Abstract
There has been rapidly increasing interest over the past decade in the potential of mindfulness-based approaches to psychological and medical treatment, including a recent growth in the area of substance abuse. Thus, the relationship between trait mindfulness and substance use has been explored in several studies. Results, however, have been mixed. While several studies of college student populations have evinced positive correlations between levels of trait mindfulness and substance use, the opposite seems to be true in clinical samples, with multiple studies showing a negative association. The current study reviews research in both non-treatment seeking college students and in clinical samples, and examines the relationship between trait mindfulness and substance dependence in a clinical sample (N = 281). Further, the study assesses the moderating effect of avoidant coping that might explain the disparate findings in the clinical versus nonclinical samples.
Keywords: addiction, mindfulness, substance use, avoidance, coping
1. Introduction
Mindfulness has been described as intentional direction of attention toward experience as it arises in the present moment, characterized by a non-judgmental, open receptivity toward all phenomena (Bishop et al., 2004). Several studies have shown that an individual’s level of mindfulness can be increased through mindfulness and meditation training (e.g., Bowen et al., 2009; Carmody & Baer, 2008). However, mindfulness can also be measured as a dispositional, naturally occurring trait, by assessing the extent to which individuals tend towards awareness and sustained attention to what is presently occurring, in the context of their everyday lives (Brown & Ryan, 2003).
Training to enhance mindfulness can be traced back thousands of years to Buddhist traditions, in which mindfulness practices form the foundation for transforming psychological suffering into healthier states of mind (Hanh, 1999). More recently, clinical trials have examined contemporary treatments integrating mindfulness-based approaches and practices for myriad clinical issues including chronic pain (Kabat-Zinn et al., 1992; Rosenzweig et al., 2010), anxiety (Hofmann, Sawyer, Witt, & Oh, 2010; Kabat-Zinn et al., 1992), depression (Hofmann et al., 2010; Segal et al., 2012), and substance use disorders (see Zgierska et al., 2009, for review).
Research on mechanisms by which these treatments affect change, however, is still in relatively early stages (Baer, 2003; Carmody & Baer, 2008; Hölzel et al., 2011). Arguably, these mechanisms involve improvements in mindfulness, or the ability to bring nonjudgmental awareness to the present moment, therefore allowing more skillful responding to distressing emotional states or behavioral impulses (Bishop et al., 2004). Indeed, several studies have found increases in measures of mindfulness following such interventions (e.g., Bowen et al., 2009; Carmody & Baer, 2008; Carmody, Reed, Kristeller, & Merriam, 2008), and a subset of these have found mindfulness to be a significant mediating factor between mindfulness training and clinical outcomes (McCracken, Gauntlett-Gilbert, & Vowles, 2007; Zgierska et al., 2009; Carmody, Baer, Lykins, & Olendzki, 2009).
1.1 Mindfulness and substance use
Within the field of addictive behaviors, a growing number of studies have assessed efficacy of mindfulness-based interventions for problematic substance use (see Chiesa & Serretti, 2013 for review), and studies to date suggest several possible mechanisms. Neurobiological mechanisms in areas associated with craving, negative affect, and substance use relapse may be affected by mindfulness training (Witkiewitz, Lustyk, & Bowen, 2012), altering basic neurobiological processes related to reactive behaviors (Brewer, Elwafi, & Davis, 2012). Data from clinical trials likewise suggest mindfulness training may lead to decreases in self-reported severity of factors related to relapse such as anxiety, depression, and stress (e.g., Zgierska et al., 2009), decreases in both craving (e.g., Bowen et al., 2009; Brewer et al., 2012; Garland et al., 2012; Zgierska et al., 2009) and reactivity to craving (e.g., Bowen & Marlatt, 2009), and an improved ability to decouple the drinking impulse from drinking behavior (Ostafin, Bauer, & Myxter, 2012). Similarly, a study by Garland et al. (2010) found mindfulness training significantly reduced stress and thought suppression, and decreased physiological reactivity to alcohol cues and heart rate variability recovery time after cue-exposure, all of which have been linked to alcohol dependence.
1.2 Mixed findings in the relationship between trait mindfulness and substance use
Given the presumed intentions of mindfulness-based treatment for substance use disorders, i.e., increasing levels of mindfulness, and the growing evidence in support of salutary effects (decreased craving, substance use, and relapse), a baseline negative association between trait mindfulness and substance abuse might be expected. However, a handful of cross-sectional studies examining this hypothesis have found otherwise. One study evaluating spirituality, mindfulness, and substance use in a non-treatment seeking college-age sample (Leigh, Bowen, & Marlatt, 2005) found that mindfulness as measured by the Freiburg Mindfulness Inventory (FMI; Buccheld, Grossman, & Walach, 2002) and heavy substance use were positively correlated. A later investigation (Leigh & Neighbors, 2009) in a sample of non-treatment seeking college-age students similarly discovered a positive association between acting with awareness (a subscale of the FMI) and alcohol use.
