Abstract
Younger Black men who have sex with men (BMSM) ages 16–29 have the highest rates of HIV in the United States. Despite increased attention to social and sexual networks as a framework for biomedical intervention, the role of measured network positions, such as bridging and their relationship to HIV risk has received limited attention. A network sample (N=620) of BMSM respondents (n=154) and their MSM and transgendered person network members (n=466) was generated through respondent driven sampling of BMSM and elicitation of their personal networks. Bridging status of each network member was determined by a constraint measure and was used to assess the relationship between this bridging and unprotected anal intercourse (UAI), sex-drug use (SDU), group sex (GS) and HIV status within the network in South Chicago. Low, moderate and high bridging was observed in 411 (66.8%), 81 (13.2%) and 123 (20.0%) of the network. In addition to age and having sex with men only, moderate and high levels of bridging were associated with HIV status (AOR 3.19; 95% CI 1.58–6.45 and AOR 3.83; 95% CI 1.23–11.95, respectively). Risk behaviors observed including UAS, GS, and SDU were not associated with HIV status, however, they clustered together in their associations with one another. Bridging network position but not risk behavior was associated with HIV status in this network sample of younger BMSM. Socio-structural features such as position within the network may be important when implementing effective HIV prevention interventions in younger BMSM populations.
Keywords: Black MSM, HIV, network analysis, bridge, risk behavior
Introduction
Black men who have sex with men (BMSM) in the United States are disproportionally at risk for HIV. Nationwide, it is estimated that 1 in 16 BMSM will be diagnosed with HIV during their lifetime (1), In Chicago, 7 times as many BMSM are infected with HIV infection as white MSM with similar sex and drug use behaviors (2). Although the precise mechanisms underlying the disparities in HIV infection among BMSM are unknown, research has suggested that BMSM experience a constellation of risk factors that increase vulnerability to infection, including higher rates of undiagnosed HIV (3), less knowledge of partner’s HIV status (4), higher levels of stigma, discrimination and minority stress experiences (5), higher underlying rates of HIV among BMSM (6), and structural factors such as poverty (7).
In addition to these factors, a growing body of research has focused on the role of networks in facilitating HIV transmission among BMSM (8–11). To date, much of this research has examined the extent to which risk is distributed and transmitted through the sexual networks of BMSM (12–15). This work has provided some explanation for high STI rates within and among different racial groups and includes the mixing between high-risk core and low-risk periphery groups, also known as disassortative mixing (16). While mixing within sex networks is likely a major factor in HIV transmission dynamics, networks of Black MSM include non-sexual ties to others that may also exert influence on more proximal factors of HIV transmission, such as high-risk behavior, including group sex, unprotected anal intercourse and using drugs during sex. Thus other (non-sexual) social network structures may explain some of the factors related to HIV risk (17–19), or perhaps to how HIV infected BMSM are organized. These social networks operate through influence and social norms that may be related to risk reduction (20).
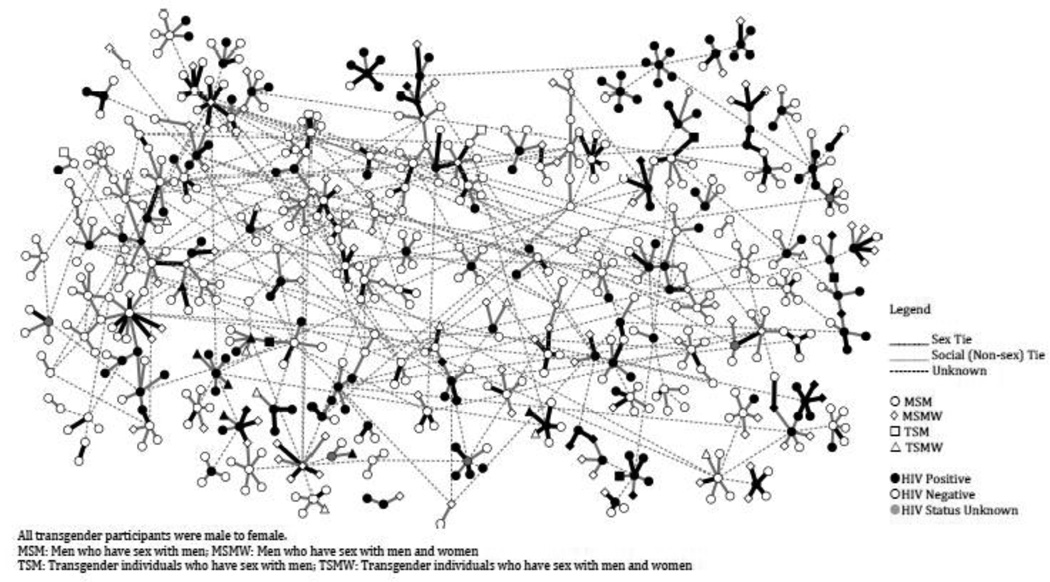
While these social norms and influence have been the focus of much attention in the behavioral sciences, the quantifiable structural position of where someone is located within the network (e.g., a bridge(21)) and how this is related to high-risk behavior and HIV transmission has received little attention. Most characterizations of structural positions, such as bridging, have relied on general approximations based upon individual demographic or behavioral characteristics and have been mostly explored in “risk networks”. For example a truck-driver status has been equated with a bridging person; an occupation that is associated with spreading HIV from sex worker to wife (22). Linking demographic and behavioral characteristics to social network structural positions is complicated and can lead to misclassification (23). Quantitatively derived network positions, however, have been effectively utilized for detection of contagious outbreaks such as influenza (24) and are likely important for explaining behavior related to transmission patterns of other infectious diseases such as HIV. Accurate quantification of social network structure that leads to bridge characterization (See network graph below), could both help explain current HIV related racial disparities and illuminate points for network-based intervention to prevent onward transmission. Importantly bridges are increasingly recognized not for their transmission potential – “risk networks”, but for their unique position and the social capital that they possess (25). Characterization of bridges, including real-time network assessment critical to intervention implementation, is becoming increasingly feasible with readily available digital communication network type data such as email, cell-phones and Facebook (26, 27).
In this network analysis, we generate a single inter-connected network of high-risk younger Black MSM and transgender persons, and evaluate the potential bridging position of network members and how they might be associated with risk behavior and HIV status.
METHODS
Setting
Between January and June of 2010, BMSM were recruited from the South Side of Chicago using respondent-driven sampling (RDS) (28). The South Side of Chicago and adjacent South suburbs, a 128 square mile region including 34 of the city’s 77 community areas and 8 south corridor suburbs, is one of the largest contiguous Black urban community in the United States (72% of 1034K people).(29) All interviews took place at a partnering community-based organization on the South Side by University of Chicago Survey Lab trained community members. All study procedures were approved by appropriate institutional review boards. Informed consent was obtained from all study respondents and waived for network members listed by respondents.
