Abstract
Objectives
Hip fractures are common, morbid, and costly health events that threaten the independence and function of older patients. The purpose of this systematic review and meta-analysis was to determine if ortho-geriatric collaboration models improve outcomes.
Data Sources
Articles in English and Spanish languages were searched in electronic databases including MEDLINE, CINAHL, EMBASE, and the Cochrane Registry from 1992 to 2012.
Study Selection
Studies were included if they described an inpatient multidisciplinary approach to hip fracture management involving an orthopedic surgeon and a geriatrician. Studies were grouped into three categories: routine geriatric consultation, geriatric ward with orthopedic consultation, and shared care. After independent review of 1,480 citations by two authors, 18 studies (9,094 patients) were identified as meeting the inclusion criteria.
Data Extraction
In-hospital mortality, length of stay, and long-term mortality outcomes were collected.
Data Synthesis
A random effects model meta-analysis determined whether the ortho-geriatric collaboration was associated with improved outcomes. The overall meta-analysis found ortho-geriatric collaboration was associated with a significant reduction of in-hospital mortality (RR 0.60, 95%CI 0.43, 0.84) and long-term mortality (RR 0.83, 95%CI 0.74, 0.94). Length of stay (SMD −0.25, 95%CI −0.44, −0.05) was significantly reduced, particularly in the shared care model (SMD −0.61, 95%CI −0.95, −0.28), but heterogeneity limited this interpretation. Other variables such as time to surgery, delirium, and functional status were measured infrequently.
Conclusions
This meta-analysis supports ortho-geriatric collaboration to improve mortality after hip repair. Further study is needed to determine the best model of ortho-geriatric collaboration, and if these partnerships improve functional outcomes.
Keywords: Hip fracture, Geriatrics, Orthopedic surgery, Aged, Mortality, Meta-analysis
Introduction
Hip fractures are a serious and common consequence of orthopedic trauma in elderly patients. Worldwide hip fracture rates are expected to increase to approximately 21 million per year by 2050.1 In the United States, the incidence of hip fractures is 309,500 per year.2 Due to the growing elderly population, this number is projected to increase to over 500,000 per year by 2040.3 Healthcare system adaptations are necessary to accommodate such a large number of patients. Hip fracture prognosis is quite poor, with one-year mortality rates estimated to range from 20% to 30%.4,5 Among those patients who were independent prior to fracture, one year after hip fracture, 25% remained in nursing homes, and 60% required assistance in one or more activities of daily living.6,7 With such critical consequences, much research is being conducted to improve these outcomes.
Older adults are typically high-risk candidates for surgery due to several factors. Many are afflicted with serious co-morbidities. A large proportion has pre-existing functional deficits that not only contribute to sustaining a fall, but also limit recovery after surgery. Homeostenosis, a decreased ability to compensate and maintain homeostasis when the body is stressed, might contribute to complications that can arise when an elderly patient undergoes surgery. Some complications are specific to older patients, and can result in geriatric syndromes associated with poor survival.8 Involvement of geriatricians may improve care of the older, complex patients with hip fracture.
Geriatrics medicine is the knowledge base and clinical skills needed to improve the health, functioning, and well-being of older persons.1 In the decline in physiology and function associated with age, a critical event, like a hip fracture, plays a major role in the future trajectory of functional levels.2, 3 Importantly, geriatric care during the critical event is aimed, not only at the acute medical treatment, but at restoring function after the event. Recently there has been increased interest in collaboration between orthopedic surgeons and geriatricians. Hospitals and health systems are implementing ortho-geriatric care to improve patient outcomes. Recent reviews have described several models of care.9–11 This systematic review and meta-analysis was performed to determine if ortho-geriatric models improve patient outcomes, and to identify if one model in particular is associated with improved outcomes. It was hypothesized that the increase in these programs would demonstrate a net benefit for patients in regards to length of stay (LOS), mortality, and cost.
Methods
Literature Search
To identify eligible studies for inclusion, a systematic search was performed of the following databases: MEDLINE, CINAHL, EMBASE, and the Cochrane Central Register of Controlled Trials. The search keywords were adapted from the literature review by Kammerlander et al.9 The searched terms were: (“hip fracture” or “femoral fracture” or “femur fracture”) AND (“geriatric” or “multidisciplinary” or “comanagement” or “co-management” or “team approach” or “protocol driven” or “integrated care”). Additionally, the terms “orthogeriatric” and “ortho-geriatric” were searched independently. Review article bibliographies were scanned to find pertinent studies that were not identified using the database search. The search included articles between January 1, 1992 and July 1, 2012.