Other studies have attempted to clarify these findings using the Five Factors of Mindfulness Questionnaire (FFMQ), developed through a factor analytic study of previous mindfulness measures (Baer, Smith, Hopkins, Krietemeyer, & Toney, 2006). The FFMQ is a reliable and empirically validated 39-item measure which assesses five proposed facets of mindfulness (describing experience, observing experience, being nonjudgmental of experience, being nonreactive toward experience, and acting with awareness). Hypothesizing that mindfulness may be most accurately measured as a multifaceted construct with potentially interacting factors relating differently to substance use outcomes, studies have assessed effects of interactions between factors on substance use. For example, a recent study (Fernandez, Wood, Stein, & Rossi, 2010) investigated the relationship between mindfulness, alcohol use, and alcohol related consequences in non-treatment seeking college-aged students, and found a significant negative relationship between two awareness-based factors (describing, acting with awareness) and alcohol use. A later study, also in a non-treatment seeking college student population (Eisenlohr-Moul, Walsh, Charnigo, Lynam, & Baer, 2012), tested the hypothesis that particular aspects of mindfulness (as measured by FFMQ subscales) interact with one another to moderate substance use. After controlling for personality, results revealed a significant interaction effect of the observing and nonreactivity to inner experience subscales on substance use, such that when non-reactivity was high, the observing subscale was negatively associated with substance use, but when non-reactivity was low, observing was positively associated with substance use. This suggests that for individuals who observe in a non-reactive manner, observation may relate to lower levels of substance use. Conversely, if observing is coupled with higher levels of reactivity, it may be more positively associated with substance use. Findings highlight the value of investigating the interrelation between subscales within the FFMQ, and the potential for interaction effects to reveal nuances that may be lost when evaluating overall scores or even individual subscales.
The majority of cross-sectional studies examining relationships between trait mindfulness and substance use, as described above, have been conducted in non-treatment-seeking college students with predominantly subclinical levels of use. However, higher levels of substance use dependence may be worthy of consideration in assessing this relationship. Indeed, studies assessing the relationship between trait mindfulness and substance use in clinical samples, in which individuals are likely to be substance dependent, have yielded an inverse relationship between these factors. For example, a recent study (Garland, Boettiger, Gaylord, Chanon, & Howard, 2012) found a significant inverse relationship between trait mindfulness and substance craving in a clinical sample in early abstinence, mediated by both negative affect and reappraisal, two factors strongly linked to relapse. Similarly, a study evaluating baseline levels of mindfulness in a treatment-seeking population (Dakwar, Mariani, & Levin, 2011), compared the mean level of trait mindfulness in the study sample to the mean in a large national non-treatment-seeking adult sample. Levels in the treatment-seeking population were below the national mean, and were inversely related to substance use.
1.3 Current study
The current study was designed to identify factors that might further clarify the discrepant findings in college student samples, where alcohol use is considered a normative behavior (Gire, 2002), versus in clinical samples. Motives have consistently been identified as predictive of substance use behaviors (Mares et al., 2013). Findings from a recent review of the youth substance use and motives literature (Kuntsche, Knibbe, Gmel & Engels, 2005) indicate that substance use in a non-clinical youth population was most strongly related to social and enhancement motives (Schelleman-Offermans, Kuntsche & Knibbe, 2011). As substance use progresses to clinical levels, however, motivates may shift to using substances as a coping method rather than social or enhancement motives (Gonzalez & Skewes, 2013; Moos, Brennan, Fondacaro, & Moos, 1990; WHO, 2004).
Motives for using substances may thus be an important factor in the relationship between mindfulness and substance use. Specifically, avoidance-based coping has been hypothesized to play an important role in the self-medication model, according to which individuals begin with experimental consumption, and learn, through repeated use, to expect relief from affective suffering through avoidance of distressing states (Khantzian, 2003). Indeed, avoidance-based coping has been consistently identified as a moderator of problematic alcohol and other substance use (Cooper, Russell, Skinner, Frone, & Mudar, 1992; Hruska, Fallon, Spoonster, Sledjeski, & Delahanty, 2011). Individuals with problematic substance use may develop a reliance on avoidant coping, and repeated negative reinforcement may provide a conditioned compulsion toward avoidance of distressing experiences through use of substances that may be preconscious, and be experienced as craving (Baker et al., 2004). Increased mindfulness may attenuate the link between negative affect and craving, indicating that training in mindfulness may enable an individual to respond skillfully rather than reactively to substance craving (Witkiewitz & Bowen, 2010).
The current study examined the function of substance use and its interaction with trait mindfulness in a clinical treatment-seeking adult population with substance use disorders. Avoidant coping was assessed as a moderating factor in the relationship between mindfulness and substance use, with the hypothesis that individuals higher in avoidant coping would evince a stronger negative relationship between mindfulness and severity of substance dependence. Dependence severity was used as a primary variable, versus quantity/frequency measures of use, due to the inconsistency of conditions prior to baseline assessment across the sample. For example, a significant proportion of participants had recently been released from inpatient treatment or incarceration and thus had constraints that severely limited access to or use of substances. Severity of dependence, therefore, may more accurately reflect the role of substance use in the individual’s life.
Specifically, the aims of the current study were to: 1) assess the overall relationship between mindfulness and severity of substance dependence, hypothesizing a negative relationship between mindfulness and dependence severity in a clinical sample, 2) examine relationships between FFMQ subscales and dependence severity, hypothesizing negative associations between dependence severity and both nonreactivity and nonjudgment, 3) test the interaction effect of observing and nonreactivity on dependence severity, hypothesizing that similar to results from previous research (Eisenlohr-Moul et al., 2012), higher levels of reactivity would moderate the effect of observing on substance use outcomes, and 4) test the interaction effect of avoidant coping, as measure by the Coping Responses Inventory subscale (Moos, 1997) and mindfulness on dependence severity, with the hypothesis that individuals higher in avoidant coping will evince a stronger negative relationship between mindfulness and severity of dependence.
