Abstract
Objective
This study investigated whether family focused therapy (FFT-CHR), an 18-session intervention that consisted of psychoeducation and training in communication and problem solving, brought about greater improvements in family communication than enhanced care (EC), a 3-session psychoeducational intervention, among individuals at clinical high risk for developing psychosis.
Method
This study was conducted within a randomized controlled trial across 8 sites. We examined 10-min problem-solving discussions at baseline and 6-month reassessment among 66 adolescents and young adults and their parents. Trained coders who were blind to treatment and time of assessment achieved high levels of interrater reliability when evaluating family discussions on categories of calm–constructive and critical– conflictual behavior.
Results
Individuals at high risk and their family members who participated in FFT-CHR demonstrated greater improvement from baseline to 6-month reassessment in constructive communication and decreases in conflictual behaviors during family interactions than those in EC. Participants in FFT-CHR showed greater increases from baseline to 6 months in active listening and calm communication and greater decreases in irritability and anger, complaints and criticism, and off-task comments compared to participants in EC. These changes occurred equally in high-risk participants and their family members.
Conclusions
A 6-month family skills training treatment can bring about significant improvement in family communication among individuals at high risk for psychosis and their parents. Future studies should examine the association between enhancements in family communication and reduced risk for the onset of psychosis among individuals at high risk.
Keywords: randomized clinical trial, expressed emotion, family problem solving, schizophrenia
Family members’ conversations about day-to-day problems may affect the nature and course of early psychosis through several interacting mechanisms. When these conversations are frustrating and heated, they become a source of psychological stress. Psychosocial stress is included in most etiologic models of schizophrenia, frequently conceptualized as a precipitating factor for psychosis in individuals with a genetic diathesis (Nuechterlein & Dawson, 1984). Youths at risk for psychosis may be particularly sensitive to stressful (Ierago et al., 2009; Johnson, Cohen, Kasen, Smailes, & Brook, 2001; Otero et al., 2011; Wahlberg et al., 1997) and protective (Gonzalez-Pinto et al., 2011; Tienari et al., 2004) factors in the family environment. When individuals with schizophrenia talk with family members who are classified as high in expressed emotion (EE; i.e., express high levels of critical comments or hostility toward them), they demonstrate higher levels of autonomic arousal than do those who talk with caregivers who are low in EE (Sturgeon, Kuipers, Berkowitz, Turpin, & Leff, 1981; Tarrier, Vaughn, Lader, & Leff, 1979). If heightened arousal is occurring on a daily basis, that may compromise neuroregulatory processes that may increase risk for psychosis (Lukoff, Synder, Ventura, & Nuechterlein, 1984).
Many individuals with schizophrenia are lacking in communication and problem-solving skills (Bellack, Sayers, Mueser, & Bennett, 1994; Stalberg, Lichtenstein, Sandin, & Hultman, 2008) that would help them to deal effectively with daily challenges in the home environment. These skill deficits may play an important role in provoking family members’ heated reactions and criticism. Youths’ irritable and conflictual behaviors may be reinforced within the family given high rates of reciprocity during family interactions (Hamilton, Asarnow, & Tompson, 1999; O’Brien et al., 2008; Patterson, 1982; Patterson & Fisher, 2002). Irritable exchanges with family members may leave individuals who are at risk for psychosis and already exhibiting impaired social functioning (Addington, Penn, Woods, Addington, & Perkins, 2008) without supportive social relationships that could help them to generate normative explanations for confusing perceptual experiences (French & Morrison, 2004), while those with constructive daily conversations may benefit from access to broader perspectives and emotional support. Moreover, interaction patterns that are established in the home environment may generalize to the peer group, where greater emotional negativity and more ineffective problem solving are related to poor adolescent social adjustment (Mc-Combs, Forehand, & Smith, 1988; Patterson, Reid, & Dishion, 1992), while prosocial problem-solving strategies and prosocial behavior predict social acceptance among adolescent peers (Pakaslahti, Karjalainen, & Keltikangas-Jarvinen, 2002).
With well-established methods for ascertaining individuals at imminent high risk for conversion to psychosis (Miller et al., 2002), researchers have begun to investigate the relationship between family environments and youths’1 symptom progression during the earliest identifiable phases of a putatively psychotic illness. Research on expressed emotion (EE) has shown that young adults with schizophrenia are more likely to relapse in 9-month to 1-year follow-ups if their caregivers are rated as high in EE (Hooley, 2007). A prior study found that 35% of a sample of caregivers of youths at clinical high risk (CHR) for psychosis could be classified as high EE and that the majority of critical remarks by family members focused on youths’ negative symptoms and irritability (O’Brien et al., 2006).
Reductions in irritable exchanges could bring relevant relief to families and perhaps prevent the escalation of caregiver criticism that seems to accompany longer periods of illness (Hooley & Richters, 1995). Conversely, caregivers’ warm and spontaneous positive statements about CHR youths during the Camberwell Family Interview predicted improvement in negative and disorganized symptoms as well as social functioning at 6-month follow-up (O’Brien et al., 2006), and parents’ and adolescents’ use of constructive communication during a 10-min problem-solving interaction predicted improvement in adolescents’ social functioning 6 months later (O’Brien et al., 2009). These findings suggest that the presence of greater constructive family communication and not only the absence of negative communication may serve an important role for youths who are exhibiting attenuated psychotic symptoms. Repetitive, high-intensity interactions over day-to-day issues affect parents’ mental health as well (Silverberg & Steinberg, 1987; Steinberg, 2001). Whether active efforts to enhance constructive communication can be successful with CHR youths and their families has yet to be investigated.
How much family therapy is necessary to improve family communication in an adolescent and young adult clinical population with attenuated psychotic symptoms? From a cost-management perspective and to reduce demands on family members’ time, less therapy would be preferable. Perhaps at this early phase of illness a few sessions that provide information about symptoms, coping options, and the importance of a low-key family environment are sufficient to stimulate family members’ adaptation to youths’ symptoms and spontaneous improvement in family communication and problem solving. In fact, some have cautioned that the provision of communication skills training may increase family stress and patient symptoms due to the implicit message that something is wrong with the family’s interaction style (Linszen et al., 1996).
On the other hand, untreated CHR patients have more severe positive symptoms than do treated patients with a first episode of psychosis (Miller, Zipursky, et al., 2003). When compared to nonpsychiatric controls, CHR individuals have striking impairments in interpersonal communication that are not significantly different from patients with first episode and multiple episodes of psychosis (Addington et al., 2008), and family burden is comparable in families of clinical high-risk and recent-onset psychosis patients (Wong et al., 2008). Given these similarities between CHR youths and those with psychotic symptoms, improvement in family communication may require more explicit communication training.
Research indicates that brief psychoeducational interventions may not be sufficient to enhance family processes in first-episode patients (González-Blanch et al., 2010). Family interventions that include communication and problem-solving training have been associated with better family communication among individuals with schizophrenia (Doane, Goldstein, Miklowitz, & Falloon, 1986) and bipolar illness (Simoneau, Miklowitz, Richards, a Saleem, & George, 1999). Based on a thorough review of the family treatment literature, Dixon et al. (2010) recommended that patients with schizophrenia who are in regular contact with their families should be offered family interventions for a minimum of 6–9 months, and Glynn, Cohen, Dixon, and Niv (2006) assert that longer family treatments (9 months to 2 years) yield better outcomes than short-term family interventions. Similarly, in a meta-analysis of 25 family intervention studies, Pitschel-Walz, Leucht, Bauml, Kissling, and Engel (2001), found that relapse rates can be significantly reduced for individuals with schizophrenia, especially if the family interventions are longer than 3 months.
Given that the majority of individuals at clinical high risk do not go on to develop psychosis (Addington et al., 2011; Cannon et al., 2008; Schlosser et al., 2011), it is important to consider the relevance of family interventions that focus on communication and problem-solving enhancement for the multiple comorbid conditions with which these youths are often diagnosed (Fusar-Poli, Nelson, Valmaggia, Yung, & McGuire, 2012; Woods, Walsh, Saksa, & McGlashan, 2010). Studies of expressed emotion have found an association between high levels of family EE and relapse across a broad range of disorders, including depression and bipolar disorder (see Butzlaff & Hooley, 1998, or Hooley & Gotlib, 2000, for reviews). Family hostility is a predictor of poor treatment outcome in anxiety disorders, including posttraumatic stress disorder, agoraphobia, and obsessive-compulsive disorder; a high level of family criticism is predictive of poor treatment outcome among those with eating disorders, weight problems, and substance use disorders (See Hooley, 2007, for a review). Further, from a general prevention of illness perspective, Repetti, Taylor, and Seeman (2002) asserted that family environments that are high in conflict and aggression and lacking in warmth and support place youth at heightened risk for disruptions in psychosocial functioning and in stress-responsive biological regulatory systems that in turn contribute to poor health behaviors, substance abuse, psychosocial impairment, and psychological disorders. Improvement in the family environment is considered vital to mental and physical health throughout development (Kumpfer & Alvarado, 2003; Repetti et al., 2002).
