symptoms but survival benefits are modest.4 Another agent, sipuleucel-T (Provenge; Dendreon Corp., Seattle, WA) is a cellular immunotherapy that has been shown to increase overall survival time for patients with mCRPC.5, 6
The AR is believed to remain active in CRPC, and several new strategies to inhibit AR signaling have recently been developed. Abiraterone acetate (Zytiga; Janssen Biotech, Inc. Horsham, PA) is an FDA-approved inhibitor of androgen biosynthesis which blocks cytochrome P450-c17 (CYP17), leading to suppression of androgens derived from the adrenal glands, the prostate tumor, and the tumor microenvironment.7 This novel therapy increased survival time by almost 4 months, increased the time to PSA progression, and was relatively well tolerated by patients.7 MDV3100 (now known as enzalutamide), an AR antagonist that prevents nuclear translocation and interaction with co-activators, has produced similar results in recent clinical trials.8, 9
Although novel cytotoxic agents, AR blocking agents and immunotherapies represent effective therapy strategies for mCRPC, important clinical questions remain. First, the absence of any reliable biomarker does not allow clinicians to decide which patients will benefit from these treatments or when to alter or terminate treatment. In addition, despite the effective blocking of androgen biosynthesis10 and AR signaling, all patients eventually progress.7, 11, 12 Furthermore, the optimal sequencing of these therapies remains unknown.
The general aim of this review is to summarize new evidence about mechanisms of castrate-resistance and novel therapeutic approaches directed at this complex and enigmatic disease state.
THE ROLE OF AR SIGNALING IN CRPC
The expression of PSA is mainly regulated by androgen response elements, suggesting that the increasing PSA during ADT implies activation of AR transcriptional activity.13 Consistent with this hypothesis, various recent findings have supported the notion that one of the most important mechanisms in CRPC development is the continuous activation of AR in prostate cancer cells.3 Several cellular and molecular alterations are related to this post-castration activation of the AR, including incomplete blockade of AR-ligand signaling, AR amplifications, AR mutations, aberrant AR co-regulator activities, and AR splice–variant expression.14
Recent data suggest that despite castration, which decreases serum androgen levels, intratumoral levels of testosterone and dihydrotestosterone (DHT) in patients with mCRPC are similar to those found in hormone therapy naïve.2 Evidence suggests that upregulation and stimulation of enzymes involved in androgen biosynthesis (including CYP17) occur within the tumor microenvironment.15–17 In a recent study, Montgomery et al. demonstrated that prostate cancer bone metastases can convert adrenal androgens to testosterone and DHT.17 Of note, metastatic prostate cancer may amplify the HSD17B3 gene and lose copy numbers of the HSD17B2 gene, leading to decreased conversion of testosterone to the less active androstenedione.18 In another recent study, Mitsiades et al. found significant heterogeneity in the expression of various steroidogenic enzymes in the tumor microenvironment among patients with mCRPC, suggesting that the combination of enzymatic blockage and potent anti-androgens is a reasonable therapeutic approach for patients with mCRPC.19 Moreover, Efstathiou et al. recently showed that abiraterone acetate effectively suppresses testosterone concentrations in both blood and the tumor microenvironment to less than picograms per milliliter.20 Despite this degree of efficacy, patients receiving abiraterone acetate will eventually show evidence of disease progression.
Enzalutamide is a novel AR antagonist that overcomes resistance to conventional anti-androgens a by blocking ligand binding, nuclear translocation, DNA binding, and co-activator recruitment of AR.21 According to a recent phase I/II study in patients with mCRPC, the use of enzalutamide is a safe, elicits PSA and radiographic response, and results in a median time to progression of 47 weeks.8 The superiority of enzalutamide over placebo was confirmed in a phase III clinical trial that showed increased overall survival (4.8 months) and improvement in all secondary end points.9 Despite these encouraging results, after a period of remission that is characterized by significant variation between patients, these tumors eventually progress.
AR amplification
CRPC is associated with increased expression of AR attributed to gene amplification and other mechanisms, including increased mRNA stability.14, 22 Prior data from microarray profiles of prostate cancer xenografts showed that higher AR mRNA was the only change related to the development of castrate-resistance.19 Interestingly, an early study showed that 80% of the tumors acquiring AR amplification also demonstrated higher levels of AR protein.23 Furthermore, studies utilizing fluorescence in situ hybridization have shown that while AR gene amplifications are observed in 20–25% of CRPCs24 and in many cancer cell lines derived from these patients, they are very rare in primary tumors.25 These gene amplifications, which are heterogeneous among cancerous cells in the same tumor,26 are related to sensitization of the AR signaling pathway to lower levels of androgens. On the other hand, AR and AR-regulated genes have been shown to be upregulated in prostate cancer xenografts after castration without any increase in the number of gene copies,22, 27 suggesting that AR amplification is not the primary mechanism of the paradoxical upregulation of certain AR target genes after castration in these models.22
AR mutations
Multiple early studies evaluating the prevalence of AR gene mutations have demonstrated variable results.28–30 Most mutations are located in the ligand-binding domain (LBD), providing a mechanistic explanation for the development of resistance to anti-androgen therapy. The results of more recent studies provide support for the hypothesis that the absence of androgens or the presence of anti-androgens acts as selective pressure for emergence of mutations in the AR gene. Various AR mutations documented in mCRPC are related to decreased specificity of AR-ligand interaction, allowing AR activation by alternative steroidal molecules, including estrogens, corticosteroids, and progesterone.31, 32 The NH2 terminal region, which is known to be critical for the interaction of AR with co-regulators, has also been shown to harbor mutations.33 Moreover, mutation analysis identified a 5–amino acid core sequence located in the NH2 terminal region, W435L, that can mediate androgen-independent AR activation.34
AR splice variants
Identification of AR splice variants in cell lines and tumor tissues derived from patients with CRPC provides an additional mechanistic explanation for the development of CRPC.35, 36 Many of these variants result from insertion of cryptic exons downstream of the coding sequences for the DNA binding domain or from deletion of exons coding for the LBD, leading to the formation of an AR molecule lacking the LBD.37, 38 The regulation of variant AR expression is poorly understood, although suppression of LBD by an androgen antagonist is known to cause increased expression of AR variants in prostate cancer cell lines.39 Sun et al. suggested that activation of AR variants leads to upregulation of steroidogenic enzymes, providing prostate cancer cells with higher levels of AR ligands.38 AR variants are also believed to increase the expression of AR-regulated genes in the absence of any ligand, providing an explanation for the activated AR signaling pathway in CRPC.38, 39
Hu et al. recently used LNCaP95 and VCaP prostate cancer cells to prove that inhibition of AR by either siRNA or enzalutamide leads to upregulation of the ARV7 ligand, one of the most frequently observed AR variants in clinical specimens.39 Of note, full-length AR and ARV7 are expressed differently in each cell line. Full-length AR activates pathways related to metabolism, biosynthesis, and secretion, whereas ARV7 increases the expression of cell-cycle genes, including the activator of the M-phase check point UBE2C.39 Moreover, when LuCaP35CR xenografts were treated with abiraterone acetate, both full-length AR and ARV7 were upregulated, but the expression of UBE2C paralleled only the expression of ARV7. This relationship was also demonstrated in clinical prostate cancer samples following ADT.39 Inhibition of AR in LNCaP and CWR22Rv1 cells did not induce activation of AR variants, providing an explanation for why some xenografts respond to AR suppression with tumor growth inhibition. In a recent report by Li et al.40, a 48-kb deletion in AR intron 1 in a subset of cells in the heterogeneous CWR-R1 cell line which was related to the expression of the AR1/2/3/CE3 splice variant (AR-V7/AR3). Following enzalutamide treatment, the AR-V7/AR3–expressing clone expanded and the presence of this variant led to tumor growth during ADT. Of interest is that treatment of AR-V7/AR3–enriched LNCaP cells with high concentrations of DHT caused upregulation of PSA but downregulation of M-phase genes, including UBE2C, CDCA5, and CCNA2. These results implicate expression of AR splice variants in the pathogenesis of CRPC, especially after enzalutamide treatment.40
Post-translational modifications of AR
Other possible mechanisms related to persistent AR transcriptional activity during ADT are post-translational alterations of AR, especially phosphorylation. Guo et al. suggested that Src-induced phosphorylation of ARY534 can lead to both AR sensitization to low levels of androgens and androgen-independent activation of AR.41 Moreover, it is believed that Etk, a non-receptor tyrosine kinase and downstream effector of Src and PI3K, is upregulated during ADT and phosphorylates AR at Y534 and Y551/552, stabilizing it and promoting its activity under androgen-depleted conditions.42
AR co-regulators and collaborating factors
Another critical mechanism implicated in the development of CRPC is the interaction between AR and co-regulators. Wang et al. showed in a castrate-resistant LNCaP derivative that AR directly regulates M phase genes including CDC20, CDK1, and UBE2C, inactivating the M-phase check point and promoting tumor growth in xenografts.43 Chromatin immunoprecipitation analysis showed enhanced activities of the AR co-stimulator MED1 and of the FoxA1 and GATA2 AR collaborating factors in castration-resistant cells, whereas silencing of these factors decreased UBE2C mRNA levels.43 Results from this study indicate that the distinctive pattern of AR transcriptional activity in castrate-resistant cells is determined largely by co-activator stimulation and accompanying chromatin modifications. It is interesting that interleukin 6–mediated nuclear receptor co-activator 1 (NCoA1, or SRC-1) phosphorylation promotes AR-dependent transcription in a ligand-independent manner, whereas MAPK-mediated phosphorylation of this co-activator may increase its affinity for AR, contributing to disease recurrence and CRPC.44
Alternatively, it is known that bicalutamide therapy reduces recruitment of the nuclear receptor co-repressor (NCoR) in cells with increased AR22 protein, suggesting negative feedback between AR and co-regulators. According to recent reports, NCoA2 (SRC-2) expression is positively associated with high tumor cell proliferation and early disease relapse.45 Downregulation of NCoA2 reduces AR target gene expression and inhibits proliferation of AR-dependent and -independent prostate cancer cells, whereas it is believed that in AR-positive cancer cells, high levels of androgens repress NCoA2 expression.46 Finally, NCoA3 (SRC-3), which is positively associated with tumor recurrence and PI3K/Akt activation, is known to be critical in the development of poorly differentiated prostate cancer.47
