Abstract
Distal forearm fractures are among the most common fractures during childhood, but it remains unclear whether they predict an increased fracture risk later in life. We studied a population-based cohort of 1776 children ≤18 years of age, from Olmsted County, MN, USA, who had a distal forearm fracture in 1935–1992. Incident fractures occurring at age ≥35 years were identified through review of complete medical records using the linkage system of the Rochester Epidemiology Project. Observed nonpathologic fractures resulting from no more than moderate trauma (fragility fractures) were compared with expected numbers estimated from fracture site–specific incidence rates, based on age, sex, and calendar year, for Olmsted County (standardized incidence ratios [SIR]). In 1086 boys (mean ± SD age; 11 ± 4 years) and 690 girls (10 ± 4 years) followed for 27,292 person-years after the age of 35 years, subsequent fragility fractures were observed in 144 (13%) men and 74 (11%) women. There was an increased risk for future fragility fractures in boys who had a distal forearm fracture (SIR, 1.9; 95% CI, 1.6–2.3) but not girls (SIR, 1.0; 95% CI, 0.8–1.2). Fragility fractures at both major osteoporotic (hip, spine, wrist, and shoulder) sites (SIR, 2.6; 95% CI, 2.1–3.3) and remaining sites (SIR, 1.7; 95% CI, 1.3–2.0) were increased in men, irrespective of age at distal forearm fracture as boys. A distal forearm fracture in boys, but not girls, is associated with an increased risk for fragility fractures as older adults. It is necessary to determine whether the increased fractures observed in men is due to persistent deficits of bone strength, continued high fracture risk activity, or both. Until then, men should be asked about a childhood distal forearm fracture and, if so, warrant further screening and counseling on measures to optimize bone health and prevent fractures.
Keywords: DISTAL FOREARM FRACTURE, CHILDHOOD, FRACTURES, OSTEOPOROSIS, EPIDEMIOLOGY
Introduction
Osteoporosis, with its attendant fractures, is generally considered a geriatric condition, but its origins may well be in childhood.(1) Most adult bone mass is achieved by the end of adolescence(2); therefore, there is growing interest in potential early-life determinants of osteoporosis because negative influences on the development of peak bone mass and structure may have a significant impact on the risk for fragility fractures later in life.
Over 40% of girls and over 50% of boys sustain at least one fracture during childhood and adolescence,(3) with distal forearm fractures being among the most common, accounting for up to one-third of all pediatric fractures.(4) Furthermore, distal forearm fractures in childhood are increasing in incidence,(5,6) particularly among girls.(5) Thus, the role of a childhood distal forearm fracture, in particular, on fracture risk later in life, would have practical clinical applications. Studies have demonstrated lower bone density or weaker bone structure in boys and girls with a distal forearm fracture compared with controls.(7–11) If a distal forearm fracture in childhood is a marker for attainment of lower peak bone mass and strength, it may serve to identify individuals at high risk for fractures later in life. Although a distal forearm fracture in adulthood has been considered a sentinel event for future fractures,(12,13) the influence of a childhood distal forearm fracture on adult fracture risk has not been established.
We therefore sought to determine whether a distal forearm fracture in childhood increases the risk for future fractures in adulthood. Studying a population-based cohort of children and adolescents with an incident distal forearm fracture for whom long-term follow-up was available, we determined the relative and absolute risks of all types of fractures on or after the age of 35 years.
Subjects and Methods
Study subjects
Population-based epidemiologic research can be conducted in Olmsted County, MN, USA, because comprehensive (inpatient as well as outpatient) community medical records for all residents are available through a unique medical records linkage system, the Rochester Epidemiology Project.(14,15) Review of medical records for research was carried out in accordance with Minnesota privacy law.(16) After approval by the Institutional Review Boards of Mayo Clinic and the Olmsted Medical Center, Rochester Epidemiology Project resources were used to identify all Olmsted County residents ≤18 years of age when they sustained a first distal forearm fracture in 1935–1992 and who had subsequent follow-up data available until at least age 35 years. The presence of a distal forearm fracture and their surrounding circumstance was confirmed (through review of radiographic reports, emergency room records, primary care or other health care provider notes, orthopedic consultation notes, and/or surgical reports) by trained nurse abstractors. We excluded open distal forearm fractures or ones that resulted from an amputation or an avulsion injury. Although the actual forces causing the distal forearm fractures we included could not be directly quantified, we categorized the distal forearm fractures into two groups based on an estimation of the forces involved: those due to relatively high energy trauma (eg, motor vehicle accidents, falls from greater than standing height, as well as recreational activities that involved power equipment or high velocity or impact, such as skiing, skateboarding, or gymnastics) or to lower energy trauma (eg, falls from standing height or less, and recreational activities that involved low energy collisions, running, or ball sports). When the circumstances were unknown, we categorized them into the low-energy trauma group for the purposes of analyses.
Fracture ascertainment over follow-up
These subjects were then followed forward in time through their linked medical records in the community (historical cohort study) until death or most recent clinical contact. All records at any local provider of medical care were searched by trained nurse abstractors for the occurrence of any subsequent fracture. Mayo Clinic records, for example, contain the details of every inpatient hospitalization and outpatient visit, all emergency room and nursing home care, as well as all radiographic and pathology reports, including autopsies, and all correspondence with each patient.(14) The records contain the clinical history and the radiologist’s report of each fracture, but the original radiographs are not available for review. Because we reviewed all inpatient and outpatient records for each subject, ascertainment of clinically-evident fractures is believed to be complete, along with additional fractures found incidentally (eg, vertebral and rib fractures) on X-rays taken for other purposes.(17) These subsequent fractures were classified according to the circumstances of the injury: by convention, fractures occurring during daily activities (eg, lifting) and falls from a standing height or less were considered moderate trauma, whereas fractures resulting from motor vehicle accidents and falls from a greater height were deemed severe trauma. In addition, we are able to distinguish pathologic fractures attributed by attending physicians to a specific bone lesion (eg, breast cancer, multiple myeloma). From all fractures identified, we defined the subset of fragility fractures (ie, a nonpathologic fracture occurring as a result of no more than moderate trauma). These were further subset as either major osteoporotic fractures (ie, fragility fractures at the typical osteoporotic sites of the proximal femur [hip], thoracic or lumbar vertebrae [spine], distal forearm [wrist] or proximal humerus [shoulder]) or other fragility fractures (ie, fragility fractures at any other skeletal site).