The primary objective of this study is to investigate, in a CHR population, whether family focused therapy (FFT-CHR), an 18-session intervention that includes psychoeducation and structured training in communication and problem solving, is associated with greater improvements in family communication than enhanced care (EC), a three-session psychoeducational intervention. The study was conducted within the eight-site North American Prodrome Longitudinal Study (NAPLS) consortium. We hypothesized that explicit training in communication and problem solving (FFT-CHR) would be more effective than brief psychoeducation in facilitating improvement in family communication for youths, mothers, and fathers from pretreatment to 6-month reassessment.
Method
Participants
The participants in this study were a subset of those recruited to NAPLS, a consortium of eight research centers: Emory University, Harvard University, University of Calgary, University of California Los Angeles, University of California San Diego, University of North Carolina, Yale University, and Zucker Hillside Hospital (Addington et al., 2012). Consistent with NAPLS criteria, individuals between the ages of 12 and 35 who were primarily English speaking, and met criteria for one of three prodromal syndromes assessed by the Structured Interview for Prodromal Symptoms (SIPS: Miller et al., 2002) were considered for inclusion. Eligible prodromal syndromes are the following:
Attenuated positive symptoms: Patients are experiencing positive symptoms (unusual thoughts, suspiciousness, grandiosity, perceptual disturbances, disorganized communication) that are subpsychotic in duration and intensity that have begun or worsened in the past year.
Brief intermittent psychosis: Patients are experiencing fully psychotic symptoms that are present only intermittently with onset in the past 3 months.
Genetic risk and deterioration: Patients either have schizotypal personality disorder or have a first-degree relative with a psychotic disorder and have experienced a significant decline in functioning in the last year (Miller, McGlashan, et al., 2003; Miller et al., 2002).
If participants met one or more of the syndromal criteria described above, releases were signed to allow for a thorough review of previous psychiatric, school, and medical records, and they were administered the Structured Clinical Interview for Diagnostic and Statistical Manual of Mental Disorders (4th ed.; DSM–IV) Axis I Disorders (First, Spitzer, Gibbon, & Williams, 2002). Exclusion criteria included a previous DSM–IV (American Psychiatric Association, 1994) diagnosis of schizophrenia or schizoaffective disorder, mental retardation, current drug or alcohol dependence, or the presence of a neurological disorder.
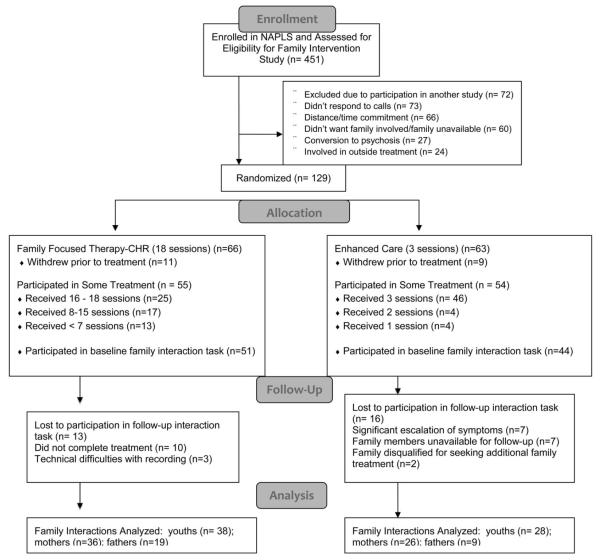
Between January 2009 and February 2012, NAPLS participants who expressed interest in a randomized clinical trial of family therapy were recruited. 129 CHR youths and their parent(s) or significant others signed informed consent documents and were randomly assigned to family focused therapy (FFT-CHR), an 18-session family treatment that included psychoeducation, communication training and problem-solving training or to an enhanced care treatment (EC) consisting of three sessions of psychoeducation, using a modification of Efron’s (1971) biased coin toss procedure (see Figure 1). Randomizations were stratified by study site and CHR individuals’ use of antipsychotic medication. This study was conducted in compliance with the Internal Review Boards for each of the participating sites.
Figure 1.
CONSORT flow diagram. NAPLS = North American Prodrome Longitudinal Study; CHR = clinical high risk.
Psychosocial Treatment Intervention
Detailed treatment manuals guided therapists’ work in each treatment condition (De Silva et al., 2009; Miklowitz et al., 2010) and the same therapists provided both FFT-CHR and EC. Treatment sessions were approximately 50 min in both conditions, and treatment was conducted with each family individually. Therapists who delivered the intervention were primarily doctoral level, with some master’s level therapists. As part of FFT-CHR, approximately six sessions focused on psychoeducation during which the therapist facilitated discussions of the youths’ symptoms, daily stressors, youth and family coping strategies, and developed prevention action plans. These same topics were addressed in an abbreviated manner during EC, the three-session treatment. As part of FFT-CHR, approximately five sessions were dedicated to communication enhancement, with the therapist introducing and modeling a new skill each week, practicing that skill with family members, organizing opportunities for family members to practice the skill with each other in session, providing feedback and coaching to participants, and assigning tasks that required family members to practice the skills between sessions. The following communication skills were introduced routinely: expressing positive feelings, active listening, making positive requests for change, expressing negative feelings, and communication clarity. Six additional sessions were devoted to problem-solving training and integration of communication and problem-solving skills. Family members were taught a structured approach that included defining problems, breaking complex problems into a series of smaller problems, brainstorming solutions, analyzing pros and cons of possible solutions, and selecting and implementing action plans (for more information regarding FFT-CHR and EC, see Schlosser et al., 2012).
Therapists were trained in FFT-CHR and EC in an initial 2-day workshop conducted by the treatment manual developers. After the workshop, clinicians took on at least two study cases with weekly or biweekly supervision from an expert supervisor (David Miklowitz or Mary O’Brien). Treatment sessions were videotaped or audiotaped, and a random selection of sessions (three sessions for every FFT-CHR, one from each of the psychoeducation, communication, and problem-solving enhancement modules; and one session for every EC) were rated for therapist fidelity using the Therapy Competence and Adherence Scales Revised (TCAS-R; Weisman et al., 2002; Miklowitz et al., 2008), an 11-item measure that rates therapists on 7-point scales ranging from 1 (very poor) to 7 (excellent) on skills in administering psychoeducation, communication, and problem-solving modules, as well as general clinician skills such as rapport, pacing, and session command. Interrater reliability for the overall fidelity scale was good with an intraclass correlation of .67. Ninety percent of treatment sessions were classified as competent and adherent on the overall fidelity scale with no significant difference in overall adherence between treatment groups. FFT-CHR sessions included a significantly greater emphasis on communication and problem-solving skills training than EC sessions, whereas provision of psychoeducation and nonspecific therapist skills such as rapport with patients or pacing of sessions did not differ between conditions (Marvin, Miklowitz, O’Brien, & Cannon, 2013).
Measures
Assessment of clinical symptoms
Prodromal symptoms were rated using the Scale of Prodromal Symptoms (SOPS) contained within the SIPS (Hawkins et al., 2004; Lemos et al., 2006). The SOPS scales range from 0 to 6 with extensive anchors for each scale point for each symptom. To reduce the number of statistical comparisons, this investigation focuses only on the positive and negative symptom scales. The positive symptom scale assesses symptoms related to unusual thought content, suspiciousness, perceptual disturbances/hallucinations, grandiosity, and disorganized communication. Symptoms of anhedonia, avolition, flat affect, decreased role functioning, and decreased comprehension/abstraction are captured by the SOPS negative symptom scale.
Assessment of family communication during problem-solving interactions
Before the start of the second therapy session, family members independently evaluated on a scale ranging from 1 (low) to 5 (high) how much family tension was created by each of 19 topics, including homework, screen time (television, gaming systems, computer, tablets, etc.), phone use, chores, waking up independently, school attendance, relationship with siblings, medications, friends, irritability with family members, bed time, curfew, eating and weight issues, use of the car, money, use of shared space, time management, communication, and recreation/vacations. Therapists identified topics that were rated highly by all participants, asked the youth to select one of those for further discussion, and read the following standardized instructions to the family: “Please discuss X and attempt to reach a resolution. You have 10 min for this discussion, and I will return after 10 min.” The same procedure was used to gather follow-up interaction data during the final treatment session that occurred 6 months after treatment initiation for the FFT-CHR group, and by either the therapist or a research assistant during the 6 month reassessment for the EC group. This procedure is similar to family behavioral observation assessment strategies used in studies of schizophrenia and bipolar disorder (e.g., Bellack, Haas, & Tierney, 1996; Blanchard, Sayers, Collins, & Bellack, 2004; Miklowitz, Goldstein, Falloon, & Doane, 1984; Strachan, Leff, Goldstein, Duone, & Burtt, 1986) and of clinically high-risk youth (O’Brien et al., 2009).