AR transcriptional activity
During the development of CRPC, AR transcriptional activity is modified and aberrant regulation of numerous genes that promote cell survival and proliferation occurs. Available data indicate that AR-stimulated genes are initially repressed but subsequently rebound during ADT. For example, Holzbeierlein et al. reported a gene-expression analysis of prostate tumors during hormonal therapy showing that multiple AR target genes were upregulated during ADT and were associated with clinical resistance to therapy.48 Moreover, Sharma et al. suggested that retinoblastoma protein loss and subsequent E2F transcriptional factor stimulation can lead to deregulation of AR and androgen-independent activation of multiple AR-stimulated genes.49 Recent reports added support to the concept that multiple alternative oncogenic pathways can contribute to generation of AR signaling that is hypersensitive to low levels of androgens.50
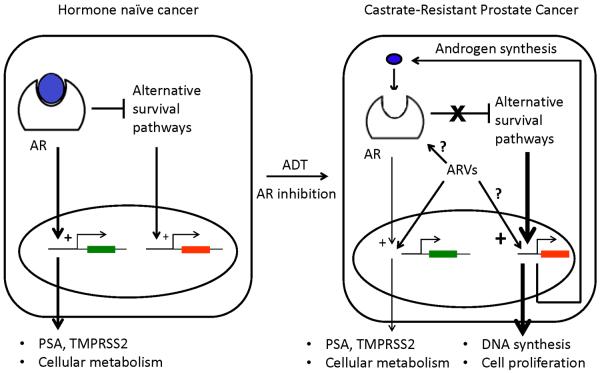
During AR-signaling, AR can act as either a transcriptional enhancer or repressor for downstream target genes depending on androgen levels. For example, Cai et al. found that with increasing androgen levels, AR directly represses transcription of the AR gene in androgen-dependent VCaP cells by inhibiting the ARBS2 enhancer located within intron 2 of the AR gene.51 In contrast, with low androgen levels following androgen deprivation, transcription of the AR gene increases. Additional AR target genes involved in androgen biosynthesis, DNA synthesis and repair, cell cycle, and proliferation are similarly repressed with high androgen levels and become de-repressed with low androgen levels. Consistent with these activities, expression of androgen repressed genes is increased in castrate-resistant VCaP–derived VCS2 cells and VCaP xenografts, and in human CRPC samples. These data suggest a model in castrate-resistance whereby androgen levels are adequate to enhance expression of AR-regulated genes related to cellular metabolism but insufficient to repress expression of AR-regulated genes related to DNA replication and cellular proliferation.51 Thus, a combination of enhanced and de-repressed AR target genes ultimately contributes to castrate-resistant progression (Figure 1).
Figure 1. Androgen deprivation therapy initiates alterations in gene expression profiles in prostate cancer cells.
Androgen deprivation therapy results in recalibration of prostate cancer tissue androgen levels that leads to alterations in androgen receptor (AR)-driven gene expression that may contribute to castrate-resistant prostate cancer. AR variants (ARVs) may contribute to altered gene expression.
ALTERNATIVE GROWTH AND SURVIVAL PATHWAYS IN CRPC
During the transition from androgen-dependence to castrate-resistance, cancer cells become driven by alternative growth signaling pathways. Many of these pathways can participate in normal cellular processes, but can also become oncogenic in the early adaptive period after ADT is begun.52 An increased understanding of the molecular interactions between androgen signaling and these alternative growth and survival pathways should lead to the identification of novel therapeutic targets.
C-myc overexpression
The proto-oncogene c-myc is a known regulator of cell growth and plays a critical role in prostate cancer development and progression. Gurel et al. showed that c-myc is frequently overexpressed in prostate intraepithelial lesions (PIN) with an incremental increase from normal tissues to low-grade PIN to high-grade PIN.53 Various mouse models have shown that c-myc overexpression in prostate luminal cells can lead to hyperplasia and PIN lesions but not invasive carcinoma.54–56 Alternatively, genetically engineered mice that express c-myc from the ARR2PB prostate-specific promoter develop PIN that progresses to prostate cancer with variable frequencies.57, 58 Interestingly, specific amplifications of the c-myc gene have been confirmed in up to 72% of CRPC59 and ADT has been suggested to increase the incidence of these amplifications.60 Finally, Bernard et al. demonstrated that while AR inhibition causes downregulation of c-myc in prostate cancer cells, prostate cancer cells that overexpress c-myc continue to grow under ADT. Together, these data support a role for cmyc activation in the development of prostate cancer and as a potential mechanism for CRPC development.61
The PI3K/Akt/mTOR pathway
The PI3K pathway is one of the most critical in human cancer.62 Various growth factors, including insulin-like growth factor (IGF) and fibroblast growth factor (FGF), regulate this pathway, leading to activation of PI3K and the formation of PIP3. PIP3 activates AKT via phosphorylation and phosphorylated Akt (pAkt) activates a number of cellular molecules involved in cell survival and proliferation, including MDM2, c-myc, GSK3β, NFκB, and mTOR. PTEN is a lipid phosphatase that functions as the main inhibitor of PI3K/Akt signaling. Genetic alterations of the PI3K signaling pathway occur in 42% and 100% of primary and metastatic prostate cancers, respectively, suggesting this pathway is crucial in the development of CRPC.52
In an initial study using the PbCre;Ptenloxp/loxp mouse model characterized by prostate-specific inactivation of PTEN, Wang et al., showed that 100% of mice developed invasive adenocarcinoma between 9 and 29 weeks, 5 of 11 had lymph node metastasis between 12 and 29 weeks, and 3 of 11 mice developed lung metastases.. Following castration, there was a time-dependent phenotype characterized by an immediate initial increase in prostate cancer cell apoptosis (3 to 6 days post-castration) that was gradually replaced overtime with the outgrowth of Pten null castrate-resistant proliferative clones.63 The results of more recent studies using Pten-knockout mice are consistent with those of this initial report, further supporting a role for Pten loss in CRPC.64–66
Results from PI3K, Akt, and mTOR inhibitors in clinical trials and xenograft studies67–69 suggested a potential interaction between AR and PI3K/Akt signaling pathways. Two recent publications reported negative feedback regulation between AR and PI3K/Akt pathways. First, Carver et al. initially observed that mice with prostate Pten deletion (Ptenloxp/loxp) had lower AR levels than their wild-type littermates, whereas treatment with BEZ235, a dual PI3K and mTOR inhibitor, and RAD001, an mTOR inhibitor, rescued AR protein levels.70 Similar results were achieved in LNCaP cells, demonstrating that PI3K pathway inhibition can upregulate AR and activate AR target gene expression.70 Subsequent experiments in LNCaP cells and Ptenloxp/loxp mice showed that this PI3K–AR interaction is mediated in part by upregulation of HER3 after inhibition of PI3K.70
Second, Mulholland et al. used the PbCre;Ptenloxp/loxp model to demonstrate that Pten loss suppresses AR transcriptional activity and generates a gene-expression profile resembling that of the castration phenotype. A mechanism for this cross talk involved negative regulation of EGR1, c-JUN, and EZH2 by PTEN.71 The results in both reports are consistent with earlier studies72, 73 and clearly demonstrate that the PI3K/Akt pathway can inhibit AR transcriptional activity and lead to castrate-resistance.
Additional experiments showed that after 7 days of enzalutamide treatment of Ptenloxp/loxp mice, despite decreased AR transcriptional activity the tumors had not significantly regressed and were histologically similar to those before treatment, although the treatment was much more effective in transgenic mice with inducible c-myc.70 Further studies revealed increased Akt phosphorylation at Ser473 in the Ptenloxp/loxp mice and in LNCaP and LAPC4 AR-positive cells after castration and enzalutamide treatment, respectively. The same treatment did not increase pAkt in PC-3 cells, which are AR negative.70
Similarly, Mulholland et al. used the PbCre;Ptenloxp/loxp model to show that castrate-resistant cancer developed in the regions of the prostate with combined Pten and AR loss. In contrast, AR-positive regions contained lower levels of pAkt with less cell proliferation after castration. These observations led to the conclusion that active AR transcriptional activity can inhibit phosphorylation of Akt to activate a potent oncogenic pathway.71 Both groups of investigators attributed this interaction to the upregulation of FKBP5 and PHLPP by AR.70, 71 It is known that FKBP5 functions as a scaffolding protein for pAkt and PHLPP, promoting pAkt dephosphorylation by PHLPP.74
Cross talk between the AR and PI3K/Akt pathways supports the rationale for combining AR and PI3/Akt inhibitors in CRPC. Although BEZ235 and enzalutamide modestly inhibit LNCaP cell proliferation as single agents, the combination significantly decreased cell numbers via apoptosis in vitro. In LNCaP xeongrafts, the combination produced a 24% reduction of tumor volume compared with vehicle-only or single therapy (i.e., BEZ235 or castration only), which resulted in 28%, 30%, and 31% increases in tumor volume, respectively.70 Mulholland et al. compared treatment of Ptenloxp/loxp mice and Ptenloxp/loxp mice carrying AR deletion (Ptenloxp/loxpARL/Y) with rapamycin only, castration only, or the combination. They found significantly enhanced tumor regression in the combination-therapy group relative to that in the two single therapy groups in both models.71 Despite these encouraging results, recent data indicate complex adaptive resistance pathways to PI3K/mTOR inhibition in vivo, and clinical data are lacking.75
Other growth and survival pathways contributing to CRPC
The RAS/MAPK pathway has also been implicated in prostate cancer development, progression, and metastasis. RAS signaling is known to decrease the androgen dependence of LNCaP cells76 and to promote metastasis in DU145 cells, and tissue specimens from patients with mCRPC display higher levels of pMAPK, a downstream target of RAS signaling.77 According to a recent report from Mulholand et al., the RAS/MAPK pathway was activated in 43% of primary prostate cancer samples and 90% of metastatic samples. Phospho-MAPK levels were more prominent in tissues derived from patients who had received ADT and were mainly observed in the basal cell compartment.78 Moreover, conditionally activated K-ras in the prostatic epithelium of transgenic mice (K-rasL/W) is not sufficient to promote prostate cancer development. However, when K-rasL/W mice were crossed with PbCre;Ptenloxp/loxp mice, simultaneous deletion of Pten and activation of RAS led to the development of poorly differentiated carcinoma within 10 weeks.78 In contrast with the PbCre;Ptenloxp/loxp mice, PbCre;Ptenloxp/loxpK-rasL/W mice developed lung and liver metastases with 100% penetrance but not bone metastasis, although their expression of AR and AR-targeted genes was much lower. Histologic and gene-expression analysis of cancer tissues showed that expression of mesenchymal markers, including N-cadherin, and cell-cycle genes, including UBE2C, was greater than in PbCre;Ptenloxp/loxp mice, suggesting that RAS pathway activation promotes the de-differentiation of prostate cancer cells.
