Abstract
PURPOSE
To evaluate the three-dimensional changes in the position of the condyles, rami, and chin from 1 to 3 years after mandibular advancement surgery.
METHOD
This prospective observational study used pre and postoperative CBCT scans of 27 subjects with skeletal Class II jaw relationship and normal or deep overbite. An automatic technique of cranial base superimposition was used to assess positional and/or bone remodeling changes that were visually displayed and quantified using 3D color maps. An analysis of covariance with presence of genioplasty, age at the time of surgery, and sex as explanatory variables was used to estimate and test the adjusted mean changes for each region of interest.
RESULTS
The chin rotated downward and backwards between the 1 and 3 years post-surgery. Changes ≥ 2mm were observed in 17% of the cases. The mandibular condyles presented displacements and/or bone remodeling ≥ 2mm on the anterior surface (21% of the cases on the left and 13% on the right side), superior surfaces (8% on both sides) and lateral poles (17% on the left and 4% on the right side). The posterior borders of the rami exhibited symmetric lateral or rotational displacements in 4% of the cases.
CONCLUSION
In the hierarchy of surgical stability, mandibular advancement surgery is considered one of the most stable surgical procedures However, between 1 and 3 years post-surgery approximately 20% of the patients had 2-4 mm changes in the horizontal and vertical chin position, and/or changes in condylar position and adaptive bone remodeling.
INTRODUCTION
The construction of virtual 3D craniofacial surface models of patients has recently allowed scientific investigation of bone remodeling that leads to morphological changes. Registration of craniofacial surface models now enables the quantification and localization of the changes related to orthodontic/surgical protocols in the treatment of dentofacial disharmonies not readily apparent in 2D films.1
Over the last half century ortho-surgical treatment has been routinely used to address maxillamandibular discrepancies at skeletal maturity. Since the late 1950's2-6, stability of orthognathic surgery procedures has been well documented using 2D cephalometry and mandibular advancement surgery has been reported to be one of the most stable surgical procedures.6 Recent short-term studies, using CBCT for the 3D analysis of cranial and facial hard7-10 and soft11 tissues, have shown the regional remodeling that occurs in the first year after surgery.
While previous studies have quantified surgical displacements and short-term adaptation following mandibular advancement, the assessment of long-term results also are important.12-13 The purpose of this study was to analyze long-term 3D alterations in the rami, condyles and chin between one and three years after surgery in patients treated with mandibular advancement.
MATERIALS AND METHODS
The sample in this observational prospective study comprised 27 patients (18 female and 9 male) with an average age of 26.7 ± 13.2 years who received orthodontic treatment in preparation for mandibular advancement surgery. All mandibular advancements were performed using bilateral sagittal split osteotomy (BSSO) and rigid fixation with plates and screws.14-15 All patients were operated at the University of North Carolina (UNC) Memorial Hospital (North Carolina, USA) by a surgeon and assisting resident from the Department of Oral and Maxillofacial Surgery. The inclusion criteria consisted of pre-surgical Class II skeletal malocclusions with mandibular deficiency, 5-mm minimum overjet pre-surgery, and normal or increased overbite. The exclusion criteria were excessive anterior facial height, anterior open bite, and skeletal deformities from trauma, cleft lip and palate, syndromic or degenerative conditions, such as rheumatoid arthritis. The research protocol was approved by the Biomedical Institutional Review Board, and all of the participants signed an informed consent form.
The CBCT scans were performed before the surgery (T1), one year after the surgery (T2) and three years after the surgery (T3) with the NewTom 3G scanner (Aperio Services, Sarasota, FL). The imaging protocol involved a 36-second head exposure for a FOV corresponding to a 12 inch field of view. The patients maintained centric occlusion during the scan by biting on a wax bite. A trained radiology technician supervised the procedure.
The segmentation of the images of the anatomical structures of interest and the 3D model construction were performed using the ITK-SNAP open-source software (www.itksnap.org).16 The 3D models were constructed from CBCT images with a voxel dimension of 0.5 × 0.5 × 0.5 mm. These virtual models included the cranial base, maxilla and mandible (right and left condyles, right and left rami, body and symphysis) (Figure 1). A fully automated registration method for the superimposition of the models was performed with the IMAGINE open-source software (http://www.ia.unc.edu/dev/download/imagine/index.htm) that compares two images using the intensity of the gray scale for each voxel on the cranial base because this structure is not altered by surgery.8,17 The pre-surgical cranial base was used as a reference for superimposition of the one-year and three-year post-surgical images (Figure 2).
