Abstract
Cardiac computed tomography (CT) has emerged as a noninvasive modality for the assessment of coronary artery disease (CAD), and has been rapidly integrated into clinical cares. CT has changed the traditional risk stratification based on clinical risk to image-based identification of patient risk. Cardiac CT, including coronary artery calcium score and coronary CT angiography, can provide prognostic information and is expected to improve risk stratification of CAD. Currently used conventional cardiac CT, provides accurate anatomic information but not functional significance of CAD, and it may not be sufficient to guide treatments such as revascularization. Recently, myocardial CT perfusion imaging, intracoronary luminal attenuation gradient, and CT-derived computed fractional flow reserve were developed to combine anatomical and functional data. Although at present, the diagnostic and prognostic value of these novel technologies needs to be evaluated further, it is expected that all-in-one cardiac CT can guide treatment and improve patient outcomes in the near future.
Keywords: Cardiac computed tomography, Prognosis, Risk stratification
INTRODUCTION
In the diagnosis and management of coronary artery disease, risk stratification strategy aims to identify patients who are likely to have significant coronary artery disease (CAD) that might benefit from revascularization and/or aggressive medical treatment. The traditional risk stratification algorithm is based on risk factors including age, gender, smoking, blood pressure, cholesterol, and diabetes. In patients presenting with suspected CAD, a common strategy of risk stratification is the identification of ischemia by using functional modalities such as exercise electrocardiogram, dobutamine stress echocardiogrphy, or nuclear myocardial perfusion imaging. Cardiac computed tomography (CT) has emerged as a new noninvasive imaging modality for the assessment of CAD. During the past decade, cardiac CT has rapidly integrated into clinical care and has changed the traditional risk stratification based on clinical risk to image-based identification of patient risk. In this review, we discuss the current role and limits of cardiac CT in the risk stratification of patients with suspected CAD. We also introduce recent advances of cardiac CT, which allow simultaneous evaluation of the functional significance of CAD.
Prognostic Value of Coronary Arery Calcium Score
Coronary artery calcium is a marker of coronary atherosclerosis, and the quantity of coronary artery calcification is correlated with the coronary atherosclerotic plaque burden. Numerous studies have demonstrated that the coronary artery calcium score is associated with the risk of future cardiovascular events (1-5), and the detection of coronary artery calcification with cardiac CT has been extensively used for risk stratification. In a recent study from Multi-Ethnic Study of Atherosclerosis (MESA) (4), in a population-based cohort of individuals without known cardiovascular disease, 6722 subjects were followed for a median follow-up period of 3.8 years. The coronary calcium score contributed to the risk of both major coronary events (death from coronary heart disease and myocardial infarction [MI]) and any coronary events independently of other traditional risk factors. A doubling of the calcium score increased the estimated probability of both major events and any other coronary events by approximately 25%. In another study from MESA (5), 5878 subjects without known CAD were followed up for a median of 5.8 years. By adding calcium score to the prediction model based on traditional risk factors, 26% of the subjects were reclassified into lower or higher risk groups. In patients with adverse events (n = 209), 23% were reclassified as high risk, while in patients without adverse events (n = 2669), 13% were reclassified as low risk. In the entire cohort, net reclassification improvement was 0.25 (p < 0.001), demonstrating that adding calcium score to traditional risk factors significantly improved the classification of risk.
Although coronary artery calcium scoring reflects the coronary atherosclerotic plaque burden, the absence of coronary artery calcification does not exclude obstructive CAD with non-calcified plaque. Therefore, potentially vulnerable lesions may not be identified by calcium scoring (6, 7). In addition, most studies evaluating the prognostic value of calcium scoring were performed in western countries, so the relationship between the coronary artery calcium score and the risk of coronary events in various ethnic groups needs to be further studied. A recent study by Yoon et al. (7) evaluated the diagnostic usefulness of 'zero calcium score criteria' as a decision-making strategy to rule out CAD in the emergency department. Of 136 Korean patients who presented to the emergency department with acute chest pain, 92 (68%) had no detectable coronary calcification. However, 14 out of 92 (15%) had obstructive CAD in coronary CT angiography. In this study, 45 patients (33%) were subsequently diagnosed as having acute coronary syndrome, and 38% (17/45) of them showed zero calcium score.
Prognostic Value of Coronary CT Angiography
Coronary CT angiography has emerged as a noninvasive alternative for visualizing coronary arteries, and provides comprehensive information regarding the coronary anatomy, the presence of obstructive and nonobstructive CAD, and plaque characteristics. Coronary CT angiography has been shown to have high diagnostic accuracy to detect and exclude obstructive CAD (8-10). In addition, the data supporting the prognostic value of coronary CT angiography is also accumulating. A meta-analysis by Hulten et al. (11) evaluated 18 studies, including 9592 patients with a median follow-up of 20 months. The absence of CAD in coronary CT angiography an excellent prognosis with a pooled annualized event rate of major adverse cardiac events (death, MI, and revascularization) of 0.17%. Where coronary CT angiographic findings were abnormal, there were incrementally increasing adverse cardiac events with increasing CAD severity by coronary CT angiography.