2. Methods
2.1 Sample
The current study is a secondary analyses of baseline data from a trial assessing outcomes of a mindfulness-based relapse prevention program (Bowen, Chawla, & Marlatt, 2010) in comparison to cognitive behavioral treatment and standard care. The parent study from which the data were drawn was conducted in an adult outpatient substance abuse treatment program. Participants (N = 281) had recently completed inpatient or intensive outpatient treatment and were transitioning into aftercare (see Bowen et al., in press, for full description). Current data are drawn from the baseline assessment, conducted prior to study randomization. (See Table 1 for participant characteristics.)
Table 1.
Baseline Demographics and Substance Use (N=281)
| Variable | N | (%) |
|---|---|---|
| Sex | ||
| Male | 201 | (61.5) |
| Female | 79 | (28.1) |
| Other | 1 | (0.4) |
| Race | ||
| Asian | 2 | (0.7) |
| Black/African-American | 61 | (21.6) |
| Hawaiian/Pacific Islander | 2 | (0.7) |
| Hispanic or Latino | 22 | (7.8) |
| Native American | 18 | (6.4) |
| White/Caucasian | 146 | (51.6) |
| Other | 5 | (1.8) |
| Mixed | 27 | (9.5) |
| Substance of Choice | ||
| Alcohol | 140 | (49.1) |
| Crack cocaine | 36 | (12.6) |
| Powder cocaine | 6 | (2.1) |
| Marijuana | 27 | (9.5) |
| Methamphetamine | 34 | (11.9) |
| Heroin | 27 | (9.5) |
| Other opiates | 13 | (4.6) |
| Other | 2 | (0.7) |
| Variable | Mean + SD |
|---|---|
| Age | 38.44 + 10.92 |
| Severity of Dependence | 9.43 + 4.18 |
| Avoidant Coping | 43.12 + 10.06 |
| FFMQ | |
| Total | 3.38 + .45 |
| Awareness | 3.37 + .8 |
| Observe | 3.29 + .81 |
| Describe | 3.39 + .71 |
| Nonreact | 3.18 + .62 |
| Nonjudgment | 3.69 + .85 |
Note. FFMQ = Five Factor Mindfulness Questionnaire
2.2 Measures
Demographic information such as age, race/ethnicity and gender was collected at baseline. Mindfulness was assessed using the total scores and subscales of the 39-item five-point Likert scale Five Factor Mindfulness Questionnaire (FFMQ; (Baer et al., 2006)). Subscales include Acting with Awareness (α = .86), Observing (α = .84), Describing (α = .84), and Nonjudgment (α = .84), each of which are made up of eight items, while the fifth subscale, Nonreactivity (α = .72), contains seven items. Internal consistency for the total scale was α = .86. Substance use was measured using the Severity of Dependence Scale (SDS; (Gossop, Darke, Griffiths, & Hando, 1995), a five-item, four-point Likert scale assessment. Internal consistency was α = .86. The 24-item Avoidant Coping subscale of the Coping Responses Inventory – Adult Form (CRI; (Moos, 1997) measured avoidant coping responses used in stressful situations, using a five-point Likert scale. Internal consistency of the subscale in the present study was α = .73.
2.3 Analyses
Moderated regression analyses were used to assess the relationships between mindfulness and substance dependence severity. In step 1, to control for potential confounds of age and gender on severity of dependence (Bischof, Rumpf, Meyer, Hapke, & John, 2005; Stevens, Andrade, & Ruiz, 2009), severity of dependence was regressed onto the covariate variables of age and gender. Predictor variables were then entered in steps 2 and 3, and product variables in step 4. All continuous predictors were standardized prior to use in regression models. The interaction effect between avoidant coping and mindfulness on dependence severity was subsequently probed by regressing the outcome (dependence severity) onto the predictor (mindfulness) for each of two groups, representing two levels of the dichotomized moderator (i.e., high and low avoidant coping) (Aiken & West, 1991). All analyses were performed using SPSS 13.
3. Results
Data were examined for outliers and normality of distribution and were found to be within acceptable range. Mean values on primary variables can be found in Table 1. Statistics for all analyses are displayed in Table 2.
Table 2.
Summary of Multiple Regression Analysis for Variables Predicting Severity of Dependence Scores, Controlling for Age and Gender (N=281)
| Predictor | B | SE B | β |
|---|---|---|---|
| FFMQ | |||
| Total Score | −2.36 | .54 | −.25*** |
| Observe | .04 | .32 | .008 |
| Aware | −1.77 | .30 | −.33*** |
| Describe | −.98 | .34 | −.17** |
| Nonjudgment | −1.34 | .29 | −.27*** |
| Nonreact | .27 | .42 | .038 |
| Observe X Nonreact | −.24 | .44 | −.03 |
| Avoidant Coping | .07 | .03 | .16* |
| Avoidant Coping X FFMQ total | −.12 | .06 | −.13* |
Note. FFMQ = Five Factor Mindfulness Questionnaire
p < .05.
p < .01.
p < .001.