Statistical analysis
Observed fractures were compared with the numbers expected based on fracture site–specific incidence rates in the Olmsted County population (standardized incidence ratios [SIR]). Expected numbers were derived by applying calendar year–specific, age-specific, and sex-specific incidence rates from the local population for the various fractures to the calendar year–specific, age-specific, and sex-specific person-years of follow-up in the cohort and summing over the strata; 95% confidence intervals (95% CI) for the SIRs were calculated assuming the expected rates are fixed and the observed fractures follow a Poisson distribution.(18) We examined the risk for any incident fracture occurring on or after the age of 35 years as well as the risk for fractures related to specific causes (fragility fractures, severe trauma fractures, etc). In each case, analyses were based on the first relevant fracture. Analyses were stratified by sex and then by chronological age at the initial distal forearm fracture (<9 years, 9–11 years, 12–14 years, 15–18 years), recognizing that the peak incidence of distal forearm fractures is betweenages8and11yearsingirlsandbetween11and14yearsin boys.(5) The cumulative incidence of an incident fracture on or after age 35 years was estimated using the Kaplan-Meier method,(19) which was also used to assess survival. Since observed survival did not differ from that expected, it was not necessary to adjust cumulative incidence curves for the competing risk of death. Analyses were performed using SAS version 9 (SAS Institute, Cary, NC, USA) and R (R Foundation for Statistical Computing, Vienna, Austria).
Results
We identified 1776 Olmsted County children who were ≤18 years of age (1086 boys and 690 girls; 74% from the central city of Rochester) when they had an incident distal forearm fracture between January 1, 1935 and December 31, 1992, and who had available follow-up until at least the age of 35 years. Reflecting the demographics of Olmsted County during this time period, 98% were white. The mean ± SD age at distal forearm fracture was 11 ± 4 years for boys and 10 ± 4 years for girls and additional characteristics are noted in Table 1. In children who fractured one arm, only one bone at the distal forearm site was fractured in the majority of children (60% in 1060 boys and 64% in 673 girls) and in over 93% of cases it involved the radius, whereas in 40% of boys and 36% of girls both the radius and ulna were fractured at their distal forearm (Table 1). Of the 36 children who fractured both arms (24 boys and 12 girls), 14 children fractured one bone in each arm, 8 fractured both the radius and ulna in each arm, and 14 fractured one bone in one arm and both the radius and ulna in the other arm. About 40% of children only had a break that was categorized as a greenstick or torus/buckle fracture, and they were more common in the younger age groups (Table 1). The majority of distal forearm fractures were attributed to high-energy compared to lower-energy trauma (Table 1).
Table 1.
Distribution of Initial Distal Forearm Fractures by Type and Cause Among Olmsted County, MN Children (1086 Boys and 690 Girls) in 1935–1992
| Boys
|
Girls
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Age at forearm fracture
|
Age at forearm fracture
|
|||||||||
| Total | <9 years | 9–11 years | 12–14 years | 15–18 years | Total | <9 years | 9–11 years | 12–14 years | 15–18 years | |
| Subjects [fractures], n | 1086 [1110] | 337 [345] | 259 [268] | 299 [304] | 191 [193] | 690 [702] | 283 [286] | 240 [246] | 107 [110] | 60 [60] |
| Age, years, mean ± SD | 11 ± 4 | 6 ± 2 | 11 ± 1 | 13 ± 1 | 16 ± 1 | 10 ± 4 | 6 ± 2 | 10 ± 1 | 13 ± 1 | 17 ± 1 |
| Fracture site, n (%) | ||||||||||
| Radius | 620 (55.9) | 182 (52.8) | 161 (60.1) | 169 (55.6) | 108 (56.0) | 424 (60.4) | 161 (56.3) | 154 (62.6) | 69 (62.7) | 40 (66.7) |
| Ulna | 46 (4.1) | 11 (3.2) | 7 (2.6) | 15 (4.9) | 13 (6.7) | 26 (3.7) | 10 (3.5) | 5 (2.0) | 6 (5.5) | 5 (8.3) |
| Both | 440 (39.6) | 151 (43.8) | 98 (36.6) | 120 (39.5) | 71 (36.8) | 251 (35.8) | 114 (39.9) | 87 (35.4) | 35 (31.8) | 15 (25.0) |
| Uncertain | 4 (0.4) | 1 (0.3) | 2 (0.7) | 0 (0) | 1 (0.5) | 1 (0.1) | 1 (0.3) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Fracture side, n (%) | ||||||||||
| Right | 464 (42.7) | 160 (47.5) | 107 (41.3) | 116 (38.8) | 81 (42.4) | 284 (41.2) | 133 (47.0) | 94 (39.2) | 36 (33.6) | 21 (35.0) |
| Left | 596 (54.9) | 168 (49.9) | 143 (55.2) | 177 (59.2) | 108 (56.5) | 389 (56.4) | 145 (51.2) | 139 (57.9) | 68 (63.6) | 37 (61.7) |
| Bilateral | 24 (2.2) | 8 (2.4) | 9 (3.5) | 5 (1.7) | 2 (1.0) | 12 (1.7) | 3 (1.1) | 6 (2.5) | 3 (2.8) | 0 (0.0) |
| Uncertain | 2 (0.2) | 1 (0.3) | 0 (0.0) | 1 (0.3) | 0 (0.0) | 5 (0.7) | 2 (0.7) | 1 (0.4) | 0 (0.0) | 2 (3.3) |
| Greenstick/torus/buckle, n (%) | ||||||||||
| Yes | 404 (37.2) | 155 (46.0) | 111 (42.9) | 99 (33.1) | 39 (20.4) | 324 (47.0) | 158 (48.8) | 118 (49.2) | 40 (37.4) | 8 (13.3) |
| No | 659 (60.7) | 171 (50.7) | 141 (54.4) | 196 (65.6) | 151 (79.1) | 356 (51.6) | 122 (43.1) | 117 (48.8) | 66 (61.7) | 51 (85.0) |
| Uncertain | 23 (2.1) | 11 (3.3) | 7 (2.7) | 4 (1.3) | 1 (0.5) | 10 (1.4) | 3 (1.1) | 5 (2.1) | 1 (0.9) | 1 (1.7) |
| Fracture etiology, n (%) | ||||||||||
| MVA | 63 (5.8) | 3 (0.9) | 3 (3.1) | 15 (5.0) | 37 (19.4) | 13 (1.9) | 4 (1.4) | 1 (0.4) | 1 (0.9) | 7 (11.7) |
| Fall >standing | 134 (12.3) | 67 (19.9) | 33 (12.7) | 21 (7.0) | 13 (6.8) | 60 (8.7) | 38 (13.4) | 11 (4.6) | 7 (6.5) | 4 (6.7) |
| Fall ≤ standing | 142 (13.1) | 58 (17.2) | 29 (11.2) | 41 (13.7) | 14 (7.3) | 140 (20.3) | 65 (23.0) | 48 (20.0) | 18 (16.8) | 9 (15.0) |
| Recreational | 624 (57.5) | 167 (49.6) | 152 (58.7) | 196 (65.6) | 109 (57.1) | 385 (55.8) | 136 (48.1) | 151 (62.9) | 67 (62.6) | 31 (51.7) |
| Other | 38 (3.5) | 10 (3.0) | 9 (3.5) | 6 (2.0) | 13 (6.8) | 23 (3.3) | 7 (2.5) | 6 (2.5) | 7 (6.5) | 3 (5.0) |
| Unknown | 85 (7.8) | 32 (9.5) | 28 (10.8) | 20 (6.7) | 5 (2.6) | 69 (10.0) | 33 (11.7) | 23 (9.6) | 7 (6.5) | 6 (10.0) |
| Precipitating trauma, n (%) | ||||||||||
| High energy | 713 (65.7) | 207 (61.4) | 174 (67.2) | 195 (65.2) | 137 (71.7) | 387 (56.1) | 155 (54.8) | 124 (51.7) | 69 (64.5) | 39 (65.0) |
| Lower energy | 288 (26.5) | 98 (29.1) | 57 (22.0) | 84 (28.1) | 49 (25.7) | 234 (33.9) | 95 (33.6) | 93 (38.8) | 31 (29.0) | 15 (25.0) |
| Unknown | 85 (7.8) | 32 (9.5) | 28 (10.8) | 20 (6.7) | 5 (2.6) | 69 (10.0) | 33 (11.7) | 23 (9.6) | 7 (6.5) | 6 (10.0) |
Note that some statistics reflect the number of children whereas others are based on the number of fractures.