The interactions were videotaped and later transcribed and coded. Trained raters coded each transcript while viewing the respective videotaped interaction so that family members’ affect could be evaluated. All codes are described in Table 1. A tally mark was recorded for each of the categories of behavior that occurred during each speaker turn. If a speaker received a tally in a critical– conflictual category (except for the cutoff category) he or she was ineligible to receive a tally within a calm–constructive category during that particular speaker turn. However, if a speaker engaged in several different categories of critical– conflictual behaviors during a speaker turn, he or she received a tally in each of those different categories. The same was true for calm–constructive behaviors.
Table 1.
Coding Categories and Interrater Reliabilities for the 10-Min Family Problem Solving Interaction
| Codes | Definition | Example | Intraclass correlation coefficientsa |
|---|---|---|---|
| Calm–constructive | .89 | ||
| 1. Affection and Compliments |
Displays of affection; caring, touching or supportive remarks; expressing positive feelings about others’ behavior or attributes |
Smiling and patting someone gently on the arm; “We are all in this together”; “You just provided a really good example.” |
.86 |
| 2. Mild Listening | Minor indication of listening | Saying “mm-hm”; nodding head | .81 |
| 3. Active Listening | Listening empathically, eliciting another’s point of view, summarizing, asking follow-up questions |
“That sounds tough”; “Tell me more about that”; “Are you mad at Mike all the time or just when he borrows your stuff?” |
.90 |
| 4. Calm Speaking | Expressing oneself clearly and concisely in a neutral or positive tone of voice |
“I think it is reasonable to expect someone your age to be doing their own laundry.” |
.81 |
| 5. Organization | Efforts to keep the conversation on track | “I think we are talking about two different things. Which should we focus on first?” |
.84 |
| Critical–conflictual | .79 | ||
| 1. Irritability and Anger |
Using an irritated/angry tone of voice; withdrawing |
“I said I DON’T want to talk to you anymore!” | .84 |
| 2. Complaints and Criticism |
Complaints, criticisms, overgeneralizations, demanding or intrusive statements, monologues |
“Every time I go to sit down at the kitchen table what do I find but your dirty dishes”; “You never help.” |
.76 |
| 3. Cutoff | One person starts to speak before another person has finished |
Mother says, “I wanted to hear more about …” and youth cuts her off. |
.78 |
| 4. Off-Task Comments | One person goes off on a tangent during the conversation |
“Hey they have crayons here. This one is the color of my favorite ice cream. Can we get ice cream after this?” |
.60 |
Averaged across coder pairs.
A team of eight coders evaluated the problem-solving interactions. Coders were trained using practice tapes with gold standard consensus codes and then participated in biweekly coding meetings. Efforts were made to keep coders blind to whether the family was participating in FFT-CHR or EC treatment and whether the interaction was the baseline or reassessment. Coders were asked to rate each interaction on two 3-point scales regarding their certainty of the assigned treatment (FFT-CHR vs. EC) and time of interaction (baseline vs. reassessment). Seventy-three tapes were rated by coders; on 69% of the tapes, coders were either unaware of or had guessed incorrectly about the type of treatment the family had received, and on 54% coders were either unaware of or had guessed incorrectly about whether the interaction was baseline or reassessment.
Every interaction was randomly assigned to at least two coders who worked independently. Coders rated each speaker turn and then tallied the frequency with which each code had been assigned to each family member during the entire interaction. Intraclass correlations were conducted on a randomly selected third of the coded data (Table 1). Acceptable levels of interrater agreement were achieved (Shrout & Fleiss, 1979). Once coder pairs had completed independent ratings of a particular interaction, they met to resolve discrepancies and create consensus data. Consensus data were used in all further analyses.
The summed tally marks in each category for each individual were divided by the total number of speaking turns provided by that individual during the interaction to create a percentage for each category of coded behavior for each participant in the family. Percentages were used rather than summed tallies because there was variation in family size and therefore in the number of speaking opportunities. Percentages were used to create a common metric across study participants. Two summary codes, calm–constructive and critical– conflictual, were created by adding the five codes within the calm–constructive dimension and the four codes within the critical– conflictual dimension, respectively. Finally, one overall constructive behavior code was calculated for each family member by subtracting the critical– conflictual summary code from the calm–constructive summary code. Because individuals could be assigned multiple calm–constructive or critical– conflictual codes during each speaking turn (e.g., speakers obtained three tallies if they provided compliments, expressed themselves calmly, and engaged in active listening during one speaking turn; and they obtained three tallies if they cut another person off, voiced a complaint, and used an angry tone of voice during one speaking turn), the number of codes sometimes exceeded the number of speaking turns and percentages were greater than 100%.
Statistical Analyses
To evaluate the possibility that those who did not participate in the 6-month reassessment were significantly different (i.e., more or less conflictual, symptomatic, and or different demographically) than those who did participate, t tests or chi-square analyses were conducted on youths’, mothers’, and fathers’/significant others’ baseline interaction data, SOPS scales, and demographic data for the FFT-CHR group and for the EC group, with those participating in both baseline and reassessment compared to those participating in baseline alone. Also, Pearson correlations were conducted to examine whether baseline SOPS symptom scores were associated with participants’ coded interaction behavior.
For the primary analyses, multilevel analyses of variance were conducted treating family as a random variable and modeling treatment (FFT-CHR vs. EC), time (baseline and 6-month), and family member (youth, mother, and father/significant other) as crossed fixed-effect predictive factors and controlling for study site. The first analysis examined whether the Treatment × Time interaction was significant for the constructive behavior summary variable. If so, follow-up multilevel analyses of variance (ANOVAs) were conducted to evaluate whether there were significant Treatment × Time interactions for the calm–constructive as well as critical– conflictual domains. If there were significant findings for Treatment × Time on those summary variables, follow-up repeated measures analyses were conducted on the individual codes within each summary category. All statistical tests were two-tailed.
Results
Participation Rates
Of the 66 families randomized to FFT-CHR, 51 participated in the baseline interaction task that was administered at the beginning of the second family treatment session (see Figure 1). Follow-up interaction data were collected from 38 (75%) of the families who completed the baseline interaction. Of the 51, 10 families discontinued therapy and three were unable to complete the posttreatment reassessment due to technical difficulties. Of the 38 families who completed baseline and 6-month interactions, 36 included the same family members in both assessments; two included the father in baseline but not follow-up.
Of the 63 families randomized to EC, 50 attended at least two treatment sessions and were eligible to participate in the interaction task that was administered during Session 2. Data were not gathered from six of the 50 eligible families for a variety of reasons, including youths’ conversion to psychosis and technical difficulties with camera equipment. Of the 44 families who completed the baseline interaction task, 28 (64%) completed the 6-month reassessment. Seventeen EC families did not complete follow-up for a variety of reasons, including clinical emergencies during the follow-up clinical assessment; youths’ conversion to psychosis during the 6-month treatment interval and subsequent referral to first episode clinics; couple’s separation; family members’ unavailability for follow-up assessment; families’ participation in additional family treatment after the three EC sessions were completed, thus disqualifying themselves from the study; and technical difficulties with the camera equipment. There were 17 families in which everyone who participated in the baseline interaction also participated in the follow-up; for 11 families, the father participated in the baseline but did not participate in the follow-up interaction.
There were no significant differences in youths’, mothers’ or fathers’/significant others’ constructive behaviors during the baseline interaction task, youths’ baseline symptoms, and demographic variables when comparing those who did to those who did not participate in the follow-up interaction task for the FFT-CHR and EC treatment groups (See Table 2).
