Abstract
Patient: Male, 53
Final Diagnosis: Acute Warfarin toxicity
Symptoms: —
Medication: Warfarin
Clinical Procedure: —
Specialty: Hematology
Objective:
Unusual clinical course
Background:
Warfarin remains the most common anticoagulant in the management of thromboembolic diseases. However, its extensive drug interaction requires frequent monitoring and dose adjustments. Almost all antibiotics, including penicillins, have the potential to interact with warfarin causing either under or over anticoagulation which increases the risk for thrombus formation and significant bleeding respectively.
Case Report:
A 53-year-old Caucasian male with a history of protein C deficiency and recurrent intravascular thrombosis developed a dental abscess. He was treated with amoxicillin/clavulanate 500/125 mg twice daily and referred to a dentist. He developed significant bleeding after tooth extraction. INR was 20.4. He received fresh frozen plasma and vitamin K with resolution of bleeding.
Conclusions:
While rare, clinically significant prolonged prothrombin time and potentially life threatening bleeding can occur when amoxicillin/clavulanate is concomitantly administered with warfarin. Prompt recognition and intervention is necessary to avoid life threatening complications from warfarin-amoxicillin/clavulanate interaction.
MeSH Keywords: Warfarin – adverse effects, supratherapeutic INR, Amoxicillin, Protein C Deficiency, Clavulanic Acid
Background
Warfarin is the most commonly prescribed oral anticoagulant in the management of thromboembolic disease [1]. Warfarin has a narrow therapeutic window which necessitates frequent monitoring and dose adjustments in order to remain therapeutic. Many medications are known to interact with warfarin resulting in either over or under anticoagulation [2,3]. Over anticoagulation increases the risk of major bleeding. Concomitant administration of antibiotics along with warfarin is associated with a high risk of over anticoagulation. Bleeding is the most clinically important complication associated with over anticoagulation [4]. Hereinwe present a case of a 53-year-old man who presented with significant, severe bleeding from a tooth extraction after he was treated with amoxicillin/clavulanate while on warfarin.
Case Report
A 53-year-old Caucasian male with a past medical history of protein C deficiency, recurrent deep vein thrombosis, and pulmonary embolism developed a dental abscess. He was prescribed amoxicillin/clavulanate 500/125 mg twice daily and referred to a dentist. He underwent an uncomplicated outpatient tooth extraction after five days of antibiotic therapy. On the second day after the procedure, he noticed bleeding from the extraction site. On the third day, the bleeding worsened; he called his dentist and was seen urgently at the dentist’s office. Exploration of the surgical site demonstrated bleeding without hematoma formation. Several additional sutures were placed, the site was packed with gauze, and he was instructed to hold pressure if further bleeding developed. On day five, heavy bleeding returned, he noticed hematuria, and extensive bruising on his right forearm. He called his primary care physician (PCP) who instructed him to urgently contact his dentist and have his prothrombin time (PT) and international normalized ratio (INR) checked. His PT was 145 seconds, INR was 20.4. His dentist placed several more sutures and the patient was referred to the emergency room.
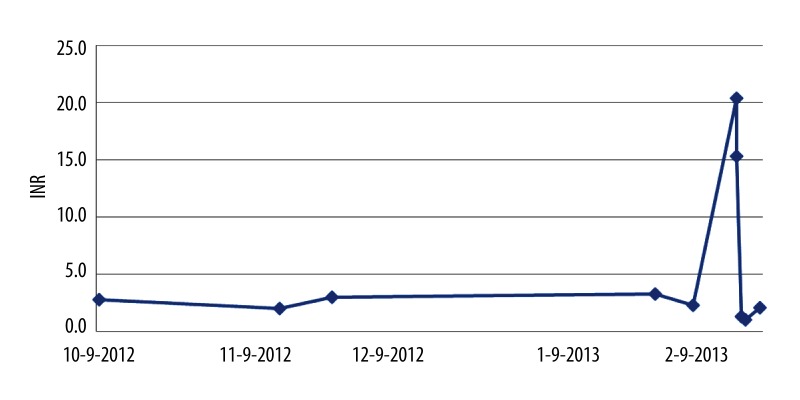
He had been taking warfarin 2 mg on Monday, Wednesday and Friday and 1 mg Tuesday, Thursday, Saturday, and Sunday for the past 20 years for chronic anticoagulation. His goal INR was in the range of 2.0–3.0, most recent INR less than one week prior to the procedure was 2.3. Figure 1 displays his INR trend over the preceding several months. His other medical problems include COPD, chronic non-union of his calcaneus following fracture, anxiety, and depression. He takes inhaled albuterol as needed, trazodone 50 mg po at bedtime, chlordiazepoxide 10 mg po 1 to 3 times a day and vicodin ES 7.5/750 1tab po as needed for pain. There had not been any recent change to his medications.