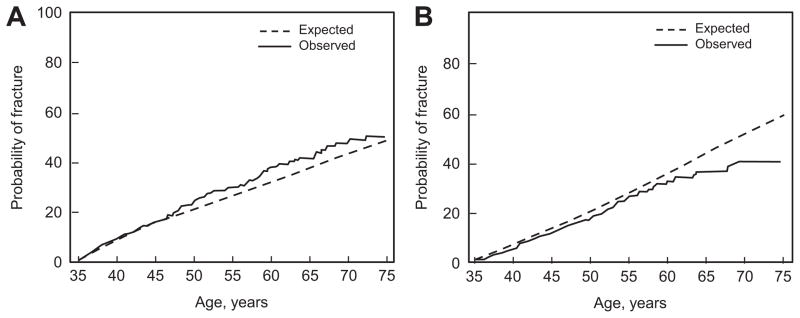
These children had their first recorded visit to a physician in the community a median 9 years prior to their initial distal forearm fracture, and they were subsequently followed for a total of 70,662 person-years (range, 16–75 years per subject) up to a maximum age of 88 years, with 27,292 person-years of follow-up after age 35 years (range, 4 days to 53 years per subject). By design, all subjects included in the analysis survived to age 35 years, and survival thereafter was similar to that expected (at age 55 years, 95% versus 95%; p = 0.869). The median age at follow-up was 49 years (range, 35–88 years) for the men and 48 years (range, 35–86 years) for the women. During follow-up beginning at age 35 years, 24% of the boys (now men) experienced at least one fracture, as did 18% of the women, and of these individuals, 104 men and 41 women had more than one fracture over follow-up. The specific fractures observed after age 35 years are delineated in Table 2. The probability of any fracture as estimated by the cumulative incidence was 30% at age 55 years for men compared with 26% for women (Fig. 1), whereas the probability of a major osteoporotic fracture, as estimated by the cumulative incidence, was similar for men and women at age 55 years (7% for men versus 8% for women; p = 0.699).
Table 2.
Distribution of All Fractures and Fragility Fractures After Age 35 Years Among 1776 Olmsted County, MN Residents (1086 Men and 690 Women) Who Had Sustained a Distal Forearm Fracture As Children in 1935–1992, by Subsequent Fracture Site and Cause
| Fracture site | Men
|
Women
|
||
|---|---|---|---|---|
| All fractures | Fragility fracturesa | All fractures | Fragility fracturesa | |
| n (%) | n (%) | n (%) | n (%) | |
| Skull/face | 20 (4.5) | 4 (2.1) | 5 (2.4) | 4 (3.5) |
| Hands/fingers | 64 (14.3) | 8 (4.1) | 15 (7.3) | 5 (4.4) |
| Distal forearm | 26 (5.8) | 5 (2.6) | 17 (8.3) | 9 (7.9) |
| Proximal humerus | 7 (1.6) | 0 (0.0) | 5 (2.4) | 2 (1.8) |
| Other arm | 17 (3.8) | 3 (1.6) | 13 (6.3) | 6 (5.3) |
| Clavicle/scapula/sternum | 22 (4.9) | 1 (0.5) | 6 (2.9) | 5 (4.4) |
| Ribs | 76 (16.9) | 48 (24.9) | 28 (13.7) | 19 (16.7) |
| Thoracic/lumbar vertebrae | 92 (20.5) | 81 (42.0) | 37 (18.0) | 32 (28.1) |
| Cervical vertebrae | 14 (3.1) | 5 (2.6) | 6 (2.9) | 3 (2.6) |
| Pelvis | 5 (1.1) | 2 (1.0) | 7 (3.4) | 5 (4.4) |
| Proximal femur | 6 (1.3) | 4 (2.1) | 5 (2.4) | 5 (4.4) |
| Other leg | 53 (11.8) | 18 (9.3) | 20 (9.8) | 10 (8.8) |
| Feet/toes | 47 (10.5) | 14 (7.3) | 41 (20.0) | 9 (7.9) |
| All sites | 449 | 193 | 205 | 114 |
Excludes severe trauma and pathologic fractures.
Fig 1.
Observed compared to expected cumulative incidence of fracture in age ≥ 35 years among Olmsted County, MN residents with a first distal forearm fracture in 1935–1992 at age ≤ 18 years and who had follow-up to at least age 35 years, by age, and separately for men (A) and women (B).
Future fracture risk in men
Among the 1086 boys with a distal forearm fracture, 265 subsequently sustained at least one fracture at age ≥35 years, 144 of whom had at least one fracture attributed to no more than moderate trauma (Table 3). Altogether, their risk of any subsequent fracture was elevated 1.2-fold (95% CI, 1.01–1.3) compared to that expected in community men generally (Table 3). However, there was no increase in their risk of fractures due to severe trauma or to a specific pathology (Table 3). Instead, the increased risk was confined to fragility fractures (Table 3, Fig. 2), especially the subset of traditional major osteoporotic fractures (SIR, 2.6; 95% CI, 2.1–3.3) and this was observed across all age groups at fracture, but particularly in boys <9 years of age (Table 3). These general patterns also persisted when the age at subsequent fracture was subdivided into 35 to 49 years and ≥50 years (Table 3). In addition, the risk of any fracture, any fragility fracture or any subsequent major osteoporotic fracture was similar whether the initial distal forearm fracture was attributed to high versus lower energy trauma or if the initial distal forearm fracture was considered a greenstick/torus/buckle fracture only or not (data not shown).
