Abstract
Study Design Literature review.
Objective To discuss the evaluation and management of subaxial cervical spine trauma (C3–7).
Methods A literature review of the main imaging modalities, classification systems, and nonsurgical and surgical treatment performed.
Results Computed tomography and reconstructions allow for accurate radiologic identification of subaxial cervical spine trauma in most cases. Magnetic resonance imaging can be utilized to evaluate the stabilizing discoligamentous complex, the nerves, and the spinal cord. The Subaxial Injury Classification (SLIC) is a new system that aids in injury classification and helps guide the decision-making process of conservative versus surgical treatment. Though promising, the SLIC system requires further validation. When the decision for surgical treatment is made, early decompression (less than 24 hours) has been associated with better neurologic recovery. Surgical treatment should be individualized based on the injury characteristics and surgeon's preferences.
Conclusions The current state of subaxial cervical spine trauma is one of great progress. However, many questions remain unanswered. We need to continue to account for the individual patient, surgeon, and hospital circumstances that effect decision making and care.
Keywords: subaxial cervical spine trauma, diagnosis, classification, treatment
Introduction
Cervical spine trauma is one of the most common sites of spinal cord injury (SCI). Anatomically, subaxial cervical spine trauma consists of injuries from C3 to C7,1 2 with more than 50% of the cervical spine injuries located between C5 and C7.3 The potential catastrophic events associated with subaxial cervical spine trauma, including tetraplegia and severe permanent disability, require a consistent and evidence-based diagnosis and treatment plan. In this article, we review critical concepts in the diagnosis, classification, and treatment of subaxial cervical spine trauma.
Diagnostic Imaging
After hemodynamic stabilization, all injured patients should be screened for subaxial cervical injuries. Today, computed tomography (CT) scans with coronal and sagittal reconstructions are available in almost all trauma centers and provide rich and detailed information about the status of the cervical spine.4 5 6 A sensitivity of 99% and specificity of 100% have been reported with multiplanar CT scan screening of cervical injuries, compared with a sensitivity of just 70% with plain radiographies.7 8 CT imaging with reconstructions provide high sensitivity for injury detection and, as such, may allow for early removal of cervical precautions, avoiding complications associated with prolonged immobilization.5 Anecdotal cases of occult ligamentous injury have been reported, however.9 10 As such, despite the advances of CT imaging, a thorough clinical assessment of the patient remains critical.
Magnetic resonance (MR) imaging is a promising technology in subaxial cervical spine trauma. MR is often used in patients with cervical SCI as well as in patients with cervical translational or distractive injuries. MR can also be utilized to identify ventral and dorsal compressive lesions (disk herniation, hematoma, bone) that may be critical for determining surgical approach. In injuries with questionable stability, MR has been used to assess the status of the discoligamentous complex (DLC): a descriptive amalgamation of the anterior longitudinal ligament, posterior longitudinal ligament, disk, facet capsules, and posterior supporting ligaments.11 12 MR may additionally be useful in the evaluation of soft tissue injuries, disk herniation, and hematomas, especially in neurologically injured patients with normal CT scan findings.13 Although MR has been shown to have a high sensitivity, a low specificity for ligamentous injury has been reported to date.11 This may increase the risk of unnecessary treatments, including surgery, in an otherwise stable injury and dictates caution in using MR findings as a definitive surgical indication.11
Classification
Accurate and reproducible injury classification is an important step in the decision-making process for all spine injuries. Moreover, effective injury classification is critical in clinical care, education, and comparative research.
Many systems have been historically proposed to classify subaxial cervical spine trauma.14 15 16 One of the most commonly used was the Magerl et al classification system, initially proposed for the thoracolumbar spine, which has been extrapolated to cervical spine injuries, classifying them as type A (axial force injuries), type B (distraction), and type C (rotational).16 However, this system is based on plain radiographs and does not consider the neurologic status of the patient, a critical determinant of surgical treatment.
Based on these potential weaknesses, the Spinal Trauma Study Group has proposed a new classification system, the Subaxial Injury Classification System (SLIC), and injury severity score.12 This system is based on three major characteristics that should be taken in account in the decision-making process: (1) injury morphology; (2) integrity of the DLC; and (3) the neurologic status of the patient. Each one of these three factors is classified in isolation, with a final score resulting from the summation of these three variables (Table 1). The system recommends treatment based on the final severity score. A score of less than 4 points supports conservative treatment and 5 or more points supports surgical treatment. Patients with 4 points may be treated conservatively or surgically, depending on surgeon's experience, patient's preference, and additional comorbid conditions. The authors of the SLIC suggested that specific confounding factors may further influence the treatment chosen, including obesity, poor bone quality, and severe systemic trauma, among others.12 Two illustrative cases of subaxial cervical spine trauma treated based on the SLIC are presented in Figs. 1 and 2.