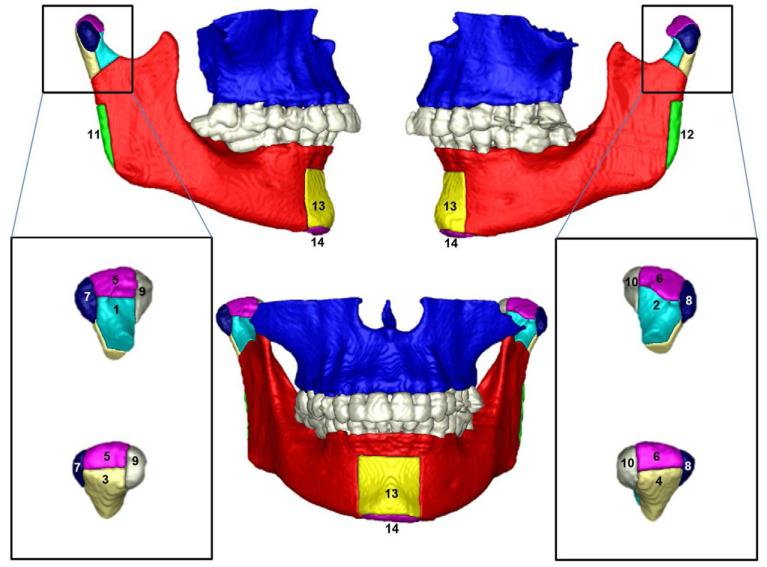
Figure 1.
Anatomic regions of interest: 1, right condyle anterior surface; 2, left condyle anterior surface; 3, right condyle posterior surface; 4, left condyle posterior surface; 5, right condyle superior surface; 6, left condyle superior surface; 7, right condyle lateral pole; 8, left condyle lateral pole; 9, right condyle medial pole; 10, left condyle medial pole; 11, right posterior border ramus; 12, left posterior border ramus; 13, anterior surface of the chin; and 14, inferior border of the mandible.
Figure 2.
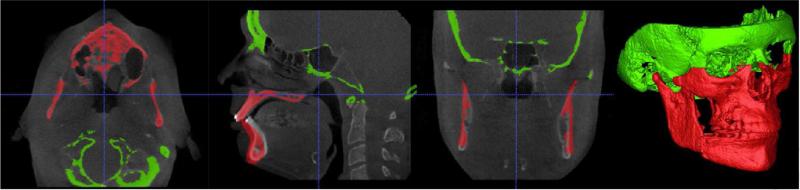
Example of the result of the superimposition on the cranial base where the pre-surgery grey level image and the surface model 1 year post-surgery are shown. Note the registration in the cranial base in the 3 planes of space as indicated by green.
After the registration steps, all reoriented virtual models, originally saved in an open source image file format (.gipl format), were converted to a 3D interchange file format (.iv format). This allowed quantitative evaluation of the greatest surface displacement by the CMF application software (developed at the M.E. Müller Institute for Surgical Technology and Biomechanics, University of Bern, Switzerland, under the funding of the Co-Me network, http://co-me.ch).18
The CMF software calculates thousands of color-coded point-to-point comparisons (surface distances in mm) between pre and 1-year post-surgery surface models (T1-T2), and between 1-year and 3-year post-surgery models (T2-T3, long-term surgical stability)(Figure 3), so that the difference between two surfaces at any location can be quantified.8 For quantitative assessment of the changes between the 3D surface models, the isoline tool was used. It allows the user to define a surface-distance value that is expressed as a contour line (isoline) that corresponds to regions having a surface distance equal to or greater than the defined value. The isoline tool was used to quantitatively measure the greatest displacements between points in the 3D surface models (in millimeters) at 14 specific anatomical areas: the (right and left) posterior condylar surfaces, the (right and left) medial condylar poles, the (right and left) anterior condylar surfaces, the (right and left) lateral condylar poles, the (right and left) superior condylar surfaces, the (right and left) posterior ramus borders, the anterior surface of the chin and the inferior border of the chin (Table I). The condylar lateral and medial poles were defined as tangents to the condylar neck, and the superior surface was defined as the articular surface separating the anterior and posterior condylar surfaces. The chin surfaces were limited bilaterally by tangents to the long axis of the canines.
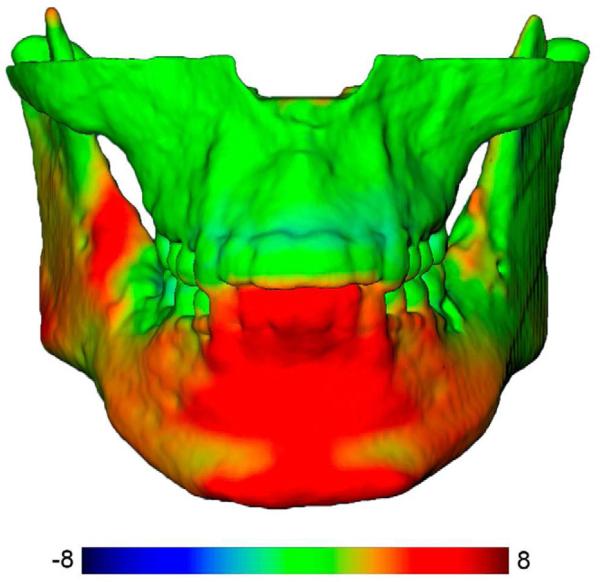
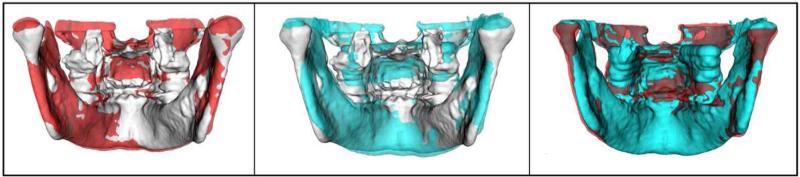
Figure 3.