Studies also have suggested superior prognostic value of coronary CT angiography compared with conventional risk factors. In a single-center study by Hadamitzky et al. (12), the prognostic value of coronary CT angiography was compared with that derived from clinical risk score and calcium score. The study followed 2223 patients undergoing both coronary artery calcium scoring and coronary CT angiography for the occurrence of cardiac death, MI, unstable angina, and late revascularization during a median follow-up period of 28 months. The coronary CT angiographic measure of CAD, with both stenosis severity and number of disease segments, was found to have significant incremental predictive value compared with the conventional risk score and the calcium score. Another single-center study by Chow et al. (13) followed 2076 patients with 64-slice coronary CT angiography for the occurrence of cardiac death and MI during a mean follow-up period of 16 months. Assessment of CAD severity, total plaque score, and left ventricular ejection fraction (LVEF) measured by coronary CT angiography had incremental prognostic value over traditional risk factors. The prognostic value of CT measure of CAD severity and LVEF were confirmed in a study from a large international multicenter cohort Coronary computed tomography angiography evaluation for clinical outcome: an international multicenter registry (14). A total of 14064 patients who underwent coronary CT angiography with concomitant CT LVEF assessment were followed for a mean of 22.5 months. CT measure of CAD severity and LVEF had independent prognostic value. In addition, both CAD severity and abnormal LVEF had incremental prognostic value over baseline clinical variables alone, and the CAD severity was incremental to LVEF + clinical variables.
Although coronary CT angiography has a good diagnostic accuracy for identification of anatomically significant CAD, and the presence of significant CAD on coronary CT angiography is associated with increased adverse cardiac events, the anatomically significant coronary stenosis does not always equate with functional significance. Therefore, the usefulness of coronary CT angiography as an alternative to stratify the risk of CAD needs to be studied. To our knowledge, 2 studies compared the prognostic value of coronary CT angiography to that from exercise or pharmacological stress tests. Cho et al. (15) followed 2977 patients with both coronary CT angiography and exercise electrocardiography for a median of 3.3 years. Both exercise electrocardiography and coronary CT angiography are independently predictive of adverse cardiac events including cardiac death, nonfatal MI, unstable angina, and late revascularization. Interestingly, in subgroup analyses, coronary CT angiography stratifies risk in both groups with negative and positive exercise electrocardiographic finding, while exercise electrocardiogram stratifies risk of adverse cardiac events only in group with moderate or severe stenosis in coronary CT angiography. When they calculated C-statistics, both exercise electrocardiography and coronary CT angiography improved risk stratification beyond clinical risk factors. However, the exercise electrocardiogram in addition to coronary CT angiography could not provide better discrimination. The incremental prognostic value of coronary CT angiography over single-photon emission computed tomography (SPECT) had been also evaluated in a single-center study involving 541 patients with a median follow-up duration of 22 months (16). The presence or absence of significant stenosis in coronary CT angiography was an independent predictor of adverse cardiac events and provides incremental value to SPECT. Further, the addition of plaque composition to presence of significant stenosis was shown to provide incremental prognostic information. The results suggest that the combined use of coronary CT angiography with functional tests may allow for improved risk stratification.
Impact of Coronary CT Angiography in Clinical Practice
Given the potential for more widespread use of coronary CT angiography in risk evaluation, the consequences of coronary CT angiography testing also need to be considered. A previous study by McEvoy et al. (17) observed 1000 asymptomatic subjects who underwent coronary CT angiography as a part of health-screening program. In the study, the presence of coronary atherosclerotic plaque was predictive of increased aspirin and statin use. Performance of coronary CT angiography was also associated with significantly more secondary testing and revascularization procedures compared to matched control subjects, but without any difference in cardiac events at 18 months. Therefore, at present, the use of coronary CT angiography for risk stratification is thought to be without any evidence-based indication in an asymptomatic population. In patients presenting with suspected CAD, the potential benefit of increased medication use driven by coronary CT angiography remains to be evaluated by randomized trials with long-term follow-up.
On the other hand, it also needs to be evaluated whether coronary CT angiography alone can reliably identify patients who may benefit from revascularization. Current guidelines recommend proof of ischemia prior to elective revascularization (18, 19). The presence of ischemia is associated with adverse clinical outcomes, and an ischemia-guided approach to revascularization is associated with improved patient outcomes (20, 21). The Fractional Flow Reserve versus Angiography for Multivessel Evaluation study was a large, multicenter, international, randomized clinical trial comparing outcomes in patients with multivessel CAD undergoing percutaneous coronary intervention either with angiographic guidance alone or with the addition of fractional flow reserve (FFR) guidance (20). At 1 year, there was a significant decrease in the primary end point in the group receiving FFR guidance compared to the group with angiographic guidance alone. The result supports the guidelines recommending proof of ischemia prior to revascularization procedure. However, coronary stenosis measured by coronary CT angiography demonstrates an unreliable accuracy to define the lesion-specific ischemia (22). It does not reflect the failure of coronary CT angiography to accurately assess coronary artery stenosis, since invasive coronary angiography could not improve the diagnostic accuracy to detect myocardial ischemia (22, 23). Eventually, to identify patients who are likely to benefit from invasive coronary angiography and revascularization, patients with CAD in coronary CT angiography need to be investigated by a subsequent functional test.
