Abstract
Objectives. We investigated the association between anticipatory stress, also known as racism-related vigilance, and hypertension prevalence in Black, Hispanic, and White adults.
Methods. We used data from the Chicago Community Adult Health Study, a population-representative sample of adults (n = 3105) surveyed in 2001 to 2003, to regress hypertension prevalence on the interaction between race/ethnicity and vigilance in logit models.
Results. Blacks reported the highest vigilance levels. For Blacks, each unit increase in vigilance (range = 0–12) was associated with a 4% increase in the odds of hypertension (odds ratio [OR] = 1.04; 95% confidence interval [CI] = 1.00, 1.09). Hispanics showed a similar but nonsignificant association (OR = 1.05; 95% CI = 0.99, 1.12), and Whites showed no association (OR = 0.95; 95% CI = 0.87, 1.03).
Conclusions. Vigilance may represent an important and unique source of chronic stress that contributes to the well-documented higher prevalence of hypertension among Blacks than Whites; it is a possible contributor to hypertension among Hispanics but not Whites.
Racial and ethnic disparities in hypertension are some of the most widely studied and consequential sources of social disparities in health in the United States.1–3 For example, recent prevalence estimates show that roughly 40% of Black adults but only 30% of White adults have hypertension.4 In addition, the incidence of hypertension occurs at younger ages for Blacks than Whites.1 These disparities are reflected in the larger burden of hypertension-related health and economic costs carried by non-White than White Americans. For example, mortality rates attributable to hypertension are roughly 15 deaths per 100 000 people for White men and women; the mortality rate for Black women is 40 per 100 000 and more than 50 per 100 000 for Black men.5 Among all health conditions, hypertension accounts for the greatest portion of disparities in years of lost life.6 Economically speaking, if Black Americans had the hypertension prevalence of White Americans, about $400 million would be saved in out-of-pocket health care expenses, about $2 billion would be saved in private insurance costs, and $375 million would be saved from Medicare and Medicaid—per year.7
Despite the tremendous amount of research devoted to clarifying the factors that generate these disparities, most studies find that they persist after adjustment for a wide range of socioeconomic, behavioral, and biomedical risk factors.8 In fact, although disparities exist for several of these risk factors (e.g., socioeconomic status), numerous studies have shown no disparities in many others (e.g., smoking, obesity for men, lipid profile).2 Despite substantial investment in interventions to eliminate hypertension disparities, evidence suggests that these disparities have actually grown over the past few decades,9 suggesting that numerous unknown factors drive disparities in hypertension.3
CHRONIC STRESS AND RACIAL DISPARITIES IN HYPERTENSION
Growing evidence links chronic psychological stress to cardiovascular disease, including hypertension, and suggests that the impact of stress may be as important as other risk factors, such as cholesterol.10 In particular, researchers argue that because of sustained effects on numerous physiological systems, the anticipation of or perseveration about (i.e., continual, perhaps involuntary, repetition of a thought) a stressor (e.g., financial or marital difficulties) is what gives chronic stress its toxic qualities.11 Indeed, researchers have reported that the physiological (i.e., autonomic) stress effects attributable to the combination of stressors and worry are similar to the physiological effects of smoking.12
Many theorize that chronic stress is an important determinant of racial/ethnic disparities in health, including hypertension.9,13 Moreover, researchers posit that perceptions of racial/ethnic discrimination (defined as chronic or acute experiences with unfair treatment or abusive behavior because of their race/ethnicity) are an important mechanism through which disparities in health, including hypertension, are produced and maintained.10,14–16 However, empirical evidence has been mixed,17,18 possibly because discrimination measures generally do not account for the anticipation or perseveration that may make this type of stressor pathogenic.