Color-coded map of the surface distances between pre surgery and 1 year after mandibular advancement surgery. The virtual surface models were registered at the cranial base. Red represents the anterior displacement of the chin and inferior displacement of the inferior border of the mandible (color-code scale of −8 to +8 mm); green represents anatomic regions that did not present changes with treatment.
Table 1.
Descriptive statistics for the greatest displacement/and or bone remodeling at each anatomic region from presurgery to 1 year postsurgery and 1 year to 3 years postsurgery.
| Region | Presurgery to 1 Year postsurgery Mean +− SD (mm) | 1 Year to 3 Year postsurgery Mean +− SD (mm) |
|---|---|---|
| Ramus | ||
| Rt Posterior Border Ramus | −0.32 +− 2.56 | 0.39 +− 1.16 |
| Lf Posterior Border Ramus | −0.44 +− 3.02 | 0.18 +− 1.32 |
| Chin | ||
| Horizontal (anterior surface) | 5.48 +− 3.53 | −0.63 +− 1.33 |
| Vertical (inferior surface) | 5.53 +− 3.49 | 1.16 +− 1.03 |
| Condyle | ||
| Rt Posterior Surface | 1.27 +− 1.75 | 0.29 +− 0.99 |
| Lf Posterior Surface | 0.72 +− 1.28 | 0.15 +− 1.14 |
| Rt Medial Pole | 0.17 +− 1.63 | −0.26 +− 0.91 |
| Lf Medial Pole | 0.42 +− 1.50 | −0.11 +− 1.15 |
| Rt Anterior Surface | −1.50 +− 1.04 | −0.46 +− 1.27 |
| Lf Anterior Surface | −1.43 +− 1.61 | −0.34 +− 1.50 |
| Rt Lateral Pole | −0.61 +− 1.66 | 0.19 +− 1.02 |
| Lf Lateral Pole | −0.91 +− 1.80 | 0.26 +− 1.18 |
| Rt Superior surface | 0.95 +− 1.72 | 0.39 +− 1.26 |
| Lf Superior Surface | 0.48 +− 1.26 | 0.33 +− 1.14 |
Between the overlaid structures, the color-coded maps and isolines indicated inward displacement as blue and a negative value and outward displacement as red and a positive value. (Figure 3). An absence of change (0mm) was indicated by green. Displacements in the same direction are shown in different colors depending on the anatomic region.1 For example, displacements in an anterior direction are displayed as red positive values in the anterior surface of the chin and in the anterior surface of the condyles, but are displayed as blue negative values in the posterior surface of the ramus and condyles. Displacements in a posterior direction are displayed as blue negative values in the anterior surface of the chin and in the anterior surface of the condyles, but are displayed as red positive values in the posterior surface of the ramus and condyles. For the inferior border of the mandible, positive values represented an inferior displacement and negative values superior displacement. Due to the adaptive capacity of the condyles, red positive values represent displacement and/or bone apposition and blue negative values indicate displacement and/or bone resorption. Semitransparent overlays were also used for visualization of the location and direction of the skeletal displacements/bone remodeling, with one of the models in an opaque view superimposed onto another partially transparent view (Figures 6-9).
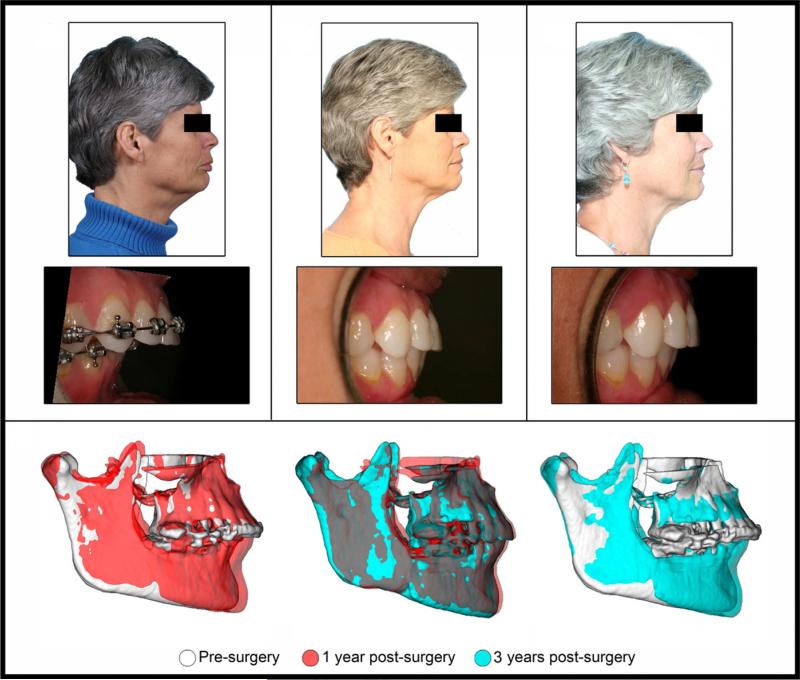
