Abstract
Background
Performing habitual physical activity (PA) is challenging for many bariatric surgery patients.
Purpose
We used electronic ecological momentary assessment to naturalistically examine whether insufficient PA among bariatric surgery patients was due to infrequent PA intentions or inadequate follow through on PA intentions.
Method
Twenty-one patients 6-months post-bariatric surgery were recruited from multiple clinics in Providence, Rhode Island, USA. Participants used a palmtop computer upon waking for 6 days to indicate whether they intended to be active, and if so, the amount of PA they intended to perform in bouts ≥10 min. Each evening, participants reported PA minutes and barriers encountered that day.
Results
All 21 participants reported intending to be active on at least 1 day but only 9 (42%) intended to be active on ≥70% of days. Twelve (57%) participants performed PA on each of the days they intended, but none achieved the amount of PA they intended on all of these days. Overall, participants had PA intentions on 81 of 123 days (66%); these were partially implemented (≥10 PA minutes) on 49 days, but fully implemented on only 15 days. Participants spent 34 min in PA, or 20 fewer minutes than intended. “Lack of time” was the only frequently cited barrier, particularly on days that PA was neither intended nor performed.
Conclusion
Few patients intended to be active on a near daily basis and all patients had difficulty in implementing their intentions. Interventions that target planning strategies may help facilitate PA intentions and limit discrepancy between intended and actual PA.
Keywords: Physical activity, Ecological momentary assessment, Behavioral intention, Obesity, Bariatric surgery
Introduction
Compliance with prescribed engagement in habitual physical activity (PA) after bariatric surgery is difficult for many patients [1–5]. This is problematic given that these patients tend to lose less weight compared to those patients who adhere to a regular program of PA [6–8]. Thus, gaining a better understanding of factors that influence PA adherence in this patient population may have important implications for increasing PA and optimizing weight loss outcomes.
A key factor in explaining behavioral adherence is intention or motivation to perform a behavior. Prominent theories of health behavior (e.g., Theory of Planned Behavior) feature behavioral intention as a proximal and important determinant of behavior [9, 10]. However, intentions are less likely to be translated into action when ability to perform the behavior is impeded by factors believed to be beyond one’s control [9, 10]. This is particularly the case with PA in obese individuals, where such factors (e.g., time, weather, pain/fear of injury, weight/health status, etc.) are frequently perceived as hindering ability to adhere to habitual PA [11–14]. To our knowledge, only one previous study has examined the role of intention in PA among obese patients after undergoing bariatric surgery [15]. Results showed that stronger intentions to exercise were related to greater self-reported leisure-time PA. Additional research in this area is clearly needed.
The assessment strategy used to measure the relationship between intention and PA behavior is important. It is well known that the retrospective self-report measures (e.g., questionnaires and interviews) that are often used to assess participants’ health behaviors from the preceding weeks and months are susceptible to bias that can affect validity [16–19]. Human memory is not often highly accurate over such periods, which may lead individuals to rely on their current behavior and/or mood state, for example, to reconstruct what they assume their behavior must have been. Social desirability bias may further influence participants to report behavior that is consistent with what participants believe researchers and clinicians want and expect. Thus, it has been suggested that retrospective self-report measures should be used with caution [20].
The current study advances knowledge of PA intentions and behavior in bariatric surgery patients by using ecological momentary assessment (EMA) to examine the relationship between PA intention and PA behavior naturalistically in real time. Modern EMA typically involves the use of a palmtop computer or mobile phone to measure participants’ current behaviors, internal states, and/or environmental conditions several times per day over several days or longer [20]. EMA is thought to be less susceptible to biases of retrospective self-report because participants report on events as they occur. Furthermore, the strategy of sampling behavior over repeated occasions may result in more reliable conclusions. The current study is the first to use EMA to assess the: (1) frequency with which patients intended to be active and the amount of PA they intended to perform; (2) extent to which PA intentions reported at the start of the day were fulfilled by the end of the day; and (3) associations between PA barriers and implementation of PA intentions.