Figure 1.
INR trend from 4 months prior to hospital admission to two weeks after.
In the emergency room, his vital signs were stable, exam revealed bleeding from the extraction site and large bruises on the forearms bilaterally. Initial lab work showed Hb 13.7 g/dL, Hct 39.6%, WBC 8,100/mcL, and platelet count of 230,000/mcL. Serum electrolytes, renal function, liver function, thyroid function were all in the normal range. Repeat INR was 15.3, urinalysis demonstrated microscopic hematuria, and stool sample was guaiac positive. He received 4 units of fresh frozen plasma and 10 mg of vitamin K IV. Warfarin was held. The patient was admitted for close observation.
The bleeding from the extraction site resolved. His INR the next day was 1.3. Warfarin therapy was reinitiated and he was discharged home with enoxaparin 100mg subcutaneous daily for 5 days and oral warfarin at his prior dose. His INR one week after discharge was 2.3.
Discussion
The anticoagulant effect of warfarin is mediated through inhibition of the vitamin K-dependent gamma-carboxylation of coagulation factors II, VII, IX, and X [5]. Almost all antibiotics have the theoretical potential to interact with Warfarin [6]. The apparent mechanism is related to a pharmacodynamic interaction via reductionin intestinal flora with subsequent reduced intrinsic vitamin K production leading to decreased vitamin K absorption. Additional mechanisms include antibiotic induced malabsorption of vitamin K and inhibition of cytochrome p450 isozymes, which reduces warfarin metabolisim [7]. Quinolones, sulfonamides, macrolides, and azole antifungals carry the highest risk of Warfarin toxicity [8–10].
Although penicillins have not consistently been shown to interact with warfarin [11], isolated cases have been reported, particularly with broad-spectrum penicillins. Narrow-spectrum penicillins are generally presumed to be safe provided the patients’ vitamin K intake is normal [12]. In a double-blind, crossover, placebo-controlled study Zhang et al demonstrated that amoxicillin/clavulanate did not alter INR in 12 patients on stable warfarin therapy who were given amoxicillin/clavulanate, of note these patients did not have active infection or inflammation [13]. There are, however, several case reports and retrospective reviews implicating amoxicillin/clavulanate as a cause of increased INR and/or increased risk of bleeding (Table 1).
Table 1.
Cases reported in the English literature of amoxicillin or amoxicillin/clavulanate induced warfarin toxicity.
| Case | Outcome | |
|---|---|---|
| Bandrowsky et al., 1996 [14] | 75-year old warfarinised patient started on amoxicillin 500mg po three times a day for 7 days | Significant post-extraction hemorrhage on day four |
| Davydov et al., 2003 [15] | 58 year old female stable INR previously after started on amoxicillin-clavulanate 500/125 mg tablets, to be taken as 1 tablet three times daily for 7 days for a suspected ear infection | Significant increase in INR to 6.2 with hematuria |
| Kelly et al., 2005 [16] | 75-year-old man receiving long-term stable Warfarin anticoagulation treated for lower respiratory tract infection with oral amoxicillin 250 mg/clavulanate potassium 125 mg three times daily for 7 days | Rectus sheath hematoma |
| Wood et al., 1993 [17] | 85-yearold female patient previously kept within the therapeutic range, who had received a 7-day course of augmentin 250 mg three times daily | Increase in INR to 10 |
| Presented Case, 2013 | A 53-year-old man with a past medical history of protein C deficiency, recurrent deep vein thrombosis, and pulmonary embolism treated for dental abscess with amoxicillin/clavulanate 500/125 mg twice daily for 5 days | INR increased to 20.3 and clinically significant bleeding from the extraction site |
We reviewed the potential interactions between our patient’s other medications and warfarin. Although acetaminophen has the potential to interact with warfarin [18], the patient had been taking acetaminophen intermittently for many years, had not recently increased his acetaminophen dose, and had never experienced major fluctuations in his INR. The temporal relationship between the administration of amoxicillin/clavulanate and development of supratherapeutic INR with bleeding implicate amoxicillin/clavulanate as the culprit. The Naranjo probability scale identifies our case as a probable adverse drug reaction [19].