Study Participants
Eligibility Criteria
Study participants include both study respondents who were interviewed, and the network members (also described as alters by the social network analysis community) about whom they reported. Study respondents were eligible to participate if they 1) self-identified as African American or Black, 2) identified as biologically male, 3) were age 18 years or older, 4) reported anal intercourse with a man within the past 12 months, and 5) were willing and able to provide informed consent at the time of the study visit.
Recruitment
Seeds were selected from two venues on the South Side of Chicago either through referral from HIV program personnel (e.g., case manager) or HIV prevention program staff. In the case of referral, requests for popular or charismatic candidates were made to maximize first wave recruitment (28). Specifically, twelve seeds were recruited using these two approaches: 1) Four seeds were recruited from a local Federally Qualified Health Center that provides HIV primary care; and 2) Eight seeds were referred from existing group Effective Behavioral Intervention prevention programs (30). Each seed was given four vouchers and asked to refer up to four MSM from their social networks, with each subsequent recruit doing the same. In order to deter duplicate enrollment, bilateral arm and wrist measurements were conducted on all respondents (31). All respondents were paid $50 for participation.
Survey Instruments
Social Network Assessment
In designing our network instrument, we followed an established method of gathering network data used in several large national surveys, including the General Social Survey (32), the National Health and Social Life Survey (33), and the National Social Life, Health, and Aging Project (34). Some studies assess people’s social and sexual networks by asking about connections with a pre-determined list of different social contacts (e.g., parents, partners, individuals who provide material support). We did not impose a conceptual framework that dictated the types of contacts that were most important to BMSM respondents. Instead, we utilized a more open approach (35), which let BMSM respondents reveal the characteristics of their personal social networks. This kept the focus on individuals with whom BMSM respondents were most subjectively engaged (36), which was appropriate given our goal of visualizing a network that includes important individuals most likely to drive any effects of structural positions that individuals occupy. The strong ties generated using this approach was ideal to complement other “weaker” ties that can be elicited through many other approaches including through RDS.
We asked a “name generator” (37) question during the course of face-to-face interviews to elicit a set of social network members who may influence respondent’s risky behaviors. The name generator was selected to identify network “confidants” (38) who may have opportunities, through everyday interactions with the respondent, to exercise normative pressure or informal control, provide social support, and to exchange information or advice regarding risky behavior: “Let’s make a list of your closest associates with whom you may share information about yourself, your physical and mental health, and your social and sexual lifestyles”. Names or other identifiers such as nicknames were entered into a roster that was recorded for future reference. We then followed up with a series of “name interpreter” questions about each network member’s relationship type, strength of tie, risk behaviors, HIV status and other sociodemographics. This process was looped over each of the five confidants listed from the initial name generator. Research has shown that five network members is optimal for time and effort to field network surveys to determine confidant type ties (39).
Duplicate information and matching algorithm
Before 1999, matching procedures to create unique identifiers using contact tracing and similar network study data have relied on reviewing sorted lists (40–42). Later studies utilized computer matching algorithms (43–48). We adopted the following approach based upon the “fuzzy matching algorithms” developed by a member of the team (SQM), and used in another recent network study (49). Because different respondents within the RDS network are likely to know some of the same people, we created a list of all the network members cited by all of the respondents in our sample, and matched any network members or respondents who we believed to be the same person. Following pre-cleaning to make sure common names were spelled in the same manner, we created a set of rules for matching cases within the network. First, two cases would have to have at least the same initials to be considered as a possible match; having the same full name also meant they were a candidate for being a match. Second, they would have to be within three years difference in terms of their ages. Third, cases would both have to be living in the Chicago area, or both living outside it. Fourth, cases would have to be both of the same race (if one was black, and another was of mixed descent where one of the races was black, they were considered as a possible match). Fifth, cases would both have to be of the same gender, or have approximately the same number of respondents who considered them male, female, or transgender. Thus, a person who was identical on all attributes with some other person, except that one respondent considered that person female and another transgender would be called a match. Sixth, and finally, no two interviewed respondents could be considered for a match.
Following this, we produced a new dataset with attributes for each of these 784 cases. If the case was composed of a respondent, and not simply from a network member (that is, one of the persons which ‘compose’ this case is someone we actually spoke to), we assigned their HIV status on the basis of HIV testing. If a case was composed of several matched network members, and no respondents, then if at least one respondent listed them as HIV infected, they were coded as such. For all other attributes we took the modal value of their reported attribute. If there was a tie between two modal values, we assigned the respondent an attribute value on the basis of who they were closest to (50). Because eligibility criteria included only MSM, other network members including biologically born women and men who have sex with women only were beyond the scope of the current analysis and the effects of these individuals on MSM have been examined elsewhere (15, 51–53). Members of the team who created the matching algorithm were not involved with any of the subsequent analyses of structural position.
Bridging network metric
In order to calculate each network members’ level of bridging we utilized the constraint metric (54):
where pij is the proportion of i’s network time and energy invested in contact j, and piq is the proportion of time and energy of i invested in another contact q. Constraint is a measure of bridging on a 0–1 scale and is low for a given individual who is connected to others who are otherwise not connected to each other. Such an individual with low constraint is one that spans structural holes in the network and can be considered a “bridge”. A constraint of 1, a high constraint, represents the lowest bridging and is usually an individual within a network who has only one tie to another network member. In most networks, structural measures are not normally distributed (20, 55); therefore we took the median of the remaining individuals who did not have a low bridging score (constraint=1) to provide a cut-off between moderate bridging and high bridging. Several alternative measures of bridging such as betweeness centrality (56) or link deletion (57) have been identified, but are better suited for larger networks. In order to ease understanding of our results, the terms bridge or bridging are used to signify constraint as just described.
Sociodemographic, Attitude and Behavior Measures
Age, education, employment, HIV status, unprotected and intercourse (UAI), were items adapted from the Centers for Disease Control and Prevention’s National HIV Behavioral Surveillance Survey, MSM Cycle (58). Sex drug use (SDU) was measured as in previous work (59, 60) and represented use of any prescription or illicit drug that makes sex easier to get, more enjoyable or last longer. Group sex (GS) was measured as “having sex with two or more individuals at the same time”. UAI, GS and SDU were assessed in frequency terms over the past year and were coded for these analyses as present if they were reported as at least monthly. All respondents were tested for HIV (Oraquick Advance HIV 1/2, Bethlehem PA) with confirmation conducted by the Chicago Department of Public Health (OraSure HIV-1 Western Blot). HIV counseling was offered onsite and HIV-infected respondents were linked to HIV care.
Analysis
Risk Network effect analysis
The primary outcomes of this study were defined in terms of risk-related behaviors: UAI, SDU, GS; and HIV status. We examined these outcomes individually according to the following model (61).
where Y is the outcome measure, X are one or more variables characterizing the respondent’s network, and Z are the additional covariates selected because of their importance in previous research; individual sociodemographics (age, sexual orientation), risk behavior (UAI, SDU, GS), HIV status, and whether the network member was a respondent or a non-respondent. Our parameter of interest is β, which describes the association between network characteristics and HIV-risk behavior and HIV status practices. Outcome measures were defined as HIV status and the reported frequency of engaging in UAI, SDU, and GS. An ordinal logistic regression model first examined the relationship of structural network metric constraint and one risk behavior outcome controlling for all covariates. A second logistic regression model examined the relationship between constraint and HIV status; again controlling for all covariates.
