Abstract
Background
Existing data on outcomes following subdural hematoma have provided limited information on medical complications and functional outcomes. Mortality rates previously reported range from 22% to 66%.
Methods
This is a retrospective cohort study of prospectively collected data from a trauma registry in Washington State from 2005 through 2008. Patients were categorized by surgical evacuation status with the hypothesis that those undergoing evacuation represented a more severe injury.
Results
The 1,427 patients included in the study had a mean age of 58 years, and most of them were male (63%). Glasgow Coma Scale (GCS) score on presentation was greater than 12 in 58%; the average Injury Severity Score (ISS) was 27.5. Mean length of stay was 9.6 days (range, 1–110), with 40% spending 2 or more days in the intensive care unit. Twenty-eight percent experienced medical complications. At discharge, 94% had GCS score of 13 or greater. Independence with expression, feeding, and locomotion at discharge was noted for 92%, 81%, and 43%, respectively. Inpatient mortality was 16% and did not differ significantly between the evacuated group (15%) and the nonevacuated group (17%).
Conclusion
This large cohort of patients with acute traumatic subdural hematoma demonstrated a lower mortality rate than those of previous reports, including among patients requiring surgical evacuation (J Trauma Acute Care Surg. 2012;73:1348–1352).
Level of Evidence
Epidemiologic study, level III.
Keywords: Acute subdural hematoma, traumatic brain injury, subdural hematoma, mortality
While subdural hematomas (SDHs) are a common form of traumatic brain injury, the outcomes of adult patients with SDH are not well described in the literature. Most previous studies of SDH included patients who received care more than 20 years ago1–4 and lack information on medical complications and functional status.5,6 All are limited by small sample size (i.e., n = 47 to 308).1–8
We had the unique opportunity to study a large cohort of patients treated for SDH in a Level I trauma center with prospectively collected, standardized information on clinical characteristics, hospital course, functional outcomes, and mortality. We hypothesized that current mortality rates are lower than previously reported. To further evaluate this, we specifically compared patients undergoing surgical evacuation with those without evacuation, with the expectation that those undergoing surgical evacuation represent a subset with increased risk for poor outcomes.
Patients and Methods
This retrospective cohort study is based on the collected experience of patients 16 years and older with a diagnosis of traumatic SDH evaluated at Harborview Medical Center in Seattle, Washington, a 413-bed Level I trauma center operated by the University of Washington. It serves a five-state area including Washington, Wyoming, Montana, Alaska, and Idaho. Standardized data, prospectively collected as part of the Harborview Medical Center Trauma Registry, were used for all analyses. This registry includes all trauma patients evaluated at Harborview Medical Center, including those who died in the emergency department and those admitted from or transferred to another facility.
Eligible patients were diagnosed with acute traumatic SDH (DRG International Classification of Diseases—9th Rev.—Clinical Modification [ICD-9-CM] diagnosis codes9 800.29, 800.79, 800.41, 800.71, 800.42, 800.72, 800.59, 800.69, 800.79, and all codes between 852.21 and 852.29) evaluated between January 1, 2005, and December 31, 2008. Of 26,149 patients in the trauma registry for the study period, 1,427 (18%) met diagnostic criteria. Seven patients were seen in the emergency department more than once during the study period; for each of these patients, one randomly selected hospital course was used.
Once patients presenting to the emergency department have had their cardiopulmonary status stabilized, they have a rapid and directed neurologic examination and appropriate imaging. In our facility, comatose patients, or those unable to follow commands, with an intracranial mass lesion and more than 5 mm of shift proceed to the operating room unless brain-dead. These patients receive routine intracranial pressure monitoring. Patients who are alert and can follow commands do not routinely have invasive monitoring and are admitted for simple observation.
Trauma registry data are prospectively recorded by nurses and physicians during routine clinical care. Trained nurse coders and clinical data specialists abstract additional data from the medical record for hospital quality improvement purposes and for reporting to the Washington State Department of Health. Data are composed of demographic information, medical history, and detailed information on presentation to the hospital including the mechanism of injury, Abbreviated Injury Scale (AIS) score for head and neck,10 the Injury Severity Score (ISS)11 and the Glasgow Coma Scale (GCS) score.12
Data gathered on the hospital course included medical complications; surgical procedures, including evacuation procedures; length of hospital stay; and days spent in the intensive care unit (ICU). For the purpose of analysis, patients were classified as “evacuated” if they underwent neurosurgical intervention for the hematoma and “nonevacuated” if they did not. Procedures included craniotomy, craniectomy, and incision or excision of brain tissue. ICD-9-CM procedure codes were used to make this distinction (ICD-9-CM 01.24, 01.25, 01.31, 01.39, 01.59, and 02.99). In-hospital mortality rate, discharge location, and functional status at discharge were assessed for all patients by nurse chart review. Functional status was measured as degree of independence in feeding, expression, and locomotion.