Table 2.
t-Tests Comparing the Constructive Behavior Scale During Baseline Interaction, Demographics, and Symptom Scales for Those Who Did and Did Not Participate in the 6-Month Interaction
| Scale and demographics | Participated in 6-month interaction |
Did not participate in 6-month interaction |
t or χ2, p |
|---|---|---|---|
| FFT-CHR participants | |||
| Constructive Behavior Scale: M (SD) n | |||
| Youth | .15 (.75) 38 | −.18 (.95) 13 | t = 1.13, p = .27 |
| Mother | .44 (.78) 36 | .40 (1.03) 12 | t < 1, p = .89 |
| Father/significant other | .59 (.62) 19 | .21 (1.40) 6 | t < 1, p = .52 |
| Age: M (SD) n | |||
| Youth | 17.2 (4.2) 38 | 17.2 (2.9) 13 | t < 1, p = .98 |
| Mother | 45.3 (6.1) 38 | 41.9 (6.9) 13 | t = 1.56, p = .13 |
| Father/significant other | 49.4 (7.2) 36 | 47.1 (9.0) 13 | t < 1, p = .40 |
| Education on 9-point scale: M (SD) n | |||
| Mother | 6.5 (1.7) 38 | 5.9 (1.1) 13 | t = 1.52, p = .14 |
| Father | 6.2 (1.7) 36 | 6.2 (2.2) 13 | t < 1, p = .95 |
| Youth SOPS baseline symptoms: M (SD) n | |||
| Positive Symptom Scale | 11.8 (3.4) 38 | 10.7 (2.6) 13 | t = 1.23, p = .23 |
| Negative Symptom Scale | 12.8 (6.3) 36 | 12.8 (5.4) 13 | t < 1, p = .98 |
| Youth gender (male): % | 55 | 85 | χ2 < 3.57, p = .06 |
| Youth antipsychotic medication: % | 17 | 31 | χ2 = 1.17, p = .28 |
|
| |||
| EC participants | |||
| Constructive Behavior Scale: M, n | |||
| Youth | .32, 28 | .07, 16 | t = 1.08, p = .29 |
| Mother | .58, 26 | .76, 12 | t < 1, p = .57 |
| Father/significant other | .68, 19 | .46, 9 | t < 1, p = .40 |
| Age: M (SD) n | |||
| Youth | 16.5 (2.5) 28 | 16.9 (4.4) 16 | t < 1, p = .72 |
| Mother | 44.6 (5.8) 27 | 47.5 (7.2) 16 | t = 1.46, p = .15 |
| Father/significant other | 49.2 (7.4) 28 | 46.4 (5.9) 16 | t = 1.37, p = .18 |
| Education on 9-point scale: M (SD) n | |||
| Mother | 6.9 (1.5) 27 | 6.3 (1.5) 16 | t = 1.45, p = .16 |
| Father | 6.3 (1.7) 28 | 6.1 (1.8) 16 | t < 1, p = .64 |
| Youth SOPS baseline symptoms: M (SD) n | |||
| Positive Symptom Scale | 11.7 (3.7) 28 | 11.2 (2.8) 16 | t < 1, p = .69 |
| Negative Symptom Scale | 11.6 (6.5) 26 | 13.3 (5.1) 13 | t < 1, p = .38 |
| Youth gender (male): % | 57 | 62 | χ2 < 1, p = .73 |
| Youth antipsychotic medication: % | 37 | 13 | χ2 = 2.66, p = .10 |
Note. FFT-CHR = family focused therapy–clinical high risk; SOPS = Scale of Prodromal Symptoms; EC = enhanced care.
Sociodemographic and Clinical Characteristics
The average age of the 66 participating youths was 16.9 years. There were no significant pretreatment differences between the FFT-CHR and EC groups on youths’ age, education, gender, ethnicity, prodromal syndromes, SOPS positive or negative symptom scale scores, Global Assessment of Functioning, use of antipsychotic medications, or family characteristics (See Table 3).
Table 3.
Clinical and Demographic Characteristics of the Sample
| Variable | EC (n = 28) | FFT-CHR (n = 38) | χ2 or t | p | Total (n = 66) |
|---|---|---|---|---|---|
| Youth characteristics | |||||
| Age: M (SD) | 16.5 (2.50) | 17.2 (4.24) | <1 | .43 | 16.9 (3.6) |
| Years of education: M (SD) | 9.96 (2.35) | 10.39 (3.09) | <1 | .54 | 10.2 (2.79) |
| Gender: % (n) | .02 | .88 | |||
| Male | 57.1 (n = 16) | 55.2 (n = 21) | 56.1 (n = 37) | ||
| Ethnicity: % (n) | 3.77 | .71 | |||
| African American | 3.6 (n = 1) | 10.5 (n = 4) | 7.6 (n = 5) | ||
| Asian American | 7.1 (n = 2) | 7.9 (n = 3) | 7.6 (n = 5) | ||
| Caucasian | 67.9 (n = 19) | 50 (n = 19) | 57.6 (n = 38) | ||
| Hispanic American | 10.7 (n = 3) | 15.8 (n = 6) | 13.6 (n = 9) | ||
| Multiracial | 7.1 (n = 2) | 7.9 (n = 3) | 7.6 (n = 5) | ||
| Native American | 3.6 (n = 1) | 2.6 (n = 1) | 3.0 (n = 2) | ||
| Declined identification | 0 | 5.3 (n = 2) | 3.0 (n = 2) | ||
| Prodromal syndrome: % (n) | 3.99 | .41 | |||
| Attenuated positive symptoms | 85.7 (n = 24) | 89.5 (n = 34) | 88.0 (n = 58) | ||
| Genetic risk and deterioration | 7.1 (n = 2) | 10.5 (n = 4) | 9.0 (n = 6) | ||
| Brief intermittent psychosis | 7.1 (n = 2) | 0.0 (n = 0) | 3.0 (n = 2) | ||
| SOPS Positive Symptoms Scale: M (SD) | 11.7 (3.66) | 11.8 (3.41) | <1 | .86 | 11.7 (3.49) |
| SOPS Negative Symptoms Scale: M (SD) | 11.6 (6.48) | 12.8 (6.32) | <1 | .47 | 12.3 (6.36) |
| Global Assessment of Functioning: M (SD) | 47.5 (10.39) | 47.2 (7.91) | <1 | .87 | 47.4 (8.96) |
| Antipsychotic medications: % (n) | 3.38 | .07 | |||
| Yes | 35.7 (n = 10) | 15.8 (n = 6) | 25.4 | ||
| DSM–IV diagnoses: % (n) | |||||
| Major Depressive Disorders | 28.6 (n = 8) | 39.5 (n = 15) | <1 | .36 | 34.8 (n = 23) |
| Bipolar Disorders | 7.1 (n = 2) | 5.3 (n = 2) | <1 | .75 | 6 (n = 4) |
| Substance Disorders | 3.6 (n = 1) | 5.3 (n = 2) | 2.84 | .42 | 4.5 (n = 3) |
| Anxiety Disorders | 50 (n = 14) | 42.1 (n = 16) | <1 | .52 | 45.5 (n = 30) |
| Eating Disorders | 3.6 (n = 1) | 0 (n = 0) | 1.38 | .24 | 1.5 (n = 1) |
| Attention Deficit Disorders | 17.9 (n = 5) | 21.1 (n = 8) | <1 | .75 | 19.5 (n = 13) |
| Learning Disorders | 7.1 (n = 2) | 10.5 (n = 4) | <1 | .64 | 9 (n = 6) |
| Developmental Disorders | 7.1 (n = 2) | 5.3 (n = 2) | <1 | .75 | 6 (n = 4) |
| Oppositional Defiant Disorder | 3.6 (n = 1) | 5.3 (n = 2) | <1 | .74 | 4.5 (n = 3) |
|
| |||||
| Family characteristics | |||||
| Fathers’ age: M (SD) | 49.2 (7.36) | 49.4 (7.23) | <1 | .90 | 49.3 (7.23) |
| Mothers’ age: M (SD) | 47.5 (7.15) | 45.3 (6.08) | 1.33 | .19 | 46.2 (6.59) |
| Fathers’ education: % (n) | <1 | .88 | |||
| Primary school | 7.1 (n = 2) | 7.9 (n = 3) | 7.8 (n = 5) | ||
| Some high school | 25 (n = 7) | 23.7 (n = 9) | 25 (n = 16) | ||
| Some college | 46.4 (n = 13) | 50 (n = 19) | 50 (n = 32) | ||
| Some graduate school | 21.4 (n = 6) | 13.2 (n = 5) | 17.2 (n = 11) | ||
| Mothers’ education: % (n) | 1.41 | .70 | |||
| Primary school | 3.6 (n = 1) | 2.6 (n = 1) | 3.1 (n = 2) | ||
| Some high school | 14.2 (n = 4) | 26.3 (n = 10) | 21.5 (n = 14) | ||
| Some college | 53.6 (n = 15) | 44.7 (n = 17) | 49.2 (n = 32) | ||
| Some graduate school | 25 (n = 7) | 26.3 (n = 10) | 26.2 (n = 17) | ||
Note. EC = enhanced care; FFT-CHR = family focused therapy–clinical high risk; SOPS = Scale of Prodromal Symptoms; DSM–IV = Diagnostic and Statistical Manual of Mental Disorders (4th ed.; American Psychiatric Association, 1994).
There were no significant correlations between baseline SOPS positive scores and youths’ (r = −.12, p = .34), mothers’ (r = −.16, p = .23), or fathers’ (r = −.29, p = .07) constructive behavior during baseline problem-solving interactions or between baseline SOPS negative symptom scores and youths’ (r = −.10, p = .45), mother’s (r = −.19, p = .16), or father’s (r = .03, p = .87) constructive behavior during baseline problem-solving interactions.