Inclusion/Exclusion Criteria
Abstracts within the parameters of the inclusion and exclusion criteria were selected for full text review. Included studies described a multidisciplinary approach to inpatient hip fracture management involving an orthopedic surgeon and a geriatrician. Studies of intertrochanteric, subtrochanteric, or femoral neck fractures were included. A control or standard care group, was required and defined as an ‘as needed’ geriatric or medicine consult at the request of the surgeon. Additionally, included studies reported at least one of the target outcomes. The multidisciplinary approach included an orthopedic surgeon and a geriatrician. The studies also had to focus on inpatient patient care rather than rehabilitation or post-discharge care.
Studies were excluded if they: were published in a language other than English or Spanish; did not present results of a control group; were published as an abstract or letter; or were published more than 20 years prior to the search period. Any studies focusing on rehabilitation, post-discharge, not including a geriatrician, or examining other fractures in addition to hip fractures were also excluded. The 20-year limit was selected because of the secular change in medical practice. In the case of multiple manuscripts derived from the same data, the results of the most recent manuscript were utilized. However, if other outcomes of interest were published in different manuscripts, we included those findings.
Study Selection
Article titles and abstracts were reviewed by authors KG and HJ to determine if they met the inclusion criteria. Articles were included for full text review based on the abstract, or if it was not discernible from the abstract, full-text articles were reviewed to determine inclusion. Two primary reviewers (KG, HJ) independently evaluated each full text article for inclusion. Any disagreements were discussed between the reviewers, and as necessary with input from a third reviewer (JR), in order to resolve differences.
Methodological Quality Assessment
Studies were assessed for quality based on the type of study, the matching of intervention and control group, and the detail of intervention that was described. Using the criteria of the United States Preventative Services Task Force (USPSTF),12 studies were graded either as good, fair, or poor.
Ortho-Geriatric Models
Three categories (models) of Ortho-geriatric interventions were identified to address a lack of consistency between the interventions. This categorization was also used to explain heterogeneity and bias in the meta-analyses.
Model 1: Routine Geriatric Consultation - Care that takes place within an orthopedic ward with consistent geriatrician consultation on older patients. In this model, the geriatrician is a consultant and the article does not describe integration and shared responsibility.
Model 2: Geriatric Ward - Care within a geriatric ward with the orthopedic surgeon acting as a consultant and responsibility for the care is with the geriatrician.
Model 3: Shared Care - An integrated care model where the patient is within an orthopedic ward, but both the orthopedic surgeon and geriatrician share responsibility for the care of the patient. Articles selected with this model describe the geriatrician as an integral part of the orthopedic team with team involvement.
Data and Statistical Analysis
Study descriptors (type, size, comparison), patient characteristics (age, gender, function), and outcome measures (length of stay, time to surgery, in-hospital and one-year mortality rate, complications) were sought from each study. Long-term mortality was defined as mortality from six months to one year, as reported by the studies. In general, continuous variables were recorded as mean and standard deviation. For studies that reported median and interquartile range, mean and 95% confidence interval, or mean without standard deviation, the guidelines of the Cochrane Handbook were followed.13 For this analysis, the variable was assumed to be normal and was converted to mean and standard deviation or imputed according to published guidelines.13
Data was pooled using a random effects model meta-analysis to manage any heterogeneity that may have been introduced by the varying conditions of the included studies. A minimum of three studies was required for meta-analysis. Heterogeneity was quantified with the I2 and significance was determined using Chi-square. To assess for publication bias, funnel plots were visually examined for asymmetry, and asymmetry was statistically analyzed using the method of Peter for mortality outcomes, and Egger for continuous outcomes.14 Statistical analysis was performed with STATA 11.0 (STATA Inc, College Station, TX).
Results
The preliminary search resulted in 1,729 citations, of which 249 were removed as duplicates. After abstract review, 93 articles were identified for full text review (Figure 1). According to the exclusion criteria, 75 studies were eliminated because they were: unrelated to the topic or there was no geriatrician involvement (49), published as a letter (11), repeat publications (10), lacking control groups (3), and including other fractures (2). After completing this process 18 studies met the inclusion criteria.
Figure 1. PRIMSA for the systematic review.
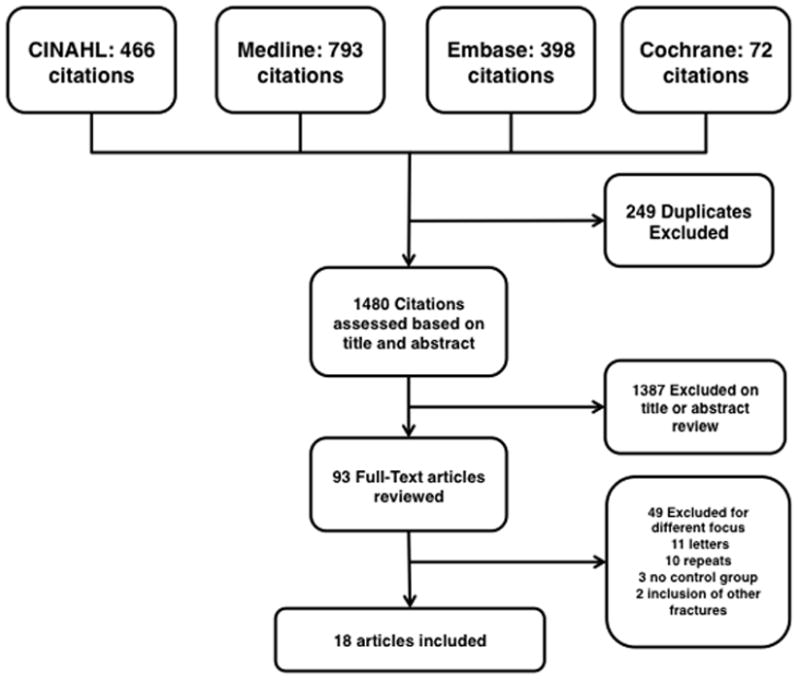
From 1480 citations, 18 articles that met the inclusion criteria were identified. The method of ortho-geriatric interaction was used to group the studies.