Table 3.
Fractures Observed Among 1086 Olmsted County, MN Male Residents Following a Childhood Distal Forearm Fracture in 1935–1992 Compared With the Numbers Expected and SIR, with 95% CIs
| Fracture type and attained age | Men
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Age at forearm fracture
| ||||||||||
| All
|
<9 years
|
9–11 years
|
12–14 years
|
15–18 years
|
||||||
| Obsa | SIR (95% CI) | Obsa | SIR (95% CI) | Obsa | SIR (95% CI) | Obsa | SIR (95% CI) | Obsa | SIR (95% CI) | |
| All ages ≥35 years | 1086 | 337 | 259 | 299 | 191 | |||||
| Any fracture | 265 | 1.2 (1.01–1.3) | 76 | 1.1 (0.9–1.4) | 58 | 1.0 (0.8–1.3) | 77 | 1.2 (0.9–1.5) | 54 | 1.2 (0.9–1.6) |
| Fragility fracture | 144 | 1.9 (1.6–2.3) | 42 | 2.0 (1.4–2.7) | 26 | 1.4 (0.9–2.1) | 45 | 2.2 (1.6–2.9) | 31 | 2.0 (1.4–2.9) |
| Major osteoporotic fracture | 72 | 2.6 (2.1–3.3) | 26 | 3.5 (2.3–5.2) | 14 | 2.1 (1.2–3.6) | 20 | 2.6 (1.6–4.0) | 12 | 2.1 (1.1–3.6) |
| Other fragility fracture | 90 | 1.7 (1.3–2.0) | 23 | 1.5 (0.9–2.2) | 15 | 1.1 (0.6–1.9) | 29 | 2.0 (1.3–2.8) | 23 | 2.2 (1.4–3.3) |
| Severe trauma fracture | 163 | 0.9 (0.8–1.1) | 46 | 0.9 (0.6–1.2) | 41 | 1.0 (0.7–1.3) | 42 | 0.8 (0.6–1.1) | 34 | 1.0 (0.7–1.4) |
| Pathologic fracture | 2 | 0.4 (0.05–1.4) | 0 | 0.0 (0.0–3.2) | 1 | 0.8 (0.02–4.6) | 0 | 0.0 (0.0–2.5) | 1 | 0.7 (0.02–4.1) |
| Ages 35–49 years | 1086 | 337 | 259 | 299 | 191 | |||||
| Any fracture | 197 | 1.2 (1.00–1.3) | 57 | 1.1 (0.8–1.4) | 50 | 1.2 (0.9–1.6) | 54 | 1.1 (0.9–1.5) | 36 | 1.2 (0.8–1.6) |
| Fragility fracture | 82 | 1.8 (1.5–2.3) | 25 | 1.9 (1.2–2.8) | 19 | 1.7 (1.04–2.7) | 23 | 1.8 (1.2–2.8) | 15 | 1.8 (1.02–3.0) |
| Major osteoporotic fracture | 38 | 3.0 (2.1–4.1) | 12 | 3.3 (1.7–5.8) | 9 | 3.0 (1.4–5.6) | 12 | 3.4 (1.8–5.9) | 5 | 2.1 (0.7–4.9) |
| Other fragility fracture | 49 | 1.4 (1.1–1.9) | 14 | 1.4 (0.8–2.3) | 10 | 1.2 (0.6–2.2) | 14 | 1.5 (0.8–2.5) | 11 | 1.8 (0.9–3.2) |
| Severe trauma fracture | 131 | 1.0 (0.8–1.1) | 36 | 0.9 (0.6–1.2) | 36 | 1.1 (0.8–1.5) | 33 | 0.9 (0.6–1.2) | 26 | 1.0 (0.7–1.5) |
| Pathologic fracture | 1 | 0.2 (0.01–1.4) | 0 | 0.0 (0.0–4.0) | 0 | 0.0 (0.0–3.8) | 0 | 0.0 (0.0–3.3) | 1 | 1.0 (0.03–5.7) |
| All ages ≥50 years | 516 | 143 | 126 | 148 | 99 | |||||
| Any fracture | 96 | 1.3 (1.03–1.6) | 27 | 1.3 (0.9–1.9) | 14 | 0.8 (0.4–1.3) | 32 | 1.5 (1.05–2.2) | 23 | 1.5 (0.96–2.3) |
| Fragility fracture | 73 | 2.2 (1.7–2.8) | 21 | 2.4 (1.5–3.7) | 10 | 1.2 (0.6–2.3) | 24 | 2.7 (1.7–4.0) | 18 | 2.5 (1.5–4.0) |
| Major osteoporotic fracture | 38 | 2.5 (1.8–3.4) | 14 | 3.6 (2.0–6.1) | 7 | 1.9 (0.8–3.9) | 9 | 2.1 (0.97–4.0) | 8 | 2.4 (1.03–4.7) |
| Other fragility fracture | 46 | 2.2 (1.6–2.9) | 12 | 2.0 (1.1–3.6) | 6 | 1.2 (0.4–2.6) | 16 | 2.8 (1.6–4.5) | 12 | 2.6 (1.4–4.6) |
| Severe trauma fracture | 40 | 0.8 (0.6–1.1) | 11 | 0.8 (0.4–1.5) | 7 | 0.6 (0.2–1.2) | 12 | 0.9 (0.5–1.6) | 10 | 1.1 (0.5–2.0) |
| Pathologic fracture | 1 | 0.8 (0.02–4.6) | 0 | 0.0 (0.0–16) | 1 | 4.1 (0.1–23) | 0 | 0.0 (0.0–10) | 0 | 0.0 (0.0–9.8) |
Results are shown for all and by age group at the initial distal forearm fracture.
Obs = number observed; SIR = standardized incidence ratio; CI = confidence interval.
Note that the number of fractures observed may differ from those reported in Table 2 because only the first fracture of each type [within a time frame] per patient was counted in these analyses.
Fig 2.
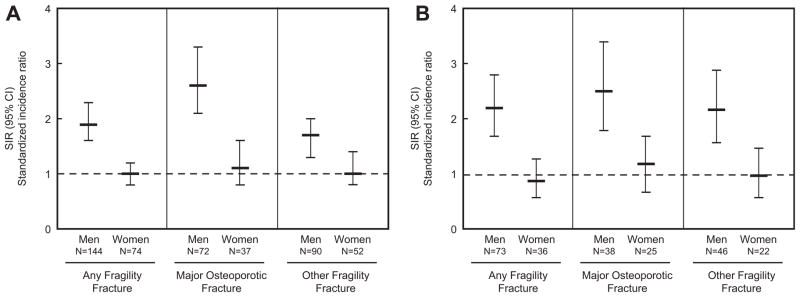
Standardized incidence ratio (SIR) for the risk of future fragility fracture occurring at age ≥35 years (A) or age ≥50 years (B) for Olmsted County, MN men and women following a distal forearm fracture in childhood at age ≤18 years in 1935–1992.