Topics That Created Tension for Family Members
Youths reported that irritability with family members created the greatest tension in their homes (M = 3.23; SD = 1.39), followed by communication (M = 3.03; SD = 1.37) and chores (M = 3.01; SD = 1.35). Mothers reported that chores generated the most tension at home (M = 3.43; SD = 1.46), followed by communication (M = 3.36; SD = 1.24) and irritability with family members (M = 3.24; SD = 1.51); fathers/significant others reported that chores generated the most tension (M = 3.37; SD = 1.27), followed by irritability with family members (M = 3.21; SD = 1.34) and communication (M = 3.14; SD = 1.32).
Family Communication During Problem-Solving Interactions
The mean duration of baseline interactions was 9.64 min (range 3.38–10.83) and of follow-up interactions was 9.20 min (range 3.48–10.97). There were no significant differences between treatment groups in duration of family problem-solving interaction at baseline, t(94) < 1, p = ns; EC M = 9.6, SD = 1.2; FFT-CHR M = 9.6, SD = 1.4, or follow-up, t(64) < 1, p = ns; EC M = 9.4, SD = 1.9; FFT-CHR M = 9.1, SD = 1.9.
Family communication
Given that the coded data were expressed as proportions and were mildly skewed, the codes were transformed using square root or log transformations, producing distributions that closely approximated normal Gaussian curves. We report means and standard deviations of the raw variables for ease of interpretation.
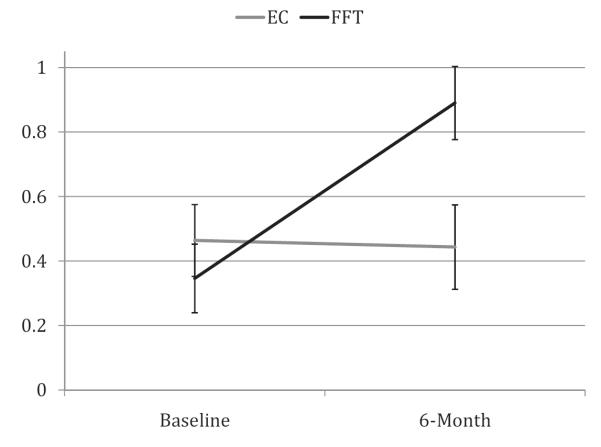
For the constructive behavior summary code there was a significant Treatment × Time interaction (see Table 4) with family members in EC (n = 28) exhibiting similar levels of constructive behavior at baseline and 6 months, whereas family members in FFT-CHR (n = 38) demonstrated a significant increase in constructive behavior from baseline to 6 months (See Figure 2). Family members in FFT-CHR expressed significantly higher rates of constructive behavior than family members in EC at 6 months, t(280) = −2.90, p = .004. Given that the Treatment × Time analysis was significant for the constructive behavior summary code, follow-up analyses were conducted to better specify the nature of the changes in family communication. Multilevel ANOVAs identified significant Treatment × Time interactions for both the calm– constructive and critical– conflictual summary codes, with families who received EC demonstrating similar proportions of coded behavior at baseline and follow-up while families who received FFT-CHR showed a significant increase in calm– constructive, t(280) = −5.96, p < .0001, and a significant decrease in critical– conflictual behavior, t(280) = 6.50, p < .0001. Further follow-up analyses on individual codes indicated that the changes in family members’ calm– constructive behaviors were largely the result of significant increases in active listening and calm speaking among family members who had received FFT-CHR. Changes in critical– conflictual codes were due to decreases in anger and irritability, complaints and criticism, and off-task behavior by family members in FFT-CHR. In all of the analyses just summarized, the Treatment × Time × Person interaction effect was not significant (Table 4), indicating that the improved communication patterns associated with FFT-CHR held equally across the identified patient and his or her mother and/or father/significant other. Further, neither the overall summary code nor any of the subcodes varied significantly by site (all ps > .90).
Table 4.
Raw Means, Standard Deviations, and F Tests for Proportions Calculated for Coded Individual Data Analyzed by Family
| EC (n = 28) |
FFT-CHR (n = 38) |
|||||
|---|---|---|---|---|---|---|
| Baseline |
6 months |
Baseline |
6 months |
F
|
||
| Variable | M (SD) | M (SD) | M (SD) | M (SD) | TX × T | TX × T × FM |
| Constructive behavior | .46 (.76) | .47 (.81) | .29 (.85) | .87 (.51) | 16.97** | .06 |
| Calm–constructive codes | .94 (.40) | .94 (.39) | .85 (.41) | 1.13 (.33) | 13.97** | .59 |
| 1. Affection and Compliments | .05 (.07) | .06 (.08) | .03 (.05) | .04 (.06) | 0 | .16 |
| 2. Mild Listening | 04 (.08) | .06 (.09) | .05 (.07) | .05 (.08) | .01 | 1.48 |
| 3. Active Listening | .21 (.19) | .19 (.18) | .19 (.17) | .26 (.20) | 9.47** | 1.71 |
| 4. Calm Speaking | .60 (.24) | .61 (.23) | .56 (.26) | .74 (.17) | 9.06** | 1.61 |
| 5. Organization | .04 (.06) | .03 (.04) | .03 (.05) | .03 (.05) | 2.48 | .36 |
| Critical–conflictual codes | .49 (.40) | .48 (.47) | .57 (.47) | .24 (.25) | 18.00** | .28 |
| 1. Irritability and Anger | .15 (.23) | .14 (.23) | .23 (.25) | .08 (.13) | 9.51** | .15 |
| 2. Complaints and Criticism | .07 (.10) | .07 (.12) | .08 (.11) | .03 (.06) | 8.70** | .92 |
| 3. Cutoffs | .17 (.16) | .14 (.15) | .14 (.13) | .08 (.09) | 2.33 | 2.60 |
| 4. Off-Task Comments | .07 (.13) | .11 (.17) | .08 (.14) | .04 (.09) | 16.50** | .08 |
Note. EC = enhanced care; FFT-CHR = family focused therapy–clinical high risk; TX = treatment; T = time; FM = family member.
p < .01.
Figure 2.
Proportions of family members’ constructive behavior during problem-solving interactions. Error bars represent standard errors of the mean. EC = enhanced care; FFT = family focused therapy.
Discussion
This study examined changes in constructive communication during family problem-solving interactions among youths at clinical high risk for psychosis and their families who participated in a randomized controlled trial of family focused treatment. Youths, mothers, and fathers/significant others who participated in family treatment that provided psychoeducation, communication and problem-solving training demonstrated improvement from baseline to follow-up in constructive communication during family problem-solving interactions, whereas those who received three sessions of psychoeducation maintained pretreatment levels of constructive communication. Family members who participated in FFT-CHR spoke more calmly and clearly, engaged in more active listening, demonstrated less irritable and angry affect, complained less about other family members, made fewer critical remarks, and provided fewer off-task comments during follow-up problem-solving interactions compared to baseline. Essentially, FFT-CHR appears to be effective in lowering high EE behaviors and enhancing supportive family communication. Importantly, these effects were consistent across the identified patient as well as the family members participating in therapy.
These findings were not due to differential attrition rates between treatment groups. Analyses of constructive behaviors during baseline interactions, youths’ baseline symptoms, and demographic variables comparing those who did to those who did not participate in follow-up interactions found that there were no significant differences in youths’, mothers’, or fathers’/significant others’ baseline constructive behavior or demographics for either the FFT-CHR or EC group. Also, it is unlikely that coder bias would have accounted for these findings since coders were blind to treatment group and were able to guess the baseline versus follow-up status of the interaction as often as they would by chance.
Improvement in family communication is an important treatment outcome for CHR youths and their families. At baseline, youths, mothers, and fathers/significant others all rated irritability among family members and family communication as two of the top three sources of tension within their families. Evidence that irritability and criticism had been reduced and that communication had become more calm and supportive during family problem-solving discussions within a clinic setting suggests that family members have developed skills to reduce tension in areas they deem important. Whether these skills are used in the day-to-day lives of families remains to be determined.
Our results are consistent with studies conducted on individuals with schizophrenia and bipolar illness that found that explicit training in communication and problem-solving techniques were associated with greater improvement in family atmosphere than was family support (Mueser et al., 2001), individual supportive therapy (Doane et al., 1986), or crisis management (Simoneau et al., 1999). These findings contrast with previous work conducted on older patients with schizophrenia (average age = 31) who had far less contact with their families than our current sample, which found that explicit training in communication and problem solving within an applied family management intervention was not more effective than family support groups in improving family communication (Bellack, Haas, Schooler, & Flory, 2000). FFT-CHR may be optimally useful for CHR youths who are spending significant amounts of time with their families and may have ample opportunity to practice communication techniques taught during treatment.