RESULTS
Matching
Out of a total possible 893 individuals that could make up the network, 85 of them were single matches, 24 of the network members were matched more than once and 6 were isolates (not connected to others in the network). Over half (61%) of matches were perfect name matches. This resulted in a final network size of 778. We examined the concordance for age and HIV status between respondent self-report and reports on these same respondents by other network members. Matched network members were within 2 years of both reports in 92% of cases. For HIV status, there was 79% concordance between self-report of HIV status and report of HIV status by other network members. The majority of discordance (17%) was for respondents self-reporting as HIV uninfected and other network members reporting that they were HIV infected.
Network Composition and visualization
The final analytic network included MSM, MSMW and transgendered persons in the network, limiting the final social network to 620. Individuals who did not meet eligibility criteria were not included (164 women (not transgender) and heterosexual men (20.9%)). These individuals were positioned on the periphery of the network and did not add contribute to the structure of the network (data not shown). Network member characteristics can be found in Table 1. Visualization of the social network can be found in Figure 1. This network graph demonstrates heterogeneity in networks including HIV infected and uninfected individuals within the same personal networks as well as no clear clustering of HIV cases or obvious patterned network structure (ie sub-groups). Calculating bridging for all network members demonstrated low, moderate and high bridging observed in 411 (66.8%), 81 (13.2%) and 123 (20.0%) network members respectively, with several risk factors associated with bridging (Table 2). The sexual network was made up of 81 separate components with the maximum component size including 13 individuals. Meaningful measures and interpretation of bridging within the sex network were not possible given the numerous separate components.
Table 1.
Attributes for Black men who have sex with men and their network members (n=620)
| Characteristics | Respondents (n=154) N (%) |
Network Members (n=466) N (%) |
|---|---|---|
| Age | ||
| <20 | 23 (14.9) | 63 (13.5) |
| 20–24 | 47 (30.5) | 131 (28.1) |
| 25–30 | 28 (18.1) | 102 (21.9) |
| 31–40 | 19 (12.3) | 61 (13.1) |
| 41+ | 28 (18.2) | 108 (23.2) |
| Race | ||
| Black/African-American | 144 (93.5) | 440 (94.4) |
| White/Caucasian | 0 (0) | 10 (2.1) |
| Native American | 0 (0) | 2 (0.4) |
| Mixed/other | 9 (5.8) | 13 (2.8) |
| Gender | ||
| Male | 151 (98.1) | 430 (92.3) |
| Transgender Female | 0 (0) | 24 (5.2) |
| Sex Partners | ||
| Men only | 142 (92.2) | 345 (74.0) |
| Men and Women | 7 (4.5) | 80 (17.2) |
| Other/Unknown | 3 (1.9) | 15 (3.2) |
| Unprotected anal sex* | 48 (31.2) | 163 (35.0) |
| Sex drug use* | 48 (31.2) | 269 (57.7) |
| Group sex* | 32 (20.8) | 104 (22.3) |
| HIV Status† | ||
| HIV+ | 66 (42.9) | 109 (23.4) |
| HIV− | 87 (56.5) | 352 (75.5) |
| Unknown | 1 (0.6) | 5 (1.1) |
Risk behavior variables were measured over the previous 12 months.
From among respondents indicating that they know network members’ HIV status Data missing: 10 for age, 2 for race, 28 for sex partners, 6 for HIV, 84 for UAS, 63 for SDU, 67 for GS
Figure 1. Social network of Black men who have sex with men (n=620), South Chicago, United States.
TABLE 2.
Ordinal logistic regression of sociodemographic factors, risk behaviors and HIV infection against bridging in a Black men who have sex with men network in Chicago (n=620).*
| Characteristic | (N=620) | Low Bridging (aOR; 95% CI) |
Moderate Bridging (aOR; 95% CI) |
High Bridging (aOR; 95% CI) |
|---|---|---|---|---|
| Age | ||||
| <20 | (86) | Ref | Ref | Ref |
| 20–24 | (178) | 0.71; (0.25–2.06) | 0.82; (0.39–1.71) | 2.58; (0.83–7.98) |
| 25–29 | (130) | 0.91; (0.29–2.89) | 0.58; (0.25–1.34) | 5.23†; (1.14–24.58) |
| 30–39 | (80) | 1.77; (0.44–7.08) | 0.37; (0.13–1.04) | 4.30; (0.76–24.21) |
| >39 | (136) | 2.70; (0.77–9.51) | 0.37†; (0.15–0.90) | 1.62; (0.41–6.52) |
| Sex partners | ||||
| Men only | (487) | Ref | Ref | Ref |
| Men and Women | (101) | 0.23‡; (0.11–0.46) | 3.41‡; (1.83–6.38) | 0.74; (0.14–3.90) |
| Group sex | ||||
| Not in the past 6 months | (417) | Ref | Ref | Ref |
| In the past 6 months | (136) | 2.66†; (1.09–6.47) | 0.64; (0.33–1.25) | 0.49; (0.16–1.46) |
| HIV | ||||
| Negative | (439) | Ref | Ref | Ref |
| Positive | (135) | 0.32‡; (0.15–0.69) | 1.90†; (1.06–3.41) | 1.33; (0.49–3.58) |
Variables significant from bivariate analysis also used in regressions with p=0.10 as cutoff included respondent type, unprotected anal sex, sex-drug use and gender
p<0.05
p<0.01, Ref=reference group.
Sociodemographic variables and bridging associated with risk behavior and HIV status
In bivariate analysis, the following variables were associated with at least one of the outcome measures (unprotected anal sex, group sex, sex-drug use and HIV status) at the p<0.1 level: age, bridging, participant type (respondent vs. named network member not interviewed) and sex partner. Sex behavior variables were not associated with HIV status when analysis was restricted to respondents only, nor the network as a whole. Variables significant at p<0.1 from bivariate analyses were entered into separate multiple regression models for each outcome in Table 3. There was a monotonic increase in HIV status with age, a common finding in HIV prevalence studies. As might be expected, risk behaviors (UAI, GS, and SDU) were associated with one another, however, were not associated with HIV status. Moderate and high levels of bridging were associated with HIV status (aOR 3.19; 95% CI 1.58–6.45 and aOR 3.83; 95% CI 1.23–11.95, respectively). When these analyses were rerun including women and heterosexual men, our findings did not change (data not shown).
TABLE 3.