Transforming growth factor β (TGF-β) is a secreted cytokine that is implicated in various cellular processes, including cell proliferation and cancer progression.79, 80 Several studies have suggested that in normal epithelial cells and early-stage cancers, TGF-β signaling may be growth suppressive.79, 81 In advanced prostate cancer, however, TGF-β1 levels are increased, suggesting a growth promoting role.82–84 It has also been shown that the expression of an isoform of this cytokine, TGF-β3, is increased in prostate cancer and that TGF-β3 signaling is upregulated in CRPC.85 Androgens regulate TGF-β1 gene transcription through positive and negative androgen response elements in the TGF-β1 promoter.86, 87 However, AR-mediated TGF-β1 expression in the context of CRPC is not well understood. Recent data support the idea that TGF-β cytokines can activate the PI3K pathway, although the role of SMAD molecules in this interaction is not clear.88, 89 One report suggested that the TGF-β and PI3K pathways contribute to EMT, which is believed to be important in CRPC pathogenesis.90 Among the most important intracellular mediators of TGF-β signaling are the SMAD isoforms. Ding et al. used a transgenic mouse model to evaluate the role of SMAD4 in prostate cancer progression and metastatic potential. In prostate intraepithelial neoplastic lesions in PTENloxp/loxp mice, TGF-β signaling is upregulated and these lesions are characterized by increased SMAD4 expression.91 Interestingly, SMAD4 was previously reported to be downregulated in human prostate cancer metastasis, and epigenetic silencing of the SMAD4 promoter was associated with advanced disease.92 Ding et al. found that Pten−/−Smad4−/− mice developed earlier and more aggressive invasive adenocarcinoma than Pten−/− mice, while Smad4−/− mice did not develop prostate cancer, Gene-expression analysis of these models showed that cyclin D1 and SPP1 were upregulated in Pten−/−Smad4−/− tumors, leading to an increased proliferation index.91
The Wnt/β-catenin pathway is dysregulated in several types of cancer, including colorectal, liver, and prostate cancer.93, 94 In one study, abnormal β-catenin expression was observed in 23% of tumor samples derived from radical prostatectomies and in 38% of CRPCs and was found to be related to high Gleason scores.95 β-Catenin activates TCF/LEF-1 transcriptional activity and upregulates genes such as MYC, MMP7, and VEGF. On the other hand, β-catenin is an important component of cadherin cell adhesion complexes which play a critical role in the development of EMT and CRPC.96 A functional relationship between Wnt/β-catenin signaling and EMT has also been suggested.97 Among the Wnt/β-catenin target genes are the transcriptional factors Twist-related proteins 1 and 2 and the zinc finger protein SNAI2, which downregulate E-cadherin, potentially contributing to EMT.98
Despite extensive research, there are conflicting results regarding the cross talk between AR and Wnt/β-catenin signaling. Some studies suggest that AR activation leads to increased β-catenin nuclear translocation and transcriptional activity.99, 100 Other studies indicate that stimulation of Wnt/β-catenin signaling leads to increased AR expression via TCF/LEF-1 binding sites on the AR promoter101 and also upregulates AR target genes.91, 92 However, AR has also been shown to compete with TCF/LEF-1 for β-catenin binding and therefore inhibit β-catenin/TCF–dependent signaling.102, 103 Consistent with the latter findings, Chesire et al., in an early study involving experiments in prostate and non-prostate cancer cells, showed that stimulation of AR by androgens can lead to AR-mediated transcriptional suppression of β-catenin/TCF transcriptional activity, whereas activation of TCF may inhibit the expression of AR-regulated genes. Administration of anti-androgens alleviated this AR-mediated suppression of TCF transcriptional activity.104 Finally, in a recent study, nuclear localization of β-catenin was found in 10 of 27 human tissue specimens derived from bone metastases of mCRPC. This localization was inversely associated with AR expression, suggesting that reduced AR expression enables β-catenin signaling.105
The IGF system has been implicated in growth regulation, apoptosis resistance, and invasion in a number of human malignancies,106–108 but its role in the development of CRPC remains controversial. Studies in prostate cancer cells have shown that IGF-1 may increase cancer cell proliferation and glucose consumption, whereas inhibition of the IGF-1 receptor (IGF-1R) suppresses prostate cancer cell invasiveness.109, 110 Xenograft studies demonstrated that increased IGF-1R and IGF-1 can lead to androgen-independent tumor growth111 Pandini et al. found that AR stimulation leads to increased expression and phosphorylation of IGF-IR in AR-positive cancer cells, enhancing their proliferation and invasiveness. More importantly, this increased AR activity was only partially blocked by anti-androgens such as bicalutamide.112
IGF is known to mediate the activity of insulin and IGF-1 and -2 in normal cells, thereby mediating increased glucose intake and glycolysis and resulting in ATP and CO2 formation via oxidative phosphorylation. In contrast with normal cells, most cancer cells rely on aerobic glycolysis—the Warburg effect. Aerobic glycolysis is less effective in generating ATP compared to oxidative phosphorylation, but cancer cells effectively adapt this type of metabolism to take up nutrients that are critical for cell proliferation and tumor growth, including nucleotides, amino acids, and lipids. At the same time, aerobic glycolysis via the pentose phosphate pathway alleviates cellular oxidative stress, providing cancer cells with a survival advantage.113 According to another recent study, the administration of aerobic glycolysis inhibitors such as 3-bromopyruvate can overcome resistance to trastuzumab in breast cancer114 while inducing cell death in myeloma cells that overexpress hexokinase II (HKII)115. Several studies substantiate the idea that prostate cancer cells activate glycolysis through AR and PI3K/Akt. In particular, Moon et al. showed that androgen administration activates glycolysis and lipogenesis in LNCaP cells through PKA-mediated phosphorylation of CREB, which leads to upregulation of HKII. In parallel, liganded AR directly stimulates the expression of PFKFB2, a known isoform of phosphofructokinase 2 (PFK2), and PI3K/Akt signaling is implicated in the phosphorylation of PFKFB2, promoting its kinase function.116 On the other hand, recent data have shown that AR stimulates AMPK which is a known negative regulator of Warburg effect117, 118. Interestingly, AR-negative cells such as PC-3 cells exhibit lower PFK activity, higher LDH activity and consume less oxygen than LNCaP (AR-positive) cells119. Ros et al. demonstrated that LNCaP, DU145, and PC-3 prostate cancer cells are more dependent on glucose than non-malignant RWPE1 cells. Furthermore, inhibition of PFKFB4, another isoform of PFK2 that functions as the phosphatase of fructose 2,6-biphosphate and promotes the pentose phosphate pathway, led to decreased tumor growth in PC-3 xenografts. By inducing the pentose phosphate pathway, this enzyme provides cells with enough NADPH for biomass synthesis and oxidative stress alleviation.120 The implication is that aerobic glycolysis, driven by multiple oncogenic pathways in prostate cancer progression and especially in the development of CRPC, may provide us with potential markers of disease progression and therapeutic targets.
The FGF pathway is believed to play a critical role not only during prostate organogenesis but also during prostate cancer development. FGF is known to be secreted by both stromal and cancer cells in the tumor microenvironment, acting by paracrine and autocrine mechanisms, respectively.121 Consistent with these data, FGF receptor 1 (FGFR1) is not expressed in benign prostate epithelium, whereas it is upregulated in 40% of poorly differentiated adenocarcinomas.122 By using a lentiviral vector to alter stromal FGF expression, Memarzadeh et al. showed that increased stromal FGF can lead to the enhanced epithelial proliferation associated with AR upregulation. Moreover, when stroma overexpressing FGF and epithelium expressing activated Akt were combined, tumor growth was more prominent.123 Spencer et al. demonstrated the development of a spectrum of prostate malignancies, including adenocarcinoma, that were positive for nuclear AR and negative for synaptophysin, with lymph node and liver metastasis in mice with conditional overexpression of FGFR1 in the prostate epithelium.124 There was a high incidence of sarcomatoid carcinoma with relatively diffuse expression of E-cadherin, which is a characteristic of EMT. A clinical trial with Dovitinib (TKI258), a multi-tyrosine kinase inhibitor with high specific activity against FGF/FGFR, is currently underway in patients with mCRPC (ClinicalTrials.gov Identifier: NCT01741116).