Table 1. The subaxial injury classification system.
| Points | |
|---|---|
| Injury morphology | |
| No abnormality | 0 |
| Compression | 1 |
| Burst | +1 |
| Distraction | 2 |
| Translation | 3 |
| Integrity of the discoligamentous complex | |
| Intact | 0 |
| Indeterminate | 1 |
| Disrupted | 2 |
| Neurologic status | |
| Intact | 0 |
| Nerve root injury | 1 |
| Complete | 2 |
| Incomplete | 3 |
| Persistent cord compression | +1 |
Fig. 1.
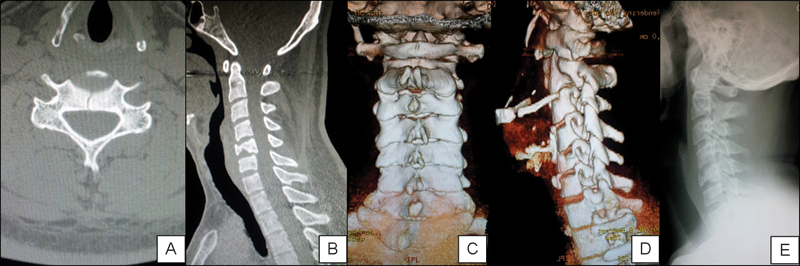
This 25-year-old man presented with neck pain after a diving injury. His neurologic exam was without deficits. (A) An axial computed tomography (CT) scan demonstrates a linear sagittal fracture crossing the vertebral body. (B) Height loss of the vertebral body is noted in the sagittal CT scan reconstruction, without canal compression. (C, D) A CT scan reconstruction shows facet joint integrity without evident posterior elements injury. The Subaxial Injury Classification score was 2 points (burst) + 0 points for discoligamentous complex status + 0 points for neurologic status = 2 points—conservative treatment was performed with a rigid cervical collar and closed radiologic follow-up. (E) Lateral cervical X-ray 8 months after treatment with good spinal alignment and fracture healing. The patient was asymptomatic.
Fig. 2.
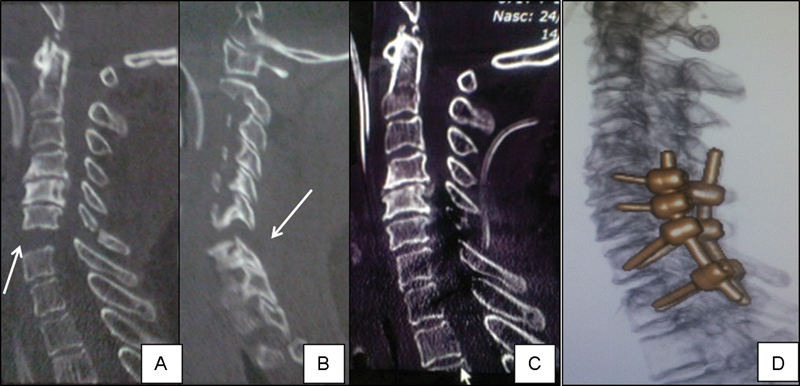
A 71-year-old woman presented after an automotive accident with an incomplete spinal cord injury (American Spine Injury Association Impairment Scale [AIS] grade B). (A, B) A distractive injury is identified at C6–7 in the sagittal CT scan reconstruction (white arrow). The Subaxial Injury Classification score was 3 points (distractive injury) + 2 points (discoligamentous complex injury) + 3 points (incomplete neurologic deficits) = 8 points—surgical treatment was performed. Postoperative sagittal (C) and 3-D reconstruction (D) CT scans showing reestablishment of cervical alignment and facet joint congruence, with lateral mass screws at C5 and C6 and pedicle screws at C7 and T1. After 6 months of follow-up, she had some neurologic improvement (AIS grade C).
Applying the SLIC—Special Considerations
Morphology
Compression injuries encompass compression fractures, burst fractures, teardrop injuries, and sagittal or coronal split fractures.12 Minimally displaced facet fractures can be present, as well as small posterior elements injuries, without evidence of distraction or rotation deformity. Distraction injuries are represented by vertical dissociation of the spinal elements and perched facet joints. Translational/rotational injuries are defined by axial listhesis of the vertebral bodies with either unilateral or bilateral facet joint dislocations. The floating lateral mass is considered a translational/rotational injury given its risk for displacement. Spinous process fractures and nondisplaced small facet fractures, although often associated with other injury patterns, are not accounted for within the described injury morphologies.
