Abstract
Bariatric surgery patients report significant pre- to postoperative increases in physical activity (PA). However, it is unclear whether objective measures would corroborate these changes. The present study compared self-reported and accelerometer-based estimates of changes in moderate-to-vigorous intensity PA (MVPA) from pre- (pre-op) to 6 months postsurgery (post-op). Twenty bariatric surgery (65% laparoscopic-adjustable gastric banding, 35% gastric bypass) patients (46.2 ± 9.8 years, 88% female, pre-op BMI = 50.8 ± 9.7 kg/m2) wore RT3 accelerometers as an objective measure of MVPA and completed the Paffenbarger Physical Activity Questionnaire (PPAQ) as a subjective measure before and 6 months after bariatric surgery. Time (min/week) spent in MVPA was calculated for the PPAQ and RT3 (≥1-min and ≥10-min bouts) at pre-op and post-op. Self-reported MVPA increased fivefold from pre-op to post-op (44.6 ± 80.8 to 212.3 ± 212.4 min/week; P < 0.005). By contrast, the RT3 showed nonsignificant decreases in MVPA for both ≥1-min (186.0 ± 169.0 to 151.2 ± 118.3 min/week) and ≥10-min (41.3 ± 109.3 to 39.8 ± 71.3 min/ week) bouts. At pre-op, the percentage of participants who accumulated ≥150-min/week of MVPA in bouts ≥10-min according to the PPAQ and RT3 was identical (10%). However, at post-op, 55% of participants reported compliance with the recommendation compared to 5% based on RT3 measurement (P = 0.002). Objectively-measured changes in MVPA from pre-op to 6 months post-op appear to be much smaller than self-reported changes. Further research involving larger samples is needed to confirm these findings and to determine whether self-report and objective PA measures are differentially associated with surgical weight loss outcomes.
INTRODUCTION
There is growing interest in the role of physical activity (PA) in promoting optimal weight loss after bariatric surgery. Previous research suggests that patients become more physically active postoperatively (1,2). In a recent study (1), patients reported increasing their moderate-to-vigorous intensity PA (MVPA) by an average of 280 min/week from pre- (pre-op) to 1 year postsurgery (post-op). Additionally, patients who went from being inactive (<200 min/week) to active (≥200 min/week) postoperatively had greater weight losses than those who remained inactive. However, these findings are based on subjective PA measures which are susceptible to over-reporting, particularly in obese individuals (3). Thus, it is unclear whether reported PA changes across pre- and postoperative intervals would be confirmed by an objective measure.
Therefore, we compared self-reported and accelerometer-based estimates of pre- to 6-month postoperative changes in MVPA. Additionally, we examined whether adherence to recommendations to accumulate ≥150 min/week of MVPA in ≥10-min bouts (4) differed according to measurement type at each time point.
METHODS
Participants and procedures
Participants aged 18–65 years, with a BMI ≥35 kg/m2, who were ambulatory and preparing to undergo Roux-en-Y gastric bypass or laparoscopic-adjustable gastric banding were given an accelerometer to wear for seven consecutive days. The PA questionnaire was administered via telephone 8 days after accelerometers were received to reflect the same week of activity. Identical procedures were conducted at 6 months postoperatively. Participants were encouraged by their surgeon to increase engagement in PA but received no formal exercise prescription. Participants were paid $15 and $20 at the pre- and postoperative time points, respectively. Study procedures were approved by the Miriam Hospital’s institutional review board (Providence, RI).
Measurement of PA
Self-reported PA
The Paffenbarger Physical Activity Questionnaire (PPAQ) quantifies activity-related energy expenditure by querying participants on the number of city blocks walked and stair flights climbed, and the duration and frequency of sports and recreational activities performed during the past week. For the current study, we calculated MVPA min/week by summing time spent walking and performing sports and recreation activities that were of at least a moderate intensity according to the PPAQ coding scheme (5). To convert city blocks walked/day into walking minutes/week, we assumed a 3.0 mph walking pace.
Objective PA
The RT3 (Stayhealthy, Monrovia, CA) is a waist-mounted accelerometer that provides data on PA patterns by converting accelerations from vertical, horizontal, and anterior–posterior planes into counts. A previously published cutoff (≥984 activity counts/ min) was used to define MVPA (≥3 METs) (6). Weekly MVPA performed in bouts of ≥1 min and ≥10 min was computed. For data to be valid, participants had to have ≥8 h of RT3 wear/day for ≥4 days (and have completed the PPAQ) at both the pre- and postoperative intervals. To make the RT3 and PPAQ measurement periods comparable, RT3 data were standardized to a 1-week period by multiplying average daily MVPA minutes by 7.