Multiple logistic regression analysis including sociodemographic, risk behavior and bridging variables for unprotected anal sex, group sex, sex-drug use and HIV infection of a Black men who have sex with men network in Chicago (n=620).
| Characteristic (N=620) |
Unprotected anal sex1 (aOR; 95% CI) |
Group sex2 (aOR; 95% CI) |
Sex-drug use3 (aOR; 95% CI) |
|
|---|---|---|---|---|
| Age | ||||
| <20 | (86) | Ref | Ref | Ref |
| 20–24 | (178) | 0.76; (0.39–1.47) | 0.48; (0.22–1.03) | 3.55‡; (1.75–7.20) |
| 25–29 | (130) | 0.63; (0.30–1.30) | 1.07; (0.48–2.36) | 5.53‡; (2.52–12.15) |
| 30–39 | (80) | 0.52; (0.23–1.19) | 0.58; (0.23–1.47) | 6.42‡; (2.71–15.22) |
| >39 | (136) | 0.63; (0.31–1.28) | 0.58; (0.26–1.30) | 3.45†; (1.65–7.22) |
| Sexual behavior | - | |||
| MSM | (487) | - | Ref. | Ref |
| MSMW | (101) | - | 1.69; (0.90–3.15) | 1.41; (0.76–2.60) |
| Bridging | - | |||
| Low (1) | (411) | Ref | - | Ref |
| Moderate (0.18–0.99) | (81) | 0.99; (0.36–2.73) | - | 0.97; (0.30–3.10) |
| High (0–0.17) | (123) | 0.65; (0.19–2.19) | - | 3.64; (0.64–20.83) |
| Unprotected anal sex | N/A | |||
| Not in the past 6 months | (325) | Ref | Ref | |
| In the past 6 months | (211) | 6.09‡; (3.67–10.10) | 3.20‡; (1.97–5.20) | |
| Group sex | N/A | |||
| Not in the past 6 months | (417) | Ref | Ref | |
| In the past 6 months | (136) | 5.95‡; (3.63–9.76) | 3.13‡; (1.70–5.75) | |
| Sex-drug use | N/A | |||
| Not in the past 6 months | (240) | Ref | Ref | |
| In the past 6 months | (317) | 2.95‡; (1.85–4.70) | 3.32‡; (1.81–6.11) | |
| Participant type | ||||
| Study respondent | (154) | Ref | Ref | Ref |
| Network member | (466) | 1.96; (0.64–5.96) | 0.51*; (0.28–0.94) | 1.52; (0.33–7.10) |
Variables included in each of the four models from bivariate analysis at p=0.10 but not significant after adjustment here are the following:
age, bridging, participant type;
age and sexual behavior;
sexual behavior, bridging and participant type;
Participant type.
p<0.05,
p<0.01,
p<0.001. N/A = not applicable. Ref=reference group.

Network demonstrating concept of bridging This hypothetical network illustrates the bridging node. At first, Node 1 appears to be an important node because it has more direct connections to other individuals in the network1. In contrast, node 13 has fewer direct connections to other individuals in the network. While node 13 has fewer connections to others in the network and can be considered less popular, node 13 acts as a bridge in the network. Having direct connections to three distinct subpopulations in the network, node 13 is best positioned to connect nodes in the network that are otherwise not connected.2
1. Degree centrality is a measure that indicates the node with the greatest number of connections. Node 1 has the highest degree centrality (7.0) because node 1 has more connections to other individuals than any other node in the network.
2. Constraint is a measure of bridging on a 0–1 scale and is low for a given node that is connected to others who are otherwise not connected to each other. Node 13 has the lowest constraint score (0.2) because this node has access to the range of the network by representing key bridges to distinct sub-groups.
DISCUSSION
To date, relatively little research has been done on how structural positions within a given social network may be related to the organization of risk behavior and HIV status within the network. In our study on the importance of structural positions, we arrived at a number of significant findings. First, we found that BMSM who were located in bridging positions were more likely to be HIV infected than those who were not. We also noted other characteristics associated with HIV infection, such as increased age and having sex solely with men, but these characteristics are traditionally associated with HIV status among MSM. Of interest, several risk behaviors we observed (unprotected anal sex, group sex, and sex-drug use, for example) were not associated with HIV status, though these behaviors were clustered together due to their associations with one another. This suggests that both HIV-infected and uninfected network members participate in these behaviors and that these behaviors are potentially overlapping. Risk behaviors such as unprotected anal sex can have variable associations with HIV seroprevalence in cross-sectional analyses. HIV-infected MSM, for example, may participate in less unprotected anal sex after learning their HIV status (62, 63), but individuals who are HIV-infected may also be more likely to engage in unprotected anal sex (64, 65) or have more sexual mixing with others regardless of condom use (15). Finally, individuals bridging the network were just as likely as other network members to participate in high-risk sex behaviors such as unprotected anal sex, sex-drug use, and group sex.
Identification of bridges or other structured network positions in HIV research has typically relied on individual level characteristics such as demographic or behavioral factors (22) (66). Most common among these has been the identification of centrally located or popular opinion leaders within high-risk networks. The importance of such centrally located individuals as effective change agents, however, has been limited (23, 67). Other characteristics that are potentially features of bridges, such as one’s “innovativeness,” have also been described as being potentially associated with bridging position (57). This includes innovativeness among individuals within a high-risk male social network (68). All of these characteristics, however, are subjective measures based on individual reporting that may be associated with structural positions such as bridging or “bridge populations” – and thus they are potentially susceptible to misclassification.
Others frame bridging quantitatively within the context of mixing between groups or as a discordance between sex partners whereby one partner belongs to a low risk “core” group and another from a high risk group (69). Within this kind of framing, bridging has been found to exert a greater influence on HIV status as compared to other drivers of HIV transmission such as concurrency (70). This has been extended to spatial bridging both for the transmission of sexually transmitted infections and HIV (71–73). These bridging network structures may accelerate or limit the spread of disease across an entire community and may be a decisive factor in determining whether epidemics are concentrated or generalized (74) within a specified boundary.
All of these bridging measurements, however, are not based on a quantified bridging structural position as in this study. We are not the first to use quantitative methods, but the actual quantification of bridges through social network metrics has mostly been conducted by researchers who study organizational structure (e.g., Burt(55)). While our findings provide a glimpse into the relationship between bridging and HIV status, the organizational sciences have developed a rich literature as to the behaviors related to bridging positions, which may help us develop interventions based upon the structural identification of bridges.
Bridges may be more efficient diffusion agents than centrally located individuals because they have fewer interconnected network members to persuade (75); they can also devote more energy to persuading and thereby be more effective change agents. Additionally, bridging individuals may be more receptive to behavior change because they have less pressure to support prevailing norms and behaviors (76) or incur a reputation cost for new and potentially disapproved behavior (25). Finally, occupying a bridging position may be indicative of attitudinal dispositions such as being open to new ideas and practices (57, 77). By virtue of their boundary-spanning positions, bridging individuals often have early access to novel information, but are also experienced in communicating the information across diverse audiences (25). Recognizing the limitations of cross-sectional data in this study, identification of bridges within a high-risk network may be of importance not only because of the potential to target such individuals to limit onward transmission through a community, but also because of the potential to recruit such individuals as change agents to intervene at the network level.