Some have begun to examine the anticipatory and perseverative stress associated with racial and ethnic discrimination. For example, researchers recently reported that anticipation of ethnic discrimination was inversely associated with health in a Swedish sample.19,20 In the United States, researchers reported poorer cardiovascular outcomes, including less elasticity in large arterial vessels and higher blood pressure reactivity for those reporting higher than lower levels of anticipated racial discrimination, which the authors termed racism-related vigilance.21,22
We examined the role of racism-related vigilance in racial/ethnic disparities in hypertension prevalence in a population-based sample. We first examined whether vigilance mediated racial/ethnic disparities in hypertension prevalence. In other words, we assessed whether racial/ethnic disparities in hypertension prevalence were reduced when we accounted for racial/ethnic disparities in vigilance. In light of racial/ethnic disparities in exposure to stressors (e.g., vigilance), many researchers theorize that mediation is an important mechanism by which stress links race/ethnicity to health.9,23–25 However, there is a dearth of empirical evidence, which may be attributable to challenges in the measurement of racially salient stress.13,25 Second, because it may be that racism-related vigilance is salient only for non-White groups, we examined whether vigilance modified racial/ethnic disparities in hypertension prevalence. In other words, we asked whether increasing levels of vigilance were associated with wider racial/ethnic disparities in hypertension prevalence. The clinical and public health implications of this research are substantial because chronic psychological stress is increasingly recognized as an important risk factor for hypertension and for cardiovascular disease more broadly.
METHODS
We used data from the Chicago Community Adult Health Study, a cross-sectional survey designed to examine the biological, social, and environmental correlates of adult physical and mental health. The study collected a multistage probability sample of 3105 adults, aged 18 years and older, living in Chicago, Illinois, stratified into 343 neighborhood clusters. Neighborhood clusters usually comprised 2 census tracts with meaningful physical and social boundaries. Study staff conducted face-to-face interviews with and took direct physical measurements from 1 respondent per household between May 2001 and March 2003, with a response rate 71.8%.
Variables
Trained technicians obtained 3 seated blood pressure measurements about 1 minute apart with Omron oscillographic devices (Omron Healthcare Inc, Lake Forest, IL). Measurements were taken in the middle of the interview after the participant had been seated for approximately 45 to 60 minutes. We took the average of the last 2 blood pressure measurements taken or, if only 2 were recorded, the average of those 2 blood pressure measurements. We defined hypertension as having a systolic blood pressure of 140 millimeters of mercury or higher, a diastolic blood pressure of 90 millimeters of mercury or higher, a report of antihypertensive medication use in the past 12 months, or a report of being told by a physician that the respondent had hypertension, a definition consistent with the literature on cardiovascular disease from the American Heart Association.5
We based racism-related vigilance measures on ethnographic research describing how participants anticipated and prepared for racial discrimination.26,27 We created a scale from responses to the following questions: In your day-to-day life, how often do you do the following things: (1) try to prepare for possible insults from other people before leaving home? (2) feel that you always have to be very careful about your appearance to get good service or avoid being harassed? and (3) try to avoid certain social situations and places? Responses were on a Likert-like scale (0 = never, 1 = < once/year, 2 = a few times/year, 3 = a few times/month, and 4 = ≥ once/week). We reverse-coded responses and summed to create a continuous scale, with higher values representing higher levels of vigilance (Cronbach α = 0.66). We categorized respondents as non-Hispanic White (White), non-Hispanic Black (Black), Hispanic, and non-Hispanic other (which included American Indian, Asian, and Pacific Islander). Because the last racial category constituted only 4% of the sample and was a mixture of races, making interpretation difficult, we reported these results in the tables for completeness, but did not analyze them.
Analyses
For descriptive analyses, we estimated means with standard errors of continuous variables and percentages of categorical variables in the total sample and by race/ethnicity. We included standard errors rather than standard deviations because we used multiply imputed data. We also estimated the percentages of each response of the vigilance measure in the total sample and by race/ethnicity. We used the t test and the χ2 test to test for differences by race/ethnicity. For our main analyses, we regressed hypertension on race/ethnicity, vigilance, their interaction, and covariates with logit models. We first regressed hypertension prevalence on race/ethnicity, with control for age, gender, and immigrant generation (≥ third, second, first; model 1). We then added education (< 12, 12–15, > 15 years) and annual household income (logged; model 2).
To examine whether vigilance mediated racial/ethnic disparities in hypertension, we then ran a series of 3 models, as recommended in the literature.28 In separate models, we regressed vigilance on race/ethnicity in a linear model and hypertension prevalence on vigilance in a logit model, with control for the variables in model 2, except race/ethnicity. We did not show these results in the tables, because, although 2 criteria for mediation were met (i.e., race/ethnicity was associated with vigilance and vigilance was associated with hypertension prevalence), the third criterion was not met (the addition of vigilance to model 2 [i.e., model 3] did not attenuate the association between race/ethnicity and hypertension prevalence).
