Abstract
Von Hippel-Lindau (VHL) syndrome is a rare neoplastic disorder characterized by central nervous system (CNS) and visceral tumors. We here present 68Ga-labelled [1, 4, 7, 10-tetraazacyclododecane-1, 4, 7, 10-tetraacetic acid]-1-Nal3-Octreotide positron emission tomography computed tomography findings in a 52 year old female with VHL syndrome, demonstrating both CNS and visceral tumors.
Keywords: Von Hippel-Lindau syndrome, 68Ga-DOTANOC, PET-CT, Hemangioblastoma, RCC, NET
INTRODUCTION
Von Hippel-Lindau (VHL) syndrome is an autosomal dominant neoplastic disorder. It is commonly characterised by retinal and central nervous system (CNS) hemangioblastomas, clear cell renal cell carcinoma (RCC), pheochromocytoma, pancreatic islet tumors and endolymphatic sac tumors (1). Diagnosis is generally clinical, although specific gene mutation can be demonstrated (2). Imaging plays an important role in diagnosis. 68Ga-labelled [1, 4, 7, 10-tetraazacyclododecane-1, 4, 7, 10-tetraacetic acid]-1-Nal3-Octreotide (68Ga-DOTANOC) positron emission tomography computed tomography (PET-CT) is now being routinely employed for somatostatin receptor (SSTR), based PET imaging at many centers. It binds to the cell membrane SSTR receptors (subtype 2, 3 and 5) and can be employed for high resolution PET imaging. 68Ga-DOTANOC PET-CT has proven to be very useful for imaging of neuroendocrine tumors (NET). We here present a case of a 52 year old lady with VHL syndrome, where 68Ga-DOTANOC PET-CT demonstrated both CNS and visceral tumors.
CASE REPORT
A 52-year-old lady remove was presented with an abdominal lump of 6-month in duration. She gave history of left eye surgery five years back, following an episode of sudden onset loss of vision. Since then, she had loss of vision in the left eye. There were no other CNS symptoms. She also gave history of similar eye surgery in her younger son (age-28 years), following a similar episode of unilateral loss of vision. On examination, she was not hypertensive. She had no perception of light in the left eye, while the right eye visual acuity was normal. Because of the presence of secondary cataract in the left eye, her posterior chamber could not be evaluated. There were no cerebellar signs. Abdominal examination revealed a large lump in the right upper and lower quadrant. Complete hemogram, renal function tests and liver function tests were normal.
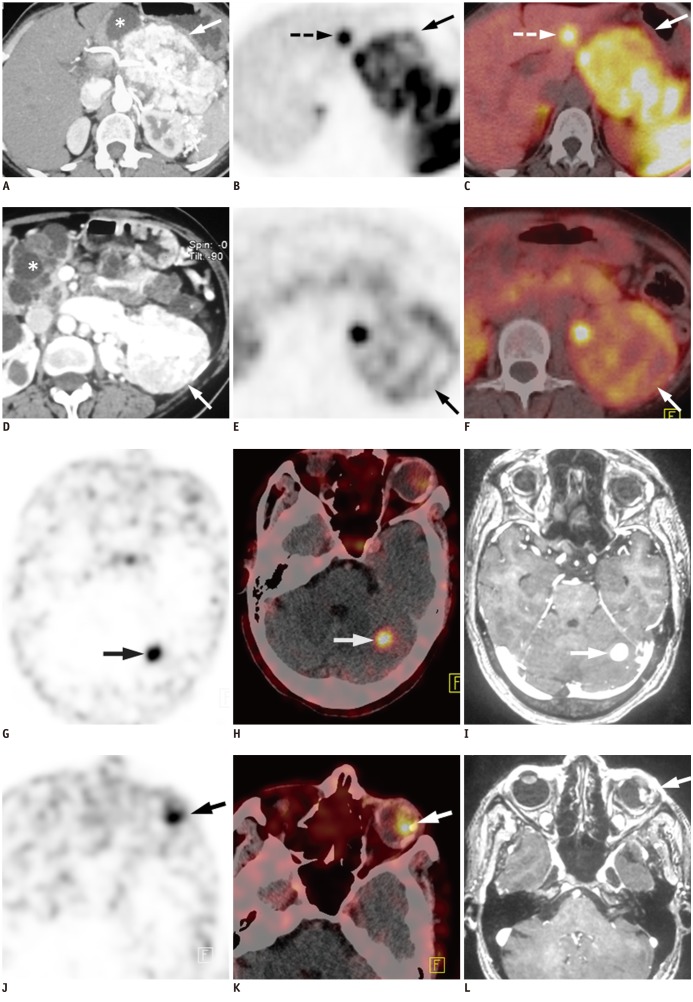
Contrast enhanced CT of the abdomen revealed a hypervascular mass (7.8 × 5.8 × 5.1 cm), arising from the interpolar region of the left kidney with multiple feeding vessels arising from the left renal artery and supplying the mass (Fig. 1A, D). The findings were suspicious for RCC. Multiple cortical cysts were also seen in both kidneys. Another large (9.6 × 7.4 × 5.4 cm) hypervascular mass lesion was seen in the body and tail of the pancreas, which was suspicious for metastasis from RCC (Fig. 1A). Bilateral adrenals were normal. Because of the hypervascular nature of pancreatic mass biopsy was not attempted.