We calculated statistics, both descriptive and for comparison by evacuation status, using Stata 11 (StataCorp, College Station, TX). p values are from χ2 tests for categorical variables and t tests for continuous variables. The University of Washington Institutional Review Board reviewed and approved all study procedures.
Results
Characteristics of the 1,427 study patients are shown in Table 1. The majority were male (63%), the mean age was 58 years (range, 16–105 years), and most were white (79%). Medical history included hypertension (37%), cardiac disease (20%), diabetes mellitus (15%), and previous trauma (8%). Alcohol abuse was reported in 12% and drug abuse in 6%. Many of the patients had multiple comorbid medical or lifestyle-related conditions, with 18% having three and an additional 14% having four or more comorbid conditions.
Table 1. Demographic, Medical Comorbidity, and Lifestyle Characteristics of Adult Patients With Acute Traumatic SDH Stratified by Receipt of Surgical Intervention.
| Variable | All Patients With SDH | Evacuated | Not Evacuated |
|---|---|---|---|
|
|
|
|
|
| (n = 1,427) | (n = 248) | (n = 1,179) | |
| Male, n (%) | 901 (63%) | 163 (66%) | 738 (63%) |
| Age* | |||
| Mean (SD) | 58.2 (22.6) | 60.8 (21.4) | 57.6 (22.8) |
| Range | 16–105 | 16–95 | 16–105 |
| Age categories, n (%)* | |||
| 16–25 | 172 (12) | 29 (12) | 143 (12) |
| 26–40 | 180 (13) | 20 (8) | 160 (14) |
| 41–55 | 282 (20) | 33 (13) | 249 (21) |
| 56–70 | 270 (19) | 67 (27) | 203 (17) |
| 71–85 | 363 (25) | 73 (29) | 290 (25) |
| >85 | 160 (11) | 26 (10) | 134 (11) |
| Race, n (%)† | |||
| White | 1,117 (79) | 183 (75) | 934 (80) |
| Asian or Pacific Islander | 94 (7) | 25 (10) | 69 (6) |
| African American | 63 (4) | 11 (4) | 52 (4) |
| Native American | 25 (2) | 3 (1) | 22 (2) |
| Other | 116 (8) | 23 (9) | 93 (8) |
| Medical history, n (%) | |||
| Hypertension* | 525 (37) | 108 (44) | 417 (35) |
| Cardiac disease | 282 (20) | 54 (22) | 228 (19) |
| Diabetes | 207 (15) | 39 (16) | 168 (14) |
| Previous trauma* | 116 (8) | 29 (12) | 87 (7) |
| Gastroenterologic disease/cirrhosis* | 119 (8) | 26 (10) | 93 (8) |
| Psychiatric disease | 98 (7) | 15 (6) | 83 (7) |
| Respiratory illness | 99 (7) | 17 (7) | 82 (7) |
| Cancer | 106 (7) | 12 (5) | 94 (8) |
| Stroke* | 106 (7) | 28 (11) | 78 (7) |
| Seizure disorder | 76 (5) | 17 (7) | 59 (5) |
| Dementia | 75 (5) | 16 (6) | 59 (5) |
| Other* | 273 (19) | 56 (23) | 217 (18) |
| Lifestyle history, n (%) | |||
| Tobacco use | 174 (12) | 28 (11) | 146 (12) |
| Alcohol abuse* | 171 (12) | 41 (17) | 130 (11) |
| Drug abuse | 80 (6) | 8 (3) | 72 (6) |
| No. comorbidities, n (%)‡ | |||
| None | 367 (26) | 49 (20) | 318 (27) |
| 1 | 297 (21) | 48 (19) | 249 (21) |
| 2 | 298 (21) | 54 (22) | 244 (20) |
| 3 | 259 (18) | 54 (22) | 205 (17) |
| 4 or more | 206 (14) | 43 (17) | 163 (14) |
| Unknown | 141 (10) | 24 (10) | 117 (10) |
p < 0.05.