The first analysis assessed the relationship between total scores on the FFMQ and the SDS, revealing a significant negative relationship. Secondly, in examining the relationship between the five subfactors of the FFMQ and dependence the SDS, significant relationships were found between acting with awareness, describing, and nonjudgment and the SDS. However, the observing and nonreactivity subscales were not significantly related to SDS.
Finally, two moderating hypotheses were tested using moderated regression analyses, with mean centered interaction variables. Interaction effects of observing-by-nonreactivity on SDS scores were nonsignificant. Analyses of an interaction of avoidant coping and FFMQ total score on SDS revealed a significant moderating effect, such that individuals with higher avoidant coping had a stronger negative relationship between mindfulness and severity of dependence. As shown in Figure 1, probing the moderation effect indicated that individuals lower in avoidant coping did not evince the strong, negative association between mindfulness and dependence severity (β= −.170, p = 081) that was present for individuals higher in avoidant coping (β = −.261, p = 003).
Figure 1.
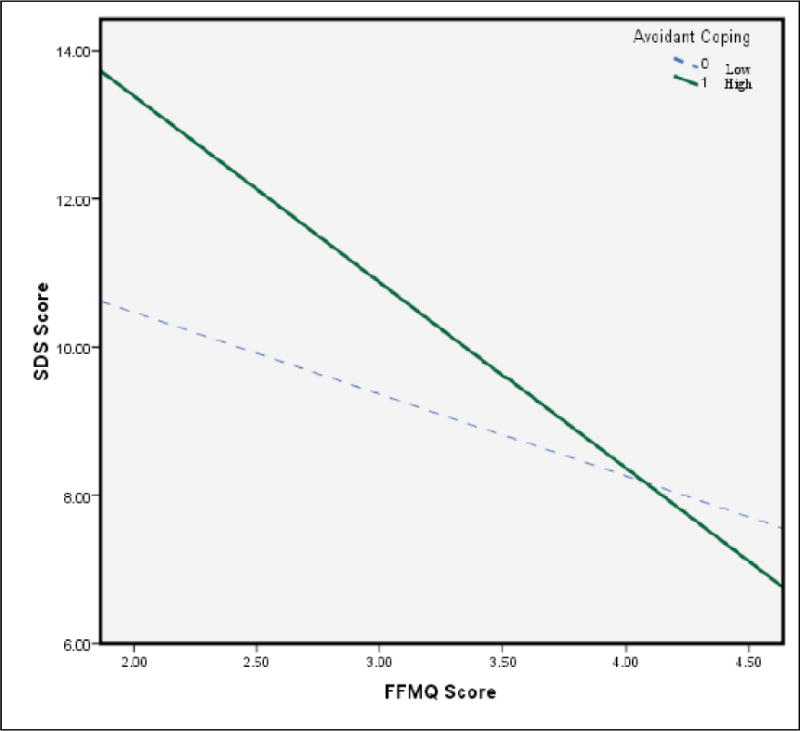
Relationship between mindfulness and severity of dependence in low versus high levels of avoidant coping.
Note. SDS = Severity of Dependence Scale; FFMQ = Five Factor Mindfulness Scale.
4. Discussion
This cross-sectional study of an adult treatment-seeking population provides further evidence of a significant relationship between factors of trait mindfulness and substance use in a clinical population. The present study investigated the relationship between self-reported trait mindfulness and substance use related problems in a treatment-seeking, as opposed to a college student population.
The study had several aims. First, analyses assessed the relationship between trait mindfulness, and facets thereof, and severity of substance dependence in an adult clinical population, in an effort to provide further data on this relationship in clinical versus non-clinical populations. Similar to the previously discussed prior studies in clinical samples, results suggested a negative relationship between mindfulness and severity of dependence in treatment-seeking adults with substance use disorders. In further analyses of the subscales of the mindfulness measure, significant negative relationships were found between substance dependence severity and the FFMQ subscales acting with awareness, describing, and nonjudgment.
Next, the study attempted to replicate the interaction effect in previous research (Eisenlohr-Moul et al., 2012) between the observing and nonjudgment subscales, suggesting that it may not only the observation of experience, but the relationship to the experience (i.e., reactive versus non) that is an important factor regarding the relationship of mindfulness to substance use. The current data failed to evince a significant effect of this interaction on dependence severity. This is a curious finding, for which there are several possible explanations. It may simply be artifactual, or could be a function of the different substance use outcome measures used in the two studies. Alternatively, it could indicate a true absence of this moderating relationship in a clinical sample versus in college students. The latter possibility is interesting, and may be due to the greater intractability of reactive cognitive and behavioral patterns in a clinical population, decreasing the potential influence of higher levels of observation of experience on reactivity.
The current study also attempted to replicate the negative relationship between both describing and acting with awareness and alcohol use reported in previous literature (Fernandez et al., 2010). The current study indeed evinced similar findings, and found an additional negative relationship between nonjudgment and substance dependence.