Fig. 1.
52-year-old female with Von Hippel-Lindau syndrome.
Transaxial contrast enhanced CT (A) of abdomen show large (9.6 × 7.4 × 5.4 cm) mass lesion in region of body and tail of pancreas with intense post contrast enhancement (arrow). Multiple cysts of varying sizes are noted in rest of pancreas (asterix). Also, note tortuous blood vessels in peripancreatic and perisplenic location. Transaxial PET (B) and PET-CT (C) images show intense heterogeneous uptake of 68Ga-labelled [1, 4, 7, 10-tetraazacyclododecane-1, 4, 7, 10-tetraacetic acid]-1-Nal3-Octreotide (68Ga-DOTANOC) (SUVmax = 18.6) in pancreatic mass (arrow), thus confirming it to be NET. Focal 68Ga-DOTANOC uptake (SUVmax = 13.2) was also seen in segment III of liver (B, C, broken arrow) suggesting liver metastasis from pancreatic NET. This was confirmed at fine needle aspiration cytology. Transaxial contrast enhanced CT (D) of abdomen also shows another mass (7.8 × 5.8 × 5.1 cm) arising from interpolar region of left kidney and showing intense post contrast enhancement (arrow). Multiple feeding vessels are seen to arise from left renal artery and supply mass. These findings were suggestive of RCC. Also noted are bilateral multiple renal cortical cysts (asterix). PET (E) and PET-CT (F) images reveal mild 68Ga-DOTANOC uptake (SUVmax = 3.1) in renal mass (arrow). Transaxial PET (G) and PET-CT (H) images of brain show focal area of 68Ga-DOTANOC uptake (SUVmax = 9.9) in hypodense lesion (2 × 2 cm) in left cerebellum (arrow). Transaxial T2 weighted gadolinium enhanced MRI (I) of brain reveals nodular lesion in lateral half of left cerebellar hemisphere with intense post contrast enhancement (arrow), suggesting hemangioblastoma. Transaxial PET (J) and PET-CT (K) images also revealed focal 68Ga-DOTANOC uptake (SUVmax = 8.3) in lateral part of left globe, corresponding to heterogeneous nodular lesion (arrow). Transaxial T2 weighted gadolinium enhanced MRI (L) showed eccentric nodule in lateral part of left globe with intense post contrast enhancement, suggesting retinal hemangioblastoma (arrow).
Subsequently, SSTR PET-CT was done with 68Ga-DOTANOC to characterize the pancreatic mass. PET-CT revealed intense 68Ga-DOTANOC uptake (maximum standardised uptake value [SUVmax] = 18.6) in the pancreatic mass, characterizing it as a NET (Fig. 1B, C). It also demonstrated a solitary liver metastasis (segment III) with intense 68Ga-DOTANOC uptake (SUVmax = 13.2), confirming it to arising from pancreatic NET (Fig. 1B, C). The left renal mass showed only a mild 68Ga-DOTANOC uptake (SUVmax = 3.1) (Fig. 1E, F). Interestingly, a hypodense lesion was seen in the left cerebellum, showing increased 68Ga-DOTANOC uptake (SUVmax = 9.9) (Fig. 1G, H). Another focus of 68Ga-DOTANOC uptake was seen in a lateral part of the left globe (SUVmax = 8.3) corresponding to a heterogeneous lesion seen on CT (Fig. 1J, K).