The studies are grouped by model and summarized in Table 1. Overall, eight studies were prospective randomized,15–22 four were prospective cohort with retrospective controls,23–26 and six were retrospective chart reviews.27–32 All studies were either good or fair quality. Table 2 shows results from the meta-analysis. Figures 2 and 3 display overall meta-analysis results for inhospital and long-term mortality outcomes.
Table 1.
Included Studies: Model of Care and Reported Outcomes
| Model | Author Year | Study Design | Quality | n (i) | n (c) | Age (SD) (i) | Age (SD) (c) | % In- hospital Mortality (i) | % In- hospital Mortality (c) | % Long- Term Mortality (i) | % Long- Term Morality (c) | Length of Stay (SD) (i) | Length of Stay (SD) (c) | Time To Surgery (SD) (i) | Time To Surgery (SD) (c) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Deschodt13, 31 (2012) | CT | G | 94 | 77 | 80.4 (7) | 81.1 (7.2) | 21.3 | 22.1 | 11.1 (5.1) | 12.4 (8.5) | ||||
| 1 | Leung30 (2011) | RCR | F | 278 | 270 | 83 (7.7) | 82.5 (7.7) | 11.5 | 20.4 | 9.3 (4.4)* | 10.8 (5.8) | 1.9 (1.9)* | 2.3 (2) | ||
| 1 | Cogan26 (2010) | RCR | F | 98 | 103 | 75 (n/a) | 82 (n/a) | 8 | 20 | 34 | 45 | 30.3 (n/a) | 23.1 (n/a) | 1.9 (0.9) | 1.9 (1.9) |
| 1 | Fisher22 (2006) | PCRC | F | 447 | 504 | 81.9 (8) | 81.3 (8.2) | 4.7* | 7.7 | 15.9 (14.9) | 16.4 (17.6) | ||||
| 1 | Shyu14 (2008) | PR | G | 80 | 82 | 77.4 (8.2) | 78.9 (7.3) | 16 | 18 | 10.1 (3.7) | 9.7 (5.0) | ||||
| 1 | Khan23 (2002) | PCRC | F | 208 | 537 | 82 (n/a) | 81 (n/a) | 11.1 | 10.4 | 26.9 (n/a) | 26.1 (n/a) | ||||
| 1 | Naglie16 (2002) | PR | G | 141 | 139 | 83.8 (6.9) | 84.6 (7.3) | 5 | 9.4 | 12.1a | 15.2a | 29.2 (22.6) | 20.9 (19)* | 1.3 (1.0) | 1.4 (1.3) |
| 1 | Marcantonio15 (2001) | PR | G | 62 | 64 | 78 (8) | 80 (8) | 5 (2) | 5 (2) | ||||||
| 1 | Swanson18 (1998) | PR | F | 38 | 33 | 78.5 (n/a) | 77.8 (n/a) | 5.2 | 6.1 | 7.9a | 12.2a | 21 (11.3) b* | 32.5 (25)b | 1 (6.0) c | 2 (9.8) c |
| 1 | Antonelli Incalzi21 (1993) | PCRC | F | 287 | 216 | 79.1 (6.7) | 80.2 (6.4) | 8.4* | 18 | 26.2 (14.4)* | 32.9 (30.9) | ||||
| 2 | Adunsky25 (2011) | RCR | F | 847 | 2267 | 82 (6.9)* | 80.8 (8) | 14.8 | 17.3 | 32.1 (19.9) | 25 (31.1)* | 3 (2.9) | 2.9 (6.5)* | ||
| 2 | Miura24 (2009) | PCRC | F | 91 | 72 | 79.9 (11) | 80.5 (10) | 4.6 (1.1)* | 6.1 (2.4) | ||||||
| 2 | Stenvall17 (2007) | PR | G | 102 | 97 | 82.3 (6.6) | 82 (5.9) | 5.9 | 7.2 | 16 | 18 | 30 (18.1)* | 40 (40.6) | ||
| 3 | Gregersen28 (2011) | RCR | F | 233 | 262 | 82.6 (7.8) | 82.1 (7.7) | 8 | 6 | 16a | 15a | 13 (n/a) | 15 (n/a) | 0.9 (0.8) | 0.7 (1) |