Future fracture risk in women
Among the 690 girls with a distal forearm fracture, 122 sustained at least one fracture after age 35 years, 74 of whom had at least one fragility fracture at any skeletal site, and 37 had at least one major osteoporotic fracture (Table 4). However, we found no increased risk for any fracture, any fragility fracture, or any major osteoporotic fracture relative to expected fracture rates in community women generally (Table 4, Fig. 2). Interestingly, there was a modest decreased risk in severe trauma fractures after age 35 years (SIR, 0.8; 95% CI, 0.6–0.98) (Table 4). We did note a possible trend, although not statistically significant, for a modest increased risk for future fragility fractures in women aged 35 to 49 years (SIR, 1.2; 95% CI, 0.8–1.6) but not necessarily for women aged ≥50 years (SIR, 0.9; 95% CI, 0.6–1.3) (Table 4). As in the men, there was no difference in our findings whether the initial distal forearm fracture resulted from trauma attributed to high-energy versus lower-energy or if it was a greenstick/torus/buckle fracture only or not (data not shown).
Table 4.
Fractures observed Among 690 Olmsted County, MN Females Following a Childhood Distal Forearm Fracture in 1935–1992 Compared With the Numbers Expected and SIRs, With 95% CIs
| Fracture type and attained age | Women
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Age at forearm fracture
| ||||||||||
| Total
|
<9 years
|
9–11 years
|
12–14 years
|
15–18 years
|
||||||
| Obsa | SIR (95% CI) | Obsa | SIR (95% CI) | Obsa | SIR (95% CI) | Obsa | SIR (95% CI) | Obsa | SIR (95% CI) | |
| All ages ≥35 years | 690 | 283 | 240 | 107 | 60 | |||||
| Any fracture | 122 | 0.8 (0.7–0.98) | 53 | 0.9 (0.7–1.2) | 45 | 1.0 (0.8–1.4) | 15 | 0.5 (0.3–0.8) | 9 | 0.6 (0.2–1.04) |
| Fragility fracture | 74 | 1.0 (0.8–1.2) | 32 | 1.1 (0.7–1.5) | 28 | 1.3 (0.9–1.9) | 9 | 0.6 (0.3–1.1) | 5 | 0.6 (0.2–1.3) |
| Major osteoporotic fracture | 37 | 1.1 (0.8–1.6) | 16 | 1.3 (0.7–2.1) | 12 | 1.3 (0.7–2.3) | 7 | 1.0 (0.4–2.0) | 2 | 0.5 (0.1–1.8) |
| Other fragility fracture | 52 | 1.0 (0.8–1.4) | 23 | 1.2 (0.7–1.7) | 22 | 1.5 (0.96–2.3) | 4 | 0.4 (0.1–0.99) | 3 | 0.5 (0.1–1.6) |
| Severe trauma fracture | 64 | 0.8 (0.6–0.98) | 29 | 0.9 (0.6–1.2) | 22 | 0.9 (0.5–1.3) | 8 | 0.5 (0.2–1.02) | 5 | 0.6 (0.2–1.3) |
| Pathologic fracture | 5 | 1.2 (0.4–2.8) | 2 | 1.5 (0.2–5.5) | 3 | 2.6 (0.5–7.6) | 0 | 0.0 (0.0–3.4) | 0 | 0.0 (0.0–6.5) |
| All ages 35–49 years | 690 | 283 | 240 | 107 | 60 | |||||
| Any fracture | 85 | 0.9 (0.7–1.1) | 39 | 1.0 (0.7–1.4) | 33 | 1.1 (0.7–1.5) | 6 | 0.4 (0.1–0.8) | 7 | 0.8 (0.3–1.6) |
| Fragility fracture | 45 | 1.2 (0.8–1.6) | 22 | 1.4 (0.9–2.2) | 17 | 1.4 (0.8–2.2) | 2 | 0.3 (0.04–1.1) | 4 | 1.1 (0.3–2.8) |
| Major osteoporotic fracture | 15 | 1.3 (0.8–2.2) | 6 | 1.3 (0.5–2.8) | 6 | 1.7 (0.6–3.7) | 1 | 0.5 (0.01–2.8) | 2 | 1.8 (0.2–6.3) |
| Other fragility fracture | 35 | 1.2 (0.9–1.7) | 19 | 1.6 (1.0–2.6) | 13 | 1.4 (0.8–2.4) | 1 | 0.2 (0.01–1.1) | 2 | 0.7 (0.1–2.6) |
| Severe trauma fracture | 45 | 0.7 (0.5–0.99) | 19 | 0.8 (0.5–1.2) | 18 | 0.9 (0.6–1.5) | 4 | 0.4 (0.1–0.97) | 4 | 0.7 (0.2–1.7) |
| Pathologic fracture | 3 | 1.0 (0.2–2.8) | 1 | 0.9 (0.02–4.9) | 2 | 2.1 (0.3–7.7) | 0 | 0.0 (0.0–5.7) | 0 | 0.0 (0.0–8.6) |
| Age ≥50 years | 292 | 119 | 87 | 50 | 36 | |||||
| Any fracture | 50 | 0.9 (0.7–1.2) | 20 | 0.9 (0.6–1.4) | 17 | 1.2 (0.7–1.9) | 10 | 0.8 (0.4–1.4) | 3 | 0.4 (0.1–1.1) |
| Fragility fracture | 36 | 0.9 (0.6–1.3) | 13 | 0.8 (0.4–1.4) | 13 | 1.4 (0.7–2.4) | 8 | 0.9 (0.4–1.7) | 2 | 0.4 (0.1–1.3) |
| Major osteoporotic fracture | 25 | 1.2 (0.7–1.7) | 11 | 1.4 (0.7–2.4) | 8 | 1.4 (0.6–2.8) | 6 | 1.2 (0.4–2.5) | 0 | 0.0 (0.0–1.3) |
| Other fragility fracture | 22 | 1.0 (0.6–1.5) | 6 | 0.7 (0.2–1.5) | 10 | 1.9 (0.9–3.5) | 4 | 0.8 (0.2–1.9) | 2 | 0.7 (0.1–2.6) |
| Severe trauma fracture | 23 | 1.0 (0.6–1.5) | 12 | 1.3 (0.7–2.3) | 6 | 0.9 (0.3–2.0) | 4 | 0.8 (0.2–2.1) | 1 | 0.3 (0.01–1.9) |
| Pathologic fracture | 2 | 2.1 (0.2–7.5) | 1 | 5.7 (0.1–32) | 1 | 4.7 (0.1–26) | 0 | 0.0 (0.0–8.5) | 0 | 0.0 (0.0–27) |
Results are shown for all and by age group at the initial distal forearm fracture.