As with any study, our findings must be interpreted within the context of study limitations. One limitation is due to the cross-sectional nature of our network data, which does not allow us to determine causality. We do not know whether a bridging position leads to HIV infection, or whether individuals gravitate to bridging positions following a diagnosis of HIV (perhaps through network partitioning), or both. Risk network researchers, for example, may suggest that bridges are positioned to become HIV-infected, but this assumes that the social network approximates the sexual, which it did not in this study. Similarly, organizational network researchers might posit that HIV infected persons position themselves strategically to control information flow, connecting to relatively isolated individuals who are otherwise not connected. Both of these hypotheses could be valid and warrant further research to determine how network position might be related to HIV serostatus in a social network. A second limitation is that our network does not include all ties or individuals, including women, and may not represent all BMSM. Women and heterosexual men did not contribute to the structure of this network (data not shown). Previously we have estimated that there are nearly 10× the number of MSM in this area than what were included in our sample (78), although we do not know if they are all part of one network component. Given the chain referral sampling methods utilized and boundary specification (79) which limited our sampling frame to the South Side of Chicago, we developed a fair amount of network redundancy making the network we characterized a likely sub-network within the South Side. Limiting our focus to closer associates may have excluded some weak ties, although at least some weak ties were included through RDS chains. Including additional weak ties (e.g., by using a roster or density matrix) could improve social network research for MSM. Using one name generator may limit the number of strong or close ties evident in the network. Additionally, we did not measure whether the confidants in fact provided social support, information control and exchange of information or advice. Regardless, we wished to keep the focus on individuals with whom BMSM were most subjectively engaged (36), which was appropriate given our goal of visualizing a network that includes important individuals most likely to drive any effects of structural positions that individuals occupy. Other approaches to network generation could be considered, including using multiple name generators concurrently that get at specific functions (ie. provide social support, inject drugs with etc.)(80, 81). Other individuals who were not eligible for participation such as women and heterosexual men may play important roles in the lives of BMSM (15, 51, 52). Finally, our matching algorithm might produce misclassifications with respect to risk behaviors and HIV status. While our matching algorithm is similar to that used in other risk network studies (43–48), full last names were less common, which could lead to misidentification of network members. Despite this, our concordance rate between self-reported HIV status and behavior and the reports of others on that behavior and HIV status was high at nearly 80%. It is difficult to predict which of the biases inherent to our data collection methods might have predominated. For example, social desirability bias is commonly present during risk surveys and the high rate of HIV positive unaware (15% overall and 50% in those under 20 years of age) may have been underestimated in our self-reported HIV status prevalence. Both of these forces may make reports on one’s HIV status from close confidants potentially more accurate than self-reports. Regardless, new approaches to validate, improve or weigh the accuracy of reports on network members are needed.
This study demonstrates that network structure as an emergent property in HIV prevention may be of importance when classifying at-risk individuals or at least identifying individuals who may be HIV infected. This could complement traditionally utilized individual level risk, and allow for more effectively targeted HIV prevention interventions both at the individual level, as well as the network level where halting transmission pathways is critical. Moreover, identification of bridges could be explored in future interventions to serve as change agents to diffuse novel prevention modalities through high-risk networks.
Acknowledgements
This work was supported by NIH grants: R01 DA033875, U54 RR023560 and R21MH098768 We would like to thank the study respondents for their time and Don Fette for reading an earlier version of this manuscript.
References
- 1.Hall HI, An Q, Hutchinson AB, Sansom S. Estimating the lifetime risk of a diagnosis of the HIV infection in 33 states, 2004–2005. J Acquir Immune Defic Syndr. 2008 Nov 1;49(3):294–297. doi: 10.1097/QAI.0b013e3181893f17. PubMed PMID: 18978477. Epub 2008/11/04. eng. [DOI] [PubMed] [Google Scholar]
- 2.CDPH. HIV Prevalence and Unrecognized Infection among Men Who Have Sex with Men – Chicago. Chicago: Chicago Department of Public Health; 2008. [Google Scholar]
- 3.MacKellar DA, Valleroy LA, Secura GM, Behel S, Bingham T, Celentano DD, et al. Unrecognized HIV infection, risk behaviors, and perceptions of risk among young men who have sex with men - Opportunities for advancing HIV prevention in the third decade of HIV/AIDS. Jaids-J Acq Imm Def. 2005 Apr 15;38(5):603–614. doi: 10.1097/01.qai.0000141481.48348.7e. PubMed PMID: ISI:000228018200015. English. [DOI] [PubMed] [Google Scholar]
- 4.Oster AM, Wiegand RE, Sionean C, Miles IJ, Thomas PE, Melendez-Morales L, et al. Understanding disparities in HIV infection between black and white MSM in the United States. AIDS. 2011 May 15;25(8):1103–1112. doi: 10.1097/QAD.0b013e3283471efa. PubMed PMID: 21505305. Epub 2011/04/21. eng. [DOI] [PubMed] [Google Scholar]
- 5.Meyer IH. Minority stress and mental health in gay men. J Health Soc Behav. 1995 Mar;36(1):38–56. PubMed PMID: 7738327. Epub 1995/03/01. eng. [PubMed] [Google Scholar]