Methods
Participants and Procedures
Participants were recruited from surgery clinics in Providence, RI, USA and had laparoscopic adjustable gastric banding (LAGB) or Roux-en-Y gastric bypass surgery (RYGB) approximately 6 months before study enrollment. Recruitment procedures have been described in detail previously [4]. Of 32 patients who expressed interest in the study and granted permission to be contacted, 21 attended a study orientation during which they provided consent, received training on how to use the EMA electronic device, and had their height and weight measured. Participant’s preoperative weights were obtained from their medical record. Participants were encouraged to exercise as part of the routine standard care offered by the bariatric surgery team but were not given any exercise goals as part of this study. The study was described to participants as an evaluation of health behaviors in bariatric surgery patients.
The battery-operated PalmPilot m500 handheld computer was used to collect all EMA data. The Satellite Forms software package was used to develop and deliver the survey forms used to collect participant data via the device during EMA. Participants used a stylus to select response options to multiple choice options on a touch screen. Training participants in the use of this device consisted of at least a 1-day simulation of responding to questions about PA intentions; reporting frequency, intensity and duration of PA performed; and indicating barriers to PA. Participants completed practice ratings until they could report in response to hypothetical scenarios without error. Participants were instructed to begin the EMA protocol immediately after conclusion of the training session and continue reporting for at least 6 consecutive days. On average participants required less than 5 min to complete each EMA assessment. At the end of the 6-day EMA protocol, participants returned the device to the research laboratory where the device was connected to a personal computer to download the EMA data. To promote compliance with responding, participants were sent reminders in the form of an audible tone at six semi-random times during the day for either the first or last 3 days of their participation (randomly assigned). Participants received $50 after completing all study requirements. Study procedures were approved by The Miriam Hospital Institutional Review Board (Providence, RI, USA).
Measures
EMA of PA Intentions, Behaviors and Barriers
Upon waking each day, participants were asked whether they intended to be active that day, and if so, the number of PA minutes they intended to accumulate in bouts of at least 10 min in duration. Each evening, participants provided information on PA performed that day including minutes of PA performed and the intensity at which different activities were performed using the talk test [21]. Participants also indicated “yes” or “no” to whether they encountered any of a number of listed barriers (i.e., lack of time, too tired, pain or discomfort, lack of equipment, no place to exercise, poor weather, having to exercise alone, illness, and do not like exercise) each evening, regardless of reported PA levels. Participants also responded to questions about eating behavior that have been reported on previously [4]. Given that participants started and ended their days at varying times, the questions asked upon waking and in the evening were completed at times selected by the participant and were not prompted.
Demographic characteristics
Data on demographics (i.e., age, race/ethnicity, marital status, and education level) were collected via questionnaire.
Statistical Analysis
Descriptive statistics were generated for all variables, including means and standard errors (SE) for continuous variables and raw counts with percentages for categorical variables. Linear mixed models adjusting for non-independence of observations were used to estimate means and SEs for continuous variables assessed via EMA (i.e., minutes of PA) and to evaluate the association between minutes of intended and performed PA. A nonlinear mixed model adjusting for non-independence of observations was used to evaluate the proportion of days that lack of time was reported as a barrier to PA (yes/no; outcome modeled using the Bernoulli distribution), comparing days that participants reported no intention to be active and did not accumulate any PA, versus days they reported PA intentions, but did not fully implement their intention. Data from 123 days of EMA in which participants completed both a morning and an evening rating were included in the analysis. The 3 days with insufficient adherence to the EMA protocol that were excluded from analysis were distributed over three participants, thus allowing each participant to contribute roughly equally to all analysis.