Obs = number observed; SIR = standardized incidence ratio; CI = confidence interval.
Note that the number of fractures observed may differ from those reported in Table 2 because only the first fracture of each type [within a time frame] per patient was counted in these analyses.
Discussion
Fractures occurring before the age of 40 years are currently ignored in assessing future fracture risk (http://www.nof.org/). However, key risk factors for fracture in older men and women are determined early in life, including peak bone mass as well as bone geometry, one of the main biomechanical determinants of bone strength.(20) Furthermore, low bone mass in childhood predicts the risk for subsequent fractures during later childhood or adolescence.(21) With over 40% of boys and girls sustaining a fracture during their growing years,(3) and with distal forearm fractures accounting for up to one-third of all these fractures,(4) the role of a distal forearm fracture on future fracture risk during adulthood could have important public health implications. Indeed, based on our study findings, boys, not girls, who sustain a distal forearm fracture have an increased risk for future fragility fractures during adulthood, and this was irrespective of their age at the time of the forearm fracture.
Although distal forearm fractures are more frequent among boys than girls,(4) which we also observed in our study, fractures, in general, are less common among older men compared with women of similar age. However, among the boys with a distal forearm fracture, not only was their risk of fracture significantly higher than expected for community men, their absolute risk of fracture was significantly greater than women. The increase was confined to fragility fractures, especially the subset of those traditionally considered major osteoporotic fractures (at the hip, spine, wrist, and shoulder), where the risk was elevated over twofold. The risk was increased for any age at distal forearm fracture but seemed to be accentuated among those whose initial forearm fracture occurred before 9 years of age. This association observed may be due to genetic and/or acquired factors that negatively impact bone mass and strength. Parfitt(22) suggested that distal forearm fractures in boys may be due to the mismatch between an age-related increase in physical activity, leading to greater skeletal loads(23) from falls, etc., and transient defects in cortical bone developing during the growth spurt that reduce bone strength.(24) Whether there are other deficits that actually persist in these boys has been unclear, but a recent study by Buttazzoni and colleagues(25) reported that men with a fracture in childhood had persistent deficits in bone density and structure roughly 25 years later when compared with control men who had no childhood fracture. Their bone size at the radius and tibia, in particular, tended to be smaller compared with controls. Larger bone size confers a biomechanical advantage for bone strength and is considered one of the key factors responsible for the lower overall risk of fractures among aging men compared with women.(26)
By contrast, we found no overall increased risk of a subsequent fracture among girls who had sustained a distal forearm fracture in childhood. It is possible that this represents a behavioral change in these girls with avoidance in fracture risk activities, generally. This may be likely given the modest protective effect a distal forearm fracture in childhood had on severe trauma fractures in adult women. On the other hand, the accelerated bone loss at the menopause in women(27) may lead to a greater net negative influence on ultimate bone strength and subsequent fracture risk. This may be another possible explanation, as we did note a trend for a modest increased risk for fragility fractures among women who were 35 to 49 years of age, and likely premenopausal, but not necessarily in women age 50 and older, who were most likely postmenopausal. The risks observed, however, were modest and not statistically significant for any robust conclusion. Although several studies have reported deficits in bone density among adolescent girls with a distal forearm fracture,(7,10,28) they may be transient. In the study by Buttazzoni and colleagues,(25) the deficits in bone density and structure observed in adult women with a childhood fracture were smaller relative to those seen in their male counterparts and were not statistically significant when compared with their female controls.
Two studies that examined the risk of any childhood fracture on future fractures in adulthood found no increased risk.(29,30) One large study found no increased risk of fracture in either older men or women who reported any fracture between ages 8 and 18 years.(29) Only 9% of the men and 4% of the women in that study recalled any earlier fracture. Similarly, Wu and colleagues(30) found no association between a self-report of fractures that occurred before age 20 years and subsequent fracture risk among 90 postmenopausal women, but only 9% of those women reported a childhood fracture. Given that the cumulative incidence of fractures in childhood is estimated at 42% in girls and 54% in boys,(3) ascertainment bias may have impacted findings in these two studies. Any fracture in childhood was also considered in these studies, not just distal forearm fractures, as in our study. That fractures in younger age groups were not included in the study by Pye and colleagues(29) may yet be another explanation for the different results observed for men compared with our study. Nonetheless, despite potential differences and limitations, both studies reported no increased risk for future fractures in women, similar to our overall results.
The main strengths of this study are our unique capability for long-term follow-up of a large cohort of community boys and girls with an initial distal forearm fracture and for complete ascertainment of fractures over follow-up. Long-term follow-up is important as demonstrated by a previous study of young women with anorexia nervosa, whose excess risk of osteoporotic fractures did not become evident until roughly 25 years or later after diagnosis.(31) Despite the lengthy follow-up, we still had only a limited number of subjects who had reached the ages when hip fractures, the most important sequelae of osteoporosis, are particularly common. It would have been interesting to determine if those with a second distal forearm fracture as children were at particularly increased risk for fractures as adults, especially among the girls, but there were only 95 boys and 45 girls who met these criteria. We saw no differences in the risk of subsequent fractures among the childhood distal forearm fractures that we informally attributed to either high-energy or lower-energy trauma; however, the original medical records did not always have sufficient detail of the initial forearm fracture to allow for a more complete trauma classification.(32) On the other hand, childhood fractures due to both high-energy or lower-energy trauma have been reported to be associated with low bone density in children,(33) similar to adults.(34) In addition, we had no specific information on bone age or pubertal stage at the time of the initial distal forearm fracture; although we previously showed that bone age and chronological age are similar in otherwise healthy children.(24) A further limitation may be the generalizability of these data from a predominantly white population,(14,15) but fractures are less common in nonwhite children.(35) Our incidence rates of distal forearm fracture among children in our population are consistent with existing literature(5) and the incidence of hip fractures in this community is comparable to national figures for U.S. whites, generally,(36) so we would expect our findings to be generalizable to U.S. whites. Although we studied a large population-based sample, our power was still limited for exploring the risk of future fractures by age of childhood forearm fracture, particularly in women.