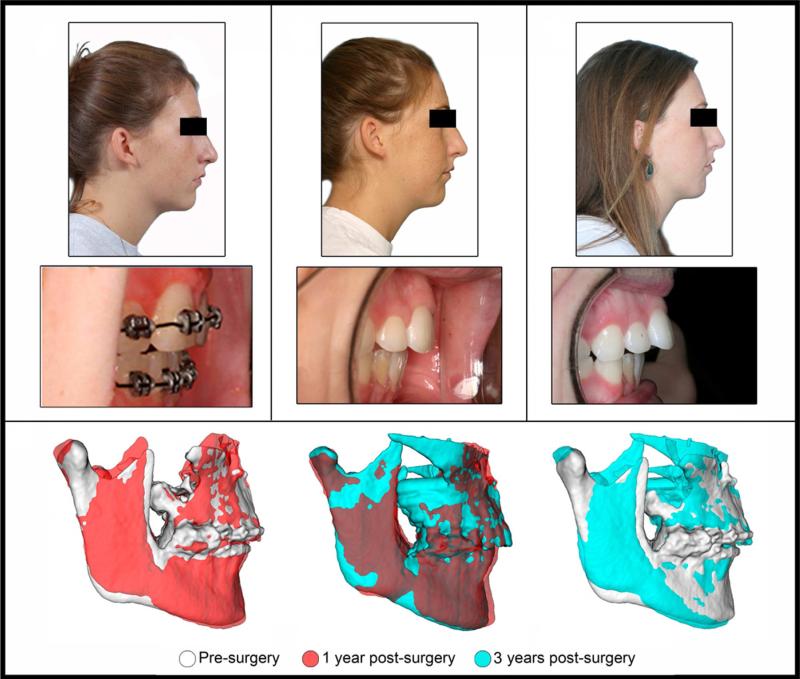
Figure 6.
Facial profile and intra-oral photos of patient who showed stability of the mandibular advancement when we compared pre-surgery, 1 year post-surgery and 3 years post-surgery 3D models. The bottom row shows lateral views of the semitransparency superimpositions. Note that small changes in chin position were observed between 1 and 3 years post-surgery, and the condylar position and morphology remained stable.
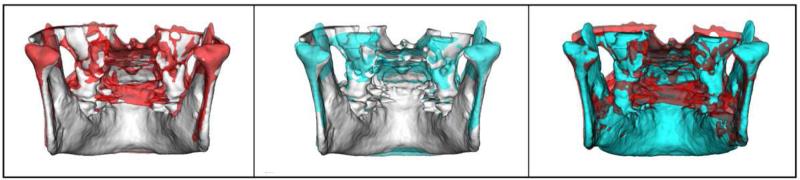
Figure 9.
Posterior view of semi-transparent superimpositions of patient in Fig. 7. Overlay of pre-surgery (white) and 1 year post-surgery (red) surface models shows superior displacement and bone remodeling of the condyles. Overlay of pre-surgery (white) and 3 years post-surgery (blue) surface models shows superior displacement and further bone remodeling of the condyles. Overlay of 1 year post-surgery (red) and 3 years post-surgery (blue) surface models shows the progression of bone remodeling in the condyles.
Statistical analysis
The reproducibility of the method was tested in 10 randomly selected superimpositions. The greatest displacement in each area was measured twice at 15-day intervals; the agreement between the repeated measures was assessed using intraclass correlation (ICC).
An analysis of covariance was performed for each anatomical area considering the presence of genioplasty, age at the time of surgery and gender as explanatory variables to estimate and test whether the average adjusted change from one to three years after surgery was 0. The level of significance was set at 0.05. The percentage of patients who exhibited positive or negative displacement greater than 2 mm at each region was calculated.
RESULTS
The agreement between the repeated measurements using the isoline tool was excellent, with ICCs above 0.99 in all of the anatomical areas of interest measurements.
Two-thirds of the subjects were female (67%). Forty percent of the subjects also had a genioplasty. The follow-up in years for Time 2 was 1.1 ± 0.2 and for Time 3 was 3.4 ± 0.4. The average changes from presurgery to 1 year postsurgery were smallest on the posterior border of the ramus and on the medial poles of the condyle. As expected, the average displacement was the largest for the chin (Table I). On average, smaller than .5mm changes between 1 and 3 year post-surgery occurred in almost all anatomic regions, and average changes in overbite was −0.1 ± 0.8mm and overjet was −0.5 ± 0.9mm. The largest average changes occurred on the anterior and inferior surface of the chin (Table I) even after adjusting for the presence of a genioplasty, age at the time of surgery, and gender (Table II). The small adjusted mean alterations observed in 13 out of the 14 areas of interest were not statistically different from zero. The inferior border of the mandible was the only area that had a statistically significant average change. The 1.11mm average change indicated an inferior displacement of the chin.
Table 2.