Results
Participant Characteristics
The 21 participants were 48.5±2.8 years old, primarily female (81%), White (71.4%), and married (57.1%), with less than a 4-year college degree (66.7%). Before surgery, they weighed 128.1±4.2 kg, with a body mass index (BMI) of 48.1±1.8. Upon study enrollment 6.1±0.5 months after surgery (7 RYGB and 14 LAGB), participants had lost 21.4±1.7% of their initial body weight to achieve a new weight of 100.6± 3.5 kg, and a BMI of 37.8±1.6.
PA Intentions and PA Behavior
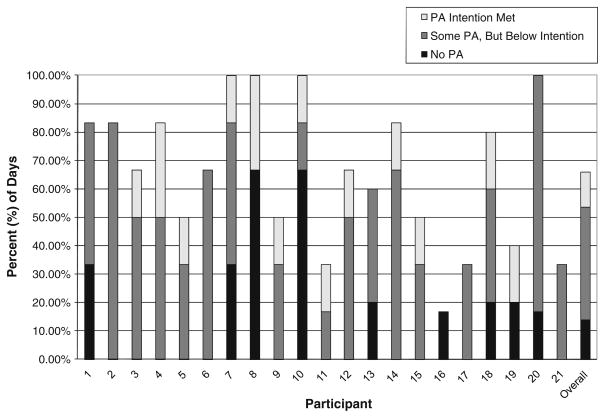
Figure 1 depicts the frequency of PA intentions and the extent to which intended amounts of PA were achieved for each of the 21 participants. All participants intended to be active on at least 1 day. However, only 9 of the 21 (42%) intended to be active on ≥70% of days. Twelve participants (57.1%) performed some PA on each of the days they intended to be active, but none achieved their target PA amount on all of these days.
Fig. 1.
Frequency of physical activity intentions and extent to which intended amounts of physical activity were achieved: by participant and across days. White bars PA intention met; gray bars some PA, but below intention; black bars no PA. Note. The total height of the bar represents the percentage of days that each participant intended to be active. The shading represents the degree to which the intended amount of PA was achieved
As represented by the far right bar in Fig. 1, participants reported an intention to be physically active on 81 of 123 days (65.9%) and planned to perform an average of 53.7±3.6 min of activity per day. Participants partially implemented their intention (performed at least 10 min of PA) on 49 (60.5%) of the 81 days, but fully implemented their intentions on only 15 (18.5%) of these 81 days. On days that participants intended to be active and performed some PA, they spent an average of 42.2±3.9 min in PA. However, averaging across all days that they intended to be active (including those when PA was not performed), participants performed 34.0±3.4 min of PA. The average discrepancy between intended and actual PA was a deficit of 19.6±3.5 min. The number of minutes that participants planned to be active was similar on days that PA was actually performed (52.8±3.5 min) versus not performed (52.1±3.8). Higher minutes of intended PA were associated with higher minutes of performed PA (coefficient=0.3, SE=0.2, p=0.029).
Participants reported no intention to be physically active on 42 of 123 days (34.2%). PA was performed in the absence of a previously reported intention on only 1 of these 42 days (2.4%), for 10 min, during the EMA period.
PA Barriers
“Lack of time” was the most commonly endorsed PA barrier (reported on 34.2% of EMA days, n=42 days), followed by “too tired” (7.3% of EMA days, n=9 days), “pain or discomfort” (4.9% of EMA days, n=6 days), “poor weather” (4.1% of EMA days, n=5 days), “lack of equipment” (1.6% of EMA days, n=2 days), “no place to exercise” (1.6% of EMA days, n=2 days), “do not like exercise” (1.6% of EMA days, n=2 days), “illness” (0.8% of EMA days, n= 1 days), and “having to exercise alone” (0% of EMA days, n=0 days). The proportion of days that “lack of time” reported as a barrier was greater on days that participants reported no intention to be active and did not accumulate any PA (33 of 42 days), versus days they reported PA intentions, but did not fully implement their intention (9 of 66 days; adjusted OR=22.7, p<0.001).