Twelve missing values include 3 evacuated and 9 not evacuated.
Calculated as a total of medical and lifestyle history.
Of the 1,427 patients, 248 (17%) underwent surgical intervention for subdural evacuation and 1,179 (83%) had no surgical evacuation. Evacuated patients were slightly older, tended to be nonwhite, and were more likely to have a history of hypertension, stroke, and alcohol abuse than the nonevacuated group.
Information on mechanism of traumatic injury and initial assessment are shown in Table 2. Most injuries were caused by falls (57%) and motor vehicle crashes (28%), and 63% of the patients were referred from outside medical facilities. More evacuated than nonevacuated patients were injured in a fall (67% vs. 55%) and referred from an outside facility (78% vs. 61%). On evaluation in the emergency department, most of the patients with SDH (58%) had a GCS score of 13 or greater, and 35% had a GCS score of 8 or less. The percentage of patients with GCS score of 5 or less was higher among those who were evacuated than those not evacuated (34% vs. 28%). Mean (SD) total AIS score was 7.7 (3.2) for all patients. There was no difference between evacuated and not evacuated groups. Most of the patients had AIS head and neck injury rating of severe (47%) or critical (52%). More evacuated patients had critical AIS rating for head and neck than nonevacuated (98% vs. 43%, respectively). The mean ISS was 27.5 (range, 10–75). There was no difference in ISS based on evacuation status. The Trauma and Injury Severity Score (TRISS) probability of survival was lower for evacuated patients (0.854) than nonevacuated patients (0.909). In the emergency department, most patients had systolic blood pressure between 91 mm Hg and 140 mm Hg (70%) and were afebrile (temperature ≤ 37.5°C, 88%).
Table 2. Characteristics of Patient Injury and Initial Assessment in the Emergency Department.
| Variable | All SDH | Evacuated | Not Evacuated |
|---|---|---|---|
|
|
|
|
|
| (n = 1,427) | (n = 248) | (n = 1,179) | |
| Mechanism of injury, n (%)*† | |||
| Fall | 773 (57) | 159 (67) | 614 (55) |
| Motor vehicle crash | 378 (28) | 45 (19) | 333 (30) |
| Assault | 112 (8) | 16 (7) | 96 (8) |
| Bicycle Crash | 36 (3) | 5 (2) | 31 (3) |
| Other | 60 (4) | 11 (5) | 49 (4) |
| Referred from outside facility, (%)‡ | |||
| Yes | 904 (63) | 179 (78) | 725 (61) |
| No | 523 (37) | 69 (28) | 454 (38) |
| GCS score in emergency department, n (%)*§ | |||
| Mild (13–15) | 773 (58) | 110 (49) | 663 (60) |
| Moderate (9–12) | 89 (7) | 21 (9) | 68 (6) |
| Severe (6–8) | 80 (6) | 18 (8) | 62 (6) |
| Very severe (3–5) | 386 (29) | 77 (34) | 309 (28) |
| Acute injury scale–total | |||
| Mean (SD) | 7.7 (3.2) | 7.4 (2.6) | 7.7 (3.3) |
| Acute injury scale–Head and Neck, n (%)‖ | |||
| Serious (3) | 6 (<1) | 0 (0) | 6 (<1) |
| Severe (4) | 668 (47) | 3 (1) | 665 (56) |
| Critical (5) | 746 (52) | 244 (98) | 502 (43) |
| Fatal (6) | 7 (<1) | 1 (1) | 6 (<1) |
| ISS | |||
| Mean (SD) | 27.5 | 29.8 | 27 |
| Range | 10–75 | 17–75 | 10–75 |
| 10–18 | 405 (28) | 2 (<1) | 403 (34) |
| 19–32 | 681 (48) | 188 (76) | 493 (42) |
| 33–74 | 330 (23) | 57 (23) | 273 (23) |
| 75 | 11 (1) | 1 (<1) | 10 (1) |
| TRISS* | 0.902 | 0.854 | 0.909 |
Missing values: mechanism of injury (98), 13 evacuated, 84 not evacuated; GCS score (99), 22 evacuated, 77 not evacuated; TRISS (574), 115 evacuated, 459 not evacuated.
p < 0.01.
p < 0.002.
p = 0.01.
p < 0.001.