Adjusted mean change from 1 to 3 years post-surgery
| Region | adjusted mean +− SE (mm) | P value |
|---|---|---|
| Ramus | ||
| Rt Posterior Border Ramus | 0.38 +− 0.31 | 0.23 |
| Lf Posterior Border Ramus | 0.12 +− 0.34 | 0.72 |
| Chin | ||
| Horizontal (Anterior Surface ) | −0.42 +− 0.32 | 0.20 |
| Vertical (Inferior surface) | 1.11 +− 0.22 | <.0001 |
| Condyle | ||
| Rt Posterior Surface | 0.19 +− 0.26 | 0.47 |
| Lf Posterior Surface | 0.02 +− 0.28 | 0.95 |
| Rt Medial Pole | −0.19 +− 0.21 | 0.38 |
| Lf Medial Pole | −0.07 +− 0.30 | 0.81 |
| Rt Anterior Surface | −0.32 +− 0.33 | 0.34 |
| Lf Anterior Surface | −0.27 +− 0.33 | 0.43 |
| Rt Lateral Pole | 0.29 +− 0.25 | 0.27 |
| Lf Lateral Pole | 0.34 +− 0.30 | 0.26 |
| Rt Superior surface | 0.12 +− 0.29 | 0.70 |
| Lf Superior Surface | 0.19 +− 0.30 | 0.54 |
Virtually all patients had more than 2mm of anterior movement of the chin at 1 year postsurgery. Approximately 40% had more than 4mm anterior displacement of the anterior surface of the chin (Figure 4).
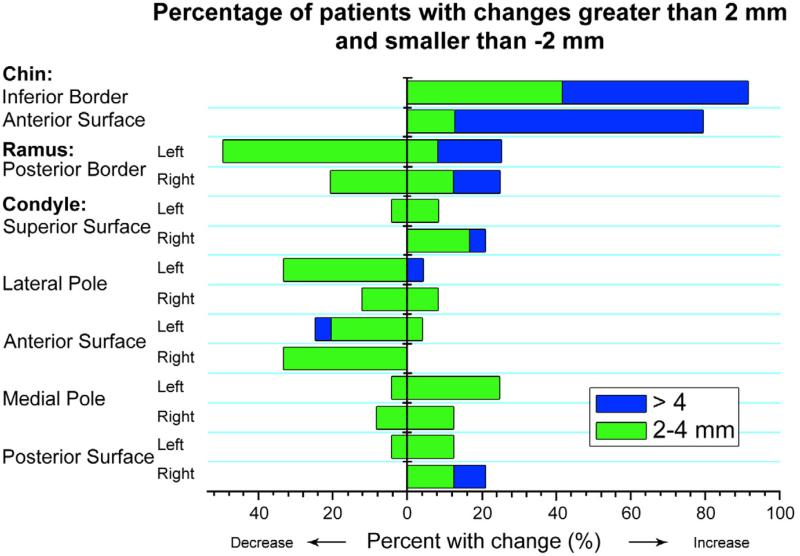
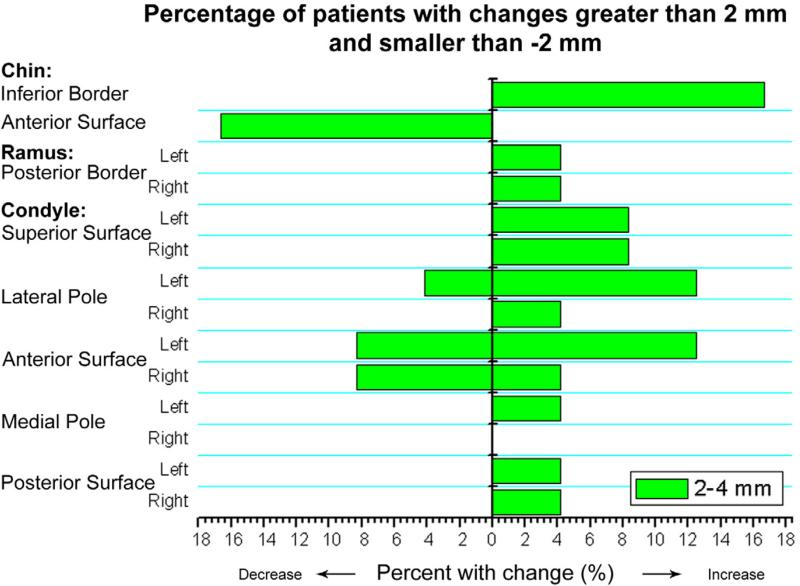
Figure 4.
Percentage of patients with changes greater than 2mm or less than −2mm for each of the anatomic regions of interest from presurgery to 1 year postsurgery. Patients with displacements between –2 and 2 mm are not represented. Note that positive or negative values of displacements represent different directional movements depending on the specific region of interest. Increase = anterior displacement for anterior surface of the chin and anterior surface of the condyles but posterior direction for posterior surface of the ramus and condyles; inferior displacement of the inferior border of the chin. Decrease = anterior displacement of posterior surface of the ramus and condyles; posterior direction in anterior surface of the chin and anterior surface of the condyles; superior displacement of the inferior border of the mandible.
The greatest long-term displacements and/or bone remodeling in the condylar areas occurred at the anterior surfaces (21% of the cases on the left side and 13% on the right side), superior surfaces (8% on both sides) and the lateral condylar poles (17% of the cases on the left side and 4% on the right side, Figure 5).