Integrity of Discoligamentous Complex
The status of the DLC is defined as disrupted in patients with distraction and translation/rotational morphologies, receiving 2 points for DLC injury. Other patients with compression injuries or those with radiographically stable injuries are inferred to have an intact DLC. The indeterminate state of the DLC is the most controversial aspect of the SLIC system. The lack of specificity of MR can overestimate injuries to the DLC, leading to a higher severity score and unnecessary surgeries.8 Based on this, it should be used cautiously in the medical decision-making process.11 12 In patients with more stable injuries, MR should not be used in isolation to access the status of the DLC.
Another important clinical confounding factor is the presence of concomitant cervical degenerative disease in the setting of a cervical spine trauma. For instance, in patients with cervical spinal stenosis, incomplete neurologic deficits, and no evidence of fracture or dislocations, the SLIC final assessment results in 4 points (0 for morphology + 3 for incomplete deficit + 1 for persistent cord compression + 0 for DLC status).17 This clinical scenario is typical for a central cord syndrome. Though surgical treatment may be advisable in this situation, other reports have continued to recommend nonoperative management.17 Last, patients may also present with degenerative spondylolisthesis. This finding can be differentiated from traumatic injuries by the presence of facet joint arthritis or osteophytes, without signs of acute fracture or translational injury, and should be scored as 0 for morphology.2
Neurologic Status
The neurologic status is among the most important determinants of surgical treatment and is also the most important prognostic factor in SCI patients. Patients with American Spine Injury Association (ASIA) Impairment Scale (AIS) grade A (complete injury) receive 2 points.18 Patients with AIS grade B, C, and D (incomplete deficits) receive 3 points. Neurologic impairment is most often defined by motor and sensory examination. However, some patients may have other symptoms of cord dysfunction, such as paresthesias, loss of motor dexterity, or balance impairment.2 These are currently not accounted for by the SLIC system but, depending on the intensity of these symptoms, may need to be considered in the neurologic classification of patients.
After understanding the system nuances, the clinical application can be easily incorporated in daily practice. Studies of reproducibility of the SLIC among surgeons suggest that the system is easily applied and comprehensive.19 20 We applied the SLIC in a retrospective series of patients treated for subaxial cervical spine trauma, determining that the system matched with the proposed treatment in up to 90% of patients treated with conservative or surgical approaches.2 High-quality, prospective evidence validating the SLIC system, however, is lacking.
Treatment
Methylprednisolone for Spinal Cord Injuries
The potential benefits in neurologic recovery with early administration of high doses methylprednisolone in patients with acute closed SCI have been reported by the National Acute Spinal Cord Injuries Studies (NASCIS II, III).21 However, many other authors have pointed out flaws in the studies, questioning the widespread use of steroids in acute SCI.22 23 These concerns include limited clinical benefits, a post hoc analysis, statistical artifacts, and the significance of the potential complications of high doses of corticosteroids use.22 23 Considering these points, methylprednisolone administration in the setting of an acute SCI should be considered when the potential risks are balanced with the potentially limited benefits of its use.
Management in the Emergency Room
During clinical stabilization, following standard trauma protocols, patients should be maintained in supine position with a rigid cervical collar and lateral immobilization.1 Radiologic screening should be based on CT scan with multiplanar reconstructions.24 After a thorough examination, patients without pain, neurologic deficit, and radiologic abnormalities can have their cervical collars removed. MR can be performed as a complementary radiologic study, by surgeon discretion, but it may have its greatest impact in patients with cervical burst fractures, with neurologic deficits, or with uncertain injuries on CT scan.
In patients with a cervical dislocation, early closed reduction with traction is an important part of treatment.3 Reduction can simplify surgical treatment as well as provide prompt decompression of the neural tissues in neurologically impaired patients. Cervical traction for close reduction can be safely performed in the emergency department or after patient admission to a definitive hospital bed or intensive care unit. Up to 70% of the cervical fractures can be realigned with traction.3 25 Usually the weight necessary is ∼5 pounds (2.5 kg) per level of injury and can be performed in neutral, flexion, or extension position, according to injury characteristic.3 Close clinical and radiologic observations are mandatory in patients undergoing cervical traction until performing definitive surgical stabilization. Weight can be increased rapidly as allowed by a reliable, new neurologic examination and new cervical radiographs. An earlier reduction may potentially improve ultimate neurologic function and should always be attempted.