Urine toxicology result was positive in 269 of the 825 patients tested, with the most common intoxicants being cannabis (29%, n = 79), opiates (18%, n = 49), cocaine (18%, n = 48), and barbiturates (12%, n = 33).
Data on the hospital course are presented in Table 3. Most patients were hospitalized in the ICU at some point during their hospital course (86%), and 46% spent 1 day in the ICU. The mean total length of the hospital stay was 9.6 days (range, 1–110 days). Evacuated patients had longer ICU and total hospital stays than nonevacuated patients. In this cohort, 24% had a surgical procedure other than the evacuation of the SDH, with additional surgical procedures more common in the evacuated group (51%) than the in nonevacuated group (19%).
Table 3. Hospital Course of 1,427 Patients With SDH.
| Variable | All SDH | Evacuated | Not Evacuated |
|---|---|---|---|
|
|
|
|
|
| (n = 1,427) | (n = 248) | (n = 1,179) | |
| Total days in ICU | |||
| Mean (SD) | 3.4 (6.1) | 5.6 (7.2) | 2.9 (5.7) |
| 0, n (%) | 200 (14) | 8 (3) | 192 (16) |
| 1, n (%) | 652 (46) | 56 (23) | 596 (51) |
| 2, n (%) | 162 (11) | 45 (18) | 117 (10) |
| 3–5, n (%) | 180 (13) | 67 (27) | 113 (10) |
| 6–10, n (%) | 114 (8) | 35 (14) | 79 (7) |
| >10, n (%) | 119 (8) | 37 (15) | 82 (7) |
| Total length of hospital stay, d* | |||
| Mean (SD) | 9.6 (12.7) | 15.1 (15.1) | 8.4 (11.8) |
| 1, n (%) | 267 (19) | 3 (1) | 264 (23) |
| 2, n (%) | 152 (11) | 7 (3) | 145 (12) |
| 3, n (%) | 121 (9) | 15 (6) | 106 (9) |
| 4, n (%) | 118 (8) | 18 (7) | 100 (9) |
| 5–7, n (%) | 238 (17) | 50 (20) | 188 (16) |
| 7–14, n (%) | 244 (17) | 72 (29) | 172 (15) |
| 14–30, n (%) | 190 (13) | 55 (22) | 135 (12) |
| >30, n (%) | 91 (6) | 28 (11) | 63 (5) |
| Did patient have other surgery? | |||
| Yes, n (%) | 347 (24) | 128 (51) | 219 (19) |
Ten missing values: 7 died at admission, 3 died in hospital—none evacuated.
Medical complications were noted in 28% of patients during the hospital stay (Table 4). The most common complications were pneumonia (8%), urinary tract infection (7%), and acute respiratory distress syndrome (3%). There were no significant differences in complications by evacuation status.
Table 4. Medical Complications Noted in a Cohort of 1,427 Patients With Acute Traumatic SDH.
| Variable | All SDH | Evacuated | Not Evacuated |
|---|---|---|---|
|
|
|
|
|
| (n = 1,427) | (n = 248) | (n = 1,179) | |
| Medical complication, n (%) | |||
| No | 1,021 (72) | 91 (37) | 315 (27) |
| Yes | 406 (28) | 157 (63) | 864 (73) |
| Pulmonary, n (%) | 160 (11) | 51 (21) | 104 (9) |
| Pneumonia | 111 (8) | 39 (15) | 72 (6) |
| ARDS | 43 (3) | 15 (6) | 28 (2) |
| Respiratory arrest | 25 (2) | 9 (4) | 16 (1) |
| Hemothorax or pneumothorax | 10 (<1) | 5 (2) | 5 (<1) |
| Difficult airway | 8 (1) | 1 (<1) | 7 (<1) |
| Infectious, n (%) | 134 (9) | 29 (12) | 105 (9) |
| Urinary tract infection | 106 (7) | 20 (8) | 86 (7) |
| Wound infection | 14 (1) | 6 (2) | 8 (<1) |
| Sepsis | 22 (2) | 5 (2) | 17 (1) |
| Cardiovascular, n (%) | 66 (5) | 20 (8) | 46 (4) |
| Major arrhythmia | 28 (2) | 8 (3) | 20 (2) |
| Pulmonary edema | 15 (1) | 6 (2) | 9 (<1) |
| Myocardial infarction | 16 (1) | 4 (2) | 12 (1) |
| Cardiac arrest | 12 (<1) | 4 (2) | 8 (<1) |
| Congestive heart failure | 8 (<1) | 2 (<1) | 6 (<1) |
| Hematologic, n (%) | 36 (3) | 8 (3) | 28 (2) |
| Thrombosis, central venous or deep vein | 23 (2) | 6 (2) | 17 (1) |
| Pulmonary embolism | 16 (1) | 4 (2) | 12 (1) |
| Acute renal failure, n (%) | 20 (1) | 3 (1) | 17 (1) |
| Alcohol or drug withdrawal, n (%) | 28 (2) | 2 (<1) | 26 (2) |
ARDS, adult respiratory distress syndrome.