Figure 5.
Percentage of patients with changes greater than 2mm or less than −2mm between 1-year and 3-year follow-up. Patients with displacements between –2 and 2 mm are not represented. Note that positive or negative values of displacements represent different directional movements depending on the specific region of interest. Increase = anterior displacement for anterior surface of the chin and anterior surface of the condyles but posterior direction for posterior surface of the ramus and condyles; inferior displacement of the inferior border of the chin. Decrease = anterior displacement of posterior surface of the ramus and condyles; posterior direction in anterior surface of the chin and anterior surface of the condyles; superior displacement of the inferior border of the mandible.
Regarding changes in the chin area between 1 and 3 years post-surgery, 17% of the cases presented inferior displacement and 17% of the cases presented posterior displacement between 2 and 4 mm. Overbite changes greater than 1mm were noted for 17% of the cases and overjet changes greater than 1.5mm were noted for 17% of the cases. The posterior border of the ramus exhibited symmetric 4% displacement on both sides, with lateral or rotational long-term adaptation of the ramus (Figure 5).
DISCUSSION
A series of studies published since the 1990s based on the data of the Dentofacial Program of the University of North Carolina5-6,12-13,19-20 categorized the stability of orthognathic surgical procedures for different dentofacial disharmonies, utilizing 2D superimpositions or cephalometric measurements at different time points. Those studies provided parameters for orthodontists and oral-maxillofacial surgeons for decision-making in the treatment of skeletal malocclusions involving the maxilla and mandible. Proffit et al,20 in 2007, updated the hierarchy of orthognathic surgery stability with follow-up to five years after surgery and stressed the importance of the long-term assessment of surgical orthodontic procedures. The present study quantified the 3D surgical displacements and bone remodeling following mandibular advancement between one and three years after surgery.
A fully automated voxel-wise registration of the cranial base 3D superimposition has recently been applied to assess the stability of dental, skeletal and soft tissue alterations one year after jaw surgery. 1,7-12,17 The work of Carvalho et al10 and Motta et al1 cannot be directly compared to the present study, because 1/3 of the sample at 1 year follow up did not return for the long term assessments, and other patients have been recruited and added to the sample. The 3D image analysis methods in the present study have also focused on additional anatomic regions of interest to better evaluate local bone remodeling changes in the condylar surfaces and the inferior border of the mandible.
In these short-term studies1,10 the chin position varied between splint removal and 1 year post-surgery. Recorded changes indicated forward movement by 2 mm or more in five cases (19% ) and relapsed (displacement ≤ −2 mm) in seven cases (26%). In addition, the posterior border of the ramus exhibited 2 mm or more posterior displacement in six rami and anterior displacement in two (n=54). In the present study, 4 patients (17% of the cases) had ≥ 2mm downward rotation of the inferior border of the mandible and posterior displacement of the anterior surface of the chin, with partial relapse of the amount of mandibular advancement from 1 to 3 years after surgery. Overbite changes for these patients were >1mm and overjet changes were >1.5mm, as partial dental compensation occurred to the observed skeletal changes. Only 1 patient (4%) presented ≥2mm bilateral posterior rotation of the ramus during this time interval.
Carvalho et al.10 reported that, between the immediate post-surgical period and the 1 year follow up for 27 patients treated with mandibular advancement (54 condyles), 3 condyles exhibited ≥2 mm anterior-inferior displacement and 6 condyles had posterior-superior displacement. The present study has shown that small condylar changes continue to occur beyond the first year post-surgery with variable direction of changes: between 1 and 3 years post-surgery follow-up of 24 patients (48 condyles), 4 condyles presented ≥ 2mm changes indicative of anterior displacements and/or bone apposition and 4 condyles had ≤−2mm indicative of posterior displacements and/or bone resorption in the anterior surface of the condyle. Four condyles also presented ≥ 2mm superior displacement as shown in the patient in Figures 7 and 9, and 4 condyles presented ≥ 2mm lateral displacements and/or bone apposition in the lateral poles, leading to changes in condylar torque relative to the ramus.
Figure 7.
Facial profile and intra-oral photos of patient who showed stability of the mandibular advancement when we compared pre-surgery, 1 year post-surgery and 3 years post-surgery. The bottom row shows lateral views of the skeletal semitransparency superimpositions of same patient. Note that at 1 year post-surgery the chin advancement had returned to its original position. Between 1 year and 3 years post-surgery the downward and backward displacement of the mandible progressed, compromising the surgical outcome.
In summary, the results of the present study indicate that, over the three-year-period, mandibular advancement surgery was, on average, stable, which corroborates previous studies’ findings.5-6, 20-22 However, ≥2 mm downward and backward rotation of the chin, as well as condylar displacement and/or remodeling adaptive changes were observed in 17% of the patients. Previous studies23-28 have questioned whether condylar displacements or remodeling after orthognathic surgery might cause temporomandibular disorders (TMD) or relapse-related displacements. Draenert et al.29 emphasized that, although the condylar position might change after surgery, the treatment results do not alter the clinical characteristics of the temporomandibular joints although symptoms might worsen in patients already exhibiting TMD before surgery.