Statistical analysis
Analyses were performed using SPSS for Windows (14.0). Paired-sample t-tests were used to examine changes in self-reported and objectively-measured MVPA. Repeated-measures ANOVA was used to examine whether changes in MVPA differed by mode of measurement and McNemar’s test to compare the proportion of participants who accumulated ≥150 min/week of MVPA in bouts ≥10 min (3).
RESULTS
Participants
Participants (N = 31) were given an RT3 and asked to complete the PPAQ at pre-op and 6 months post-op. Of these, 25 (81%) completed the PPAQ at both times. Twenty of these 25 had ≥4 valid RT3 wear days. Subsequent analyses focus on these 20 participants. On average, participants were 47.1 ± 9.6 years of age, with BMI = 50.1 ± 9.1 kg/m2 and weighed 137.9 ± 32.1 kg. Most were female (85%) and Caucasian (85%), and 65% had the laparoscopic-adjustable gastric banding operation.
Differences in MVPA changes between self-report and objective measures
Participants wore the RT3 for an average of 13.9 ± 3.9 h/day over 6.5 ± 1.2 days. Figure 1 shows that pre- to postoperative changes in MVPA were significantly different between the PPAQ and RT3 (both ≥1- and ≥10-min bouts) (Ps < 0.005). Although participants reported an average weekly increase of 168 min of MVPA on the PPAQ, RT3-measured MVPA decreased by 35 min for ≥1-min bouts and 1.5 min for ≥10-min bouts. Changes in MVPA according to the PPAQ were not significantly associated with changes in RT3-measured MVPA (both ≥1- and ≥10-min bouts) (Ps > 0.25). Results of analyses including participants with ≥1 valid days of RT3 wear (n = 25) were similar (data not shown).
Figure 1.
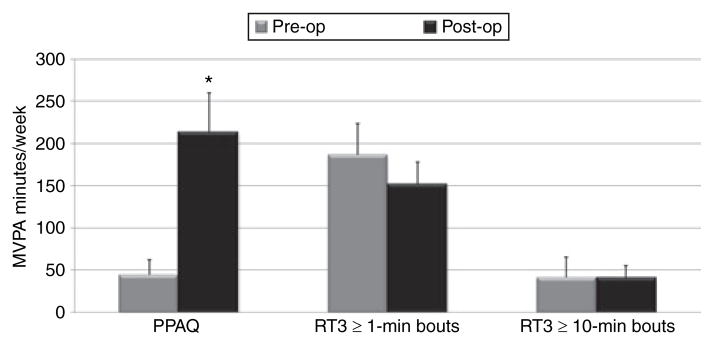
Physical activity at pre- and 6 months postsurgery according to a self-report measure and an objective measure. *P = 0.004, PPAQ postsurgery (post-op) significantly different from PPAQ presurgery (pre-op); mean (s.e.m.) shown; PPAQ, Paffenbarger Physical Activity Questionnaire; RT3, accelerometer; MVPA, moderate-to-vigorous intensity physical activity.
Preoperatively, the percentage (10%) of participants identified by the PPAQ and RT3 as meeting the recommendation to accumulate ≥150 min/week of MVPA in bouts ≥10 min was identical. Postoperatively, 55% reported compliance with the recommendation compared to 5% based on RT3 measurement (P = 0.002). Similarly, MVPA according to the PPAQ was significantly associated with RT3-measured MVPA (both ≥1- and ≥10-min bouts) preoperatively (rs > 0.50, Ps < 0.05) but not postoperatively (Ps > 0.10).
DISCUSSION
This is the first study to compare self-reported and accelerometer-based estimates of pre- to postoperative PA changes in a bariatric surgery population. Consistent with previous research (1), our participants reported a near five-fold increase in MVPA. By contrast, objective accelerometer data indicated no significant changes in MVPA, suggesting limited concordance between the two measures. Additionally, postoperatively, the majority (55%) of participants reported engaging in ≥150 min/week of MVPA; however only one participant met this recommendation according to the accelerometer.