To examine whether vigilance modified racial/ethnic disparities in hypertension, we added the interaction between race/ethnicity and vigilance (model 4). In our final model, we controlled for numerous additional hypertension risk factors: body mass index (defined as weight in kilograms divided by the square of height in meters), average intensity of weekly physical activity (0 = in bed or chair or no exercise, 1 = light exercise, 2 = light–moderate exercise, 3 = moderate–heavy exercise, 4 = heavy exercise), smoking status (never, former, current), average number of alcoholic drinks per month, and diabetes status (report of being told by a physician that the respondent had diabetes). In this model, to examine the role of racism-related vigilance in the presence of perceived discrimination, we also included 2 widely used measures of perceived unfair treatment (model 5).14 We measured major events of unfair treatment as the sum of affirmative responses to the following 4 questions: Have you ever been unfairly (1) fired or denied a promotion? (2) not hired for a job? (3) treated by the police? (4) prevented from moving into a neighborhood? We measured everyday unfair treatment on a scale created from the following questions: In your day-to-day life, how often (1) are you treated with less courtesy or respect than other people? (2) are you threatened or harassed? (3) do you receive poorer service than other people at restaurants and stores? (4) do people act as if you are not smart? (5) do people act as if they are afraid of you? Responses were on a Likert-like scale (1 = ≥ once/week, 2 = a few times/month, 3 = a few times/year, 4 = ≤ once/year, 5 = never). We reverse-coded and summed responses to create a continuous scale in which higher numbers represented reports of more frequent unfair activity.
We calculated the partial effects of vigilance for each racial/ethnic group after estimation, as the product of a vigilance coefficient (i.e., the association between vigilance and hypertension prevalence for Whites) and the appropriate interaction coefficient (i.e., the association between vigilance and hypertension prevalence for Blacks or Hispanics, beyond the association for Whites). We estimated the partial effects while holding covariates at their reference category (for categorical variables) or mean (for continuous variables).
We handled missing information on blood pressure, income, and vigilance in 2 ways, according to the amount of missing data and existence of influential outliers. First, for variables with substantial missing information, we multiply imputed blood pressure (n = 155) and income (n = 501) data with IVEware 0.2 (University of Michigan, Ann Arbor) via SAS 9.2 (SAS Institute, Cary, NC). Second, we excluded respondents with missing information on vigilance (n = 11) from final analyses, for a final sample size of 3094. In sensitivity analyses, we ran all models on the unimputed data set, and the results were similar to those presented (results not shown). We also included different transformations of the vigilance measure, specifically continuous measures, which we squared and cubed, and an ordinal measure of the quartiles of the distribution (data not shown, but qualitatively similar to those presented). To examine whether this vigilance measure was different than other stress measures, we included a stressful life events inventory in model 4 in sensitivity analyses. Results were nearly identical to those presented. We weighted all analyses to account for complex survey design, differential selection into the sample, nonresponse, and household size. With respect to age, race/ethnicity, and gender, the distribution of the weighted sample and the 2000 Census estimates were comparable to the City of Chicago. We conducted all analyses in Stata 11.0MP (StataCorp, College Station, TX) with both the MI and SVY suite of commands to account for the multiply imputed data and complex survey design, respectively.
RESULTS
Descriptive statistics for hypertension prevalence and the covariates, broken down by race/ethnicity, are presented in Table 1. Similar to national estimates, hypertension in this sample was significantly more prevalent among Blacks (49%) than Whites (33%) and Hispanics (32%). Vigilance was highest among Blacks (mean = 3.8; SE = 0.1), followed by Hispanics (mean = 2.5; SE = 0.1), and Whites (mean = 1.8; SE = 0.1). Furthermore, Blacks were more likely to report the highest frequency of vigilant behaviors. For example, 14% of Blacks reported preparing for insults weekly; only 2% of Whites and 5% of Hispanics reported this type of vigilance (Table A, available as a supplement to the online version of this article at http://www.ajph.org).