The main objective of traction is to obtain and maintain closed reduction on lateral cervical radiographs. During reduction, surgeons should be aware of the risk of over distraction as well as the potential for neurologic worsening. Regarding Gardner-Wells tong application, the patient is placed in a neutral supine position. After local asepsis, local and periosteal infiltration with anesthetic is performed. The pins are placed below the greatest diameter of the skull. The surgeon must avoid entering the temporal muscle and artery, as such the common site is generally 1 cm above the pinna and 1 cm posterior to the external auditory meatus. The pins can be placed asymmetrically (slightly anterior or posterior) to influence flexion or extension according to injury morphology/dislocation. As an example, cervical flexion (tongs placed slightly posterior) can help achieve reduction of locked facet joints. In unilateral locked facet joint, some flexion and rotation away from the luxation side can help achieve reduction. In addition to pin placement, in the setting of a reliable examination, the surgeon can also obtain a reduction by flexing and/or rotating the cervical spine to further “unlock” dislocated facet joints by recreating the traumatic deformity. Once a facet reduction is obtained, cervical extension and lower-weight in-line traction (15 to 20 pounds) can be utilized to maintain the reduction.
Patients in whom a reliable neurologic exam cannot be obtained should not undergo closed reduction. This includes obtunded patients, inebriated patients, sedated or intubated patients, and patients who cannot comply with a neurologic examination. Traction is also contraindicated in patients with rostral injuries, especially distractive ones, such as atlantoaxial or occipitocervical dislocations.25 26 An MR prior to closed reduction is recommended to identify a traumatic cervical disk herniation. However, routine pre-reduction MR can delay spinal decompression and increase hospital costs.26 27 As such, it commonly obtained prior to reduction only in select patients, most notably surgical patients who are unable to undergo a safe, closed reduction.
Nonsurgical Treatment
Injuries with SLIC score of less than 3, and sometimes 4, points are treated nonsurgically. As they are generally stable lesions, the use of a cervical orthosis is not mandatory. However, a cervical collar may help in healing of soft tissue injuries and in the management of acute pain. Though no evidence-based guidelines are available, we have generally prescribed a rigid cervical collar for 6 to 12 weeks when stable fractures are present, performing clinical and radiologic follow-up. Soft collars may be used in mild cervical trauma without evident bone fractures. Another potential advantage of prescribing an orthosis is to emphasize, to the patient and those around them, the importance of activity restrictions and risk-behavior modifications.
Surgical Treatment
Timing for Surgery in Patients with Neurologic Deficits
Once surgical treatment is chosen, the benefits of early decompression have been well demonstrated. The Surgical Timing in Acute Spinal Cord Injury Study (STASCIS) was a multicenter international prospective cohort study with patients aged from 16 to 80 with a cervical SCI.28 The primary outcome was neurologic status at 6-month follow-up. Early surgery (<24 hours after injury) was performed in 182 patients (mean of 14.2 ± 5.2 hours), and 131 patients underwent late surgery (48.3 ± 29.3 hours). Follow-up was available in 222 patients at 6 months after injury. In 19.8% of the patients in the early group, there was a ≥ 2 grade improvement in ASIA Impairment Scale compared with a 8.8% rate of improvement in the late decompression group (odds ratio = 2.57, 95% confidence interval: 1.11 to5.97). There were no differences regarding complications when comparing the two groups, attesting that early decompression poses no additional risks. The authors concluded that early decompression was safe and associated with improvement in neurologic outcome in cervical spine injuries.28
Given these recent clinical data and the breadth of preclinical animal data, we emphasize that neurologic decompression should be performed as soon as possible considering the availability of sufficient human and structural resources as well as the patient's clinical conditions.
Anterior versus Posterior Approaches
In addition to the timing of surgical treatment, the best approach (anterior, posterior, combined) is another critical decision point. As a general rule, the approach is chosen based on the needs of cervical decompression, reconstruction, and stabilization. Anterior approaches have the advantages of supine position, minor surgical trauma, and direct anterior decompression of the neural elements, removing ventral compressive structures such as disk and bone.3 Anterior stabilization can be also used successfully in select posterior injuries.29 Posterior approaches, based on rigid fixation techniques with lateral mass or pedicle screws, are a good alternative for distraction and translation/rotational injuries, as reduction forces can be directly applied to realign the spine.