Limitations
These findings were achieved within the constraints of a randomized clinical trial that did not allow for exact matching of family requests for communication and problem-solving training with the provision of those techniques. Possibly, improvement in family communication is more striking when conducted exclusively with families who have specifically sought out those interventions. Nonetheless, these results do provide an empirical basis for recommending FFT-CHR to CHR youths and their family members who are seeking to improve family communication and reduce irritability among family members.
The generalizability of the results is limited by the fact that CHR youths who are living with their families of origin or their significant others and are willing to participate in a randomized clinical trial of family therapy represent only a portion of the total sample of CHR youths. Some CHR youths are alienated from their families and some youths and/or parents refuse to participate in family treatment. Additional empirically based individual approaches to treatment (Morrison et al., 2004) may be important alternatives for CHR youths. However, few individual interventions with this population have focused on the development of communication and problem-solving skills.
The majority of participants in this study did not have comorbid substance dependence disorders. Although a manual has been developed for addressing substance issues within the context of FFT-CHR treatment (Goldstein, Goldstein, & Miklowitz, 2008), the effectiveness of those approaches with a CHR population has yet to be evaluated. Also, approximately half of the families that were randomized did not complete the 6-month interaction task. While factors such as motivation were not measured, it is possible that only the most enthusiastic and conscientious families completed the study, and improvement in family communication in response to this structured treatment may require those family characteristics. At the same time, those family characteristics alone were not sufficient to stimulate improvement in family communication among families who received three sessions of psychoeducation.
Because we compared a relatively intensive 18-session family treatment to a brief three-session family treatment, it is not clear whether the training in communication and problem-solving techniques rather than a stronger dose of therapist contact led to the improvements in communication for the FFT-CHR group. Also this was a clinic-based study with highly trained, enthusiastic, and well-supervised therapists. It is unclear whether the same results would be found with a community-based sample with randomly selected therapists, less rigorous training and supervision, and a broader array of patients. However, this study was conducted across eight sites using many different therapists and a variety of patients with substantial diagnostic comorbidity.
Conclusion
While much investigation of family treatment with CHR populations remains to be done, this study offers a preliminary indication that relatively brief (18-session) family treatment that is clearly articulated and well supervised can bring about significant improvements in family communication, a domain of high importance to CHR youths and families. Future work will examine whether family intervention and its effect on communication leads to reduction in prodromal symptoms and risk for conversion to psychosis and improvement in functional outcomes for CHR youths.
Acknowledgments
This study was supported by a Challenge Grant (RC1 MH088546) to Tyrone D. Cannon and by a gift to the UCLA Foundation from the International Mental Health Research Organization (IMHRO). Development of the treatment manuals was supported by gifts from the Rinaldi, Lindner, and Staglin families.
The authors would like to thank the families who participated in this randomized trial, therapists on the project (Ayesha Delany Brumsey, Kristin A. Candan, Sandra D. De Silva, Isabel Domingues, Michelle Friedman-Yakoobian, Erin Jones, Stephanie Lord, Nora MacQuarrie, Catherine Marshall, Sarah Marvin, Shauna McManus, Silvia Saade, Danielle Schlosser, Shana Smith, Katherine Tsai, Miguel Villodas, Barbara C. Walsh, Kanchana Wijesekera, Kristen A. Woodberry, and Jamie L. Zinberg), transcribers and coders (Elizabeth Cabana, Anna Chen, Kelsey Hwang, Zia Kanani, Lynn Leveille, Amber Kincaid, Ashley Kusuma, Grace Lee, Phuong Nguyen, Stefan Nguyen, Christine Sayegh, and Alex Wonnaparhown), and project coordinators (Angie Andaya, Elisa Rodriguez, and Serine Uguryan).
Footnotes
The term youth is used throughout this article to describe youths and young adults.
Contributor Information
Mary P. O’Brien, Department of Psychiatry, University of California, Los Angeles, School of Medicine
David J. Miklowitz, Department of Psychiatry, University of California, Los Angeles, School of Medicine
Kristin A. Candan, Division of Psychiatry Research, The Zucker Hillside Hospital, North Shore–Long Island Jewish Health System, Glen Oaks, New York
Catherine Marshall, Hotchkiss Brain Institute, Department of Psychiatry, University of Calgary, Calgary, Alberta, Canada.
Isabel Domingues, Department of Psychiatry, University of California, San Diego.
Barbara C. Walsh, Department of Psychiatry, Yale University School of Medicine
Jamie L. Zinberg, Department of Psychology, University of California, Los Angeles
Sandra D. De Silva, Center for the Assessment and Prevention of Prodromal States, University of California, Los Angeles
Kristen A. Woodberry, Beth Israel Deaconess Medical Center, Harvard Medical School
Tyrone D. Cannon, Department of Psychiatry and Department of Psychology, University of California, Los Angeles
References
- Addington J, Cadenhead K, Cornblatt B, Mathalon D, McGlashan T, Perkins D, Cannon TD. North American Prodrome Longitudinal Study (NAPLS 2): Overview and recruitment. Schizophrenia Research. 2012;142(1–3):77–82. doi: 10.1016/j.schres.2012.09.012. doi:10.1016/j.schres.2012.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Addington J, Cornblatt BA, Cadenhead KS, Cannon TD, McGlashan TH, Perkins DO, Heinssen R. At clinical high risk for psychosis: Outcome for nonconverters. American Journal of Psychiatry. 2011;168:800–805. doi: 10.1176/appi.ajp.2011.10081191. doi:10.1176/appi.ajp.2011.10081191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Addington J, Penn D, Woods SW, Addington D, Perkins DO. Social functioning in individuals at clinical high risk for psychosis. Schizophrenia Research. 2008;99:119–124. doi: 10.1016/j.schres.2007.10.001. doi:10.1016/j.schres.2007.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: 1994. Author. [Google Scholar]
- Bellack AS, Haas GL, Schooler NR, Flory JD. Effects of behavioural family management on family communication and patient outcomes in schizophrenia. British Journal of Psychiatry. 2000;177:434–439. doi: 10.1192/bjp.177.5.434. doi:10.1192/bjp.177.5.434. [DOI] [PubMed] [Google Scholar]
- Bellack AS, Haas GL, Tierney AM. A strategy for assessing family interaction patterns in schizophrenia. Psychological Assessment. 1996;8:190–199. doi:10.1037/1040-3590.8.2.190. [Google Scholar]
- Bellack AS, Sayers M, Mueser KT, Bennett M. Evaluation of social problem solving in schizophrenia. Journal of Abnormal Psychology. 1994;103:371–378. doi: 10.1037//0021-843x.103.2.371. doi:10.1037/0021-843X.103.2.371. [DOI] [PubMed] [Google Scholar]
- Blanchard JJ, Sayers SL, Collins LM, Bellack AS. Affectivity in the problem-solving interactions of schizophrenia patients and their family members. Schizophrenia Research. 2004;69:105–117. doi: 10.1016/j.schres.2003.07.008. doi:10.1016/j.schres.2003.07.008. [DOI] [PubMed] [Google Scholar]
- Butzlaff RL, Hooley JM. Expressed emotion and psychiatric relapse: A meta-analysis. Archives of General Psychiatry. 1998;55:547–552. doi: 10.1001/archpsyc.55.6.547. [DOI] [PubMed] [Google Scholar]
- Cannon TD, Cadenhead K, Cornblatt B, Woods SW, Addington J, Walker E, Heinssen R. Prediction of psychosis in youth at high clinical risk. Archives of General Psychiatry. 2008;65:28–37. doi: 10.1001/archgenpsychiatry.2007.3. doi:10.1001/archgenpsychiatry.2007.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Silva S, Zinberg JL, O’Brien MP, Schlosser DA, Miklowitz DJ, Cannon TD. Treatment manual for NAPLS enhanced care condition (EC) University of California at Los Angeles; 2009. Unpublished manuscript. [Google Scholar]
- Dixon LB, Dickerson F, Bellack AS, Bennett M, Dickinson D, Goldberg RW, Kreyenbuhl J. The 2009 Schizophrenia PORT psychosocial treatment recommendations and summary statements. Schizophrenia Bulletin. 2010;36:48–70. doi: 10.1093/schbul/sbp115. doi:10.1093/schbul/sbp115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doane JA, Goldstein MJ, Miklowitz DJ, Falloon IR. The impact of individual and family treatment on the affective climate of families of schizophrenics. British Journal of Psychiatry. 1986;148:279–287. doi: 10.1192/bjp.148.3.279. doi:10.1192/bjp.148.3.279. [DOI] [PubMed] [Google Scholar]
- Efron B. Forcing a sequential experiment to be balanced. Biometrika. 1971;58:403–417. doi:10.1093/biomet/58.3.403. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM–IV–TR Axis I Disorders: Research version, patient edition (SCID-I/P) New York State Psychiatric Institute; New York, NY: 2002. [Google Scholar]
- French P, Morrison AP. Early detection and cognitive therapy for people at high risk of developing psychosis: A treatment approach. Wiley; West Sussex, England: 2004. [Google Scholar]
- Fusar-Poli P, Nelson B, Valmaggia L, Yung AR, McGuire PK. Comorbid depressive and anxiety disorders in 509 individuals with an at-risk mental state: Impact on psychopathology and transition to psychosis. Schizophrenia Bulletin. 2012 doi: 10.1093/schbul/sbs136. Advance online publication. doi:10.1093/schbul/sbs136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glyn SM, Cohen AN, Dixon LB, Niv N. The potential impact of the recovery movement on family interventions for schizophrenia: Opportunities and obstacles. Schizophrenia Bulletin. 2006;32:451–463. doi: 10.1093/schbul/sbj066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein BI, Goldstein TR, Miklowitz DJ. Integrating a substance use disorder (SUD) perspective into family-focused therapy of adolescents with bipolar disorder (FFT-A) 2008. Unpublished manuscript.