| 3 | Gonzalez- Montalvo20 (2010) | PR | G | 101 | 123 | 85.1 (7.1) | 86.8 (6.4) | 12 (3.7)c* | 18 (7.5)c | ||||||
| 3 | Friedman27 (2009) | RCR | F | 193 | 121 | 84.7 (7.8) | 81.6 (8.7) | 1.6 | 2.5 | 4.6 (3.3)* | 8.3 (6.3) | 1.0 (0.7)* | 1.6 (2.7) | ||
| 3 | Vidan19 (2005) | PR | G | 155 | 164 | 81.1 (7.8) | 82.6 (7.4) | 0.6* | 5.5 | 18.9 | 25.3 | 16 (4.5) c | 18 (8.3) c | 3.2 (1.8) | 3.3 (2.2) |
| 3 | Khasraghi29 (2005) | RCR | F | 273 | 237 | 79.9 (7.3) | 80 (7.1) | 5.7 (n/a)* | 8.1 (n/a) | 1.1 (n/a)* | 1.9 (n/a) |
CT controlled trial, PR prospective randomized, PCRC prospective cohort retrospective control, RCR retrospective chart review, G good, F fair, P poor, * sig. dif. between intervention and control, (i) intervention, (c) control, a 12 mo. mortality, b SD approximated from 95% CI, c SD approximated from interquartile range, Model 1 routine geriatric consultation, Model 2 geriatric ward with orthopedic consultation, Model 3 shared care
Table 2.
Meta-analysis results
| In-Hospital Mortality RR [95% CI] I2, p n |
Long term Mortality RR [95% CI] I2, p n |
Length of Stay SMD [95% CI] I2, p n |
Time to Surgery SMD [95% CI] I2, p n |
|
|---|---|---|---|---|
| All Three Models Combined | 0.60 [0.43, 0.84], 28.4%, p = 0.19 n = 9 |
0.83 [0.74, 0.94], 0.0%, p = 0.72 n = 11 |
−0.25 [−0.44, −0.05] * 96.3%, p = 0.00 n = 18 |
−0.10 [−0.22, 0.02], 79.9%, p = 0.00 n = 9 |
| Routine Geriatric Consultation (Model 1) | 0.51 [0.38, 0.69] 0.0%, p = 0.86 n = 5 |
0.78 [0.65, 0.95] 0.0%, p = 0.55 n = 7 |
−0.03 [−0.20, 0.14] 88.4%, p = 0.00 n = 10 |
−0.13 [−0.23, −0.03] 0.0%, p = 0.50 n = 4 |
| Geriatric Ward (Model 2) | N/A n = 1 |
N/A n = 2 |
−0.33, [−1.06, 0.41 97.7%, p = 0.00 n = 3 |
N/A n = 1 |
| Shared Care (Model 3) | 0.61 [0.16, 2.28] 64.3%, p = 0.06 n = 3 |
N/A n = 2 |
−0.61 [−0.95, −0.28] 93.9%, p = 0.00 n = 5 |
−0.15 [−0.44, 0.15]* 89.8%, p = 0.00 n = 4 |
n number of studies included in analysis, RR relative risk, SMD standardized mean difference, CI Confidence Interval, I2 test for heterogeneity, p significance of meta-analysis results, * there may be evidence of publication bias in these analyses, Model 1 routine geriatric consultation, Model 2 geriatric ward with orthopedic consultation, Model 3 shared care
Figure 2. Meta-analysis forest plot: in-hospital mortality.
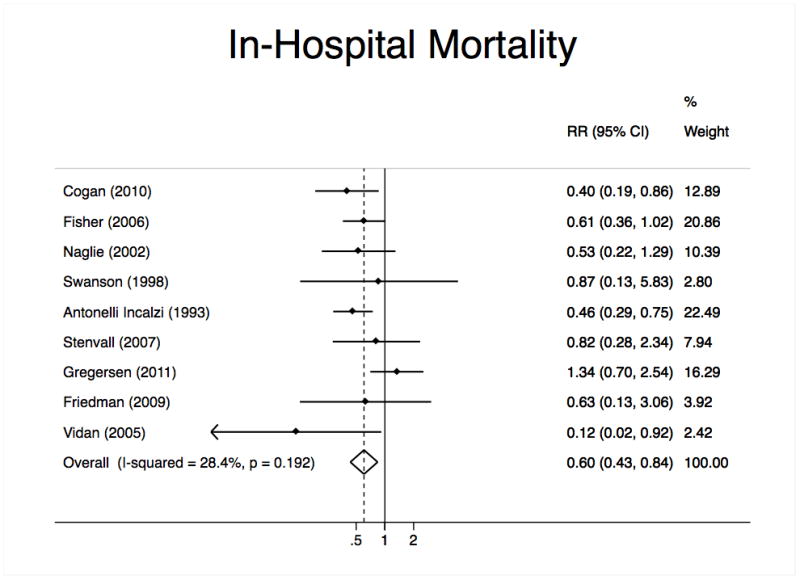
The panel below displays the overall analysis for geriatric interventions on orthopedic wards. This forest plot represents inhospital mortality outcome.