Discussion
Severely obese individuals who undergo bariatric surgery often find it challenging to adhere to a regular structured PA routine [1–5]. The present study employed EMA methodology to discern, over multiple days, whether insufficient PA in a bariatric surgery patient sample was due to low occurrence of PA intentions or failure to follow through on PA intentions. Our findings suggest that both of these issues contribute to bariatric surgery patients’ lower PA levels. Of the 21 participants, 12 or the majority (58%) did not intend to be active on a near daily basis, and 8 of these 12 participants intended to be active on only half or less of days. Clearly, when participants did not intend to be active, they did not perform PA, but even when they did intend to be active, they only performed the amount of PA they intended on 18.5% of days. On average, participants fell 20 min short of their intended PA target on days that they intended to be active. Thus, it appears that most bariatric surgery patients do not intend to be active on most days and all have difficulty in fully implementing their intentions.
Intention or motivation to perform a behavior is featured as an important determinant of behavior in several health behavior theories [10]. Accordingly, we found that PA was rarely performed in the absence of an intention. Additionally, our findings suggest that participants’ lack of PA intentions frequently owed to time constraints. Although it is unclear whether participants’ perception of “lack of time” is congruent with reality or merely a proxy for low PA motivation; interventions that provide guidance in time management may help to increase the frequency of both PA intentions and behavior among bariatric surgery patients.
Consistent with previous research in examining the role of intention in PA behavior in obese individuals [13, 15] and the general population [22], we found that intention to engage in PA was associated with more frequent engagement in PA. Moreover, participants who intended to perform greater PA or set higher PA goals engaged in higher levels of PA. Similarly, a previous study showed that obese individuals who were prescribed higher PA goals within the context of behavioral weight loss treatment engaged in higher levels of PA [23]. Consequently, future research is needed to test which goal setting approaches are most efficacious for increasing PA in bariatric surgery patients.
Our findings also suggest that intention to engage in higher PA levels alone may be insufficient to fully achieve desired PA levels. Even on days that participants intended to be active, they rarely performed the amount of PA they intended. Past research suggests that this discrepancy may be due to factors such as placing less value on the positive health consequences of PA and beliefs that engaging in regular PA is too tiring or time consuming [24]. In line with this latter barrier, studies also suggest that incongruence between PA intentions and behavior may be a product of inadequate planning. Planning has a direct influence on PA behavior and is also a mediator of the relationship between PA intentions and behavior such that those who intend to engage in PA are more likely to plan and those who do plan are more likely to engage in PA [25, 26]. Thus, interventions that focus on helping bariatric surgery patients plan when, where, and how they will perform PA may help them bridge the division between their intended and actual levels of PA.
This study is novel in that it is the first to utilize EMA to conduct a naturalistic, real-time assessment of the relationship between PA intentions and behavior in severely obese patients after bariatric surgery. However, our findings should be viewed within the context of certain limitations. Our study was conducted among a small group of patients who may have had more frequent PA intentions compared to the general bariatric surgery population. Our small sample comprised mostly of female patients who underwent different surgical procedures (that produce different rates of weight loss) limited our ability to produce valid estimates of associations between PA intentions/behavior and factors such as gender, BMI, and weight loss. Consequently, future studies incorporating larger and more diverse samples are needed so that appropriate analyses can be conducted to explore factors underlying the PA intention and behavior relationship in this population.
It is promising that participants reported an average of 34 PA minutes on days that PA was intended, which if performed consistently would fulfill national recommendations [27]. However, this finding should be interpreted with caution. While the EMA protocol required participants to report on PA each day, thereby limiting retrospective bias, participants may still have overestimated their PA. Moreover, given our previous work showing that patients’ postoperative PA levels are much higher when assessed via self-report versus objective measures [5], future EMA studies in this area should incorporate an objective PA measure (i.e., accelerometry).