Novel Technologies for Functional Assessment
Comprehensive noninvasive imaging including both information on anatomic coronary stenosis and functional information about the hemodynamic significance of coronary stenosis would be desirable to guide treatment. One strategy is to use hybrid imaging techniques, such as SPECT-CT or PET-CT, with aims to maximize the advantages of both functional and anatomic imaging method (24, 25). Recently, Pazhenkottil et al. (26) reported the prognostic value of SPECT-CT in 324 patients with known or suspected CAD. Patients with matched defect on hybrid imaging showed the worst event-free survival followed by those with unmatched findings, then those with normal findings. The hybrid imaging may provide better diagnostic and prognostic value compared to functional or anatomic imaging alone. However, these modalities still require two separate imaging technologies, resulting in additional cost, time, and radiation exposure (24). On the basis of these considerations, several methods were developed to combine anatomical data from coronary CT angiography with the hemodynamic significance during a single examination.
CT Myocardial Perfusion Imaging
The first strategy is to combine coronary CT angiography with adenosine stress CT perfusion imaging (Figs. 1, 2). Recently, Ko et al. (27) evaluated the diagnostic performance of adenosine stress CT perfusion acquired using 320-detector row CT when used with coronary CT angiography for detecting ischemia as determined by FFR. In 42 patients with significant stenosis in invasive angiography, the presence of a perfusion defect in territories with a ≥ 50% diameter stenosis is highly specific for ischemia, while the presence of normal perfusion in territories subtended by an artery with a < 50% stenosis excludes ischemia with 100% accuracy (Fig. 3). In the study, coronary CT angiography combined with CT myocardial perfusion imaging was highly accurate in the detection and exclusion of ischemia when coronary CT angiography and CT perfusion findings were concordant.
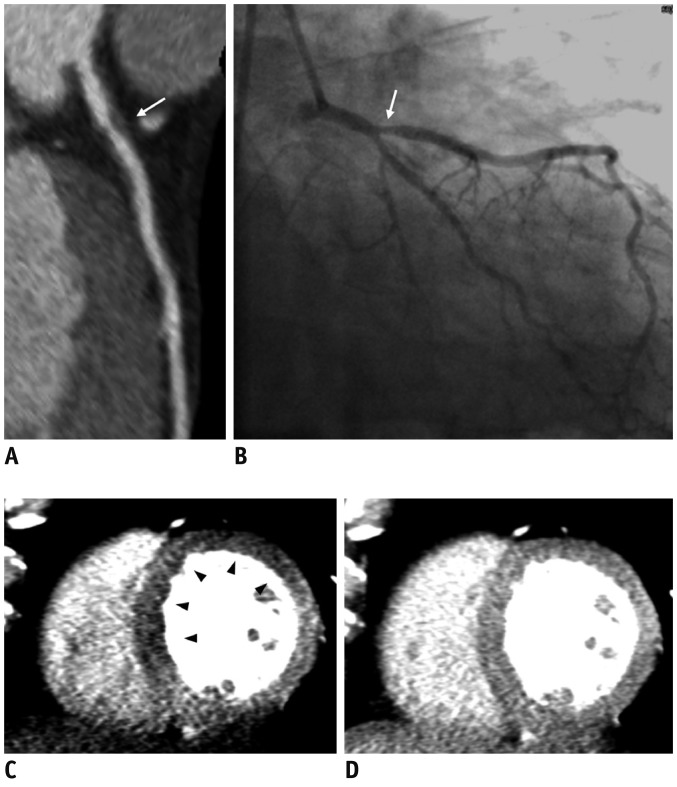
Fig. 1.
Case of computed tomography (CT) myocardial perfusion imaging.
54-year-old male patient with chest pain. Coronary CT angiography (A) showed stenosis in proximal left anterior descending artery (white arrow). Invasive coronary angiography (B) also showed presence of significant stenosis in proximal LAD (white arrow), and fractional flow reserve of 0.79 confirmed functional significance of lesion. Stress (C) and rest (D) CT myocardial perfusion imaging showed ischemia (black arrowheads) of LAD territory (images were provided by Dr. Dong Hyun Yang from Asan Medical Center, Korea). LAD = left anterior descending artery.
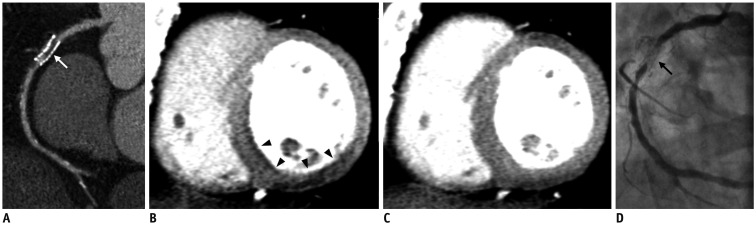
Fig. 2.
Case of computed tomography (CT) myocardial perfusion imaging.