- González-Blanch C, Martin-Muñoz V, Pardo-García G, Martinez-García O, Álvarez-Jiménez M, Rodríguez-Sánchez JM, Crespo-Facorro B. Effects of family psychoeducation on expressed emotion and burden of care in first-episode psychosis: A prospective observational study. Spanish Journal of Psychology. 2010;13:389–395. doi: 10.1017/s1138741600003942. doi:10.1017/S1138741600003942. [DOI] [PubMed] [Google Scholar]
- Gonzalez-Pinto A, Ruiz de Azua S, Ibanez B, Otero-Cuesta S, Castro-Fornieles J, Graell-Berna M, Arango C. Can positive family factors be protective against the development of psychosis? Psychiatry Research. 2011;186:28–33. doi: 10.1016/j.psychres.2010.05.015. [DOI] [PubMed] [Google Scholar]
- Hamilton EB, Asarnow J, Tompson M. Family interaction styles of children with depressive disorders, schizophrenia-spectrum disorders, and normal controls. Family Process. 1999;38:463–476. doi: 10.1111/j.1545-5300.1999.00463.x. [DOI] [PubMed] [Google Scholar]
- Hawkins KA, McGlashan TH, Quinlan D, Miller TJ, Perkins DO, Zipursky RB, Woods SW. Factorial structure of the Scale of Prodromal Symptoms. Schizophrenia Research. 2004;68:339–347. doi: 10.1016/S0920-9964(03)00053-7. doi:10.1016/S0920-9964(03)00053-7. [DOI] [PubMed] [Google Scholar]
- Hooley JM. Expressed emotion and relapse of psychopathology. Annual Review of Clinical Psychology. 2007;3:329–352. doi: 10.1146/annurev.clinpsy.2.022305.095236. doi:10.1146/annurev.clinpsy.2.022305.095236. [DOI] [PubMed] [Google Scholar]
- Hooley JM, Gotlib IH. A diathesis-stress conceptualization of expressed emotion and clinical outcome. Journal of Applied and Preventive Psychology. 2000;9:135–151. [Google Scholar]
- Hooley JM, Richters JE. Expressed emotion: A developmental perspective. In: Cicchetti D, Toth SL, editors. Rochester Symposium on Developmental Psychopathology. Vol. 6. University of Rochester Press; Rochester, NY: 1995. pp. 133–166. [Google Scholar]
- Ierago L, Malsol C, Singeo T, Kishigama Y, Blailes F, Ord L, Ngiralmau H. Adoption, family relations and psychotic symptoms among Palauan adolescents who are genetically at risk for developing schizophrenia. Social Psychiatry and Epidemiology. 2010;45:1105–1114. doi: 10.1007/s00127-009-0154-x. doi:10.1007/s00127-009-0154-x. [DOI] [PubMed] [Google Scholar]
- Johnson JG, Cohen P, Kasen S, Smailes E, Brook JS. Association of maladaptive parental behavior with psychiatric disorder among parents and their offspring. Archives of General Psychiatry. 2001;58:453–460. doi: 10.1001/archpsyc.58.5.453. [DOI] [PubMed] [Google Scholar]
- Kumpfer KL, Alvarado R. Family-strengthening approaches for the prevention of youth problem behaviors. American Psychologist. 2003;58:457–465. doi: 10.1037/0003-066X.58.6-7.457. [DOI] [PubMed] [Google Scholar]
- Lemos S, Vallina O, Fernandez P, Ortega JA, Garcia P, Gutierrez A, Miller T. Predictive validity of the Scale of Prodromal Symptoms (SOPS) Actas Españolas de Psiquiatría. 2006;34:216–223. [PubMed] [Google Scholar]
- Linszen D, Dingemans P, ven der Does JW, Nugter A, Scholte P, Lenoir R, Goldstein MJ. Treatment, expressed emotion and relapse in recent onset schizophrenic disorders. Psychological Medicine. 1996;26:333–342. doi: 10.1017/s0033291700034723. doi:10.1017/S0033291700034723. [DOI] [PubMed] [Google Scholar]
- Lukoff D, Synder KS, Ventura J, Nuechterlein KH. Life events, familial stress and coping in the developmental course of schizophrenia. Schizophrenia Bulletin. 1984;10:258–292. doi: 10.1093/schbul/10.2.258. [DOI] [PubMed] [Google Scholar]
- Marvin SE, Miklowitz DJ, O’Brien MP, Cannon TD. Family-focused therapy for youth at clinical high risk of psychosis: Treatment fidelity within a multisite randomized trial. 2013. Manuscript submitted for publication. [DOI] [PMC free article] [PubMed]
- McCombs A, Forehand R, Smith K. The relationship between maternal problem-solving style and adolescent social adjustment. Journal of Family Psychology. 1988;2:57–66. doi:10.1037/h0080479. [Google Scholar]
- Miklowitz DJ, Axelson DA, Birmaher B, George EL, Taylor DO, Schneck CD, Brent DA. Family-focused treatment for adolescents with bipolar disorder: Results of a 2-year randomized trial. Archives of General Psychiatry. 2008;65:1053–1061. doi: 10.1001/archpsyc.65.9.1053. doi:10.1001/archpsyc.65.9.1053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miklowitz DJ, Goldstein MJ, Falloon IR, Doane JA. Interactional correlates of expressed emotion in the families of schizophrenics. British Journal of Psychiatry. 1984;144:482–487. doi: 10.1192/bjp.144.5.482. doi:10.1192/bjp.144.5.482. [DOI] [PubMed] [Google Scholar]
- Miklowitz DJ, O’Brien MP, Schlosser DA, Zinberg JZ, De Silva S, George EL, Cannon TD. Clinician’s treatment manual for Family-Focused Therapy for Prodromal Youth (FFT-PY) 2010. Unpublished treatment manual.