Figure 3. Meta-analysis forest plot: long-term mortality.
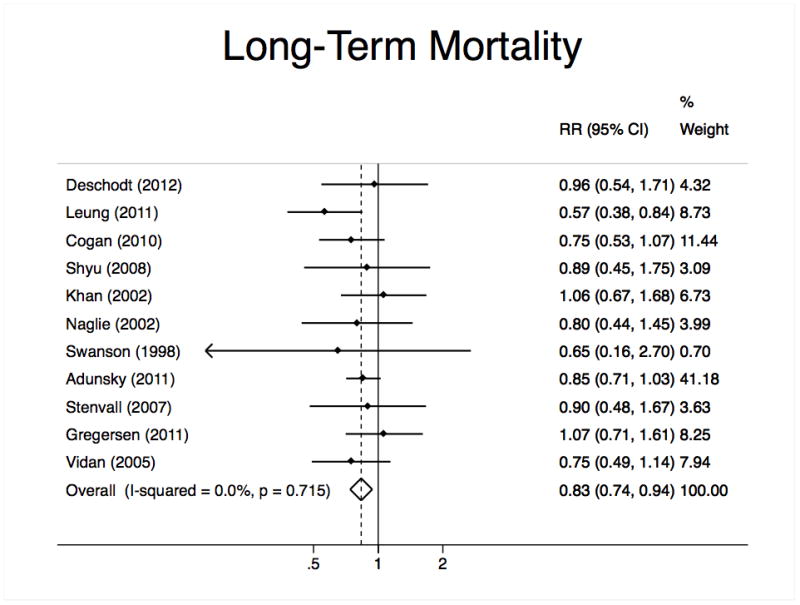
The panel below displays the overall analysis for geriatric interventions on orthopedic wards. This forest plot represents long-term mortality outcome.
Models of Ortho-geriatric Interventions
Routine Geriatric Consultation (Model 1)
Ten studies fell into the category of an orthopedic ward with routine geriatric consultation.15–18,20,23–25,28,32 Five of the studies were prospective controlled trials,16–18,20,33 three had prospective cohorts and retrospective controls,23–25 and two were retrospective chart reviews.28,32 The total number of patients in this group was 1,733 in the intervention, and 2,025 in the control. The mean age of the intervention group was 80.9, and 81.3 years for the control. Meta-analysis results on studies reporting in-hospital mortality showed a significant decrease in long-term mortality, in-hospital mortality, and time to surgery. Heterogeneity was insignificant in these measures. Length of stay was not significantly different, but was confounded by heterogeneity. See Table 2 for details. Three studies reported post-op delirium to be significantly lower in the intervention than the control group.15,17,24 Function was reported by 5 studies,16,18,20,32,33 three of which reported improved function with intervention.16,20,32
Geriatric Ward (Model 2)
Of the three studies that fell in the geriatric ward category: one was a randomized controlled study,19 one a prospective cohort with a retrospective control,26 and one a retrospective chart review.27 The total number of patients in this group was 1,040 in the intervention and 2,436 in the control. The mean age of the intervention group was 82.2 years, and 80.8 years for the control. The low number of published reports for this model reduced the ability to perform meta-analysis. Length of stay exhibited a great deal of heterogeneity, and limited the potential to draw solid conclusions. See Table 2 for further details.
Shared Care (Model 3)
Five studies fell within the category of Shared Care, all including patients with only hip fractures. Two of the studies were randomized controlled trials,21,22 whereas the other three were retrospective chart reviews.29–31 The total number of patients in the pooled intervention group was 955 and 905 in the control. The age mean and standard deviation was 82.3 +/− 2 years in the intervention, and 82.2 +/− 1.7 in the control. In this model, meta-analysis showed evidence for a shortened length of stay in the intervention group, but exhibited a large heterogeneity. The other measures of in-hospital mortality, long-term mortality, and time to surgery showed no statistical difference. Heterogeneity was also significant for in-hospital time to mortality, and moderate in long-term mortality. The three studies that reported post-op complications21,29,31 found a significant reduction in the intervention group. See Table 2 for details.