- 6.Kelley CF, Rosenberg ES, O'Hara BM, Frew PM, Sanchez T, Peterson JL, et al. Measuring Population Transmission Risk for HIV: An Alternative Metric of Exposure Risk in Men Who Have Sex with Men (MSM) in the US. PLoS One. 2012;7(12):e53284. doi: 10.1371/journal.pone.0053284. PubMed PMID: 23285274. Pubmed Central PMCID: 3532405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Millett GA, Peterson JL, Flores SA, Hart TA, Jeffries WLt, Wilson PA, et al. Comparisons of disparities and risks of HIV infection in black and other men who have sex with men in Canada, UK, and USA: a meta-analysis. Lancet. 2012 Jul 28;380(9839):341–348. doi: 10.1016/S0140-6736(12)60899-X. PubMed PMID: 22819656. [DOI] [PubMed] [Google Scholar]
- 8.Adimora AA, Schoenbach VJ, Doherty IA. HIV and African Americans in the southern United States: sexual networks and social context. Sex Transm Dis. 2006 Jul;33(7 Suppl):S39–S45. doi: 10.1097/01.olq.0000228298.07826.68. PubMed PMID: 16794554. Epub 2006/06/24. eng. [DOI] [PubMed] [Google Scholar]
- 9.Harawa NT, Greenland S, Bingham TA, Johnson DF, Cochran SD, Cunningham WE, et al. Associations of race/ethnicity with HIV prevalence and HIV-related behaviors among young men who have sex with men in 7 urban centers in the United States. J Acquir Immune Defic Syndr. 2004 Apr 15;35(5):526–536. doi: 10.1097/00126334-200404150-00011. PubMed PMID: 15021318. Epub 2004/03/17. eng. [DOI] [PubMed] [Google Scholar]
- 10.Millett GA, Flores SA, Peterson JL, Bakeman R. Explaining disparities in HIV infection among black and white men who have sex with men: a meta-analysis of HIV risk behaviors. AIDS. 2007;21:2083–2091. doi: 10.1097/QAD.0b013e3282e9a64b. [DOI] [PubMed] [Google Scholar]
- 11.Peterson JL, Rothenberg R, Kraft JM, Beeker C, Trotter R. Perceived condom norms and HIV risks among social and sexual networks of young African American men who have sex with men. Health Educ Res. 2009 Feb 1;24(1):119–127. doi: 10.1093/her/cyn003. 2009. [DOI] [PubMed] [Google Scholar]
- 12.Mimiaga MJ, Reisner SL, Cranston K, Isenberg D, Bright D, Daffin G, et al. Sexual Mixing Patterns and Partner Characteristics of Black MSM in Massachusetts at Increased Risk for HIV Infection and Transmission. Journal of Urban Health-Bulletin of the New York Academy of Medicine. 2009 Jul;86(4):602–623. doi: 10.1007/s11524-009-9363-6. PubMed PMID: WOS:000267592500009. English. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hurt CB, Beagle S, Leone PA, Sugarbaker A, Pike E, Kuruc J, et al. Investigating a Sexual Network of Black Men Who Have Sex With Men: Implications for Transmission and Prevention of HIV Infection in the United States. Jaids-J Acq Imm Def. 2012 Dec 1;61(4):515–521. doi: 10.1097/QAI.0b013e31827076a4. PubMed PMID: WOS: 000311083200019. English. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Laumann EO, Ellingson S, Mahay J, Paik A, Youm Y. The Sexual Organization of the City. Chicago: University of Chicago; 2004. [Google Scholar]
- 15.Schneider JA, Cornwell B, Ostrow D, Michaels S, Schumm P, Laumann EO, et al. Network Mixing and Network Influences Most Linked to HIV Infection and Risk Behavior in the HIV Epidemic Among Black Men Who Have Sex With Men. Am J Public Health. 2013 Jan;103(1):e28–e36. doi: 10.2105/AJPH.2012.301003. PubMed PMID: 23153147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Newman MEJ. Mixing patterns in networks. Physical Review E. 2003;67(2):e026126. doi: 10.1103/PhysRevE.67.026126. [DOI] [PubMed] [Google Scholar]
- 17.Tobin KE, German D, Spikes P, Patterson J, Latkin C. A comparison of the social and sexual networks of crack-using and non-crack using African American men who have sex with men. J Urban Health. 2011 Dec;88(6):1052–1062. doi: 10.1007/s11524-011-9611-4. PubMed PMID: 21882072. Pubmed Central PMCID: 3232415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Latkin C, Yang C, Tobin K, Roebuck G, Spikes P, Patterson J. Social network predictors of disclosure of MSM behavior and HIV-positive serostatus among African American MSM in Baltimore, Maryland. AIDS and behavior. 2012 Apr;16(3):535–542. doi: 10.1007/s10461-011-0014-z. PubMed PMID: 21811844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schneider JA, Michaels S, Bouris A. Family network proportion and HIV risk among Black men who have sex with men. JAIDS Journal of Acquired Immune Deficiency Syndromes. 2012 doi: 10.1097/QAI.0b013e318270d3cb. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Valente TW. Models, Methods and Application. Oxford: Oxford University Press; 2010. Social Networks and Health. [Google Scholar]
- 21.Granovetter MS. The strength of weak ties. The American Journal of Sociology. 1973;78(6):1360–1380. [Google Scholar]
- 22.Morris M, Podhisita C, Wawer MJ, Handcock MS. Bridge populations in the spread of HIV/AIDS in Thailand. AIDS. 1996 Sep;10(11):1265–1271. doi: 10.1097/00002030-199609000-00013. PubMed PMID: 8883589. [DOI] [PubMed] [Google Scholar]
- 23.Schneider JA, Laumann EO. Alternative explanations for negative findings in the community popular opinion leader multisite trial and recommendations for improvements of health interventions through social network analysis. J Acquir Immune Defic Syndr. 2011 Apr;56(4):e119–e120. doi: 10.1097/QAI.0b013e318207a34c. PubMed PMID: 21350361. Epub 2011/02/26. eng. [DOI] [PubMed] [Google Scholar]
- 24.Christakis NA, Fowler JH. Social network sensors for early detection of contagious outbreaks. PLoS One. 2010;5(9):e12948. doi: 10.1371/journal.pone.0012948. PubMed PMID: 20856792. Pubmed Central PMCID: 2939797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Burt RS. Neighbor Networks. Oxford: Oxford University Press; 2010. [Google Scholar]
- 26.Kossinets G, Watts DJ. Empirical analysis of an evolving social network. Science. 2006 Jan 6;311(5757):88–90. doi: 10.1126/science.1116869. PubMed PMID: 16400149. Epub 2006/01/10. eng. [DOI] [PubMed] [Google Scholar]
- 27.Aral S, Walker D. Identifying influential and susceptible members of social networks. Science. 2012 Jul 20;337(6092):337–341. doi: 10.1126/science.1215842. PubMed PMID: 22722253. [DOI] [PubMed] [Google Scholar]
- 28.Heckathorn D. Respondent-Driven Sampling: A New Approach to the Study of Hidden Populations. Social Problems. 1997;44(2) [Google Scholar]
- 29.U.S. Census Bureau. 2005–2009 American Community Survey 5-Year Estimates. [Accessed 3 January 2011]; [Google Scholar]
- 30.Centers for Disease C. 2009 compendium of evidence-based HIV prevention interventions 2010. [Last accessed May 2010]; Available from: http://www.cdc.gov/hiv/topics/research/prs/evidence-based-interventions.htm.