Hepatocyte growth factor and its receptor, c-Met, have been implicated in the regulation of cell growth, cell motility, morphogenesis, and angiogenesis by autocrine and/or paracrine mechanisms.125, 126 c-Met is highly expressed in AR-negative prostate cancer cell lines such as PC-3 and DU145 and in basal and intermediate cells in the prostate epithelium but only minimally expressed in AR-positive prostate cancer cells, including LNCaP and CWR22, and in luminal cells in the prostate epithelium.127 Of note, increased c-Met expression has been found in prostate cancer tissues with a greater incidence of staining in metastatic tumor samples.127 Finally, Verras et al. showed that AR downregulates c-Met expression by interfering with Sp1, a known transcriptional factor that stimulates c-Met expression.128 These data support the idea that c-Met signaling is negatively regulated by AR and is potentially de-repressed during the development of castrate-resistance. In a recently reported study, Cabozantinib (XL184), a multi-tyrosine kinase inhibitor with high-specific activity against c-Met, produced significant responses in patients with mCRPC characterized by improvements in bone scan, lymphadenopathy, and bone pain (PMID: 23169517).
Recent data substantiate the concept of negative cross talk between AR- and EMT-promoting pathways and that overexpression of self-renewal pathways can be sufficient for tumor progression during ADT. Sun et al. recently reported that castration can induce EMT in normal mouse prostate, characterized by increased expression of N-cadherin and vimentin and by low expression of E-cadherin and the acquisition of stem cell characteristics. They confirmed these results in LucaP35 xenografts, which showed increased TGF-β, IGF1, FGFR2, and platelet-derived growth factor signaling after ADT. The authors also found negative cross talk between AR and Zeb1, which may be related to EMT.129 Zhu et al. found that long-term ADT can promote EMT and metastasis through downregulation of AR expression, suggesting that intermittent ADT is a promising option for patients with late disease.130 Finally, Jeter et al. showed that LNCaP cells and xenografts overexpressing NANOG, a known self-renewal and pluripotency gene, are resistant to ADT and characterized by c-myc and Ki-67 upregulation and AR and PSA downregulation, suggesting that NANOG can mediate castrate-resistant progression.131
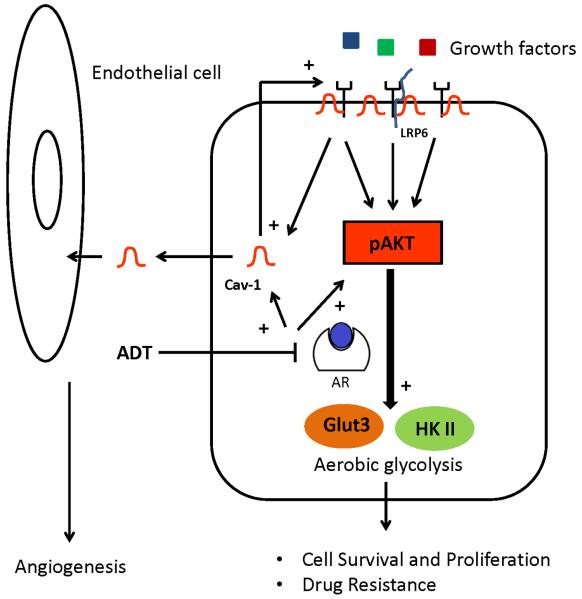
Caveolin-1 (Cav-1) is a major structural component of caveolae that is known to interact with critical components of multiple oncogenic pathways, including receptor tyrosine kinases, serine/threonine kinases, phospholipases, G-coupled protein receptors, and Src family kinases. These proteins are located in caveolar membranes, where they interact with Cav-1 through the Cav-1 scaffolding domain.132,133 Elevated expression of Cav-1 is associated with multiple human malignancies, including prostate cancer134, 135: Serum Cav-1 levels are higher in men with prostate cancer than in those with benign prostate hyperplasia,136 and high serum levels have been associated with elevated risk of cancer recurrence after radical prostatectomy.137 Moreover, Cav-1 levels were found to be elevated in metastatic mouse and human prostate cancer,138 and this molecule was found to be a downstream effector of testosterone-mediated prostate cancer cell survival and clonal growth.139 On the other hand, Cav-1 is known to be highly expressed and secreted by AR-negative cells, and increased levels of Cav-1 expression have been observed after ADT.140 Further, downregulation of Cav-1 in cell and animal models converted androgen-insensitive metastatic mouse prostate cancer cells to an androgen-sensitive phenotype.141 Finally, recombinant Cav-1 is taken up by prostate cancer cells and endothelial cells in vitro and increases angiogenic activities, suggesting a significant role of Cav-1 not only in the tumor cell but also in the tumor microenvironment.142 These data suggest that Cav-1 expression provides a significant survival benefit for prostate cancer cells, especially on ADT.
Mechanistic studies show that Cav-1 induces the PI3K/Akt pathway by inhibiting the phosphatases PP1 and PP2, leading to increased phosphorylation and activity of PDK1, Akt, and Erk1/2.143 Since PI3K/Akt is a critical survival pathway for prostate cancer cells, especially during ADT, and this explains the significance of Cav-1 expression in AR-negative cells. In a subsequent study, FGF, VEGF, and TGF-β1 downstream pathways induced the secretion of Cav-1 in AR-negative cells. Cav-1 upregulates multiple oncogenic pathways through PI3K/Akt and mRNA stabilization, suggesting the presence of a positive feedback loop between Cav-1 and these oncogenic pathways.144 In accord with these findings, Tahir et al. showed that sunitinib and dasatinib treatment of PC-3 and DU145 cells and xenografts decreased Cav-1 expression in cells and serum Cav-1 levels, respectively, in mice and serum Cav-1 levels were positively associated with tumor growth. Finally, the co-administration of anti-Cav-1 antibody with sunitinib and dasatinib led to greater tumor regression than did either treatment alone, further supporting the concept that Cav-1 mediates activation of multiple oncogenic pathways in the prostate cancer cell.145 Recently, Tahir et al. demonstrated an interaction between Cav-1 and LRP6 in the cellular membrane, which leads to the activation of IGF-1R/IR and results in stimulation of Akt-mTORC1—mediated activation of aerobic glycolysis that includes upregulation of HK2 and GLUT3146. These data, combined with the latest discoveries implying the participation of aerobic glycolysis in prostate cancer progression, suggest a possible role of Cav-1 as an inducer of multiple oncogenic pathways, with aerobic glycolysis being the final target (Figure 2).
Figure 2. Stimulation of aerobic glycolysis in the development of castrate-resistant prostate cancer.
Stimulation of PI3K/Akt signaling, driven in part by Cav-1-LRP6 signaling may lead to elevated levels of glycolytic enzymes and increased aerobic glycolysis in castrate-resistant prostate cancer.
CONCLUSION
Metastatic prostate cancer remains an incurable disease since in the majority of cases it eventually progresses upon ADT, while no chemotherapy or target agent has presented significant efficacy against CRPC. Moreover, there are no reliable biomarkers to monitor disease progression or guide the therapeutic decisions. The evolution of CRPC involves both androgen-stimulated and -repressed genes related to numerous alternative growth and survival pathways activated during the development of this disease upon ADT. The interactions between AR signaling and alternative survival pathways are cell-type and context-dependent and currently under extensive investigation. These oncogenic pathways, e.g., PI3K/Akt, are differentially activated in prostate tumors and ADT provides selective pressure in favor of castrate-resistant growth. Extrapolation of this complex information will hopefully lead to the discovery of new markers for disease monitoring and novel and combined therapies targeting critical pathways which provide survival advantage to prostate cancer cells.
ACKNOWLEDGMENTS
This research is supported in part by the National Institutes of Health through MD Anderson's Cancer Center Support Grant, 5 P30 CA016672. The authors thank Karen F. Phillips, ELS, for her expert editorial assistance.
Footnotes
CONFLICT OF INTEREST The authors do not declare any conflicts of interest.