Surgeons should pay attention to the presence of a significant anterior disk herniation associated with facet dislocations. Reduction in this setting, without a reliable neurologic examination, can lead to neurologic deterioration due to worsening of the anterior cord compression.30 Closed reduction in an awake patient prior to doing posterior stabilization is safer than intraoperative direct posterior reduction in the presence of anterior compression, avoiding posterior migration of the disk against the spinal cord. An MR is recommended to access the presence of an important disk herniation prior to open surgical reduction to avoid clinical worsening.
Brodke et al evaluated the results of 52 patients with reduced unstable cervical spine injuries who were randomized for anterior versus posterior stabilization and fusion.31 Patients who required reduction and decompression were not included in the study. They reported no significant differences in neurologic recovery, fusion rates, or long-term complaints with regards to the approach chosen. Similarly, Kwon et al performed a prospective randomized study comparing anterior versus posterior stabilization for unilateral facet injuries in 42 patients.32 The authors concluded that even though anterior approaches had a lower rate of wound infections, less postoperative pain, and a higher fusion rate, they also had a higher risk of postoperative swallowing difficulty. There were no reported differences in patient outcome measures. The authors conclude that either anterior or posterior fixation approaches are valid and safe techniques to treat unilateral facet injuries.
Surgical Considerations in Specific Injuries
By considering common clinical scenarios, we can discuss general principals of the evaluation and treatment of subaxial cervical spine injuries. However, it should be emphasized that treatment should ultimately be individualized according to injury characteristics and based on surgeon experience and preference.
Vertebral Burst Fractures
Severe anterior vertebral body fractures have been assigned different nomenclature in the literature, such as quadrangular fractures, teardrop injuries, and burst fractures and dislocations.33 34 Most of the time, these more severe injury patterns have an associated DLC injury and neurologic deficits, reaching an SLIC score that recommends surgical treatment. Anterior cervical corpectomy with graft and plating is generally recommended, restoring anterior column support and providing access for direct neurologic decompression.17 When necessary, especially in cases with disruption of the posterior elements, a combined approach (anterior-posterior) can provide both direct anterior decompression and circumferential stabilization.17
Central Cord Syndrome
Most of these patients have an SLIC score of 4 points: 0 for morphology + 0 for DLC status + 4 for neurologic status (3 for incomplete injury with an extra 1 point for persistent cord compression). Some of these patients may also have an associated injury to the DLC including disk protrusions (+1 point) and extruded traumatic disk herniation (+2 points).2 17 Retrospective data suggest a benefit to surgical treatment in patients with central cord syndrome. Stevens et al reported the results of a series of 126 patients treated with central cord syndrome.35 Sixty-seven patients were surgically treated whereas 59 were managed nonoperatively. The study divided surgically treated patients in three subgroups: early surgery (<24 hours after injury), late surgery (>24 hours but in the same hospital admission), and delayed surgery (after primary hospital discharge). From the 67 patients surgically treated, 16 received early surgery, 34 received late surgery during the hospital admission (mean of 6.4 days), and 17 had late surgery after first hospital admission (mean of 137 days after injury). With a mean follow-up of 32 months, an improvement in Frankel grade was seen in the overall surgical group compared with the nonsurgically treated group. However, there were no differences regarding the three surgery subgroups. Their findings suggest that surgical intervention should be recommended in central cord syndrome, even though prospective comparative studies are still needed.
As central cord syndrome generally occurs in patients with previous cervical spondylosis, treatment should be based on the number of involved levels and the source of compression. Patients with kyphotic alignment should be preferentially treated by an anterior approach or an anterior followed by a posterior approach, whereas patients with lordotic sagittal alignment and multilevel compression can be treated by laminoplasty or laminectomy and fusion.17
Unilateral/Bilateral Facet Injuries
These injuries can be surgically treated using an anterior or a posterior stabilization with similar outcomes.17 32 A high rate of minor and asymptomatic herniated disks can be found in up to half of the patients with facet subluxation, but after reduction, stabilization can be performed by an anterior or a posterior approach, despite the presence of a disk herniation.36 37 With regards to unilateral facet joint injuries, as mentioned previously, there is good evidence suggesting similar outcomes comparing anterior and posterior approaches.32
Anterior reduction of facet dislocation is feasible in many cases. After complete disk and posterior ligament resection, pins can be inserted from 10 to 20 degrees of convergence. Distractor placement results in local kyphosis, unlocking the posterior facet joints with additional posterior force applied in the rostral body.38 In unilateral dislocation, the pins are placed in a similar fashion but with additional coronal separation of 10 to 20 degrees to allow for rotation. Distractor placement results in kyphosis (similarly to bilateral dislocation) as well as derotation; a manual posterior force is applied in the rostral body, resulting in reestablishment of facet joint congruence.38 Continuous intraoperative traction and the use of a Cobb elevator in the disk can be further utilized to disengage dislocated facets and facilitate obtaining a reduction. These maneuvers also provide distraction, allowing for the removal of an anterior disk herniation. Most of the times, anterior cervical diskectomy and interbody fusion is sufficient to remove the disk fragment present into the canal. If not, the disk cannot be removed; for example, in large retrovertebral herniations, the procedure can be converted to an anterior corpectomy.