The primary factor influencing the risk of bleeding is intensity of anticoagulation, the risk of major bleeding (e.g., intracranial, retroperitoneal, gastrointestinal) has been reported to increase when the INR is greater than 4.0 [20,21]. Hemorrhagic complications increase steeply when the INR is greater than 5.0.
The management of patients with warfarin toxicity depends on the level of INR and the presence or absence of clinically significant bleeding. Recommendation set forth by the American College of Chest Physicians include indications for both vitamin K and blood products (such as fresh frozen plasma) (Table 2) [22].
Table 2.
Treatment of patients with supratherapeutic anticoagulation according to guidelines set forth by the American College of Chest Physicians.
| INR | Bleeding present | Recommended action |
|---|---|---|
| >Therapeutic to 5.0 | No | Lower warfarin dose, or Omit a dose and resume warfarin at a lower dose when INR is in therapeutic range, or No dose reduction needed if INR is minimally prolonged |
| >5.0 to 9.0 | No | Omit the next 1 to 2 doses of warfarin, monitor INR more frequently, and resume treatment at a lower dose when INR is in therapeutic range, or Omit a dose and administer 1 to 2.5 mg oral vitamin K1 for patients at increased risk of bleeding (e.g., history of bleeding, stroke, renal insufficiency, anemia, and hypertension) |
| >9.0 | No | Hold warfarin and administer 2.5 to 5 mg oral vitamin K1. Monitor INR more frequently and administer more vitamin K1 as needed, Resume warfarin at a lower dose when INR is in therapeutic range |
| Any | Serious or life-threatening | Hold warfarin and administer 10 mg vitamin K1 by slow IV infusion; supplement with prothrombin complex concentrate, fresh frozen plasma, or recombinant human factor VIIa, depending on clinical urgency. Monitor and repeat as needed |
Conclusions
While rare, clinically significant increased INR and potentially life threatening bleeding can occur when amoxicillin/clavulanate is concomitantly administered with warfarin. Prompt recognition and intervention is necessary to avoid life threatening complications from warfarin-amoxicillin/clavulanate interaction.
References:
- 1.Jacobs LG. Warfarin pharmacology, clinical management, and evaluation of hemorrhagic risk for the elderly. Clin Geriatr Med. 2005;22:17–32. doi: 10.1016/j.cger.2005.09.001. [DOI] [PubMed] [Google Scholar]
- 2.Holbrook AM, Pereira JA, Labiris R, et al. Systematic overview of warfarin and its drug and food interactions. Arch Intern Med. 2005;165:1095–106. doi: 10.1001/archinte.165.10.1095. [DOI] [PubMed] [Google Scholar]
- 3.Penning-van Beest F, Erkens J, Petersen KU, et al. Main comedications associated with major bleeding during anticoagulant therapy with coumarins. Eur J ClinPharmacol. 2005;61:439–44. doi: 10.1007/s00228-005-0947-0. [DOI] [PubMed] [Google Scholar]
- 4.Freedman MD, Olatidoye AG. Clinically significant drug interactions with the oral anticoagulants. Drug Safety. 1994;10(5):381–94. doi: 10.2165/00002018-199410050-00003. [DOI] [PubMed] [Google Scholar]
- 5.Freedman MD. Oral anticoagulants: pharmacodynamics, clinical indications and adverse effects. J Clin Pharmacol. 1992;32(3):196–209. doi: 10.1002/j.1552-4604.1992.tb03827.x. [DOI] [PubMed] [Google Scholar]
- 6.Rice PJ, Perry RJ, Afzal Z, Stockley IH. Antibacterial prescribing and warfarin: a review. Br Dent J. 2003;194(8):411–15. doi: 10.1038/sj.bdj.4810049. [DOI] [PubMed] [Google Scholar]