64-year-old male patient with history of percutaneous coronary intervention to right coronary artery (RCA) was referred with effort angina. Coronary CT angiography (A) showed stenosis in RCA stent (white arrow), and stress (B) and rest (C) CT myocardial perfusion imaging showed ischemia (black arrowheads) of RCA territory. Invasive coronary angiography (D) confirmed presence of significant in-stent restenosis (black arrow) (Images were provided by Dr. Dong Hyun Yang from Asan Medical Center, Korea).
Fig. 3.
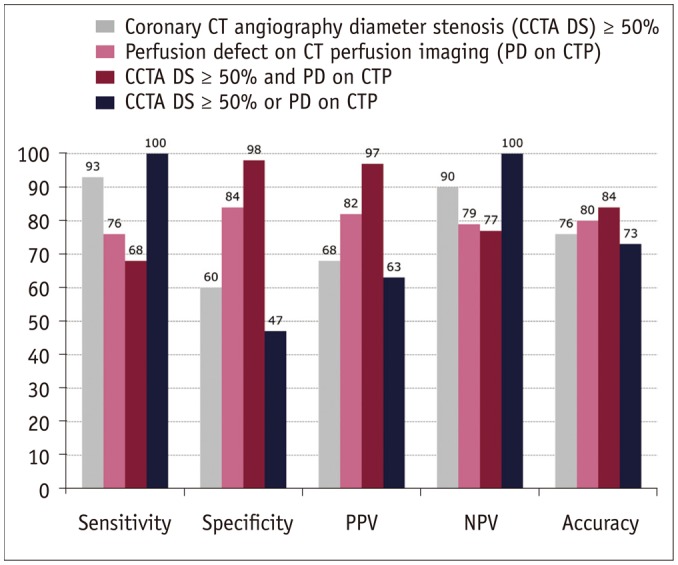
Diagnostic accuracy of coronary computed tomography (CT) angiography and CT myocardial perfusion imaging to detect functionally significant stenosis, defined as fractional flow reserve ≤ 0.80 (27). PPV = positive predictive value, NPV = negative predictive value
However, at present, there are several limitations that are innate to CT myocardial perfusion imaging. First, beam hardening, motion, and reconstruction artifacts are still important limitations of CT myocardial perfusion imaging. Second, the current CT myocardial perfusion imaging technique is limited in the quantification of myocardial blood flow. MR myocardial perfusion imaging which continuously visualized the wash-in and wash-out of contrast with cine imaging enables estimation of myocardial blood flow by mathematical calculation from the upslope and peak contrast enhancement. In contrast, the 'snapshot' approach of CT myocardial perfusion imaging, which acquires images at the peak myocardial enhancement, does not allow for myocardial blood flow quantification. Recently, dynamic CT myocardial perfusion imaging was proposed, and various methods to calculate myocardial blood flow using CT have been reported. George et al. (28) reported that myocardial blood flow measurements using a model-based deconvolution method correlated well with microsphere myocardial blood flow in a canine model. Nakauchi et al. (29) demonstrated that dynamic CT perfusion imaging with deconvolution analysis could quantitatively evaluate myocardial perfusion abnormalities in patients with acute myocardial infarction. However, the dynamic CT perfusion imaging needs to be evaluated in more patients including stable angina. Third, although the ability to perform myocardial perfusion imaging with coronary CT angiography may provide a more conclusive cardiac evaluation, additional stress myocardial perfusion imaging requires the administration of adenosine, larger volumes of iodinated contrast agent, and radiation exposure (27). Dynamic CT perfusion imaging requires repeated exposure to radiation to acquire the data for the generation of an accurate time-density curve (29). Finally, before incorporation of this technique into routine clinical practice, large multicenter studies are required to investigate its diagnostic and prognostic value as a stand-alone imaging modality for coronary artery disease.
Intracoronary Luminal Attenuation of Coronary CT Angiography
Analysis of the intracoronary luminal attenuation is available from standard coronary CT angiographic data without modification of acquisition protocols or additional imaging, and has been known to reflect the intracoronary blood flow. Transluminal attenuation gradient (TAG) and corrected coronary opacification (CCO) have been developed to evaluate the severity of coronary stenosis (30-32). In previous studies, both TAG and CCO seem to predict abnormal coronary blood flow estimated by Thrombosis in Myocardial Infarction frame count, so they are expected to increase the diagnostic performance of coronary CT angiography (32). However, when Choi et al. (33) validated TAG and CCO with invasively measured FFR, the addition of TAG or CCO did not result in improved reclassification of coronary CT angiographic evaluation of coronary stenosis. At present, the discrimination performance of intraluminal attenuation-based methods for the evaluation of hemodynamically significant stenosis seems to be limited. However, the diagnostic accuracy of TAG is expected to be improved with the use of newer scanners with wide-area coverage, which allows single-beat imaging, since the lack of temporal uniformity might limit the performance of TAG in previous studies (32-34).