In cases of an anterior approach and incomplete reduction, a combined approach should be performed, with open posterior reduction. Locked facet joints not reducible by traction or anterior open approaches should be treated with a posterior direct approach. Patients with severe disk collapse treated by a posterior approach can develop segmental collapse and important kyphosis, even though its relationship with clinical outcome remains uncertain.18 39
Severe Fracture Dislocation/Subluxation
Although surgical decision making can be straightforward, these injuries are among the most challenging to treat. Combined approaches are generally required for spinal canal decompression, anterior column height restoration, and reconstruction of the posterior tension band. Alternatively, severe distraction injuries can be seen in patients with ankylosing spondylitis, diffuse idiopathic skeletal hyperostosis (DISH), or severe osteoarthritis. These represent unstable injury patterns with a highly reported rate of neurologic injury and/or progressive decline. In this context, extended posterior fixation is advised as the disease processes create significant spinal stiffness and long lever arms on the fusion construct.40
Conclusions
The current state of subaxial cervical spine trauma is one of great progress. Rapid emergency evaluation and treatment of the injured patient allows for early identification of cervical injuries. The SLIC system represents an improvement in the classification of injured patients, and early surgical decompression has been shown to improve neurologic outcome in patients with spinal cord injuries. However, many questions remain unanswered. The role of MR in the assessment of acute trauma remains uncertain. Current classification systems require prospective validation and may require further revisions. Last, although we have moved toward standardized care of the traumatized patient, we need to continue to account for the individual patient, surgeon, and hospital circumstances that effect decision making and care.
Footnotes
Disclosures None
References
- 1.Torretti J A, Sengupta D K. Cervical spine trauma. Indian J Orthop. 2007;41(4):255–267. doi: 10.4103/0019-5413.36985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Joaquim A F, Lawrence B, Daubs M, Brodke D, Patel A A. Evaluation of the subaxial injury classification system. J Craniovertebr Junction Spine. 2011;2(2):67–72. doi: 10.4103/0974-8237.100057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Aebi M. Surgical treatment of upper, middle and lower cervical injuries and non-unions by anterior procedures. Eur Spine J. 2010;19(1) 01:S33–S39. doi: 10.1007/s00586-009-1120-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Joaquim A F, Patel A P. Occipito-cervical trauma: evaluation, classification and treatment. Contemporary Spine Surgery. 2010;11(4):1–5. [Google Scholar]
- 5.Joaquim A F, Patel A P. Occipito-cervical trauma: evaluation, classification and treatment. Contemporary Neurosurgery. 2010;32(12):1–6. [Google Scholar]
- 6.Joaquim A F, Patel A P. C1 and C2 spine trauma: evaluation, classification and treatment. Contemporary Spine Surgery. 2010;11(3):1–7. [Google Scholar]
- 7.Sanchez B, Waxman K, Jones T, Conner S, Chung R, Becerra S. Cervical spine clearance in blunt trauma: evaluation of a computed tomography-based protocol. J Trauma. 2005;59(1):179–183. doi: 10.1097/01.ta.0000171449.94650.81. [DOI] [PubMed] [Google Scholar]
- 8.Antevil J L, Sise M J, Sack D I, Kidder B, Hopper A, Brown C V. Spiral computed tomography for the initial evaluation of spine trauma: a new standard of care? J Trauma. 2006;61(2):382–387. doi: 10.1097/01.ta.0000226154.38852.e6. [DOI] [PubMed] [Google Scholar]
- 9.Schenarts P J Diaz J Kaiser C Carrillo Y Eddy V Morris J A Jr Prospective comparison of admission computed tomographic scan and plain films of the upper cervical spine in trauma patients with altered mental status J Trauma 2001514663–668., discussion 668–669 [DOI] [PubMed] [Google Scholar]