Although we attempted to examine the relationship of different PA barriers to bariatric surgery patients’ PA-related intentions and behavior, “lack of time” was the only barrier that participants endorsed with any regularity. Consequently, additional research is needed to identify other barriers to PA and their association with intentions and motivation to exercise in bariatric surgery patients. We did not assess constructs shown to influence PA intention, particularly attitude, social norms, and perceived behavioral control [13, 15, 22, 26, 28, 29]. Future studies are needed to examine variables that influence PA intentions in bariatric surgery patients and thus can be targeted to increase PA. Finally, while we only studied bariatric surgery patients, infrequent PA intentions and/or failure to follow through on PA intentions is a common problem in the general population as evidenced by low adherence to PA recommendations [30]. However, obese individuals, including those who have undergone bariatric surgery, appear to experience greater difficulty in this domain than individuals who have a normal weight [1–5, 8, 31, 32] and thus may require additional intervention to modify PA intentions and behavior.
In conclusion, we found that the majority of bariatric surgery patients in our sample did not intend to be active on nearly daily basis. Additionally, when patients did intend to be active, they rarely performed the amount of PA they intended. Thus, future studies are needed to determine whether planning strategies can help bariatric surgery patients to increase and successfully implement PA intentions so as to promote greater PA participation and consistency.
Acknowledgments
Appreciation is expressed to Jennifer Trautvetter, B.A. for assisting with participant recruitment. Dr. Bond is supported by the National Institutes of Health grant K01 DK083438, Increasing physical activity among inactive bariatric surgery patients.
Contributor Information
Dale S. Bond, Email: dbond@lifespan.org, Department of Psychiatry and Human Behavior, Warren Alpert Medical School of Brown University, The Miriam Hospital/Weight Control and Diabetes Research Center, 196 Richmond Street, Providence, RI, USA 02903
J. Graham Thomas, Department of Psychiatry and Human Behavior, Warren Alpert Medical School of Brown University, The Miriam Hospital/Weight Control and Diabetes Research Center, 196 Richmond Street, Providence, RI, USA 02903.
Beth A. Ryder, Department of Surgery, Warren Alpert Medical School of Brown University, Rhode Island Hospital, Providence, RI, USA
Sivamainthan Vithiananthan, Department of Surgery, Warren Alpert Medical School of Brown University, The Miriam Hospital, Providence, RI, USA.
Dieter Pohl, Department of Surgery, Roger Williams Hospital, Providence, RI, USA.
Rena R. Wing, Department of Psychiatry and Human Behavior, Warren Alpert Medical School of Brown University, The Miriam Hospital/Weight Control and Diabetes Research Center, 196 Richmond Street, Providence, RI, USA 02903
References
- 1.Welch G, Wesolowski C, Piepul B, Kuhn J, Romanelli J, Garb J. Physical activity predicts weight loss following gastric bypass surgery: findings from a support group survey. Obes Surg. 2008;18:517–24. doi: 10.1007/s11695-007-9269-x. [DOI] [PubMed] [Google Scholar]
- 2.Bond DS, Phelan S, Leahey TM, Hill JO, Wing RR. Weight-loss maintenance in successful weight losers: surgical vs non-surgical methods. Int J Obes (Lond) 2009;33:173–80. doi: 10.1038/ijo.2008.256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Toussi R, Fujioka K, Coleman KJ. Pre- and postsurgery behavioral compliance, patient health and postbariatric surgical weight loss. Obesity (Silver Spring) 2009;17:996–1002. doi: 10.1038/oby.2008.628. [DOI] [PubMed] [Google Scholar]