Finally, as hypothesized, the current study revealed a moderating effect of avoidant coping on the relationship between the overall mindfulness score and severity of substance dependence, such that that those higher in avoidance coping had a stronger negative relationship between mindfulness and severity of dependence. This moderating effect suggests that for individuals using substances to avoid challenging experiences (with answer choices such as, “try to forget the whole thing”), mindfulness may be a protective factor, with higher levels of mindfulness relating to less severe substance dependence. In contradistinction, individuals in a college student sample may be using substances for more appetitive (versus avoidant) reasons, such as sensation seeking (Bowker, 1977; Palmgreen, Lorch, Stephenson, Hoyle, & Donohew, 2007; Zuckerman, 2007; Zuckerman, Ball, & Black, 1990). As use progresses, however, as exemplified by the increase in coping motives in the adult treatment-seeking population, it may become a function of negative reinforcement (Koob, 2013), or avoidance. It may be that for individuals who have developed symptoms of dependence, significant neurobiological, motivational, and learning components influence their experience, and the role of substance use in their lives (WHO, 2004). Lack of mindfulness may be related to higher severity of dependence as individuals use to avoid their aversive experiences, such as negative affect or physical discomfort, a target in mindfulness training (e.g., Bowen, Chawla, & Witkiewitz, In press).
Findings from this study can inform our clinical interventions for substance use disorders by helping us better understand the potential benefits of mindfulness training in treatment. First, the differing motives or functions of substance use are important to consider. Individuals early in their use, for example, may be sensation seeking or looking to enhance positive experiences, versus individuals with more severe dependence, who may be using to avoid discomfort. Treatments could benefit from targeting these motives and processes specifically. The current study’s finding that mindfulness may be helpful for those higher in avoidant coping suggests that treatments aimed to increase mindfulness may indeed help mitigate the use of substance to alleviate discomfort for individuals with higher levels of addiction severity, and specifically those with avoidant coping tendencies. Explicit training in the ability and willingness to stay with discomfort rather than avoid it (e.g., Bowen et al., 2010) can be a useful direct target and practice in treatment.
4.1 Limitations
Alongside the contributions of the current study, there are limitations to consider. Measurement of mindfulness in itself poses several challenges and limitations. First, different mindfulness scales were used across the studies reviewed (FMI, MAAS, and FFMQ), thus rendering a true comparison of results unfeasible. Second, and perhaps most importantly, the operationalization of mindfulness as a construct has recently received criticism, with concerns regarding response biases in self-report data, the reliability of questionnaire usage in meditating and non-meditating populations, and the misappropriation of Buddhist terms in construct definition, among others (Grossman & Van Dam, 2011). Additionally, fundamental conceptual issues have been raised around the validity of attempting to operationalize and quantify a construct developed and refined over two millennia of qualitative self-inquiry (Grossman & Van Dam, 2011). Although these concerns may represent significant limitations in the scientific study and investigation of mindfulness as a psychological construct, scientific investigation requires definition and measurement of the hypothesized active ingredients within a given treatment paradigm (Baer, 2011; Brown, Ryan, Loverich, Biegel, & West, 2011).
Additionally, in consideration of the environmental strictures on access to substances for period of report, dependence severity was used as a primary outcome measure rather than the more traditional measure of quantity/frequency of substance use, as in the previous studies on which this is based. The SDS includes such items as, “Did you think your substance use was out of control?” and “How difficult did you find it to stop go without [substance]?” Although SDS has been shown to be highly correlated with quantity and frequency across multiple substances (González-Sáiz et al., 2009; Piontek, Kraus, & Klempova, 2008), it may measure the function of and relationship to substance use rather than the rather than the use patterns. As both the more traditional count measures as well as an individual’s relationship to the substance use are worthy of assessment, future studies would benefit from inclusion of both.
Finally, findings are cross-sectional, thus causal inferences need to be made with caution, as relationships between mindfulness, coping, and substance use may be bidirectional or recursive. Future studies might further examine these relationships using longitudinal models to reveal the progression from positively reinforcing motivations, as may be true in a college student population, to a pattern of negative reinforcement, as seen in the self-medicating cycles of substance dependence, and examine the role of mindfulness in this progression. Similarly, mindfulness-based interventions might further examine changes in components of mindfulness as they relate to post-treatment substance use and relapse.
In summary, the current study suggests the relationship between mindfulness and substance use may be different for clinical versus nonclinical samples. While some have argued that unexpected findings in previous studies (Leigh et al., 2005; Leigh & Neighbors, 2009) are due to measurement issues (e.g., Grossman & Van Dam, 2011), results from the current study suggest it may be due to the function of substance use or the level of severity of substance dependence. This highlights the need for consideration of context and function, as measurement of use alone may not represent the true nature of the complexities of and differences in roles of substance use in individuals’ lives, and how it may relate to constructs such as mindfulness.
Highlights.
There is scientific debate about how mindfulness and substance use are related.
We found a negative relationship between these factors in a clinical sample.
Findings suggest opposite trends in clinical (versus non) samples.
We found a significant moderating effect of avoidant coping in this relationship.
Results point to the importance of considering the function of substance use.
Acknowledgments
We would like to acknowledge the immeasurable contribution of G. Alan Marlatt, who served as the original PI on the grant funding this study, and without whom this work would not have happened. We would also like to acknowledge Recovery Centers of King County for their collaboration in this trial. Additionally, we thank the several individuals on the research team who ensured the success of the countless day-to-day details involved in such a study.
Role of Funding Sources
Funding for this study was provided by National Institute on Drug Abuse (5R01DA025764-02). NIDA had no role in the study design, collection, analysis or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributors
Sarah Bowen and Matthew Enkema were involved in design of the study. Both authors conducted literature searches, provided summaries of previous research studies, and conducted the statistical analysis. Both authors contributed to the writing of all manuscript drafts and have approved the final manuscript.