Discussion
The purpose of this review and meta-analysis was to determine the benefit of ortho-geriatric services. In this work, it was found that the majority of studies examining geriatric interventions have benefit versus standard care, although the exact outcomes differ among studies. As new models of care adapt to the changing healthcare system, it is unclear which model may work best. Geriatric and orthopedic co-management has been the latest trend. However, routine geriatric consultation within an orthopedic ward has the largest number of studies with many of the newer studies describing a variation of this model. In this analysis, most models reduced length of stay, and many reduced point mortality. Yet, much of this evidence needs to be interpreted with caution, as the number of studies is relatively few.
This review and meta-analysis demonstrates that orthopedic geriatric collaboration improves outcomes for older patients. Care models have evolved with changes to the healthcare system. As a result, an older model, such as a dedicated geriatrics ward, has been deemed impractical to implement. Additionally, with the current and projected shortage of geriatricians, few facilities are going to be able to support a full geriatric ward.
These results are consistent with previous reviews that have found improvements with geriatric interventions.9,10 However, within each healthcare system, there is a novel mechanism, and each study described a model that is slightly different from the others. This was addressed by providing careful consideration of the published work prior to assignment in a specific model.
Training in geriatric medicine includes specific training in team building, functional assessment, and aging physiology that is not uniformly included in internal medicine or family practice training. Additionally, market forces have created a self-selective environment where geriatricians are passionate about caring for older patients, albeit in different settings. These same market forces have created a declining number of physicians with certification in geriatrics. Thus, the sustainability of ortho-geriatric collaboration is unclear.
This manuscript raises several elements that should be considered as hospital medicine physicians fill the need for collaboration. First, as needed (PRN) consults should be avoided in favor of consistently scheduled consults, and collaborative models, for older hip fracture patients. Second, team-based care training is a requirement for improving outcomes. Finally, understanding the interplay of age-related physiology, perioperative stress, and functional outcomes is a critical focus of care. While there are insufficient geriatricians to staff ortho-geriatric services, geriatricians should play a key role in the training of professionals who do.
The potential of publication bias (negative studies not being published) playing a role in the findings was also explored. Publication bias can create an illusion that some interventions have a larger impact than actually exists. Of the analyses performed, evidence of publication bias was found in the overall length of stay, and the shared care time to surgery, both of which also had significant heterogeneity. Most studies in this review are retrospective medical record reviews, and are not randomized controlled studies. Due to inherent interests, the studies may opt for control groups and outcomes that demonstrate benefit. Additionally, we attempted to include data from individual studies only once despite multiple publications using that data. Our method for determining this was to contact study authors and match authors, institutions, study dates, and sample sizes. Subjectivity may have resulted in the exclusion of some studies. This was addressed by analyzing for publication bias, and by grading the evidence to provide some structure. Complications and function were not defined identically across studies, creating comparison and summary statistic calculation impracticalities that resulted in their exclusion.
This study examined traditional outcomes related to hip fracture surgery, such as mortality and length of stay. However, relatively few studies reported functional recovery or postoperative quality of life. This reduced reporting may mask the overall impact of hip fracture and recovery, because the population most susceptible to falls and undergoing hip fracture surgery is older and frailer. Thus, there is an inherent bias toward increased mortality. The fundamental purpose in hip fracture repair is to return the patient to the preoperative functional state. Ortho-geriatric collaborations may do this better, but at present it is not measured with sufficient standardization to make a definitive statement.
As healthcare in the United States moves toward more integrated models with alternate payment sources, there is going to be a strong push for increased collaboration. The early evidence of this can be seen in ortho-geriatrics collaborations which appear to be moving from an orthopedics with geriatric consult model to a co-management model. Further collaborative models will also enhance outcomes.
Some of the strengths of this review include a comprehensive search encompassing several databases, and using USPSTF guidelines for evidence grading. The study summarized geriatrics intervention with orthopedic surgeon care of hip fracture patients, and when appropriate, conducted meta-analyses to summarize the impact of similar studies. Finally, this study summarized a comprehensive field as a foundation for future work.
In conclusion, the trend in healthcare has been towards integrated multi-disciplinary care that parallels the geriatric orthopedic co-management model. Clear benefits of geriatric intervention were identified, however, the best model of ortho-geriatric collaboration is dependent on factors that were impossible to measure. In future studies, an increase in standardization of outcomes reporting, with inclusion of non-traditional outcomes such as function, quality of life, and patient and physician satisfaction, are recommended.
Acknowledgments
The authors are indebted to Ms. Elizabeth Archambault for her edits to this manuscript.
Footnotes
Conflicts of Interest and Source of Funding:
Dr. Javedan works for an ortho-geriatric co-management service at Brigham and Women’s Hospital. The authors have no other financial conflicts of interest to declare.
Support for this research was made possible through NIH grant #: 1T35AG038027-02. Dr. Rudolph is supported by a VA Rehabilitation Research and Development Career Development Award.
Presented in part at the American Geriatric Society Meeting, Grapevine, TX, May 3, 2013.