Relative to women, men are generally protected from fractures in midlife, with incidence rates rising mostly after age 70 years.(37) The men who had a distal forearm fracture in childhood, however, were already at over a twofold greater risk of a fragility fracture compared with middle-aged men in the underlying community. Moreover, the proportion of boys with a distal forearm fracture who went on to suffer further fractures in adulthood was slightly higher than observed even for women, who are more likely to sustain a fracture with older age.(37) In particular, vertebral fractures were fairly common in these men, even more so than in women, which is also a reversal of what is usually observed.(37) These findings were consistent when we restricted our analyses to subjects who had a fracture at age 50 years or later. Whether this further indicates that these boys are more likely to have weaker bones overall, rather than simply representing individuals who are more likely to be engaged in continued high fracture risk behavior, is unknown. It may also represent a combination of both factors.
In conclusion, we found that boys, not girls, who had a distal forearm fracture during childhood were associated with an increased risk of future fragility fractures as adults. Further work is needed to determine whether this increased risk in older men is due to deficits in bone strength established in childhood that track into adulthood, to continued high risk-taking behavior for fractures, or perhaps, to a combination of these factors. Nonetheless, until these issues can be better clarified, our findings have potential public health implications and suggest that older men should be asked about a history of a childhood distal forearm fracture, and if so, would warrant further screening as well as counseling on measures to optimize bone health and prevent fractures.
Acknowledgments
This work was supported by research grant P01 AG004875 from the National Institute on Aging and made possible by the Rochester Epidemiology Project (R01 AG034676 from the National Institute on Aging). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. We thank Marcia Erickson, RN, Wendy Gay, RN, Julie Gingras, RN, Joan LaPlante, RN, Constance Neuman, RN, and Cynthia Nosek, RN. for their work in data abstraction. The funding agencies had no role in the design or conduct of the study; collection, management, analysis, or interpretation of the data; nor the preparation, review, or approval of the manuscript.
Footnotes
Disclosures
SA serves on a scientific advisory board for Merck & Co. All other authors state that they have no conflicts of interest.
Authors’ roles: Study design: SA, LJM. Study contact: SA. Supervision of data collection: SA. Data analysis: SJA, EJA. Data interpretation: SA, LJM, SK. Drafting of manuscript: SA, LJM. Revising of manuscript: SA, LJM, SJA, EJA, MBD, SK, PRF, SK. Approving final manuscript: SA, LJM, SJA, EJA, MBD, SK, PRF, SK. SA takes responsibility for the integrity of the data analysis.
References
- 1.Cooper C, Westlake S, Harvey N, Javaid K, Dennison E, Hanson M. Review: developmental origins of osteoporotic fracture. Osteoporos Int. 2006;17(3):337–47. doi: 10.1007/s00198-005-2039-5. [DOI] [PubMed] [Google Scholar]
- 2.Baxter-Jones AD, Faulkner RA, Forwood MR, Mirwald RL, Bailey DA. Bone mineral accrual from 8 to 30 years of age: an estimation of peak bone mass. J Bone Miner Res. 2011;26(8):1729–39. doi: 10.1002/jbmr.412. [DOI] [PubMed] [Google Scholar]
- 3.Jones IE, Williams SM, Dow N, Goulding A. How many children remain fracture-free during growth? a longitudinal study of children and adolescents participating in the Dunedin Multidisciplinary Health and Development Study. Osteoporos Int. 2002;13 (12):990–5. doi: 10.1007/s001980200137. [DOI] [PubMed] [Google Scholar]
- 4.Hedström EM, Svensson O, Bergström U, Michno P. Epidemiology of fractures in children and adolescents. Acta Orthopaedica. 2010;81 (1):148–53. doi: 10.3109/17453671003628780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Khosla S, Melton LJ, 3rd, Dekutoski MB, Achenbach SJ, Oberg AL, Riggs BL. Incidence of childhood distal forearm fractures over 30 years: a population-based study. JAMA. 2003;290(11):1479–85. doi: 10.1001/jama.290.11.1479. [DOI] [PubMed] [Google Scholar]
- 6.Mayranpaa MK, Makitie O, Kallio PE. Decreasing incidence and changing pattern of childhood fractures: a population-based study. [Erratum appears in J Bone Miner Res. 2011 Feb;26(2):439] J Bone Miner Res. 2009;25(12):2752–9. doi: 10.1002/jbmr.155. [DOI] [PubMed] [Google Scholar]
- 7.Goulding A, Cannan R, Williams SM, Gold EJ, Taylor RW, Lewis-Barned NJ. Bone mineral density in girls with forearm fractures. J Bone Miner Res. 1998;13(1):143–8. doi: 10.1359/jbmr.1998.13.1.143. [DOI] [PubMed] [Google Scholar]
- 8.Skaggs DL, Loro ML, Pitukcheewanont P, Tolo V, Gilsanz V. Increased body weight and decreased radial cross-sectional dimensions in girls with forearm fractures. J Bone Miner Res. 2001;16(7):1337–42. doi: 10.1359/jbmr.2001.16.7.1337. [DOI] [PubMed] [Google Scholar]
- 9.Goulding A, Jones IE, Taylor RW, Williams SM, Manning PJ. Bone mineral density and body composition in boys with distal forearm fractures: a dual-energy X-ray absorptiometry study. J Pediatr. 2001;139(4):509–15. doi: 10.1067/mpd.2001.116297. [DOI] [PubMed] [Google Scholar]
- 10.Ma D, Jones G. The association between bone mineral density, metacarpal morphometry, and upper limb fractures in children: a population-based case-control study. J Clin Endocrinol Metab. 2003;88(4):1486–91. doi: 10.1210/jc.2002-021682. [DOI] [PubMed] [Google Scholar]
- 11.Kalkwarf HJ, Laor T, Bean JA. Fracture risk in children with a forearm injury is associated with volumetric bone density and cortical area (by peripheral QCT) and areal bone density (by DXA) Osteoporos Int. 2011;22(2):607–16. doi: 10.1007/s00198-010-1333-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cuddihy MT, Gabriel SE, Crowson CS, Atkinson EJ, Tabini C, O’Fallon WM, Melton LJ., 3rd Osteoporosis intervention following distal forearm fractures: a missed opportunity? Arch Intern Med. 2002;162(4):421–6. doi: 10.1001/archinte.162.4.421. [DOI] [PubMed] [Google Scholar]