Conflict of Interest
The authors declare that they have no conflicts of interest
Contributor Information
Sarah Bowen, Email: swbowen@uw.edu, Center for the Study of Health and Risk Behaviors, Department of Psychiatry, University of Washington, Box 354944, 1100 NE 45th St, Suite 300, Seattle, WA 98105, USA, 206-685-2995.
Matthew C. Enkema, Email: menkema@uw.edu, Innovative Programs Research Group, School of Social Work, University of Washington, Box 354690, 909 NE 43rd St, Suite 304, Seattle, WA 98105, 206-755-8825.
References
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Thousand Oaks, CA US: Sage Publications, Inc; 1991. [Google Scholar]
- Baer RA. Mindfulness training as a clinical intervention: A conceptual and empirical review. Clinical Psychology: Science and Practice. 2003;10:125–143. doi: 10.1093/clipsy/bpg015. [DOI] [Google Scholar]
- Baer RA. Measuring mindfulness. Contemporary Buddhism. 2011;12:241–261. [Google Scholar]
- Baer RA, Smith GT, Hopkins J, Krietemeyer J, Toney L. Using Self-Report Assessment Methods to Explore Facets of Mindfulness. Assessment. 2006;13(1):27–45. doi: 10.1177/1073191105283504. [DOI] [PubMed] [Google Scholar]
- Bischof G, Rumpf HJ, Meyer C, Hapke U, John U. Gender differences in temptation to drink, self-efficacy to abstain and coping behavior in treated alcohol-dependent individuals: Controlling for severity of dependence. Addiction Research & Theory. 2005;13(2):129–136. doi: 10.1080/16066350412331335305. [DOI] [Google Scholar]
- Bishop SR, Lau M, Shapiro SL, Carlson L, Anderson ND, Carmody J, Devins G. Mindfulness: A Proposed Operational Definition. Clinical Psychology: Science and Practice. 2004;11:230–241. doi: 10.1093/clipsy.bph077. [DOI] [Google Scholar]
- Bowen S, Chawla N, Marlatt GA. Mindfulness-based relapse prevention for addictive behaviors: A clinician’s guide. New York, NY, US: Guilford Press; 2010. [Google Scholar]
- Bowen S, Chawla N, Witkiewitz K. Mindfulness-Based Relapse Prevention for Addictive Behaviors. In: Baer RA, editor. Mindfulness-Based Treatment Approaches: A Clinician’s Guide. second. San Diego, CA, US: Elsevier Academic Press; (In press) [Google Scholar]
- Bowen S, Marlatt GA. Surfing the urge: Brief mindfulness-based intervention for college student smokers. Psychology of Addictive Behaviors. 2009;23(4):666–671. doi: 10.1037/a0017127. [DOI] [PubMed] [Google Scholar]
- Bowen S, Witkiewitz K, Clifasefi S, Grow J, Chawla N, Hsu S, Douglas H, Harrop E, Collins S, Lustyk K, Larimer M. Relative Efficacy of Mindfulness-based Relapse Prevention, Relapse Prevention and Standard Aftercare Treatment in Preventing Relapse to Substance Use. JAMA Psychiatry. doi: 10.1001/jamapsychiatry.2013.4546. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowen S, Witkiewitz K, Dillworth TM, Chawla N, Simpson TL, Ostafin BD, Marlatt GA. Mindfulness meditation and substance use in an incarcerated population. Psychology of Addictive Behaviors. 2006;20(3):343–347. doi: 10.1037/0893-164x.20.3.343. [DOI] [PubMed] [Google Scholar]
- Bowker LH. Motives for drug use: An application of Cohen’s typology. International Journal of the Addictions. 1977;12(8):983–991. doi: 10.3109/10826087709027266. [DOI] [PubMed] [Google Scholar]
- Brown K, Ryan RM. The benefits of being present: Mindfulness and its role in psychological well-being. Journal Of Personality And Social Psychology. 2003;84(4):822–848. doi: 10.1037/0022-3514.84.4.822. [DOI] [PubMed] [Google Scholar]
- Brewer JA, Elwafi HM, Davis JH. Craving to Quit: Psychological Models and Neurobiological Mechanisms of Mindfulness Training as Treatment for Addictions. Psychology of Addictive Behaviors. 2012 doi: 10.1037/a0028490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown KW, Ryan RM, Loverich TM, Biegel GM, West AM. Out of the armchair and into the streets: Measuring mindfulness advances knowledge and improves interventions: Reply to Grossman (2011) Psychological Assessment. 2011;23(4):1041–1046. doi: 10.1037/a0025781. [DOI] [Google Scholar]
- Buccheld N, Grossman P, Walach H. Achtsamkeit in Vipassana-Meditation and Psychotherapie: Die Entwicklung des “Freiburger Fragebogens zur Achtsamkeit.” Mindfulness in Vipassana meditation and psychotherapy: Development of the Freiburg Mindfulness Questionnaire. Zeitschrift-fuer-Klinische-Psychologie,-Psychiatrie-und-Psychotherapie. 2002;50(2):153–172. [Google Scholar]
- Carmody J, Baer RA. Relationships between mindfulness practice and levels of mindfulness, medical and psychological symptoms and well-being in a mindfulness-based stress reduction program. Journal of Behavioral Medicine. 2008;31(1):23–33. doi: 10.1007/s10865-007-9130-7. [DOI] [PubMed] [Google Scholar]