- 4.Thomas JG, Bond DS, Ryder BA, Leahey TM, Vithiananthan S, Roye GD, et al. Ecological momentary assessment of recommended postoperative eating and activity behaviors. Surg Obes Relat Dis. 2011;7:206–12. doi: 10.1016/j.soard.2010.10.007. [DOI] [PubMed] [Google Scholar]
- 5.Bond DS, Jakicic JM, Unick JL, Vithiananthan S, Pohl D, Roye GD, et al. Pre- to postoperative physical activity changes in bariatric surgery patients: self-report vs. objective measures. Obesity (Silver Spring) 2010;18:2395–7. doi: 10.1038/oby.2010.88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Evans RK, Bond DS, Wolfe LG, Meador JG, Herrick JE, Kellum JM, et al. Participation in 150 min/wk of moderate or higher intensity physical activity yields greater weight loss after gastric bypass surgery. Surg Obes Relat Dis. 2007;3:526–30. doi: 10.1016/j.soard.2007.06.002. [DOI] [PubMed] [Google Scholar]
- 7.Bond DS, Phelan S, Wolfe LG, Evans RK, Meador JG, Kellum JM, et al. Becoming physically active after bariatric surgery is associated with improved weight loss and health-related quality of life. Obesity (Silver Spring) 2009;17:78–83. doi: 10.1038/oby.2008.501. [DOI] [PubMed] [Google Scholar]
- 8.Josbeno DA, Kalarchian M, Sparto PJ, Otto AD, Jakicic JM. Physical activity and physical function in individuals post-bariatric surgery. Obes Surg. 2011;21(8):1243–9. doi: 10.1007/s11695-010-0327-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Azjen I. The theory of planned behavior. Organ Behav Hum Decis Process. 1991;50:179–211. [Google Scholar]
- 10.Maddux JE, DuCharme KA. Behavioral intentions in theories of health behavior. In: Gochman DS, editor. Handbook of health behavior research 1: personal and social determinants. New York: Plenum; 2007. pp. 133–51. [Google Scholar]
- 11.Andersen RE, Jakicic JM. Interpreting the physical activity guidelines for health and weight management. J Phys Act Health. 2009;6:651–6. doi: 10.1123/jpah.6.5.651. [DOI] [PubMed] [Google Scholar]
- 12.Napolitano MA, Papandonatos GD, Borradaile KE, Whiteley JA, Marcus BH. Effects of weight status and barriers on physical activity adoption among previously inactive women. Obesity (Silver Spring) 2011;19(11):2183–9. doi: 10.1038/oby.2011.87. [DOI] [PubMed] [Google Scholar]
- 13.Godin G, Amireault S, Belanger-Gravel A, Vohl MC, Perusse L. Prediction of leisure-time physical activity among obese individuals. Obesity (Silver Spring) 2009;17:706–12. doi: 10.1038/oby.2008.599. [DOI] [PubMed] [Google Scholar]
- 14.Wouters EJ, Larsen JK, Zijlstra HA, van Ramshorst B, Geenen R. Physical activity after surgery for severe obesity: the role of exercise cognitions. Obes Surg. 2011;21(12):1894–9. doi: 10.1007/s11695-010-0276-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hunt HR, Gross AM. Prediction of exercise in patients across various stages of bariatric surgery: a comparison of the merits of the theory of reasoned action versus the theory of planned behavior. Behav Modif. 2009;33:795–817. doi: 10.1177/0145445509348055. [DOI] [PubMed] [Google Scholar]
- 16.Stone AA, Shiffman S, Atienza AA, Nebeling L. Historical roots and rationale of ecological momentary assessment (EMA) In: Stone AA, Shiffman S, Nebeling L, editors. The science of real-time data capture: self-reports in health research. New York: Oxford University Press; 2007. pp. 3–10. [Google Scholar]
- 17.Schwarz N. Retrospective and concurrent self-reports: the rationale for real-time data capture. In: Stone AA, Shiffman S, Nebeling L, editors. The science of real-time data capture: Self-reports in health research. New York: Oxford University Press; 2007. pp. 11–26. [Google Scholar]