- 10.Menaker J Philp A Boswell S Scalea T M Computed tomography alone for cervical spine clearance in the unreliable patient—are we there yet? J Trauma 2008644898–903., discussion 903–904 [DOI] [PubMed] [Google Scholar]
- 11.Rihn J A, Fisher C, Harrop J, Morrison W, Yang N, Vaccaro A R. Assessment of the posterior ligamentous complex following acute cervical spine trauma. J Bone Joint Surg Am. 2010;92(3):583–589. doi: 10.2106/JBJS.H.01596. [DOI] [PubMed] [Google Scholar]
- 12.Vaccaro A R, Hulbert R J, Patel A A. et al. The subaxial cervical spine injury classification system: a novel approach to recognize the importance of morphology, neurology, and integrity of the disco-ligamentous complex. Spine. 2007;32(21):2365–2374. doi: 10.1097/BRS.0b013e3181557b92. [DOI] [PubMed] [Google Scholar]
- 13.Kaiser M L, Whealon M D, Barrios C, Kong A P, Lekawa M E, Dolich M O. The current role of magnetic resonance imaging for diagnosing cervical spine injury in blunt trauma patients with negative computed tomography scan. Am Surg. 2012;78(10):1156–1160. doi: 10.1177/000313481207801032. [DOI] [PubMed] [Google Scholar]
- 14.Holdsworth F. Fractures, dislocations, and fracture-dislocations of the spine. J Bone Joint Surg Am. 1970;52(8):1534–1551. [PubMed] [Google Scholar]
- 15.Allen B L Jr, Ferguson R L, Lehmann T R, O'Brien R P. A mechanistic classification of closed, indirect fractures and dislocations of the lower cervical spine. Spine. 1982;7(1):1–27. doi: 10.1097/00007632-198200710-00001. [DOI] [PubMed] [Google Scholar]
- 16.Magerl F, Aebi M, Gertzbein S D, Harms J, Nazarian S. A comprehensive classification of thoracic and lumbar injuries. Eur Spine J. 1994;3(4):184–201. doi: 10.1007/BF02221591. [DOI] [PubMed] [Google Scholar]
- 17.Dvorak M F, Fisher C G, Fehlings M G. et al. The surgical approach to subaxial cervical spine injuries: an evidence-based algorithm based on the SLIC classification system. Spine. 2007;32(23):2620–2629. doi: 10.1097/BRS.0b013e318158ce16. [DOI] [PubMed] [Google Scholar]
- 18.Marino R J, Barros T, Biering-Sorensen F. et al. International standards for neurological classification of spinal cord injury. J Spinal Cord Med. 2003;26 01:50–56. doi: 10.1080/10790268.2003.11754575. [DOI] [PubMed] [Google Scholar]
- 19.Lee W J, Yoon S H, Kim Y J, Kim J Y, Park H C, Park C O. Interobserver and intraobserver reliability of sub-axial injury classification and severity scale between radiologist, resident and spine surgeon. J Korean Neurosurg Soc. 2012;52(3):200–203. doi: 10.3340/jkns.2012.52.3.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Whang P G, Patel A A, Vaccaro A R. The development and evaluation of the subaxial injury classification scoring system for cervical spine trauma. Clin Orthop Relat Res. 2011;469(3):723–731. doi: 10.1007/s11999-010-1576-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bracken M B, Shepard M J, Collins W F. et al. A randomized, controlled trial of methylprednisolone or naloxone in the treatment of acute spinal-cord injury. Results of the Second National Acute Spinal Cord Injury Study. N Engl J Med. 1990;322(20):1405–1411. doi: 10.1056/NEJM199005173222001. [DOI] [PubMed] [Google Scholar]
- 22.Nesathurai S. Steroids and spinal cord injury: revisiting the NASCIS 2 and NASCIS 3 trials. J Trauma. 1998;45(6):1088–1093. doi: 10.1097/00005373-199812000-00021. [DOI] [PubMed] [Google Scholar]
- 23.Botelho R V, Daniel J W, Boulosa J L. et al. [Effectiveness of methylprednisolone in the acute phase of spinal cord injuries—a systematic review of randomized controlled trials] Rev Assoc Med Bras. 2009;55(6):729–737. doi: 10.1590/s0104-42302009000600019. [DOI] [PubMed] [Google Scholar]