- 7.Kaminsky LS, Zhang ZY. Human P450 metabolism of warfarin. Pharmacol Thera. 1997;73(1):67–74. doi: 10.1016/s0163-7258(96)00140-4. [DOI] [PubMed] [Google Scholar]
- 8.Schelleman H, Bilker WB, Brensinger CM, et al. Warfarin with fluoroquinolones, sulfonamides, or azole antifungals: interactions and the risk of hospitalization for gastrointestinal bleeding. Clin Pharmacol Ther. 2008;84(5):581–88. doi: 10.1038/clpt.2008.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Glasheen JJ, Fugit RV, Prochazka AV. The risk of overanticoagulation with antibiotic use in outpatients on stable warfarin regimens. J Gen Inter Med. 2005;20(7):653–56. doi: 10.1111/j.1525-1497.2005.0136.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Baillargeon J, Holmes HM, Lin YL, et al. Concurrent use of warfarin and antibiotics and the risk of bleeding in older adults. Am J Med. 2012;125(2):183–89. doi: 10.1016/j.amjmed.2011.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Anticoagulant Clinic Study Group . Pharm J (Pharmacy Practice Suppl) Vol. 257. Buckley; 1996. A multicentre survey of antibiotics on the INR of anticoagulated patients; p. R30. [Google Scholar]
- 12.Buckley NA, Dawson AH. Drug interactions with warfarin. Med J Austr. 1992;157:479–83. [PubMed] [Google Scholar]
- 13.Zhang Q, Simoneau G, Verstuyft C, et al. Amoxicillin/clavulanic acid-warfarin drug interaction: a randomized controlled trial. Br J Clin Pharmacol. 2011;71(2):232–36. doi: 10.1111/j.1365-2125.2010.03824.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bandrowsky T, Vorono AA, Borris TJ, Marcantoni HW. Amoxicillin-related postextraction bleeding in an anticoagulated patient with tranexamic acid rinses. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996;82(6):610–12. doi: 10.1016/s1079-2104(96)80433-1. [DOI] [PubMed] [Google Scholar]
- 15.Davydov L, Yermolnik M, Cuni LJ. Warfarin and amoxicillin/clavulanate drug interaction. The Ann Pharmacother. 2003;37(3):367–70. doi: 10.1345/aph.1C243. [DOI] [PubMed] [Google Scholar]
- 16.Kelly M, Moran J, Byrne S. Formation of rectus sheath hematoma with antibiotic use and warfarin therapy: a case report. Am J Geriatr Pharmacother. 2005;3(4):266–69. [PubMed] [Google Scholar]
- 17.Wood GD, Deeble T. Warfarin: dangers with antibiotics. Dent Update. 1993;20(8):350–52. [PubMed] [Google Scholar]
- 18.Shek KL, Chan LN, Nutescu E. Warfarin-acetaminophen drug interaction revisited. Pharmacotherapy. 1999;19:1153–58. doi: 10.1592/phco.19.15.1153.30584. [DOI] [PubMed] [Google Scholar]
- 19.Naranjo CA, Busto U, Sellers EM, et al. A method for estimating the probability of adverse drug reactions. Clin Pharmacol. 1981;30:239. doi: 10.1038/clpt.1981.154. [DOI] [PubMed] [Google Scholar]
- 20.Howard PA, Ellerbeck EF, Engelman KK, Patterson KL. The nature and frequency of potential warfarin drug interactions that increase the risk of bleeding in patients with atrial fibrillation. Pharmacoepidemiol Drug Saf. 2002;11(7):569–76. doi: 10.1002/pds.748. [DOI] [PubMed] [Google Scholar]
- 21.Ansell J, Hirsh J, Poller L, et al. The pharmacology and management of the vitamin K antagonists: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest. 2004;126(3 Suppl.):204S–33S. doi: 10.1378/chest.126.3_suppl.204S. [DOI] [PubMed] [Google Scholar]
- 22.Ansell J, Hirsh J, Hylek E, et al. Pharmacology and management of the vita-min K antagonists. Chest. 2008;133(Suppl.6):160S–98S. doi: 10.1378/chest.08-0670. [DOI] [PubMed] [Google Scholar]