The 3D analysis of CBCTs in this study gives additional information regarding bone remodeling and positional changes following mandibular advancement compared to traditional cephalometric methods. In this study, to measure distances between the bone surfaces at 2 time points, the closest surface point method was used. Current open source and commercially available software (such as Geomagic Studio, Geomagic U.S. Corp, Research Triangle Park, NC, and Vultus, 3dMD, Atlanta, GA) calculate the closest points between 2 surfaces that were displaced with treatment. Quantification of surface distances by using closest points requires careful interpretation and comparisons with the semi-transparent overlays to determine areas of bone remodeling versus displacement (Figures 8 and 9), since closest point distances do not quantify vectorial magnitudes of 3D displacements and the closest points might not be homologous in both surfaces. For this reason, when changes over time are of interest, quantification with isolines provides absolute positive or negative values of displacements and aids assessment of the direction of displacement.
Figure 8.
Posterior view of semi-transparent superimpositions of patient in Fig. 6. Overlays of pre-surgery (white), 1 year post-surgery (red) and 3 years post-surgery (blue) surface models are shown. Note the stability of condylar position and morphology in the long-term follow up.
CONCLUSION
The present study indicates that from one to three years after surgery approximately one out of six patients who have mandibular advancement surgery will experience clinical changes (2 to 4mm) in the horizontal and vertical chin position. On average, small changes will occur in condylar position and adaptive bone remodeling.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Motta AT, Cevidanes LH, Carvalho FA, Almeida MA, Phillips C. Three-dimensional regional displacements after mandibular advancement surgery: one year of follow-up. J Oral Maxillofac Surg. 2011;69(5):1447–57. doi: 10.1016/j.joms.2010.07.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Trauner R, Obwegeser H. The surgical correction of mandibular prognathism and retrognathia with consideration of genioplasty. I. Surgical procedures to correct mandibular prognathism and reshaping of the chin. Oral Surg. Oral Med. Oral Pathol. 1957;10(7):677–89. doi: 10.1016/s0030-4220(57)80063-2. [DOI] [PubMed] [Google Scholar]
- 3.Dal Pont G. Retromolar osteotomy for the correction of prognathism. J Oral Surg Anesth Hosp Dent Serv. 1961;19:42–7. [PubMed] [Google Scholar]
- 4.Proffit WR, Phillips C, Douvartzidis N. A comparison of outcomes of orthodontic and surgical-orthodontic treatment of Class II malocclusion in adults. Am J Orthod Dentofacial Orthop. 1992;101(6):556–65. doi: 10.1016/0889-5406(92)70131-S. [DOI] [PubMed] [Google Scholar]
- 5.Proffit WR, Turvey TA, Phillips C. Orthognathic surgery: a hierarchy of stability. Int J Adult Orthodon Orthognath Surg. 1996;11(3):191–204. [PubMed] [Google Scholar]
- 6.Bailey LJ, Proffit WR, White R., Jr Assessment of patients for orthognathic surgery. Semin Orthod. 1999;5(4):209–22. doi: 10.1016/s1073-8746(99)80015-2. [DOI] [PubMed] [Google Scholar]
- 7.Cevidanes LH, Bailey LJ, Tucker SF, Styner MA, Mol A, Phillips CL, Proffit WR, Turvey T. Three-dimensional cone-beam computed tomography for assessment of mandibular changes after orthognathic surgery. Am J Orthod Dentofacial Orthop. 2007;131(1):44–50. doi: 10.1016/j.ajodo.2005.03.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cevidanes LH, Oliveira AE, Grauer D, Styner M, Proffit WR. Clinical application of 3D imaging for assessment of treatment outcomes. Semin Orthod. 2011;17(1):72–80. doi: 10.1053/j.sodo.2010.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cevidanes LH, Franco AA, Gerig G, Proffit WR, Slice DE, Enlow DH, Yamashita HK, Kim YJ, Scanavini MA, Vigorito JW. Assessment of mandibular growth and response to orthopedic treatment with 3-dimensional magnetic resonance images. Am J Orthod Dentofacial Orthop. 2005;128(1):16–26. doi: 10.1016/j.ajodo.2004.03.032. [DOI] [PubMed] [Google Scholar]