REFERENCES
- 1.Huggins C. Prostatic cancer treated by orchiectomy; the five year results. J Am Med Assoc. 1946;131:576–81. doi: 10.1001/jama.1946.02870240008003. [DOI] [PubMed] [Google Scholar]
- 2.Harris WP, Mostaghel EA, Nelson PS, Montgomery B. Androgen deprivation therapy: progress in understanding mechanisms of resistance and optimizing androgen depletion. Nat Clin Pract Urol. 2009;6(2):76–85. doi: 10.1038/ncpuro1296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Marques RB, Dits NF, Erkens-Schulze S, van Weerden WM, Jenster G. Bypass mechanisms of the androgen receptor pathway in therapy-resistant prostate cancer cell models. PLoS One. 2010;5(10):e13500. doi: 10.1371/journal.pone.0013500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dayyani F, Gallick GE, Logothetis CJ, Corn PG. Novel therapies for metastatic castrate-resistant prostate cancer. Journal of the National Cancer Institute. 2011;103(22):1665–75. doi: 10.1093/jnci/djr362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Small EJ, Schellhammer PF, Higano CS, et al. Placebo-controlled phase III trial of immunologic therapy with sipuleucel-T (APC8015) in patients with metastatic, asymptomatic hormone refractory prostate cancer. J Clin Oncol. 2006;24(19):3089–94. doi: 10.1200/JCO.2005.04.5252. [DOI] [PubMed] [Google Scholar]
- 6.Higano CS, Schellhammer PF, Small EJ, et al. Integrated data from 2 randomized, double-blind, placebo-controlled, phase 3 trials of active cellular immunotherapy with sipuleucel-T in advanced prostate cancer. Cancer. 2009;115(16):3670–9. doi: 10.1002/cncr.24429. [DOI] [PubMed] [Google Scholar]
- 7.de Bono JS, Logothetis CJ, Molina A, et al. Abiraterone and increased survival in metastatic prostate cancer. N Engl J Med. 2011;364(21):1995–2005. doi: 10.1056/NEJMoa1014618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Scher HI, Beer TM, Higano CS, et al. Antitumour activity of MDV3100 in castration-resistant prostate cancer: a phase 1–2 study. Lancet. 2010;375(9724):1437–46. doi: 10.1016/S0140-6736(10)60172-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Scher HI, Fizazi K, Saad F, et al. Increased survival with enzalutamide in prostate cancer after chemotherapy. N Engl J Med. 2012;367(13):1187–97. doi: 10.1056/NEJMoa1207506. [DOI] [PubMed] [Google Scholar]
- 10.Efstathiou E, Titus M, Tsavachidou D, et al. Effects of abiraterone acetate on androgen signaling in castrate-resistant prostate cancer in bone. J Clin Oncol. 2012;30(6):637–43. doi: 10.1200/JCO.2010.33.7675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tran C, Ouk S, Clegg NJ, et al. Development of a second-generation antiandrogen for treatment of advanced prostate cancer. Science. 2009;324(5928):787–90. doi: 10.1126/science.1168175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fizazi K, Scher HI, Molina A, et al. Abiraterone acetate for treatment of metastatic castration-resistant prostate cancer: final overall survival analysis of the COU-AA-301 randomised, double-blind, placebo-controlled phase 3 study. Lancet Oncol. 2012;13(10):983–92. doi: 10.1016/S1470-2045(12)70379-0. [DOI] [PubMed] [Google Scholar]
- 13.Attard G, Cooper CS, de Bono JS. Steroid hormone receptors in prostate cancer: a hard habit to break? Cancer Cell. 2009;16(6):458–62. doi: 10.1016/j.ccr.2009.11.006. [DOI] [PubMed] [Google Scholar]
- 14.Scher HI, Sawyers CL. Biology of progressive, castration-resistant prostate cancer: directed therapies targeting the androgen-receptor signaling axis. J Clin Oncol. 2005;23(32):8253–61. doi: 10.1200/JCO.2005.03.4777. [DOI] [PubMed] [Google Scholar]
- 15.Mohler JL, Gregory CW, Ford OH, 3rd, et al. The androgen axis in recurrent prostate cancer. Clinical cancer research : an official journal of the American Association for Cancer Research. 2004;10(2):440–8. doi: 10.1158/1078-0432.ccr-1146-03. [DOI] [PubMed] [Google Scholar]
- 16.Locke JA, Guns ES, Lubik AA, et al. Androgen levels increase by intratumoral de novo steroidogenesis during progression of castration-resistant prostate cancer. Cancer Res. 2008;68(15):6407–15. doi: 10.1158/0008-5472.CAN-07-5997. [DOI] [PubMed] [Google Scholar]
- 17.Montgomery RB, Mostaghel EA, Vessella R, et al. Maintenance of intratumoral androgens in metastatic prostate cancer: a mechanism for castration-resistant tumor growth. Cancer Res. 2008;68(11):4447–54. doi: 10.1158/0008-5472.CAN-08-0249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Saloniemi T, Jokela H, Strauss L, Pakarinen P, Poutanen M. The diversity of sex steroid action: novel functions of hydroxysteroid (17beta) dehydrogenases as revealed by genetically modified mouse models. J Endocrinol. 2012;212(1):27–40. doi: 10.1530/JOE-11-0315. [DOI] [PubMed] [Google Scholar]
- 19.Mitsiades N, Sung CC, Schultz N, et al. Distinct Patterns of Dysregulated Expression of Enzymes Involved in Androgen Synthesis and Metabolism in Metastatic Prostate Cancer Tumors. Cancer Res. 2012;72(23):6142–52. doi: 10.1158/0008-5472.CAN-12-1335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Efstathiou E, Titus M, Tsavachidou D, et al. Effects of Abiraterone Acetate on Androgen Signaling in Castrate-Resistant Prostate Cancer in Bone. Journal of Clinical Oncology. 2012;30(6):637–43. doi: 10.1200/JCO.2010.33.7675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Attard G, Swennenhuis JF, Olmos D, et al. Characterization of ERG, AR and PTEN gene status in circulating tumor cells from patients with castration-resistant prostate cancer. Cancer Res. 2009;69(7):2912–8. doi: 10.1158/0008-5472.CAN-08-3667. [DOI] [PubMed] [Google Scholar]
- 22.Chen CD, Welsbie DS, Tran C, et al. Molecular determinants of resistance to antiandrogen therapy. Nat Med. 2004;10(1):33–9. doi: 10.1038/nm972. [DOI] [PubMed] [Google Scholar]
- 23.Edwards J, Krishna NS, Grigor KM, Bartlett JM. Androgen receptor gene amplification and protein expression in hormone refractory prostate cancer. Br J Cancer. 2003;89(3):552–6. doi: 10.1038/sj.bjc.6601127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bubendorf L, Kononen J, Koivisto P, et al. Survey of gene amplifications during prostate cancer progression by high-throughout fluorescence in situ hybridization on tissue microarrays. Cancer Res. 1999;59(4):803–6. [PubMed] [Google Scholar]
- 25.Mao X, Yu Y, Boyd LK, et al. Distinct genomic alterations in prostate cancers in Chinese and Western populations suggest alternative pathways of prostate carcinogenesis. Cancer Res. 2010;70(13):5207–12. doi: 10.1158/0008-5472.CAN-09-4074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ruiz C, Lenkiewicz E, Evers L, et al. Advancing a clinically relevant perspective of the clonal nature of cancer. Proc Natl Acad Sci U S A. 2011;108(29):12054–9. doi: 10.1073/pnas.1104009108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sirotnak FM, She Y, Khokhar NZ, Hayes P, Gerald W, Scher HI. Microarray analysis of prostate cancer progression to reduced androgen dependence: studies in unique models contrasts early and late molecular events. Mol Carcinog. 2004;41(3):150–63. doi: 10.1002/mc.20051. [DOI] [PubMed] [Google Scholar]
- 28.Tilley WD, Wilson CM, Marcelli M, McPhaul MJ. Androgen receptor gene expression in human prostate carcinoma cell lines. Cancer Res. 1990;50(17):5382–6. [PubMed] [Google Scholar]
- 29.Thompson J, Hyytinen ER, Haapala K, et al. Androgen receptor mutations in high-grade prostate cancer before hormonal therapy. Lab Invest. 2003;83(12):1709–13. doi: 10.1097/01.lab.0000107262.40402.44. [DOI] [PubMed] [Google Scholar]
- 30.Haapala K, Hyytinen ER, Roiha M, et al. Androgen receptor alterations in prostate cancer relapsed during a combined androgen blockade by orchiectomy and bicalutamide. Lab Invest. 2001;81(12):1647–51. doi: 10.1038/labinvest.3780378. [DOI] [PubMed] [Google Scholar]
- 31.Zhao XY, Malloy PJ, Krishnan AV, et al. Glucocorticoids can promote androgen-independent growth of prostate cancer cells through a mutated androgen receptor. Nat Med. 2000;6(6):703–6. doi: 10.1038/76287. [DOI] [PubMed] [Google Scholar]
- 32.Culig Z, Hobisch A, Cronauer MV, et al. Mutant androgen receptor detected in an advanced-stage prostatic carcinoma is activated by adrenal androgens and progesterone. Mol Endocrinol. 1993;7(12):1541–50. doi: 10.1210/mend.7.12.8145761. [DOI] [PubMed] [Google Scholar]
- 33.Steinkamp MP, O'Mahony OA, Brogley M, et al. Treatment-dependent androgen receptor mutations in prostate cancer exploit multiple mechanisms to evade therapy. Cancer Res. 2009;69(10):4434–42. doi: 10.1158/0008-5472.CAN-08-3605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dehm SM, Regan KM, Schmidt LJ, Tindall DJ. Selective role of an NH2-terminal WxxLF motif for aberrant androgen receptor activation in androgen depletion independent prostate cancer cells. Cancer Res. 2007;67(20):10067–77. doi: 10.1158/0008-5472.CAN-07-1267. [DOI] [PubMed] [Google Scholar]