- 31.Heckathorn DD, Semaan S, Broadhead RS, Hughes JJ. Extensions of Respondent-Driven Sampling: A New Approach to the Study of Injection Drug Users Aged 18–25. Aids Behav. 2002;6(1):55–68. [Google Scholar]
- 32.Gilman SE, Cochran SD, Mays VM, Hughes M, Ostrow DG, Kessler RC. Risk of psychiatric disorders among individuals reporting same-sex partners in the National Comorbidity Survey. American Journal of Public Health. 2001;91(6):933–939. doi: 10.2105/ajph.91.6.933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Laumann EO, Gagnon JH, Michael RT, Michaels S. The Social Organization of Sexuality: Sexual Practices in the United States. Chicago,IL: University Of Chicago Press; 1994. [Google Scholar]
- 34.Cornwell B, Schumm LP, Laumann EO, Graber J. Social Networks in the NSHAP Study: Rationale, Measurement, and Preliminary Findings. J Gerontol B-Psychol. 2009 Nov;64:I47–I55. doi: 10.1093/geronb/gbp042. PubMed PMID: ISI:000271718300006. English. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Marsden PV. Core discussion networks of Americans. American Sociological Review. 1987;52(1):122–131. [Google Scholar]
- 36.Laumann EO, Marsden PV, Prensky D. The boundary specification problem in network analysis. In: Burt RS, Minor MJ, editors. Applied Network Analysis. New York, NY: Sage Publications; 1983. pp. 18–34. [Google Scholar]
- 37.Marsden PV. Core discussion networks of Americans. American Sociological Review. 1987;52(1):122–131. [Google Scholar]
- 38.McPherson M, Smith-Lovin L, Brashears ME. Social Isolation in America: Changes in Core Discussion Networks over Two Decades. American Sociological Review. 2006;71(3):353–375. [Google Scholar]
- 39.Burt RS. Network items and the general social survey. Social Networks. 1984;6:293–339. [Google Scholar]
- 40.Auerbach DM, Darrow WW, Jaffe HW, Curran JW. Cluster of cases of the acquired immune deficiency syndrome. Patients linked by sexual contact. Am J Med. 1984 Mar;76(3):487–492. doi: 10.1016/0002-9343(84)90668-5. PubMed PMID: 6608269. Epub 1984/03/01. eng. [DOI] [PubMed] [Google Scholar]
- 41.Friedman SR, Neaigus A, Jose B, Curtis R, Goldstein M, Ildefonso G, et al. Sociometric risk networks and risk for HIV infection. Am J Public Health. 1997 Aug;87(8):1289–1296. doi: 10.2105/ajph.87.8.1289. PubMed PMID: 9279263. Pubmed Central PMCID: 1381088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Potterat J, Woodhouse DE, Muth SQ, Rothenberg R, Darrow WW, Klovdahl AS, et al. Network dynamism: history and lessons of the Colorado Springs study. In: Morris M, editor. Network epidemiolgy: A Handbook for Network Survey Design. Oxford University Press; 2004. [Google Scholar]
- 43.Potterat JJ, Muth SQ, Rothenberg RB, Zimmerman-Rogers H, Green DL, Taylor JE, et al. Sexual network structure as an indicator of epidemic phase. Sex Transm Infect. 2002 Apr;78(Suppl 1):i152–i158. doi: 10.1136/sti.78.suppl_1.i152. PubMed PMID: 12083436. Pubmed Central PMCID: 1765821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Latkin CA, Knowlton AR, Sherman S. Routes of drug administration, differential affiliation, and lifestyle stability among cocaine and opiate users: Implications to HIV prevention. J Subst Abuse. 2001;13(1–2):89–102. doi: 10.1016/s0899-3289(01)00070-0. PubMed PMID: ISI:000170677800008. English. [DOI] [PubMed] [Google Scholar]
- 45.Rothenberg R, Hoang TDM, Muth SQ, Crosby R. The Atlanta urban adolescent network study: A network view of STD prevalence. Sexually Transmitted Diseases. 2007 Aug;34(8):525–531. doi: 10.1097/01.olq.0000258132.06764.a1. PubMed PMID: WOS:000248287200001. English. [DOI] [PubMed] [Google Scholar]
- 46.Sena AC, Muth SQ, Heffelfinger JD, O'Dowd JO, Foust E, Leone P. Factors and the sociosexual network associated with a syphilis outbreak in rural North Carolina. Sex Transm Dis. 2007 May;34(5):280–287. doi: 10.1097/01.olq.0000237776.15870.c3. PubMed PMID: 17139235. [DOI] [PubMed] [Google Scholar]
- 47.Helleringer S, Kohler HP, Chimbiri A. Characteristics of external/bridge relationships by partner type and location where sexual relationship took place. AIDS. 2007 Nov 30;21(18):2560–2561. doi: 10.1097/QAD.0b013e3282f112bd. PubMed PMID: 18025903. [DOI] [PubMed] [Google Scholar]
- 48.Doherty IA, Adimora AA, Muth SQ, Serre ML, Leone PA, Miller WC. Comparison of sexual mixing patterns for syphilis in endemic and outbreak settings. Sex Transm Dis. 2011 May;38(5):378–384. doi: 10.1097/OLQ.0b013e318203e2ef. PubMed PMID: 21217418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Doherty IA, Schoenbach VJ, Adimora AA. Sexual Mixing Patterns and Heterosexual HIV Transmission Among African Americans in the Southeastern United States. Jaids-J Acq Imm Def. 2009 Sep 1;52(1):114–120. doi: 10.1097/QAI.0b013e3181ab5e10. PubMed PMID: ISI:000269373400016. English. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Morrison DM, Casey EA, Beadnell BA, Hoppe MJ, Gillmore MR, Wilsdon A, et al. Effects of friendship closeness in an adolescent group HIV prevention intervention. Prev Sci. 2007 Dec;8(4):274–284. doi: 10.1007/s11121-007-0075-4. PubMed PMID: 17846890. [DOI] [PubMed] [Google Scholar]
- 51.Garofalo R, Mustanski B, Donenberg G. Parents know and parents matter; is it time to develop family-based HIV prevention programs for young men who have sex with men? J Adolesc Health. 2008 Aug;43(2):201–204. doi: 10.1016/j.jadohealth.2008.01.017. PubMed PMID: 18639797. Pubmed Central PMCID: 2601675. Epub 2008/07/22. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Schneider J, Michaels S, Bouris A. Family network proportion and HIV risk among Black men who have sex with men. J Acquir Immune Defic Syndr. 2012 Sep 22; doi: 10.1097/QAI.0b013e318270d3cb. PubMed PMID: 23011395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lauby JL, Marks G, Bingham T, Liu KL, Liau A, Stueve A, et al. Having Supportive Social Relationships is Associated with Reduced Risk of Unrecognized HIV Infection Among Black and Latino Men who Have Sex with Men. AIDS Behav. 2011 Jul 30; doi: 10.1007/s10461-011-0002-3. PubMed PMID: 21805191. Epub 2011/08/02. Eng. [DOI] [PubMed] [Google Scholar]
- 54.Burt RS. Structural holes: The social structure of competition. Cambridge, MA: Harvard University Press; 1992. [Google Scholar]
- 55.Burt RS. An Introduction to Social Capital. Oxford: Oxford University Press; 2005. Brokerage and Closure. [Google Scholar]
- 56.Freeman LC. Centrality in social networks: Conceptual clarification. Social Networks. 1979;1:215–239. [Google Scholar]