- 10.Carvalho Fde A, Cevidanes LH, da Motta AT, Almeida MA, Phillips C. Three-dimensional assessment of mandibular advancement 1 year after surgery. Am J Orthod Dentofacial Orthop. 2010 Apr;137(4 Suppl):S53, e1–12. doi: 10.1016/j.ajodo.2010.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Almeida RC, Cevidanes LH, Carvalho FA, Motta AT, Almeida MA, Styner M, Turvey T, Proffit WR, Phillips C. Soft tissue response to mandibular advancement using 3D CBCT scanning. Int J Oral Maxillofac Surg. 2011;40(4):353–9. doi: 10.1016/j.ijom.2010.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bailey LJ, Cevidanes LH, Proffit WR. Stability and predictability of orthognathic surgery. Am J Orthod Dentofacial Orthop. 2004;126(3):273–7. doi: 10.1016/S0889540604005207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Proffit WR, Phillips C, Turvey TA. Long-term stability of adolescent versus adult surgery for treatment of mandibular deficiency. Int J Oral Maxillofac Surg. 2010;39(4):327–32. doi: 10.1016/j.ijom.2010.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Epker BN. Modifications in the sagittal osteotomy of the mandible. J Oral Surg. 1977;35(2):157–9. [PubMed] [Google Scholar]
- 15.Bell WH, Jacobs JD. Combined orthodontic-surgical correction of moderate mandibular deficiency. Am J Orthod. 1979;75(5):481–506. doi: 10.1016/0002-9416(79)90068-x. [DOI] [PubMed] [Google Scholar]
- 16.Yushkevich PA, Piven J, Hazlett HC, Smith RG, Ho S, Gee JC, Gerig G. User-guided 3D active contour segmentation of anatomical structures: significantly improved efficiency and reliability. Neuroimage. 2006;31(3):1116–28. doi: 10.1016/j.neuroimage.2006.01.015. [DOI] [PubMed] [Google Scholar]
- 17.Cevidanes LH, Styner MA, Proffit WR. Image analysis and superimposition of 3-dimensional cone-beam computed tomography models. Am J Orthod Dentofacial Orthop. 2006;129(5):611–8. doi: 10.1016/j.ajodo.2005.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chapuis J, Schramm A, Pappas I, Hallermann W, Schwenzer-Zimmerer K, Langlotz F, Caversaccio M. A new system for computer-aided preoperative planning and intraoperative navigation during corrective jaw surgery. IEEE Trans Inf Technol Biomed. May. 2007;11(3):274–87. doi: 10.1109/titb.2006.884372. [DOI] [PubMed] [Google Scholar]
- 19.Simmons KE, Turvey TA, Phillips C, Proffit WR. Surgical-orthodontic correction of mandibular deficiency: five-year follow-up. Int J Adult Orthodon Orthognath Surg. 1992;7(2):67–79. [PubMed] [Google Scholar]
- 20.Proffit WR, Turvey TA, Phillips C. The hierarchy of stability and predictability in orthognathic surgery with rigid fixation: an update and extension. Head Face Med. 2007;3:21. doi: 10.1186/1746-160X-3-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Miguel JA, Turvey TA, Phillips C, Proffit WR. Long-term stability of two-jaw surgery for treatment of mandibular deficiency and vertical maxillary excess. Int J Adult Orthodon Orthognath Surg. 1995;10(4):235–45. [PubMed] [Google Scholar]
- 22.Watzke IM, Turvey TA, Phillips C, Proffit WR. Stability of mandibular advancement by sagittal osteotomy with screw and wire fixation: A comparative study. J Oral Maxillofac Surg. 1990;48(2):108–121. doi: 10.1016/s0278-2391(10)80197-1. [DOI] [PubMed] [Google Scholar]
- 23.Ow A, Cheung LK. Bilateral sagittal split osteotomies versus mandibular distraction osteogenesis: a prospective clinical trial comparing inferior alveolar nerve function and complications. Int J Oral Maxillofac Surg. 2010;39(8):756–60. doi: 10.1016/j.ijom.2010.04.001. [DOI] [PubMed] [Google Scholar]
- 24.Ow A, Cheung LK. Bilateral sagittal split osteotomies and mandibular distraction osteogenesis: a randomized controlled trial comparing skeletal stability. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109(1):17–23. doi: 10.1016/j.tripleo.2009.07.030. [DOI] [PubMed] [Google Scholar]
- 25.De Clercq CA, Neyt LF, Mommaerts MY, Abeloos JV, De Mot BM. Condylar resorption in orthognathic surgery: a retrospective study. Int J Adult Orthodon Orthognath Surg. 1994;9(3):233–40. [PubMed] [Google Scholar]
- 26.Hwang SJ, Haers PE, Zimmermann A, Oechslin C, Seifert B, Sailer HF. Surgical risk factors for condylar resorption after orthognathic surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;89(5):542–52. doi: 10.1067/moe.2000.105239. [DOI] [PubMed] [Google Scholar]
- 27.You MS, Yang HJ, Hwang SJ. Postoperative functional remodeling of preoperative idiopathic condylar resorption: a case report. J Oral Maxillofac Surg. 2011;69(4):1056–63. doi: 10.1016/j.joms.2010.01.012. [DOI] [PubMed] [Google Scholar]
- 28.Kobayashi T, Izumi N, Kojima T, Sakagami N, Saito I, Saito C. Progressive condylar resorption after mandibular advancement. Br J Oral Maxillofac Surg. 2011;50(2):176–80. doi: 10.1016/j.bjoms.2011.02.006. [DOI] [PubMed] [Google Scholar]
- 29.Draenert FG, Erbe C, Zenglein V, Kämmerer PW, Wriedt S, Al Nawas B. 3D analysis of condylar position after sagittal split osteotomy of the mandible in mono and bimaxillary orthognathic surgery - a methodology study in 18 patients. J Orofac Orthop. Nov. 2010;71(6):421–9. doi: 10.1007/s00056-010-1021-9. [DOI] [PubMed] [Google Scholar]