- 24.Mower W R Hoffman J R Pollack C V Jr Zucker M I Browne B J Wolfson A B; NEXUS Group. Use of plain radiography to screen for cervical spine injuries Ann Emerg Med 20013811–7. [DOI] [PubMed] [Google Scholar]
- 25.Hadley M N Guidelines for management of acute cervical injuries Neurosurgery 200250(3, Suppl):S1. [DOI] [PubMed] [Google Scholar]
- 26.Farmer J, Vaccaro A, Albert T J, Malone S, Balderston R A, Cotler J M. Neurologic deterioration after cervical spinal cord injury. J Spinal Disord. 1998;11(3):192–196. [PubMed] [Google Scholar]
- 27.Rosenfeld J F, Vaccaro A R, Albert T J, Klein G R, Cotler J M. The benefits of early decompression in cervical spinal cord injury. Am J Orthop. 1998;27(1):23–28. [PubMed] [Google Scholar]
- 28.Fehlings M G, Vaccaro A, Wilson J R. et al. Early versus delayed decompression for traumatic cervical spinal cord injury: results of the Surgical Timing in Acute Spinal Cord Injury Study (STASCIS) PLoS ONE. 2012;7(2):e32037. doi: 10.1371/journal.pone.0032037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Woodworth R S, Molinari W J, Brandenstein D, Gruhn W, Molinari R W. Anterior cervical discectomy and fusion with structural allograft and plates for the treatment of unstable posterior cervical spine injuries. J Neurosurg Spine. 2009;10(2):93–101. doi: 10.3171/2008.11.SPI08615. [DOI] [PubMed] [Google Scholar]
- 30.Eismont F J, Arena M J, Green B A. Extrusion of an intervertebral disc associated with traumatic subluxation or dislocation of cervical facets. Case report. J Bone Joint Surg Am. 1991;73(10):1555–1560. [PubMed] [Google Scholar]
- 31.Brodke D S, Anderson P A, Newell D W, Grady M S, Chapman J R. Comparison of anterior and posterior approaches in cervical spinal cord injuries. J Spinal Disord Tech. 2003;16(3):229–235. doi: 10.1097/00024720-200306000-00001. [DOI] [PubMed] [Google Scholar]
- 32.Kwon B K, Fisher C G, Boyd M C. et al. A prospective randomized controlled trial of anterior compared with posterior stabilization for unilateral facet injuries of the cervical spine. J Neurosurg Spine. 2007;7(1):1–12. doi: 10.3171/SPI-07/07/001. [DOI] [PubMed] [Google Scholar]
- 33.Ianuzzi A, Zambrano I, Tataria J. et al. Biomechanical evaluation of surgical constructs for stabilization of cervical teardrop fractures. Spine J. 2006;6(5):514–523. doi: 10.1016/j.spinee.2005.12.001. [DOI] [PubMed] [Google Scholar]
- 34.Fisher C G, Dvorak M F, Leith J, Wing P C. Comparison of outcomes for unstable lower cervical flexion teardrop fractures managed with halo thoracic vest versus anterior corpectomy and plating. Spine. 2002;27(2):160–166. doi: 10.1097/00007632-200201150-00008. [DOI] [PubMed] [Google Scholar]
- 35.Stevens E A, Marsh R, Wilson J A, Sweasey T A, Branch C L Jr, Powers A K. A review of surgical intervention in the setting of traumatic central cord syndrome. Spine J. 2010;10(10):874–880. doi: 10.1016/j.spinee.2010.07.388. [DOI] [PubMed] [Google Scholar]
- 36.Eismont F J, Arena M J, Green B A. Extrusion of an intervertebral disc associated with traumatic subluxation or dislocation of cervical facets. Case report. J Bone Joint Surg Am. 1991;73(10):1555–1560. [PubMed] [Google Scholar]
- 37.Grant G A Mirza S K Chapman J R et al. Risk of early closed reduction in cervical spine subluxation injuries J Neurosurg 199990(1, Suppl):13–18. [DOI] [PubMed] [Google Scholar]
- 38.Kim S Sebastian C T Nathan D J Park J Kim D. In: Kim D Ludwig S C Vaccaro A V Chang J, eds. Atlas of Spine Trauma: Adult and Pediatric Philadelphia, PA: Saunders; 2008135–150. [Google Scholar]
- 39.Lifeso R M, Colucci M A. Anterior fusion for rotationally unstable cervical spine fractures. Spine. 2000;25(16):2028–2034. doi: 10.1097/00007632-200008150-00005. [DOI] [PubMed] [Google Scholar]
- 40.Einsiedel T, Schmelz A, Arand M. et al. Injuries of the cervical spine in patients with ankylosing spondylitis: experience at two trauma centers. J Neurosurg Spine. 2006;5(1):33–45. doi: 10.3171/spi.2006.5.1.33. [DOI] [PubMed] [Google Scholar]