References
- 1.Gullberg B, Johnell O, Kanis JA. World-wide projections for hip fracture. Osteoporosis International. 1997;7:407–13. doi: 10.1007/pl00004148. [DOI] [PubMed] [Google Scholar]
- 2.Butler M, Forte M, Kane RL, et al. AHRQ Publication No 09–E013. Rockville, MD: Agency for Healthcare Research and Quality; Aug, 2009. Treatment of common hip fractures. Evidence Report/Technology Assessment, No. 184. [PubMed] [Google Scholar]
- 3.Zuckerman JD. Hip fracture. N Engl J Med. 1996;334:1519–25. doi: 10.1056/NEJM199606063342307. [DOI] [PubMed] [Google Scholar]
- 4.Leibson CL, Tosteson AN, Gabriel SE, Ransom JE, Melton LJ. Mortality, disability, and nursing home use for persons with and without hip fracture: a population-based study. J Am Geriatr Soc. 2002;50:1644–50. doi: 10.1046/j.1532-5415.2002.50455.x. [DOI] [PubMed] [Google Scholar]
- 5.Keene GS, Parker MJ, Pryor GA. Mortality and morbidity after hip fractures. British Medical Journal. 1993;307:1248–60. doi: 10.1136/bmj.307.6914.1248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Magaziner J, Hawkes W, Hebel JR, et al. Recovery from hip fracture in eight areas of function. J Gerontol A Biol Sci Med Sci. 2000;55:M498–507. doi: 10.1093/gerona/55.9.m498. [DOI] [PubMed] [Google Scholar]
- 7.Cooper C, Cummings S, Lyons A, et al. The crippling consequences of fractures and their impact on quality of life. American Journal of Medicine. 1997;103:12S–9S. doi: 10.1016/s0002-9343(97)90022-x. [DOI] [PubMed] [Google Scholar]
- 8.Marcantonio ER, Flacker JM, Michaels M, Resnick NM. Delirium is independently associated with poor functional recovery after hip fracture. J Am Geriatr Soc. 2000;48:618–24. doi: 10.1111/j.1532-5415.2000.tb04718.x. [DOI] [PubMed] [Google Scholar]
- 9.Kammerlander C, Roth T, Friedman SM, et al. Ortho-geriatric service--a literature review comparing different models. Osteoporos Int. 2010;21:S637–46. doi: 10.1007/s00198-010-1396-x. [DOI] [PubMed] [Google Scholar]
- 10.Giusti A, Barone A, Razzano M, Pizzonia M, Pioli G. Optimal setting and care organization in the management of older adults with hip fracture. European Journal of Physical & Rehabilitation Medicine. 2011;47:281–96. [PubMed] [Google Scholar]
- 11.Liem IS, Kammerlander C, Suhm N, Kates SL, Blauth M. Literature review of outcome parameters used in studies of geriatric fracture centers. Arch Orthop Trauma Surg. 2012;2:2. doi: 10.1007/s00402-012-1594-4. [DOI] [PubMed] [Google Scholar]
- 12.U.S. Preventive Services Task Force Grade Definitions. [Accessed July 13, 2012];USPSTF web site. 2008 May; Available from: http://www.uspreventiveservicestaskforce.org/uspstf/grades.htm.
- 13.Higgins J, Green Se, editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. The Cochrane Collaboration; 2011. [Google Scholar]
- 14.Sterne JAC. Meta-Analysis in Stata: Tests for Publication Bias in Meta-analysis. College Station, Texas: Stata Press; 2009. pp. 138–61. [Google Scholar]
- 15.Deschodt M, Braes T, Flamaing J, et al. Preventing delirium in older adults with recent hip fracture through multidisciplinary geriatric consultation. Journal of the American Geriatrics Society. 2012;60:733–9. doi: 10.1111/j.1532-5415.2012.03899.x. [DOI] [PubMed] [Google Scholar]
- 16.Shyu YL, Liang J, Wu C, et al. Interdisciplinary intervention for hip fracture in older Taiwanese: benefits last for 1 year. Journals of Gerontology Series A: Biological Sciences & Medical Sciences. 2008;63A:92–7. doi: 10.1093/gerona/63.1.92. [DOI] [PubMed] [Google Scholar]
- 17.Marcantonio ER, Flacker JM, Wright RJ, Resnick NM. Reducing delirium after hip fracture: a randomized trial. J Am Geriatr Soc. 2001;49:516–22. doi: 10.1046/j.1532-5415.2001.49108.x. [DOI] [PubMed] [Google Scholar]
- 18.Naglie G, Tansey C, Kirkland JL, et al. Interdisciplinary inpatient care for elderly people with hip fracture: a randomized controlled trial. CMAJ: Canadian Medical Association Journal. 2002;167:25–32. [PMC free article] [PubMed] [Google Scholar]