- 18.Smyth J, Wonderlich S, Crosby R, Miltenberger R, Mitchell J, Rorty M. The use of ecological momentary assessment approaches in eating disorder research. Int J Eat Disord. 2001;30:83–95. doi: 10.1002/eat.1057. [DOI] [PubMed] [Google Scholar]
- 19.Gorin AA, Stone AA. Recall biases and cognitive errors in retrospective self-reports: a call for momentary assessments. In: Baum A, Revenson T, Singer J, editors. Handbook of health psychology. Lawrence Erlbaum Associates; Mahwah: 2001. pp. 405–13. [Google Scholar]
- 20.Thomas JG, Bond DS, Sarwer DB, Wing RR. Technology for behavioral assessment and intervention in bariatric surgery. Surg Obes Relat Dis. 2011;7:548–57. doi: 10.1016/j.soard.2011.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Persinger R, Foster C, Gibson M, Fater DC, Porcari JP. Consistency of the talk test for exercise prescription. Med Sci Sports Exerc. 2004;36:1632–6. [PubMed] [Google Scholar]
- 22.Rhodes RE, Courneya KS, Blanchard CM, Plotnikoff RC. Prediction of leisure-time walking: an integration of social cognitive, perceived environmental, and personality factors. Int J Behav Nutr Phys Act. 2007;4:51. doi: 10.1186/1479-5868-4-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jeffery RW, Wing RR, Sherwood NE, Tate DF. Physical activity and weight loss: does prescribing higher physical activity goals improve outcome? Am J Clin Nutr. 2003;78:684–9. doi: 10.1093/ajcn/78.4.684. [DOI] [PubMed] [Google Scholar]
- 24.Godin G, Shephard RJ, Colantonio A. The cognitive profile of those who intend to exercise but do not. Public Health Rep. 1986;101:521–6. [PMC free article] [PubMed] [Google Scholar]
- 25.Reuter T, Ziegelmann JP, Lippke S, Schwarzer R. Long-term relations between intentions, planning, and exercise: a 3-year longitudinal study after orthopedic rehabilitation. Rehabil Psychol. 2009;54:363–71. doi: 10.1037/a0017830. [DOI] [PubMed] [Google Scholar]
- 26.Conner M, Sandberg T, Norman P. Using action planning to promote exercise behavior. Ann Behav Med. 2010;40:65–76. doi: 10.1007/s12160-010-9190-8. [DOI] [PubMed] [Google Scholar]
- 27.Haskell WL, Lee IM, Pate RR, Powell KE, Blair SN, Franklin BA, et al. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Med Sci Sports Exerc. 2007;39:1423–34. doi: 10.1249/mss.0b013e3180616b27. [DOI] [PubMed] [Google Scholar]
- 28.Boudreau F, Godin G. Understanding physical activity intentions among French Canadians with type 2 diabetes: an extension of Ajzen’s theory of planned behaviour. Int J Behav Nutr Phys Act. 2009;6:35. doi: 10.1186/1479-5868-6-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Vallance JK, Murray TC, Johnson ST, Elavsky S. Understanding physical activity intentions and behavior in postmenopausal women: an application of the theory of planned behavior. Int J Behav Med. 2011;18:139–49. doi: 10.1007/s12529-010-9100-2. [DOI] [PubMed] [Google Scholar]
- 30.Troiano RP, Berrigan D, Dodd KW, Mâsse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40:181–8. doi: 10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- 31.Davis JN, Hodges VA, Gillham MB. Physical activity compliance: differences between overweight/obese and normal-weight adults. Obesity. 2006;14:2259–65. doi: 10.1038/oby.2006.265. [DOI] [PubMed] [Google Scholar]
- 32.Bond DS, Jakicic JM, Vithiananthan S, Thomas JG, Leahey TL, Sax HC, et al. Objective quantification of physical activity in bariatric surgery candidates and normal-weight controls. Surg Obes Relat Dis. 2010;6:72–8. doi: 10.1016/j.soard.2009.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]