Mortality and functional outcomes are shown in Table 5. In-hospital mortality was 14%, with no significant difference between evacuated and nonevacuated patients. Traumatic brain injury was the leading cause of death in all groups (71%), followed by multiple injuries (11%) and pulmonary complications (10%). At discharge, GCS score was 13 or greater in 94% of all surviving patients with SDH. While most patients (55%) were discharged home, a skilled nursing facility and rehabilitation center were required by 27% and 14%, respectively, at discharge. Most were independently functioning without assistance of any devices at discharge in the areas of feeding (81%) and expression (92%), with less independence in locomotion (43%). Independent functioning among evacuated patients was more common across all domains when compared to the none-vacuated group.
Table 5. Mortality and Functional Status of 1,427 Patients With Acute Traumatic SDH.
| Variable | All SDH | Evacuated | Not Evacuated |
|---|---|---|---|
|
|
|
|
|
| (n = 1,427) | (n = 248) | (n = 1,179) | |
| Mortality, n (%) | |||
| Died | 200 (14) | 32 (13) | 168 (14) |
| Discharged alive | 1,233 (86) | 217 (87) | 1,016 (86) |
| Cause of death, n (%) | |||
| Traumatic brain injury | 142 (71) | 23 (72) | 119 (71) |
| Pulmonary | 20 (10) | 6 (19) | 14 (8) |
| Polytrauma | 22 (11) | 1 (3) | 21 (13) |
| Cardiac | 16 (8) | 2 (6) | 14 (8) |
| GCS score at discharge, | |||
| n (%)*† | |||
| Mild (13–15) | 1,090 (94) | 184 (88) | 906 (95) |
| Moderate (9–012) | 40 (3) | 13 (6) | 27 (3) |
| Severe (6–8) | 20 (2) | 5 (2) | 15 (2) |
| Very severe (3–5) | 9 (1) | 8 (4) | 1 (<1) |
| Discharge location, n (%)*† | |||
| Home | 658 (55) | 71 (33) | 587 (60) |
| Skilled nursing facility | 315 (27) | 69 (33) | 246 (25) |
| Rehabilitation | 164 (14) | 60 (28) | 104 (11) |
| Other acute care facility | 53 (4) | 12 (6) | 41 (4) |
| Level of functioning–feeding, n (%)*† | |||
| Independent | 937 (81) | 139 (66) | 798 (84) |
| Independent with device | 16 (1) | 4 (2) | 12 (1) |
| Partially dependent | 127 (11) | 35 (17) | 92 (10) |
| Totally dependent | 80 (7) | 33 (15) | 47 (5) |
| Level of functioning–locomotion, n (%)*† | |||
| Independent | 502 (43) | 62 (29) | 440 (46) |
| Independent with device | 197 (17) | 27 (13) | 170 (18) |
| Partially dependent | 320 (28) | 83 (39) | 237 (25) |
| Totally dependent | 141 (12) | 39 (19) | 102 (11) |
| Level of functioning–expression, n (%)*† | |||
| Independent | 1,071 (92) | 172 (82) | 899 (95) |
| Independent with device | 8 (1) | 3 (1) | 5 (<1) |
| Partially dependent | 32 (3) | 14 (7) | 18 (2) |
| Totally dependent | 49 (4) | 22 (10) | 27 (3) |
p < 0.001.
Missing values: GCS score at discharge (68), 6 evacuated, 62 not evacuated; discharge location (37), 4 evacuated, 33 not evacuated; level of functioning feeding, locomotion, and expression (67), 5 evacuated, 62 not evacuated.