CT-Derived Computed FFR (FFRCT)
Another strategy is to calculate FFR from coronary CT angiographic data by using computational fluid dynamics. From coronary CT angiographic images, a 3-dimensional (3D) model of the coronary tree and ventricular myocardium are reconstructed and semi-automatically segmented. Based on the principle that coronary supply meets myocardial demand at rest, and the resistance of the microcirculation at rest is inversely proportional to the size of the feeding vessel, total resting coronary flow and the microvascular resistance are calculated according to ventricular mass and the size of the feeding vessel, respectively. 3D blood flow simulations of the coronary arteries were performed, with blood modeled as a Newtonian fluid using incompressible Navier-Strokes equations, and solved subject to appropriate initial and boundary conditions with a finite element method on a parallel supercomputer. Because coronary flow and pressure are unknown a priori, a method to couple lumped parameter models of the microcirculation to the outflow boundaries of the 3D model was used. And, by using a lumped parameter model, coronary blood flow was simulated under conditions for modeling adenosine-mediated coronary hyperemia. The FFRCT ratio was obtained by dividing the mean pressure distal to the coronary stenosis by the mean aortic pressure, and then a 3D FFRCT map was generated (Fig. 4) (34-36).
Fig. 4.
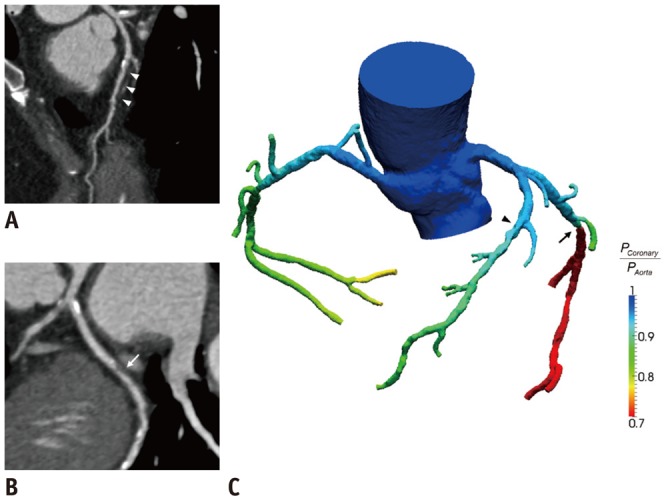
Case of computed tomography-derived computed fractional flow reserve (FFRCT).
59-year-old female patient complained effort angina. Coronary CT angiography detected (A) diffuse intermediate stenosis of left anterior descending artery (LAD) (white arrowheads) and (B) focal intermediate stenosis of left circumflex artery (LCX) (white arrow). Computation of FFRCT demonstrated that (C) LAD stenosis was not hemodynamically significant with FFRCT value over 0.8 (black arrowhead), and LCX stenosis is ischemia-causing lesion with FFRCT value of less than 0.8 (black arrow) (Images were provided by Dr. Bon-Kwon Koo from Seoul National University Hospital, Korea).
The feasibility and diagnostic performance of FFRCT were evaluated in the study entitled Diagnosis of Ischemia-Causing Stenosis Obtained Via Noninvasive Fractional Flow Reserve (35). The FFRCT is well correlated with invasively measured FFR, and showed high diagnostic performance for the detection and exclusion of coronary lesions that cause ischemia. In a head-to-head comparison study by Yoon et al. (34), FFRCT provided better diagnostic performance for the diagnosis of lesion-specific ischemia, as determined by invasive FFR, compared to coronary CT angiography stenosis and TAG. The most important difference was thought to be that FFRCT is computed from simulated hyperemia, whereas TAG is measured from resting state. Recently, the international multicenter Determination of Fractional Flow Reserve by Anatomic Computed Tomographic Angiography study confirmed the diagnostic value of FFRCT (36). In 252 patients with suspected or known CAD, adding FFRCT to coronary CT angiography improved discrimination for the diagnosis of hemodynamically significant coronary stenosis compared with CT angiographic diagnosis alone (Fig. 5).
Fig. 5.
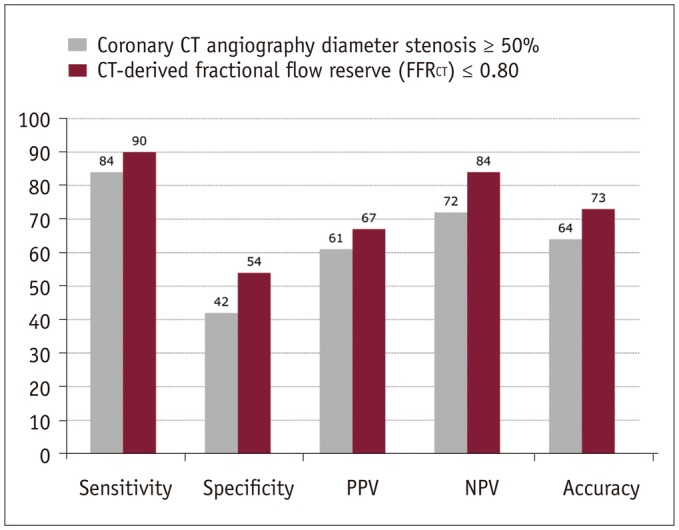
Diagnostic accuracy of coronary computed tomography (CT) angiography and FFRCT to detect functionally significant stenosis, defined as fractional flow reserve ≤ 0.80 (38). PPV = positive predictive value, NPV = negative predictive value
Computation of FFRCT from coronary CT angiography may permit an "all-in-one" approach, by which patient-specific stenosis can be assessed for lesion-specific ischemia. The FFRCT is computed from typically acquired coronary CT angiography scans without a need for additional image acquisition or administration of medication. However, the FFRCT analyses requires approximately 6 hours per case. In addition, to date, it still remains unknown whether revascularization of the ischemic lesions identified by FFRCT would achieve therapeutic reduction in ischemia or would improve outcome.