- 35.Dehm SM, Tindall DJ. Alternatively spliced androgen receptor variants. Endocr Relat Cancer. 2011;18(5):R183–96. doi: 10.1530/ERC-11-0141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Li Y, Hwang TH, Oseth LA, et al. AR intragenic deletions linked to androgen receptor splice variant expression and activity in models of prostate cancer progression. Oncogene. 2012;31(45):4759–67. doi: 10.1038/onc.2011.637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hu R, Isaacs WB, Luo J. A snapshot of the expression signature of androgen receptor splicing variants and their distinctive transcriptional activities. Prostate. 2011;71(15):1656–67. doi: 10.1002/pros.21382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sun S, Sprenger CC, Vessella RL, et al. Castration resistance in human prostate cancer is conferred by a frequently occurring androgen receptor splice variant. J Clin Invest. 2010;120(8):2715–30. doi: 10.1172/JCI41824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hu R, Lu C, Mostaghel EA, et al. Distinct transcriptional programs mediated by the ligand-dependent full-length androgen receptor and its splice variants in castration-resistant prostate cancer. Cancer Res. 2012;72(14):3457–62. doi: 10.1158/0008-5472.CAN-11-3892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Li Y, Chan SC, Brand LJ, Hwang TH, Silverstein KA, Dehm SM. Androgen receptor splice variants mediate enzalutamide resistance in castration-resistant prostate cancer cell lines. Cancer Res. 2012 doi: 10.1158/0008-5472.CAN-12-3630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Guo Z, Dai B, Jiang T, et al. Regulation of androgen receptor activity by tyrosine phosphorylation. Cancer Cell. 2006;10(4):309–19. doi: 10.1016/j.ccr.2006.08.021. [DOI] [PubMed] [Google Scholar]
- 42.Dai B, Chen H, Guo S, et al. Compensatory upregulation of tyrosine kinase Etk/BMX in response to androgen deprivation promotes castration-resistant growth of prostate cancer cells. Cancer research. 2010;70(13):5587–96. doi: 10.1158/0008-5472.CAN-09-4610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wang Q, Li W, Zhang Y, et al. Androgen receptor regulates a distinct transcription program in androgen-independent prostate cancer. Cell. 2009;138(2):245–56. doi: 10.1016/j.cell.2009.04.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ueda T, Mawji NR, Bruchovsky N, Sadar MD. Ligand-independent activation of the androgen receptor by interleukin-6 and the role of steroid receptor coactivator-1 in prostate cancer cells. J Biol Chem. 2002;277(41):38087–94. doi: 10.1074/jbc.M203313200. [DOI] [PubMed] [Google Scholar]
- 45.Gregory CW, He B, Johnson RT, et al. A mechanism for androgen receptor-mediated prostate cancer recurrence after androgen deprivation therapy. Cancer Res. 2001;61(11):4315–9. [PubMed] [Google Scholar]
- 46.Agoulnik IU, Vaid A, Nakka M, et al. Androgens modulate expression of transcription intermediary factor 2, an androgen receptor coactivator whose expression level correlates with early biochemical recurrence in prostate cancer. Cancer research. 2006;66(21):10594–602. doi: 10.1158/0008-5472.CAN-06-1023. [DOI] [PubMed] [Google Scholar]
- 47.Xu J, Wu RC, O'Malley BW. Normal and cancer-related functions of the p160 steroid receptor co-activator (SRC) family. Nature reviews. Cancer. 2009;9(9):615–30. doi: 10.1038/nrc2695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Holzbeierlein J, Lal P, LaTulippe E, et al. Gene expression analysis of human prostate carcinoma during hormonal therapy identifies androgen-responsive genes and mechanisms of therapy resistance. Am J Pathol. 2004;164(1):217–27. doi: 10.1016/S0002-9440(10)63112-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sharma A, Yeow WS, Ertel A, et al. The retinoblastoma tumor suppressor controls androgen signaling and human prostate cancer progression. J Clin Invest. 2010;120(12):4478–92. doi: 10.1172/JCI44239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Yuan X, Balk SP. Mechanisms mediating androgen receptor reactivation after castration. Urol Oncol. 2009;27(1):36–41. doi: 10.1016/j.urolonc.2008.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Cai C, He HH, Chen S, et al. Androgen receptor gene expression in prostate cancer is directly suppressed by the androgen receptor through recruitment of lysine-specific demethylase 1. Cancer Cell. 2011;20(4):457–71. doi: 10.1016/j.ccr.2011.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Taylor BS, Schultz N, Hieronymus H, et al. Integrative genomic profiling of human prostate cancer. Cancer Cell. 2010;18(1):11–22. doi: 10.1016/j.ccr.2010.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Gurel B, Iwata T, Koh CM, et al. Nuclear MYC protein overexpression is an early alteration in human prostate carcinogenesis. Mod Pathol. 2008;21(9):1156–67. doi: 10.1038/modpathol.2008.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Thompson TC, Southgate J, Kitchener G, Land H. Multistage carcinogenesis induced by ras and myc oncogenes in a reconstituted organ. Cell. 1989;56(6):917–30. doi: 10.1016/0092-8674(89)90625-9. [DOI] [PubMed] [Google Scholar]
- 55.Zhang X, Lee C, Ng PY, Rubin M, Shabsigh A, Buttyan R. Prostatic neoplasia in transgenic mice with prostate-directed overexpression of the c-myc oncoprotein. Prostate. 2000;43(4):278–85. doi: 10.1002/1097-0045(20000601)43:4<278::aid-pros7>3.0.co;2-4. [DOI] [PubMed] [Google Scholar]
- 56.Iwata T, Schultz D, Hicks J, et al. MYC overexpression induces prostatic intraepithelial neoplasia and loss of Nkx3.1 in mouse luminal epithelial cells. PLoS One. 2010;5(2):e9427. doi: 10.1371/journal.pone.0009427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ellwood-Yen K, Graeber TG, Wongvipat J, et al. Myc-driven murine prostate cancer shares molecular features with human prostate tumors. Cancer Cell. 2003;4(3):223–38. doi: 10.1016/s1535-6108(03)00197-1. [DOI] [PubMed] [Google Scholar]
- 58.Yang G, Goltsov AA, Ren C, et al. Molecular cancer research : MCR. 2012. Caveolin-1 Upregulation Contributes to c-Myc-Induced High-Grade Prostatic Intraepithelial Neoplasia and Prostate Cancer. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Nupponen NN, Kakkola L, Koivisto P, Visakorpi T. Genetic alterations in hormone-refractory recurrent prostate carcinomas. Am J Pathol. 1998;153(1):141–8. doi: 10.1016/S0002-9440(10)65554-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Visakorpi T, Kallioniemi AH, Syvanen AC, et al. Genetic changes in primary and recurrent prostate cancer by comparative genomic hybridization. Cancer Res. 1995;55(2):342–7. [PubMed] [Google Scholar]
- 61.Bernard D, Pourtier-Manzanedo A, Gil J, Beach DH. Myc confers androgen-independent prostate cancer cell growth. J Clin Invest. 2003;112(11):1724–31. doi: 10.1172/JCI19035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Courtney KD, Corcoran RB, Engelman JA. The PI3K pathway as drug target in human cancer. J Clin Oncol. 2010;28(6):1075–83. doi: 10.1200/JCO.2009.25.3641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wang S, Gao J, Lei Q, et al. Prostate-specific deletion of the murine Pten tumor suppressor gene leads to metastatic prostate cancer. Cancer Cell. 2003;4(3):209–21. doi: 10.1016/s1535-6108(03)00215-0. [DOI] [PubMed] [Google Scholar]
- 64.Stiles B, Groszer M, Wang S, Jiao J, Wu H. PTENless means more. Dev Biol. 2004;273(2):175–84. doi: 10.1016/j.ydbio.2004.06.008. [DOI] [PubMed] [Google Scholar]
- 65.Gao H, Ouyang X, Banach-Petrosky WA, Shen MM, Abate-Shen C. Emergence of androgen independence at early stages of prostate cancer progression in Nkx3.1; Pten mice. Cancer Res. 2006;66(16):7929–33. doi: 10.1158/0008-5472.CAN-06-1637. [DOI] [PubMed] [Google Scholar]
- 66.Jiao J, Wang S, Qiao R, et al. Murine cell lines derived from Pten null prostate cancer show the critical role of PTEN in hormone refractory prostate cancer development. Cancer Res. 2007;67(13):6083–91. doi: 10.1158/0008-5472.CAN-06-4202. [DOI] [PubMed] [Google Scholar]
- 67.Chee KG, Longmate J, Quinn DI, et al. The AKT inhibitor perifosine in biochemically recurrent prostate cancer: a phase II California/Pittsburgh cancer consortium trial. Clin Genitourin Cancer. 2007;5(7):433–7. doi: 10.3816/CGC.2007.n.031. [DOI] [PubMed] [Google Scholar]
- 68.Kinkade CW, Castillo-Martin M, Puzio-Kuter A, et al. Targeting AKT/mTOR and ERK MAPK signaling inhibits hormone-refractory prostate cancer in a preclinical mouse model. J Clin Invest. 2008;118(9):3051–64. doi: 10.1172/JCI34764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Zhang W, Zhu J, Efferson CL, et al. Inhibition of tumor growth progression by antiandrogens and mTOR inhibitor in a Pten-deficient mouse model of prostate cancer. Cancer Res. 2009;69(18):7466–72. doi: 10.1158/0008-5472.CAN-08-4385. [DOI] [PubMed] [Google Scholar]
- 70.Carver BS, Chapinski C, Wongvipat J, et al. Reciprocal feedback regulation of PI3K and androgen receptor signaling in PTEN-deficient prostate cancer. Cancer Cell. 2011;19(5):575–86. doi: 10.1016/j.ccr.2011.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Mulholland DJ, Tran LM, Li Y, et al. Cell autonomous role of PTEN in regulating castration-resistant prostate cancer growth. Cancer Cell. 2011;19(6):792–804. doi: 10.1016/j.ccr.2011.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Lin HK, Hu YC, Lee DK, Chang C. Regulation of androgen receptor signaling by PTEN (phosphatase and tensin homolog deleted on chromosome 10) tumor suppressor through distinct mechanisms in prostate cancer cells. Mol Endocrinol. 2004;18(10):2409–23. doi: 10.1210/me.2004-0117. [DOI] [PubMed] [Google Scholar]