TABLE 1—
Sociodemographic and Health Characteristics in the Total Sample and by Race/Ethnicity: Chicago Community Adult Health Study, 2001–2003
| Characteristic | Total Sample (n = 3094), % or Mean ±SE | Non-Hispanic White (n = 981), % or Mean ±SE | Non-Hispanic Black (n = 1233), % or Mean ±SE | Hispanic (n = 800), % or Mean ±SE | Non-Hispanic Other (n = 80), % or Mean ±SE |
P |
||
| Black–Whitea | Hispanic–Whiteb | Hispanic–Blackc | ||||||
| Hypertensiond | 38 | 33 | 49 | 32 | 26 | < .001 | .771 | < .001 |
| Vigilance scoree | 2.7 ±0.1 | 1.8 ±0.1 | 3.8 ±0.1 | 2.5 ±0.1 | 2.3 ±0.3 | < .001 | < .001 | < .001 |
| Vigilance quartile | ||||||||
| 1 (lowest) | 37 | 45 | 27 | 44 | 37 | < .001 | .036 | < .001 |
| 2 | 8 | 10 | 6 | 6 | 7 | |||
| 3 | 20 | 23 | 17 | 16 | 32 | |||
| 4 | 34 | 22 | 51 | 34 | 23 | |||
| Age, y | 42.4 ±0.4 | 44.4 ±0.8 | 44.1 ±0.6 | 38.1 ±0.7 | 37.9 ±2.3 | .783 | < .001 | < .001 |
| Women | 53 | 50 | 58 | 52 | 43 | .007 | .659 | .029 |
| Immigrant generation | ||||||||
| First | 27 | 19 | 2 | 63 | 69 | < .001 | < .001 | < .001 |
| Second | 14 | 16 | 1 | 26 | 17 | |||
| ≥ third | 59 | 65 | 97 | 11 | 14 | |||
| Education, y | ||||||||
| < 12 | 23 | 11 | 24 | 44 | 4 | < .001 | < .001 | < .001 |
| 12–15 | 49 | 44 | 59 | 45 | 36 | |||
| ≥ 16 | 28 | 45 | 18 | 10 | 60 | |||
| Household incomef | 4.9 ±0.3 | 7.0 ±0.7 | 3.5 ±0.2 | 3.5 ±0.1 | 3.7 ±0.4 | < .001 | < .001 | .01 |
| BMI, kg/m2 | 28.2 ±0.2 | 26.5 ±0.2 | 29.6 ±0.3 | 29.3 ±0.3 | 25.2 ±0.4 | < .001 | < .001 | .424 |
| Physical activityg | 4.0 ±0.0 | 4.1 ±0.1 | 4.0 ±0.1 | 4.0 ±0.1 | 4.4 ±0.2 | .281 | .830 | .367 |
| Alcohol useh | 13.9 ±0.8 | 17.2 ±1.4 | 14.1 ±1.4 | 9.5 ±0.9 | 10.1 ±2.2 | .101 | < .001 | .004 |
| Smoking status | ||||||||
| Current | 25 | 26 | 31 | 18 | 19 | < .001 | < .001 | < .001 |
| Former | 20 | 26 | 18 | 16 | 16 | |||
| Never | 55 | 49 | 51 | 66 | 66 | |||
| Diabetesi | 7 | 4 | 10 | 8 | 8 | < .001 | .004 | .193 |
| Everyday discrimination experiencesj | 3.7 ±0.1 | 3.3 ±0.2 | 4.7 ±0.1 | 2.9 ±0.2 | 3.4 ±0.4 | < .001 | .088 | < .001 |
| Major discrimination experiencesk | 1.7 ±0.1 | 1.0 ±0.1 | 2.8 ±0.1 | 1.3 ±0.1 | 1.4 ±0.3 | < .001 | .008 | < .001 |
Note. BMI = body mass index. Results reported are percentages unless otherwise indicated. Standard errors are reported because standard deviations are not available with multiply imputed data. Results are weighted to account for complex survey design. Columns within a categorical variable sum to 100% (with some error caused by rounding).
Test for difference between non-Hispanic Black and non-Hispanic White.