- Carmody J, Baer RA, Lykins ELB, Olendzki N. An empirical study of the mechanisms of mindfulness in a mindfulness-based stress reduction program. Journal of Clinical Psychology. 2009;65(6):613–626. doi: 10.1002/jclp.20579. [DOI] [PubMed] [Google Scholar]
- Carmody J, Reed G, Kristeller J, Merriam P. Mindfulness, spirituality, and health-related symptoms. Journal of Psychosomatic Research. 2008;64(4):393–403. doi: 10.1016/j.jpsychores.2007.06.015. [DOI] [PubMed] [Google Scholar]
- Chiesa A, Serretti A. Are mindfulness-based intervatnions effective for substance use disorders? A systematic review of the evidence. Substance Use & Misuse, Early Online. 2013:1–22. doi: 10.3109/10826084.2013.770027. [DOI] [PubMed] [Google Scholar]
- Cooper ML, Russell M, Skinner JB, Frone MR, Mudar P. Stress and alcohol use: Moderating effects of gender, coping, and alcohol expectancies. Journal of Abnormal Psychology. 1992;101(1):139–152. doi: 10.1037/0021-843x.101.1.139. [DOI] [PubMed] [Google Scholar]
- Dakwar E, Mariani JP, Levin FR. Mindfulness impairments in individuals seeking treatment for substance use disorders. The American Journal of Drug and Alcohol Abuse. 2011;37(3):165–169. doi: 10.3109/00952990.2011.553978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenlohr-Moul TA, Walsh EC, Charnigo RJ, Jr, Lynam DR, Baer RA. The ‘what’ and the ‘how’ of dispositional mindfulness: Using interactions among subscales of the Five-Facet Mindfulness Questionnaire to understand its relation to substance use. Assessment. 2012;19(3):276–286. doi: 10.1177/1073191112446658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernandez AC, Wood MD, Stein LAR, Rossi JS. Measuring mindfulness and examining its relationship with alcohol use and negative consequences. Psychology of Addictive Behaviors. 2010;24(4):608–616. doi: 10.1037/a0021742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flannery BA, Volpicelli JR, Pettinati HM. Psychometric Properties of the Penn Alcohol Craving Scale. Alcoholism: Clinical and Experimental Research. 1999;23(8):1289–1295. doi: 10.1111/j.1530-0277.1999.tb04349.x. [DOI] [PubMed] [Google Scholar]
- Garland EL, Boettiger CA, Gaylord S, Chanon VW, Howard MO. Mindfulness is inversely associated with alcohol attentional bias among recovering alcohol-dependent adults. Cognitive Therapy and Research. 2012;36(5):441–450. doi: 10.1007/s10608-011-9378-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- González-Sáiz F, Domingo-Salvany A, Barrio G, Sánchez-Niubó A, Brugal MT, de la Fuente L, Alonso J. Severity of Dependence Scale as a diagnostic tool for heroin and cocaine dependence. European Addiction Research. 2009;15(2):87–93. doi: 10.1159/000189787. [DOI] [PubMed] [Google Scholar]
- Gonzalez VM, Skewes MC. Solitary heavy drinking, social relationships, and negative mood regulation in college drinkers. Addiction Research & Theory. 2013;21(4):285–294. doi: 10.3109/16066359.2012.714429. [DOI] [Google Scholar]
- Gossop M, Darke S, Griffiths P, Hando J. The Severity of Dependence Scale (SDS): Psychometric properties of the SDS in English and Australian samples of heroin, cocaine and amphetamine users. Addiction. 1995;90(5):607–614. doi: 10.1111/j.1360-0443.1995.tb02199.x. [DOI] [PubMed] [Google Scholar]
- Grossman P, Van Dam NT. Mindfulness, by any other name …; trials and tribulations of sati in western psychology and science. Contemporary Buddhism. 2011;12(1):219–239. doi: 10.1080/14639947.2011.564841. [DOI] [Google Scholar]
- Hanh TN. The heart of the Buddha’s teachings:: Transforming Suffering into Peace, Joy, and Liberation. New York, NY: Broadway Books; 1999. [Google Scholar]
- Hofmann SG, Sawyer AT, Witt AA, Oh D. The effect of mindfulness-based therapy on anxiety and depression: A meta-analytic review. [Meta-Analysis Research Support, N.I.H., Extramural] Journal of Consulting and Clinical Psychology. 2010;78(2):169–183. doi: 10.1037/a0018555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hölzel BK, Lazar SW, Gard T, Schuman-Olivier Z, Vago DR, Ott U. How does mindfulness meditation work? Proposing mechanisms of action from a conceptual and neural perspective. Perspectives on Psychological Science. 2011;6(6):537–559. doi: 10.1177/1745691611419671. [DOI] [PubMed] [Google Scholar]
- Hruska B, Fallon W, Spoonster E, Sledjeski EM, Delahanty DL. Alcohol use disorder history moderates the relationship between avoidance coping and posttraumatic stress symptoms. Psychology of Addictive Behaviors. 2011;25(3):405–414. doi: 10.1037/a0022439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kabat-Zinn J, Massion A, Kristeller JL, Peterson LG, Fletcher KE, Pbert L, Santorelli SR. Effectiveness of a meditation-based stress reduction intervention in the treatment of anxiety disorders. American Journal of Psychiatry. 1992;149:936–943. doi: 10.1176/ajp.149.7.936. [DOI] [PubMed] [Google Scholar]