CONCLUSIONS
Cardiac CT can provide incremental prognostic value over traditional risk stratification algorithm. Cardiac CT can also provide complementary prognostic information to functional tests with regard to risk stratification. However, to date, it has not been evaluated whether cardiac CT-guided treatment can improve the patient outcome. Recently, novel technologies with the ability of comprehensive anatomical and functional assessment were developed, including CT myocardial perfusion and computation of FFR from CT. These technologies are expected to provide better diagnostic value. However, at present, the diagnostic and prognostic value of these technologies needs to be evaluated further in the future studies.
Acknowledgments
I thank Dr. Bon-Kwon Koo from Seoul National University Hospital and Dr. Dong Hyun Yang from Asan Medical Center for their support in writing this article.
References
- 1.Raggi P, Gongora MC, Gopal A, Callister TQ, Budoff M, Shaw LJ. Coronary artery calcium to predict all-cause mortality in elderly men and women. J Am Coll Cardiol. 2008;52:17–23. doi: 10.1016/j.jacc.2008.04.004. [DOI] [PubMed] [Google Scholar]
- 2.Budoff MJ, Shaw LJ, Liu ST, Weinstein SR, Mosler TP, Tseng PH, et al. Long-term prognosis associated with coronary calcification: observations from a registry of 25,253 patients. J Am Coll Cardiol. 2007;49:1860–1870. doi: 10.1016/j.jacc.2006.10.079. [DOI] [PubMed] [Google Scholar]
- 3.Greenland P, LaBree L, Azen SP, Doherty TM, Detrano RC. Coronary artery calcium score combined with Framingham score for risk prediction in asymptomatic individuals. JAMA. 2004;291:210–215. doi: 10.1001/jama.291.2.210. [DOI] [PubMed] [Google Scholar]
- 4.Detrano R, Guerci AD, Carr JJ, Bild DE, Burke G, Folsom AR, et al. Coronary calcium as a predictor of coronary events in four racial or ethnic groups. N Engl J Med. 2008;358:1336–1345. doi: 10.1056/NEJMoa072100. [DOI] [PubMed] [Google Scholar]
- 5.Polonsky TS, McClelland RL, Jorgensen NW, Bild DE, Burke GL, Guerci AD, et al. Coronary artery calcium score and risk classification for coronary heart disease prediction. JAMA. 2010;303:1610–1616. doi: 10.1001/jama.2010.461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Henneman MM, Schuijf JD, Pundziute G, van Werkhoven JM, van der Wall EE, Jukema JW, et al. Noninvasive evaluation with multislice computed tomography in suspected acute coronary syndrome: plaque morphology on multislice computed tomography versus coronary calcium score. J Am Coll Cardiol. 2008;52:216–222. doi: 10.1016/j.jacc.2008.04.012. [DOI] [PubMed] [Google Scholar]
- 7.Yoon YE, Chang SA, Choi SI, Chun EJ, Cho YS, Youn TJ, et al. The absence of coronary artery calcification does not rule out the presence of significant coronary artery disease in Asian patients with acute chest pain. Int J Cardiovasc Imaging. 2012;28:389–398. doi: 10.1007/s10554-011-9819-0. [DOI] [PubMed] [Google Scholar]
- 8.Budoff MJ, Dowe D, Jollis JG, Gitter M, Sutherland J, Halamert E, et al. Diagnostic performance of 64-multidetector row coronary computed tomographic angiography for evaluation of coronary artery stenosis in individuals without known coronary artery disease: results from the prospective multicenter ACCURACY (Assessment by Coronary Computed Tomographic Angiography of Individuals Undergoing Invasive Coronary Angiography) trial. J Am Coll Cardiol. 2008;52:1724–1732. doi: 10.1016/j.jacc.2008.07.031. [DOI] [PubMed] [Google Scholar]
- 9.Meijboom WB, Meijs MF, Schuijf JD, Cramer MJ, Mollet NR, van Mieghem CA, et al. Diagnostic accuracy of 64-slice computed tomography coronary angiography: a prospective, multicenter, multivendor study. J Am Coll Cardiol. 2008;52:2135–2144. doi: 10.1016/j.jacc.2008.08.058. [DOI] [PubMed] [Google Scholar]
- 10.Miller JM, Rochitte CE, Dewey M, Arbab-Zadeh A, Niinuma H, Gottlieb I, et al. Diagnostic performance of coronary angiography by 64-row CT. N Engl J Med. 2008;359:2324–2336. doi: 10.1056/NEJMoa0806576. [DOI] [PubMed] [Google Scholar]
- 11.Hulten EA, Carbonaro S, Petrillo SP, Mitchell JD, Villines TC. Prognostic value of cardiac computed tomography angiography: a systematic review and meta-analysis. J Am Coll Cardiol. 2011;57:1237–1247. doi: 10.1016/j.jacc.2010.10.011. [DOI] [PubMed] [Google Scholar]