Test for difference between Hispanic and non-Hispanic White.
Test for difference between Hispanic and non-Hispanic Black.
Defined as systolic blood pressure ≥ 140 mm Hg, diastolic blood pressure ≥ 90, report of antihypertensive medication use in the past 12 mo, or report of being told by a physician that respondent had hypertension.
Range: 0 (never) to 4 (≥ once/wk).
Multiple of $10 000.
Range: 0 (in bed or chair or no exercise) to 4 (heavy exercise).
Average drinks/mo.
Report of being told by a physician that respondent had diabetes.
Range: 1 (≥ once/wk) to 5 (never).
Range; 0 to 4 affirmative answers.
Odds ratios (ORs) from logistic regression models for the race/ethnicity dummy variables, the vigilance scale, and interactions between race/ethnicity and vigilance are reported in Table 2 (the complete set of model coefficients are in Table B, available as a supplement to the online version of this article at http://www.ajph.org). Blacks and Hispanics had a higher likelihood of hypertension than Whites, after sequential adjustment for age, gender, and immigrant generation (model 1) and then income and education (model 2).
TABLE 2—
Odds Ratios of Hypertension for Race/Ethnicity, Vigilance, and the Interaction Between Race/Ethnicity and Vigilance: Chicago Community Adult Health Study, 2001–2003
| Variable | Model 1,a OR (95% CI) | Model 2,b OR (95% CI) | Model 3,b OR (95% CI) | Model 4,b OR (95% CI) | Model 5,c OR (95% CI) |
| Race/ethnicity | |||||
| Non-Hispanic White (Ref) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Non-Hispanic Black | 2.26 (1.74, 2.94) | 1.99 (1.50, 2.63) | 1.93 (1.45, 2.56) | 1.53 (1.09, 2.15) | 1.27 (0.89, 1.81) |
| Hispanic | 2.03 (1.42, 2.91) | 1.74 (1.19, 2.52) | 1.71 (1.17, 2.48) | 1.39 (0.90, 2.15) | 1.10 (0.71, 1.70) |
| Non-Hispanic other | 1.40 (0.68, 2.85) | 1.49 (0.72, 3.08) | 1.47 (0.71, 3.05) | 1.50 (0.66, 3.41) | 1.63 (0.69, 3.81) |
| Vigilance | 1.02 (0.99, 1.06) | 0.95 (0.87, 1.03) | 0.94 (0.86, 1.03) | ||
| Interactions | |||||
| Non-Hispanic Black * vigilance | 1.10 (1.00, 1.21) | 1.11 (1.00, 1.22) | |||
| Hispanic * vigilance | 1.11 (1.01, 1.23) | 1.12 (1.01, 1.24) | |||
| Non-Hispanic Other * vigilance | 1.00 (0.75, 1.35) | 0.99 (0.72, 1.35) | |||
| Partial effects of vigilanced | |||||
| Non-Hispanic White | 0.95 (0.87, 1.03) | 0.94 (0.86, 1.03) | |||
| Non-Hispanic Black | 1.04 (1.00, 1.09) | 1.04 (0.99, 1.09) | |||
| Hispanic | 1.05 (0.99, 1.12) | 1.06 (0.95, 1.13) |
Note. CI = confidence interval; OR = odds ratio. Results are weighted to account for complex survey design.
Included covariates age, gender, and immigrant generation.
Added income and education to covariates in model 1.
Added smoking, physical activity, alcohol use, body mass index, diabetes, everyday discrimination, and major discrimination to covariates in models 2 to 4.
Calculated after estimation as the product of the vigilance and interaction terms.
We examined the mediating role of vigilance in the association between race/ethnicity and hypertension prevalence in 3 models, as discussed in the literature.28 First, we examined the association between race/ethnicity and vigilance and found that, after adjustment for the covariates in model 2, Blacks reported higher levels of vigilance than did Whites (b = 1.51; 95% confidence interval [CI] = 1.18, 1.83). Hispanics did not differ from Whites in levels of vigilance (b = 0.92; 95% CI = 0.54, 1.31). Second, we examined the association between vigilance and hypertension prevalence and found that, after adjustment for the covariates in model 2 except race/ethnicity, vigilance was associated with a greater likelihood of hypertension (OR = 1.04; 95% CI = 1.00, 1.08). Third, we added vigilance to model 2 and examined whether the disparities in hypertension prevalence were attenuated (model 3). The race/ethnicity coefficients were nearly unchanged.