Discussion
We report a mortality rate of 14% for adult patients hospitalized with acute traumatic SDH, which is lower than those of previous studies among the largest sample size and most recent cohort of patients (Fig. 1). No significant difference in mortality was seen between evacuated and nonevacuated patients. Distinctively, we report prospectively collected standardized information on variables not previously reported in the literature, including medical comorbidity, length of stay, and functional outcomes. Previous studies focused primarily on the surgical patient population with higher mortality rates and provided limited information on length of stay and functional status at hospital discharge.
Figure 1.
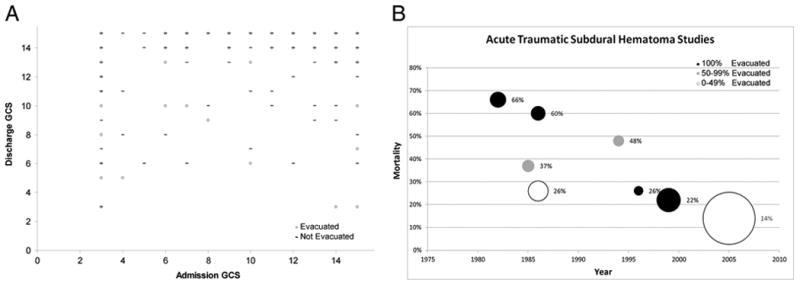
Acute traumatic SDH studies.
When we compare the mortality rate of patients in our study who underwent evacuation procedures with those of previous studies in which all patients were evacuated, the mortality we observed (14%) remains lower than studies those from the late 1990s to the mid 2000s (22–26%).5,8 The highest mortality rates observed among evacuated patients were reported for patients admitted in the 1980s to early 1990s (60–66%).2,4 We postulate that the reasons for the lower mortality rate noted in our study compared with those of published data are multifactorial. First, widespread use of computed tomographic (CT) scan imaging has likely led to detection of patients with less severe subdural bleeding than those in the past. Previous studies focus on the surgical population and factors associated with good surgical outcomes, while we describe the outcomes of all patients. A second cause of the lower mortality rates over time could be the improvement in surgical techniques and specialized care within trauma centers.13
In addition to describing the hospital course and mortality rates of patients with SDHs, we report on functional status at discharge and the discharge location. While previous studies have reported on patients' general level of independence at discharge, our study provides detailed standardized information regarding their need for partial or total assistance in the three main domains of expression, feeding, and locomotion. Most patients in the present study were discharged with mild residual neurologic injury by GCS (94% had GCS score ≥ 13), and many were independently functioning with regard to expression (92%) and feeding (81%). The majority were not independent in locomotion (57%), and almost half were discharged to either a skilled nursing facility, acute care facility, or rehabilitation center (45%).
A limitation of our study is that it uses single-center data. However, the study population includes patients presenting from a five-state referral base, with more than half of the patients (63%) referred from an outside facility. Unlike some previous study populations, our cohort includes patients with polytrauma, which may complicate the hospital course and could lead to worse functional outcomes or higher mortality rates. Thus, our findings may not be representative of patients with isolated or nontraumatic SDH. We do not have available CT data on the characteristics of the SDH, such as presence of midline shift and size, and have no data indicating the anticoagulation status of patients before injury, all of which may impact survival. While this is the first study to report information on specific domains of functional status at the time of discharge, data were not collected on the level of functioning before admission. Thus, we could not determine whether decreased mobility at discharge was related to the SDH or to other chronic disease or concomitant injury.
The rates of pulmonary embolism and deep venous thrombosis are lower than expected for this population. We are unable to explain this finding using the data available. It is possible that the represented patient population is healthier than expected, with 35% staying for less than 3 days. These patients may be mobile and less likely to develop thrombosis. It may also be that deep venous thrombosis and pulmonary embolism were underdiagnosed in sicker patients, owing to either comorbid injury or death.
In conclusion, our study found a lower mortality rate for patients admitted with acute traumatic SDH than those of previous reports. Patients may now be diagnosed at earlier stages of disease by CT imaging. In addition, the treatment of SDH may be improving owing to regionalization of care in centers of excellence. While the mortality rate may be lower, the burden of SDH on functional independence and quality of life remains to be better delineated.