- 12.Hadamitzky M, Distler R, Meyer T, Hein F, Kastrati A, Martinoff S, et al. Prognostic value of coronary computed tomographic angiography in comparison with calcium scoring and clinical risk scores. Circ Cardiovasc Imaging. 2011;4:16–23. doi: 10.1161/CIRCIMAGING.110.955351. [DOI] [PubMed] [Google Scholar]
- 13.Chow BJ, Wells GA, Chen L, Yam Y, Galiwango P, Abraham A, et al. Prognostic value of 64-slice cardiac computed tomography severity of coronary artery disease, coronary atherosclerosis, and left ventricular ejection fraction. J Am Coll Cardiol. 2010;55:1017–1028. doi: 10.1016/j.jacc.2009.10.039. [DOI] [PubMed] [Google Scholar]
- 14.Chow BJ, Small G, Yam Y, Chen L, Achenbach S, Al-Mallah M, et al. Incremental prognostic value of cardiac computed tomography in coronary artery disease using CONFIRM: COroNary computed tomography angiography evaluation for clinical outcomes: an InteRnational Multicenter registry. Circ Cardiovasc Imaging. 2011;4:463–472. doi: 10.1161/CIRCIMAGING.111.964155. [DOI] [PubMed] [Google Scholar]
- 15.Cho I, Shim J, Chang HJ, Sung JM, Hong Y, Shim H, et al. Prognostic value of multidetector coronary computed tomography angiography in relation to exercise electrocardiogram in patients with suspected coronary artery disease. J Am Coll Cardiol. 2012;60:2205–2215. doi: 10.1016/j.jacc.2012.08.981. [DOI] [PubMed] [Google Scholar]
- 16.van Werkhoven JM, Schuijf JD, Gaemperli O, Jukema JW, Boersma E, Wijns W, et al. Prognostic value of multislice computed tomography and gated single-photon emission computed tomography in patients with suspected coronary artery disease. J Am Coll Cardiol. 2009;53:623–632. doi: 10.1016/j.jacc.2008.10.043. [DOI] [PubMed] [Google Scholar]
- 17.McEvoy JW, Blaha MJ, Nasir K, Yoon YE, Choi EK, Cho IS, et al. Impact of coronary computed tomographic angiography results on patient and physician behavior in a low-risk population. Arch Intern Med. 2011;171:1260–1268. doi: 10.1001/archinternmed.2011.204. [DOI] [PubMed] [Google Scholar]
- 18.Silber S, Albertsson P, Avilés FF, Camici PG, Colombo A, Hamm C, et al. [Guidelines for percutaneous coronary interventions] Ital Heart J Suppl. 2005;6:427–474. [PubMed] [Google Scholar]
- 19.Smith SC, Jr, Feldman TE, Hirshfeld JW, Jr, Jacobs AK, Kern MJ, King SB, 3rd, et al. ACC/AHA/SCAI 2005 guideline update for percutaneous coronary intervention: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (ACC/AHA/SCAI Writing Committee to Update 2001 Guidelines for Percutaneous Coronary Intervention) Circulation. 2006;113:e166–e286. doi: 10.1161/CIRCULATIONAHA.106.173220. [DOI] [PubMed] [Google Scholar]
- 20.Tonino PA, De Bruyne B, Pijls NH, Siebert U, Ikeno F, van't Veer M, et al. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. N Engl J Med. 2009;360:213–224. doi: 10.1056/NEJMoa0807611. [DOI] [PubMed] [Google Scholar]
- 21.Hachamovitch R, Hayes SW, Friedman JD, Cohen I, Berman DS. Comparison of the short-term survival benefit associated with revascularization compared with medical therapy in patients with no prior coronary artery disease undergoing stress myocardial perfusion single photon emission computed tomography. Circulation. 2003;107:2900–2907. doi: 10.1161/01.CIR.0000072790.23090.41. [DOI] [PubMed] [Google Scholar]
- 22.Meijboom WB, Van Mieghem CA, van Pelt N, Weustink A, Pugliese F, Mollet NR, et al. Comprehensive assessment of coronary artery stenoses: computed tomography coronary angiography versus conventional coronary angiography and correlation with fractional flow reserve in patients with stable angina. J Am Coll Cardiol. 2008;52:636–643. doi: 10.1016/j.jacc.2008.05.024. [DOI] [PubMed] [Google Scholar]
- 23.Gaemperli O, Schepis T, Valenta I, Koepfli P, Husmann L, Scheffel H, et al. Functionally relevant coronary artery disease: comparison of 64-section CT angiography with myocardial perfusion SPECT. Radiology. 2008;248:414–423. doi: 10.1148/radiol.2482071307. [DOI] [PubMed] [Google Scholar]