The most obvious explanation for this discrepancy is that participants over-reported their PA postoperatively. Time spent in MVPA according to the PPAQ and RT3 were similar preoperatively, although only for bouts ≥10 min suggesting that the PPAQ captured longer, sustained periods of MVPA rather than sporadic or short bouts. The reasons for greater over-reporting postoperatively and whether this over-reporting is intentional or unintentional are not clear. Participants may have believed that they were expected to increase engagement in PA postoperatively, or felt more active because of improved functional capacity and health-related quality of life (7). However, the latter notion contrasts with previous research that suggests larger reported postoperative changes in PA contribute to greater health-related quality-of-life improvements rather than vice versa (1). Finally, although over-reporting could seemingly be attributed to participants perceiving light PA to be of a higher intensity, we found no objective support for this hypothesis as indicated by a lack of pre- to postoperative changes in RT3-measured light or total PA (data not shown).
It is also possible that accelerometer-related issues contributed to the discrepancy between self-reported and objective MVPA. The RT3 may have under-represented activity postoperatively due to weight-related differences in gait dynamics or how the device was situated. Moreover, the RT3 count threshold used to define MVPA in this study was derived from a lean sample (5), which may not appropriately define MVPA in severely obese individuals.
This study holds particular clinical relevance given the hypothesis that increasing PA may contribute to improvement and maintenance of surgical outcomes. Our findings suggest that more precise estimates of postoperative changes in PA may be obtained through use of objective measures. In addition, providing clear definitions of what constitutes structured MVPA and having patients monitor their engagement in these activities may enhance the validity and reliability of self-reported PA and help patients to increase their MVPA postoperatively.
Although limited by a small and self-selected sample, this study is the first to compare pre- to post bariatric surgery PA changes according to a subjective and objective measure. Findings showed large subjective pre- to postoperative increases in PA that were not confirmed by objective measurement. This apparent discordance requires replication in larger samples along with comparison of the extent to which subjective versus objective measures relate to postoperative weight loss and other surgical outcomes.
Acknowledgments
This research was funded by grants from the Warren Alpert Medical School of Brown University’s Center of Excellence in Women’s Health and the National Institute of Diabetes and Digestive and Kidney Diseases (K01 DK083438-01) awarded to Drs Wing and Bond, respectively. Processing and analysis of RT3 data was possible through a grant (NIDDK P30 DK042404) awarded to Dr Jakicic and the University of Pittsburgh Obesity and Nutrition Research Center (ONRC). Appreciation is expressed to Jennifer Trautvetter and Angelica Adams for their assistance with data collection.
Footnotes
DISCLOSURE
The authors declared no conflict of interest.
References
- 1.Bond DS, Phelan S, Wolfe LG, et al. Becoming physically active after bariatric surgery is associated with improved weight loss and health-related quality of life. Obesity (Silver Spring) 2009;17:78–83. doi: 10.1038/oby.2008.501. [DOI] [PubMed] [Google Scholar]
- 2.Colles SL, Dixon JB, O’Brien PE. Hunger control and regular physical activity facilitate weight loss after laparoscopic adjustable gastric banding. Obes Surg. 2008;18:833–840. doi: 10.1007/s11695-007-9409-3. [DOI] [PubMed] [Google Scholar]
- 3.Jakicic JM, Polley BA, Wing RR. Accuracy of self-reported exercise and the relationship with weight loss in overweight women. Med Sci Sports Exerc. 1998;30:634–638. doi: 10.1097/00005768-199804000-00024. [DOI] [PubMed] [Google Scholar]
- 4.Haskell WL, Lee IM, Pate RR, et al. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Med Sci Sports Exerc. 2007;39:1423–1434. doi: 10.1249/mss.0b013e3180616b27. [DOI] [PubMed] [Google Scholar]
- 5.Paffenbarger RS, Jr, Wing AL, Hyde RT. Physical activity as an index of heart attack risk in college alumni. Am J Epidemiol. 1978;108:161–175. doi: 10.1093/oxfordjournals.aje.a112608. [DOI] [PubMed] [Google Scholar]
- 6.Rowlands AV, Thomas PW, Eston RG, Topping R. Validation of the RT3 triaxial accelerometer for the assessment of physical activity. Med Sci Sports Exerc. 2004;36:518–524. doi: 10.1249/01.mss.0000117158.14542.e7. [DOI] [PubMed] [Google Scholar]
- 7.Josbeno DA, Jakicic JM, Hergenroeder A, Eid GM. Physical activity and physical function changes in obese individuals after gastric bypass surgery. Surg Obes Relat Dis. 2008 doi: 10.1016/j.soard.2008.08.003. e-pub ahead of print 14 August 2008. [DOI] [PubMed] [Google Scholar]