- Miller TJ, McGlashan TH, Rosen JL, Cadenhead K, Cannon T, Ventura J, Woods SW. Prodromal assessment with the Structured Interview for Prodromal Syndromes and the Scale of Prodromal Symptoms: Predictive validity, inter-rater reliability, and training to reliability. Schizophrenia Bulletin. 2003;29:703–715. doi: 10.1093/oxfordjournals.schbul.a007040. doi:10.1093/oxfordjournals.schbul.a007040. [DOI] [PubMed] [Google Scholar]
- Miller TJ, McGlashan TH, Rosen JL, Somjee L, Markovich P, Stein K, Woods SW. Prospective diagnosis of the initial prodrome for schizophrenia based on the Structured Interview for Prodromal Syndromes: Preliminary evidence of inter-rater reliability and predictive validity. American Journal of Psychiatry. 2002;159:863–865. doi: 10.1176/appi.ajp.159.5.863. doi:10.1176/appi.ajp.159.5.863. [DOI] [PubMed] [Google Scholar]
- Miller TJ, Zipursky RB, Perkins D, Addington J, Woods SW, Hawkins KA, McGlashan TH. The PRIME North America randomized double-blind clinical trial of olanzapine versus placebo in patients at risk of being prodromally symptomatic for psychosis: II. Baseline characteristics of the “prodromal” sample. Schizophrenia Research. 2003;61(1):19–30. doi: 10.1016/s0920-9964(02)00440-1. doi:10.1016/S0920-9964(02)00440-1. [DOI] [PubMed] [Google Scholar]
- Morrison AP, French P, Walford L, Lewis SW, Kilcommons A, Green J, Bentall RP. Cognitive therapy for the prevention of psychosis in people at ultra-high risk. British Journal of Psychiatry. 2004;185:291–297. doi: 10.1192/bjp.185.4.291. doi:10.1192/bjp.185.4.291. [DOI] [PubMed] [Google Scholar]
- Mueser KT, Sengupta A, Bellack AS, Glick ID, Schooler NR, Xie H, Keith SJ. Family treatment and medication dosage reduction in schizophrenia: Effects on patient social functioning, family attitudes, and burden. Journal of Consulting and Clinical Psychology. 2001;69:3–12. doi:10.1037/0022-006X.69.1.3. [PubMed] [Google Scholar]
- Nuechterlein KH, Dawson ME. A heuristic vulnerability-stress model of schizophrenic episodes. Schizophrenia Bulletin. 1984;10:300–312. doi: 10.1093/schbul/10.2.300. doi:10.1093/schbul/10.2.300. [DOI] [PubMed] [Google Scholar]
- O’Brien MP, Gordon JL, Bearden CE, Lopez SR, Kopelowicz A, Cannon TD. Positive family environment predicts improvement in symptoms and social functioning among adolescents at imminent risk for onset of psychosis. Schizophrenia Research. 2006;81:269–275. doi: 10.1016/j.schres.2005.10.005. doi:10.1016/j.schres.2005.10.005. [DOI] [PubMed] [Google Scholar]
- O’Brien MP, Zinberg JL, Bearden CE, Lopez SR, Kopelowicz A, Daley M, Cannon TD. Parent attitudes and parent adolescent interaction in families of youth at risk for psychosis and with recent-onset psychotic symptoms. Early Intervention in Psychiatry. 2008;2:268–276. doi: 10.1111/j.1751-7893.2008.00088.x. [DOI] [PubMed] [Google Scholar]
- O’Brien MP, Zinberg JL, Ho L, Rudd A, Kopelowicz A, Daley M, Cannon TD. Problem solving interactions and 6-month symptomatic and functional outcomes in youth at ultra-high risk for psychosis and with recent onset psychotic symptoms: A longitudinal study. Schizophrenia Research. 2009;107:198–205. doi: 10.1016/j.schres.2008.10.008. doi:10.1016/j.schres.2008.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Otero S, Moreno-Iniguez M, Paya B, Castro-Fornieles J, Gonzalez-Pinto A, Baeza I, Arango-Lopez C. Twelve-month follow-up of family communication and psychopathology in children and adolescents with a first psychotic episode (CAFEPS study) Psychiatry Research. 2011;185:72–77. doi: 10.1016/j.psychres.2009.12.007. [DOI] [PubMed] [Google Scholar]
- Pakaslahti L, Karjalainen A, Keltikangas-Jarvinen L. Relationships between adolescent prosocial problem-solving strategies, prosocial behaviour, and social acceptance. International Journal of Behavioral Development. 2002;26:137–144. doi:10.1080/01650250042000681. [Google Scholar]
- Patterson GR. A social learning approach. Vol. 3. Coercive family process. Castalia; Eugene, OR: 1982. [Google Scholar]
- Patterson GR, Fisher PA. Recent developments in our understanding of parenting: Bidirectional effects, causal models, and the search for parsimony. In: Bornstein MH, editor. Handbook of parenting. 2nd ed Erlbaum; Mahwah, NJ: 2002. [Google Scholar]
- Patterson G, Reid J, Dishion T. Antisocial boys. Castalia; Eugene, OR: 1992. [Google Scholar]
- Pitschel-Walz G, Leucht S, Bauml J, Kissling W, Engel RR. The effect of family interventions on relapse and rehospitalization in schizophrenia—A meta-analysis. Schizophrenia Bulletin. 2001;27:73–92. doi: 10.1093/oxfordjournals.schbul.a006861. [DOI] [PubMed] [Google Scholar]
- Repetti RL, Taylor SE, Seeman TE. Risky families: Family social environments and the mental and physical health of offspring. Psychological Bulletin. 2002;128:330–366. doi:10.1037/0033-2909.128.2.330. [PubMed] [Google Scholar]
- Schlosser DA, Jacobson S, Chen Q, Sugar CA, Niendam TA, Li G, Cannon TD. Recovery from an at-risk state: Clinical and functional outcomes of putatively prodromal youth who do not develop psychosis. Schizophrenia Bulletin. 2011;38:1225–1233. doi: 10.1093/schbul/sbr098. doi:10.1093/schbul/sbr098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schlosser DA, Miklowitz DJ, O’Brien MP, De Silva SD, Zinberg JZ, Cannon TD. A randomized trial of family-focused treatment for adolescents and young adults at risk for psychosis: Study rationale, design and methods. Early Intervention in Psychiatry. 2012;6:283–291. doi: 10.1111/j.1751-7893.2011.00317.x. doi:10.1111/j.1751-7893.2011.00317.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shrout PE, Fleiss JL. Intraclass correlations: Uses in assessing rater reliability. Psychological Bulletin. 1979;86:420–428. doi: 10.1037//0033-2909.86.2.420. doi:10.1037/0033-2909.86.2.420. [DOI] [PubMed] [Google Scholar]
- Silverberg S, Steinberg L. Adolescent autonomy, parent-adolescent conflict, and parental well-being. Journal of Youth and Adolescence. 1987;16:293–312. doi: 10.1007/BF02139096. doi:10.1007/BF02139096. [DOI] [PubMed] [Google Scholar]
- Simoneau TL, Miklowitz DJ, Richards JA, a Saleem R, George EL. Bipolar disorder and family communication effects of a psychoeducational treatment program. Journal of Abnormal Psychology. 1999;108:588–597. doi: 10.1037//0021-843x.108.4.588. doi:10.1037/0021-843X.108.4.588. [DOI] [PubMed] [Google Scholar]
- Stalberg G, Lichtenstein P, Sandin S, Hultman CM. Video-based assessment of interpersonal problem solving skills in patients with schizophrenia, their siblings and non-psychiatric controls. Scandinavian Journal of Psychology. 2008;49:77–82. doi: 10.1111/j.1467-9450.2007.00615.x. [DOI] [PubMed] [Google Scholar]
- Steinberg L. We know some things: Parent-adolescent relationships in retrospect and prospect. Journal of Research on Adolescence. 2001;11:1–19. doi:10.1111/1532-7795.00001. [Google Scholar]
- Strachan AM, Leff JP, Goldstein MJ, Duone JA, Burtt C. Emotional attitudes and direction of communication in the families of schizophrenics: A cross-national replication. British Journal of Psychiatry. 1986;149:279–287. doi: 10.1192/bjp.149.3.279. doi:10.1192/bjp.149.3.279. [DOI] [PubMed] [Google Scholar]
- Sturgeon D, Kuipers L, Berkowitz R, Turpin G, Leff J. Psychophysiological responses of schizophrenic patients to high and low expressed emotion relatives. British Journal of Psychiatry. 1981;138:40–45. doi: 10.1192/bjp.138.1.40. doi:10.1192/bjp.138.1.40. [DOI] [PubMed] [Google Scholar]
- Tarrier N, Vaughn C, Lader MH, Leff JP. Bodily reactions to people and events in schizophrenia. Archives of General Psychiatry. 1979;36:311–315. doi: 10.1001/archpsyc.1979.01780030077007. doi:10.1001/archpsyc.1979.01780030077007. [DOI] [PubMed] [Google Scholar]
- Tienari P, Wynne LC, Sorri A, Lahti I, Laksy K, Moring J, Wahlberg K. Genotype-environment interaction in schizophrenia-spectrum disorder. British Journal of Psychiatry. 2004;184:216–222. doi: 10.1192/bjp.184.3.216. [DOI] [PubMed] [Google Scholar]
- Wahlberg K, Wynne LC, Oja H, Keskitalo P, Pykalainen L, Lahti I, Tienari P. Gene-environment interaction in vulnerability to schizophrenia: Findings from the Finnish Adoptive Family Study of Schizophrenia. American Journal of Psychiatry. 1997;154:355–362. doi: 10.1176/ajp.154.3.355. [DOI] [PubMed] [Google Scholar]
- Weisman A, Tompson MC, Okazaki S, Gregory J, Goldstein MJ, Rea M, Miklowitz DJ. Clinicians’ fidelity to a manual-based family treatment as a predictor of the one-year course of bipolar disorder. Family Process. 2002;41:123–131. doi: 10.1111/j.1545-5300.2002.40102000123.x. doi:10.1111/j.1545-5300.2002.40102000123.x. [DOI] [PubMed] [Google Scholar]
- Wong C, Davidson L, McGlashan T, Gerson R, Malaspina D, Corcoran C. Comparable family burden in families of clinical high-risk and recent-onset psychosis patients. Early Intervention in Psychiatry. 2008;2:256–261. doi: 10.1111/j.1751-7893.2008.00086.x. doi:10.1111/j.1751-7893.2008.00086.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woods SW, Walsh BC, Saksa JR, McGlashan TH. The case for including attenuated psychotic symptoms syndrome in DSM-5 as a psychosis risk syndrome. Schizophrenia Research. 2010;123:199–207. doi: 10.1016/j.schres.2010.08.012. doi:10.1016/j.schres.2010.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]