- 13.Haentjens P, Johnell O, Kanis JA, Bouillon R, Cooper C, Lamraski G, Vanderschueren D, Kaufman JM, Boonen S. Evidence from data searches and life-table analyses for gender-related differences in absolute risk of hip fracture after Colles’ or spine fracture: Colles’ fracture as an early and sensitive marker of skeletal fragility in white men. J Bone Miner Res. 2004;19(12):1933–44. doi: 10.1359/JBMR.040917. [DOI] [PubMed] [Google Scholar]
- 14.Melton LJ., 3rd History of the Rochester Epidemiology Project. Mayo Clin Proc. 1996;71(3):266–74. doi: 10.4065/71.3.266. [DOI] [PubMed] [Google Scholar]
- 15.St Sauver JL, Grossardt BR, Leibson CL, Yawn BP, Melton LJ, 3rd, Rocca WA. Generalizability of epidemiological findings and public health decisions: an illustration from the Rochester Epidemiology Project. Mayo Clin Proc. 2012;87(2):151–60. doi: 10.1016/j.mayocp.2011.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Melton LJ., 3rd The threat to medical-records research. N Engl J Med. 1997;337(20):1466–70. doi: 10.1056/NEJM199711133372012. [DOI] [PubMed] [Google Scholar]
- 17.Melton LJ, 3rd, Crowson CS, O’Fallon WM. Fracture incidence in Olmsted County, Minnesota: comparison of urban with rural rates and changes in urban rates over time. Osteoporos Int. 1999;9(1):29–37. doi: 10.1007/s001980050113. [DOI] [PubMed] [Google Scholar]
- 18.Cox DR. Some simple approximate tests for Poisson variates. Biometrika. 1953;40:354–60. [Google Scholar]
- 19.Kaplan EL, Meier P. Non-parametric estimation from incomplete observations. J Am Stat Assoc. 1958;53(282):457–81. [Google Scholar]
- 20.Duan Y, Beck TJ, Wang XF, Seeman E. Structural and biomechanical basis of sexual dimorphism in femoral neck fragility has its origins in growth and aging. J Bone Miner Res. 2003;18(10):1766–74. doi: 10.1359/jbmr.2003.18.10.1766. [DOI] [PubMed] [Google Scholar]
- 21.Clark EM, Tobias JH, Ness AR. Association between bone density and fractures in children: a systematic review and meta-analysis. Pediatrics. 2006;117(2):e291–7. doi: 10.1542/peds.2005-1404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Parfitt AM. The two faces of growth: benefits and risks to bone integrity. Osteoporos Int. 1994;4(6):382–98. doi: 10.1007/BF01622201. [DOI] [PubMed] [Google Scholar]
- 23.Bailey DA, Wedge JH, McCulloch RG, Martin AD, Bernhardson SC. Epidemiology of fractures of the distal end of the radius in children as associated with growth. J Bone Joint Surg Am. 1989;71(8):1225–31. [PubMed] [Google Scholar]
- 24.Kirmani S, Christen D, van Lenthe GH, Fischer PR, Bouxsein ML, McCready LK, Melton LJ, 3rd, Riggs BL, Amin S, Muller R, Khosla S. Bone structure at the distal radius during adolescent growth. J Bone Miner Res. 2009;24(6):1033–42. doi: 10.1359/JBMR.081255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Buttazzoni C, Rosengren EB, Tveit M, Landin L, Nilsson JA, Karlsson MK. A childhood fracture predicts low bone mass in young adulthood —a 27-year prospective controlled study. J Bone Miner Res. 2013 Feb;28(2):351–9. doi: 10.1002/jbmr.1743. [DOI] [PubMed] [Google Scholar]
- 26.Riggs BL, Melton LJ, 3rd, Robb RA, Camp JJ, Atkinson EJ, Peterson JM, Rouleau PA, McCollough CH, Bouxsein ML, Khosla S. Population-based study of age and sex differences in bone volumetric density, size, geometry, and structure at different skeletal sites. J Bone Miner Res. 2004;19(12):1945–54. doi: 10.1359/JBMR.040916. [DOI] [PubMed] [Google Scholar]
- 27.Khosla S, Melton LJ, 3rd, Riggs BL. The unitary model for estrogen deficiency and the pathogenesis of osteoporosis: is a revision needed? J Bone Miner Res. 2011;26(3):441–51. doi: 10.1002/jbmr.262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Goulding A, Jones IE, Taylor RW, Manning PJ, Williams SM. More broken bones: a 4-year double cohort study of young girls with and without distal forearm fractures. J Bone Miner Res. 2000;15 (10):2011–8. doi: 10.1359/jbmr.2000.15.10.2011. [DOI] [PubMed] [Google Scholar]
- 29.Pye SR, Tobias J, Silman AJ, Reeve J, O’Neill TW. Childhood fractures do not predict future fractures: results from the European Prospective Osteoporosis Study. J Bone Miner Res. 2009;24(7):1314–8. doi: 10.1359/jbmr.090220. [DOI] [PubMed] [Google Scholar]
- 30.Wu F, Mason B, Horne A, Ames R, Clearwater J, Liu M, Evans MC, Gamble GD, Reid IR. Fractures between the ages of 20 and 50 years increase women’s risk of subsequent fractures. Arch Intern Med. 2002;162(1):33–6. doi: 10.1001/archinte.162.1.33. [DOI] [PubMed] [Google Scholar]
- 31.Lucas AR, Melton LJ, 3rd, Crowson CS, O’Fallon WM. Long-term fracture risk among women with anorexia nervosa: a population-based cohort study. Mayo Clin Proc. 1999;74(10):972–7. doi: 10.4065/74.10.972. [DOI] [PubMed] [Google Scholar]
- 32.Landin L, Nilsson BE. Bone mineral content in children with fractures. Clin Orthop Relat Res. 1983;(178):292–6. [PubMed] [Google Scholar]
- 33.Clark EM, Ness AR, Tobias JH. Bone fragility contributes to the risk of fracture in children, even after moderate and severe trauma. J Bone Miner Res. 2008;23(2):173–9. doi: 10.1359/jbmr.071010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mackey DC, Lui LY, Cawthon PM, Bauer DC, Nevitt MC, Cauley JA, Hillier TA, Lewis CE, Barrett-Connor E, Cummings SR. Study of Osteoporotic Fractures (SOF) and Osteoporotic Fractures in Men Study (MrOS) Research Groups. High-trauma fractures and low bone mineral density in older women and men. JAMA. 2007;298 (20):2381–8. doi: 10.1001/jama.298.20.2381. [DOI] [PubMed] [Google Scholar]
- 35.Wren TA, Shepherd JA, Kalkwarf HJ, Zemel BS, Lappe JM, Oberfield S, Dorey FJ, Winer KK, Gilsanz V. Racial disparity in fracture risk between white and nonwhite children in the United States. J Pediatr. 2012 Dec;161(6):1035–40. doi: 10.1016/j.jpeds.2012.07.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Melton LJ, 3rd, Kearns AE, Atkinson EJ, Bolander ME, Achenbach SJ, Huddleston JM, Therneau TM, Leibson CL. Secular trends in hip fracture incidence and recurrence. Osteoporos Int. 2009;20(5):687–94. doi: 10.1007/s00198-008-0742-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.van Staa TP, Dennison EM, Leufkens HG, Cooper C. Epidemiology of fractures in England and Wales. Bone. 2001;29(6):517–22. doi: 10.1016/s8756-3282(01)00614-7. [DOI] [PubMed] [Google Scholar]