Gadolinium enhanced magnetic resonance imaging (MRI) of the brain was done to characterise the CNS lesions seen on 68Ga-DOTANOC PET-CT. It showed a nodular lesion (2 × 2 cm) in the lateral half of the left cerebellar hemisphere with intense post contrast enhancement (Fig. 1I). An eccentric nodule was also noted in the lateral part of the left globe with intense post contrast enhancement (Fig. 1L). MRI findings were consistent with hemangioblastoma of the left retina and cerebellum. Imaging findings confirmed the diagnosis of VHL syndrome. Therefore, serum and urinary catecholamines levels were done for screening of pheochromocytoma and paraganglioma, and were found to be normal. Fine needle aspiration cytology from the liver lesion confirmed the diagnosis of metastatic NET. The patient is now being worked up for palliative radionuclide therapy with 177Lu-DOTATATE.
DISCUSSION
Von Hippel-Lindau syndrome is an autosomal dominantly inherited neoplastic disorder that demonstrates age-dependent penetrance and marked phenotypic variability. The basic underlying abnormality is mutations in the VHL tumour suppressor gene located on the short arm of chromosome 3 (3). Tumors are initiated by biallelic VHL inactivation and are associated with abnormal activation of the hypoxic gene response pathways. The most frequent tumors are retinal and CNS hemangioblastomas, followed by clear cell RCC, pheochromocytoma, pancreatic islet tumors and endolymphatic sac tumors (4). In addition, renal and pancreatic cysts, as well as epididymal or broad ligament cystadenomas also occur. All of the tumors that are typically found in VHL disease can occur as a sporadic event and so a clinical diagnosis of VHL disease in a patient without a positive family history requires the presence of two tumors (e.g., two haemangioblastomas or a haemangioblastomas and a visceral tumour). Although specific gene mutation can be demonstrated, diagnosis is generally clinical and depends primarily on imaging (2).
In the present case, 68Ga-DOTANOC PET-CT demonstrated both CNS and visceral tumors. Pancreatic tumors occur in 5-10% of cases of VHL and are usually solid nonsecretory islet cell tumors. 68Ga-DOTANOC PET-CT is very useful for the diagnosis and staging of pancreatic NET (5). Given the hypervascular nature of both RCC and NET, it could be difficult to differentiate metastatic RCC from pancreatic NET on CECT alone, as was in the present case. The problem became more complex as the pancreatic tumor was non-functioning. In our patient, 68Ga-DOTANOC PET-CT not only characterized the pancreatic mass as NET, it also demonstrated liver metastasis from the pancreatic NET. The left RCC also demonstrated mild 68Ga-DOTANOC uptake, confirming SSTR expression. Therefore, it should be remembered that primary RCC may also express SSTR, especially in cases with high aggressive behaviour (6). However, the clinical and diagnostic value of this observation remains unknown. Although there were no catecholamine producing tumor in the present patient, VHL syndrome is associated with higher risk of such tumors. Risk of pheochromocytoma and paraganglioma in VHL varies according to the clinical subtype and underlying VHL mutation. 68Ga-DOTANOC PET-CT has shown high accuracy for diagnosis and localisation of pheochromocytoma and paraganglioma (7). Therefore, it can be used to localize the lesion if biochemical workups are suggestive of catecholamine secreting tumors.
Central nervous system hemangioblastomas are cardinal feature of VHL syndrome and occur in 60-80% of VHL patients, with cerebellum being the most common site (8). VHL syndrome associated hemangioblastomas frequently expresses SSTR (9). Ambrosini et al. (10) have previously demonstrated in vivo SSTR expression in VHL associated hemangioblastoma with 68Ga-DOTANOC PET-CT. In the present case 68Ga-DOTANOC PET-CT detected previously unknown cerebellar hemangioblastoma, which was confirmed on contrast enhanced MRI. Retinal angiomas (hemangioblastoma) are the most common presenting feature of VHL disease as was in the present case, though not recognized at that point of time. 68Ga-DOTANOC PET-CT detected the retinal lesions and were subsequently confirmed with MRI. To our knowledge, there is no previous published report of imaging retinal hemangioblastoma with 68Ga-DOTANOC PET-CT.