- Khantzian EJ. The Self-Medication Hypothesis Revisited: The Dually Diagnosed Patient. Primary Psychiatry. 2003;10(9):47–48. 53–54. [Google Scholar]
- Koob GF. Theoretical frameworks and mechanistic aspects of alcohol addiction: Alcohol addiction as a reward deficit disorder. In: Sommer WH, Spanagel R, editors. Behavioral neurobiology of alcohol addiction. Vol. 13. New York, NY US: Springer Science + Business Media; 2013. pp. 3–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leigh J, Bowen S, Marlatt GA. Spirituality, mindfulness and substance abuse. Addictive Behaviors. 2005;30(7):1335–1341. doi: 10.1016/j.addbeh.2005.01.010. [DOI] [PubMed] [Google Scholar]
- Leigh J, Neighbors C. Enhancement motives mediate the positive association between mind/body awareness and college student drinking. Journal of Social and Clinical Psychology. 2009;28(5):650–669. doi: 10.1521/jscp.2009.28.5.650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCracken LM, Gauntlett-Gilbert J, Vowles KE. The role of mindfulness in a contextual cognitive-behavioral analysis of chronic pain-related suffering and disability. Pain. 2007;131(1–2):63–69. doi: 10.1016/j.pain.2006.12.013. [DOI] [PubMed] [Google Scholar]
- Moos RH. Coping Responses Inventory: A measure of approach and avoidance coping skills. In: Zalaquett CP, Wood RJ, editors. Evaluating stress: A book of resources. Lanham, MD US: Scarecrow Education; 1997. pp. 51–65. [Google Scholar]
- Moos RH, Brennan PL, Fondacaro MR, Moos BS. Approach and avoidance coping responses among older problem and nonproblem drinkers. Psychology and Aging. 1990;5(1):31–40. doi: 10.1037/0882-7974.5.1.31. [DOI] [PubMed] [Google Scholar]
- Ostafin BD, Bauer C, Myxter P. Mindfulness decouples the relation between automatic alcohol motivation and heavy drinking. Journal of Social and Clinical Psychology. 2012;31(7):729–745. doi: 10.1521/jscp.2012.31.7.729. [DOI] [Google Scholar]
- Palmgreen P, Lorch EP, Stephenson MT, Hoyle RH, Donohew L. Effects of the Office of National Drug Control Policy’s marijuana initiative campaign on highsensation-seeking adolescents. American Journal of Public Health. 2007;97(9):1644–1649. doi: 10.2105/ajph.2005.072843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piontek D, Kraus L, Klempova D. Short scales to assess cannabis-related problems: A review of psychometric properties. Substance Abuse Treatment, Prevention, and Policy. 2008;3 doi: 10.1186/1747-597x-3-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenzweig S, Greeson JM, Reibel DK, Green JS, Jasser SA, Beasley D. Mindfulness-based stress reduction for chronic pain conditions: Variation in treatment outcomes and role of home meditation practice. Journal of Psychosomatic Research. 2010;68(1):29–36. doi: 10.1016/j.jpsychores.2009.03.010. [DOI] [PubMed] [Google Scholar]
- Segal Z, Bieling P, Young T, MacQueen G, Cooke R, Martin L, Levitan RD. Antidepressant Monotherapy vs Sequential Pharmacotherapy and Mindfulness-Based Cognitive Therapy, or Placebo, for Relapse Prophylaxis in Recurrent Depression. Archives of General Psychiatry. 2012;67(12):1256–1264. doi: 10.1001/archgenpsychiatry.2010.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevens SJ, Andrade RAC, Ruiz BS. Women and substance abuse: Gender, age, and cultural considerations. Journal of Ethnicity in Substance Abuse. 2009;8(3):341–358. doi: 10.1080/15332640903110542. [DOI] [PubMed] [Google Scholar]
- WHO. Neuroscience of Psychoactive Substance Use and Dependence. Geneva, Switzerland: World Health Organization; 2004. p. 264. [Google Scholar]
- Witkiewitz K, Lustyk MKB, Bowen S. Retraining the Addicted Brain: A Review of Hypothesized Neurobiological Mechanisms of Mindfulness-Based Relapse Prevention. Psychology of Addictive Behaviors. 2012 doi: 10.1037/a0029258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zgierska A, Rabago D, Chawla N, Kushner K, Koehler R, Marlatt GA. Mindfulness meditation for substance use disorders: a systematic review. Substance Abuse. 2009;30(4):266–294. doi: 10.1080/08897070903250019. doi: 916722643 [pii] 10.1080/08897070903250019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zuckerman M. Sensation seeking and risky behavior. Washington, DC US: American Psychological Association; 2007. [Google Scholar]
- Zuckerman M, Ball SA, Black J. Influences of sensation seeking, gender, risk appraisal, and situational motivation on smoking. Addictive Behaviors. 1990;15(3):209–220. doi: 10.1016/0306-4603(90)90064-5. [DOI] [PubMed] [Google Scholar]