- 24.Rispler S, Keidar Z, Ghersin E, Roguin A, Soil A, Dragu R, et al. Integrated single-photon emission computed tomography and computed tomography coronary angiography for the assessment of hemodynamically significant coronary artery lesions. J Am Coll Cardiol. 2007;49:1059–1067. doi: 10.1016/j.jacc.2006.10.069. [DOI] [PubMed] [Google Scholar]
- 25.Sampson UK, Dorbala S, Limaye A, Kwong R, Di Carli MF. Diagnostic accuracy of rubidium-82 myocardial perfusion imaging with hybrid positron emission tomography/computed tomography in the detection of coronary artery disease. J Am Coll Cardiol. 2007;49:1052–1058. doi: 10.1016/j.jacc.2006.12.015. [DOI] [PubMed] [Google Scholar]
- 26.Pazhenkottil AP, Nkoulou RN, Ghadri JR, Herzog BA, Buechel RR, Küest SM, et al. Prognostic value of cardiac hybrid imaging integrating single-photon emission computed tomography with coronary computed tomography angiography. Eur Heart J. 2011;32:1465–1471. doi: 10.1093/eurheartj/ehr047. [DOI] [PubMed] [Google Scholar]
- 27.Ko BS, Cameron JD, Meredith IT, Leung M, Antonis PR, Nasis A, et al. Computed tomography stress myocardial perfusion imaging in patients considered for revascularization: a comparison with fractional flow reserve. Eur Heart J. 2012;33:67–77. doi: 10.1093/eurheartj/ehr268. [DOI] [PubMed] [Google Scholar]
- 28.George RT, Jerosch-Herold M, Silva C, Kitagawa K, Bluemke DA, Lima JA, et al. Quantification of myocardial perfusion using dynamic 64-detector computed tomography. Invest Radiol. 2007;42:815–822. doi: 10.1097/RLI.0b013e318124a884. [DOI] [PubMed] [Google Scholar]
- 29.Nakauchi Y, Iwanaga Y, Ikuta S, Kudo M, Kobuke K, Murakami T, et al. Quantitative myocardial perfusion analysis using multi-row detector CT in acute myocardial infarction. Heart. 2012;98:566–572. doi: 10.1136/heartjnl-2011-300915. [DOI] [PubMed] [Google Scholar]
- 30.Steigner ML, Mitsouras D, Whitmore AG, Otero HJ, Wang C, Buckley O, et al. Iodinated contrast opacification gradients in normal coronary arteries imaged with prospectively ECG-gated single heart beat 320-detector row computed tomography. Circ Cardiovasc Imaging. 2010;3:179–186. doi: 10.1161/CIRCIMAGING.109.854307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chow BJ, Kass M, Gagné O, Chen L, Yam Y, Dick A, et al. Can differences in corrected coronary opacification measured with computed tomography predict resting coronary artery flow? J Am Coll Cardiol. 2011;57:1280–1288. doi: 10.1016/j.jacc.2010.09.072. [DOI] [PubMed] [Google Scholar]
- 32.Choi JH, Min JK, Labounty TM, Lin FY, Mendoza DD, Shin DH, et al. Intracoronary transluminal attenuation gradient in coronary CT angiography for determining coronary artery stenosis. JACC Cardiovasc Imaging. 2011;4:1149–1157. doi: 10.1016/j.jcmg.2011.09.006. [DOI] [PubMed] [Google Scholar]
- 33.Choi JH, Koo BK, Yoon YE, Min JK, Song YB, Hahn JY, et al. Diagnostic performance of intracoronary gradient-based methods by coronary computed tomography angiography for the evaluation of physiologically significant coronary artery stenoses: a validation study with fractional flow reserve. Eur Heart J Cardiovasc Imaging. 2012;13:1001–1007. doi: 10.1093/ehjci/jes130. [DOI] [PubMed] [Google Scholar]
- 34.Yoon YE, Choi JH, Kim JH, Park KW, Doh JH, Kim YJ, et al. Noninvasive diagnosis of ischemia-causing coronary stenosis using CT angiography: diagnostic value of transluminal attenuation gradient and fractional flow reserve computed from coronary CT angiography compared to invasively measured fractional flow reserve. JACC Cardiovasc Imaging. 2012;5:1088–1096. doi: 10.1016/j.jcmg.2012.09.002. [DOI] [PubMed] [Google Scholar]
- 35.Koo BK, Erglis A, Doh JH, Daniels DV, Jegere S, Kim HS, et al. Diagnosis of ischemia-causing coronary stenoses by noninvasive fractional flow reserve computed from coronary computed tomographic angiograms. Results from the prospective multicenter DISCOVER-FLOW (Diagnosis of Ischemia-Causing Stenoses Obtained Via Noninvasive Fractional Flow Reserve) study. J Am Coll Cardiol. 2011;58:1989–1997. doi: 10.1016/j.jacc.2011.06.066. [DOI] [PubMed] [Google Scholar]
- 36.Min JK, Leipsic J, Pencina MJ, Berman DS, Koo BK, van Mieghem C, et al. Diagnostic accuracy of fractional flow reserve from anatomic CT angiography. JAMA. 2012;308:1237–1245. doi: 10.1001/2012.jama.11274. [DOI] [PMC free article] [PubMed] [Google Scholar]