We have presented here a classical case of rare VHL syndrome with cerebellar hemangioblastoma, retinal hemangioblastoma, RCC, metastatic pancreatic NET, pancreatic cysts and renal cysts, where 68Ga-DOTANOC PET-CT visualized all of the lesions. In addition, 68Ga-DOTANOC PET-CT also helped in selection of therapy with radiolabelled somatostatin analogue (177Lu-DOTATATE) in this patient. The findings of the present report are the first to highlight the utility of 68Ga-DOTANOC PET-CT based SSTR imaging in VHL syndrome for detecting CNS and visceral malignancies. Further evaluation of role of PET-CT based SSTR imaging in patients with or at risk of VHL syndrome is needed to delineate its role in routine management of such patients, both for diagnosis, as well as for deciding the therapeutic strategy. In our opinion, it should be routinely employed in such patients.
References
- 1.Richard S, Graff J, Lindau J, Resche F. Von Hippel-Lindau disease. Lancet. 2004;363:1231–1234. doi: 10.1016/S0140-6736(04)15957-6. [DOI] [PubMed] [Google Scholar]
- 2.Fanti S, Ambrosini V, Tomassetti P, Castellucci P, Montini G, Allegri V, et al. Evaluation of unusual neuroendocrine tumours by means of 68Ga-DOTA-NOC PET. Biomed Pharmacother. 2008;62:667–671. doi: 10.1016/j.biopha.2008.01.010. [DOI] [PubMed] [Google Scholar]
- 3.Maher ER, Iselius L, Yates JR, Littler M, Benjamin C, Harris R, et al. Von Hippel-Lindau disease: a genetic study. J Med Genet. 1991;28:443–447. doi: 10.1136/jmg.28.7.443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lonser RR, Glenn GM, Walther M, Chew EY, Libutti SK, Linehan WM, et al. von Hippel-Lindau disease. Lancet. 2003;361:2059–2067. doi: 10.1016/S0140-6736(03)13643-4. [DOI] [PubMed] [Google Scholar]
- 5.Kumar R, Sharma P, Garg P, Karunanithi S, Naswa N, Sharma R, et al. Role of (68)Ga-DOTATOC PET-CT in the diagnosis and staging of pancreatic neuroendocrine tumours. Eur Radiol. 2011;21:2408–2416. doi: 10.1007/s00330-011-2199-y. [DOI] [PubMed] [Google Scholar]
- 6.Reubi JC, Kvols L. Somatostatin receptors in human renal cell carcinomas. Cancer Res. 1992;52:6074–6078. [PubMed] [Google Scholar]
- 7.Naswa N, Sharma P, Nazar AH, Agarwal KK, Kumar R, Ammini AC, et al. Prospective evaluation of 68Ga-DOTA-NOC PET-CT in phaeochromocytoma and paraganglioma: preliminary results from a single centre study. Eur Radiol. 2012;22:710–719. doi: 10.1007/s00330-011-2289-x. [DOI] [PubMed] [Google Scholar]
- 8.Maher ER, Neumann HP, Richard S. von Hippel-Lindau disease: a clinical and scientific review. Eur J Hum Genet. 2011;19:617–623. doi: 10.1038/ejhg.2010.175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Reubi JC, Waser B, Laissue JA, Gebbers JO. Somatostatin and vasoactive intestinal peptide receptors in human mesenchymal tumors: in vitro identification. Cancer Res. 1996;56:1922–1931. [PubMed] [Google Scholar]
- 10.Ambrosini V, Campana D, Allegri V, Opocher G, Fanti S. 68Ga-DOTA-NOC PET/CT detects somatostatin receptors expression in von hippel-lindau cerebellar disease. Clin Nucl Med. 2011;36:64–65. doi: 10.1097/RLU.0b013e3181fef14a. [DOI] [PubMed] [Google Scholar]