We then examined the modifying role of vigilance on the association between race/ethnicity and hypertension prevalence. In model 4, we estimated this association separately for each racial/ethnic group through the introduction of interaction terms. With these interaction terms, the race/ethnicity coefficients indicated the racial/ethnic disparities in hypertension prevalence, when vigilance was zero. Blacks still showed a greater likelihood of hypertension than Whites, but the difference in odds was smaller than in previous models. Hispanics no longer showed a greater likelihood of hypertension than Whites. The vigilance coefficient in model 4 indicated that Whites (the reference racial/ethnic category) did not show an association between vigilance and hypertension prevalence. Furthermore, as shown by the interaction terms, the association for both Blacks and Hispanics was positive and statistically significantly different from that of Whites. The product of the vigilance and interaction terms showed the race/ethnicity–specific associations between vigilance and hypertension prevalence (Table 2). Vigilance had a significant and positive association with hypertension prevalence among Blacks (OR = 1.04; 95% CI = 1.00, 1.09), meaning that a 1-point increase in vigilance was associated with a 4% increase in the odds of hypertension. This association was similar for Hispanics, but only reached marginal statistical significance (OR = 1.05; 95% CI = 0.99, 1.12). Vigilance was not significantly associated with hypertension prevalence for Whites (OR = 0.95; 95% CI = 0.87, 1.03).
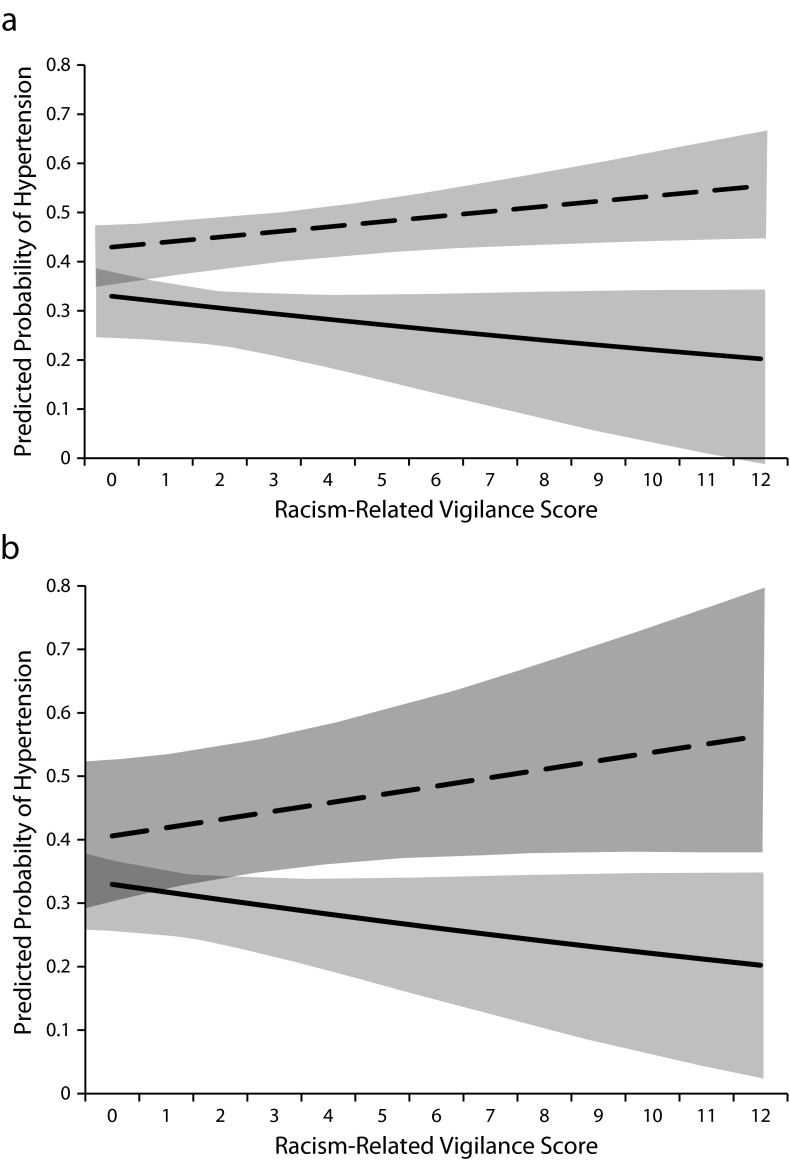
The significant interactions in model 4 between vigilance and both Black and Hispanic race/ethnicity suggest that Black–White and Hispanic–White disparities in hypertension varied significantly over levels of vigilance. These associations are seen more clearly in Figure 1, which shows plots of the predicted probabilities of hypertension prevalence for Blacks and Whites and Hispanics and Whites. As vigilance scores increased, the predicted probability of hypertension increased for Blacks and Hispanics but not Whites, which yielded an increased racial/ethnic disparity in hypertension prevalence.