- 19.Stenvall M, Olofsson B, Nyberg L, Lundstrom M, Gustafson Y. Improved performance in activities of daily living and mobility after a multidisciplinary postoperative rehabilitation in older people with femoral neck fracture: a randomized controlled trial with 1-year follow-up. J Rehabil Med. 2007;39:232–8. doi: 10.2340/16501977-0045. [DOI] [PubMed] [Google Scholar]
- 20.Swanson CE, Day GA, Yelland CE, et al. The management of elderly patients with femoral fractures. A randomised controlled trial of early intervention versus standard care. Med J Aust. 1998;169:515–8. [PubMed] [Google Scholar]
- 21.Vidan M, Serra JA, Moreno C, Riquelme G, Ortiz J. Efficacy of a comprehensive geriatric intervention in older patients hospitalized for hip fracture: a randomized, controlled trial. J Am Geriatr Soc. 2005;53:1476–82. doi: 10.1111/j.1532-5415.2005.53466.x. [DOI] [PubMed] [Google Scholar]
- 22.Gonzalez-Montalvo JI, Alarcon T, Gil-Garay E, Gotor P, Martin-Vega A, Mauleon JL. The orthogeriatric unit for acute patients: a new model of care that improves efficiency in the management of patients with hip fracture. Hip International. 2010;20:229–35. doi: 10.1177/112070001002000214. [DOI] [PubMed] [Google Scholar]
- 23.Antonelli Incalzi R, Gemma A, Capparella O, Bernabei R, Sanguinetti C, Carbonin PU. Continuous geriatric care in orthopedic wards: a valuable alternative to orthogeriatric units. Aging (Milano) 1993;5:207–16. doi: 10.1007/BF03324157. [DOI] [PubMed] [Google Scholar]
- 24.Fisher AA, Davis MW, Rubenach SE, Sivakumaran S, Smith PN, Budge MM. Outcomes for older patients with hip fractures: The impact of orthopedic and geriatric medicine cocare. Journal of Orthopaedic Trauma. 2006;20:172–8. doi: 10.1097/01.bot.0000202220.88855.16. [DOI] [PubMed] [Google Scholar]
- 25.Khan R, Fernandez C, Kashifl F, Shedden R, Diggory P. Combined orthogeriatric care in the management of hip fractures: a prospective study. Ann R Coll Surg Engl. 2002;84:122–4. [PMC free article] [PubMed] [Google Scholar]
- 26.Miura LN, DiPiero AR, Homer LD. Effects of a geriatrician-led hip fracture program: improvements in clinical and economic outcomes. Journal of the American Geriatrics Society. 2009;57:159–67. doi: 10.1111/j.1532-5415.2008.02069.x. [DOI] [PubMed] [Google Scholar]
- 27.Adunsky A, Lerner-Geva L, Blumstein T, Boyko V, Mizrahi E, Arad M. Improved Survival of Hip Fracture Patients Treated Within a Comprehensive Geriatric Hip Fracture Unit, Compared With Standard of Care Treatment. Journal of the American Medical Directors Association. 2011;12:439–44. doi: 10.1016/j.jamda.2010.09.003. [DOI] [PubMed] [Google Scholar]
- 28.Cogan L, Martin AJ, Kelly LA, Duggan J, Hynes D, Power D. An audit of hip fracture services in the Mater Hospital Dublin 2001 compared with 2006. Ir J Med Sci. 2010;179:51–5. doi: 10.1007/s11845-009-0377-6. [DOI] [PubMed] [Google Scholar]
- 29.Friedman SM, Mendelson DA, Bingham KW, Kates SL. Impact of a comanaged Geriatric Fracture Center on short-term hip fracture outcomes. Archives of Internal Medicine. 2009;169:1712–7. doi: 10.1001/archinternmed.2009.321. [DOI] [PubMed] [Google Scholar]
- 30.Gregersen M, Morch MM, Hougaard K, Damsgaard EM. Geriatric intervention in elderly patients with hip fracture in an orthopedic ward. J Inj Violence Res. 2011 doi: 10.5249/jivr.v4i2.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Khasraghi FA, Christmas C, Lee EJ, Mears SC, Wenz JF., Sr Effectiveness of a multidisciplinary team approach to hip fracture management. J Surg Orthop Adv. 2005;14:27–31. [PubMed] [Google Scholar]
- 32.Leung AH, Lam TP, Cheung WH, et al. An orthogeriatric collaborative intervention program for fragility fractures: a retrospective cohort study. Journal of Trauma. 2011;71:1390–4. doi: 10.1097/TA.0b013e31821f7e60. [DOI] [PubMed] [Google Scholar]
- 33.Deschodt M, Braes T, Broos P, et al. Effect of an Inpatient Geriatric Consultation Team on Functional Outcome, Mortality, Institutionalization, and Readmission Rate in Older Adults with Hip Fracture: A Controlled Trial. Journal of the American Geriatrics Society. 2011;59:1299–308. doi: 10.1111/j.1532-5415.2011.03488.x. [DOI] [PubMed] [Google Scholar]