- 73.Wang Y, Mikhailova M, Bose S, Pan CX, deVere White RW, Ghosh PM. Regulation of androgen receptor transcriptional activity by rapamycin in prostate cancer cell proliferation and survival. Oncogene. 2008;27(56):7106–17. doi: 10.1038/onc.2008.318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Brognard J, Sierecki E, Gao T, Newton AC. PHLPP and a second isoform, PHLPP2, differentially attenuate the amplitude of Akt signaling by regulating distinct Akt isoforms. Mol Cell. 2007;25(6):917–31. doi: 10.1016/j.molcel.2007.02.017. [DOI] [PubMed] [Google Scholar]
- 75.Muranen T, Selfors LM, Worster DT, et al. Inhibition of PI3K/mTOR leads to adaptive resistance in matrix-attached cancer cells. Cancer Cell. 2012;21(2):227–39. doi: 10.1016/j.ccr.2011.12.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Bakin RE, Gioeli D, Bissonette EA, Weber MJ. Attenuation of Ras signaling restores androgen sensitivity to hormone-refractory C4-2 prostate cancer cells. Cancer Res. 2003;63(8):1975–80. [PubMed] [Google Scholar]
- 77.Suzuki A, Nakano T, Mak TW, Sasaki T. Portrait of PTEN: messages from mutant mice. Cancer Sci. 2008;99(2):209–13. doi: 10.1111/j.1349-7006.2007.00670.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Mulholland DJ, Kobayashi N, Ruscetti M, et al. Pten loss and RAS/MAPK activation cooperate to promote EMT and metastasis initiated from prostate cancer stem/progenitor cells. Cancer Res. 2012;72(7):1878–89. doi: 10.1158/0008-5472.CAN-11-3132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Wakefield LM, Roberts AB. TGF-beta signaling: positive and negative effects on tumorigenesis. Curr Opin Genet Dev. 2002;12(1):22–9. doi: 10.1016/s0959-437x(01)00259-3. [DOI] [PubMed] [Google Scholar]
- 80.Padua D, Massague J. Roles of TGFbeta in metastasis. Cell Res. 2009;19(1):89–102. doi: 10.1038/cr.2008.316. [DOI] [PubMed] [Google Scholar]
- 81.Seoane J. Escaping from the TGFbeta anti-proliferative control. Carcinogenesis. 2006;27(11):2148–56. doi: 10.1093/carcin/bgl068. [DOI] [PubMed] [Google Scholar]
- 82.Steiner MS, Zhou ZZ, Tonb DC, Barrack ER. Expression of transforming growth factor-beta 1 in prostate cancer. Endocrinology. 1994;135(5):2240–7. doi: 10.1210/endo.135.5.7956947. [DOI] [PubMed] [Google Scholar]
- 83.Wikstrom P, Stattin P, Franck-Lissbrant I, Damber JE, Bergh A. Transforming growth factor beta1 is associated with angiogenesis, metastasis, and poor clinical outcome in prostate cancer. Prostate. 1998;37(1):19–29. doi: 10.1002/(sici)1097-0045(19980915)37:1<19::aid-pros4>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- 84.Jones E, Pu H, Kyprianou N. Targeting TGF-beta in prostate cancer: therapeutic possibilities during tumor progression. Expert Opin Ther Targets. 2009;13(2):227–34. doi: 10.1517/14728220802705696. [DOI] [PubMed] [Google Scholar]
- 85.Karan D, Kelly DL, Rizzino A, Lin MF, Batra SK. Expression profile of differentially-regulated genes during progression of androgen-independent growth in human prostate cancer cells. Carcinogenesis. 2002;23(6):967–75. doi: 10.1093/carcin/23.6.967. [DOI] [PubMed] [Google Scholar]
- 86.Qi W, Gao S, Wang Z. Transcriptional regulation of the TGF-beta1 promoter by androgen receptor. Biochem J. 2008;416(3):453–62. doi: 10.1042/BJ20080651. [DOI] [PubMed] [Google Scholar]
- 87.Qi W, Gao S, Chu J, Zhou L, Wang Z. Negative androgen-response elements mediate androgen-dependent transcriptional inhibition of TGF-beta1 and CDK2 promoters in the prostate gland. J Androl. 2012;33(1):27–36. doi: 10.2164/jandrol.110.011999. [DOI] [PubMed] [Google Scholar]
- 88.Van Themsche C, Mathieu I, Parent S, Asselin E. Transforming growth factor-beta3 increases the invasiveness of endometrial carcinoma cells through phosphatidylinositol 3-kinase-dependent up-regulation of X-linked inhibitor of apoptosis and protein kinase c-dependent induction of matrix metalloproteinase-9. J Biol Chem. 2007;282(7):4794–802. doi: 10.1074/jbc.M608497200. [DOI] [PubMed] [Google Scholar]
- 89.Vinals F, Pouyssegur J. Transforming growth factor beta1 (TGF-beta1) promotes endothelial cell survival during in vitro angiogenesis via an autocrine mechanism implicating TGF-alpha signaling. Mol Cell Biol. 2001;21(21):7218–30. doi: 10.1128/MCB.21.21.7218-7230.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Wilkes MC, Mitchell H, Penheiter SG, et al. Transforming growth factor-beta activation of phosphatidylinositol 3-kinase is independent of Smad2 and Smad3 and regulates fibroblast responses via p21-activated kinase-2. Cancer Res. 2005;65(22):10431–40. doi: 10.1158/0008-5472.CAN-05-1522. [DOI] [PubMed] [Google Scholar]
- 91.Ding Z, Wu CJ, Chu GC, et al. SMAD4-dependent barrier constrains prostate cancer growth and metastatic progression. Nature. 2011;470(7333):269–73. doi: 10.1038/nature09677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Aitchison AA, Veerakumarasivam A, Vias M, et al. Promoter methylation correlates with reduced Smad4 expression in advanced prostate cancer. Prostate. 2008;68(6):661–74. doi: 10.1002/pros.20730. [DOI] [PubMed] [Google Scholar]
- 93.Lai SL, Chien AJ, Moon RT. Wnt/Fz signaling and the cytoskeleton: potential roles in tumorigenesis. Cell Res. 2009;19(5):532–45. doi: 10.1038/cr.2009.41. [DOI] [PubMed] [Google Scholar]
- 94.MacDonald BT, Tamai K, He X. Wnt/beta-catenin signaling: components, mechanisms, and diseases. Dev Cell. 2009;17(1):9–26. doi: 10.1016/j.devcel.2009.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.de la Taille A, Rubin MA, Chen MW, et al. Beta-catenin-related anomalies in apoptosis-resistant and hormone-refractory prostate cancer cells. Clin Cancer Res. 2003;9(5):1801–7. [PubMed] [Google Scholar]
- 96.Takeichi M. Cadherin cell adhesion receptors as a morphogenetic regulator. Science. 1991;251(5000):1451–5. doi: 10.1126/science.2006419. [DOI] [PubMed] [Google Scholar]
- 97.Heuberger J, Birchmeier W. Interplay of cadherin-mediated cell adhesion and canonical Wnt signaling. Cold Spring Harb Perspect Biol. 2010;2(2):a002915. doi: 10.1101/cshperspect.a002915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Kypta RM, Waxman J. Wnt/beta-catenin signalling in prostate cancer. Nat Rev Urol. 2012 doi: 10.1038/nrurol.2012.116. [DOI] [PubMed] [Google Scholar]
- 99.Truica CI, Byers S, Gelmann EP. Beta-catenin affects androgen receptor transcriptional activity and ligand specificity. Cancer Res. 2000;60(17):4709–13. [PubMed] [Google Scholar]
- 100.Mulholland DJ, Cheng H, Reid K, Rennie PS, Nelson CC. The androgen receptor can promote beta-catenin nuclear translocation independently of adenomatous polyposis coli. J Biol Chem. 2002;277:17933–43. doi: 10.1074/jbc.M200135200. [DOI] [PubMed] [Google Scholar]
- 101.Egawa S, Kadmon D, Miller GJ, Scardino PT, Thompson TC. Alterations in mRNA levels for growth-related genes after transplantation into castrated hosts in oncogene-induced clonal mouse prostate carcinoma. Molecular carcinogenesis. 1992;5(1):52–61. doi: 10.1002/mc.2940050110. [DOI] [PubMed] [Google Scholar]
- 102.Mulholland DJ, Dedhar S, Coetzee GA, Nelson CC. Interaction of nuclear receptors with the Wnt/beta-catenin/Tcf signaling axis: Wnt you like to know? Endocr Rev. 2005;26(7):898–915. doi: 10.1210/er.2003-0034. [DOI] [PubMed] [Google Scholar]
- 103.Mulholland DJ, Read JT, Rennie PS, Cox ME, Nelson CC. Functional localization and competition between the androgen receptor and T-cell factor for nuclear beta-catenin: a means for inhibition of the Tcf signaling axis. Oncogene. 2003;22(36):5602–13. doi: 10.1038/sj.onc.1206802. [DOI] [PubMed] [Google Scholar]
- 104.Chesire DR, Isaacs WB. Ligand-dependent inhibition of beta-catenin/TCF signaling by androgen receptor. Oncogene. 2002;21(55):8453–69. doi: 10.1038/sj.onc.1206049. [DOI] [PubMed] [Google Scholar]
- 105.Wan X, Liu J, Lu JF, et al. Activation of beta-catenin signaling in androgen receptor-negative prostate cancer cells. Clin Cancer Res. 2012;18(3):726–36. doi: 10.1158/1078-0432.CCR-11-2521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Yee D. The insulin-like growth factor system as a treatment target in breast cancer. Semin Oncol. 2002;29(3 Suppl 11):86–95. doi: 10.1053/sonc.2002.34060. [DOI] [PubMed] [Google Scholar]
- 107.LeRoith D, Roberts CT., Jr. The insulin-like growth factor system and cancer. Cancer Lett. 2003;195(2):127–37. doi: 10.1016/s0304-3835(03)00159-9. [DOI] [PubMed] [Google Scholar]
- 108.Baserga R, Peruzzi F, Reiss K. The IGF-1 receptor in cancer biology. Int J Cancer. 2003;107(6):873–7. doi: 10.1002/ijc.11487. [DOI] [PubMed] [Google Scholar]
- 109.Burfeind P, Chernicky CL, Rininsland F, Ilan J. Antisense RNA to the type I insulin-like growth factor receptor suppresses tumor growth and prevents invasion by rat prostate cancer cells in vivo. Proc Natl Acad Sci U S A. 1996;93(14):7263–8. doi: 10.1073/pnas.93.14.7263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Heidegger I, Ofer P, Doppler W, Rotter V, Klocker H, Massoner P. Diverse functions of IGF/insulin signaling in malignant and noncancerous prostate cells: proliferation in cancer cells and differentiation in noncancerous cells. Endocrinology. 2012;153(10):4633–43. doi: 10.1210/en.2012-1348. [DOI] [PubMed] [Google Scholar]