- 57.Valente TW, Fujimoto K. Bridging: Locating Critical Connectors in a Network. Soc Networks. 2010 Jul 1;32(3):212–220. doi: 10.1016/j.socnet.2010.03.003. PubMed PMID: 20582157. Pubmed Central PMCID: 2889704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Sanchez T, Finlayson T, Drak A, Behel S, Cribbin M, Dinenno E, et al. Human immunodeficiency virus (HIV) risk, prevention, and testing behaviors--United States, National HIV Behavioral Surveillance System: men who have sex with men, November 2003–April 2005. MMWR Surveill Summ. 2006;55(6):1–16. [PubMed] [Google Scholar]
- 59.Ostrow DG, Plankey MW, Cox C, Li X, Shoptaw S, Jacobson LP, et al. Specific sex drug combinations contribute to the majority of recent HIV seroconversions among MSM in the MACS. Journal of Acquired Immune Deficiency Syndromes(1999) 2009;51(3):349–355. doi: 10.1097/QAI.0b013e3181a24b20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ostrow DG, Stall RC. Alcohol, tobacco, and drug use among gay and bisexual men. In: Wolitski RJ, Stall R, Valdiserri RO, editors. Unequal Opportunity: Health Disparities Affecting Gay and Bisexual Men in the United States. Oxford, UK: Oxford University Press; 2008. pp. 121–158. [Google Scholar]
- 61.McCullagh P, Nelder JA. Generalized Linear Models. Boca Raton,FL: CRC Press; 1999. [Google Scholar]
- 62.Wolitski RJ, Bailey CJ, Leary AO, Gomez CA, Parsons JT, Sums Self-perceived responsibility of HIV-Seropositive men who have sex with men for preventing HIV transmission. Aids and Behavior. 2003 Dec;7(4):363–372. doi: 10.1023/b:aibe.0000004728.73443.32. PubMed PMID: WOS:000186690700003. English. [DOI] [PubMed] [Google Scholar]
- 63.Nimmons D, Folkman S. Other-sensitive motivation for safer sex among gay men: expanding paradigms for HIV preventio. AIDS and Behavior. 1999;3(4):313–324. [Google Scholar]
- 64.Crepaz N, Marks G, Liau A, Mullins MM, Aupont LW, Marshall KJ, et al. Prevalence of unprotected anal intercourse among HIV-diagnosed MSM in the United States: a meta-analysis. Aids. 2009 Aug 24;23(13):1617–1629. doi: 10.1097/QAD.0b013e32832effae. PubMed PMID: WOS:000269333900001. English. [DOI] [PubMed] [Google Scholar]
- 65.Bruce D, Harper GW, Suleta K HIV AMTN. Sexual Risk Behavior and Risk Reduction Beliefs Among HIV-Positive Young Men Who have Sex with Men. Aids and Behavior. 2013 May;17(4):1515–1523. doi: 10.1007/s10461-012-0155-8. PubMed PMID: WOS:000318171800031. English. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kelly JA. Popular opinion leaders and HIV prevention peer education: resolving discrepant findings, and implications for the development of effective community programmes. AIDS Care. 2004 Feb;16(2):139–150. doi: 10.1080/09540120410001640986. PubMed PMID: 14676020. Epub 2003/12/17. eng. [DOI] [PubMed] [Google Scholar]
- 67.Group NCHSPT. Results of the NIMH collaborative HIV/sexually transmitted disease prevention trial of a community popular opinion leader intervention. J Acquir Immune Defic Syndr. 2010 Jun;54(2):204–214. doi: 10.1097/QAI.0b013e3181d61def. PubMed PMID: 20354444. Pubmed Central PMCID: 2904551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Schneider JA, Zhou AN, Gandham SR, Kapur A, Oruganti G, Laumann EO, et al. Selection of candidate peer change agents for HIV prevention based upon their structural position. International Network of Social Network Analysis 32nd Annual Meeting; Redondo Beach. 2012. [Google Scholar]
- 69.Laumann EO, Youm Y. Racial/ethnic group differences in the prevalence of sexually transmitted diseases in the United States: a network explanation. Sex Transm Dis. 1999 May;26(5):250–261. doi: 10.1097/00007435-199905000-00003. PubMed PMID: 10333277. Epub 1999/05/20. eng. [DOI] [PubMed] [Google Scholar]
- 70.Doherty IA, Shiboski S, Ellen JM, Adimora AA, Padian NS. Sexual bridging socially and over time: a simulation model exploring the relative effects of mixing and concurrency on viral sexually transmitted infection transmission. Sex Transm Dis. 2006 Jun;33(6):368–373. doi: 10.1097/01.olq.0000194586.66409.7a. PubMed PMID: 16721330. [DOI] [PubMed] [Google Scholar]
- 71.Youm Y. A sociological interpretation of emerging properties in STI transmission dynamics: walk-betweenness of sexual networks. Sex Transm Infect. 2010 Dec;86(Suppl 3):iii24–iii28. doi: 10.1136/sti.2010.044008. PubMed PMID: 21098054. [DOI] [PubMed] [Google Scholar]
- 72.Kerani RP, Golden MR, Whittington WL, Handsfield HH, Hogben M, Holmes KK. Spatial bridges for the importation of gonorrhea and chlamydial infection. Sex Transm Dis. 2003 Oct;30(10):742–749. doi: 10.1097/01.OLQ.0000092351.75454.41. PubMed PMID: 14520171. [DOI] [PubMed] [Google Scholar]
- 73.Nordvik MK, Liljeros F, Osterlund A, Herrmann B. Spatial bridges and the spread of Chlamydia: the case of a county in Sweden. Sex Transm Dis. 2007 Jan;34(1):47–53. doi: 10.1097/01.olq.0000222722.79996.4b. PubMed PMID: 16773031. [DOI] [PubMed] [Google Scholar]
- 74.Anderson R, May R. Infectious Diseases of Humans: Dynamics and Control. New York: Oxford University Press; 1991. [Google Scholar]
- 75.Holme P, Ghoshal G. The Diplomat's Dilemma: Maximal Power for Minimal Effort in Social Networks. Understanding Complex Systems. 2009 [Google Scholar]
- 76.Cancian F. The innovator’s situation: Upper-middle-class conservatism in agricultural communities. Palo Alto: Stanford University Press; 1979. [Google Scholar]
- 77.Laumann EO. Bonds of Pluralism: The Form and Substance of Urban Social Networks. New York: John Wiley and Sons Inc; 1973. [Google Scholar]
- 78.Schneider JA, Green K, Nelson C, Westbrook M, Michaels S, Benbow N, et al. Estimating the number of Black men who have sex with men in Chicago: Cost implications of continued high HIV incidence. National African American MSM Leadership Conference on HIV/AIDS and other Health Disparities; January 19–22; New Orleans, LA. 2012. [Google Scholar]
- 79.Laumann EO, Marsden PV, Prensky D. The Boundary Specification Problem in Network Analysis. In: Freeman LC, White DR, Romney AK, editors. Research Methods in Social Network Analysis. Fairfax, VA: George Mason University Press; 1989. [Google Scholar]
- 80.Latkin CA, Sherman S, Knowlton A. HIV prevention among drug users: Outcome of a network-oriented peer outreach intervention. Health Psychology. 2003 Jul;22(4):332–339. doi: 10.1037/0278-6133.22.4.332. PubMed PMID: WOS:000184530300001. English. [DOI] [PubMed] [Google Scholar]
- 81.Latkin CA, Donnell D, Metzger D, Sherman S, Aramrattna A, Davis-Vogel A, et al. Soc Sci Med. 2008. Dec 12, The efficacy of a network intervention to reduce HIV risk behaviors among drug users and risk partners in Chiang Mai, Thailand and Philadelphia, USA. PubMed PMID: 19070413. [DOI] [PMC free article] [PubMed] [Google Scholar]