Acknowledgments
Disclosure: This work was supported by the National Cancer Institute at the National Institutes of Health (2 KO5 CA104699-06 to J.G.E.).
Footnotes
This study was presented in part at Hospital Medicine 2011, Dallas, Texas, on May 2011.
Authorship: C.G.R. was responsible for the literature search, data collection and analysis, study design, writing, and figures. R.E.T. contributed to the data collection and analysis, study design, writing, and figures. P.K.C., N.R.T., and J.G.E. contributed to the study design, data analysis and interpretation, and the written report. R.G.E. contributed to the written report.
References
- 1.Dent DL, Croce MA, Menke PG, Young BH, Hinson MS, Kudsk KA, et al. Prognostic factors after acute subdural hematoma. J Trauma. 1995;39:36–42. doi: 10.1097/00005373-199507000-00005. discussion 42–43. [DOI] [PubMed] [Google Scholar]
- 2.Wilberger JE, Jr, Harris M, Diamond DL. Acute subdural hematoma: morbidity and mortality related to timing of operative intervention. J Trauma. 1990;30:733–736. [PubMed] [Google Scholar]
- 3.Abe M, Udono H, Tabuchi K, Uchino A, Yoshikai T, Taki K. Analysis of ischemic brain damage in cases of acute subdural hematomas. Surg Neurol. 2003;59:464–472. doi: 10.1016/s0090-3019(03)00078-8. discussion 472. [DOI] [PubMed] [Google Scholar]
- 4.Koc RK, Akdemir H, Oktem IS, Meral M, Menku A. Acute subdural hematoma: outcome and outcome prediction. Neurosurg Rev. 1997;20:239–244. doi: 10.1007/BF01105894. [DOI] [PubMed] [Google Scholar]
- 5.Tian HL, Chen SW, Xu T, Hu J, Rong BY, Wang G, et al. Risk factors related to hospital mortality in patients with isolated traumatic acute subdural haematoma: analysis of 308 patients undergone surgery. Chin Med J (Engl) 2008;121:1080–1084. [PubMed] [Google Scholar]
- 6.Depreitere B, Van Calenbergh F, van Loon J. A clinical comparison of non-traumatic acute subdural haematomas either related to coagulopathy or of arterial origin without coagulopathy. Acta Neurochir (Wien) 2003;145:541–546. doi: 10.1007/s00701-003-0020-7. discussion 546. [DOI] [PubMed] [Google Scholar]
- 7.Servadei F, Nasi MT, Cremonini AM, Giuliani G, Cenni P, Nanni A. Importance of a reliable admission Glasgow Coma Scale score for determining the need for evacuation of posttraumatic subdural hematomas: a prospective study of 65 patients. J Trauma. 1998;44:868–873. doi: 10.1097/00005373-199805000-00021. [DOI] [PubMed] [Google Scholar]
- 8.Tallon JM, Ackroyd-Stolarz S, Karim SA, Clarke DB. The epidemiology of surgically treated acute subdural and epidural hematomas in patients with head injuries: a population-based study. Can J Surg. 2008;51:339–345. [PMC free article] [PubMed] [Google Scholar]
- 9.ICD-9-CM: International Classification of Diseases, 9th revision. Los Angeles, CA: Practice Management Information Corporation; 2006. [Google Scholar]
- 10.Rating the severity of tissue damage. I. the abbreviated scale. JAMA. 1971;215:277–280. doi: 10.1001/jama.1971.03180150059012. [DOI] [PubMed] [Google Scholar]
- 11.Baker SP, O'Neill B, Haddon W, Jr, Long WB. The Injury Severity Score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14:187–196. [PubMed] [Google Scholar]
- 12.Jennett B, Teasdale G, Braakman R, Minderhoud J, Knill-Jones R. Predicting outcome in individual patients after severe head injury. Lancet. 1976;1:1031–1034. doi: 10.1016/s0140-6736(76)92215-7. [DOI] [PubMed] [Google Scholar]
- 13.DuBose JJ, Browder T, Inaba K, Teixeira PG, Chan LS, Demetriades D. Effect of trauma center designation on outcome in patients with severe traumatic brain injury. Arch Surg. 2008;143:1213–1217. doi: 10.1001/archsurg.143.12.1213. discussion 1217. [DOI] [PubMed] [Google Scholar]