- 111.Nickerson T, Chang F, Lorimer D, Smeekens SP, Sawyers CL, Pollak M. In vivo progression of LAPC-9 and LNCaP prostate cancer models to androgen independence is associated with increased expression of insulin-like growth factor I (IGF-I) and IGF-I receptor (IGF-IR) Cancer Res. 2001;61(16):6276–80. [PubMed] [Google Scholar]
- 112.Pandini G, Mineo R, Frasca F, et al. Androgens up-regulate the insulin-like growth factor-I receptor in prostate cancer cells. Cancer Res. 2005;65(5):1849–57. doi: 10.1158/0008-5472.CAN-04-1837. [DOI] [PubMed] [Google Scholar]
- 113.Vander Heiden MG, Cantley LC, Thompson CB. Understanding the Warburg effect: the metabolic requirements of cell proliferation. Science. 2009;324(5930):1029–33. doi: 10.1126/science.1160809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Zhao Y, Liu H, Liu Z, et al. Overcoming trastuzumab resistance in breast cancer by targeting dysregulated glucose metabolism. Cancer Res. 2011;71(13):4585–97. doi: 10.1158/0008-5472.CAN-11-0127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Nakano A, Miki H, Nakamura S, et al. Up-regulation of hexokinaseII in myeloma cells: targeting myeloma cells with 3-bromopyruvate. J Bioenerg Biomembr. 2012;44(1):31–8. doi: 10.1007/s10863-012-9412-9. [DOI] [PubMed] [Google Scholar]
- 116.Moon JS, Jin WJ, Kwak JH, et al. Androgen stimulates glycolysis for de novo lipid synthesis by increasing the activities of hexokinase 2 and 6-phosphofructo-2-kinase/fructose-2,6-bisphosphatase 2 in prostate cancer cells. Biochem J. 2011;433(1):225–33. doi: 10.1042/BJ20101104. [DOI] [PubMed] [Google Scholar]
- 117.Massie CE, Lynch A, Ramos-Montoya A, et al. The androgen receptor fuels prostate cancer by regulating central metabolism and biosynthesis. EMBO J. 2011;30(13):2719–33. doi: 10.1038/emboj.2011.158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Faubert B, Boily G, Izreig S, et al. AMPK Is a Negative Regulator of the Warburg Effect and Suppresses Tumor Growth In Vivo. Cell Metab. 2013;17(1):113–24. doi: 10.1016/j.cmet.2012.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Vaz CV, Alves MG, Marques R, et al. Androgen-responsive and nonresponsive prostate cancer cells present a distinct glycolytic metabolism profile. Int J Biochem Cell Biol. 2012;44(11):2077–84. doi: 10.1016/j.biocel.2012.08.013. [DOI] [PubMed] [Google Scholar]
- 120.Ros S, Santos CR, Moco S, et al. Functional metabolic screen identifies 6-phosphofructo-2-kinase/fructose-2,6-biphosphatase 4 as an important regulator of prostate cancer cell survival. Cancer Discov. 2012;2(4):328–43. doi: 10.1158/2159-8290.CD-11-0234. [DOI] [PubMed] [Google Scholar]
- 121.Lin Y, Wang F. FGF signalling in prostate development, tissue homoeostasis and tumorigenesis. Biosci Rep. 2010;30(5):285–91. doi: 10.1042/BSR20100020. [DOI] [PubMed] [Google Scholar]
- 122.Ozen M, Giri D, Ropiquet F, Mansukhani A, Ittmann M. Role of fibroblast growth factor receptor signaling in prostate cancer cell survival. J Natl Cancer Inst. 2001;93(23):1783–90. doi: 10.1093/jnci/93.23.1783. [DOI] [PubMed] [Google Scholar]
- 123.Memarzadeh S, Xin L, Mulholland DJ, et al. Enhanced paracrine FGF10 expression promotes formation of multifocal prostate adenocarcinoma and an increase in epithelial androgen receptor. Cancer Cell. 2007;12(6):572–85. doi: 10.1016/j.ccr.2007.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Spencer WC, Zeller G, Watson JD, et al. A spatial and temporal map of C. elegans gene expression. Genome research. 2011;21(2):325–41. doi: 10.1101/gr.114595.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Birchmeier C, Birchmeier W, Gherardi E, Vande Woude GF. Met, metastasis, motility and more. Nat Rev Mol Cell Biol. 2003;4(12):915–25. doi: 10.1038/nrm1261. [DOI] [PubMed] [Google Scholar]
- 126.Varkaris A, Corn PG, Gaur S, Dayyani F, Logothetis CJ, Gallick GE. The role of HGF/c-Met signaling in prostate cancer progression and c-Met inhibitors in clinical trials. Expert Opin Investig Drugs. 2011;20(12):1677–84. doi: 10.1517/13543784.2011.631523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Knudsen BS, Gmyrek GA, Inra J, et al. High expression of the Met receptor in prostate cancer metastasis to bone. Urology. 2002;60(6):1113–7. doi: 10.1016/s0090-4295(02)01954-4. [DOI] [PubMed] [Google Scholar]
- 128.Verras M, Lee J, Xue H, Li TH, Wang Y, Sun Z. The androgen receptor negatively regulates the expression of c-Met: implications for a novel mechanism of prostate cancer progression. Cancer Res. 2007;67(3):967–75. doi: 10.1158/0008-5472.CAN-06-3552. [DOI] [PubMed] [Google Scholar]
- 129.Sun Y, Wang BE, Leong KG, et al. Androgen deprivation causes epithelial-mesenchymal transition in the prostate: implications for androgen-deprivation therapy. Cancer research. 2012;72(2):527–36. doi: 10.1158/0008-5472.CAN-11-3004. [DOI] [PubMed] [Google Scholar]
- 130.Zhu ML, Kyprianou N. Role of androgens and the androgen receptor in epithelial-mesenchymal transition and invasion of prostate cancer cells. FASEB J. 2010;24(3):769–77. doi: 10.1096/fj.09-136994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Jeter CR, Liu B, Liu X, et al. NANOG promotes cancer stem cell characteristics and prostate cancer resistance to androgen deprivation. Oncogene. 2011;30(36):3833–45. doi: 10.1038/onc.2011.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Sternberg PW, Schmid SL. Caveolin, cholesterol and Ras signalling. Nat Cell Biol. 1999;1(2):E35–7. doi: 10.1038/10028. [DOI] [PubMed] [Google Scholar]
- 133.Williams TM, Lisanti MP. Caveolin-1 in oncogenic transformation, cancer, and metastasis. Am J Physiol Cell Physiol. 2005;288(3):C494–506. doi: 10.1152/ajpcell.00458.2004. [DOI] [PubMed] [Google Scholar]
- 134.Shatz M, Liscovitch M. Caveolin-1: a tumor-promoting role in human cancer. Int J Radiat Biol. 2008;84(3):177–89. doi: 10.1080/09553000701745293. [DOI] [PubMed] [Google Scholar]
- 135.Thompson TC, Tahir SA, Li L, et al. The role of caveolin-1 in prostate cancer: clinical implications. Prostate Cancer Prostatic Dis. 2010;13(1):6–11. doi: 10.1038/pcan.2009.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Tahir SA, Ren C, Timme TL, et al. Development of an immunoassay for serum caveolin-1: a novel biomarker for prostate cancer. Clin Cancer Res. 2003;9(10 Pt 1):3653–9. [PubMed] [Google Scholar]
- 137.Tahir SA, Frolov A, Hayes TG, et al. Preoperative serum caveolin-1 as a prognostic marker for recurrence in a radical prostatectomy cohort. Clin Cancer Res. 2006;12(16):4872–5. doi: 10.1158/1078-0432.CCR-06-0417. [DOI] [PubMed] [Google Scholar]
- 138.Yang G, Truong LD, Timme TL, et al. Elevated expression of caveolin is associated with prostate and breast cancer. Clin Cancer Res. 1998;4(8):1873–80. [PubMed] [Google Scholar]
- 139.Li L, Yang G, Ebara S, et al. Caveolin-1 mediates testosterone-stimulated survival/clonal growth and promotes metastatic activities in prostate cancer cells. Cancer Res. 2001;61(11):4386–92. [PubMed] [Google Scholar]
- 140.Mouraviev V, Li L, Tahir SA, et al. The role of caveolin-1 in androgen insensitive prostate cancer. The Journal of Urology. 2002;168(4 Pt 1):1589–96. doi: 10.1016/S0022-5347(05)64526-0. [DOI] [PubMed] [Google Scholar]
- 141.Nasu Y, Timme TL, Yang G, et al. Suppression of caveolin expression induces androgen sensitivity in metastatic androgen-insensitive mouse prostate cancer cells. Nat Med. 1998;4(9):1062–4. doi: 10.1038/2048. [DOI] [PubMed] [Google Scholar]
- 142.Tahir SA, Yang G, Goltsov AA, et al. Tumor cell-secreted caveolin-1 has proangiogenic activities in prostate cancer. Cancer Res. 2008;68(3):731–9. doi: 10.1158/0008-5472.CAN-07-2668. [DOI] [PubMed] [Google Scholar]
- 143.Li L, Ren CH, Tahir SA, Ren C, Thompson TC. Caveolin-1 maintains activated Akt in prostate cancer cells through scaffolding domain binding site interactions with and inhibition of serine/threonine protein phosphatases PP1 and PP2A. Mol Cell Biol. 2003;23(24):9389–404. doi: 10.1128/MCB.23.24.9389-9404.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Li L, Ren C, Yang G, Goltsov AA, Tabata K, Thompson TC. Caveolin-1 promotes autoregulatory, Akt-mediated induction of cancer-promoting growth factors in prostate cancer cells. Mol Cancer Res. 2009;7(11):1781–91. doi: 10.1158/1541-7786.MCR-09-0255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Tahir SA, Kurosaka S, Tanimoto R, Goltsov AA, Park S, Thompson TC. Serum caveolin-1, a biomarker of drug response and therapeutic target in prostate cancer models. Cancer Biol Ther. 2012;14(2) doi: 10.4161/cbt.22633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Tahir SA, Yang G, Goltsov AA, et al. Caveolin-1-LRP6 Signaling Module Stimulates Aerobic Glycolysis in Prostate Cancer. Cancer Res. 2013 doi: 10.1158/0008-5472.CAN-12-3040. [DOI] [PMC free article] [PubMed] [Google Scholar]