FIGURE 1—
Association between racism-related vigilance score and predicted probability of hypertension prevalence for (a) non-Hispanic Black vs non-Hispanic White adults and (b) Hispanic vs non-Hispanic White adults: Chicago Community Adult Health Study, 2001–2003.
Note. Results weighted to account for complex survey design and adjusted for age, gender, immigrant generation, education, and annual household income. The dashed lines represent the association for (a) Blacks and (b) Hispanics. The solid lines represent the association for Whites. The shaded areas represent the 95% confidence interval.
After adjustment for hypertension risk factors and measures of discrimination (model 5), the racial/ethnic disparity in hypertension prevalence when vigilance was zero was attenuated for both Blacks and Hispanics and was no longer statistically significant for Blacks (OR = 1.27; 95% CI = 0.89, 1.81; Table 2). The other coefficients in the interaction did not change markedly with further adjustment of the hypertension risk factors. These results were nearly identical to a separate model that included the hypertension risk factors but did not include the discrimination measures (results not shown).
DISCUSSION
We examined the notion that a racially salient stressor contributes to racial/ethnic disparities in hypertension prevalence. Our results suggest that the stress of racism-related vigilance, with its anticipatory and perseverative qualities, is an important determinant of racial disparities in hypertension. We found that Blacks reported higher levels of vigilance than both Whites and Hispanics. Not only did they have the highest mean vigilance score, but they were also more likely to report weekly vigilance than were the other racial/ethnic groups. We found that vigilance was positively associated with hypertension prevalence for Blacks but not Whites. As vigilance increased, the Black–White disparity in hypertension prevalence also increased. Although not statistically significant, our results suggested similar experiences for Hispanics. Research has shown that racial bias and discrimination are embedded in numerous domains of US society that are relevant to health, ranging from education to employment to neighborhood quality to health care access and quality.29–33
Although bias and discrimination are pervasive, it is the certain threat of discrimination combined with the uncertainty of exactly which situations it will occur in that is likely driving vigilant behavior. Uncertainty is derived from at least 2 sources: first, bias and discrimination are not present in every situation, and second, the nature of modern discrimination is often subtle and ambiguous.34 The resulting heightened vigilance reflects the reality that one can never truly relax and must always be prepared for discrimination. For example, psychologists use the term racial microaggressions to describe
brief and commonplace daily verbal, behavioral, or environmental indignities, whether intentional or unintentional, that communicate hostile, derogatory, or negative racial slights and insults toward people of color.34(p271)
Moreover, psychologists have shown that uncertainty regarding a stressor results in vigilance about that stressor.35
Social scientists have documented that Blacks prepare themselves daily for bias and discrimination through such behaviors as the anticipation of discrimination and the negotiation of social spaces (e.g., avoiding certain places).27 The perseverative and anticipatory nature of vigilance sets it apart from traditional notions of perceived racial discrimination. For decades, a large scientific and lay literature has provided evidence of both the perseverative and anticipatory consequences of interpersonal and societal discrimination. In qualitative studies, social scientists often report on the way Blacks continually think about the potential for discrimination.36 It may be that racism-related vigilance is particularly toxic for Blacks because it reflects living with the threat of and preparation for discrimination in the daily negotiation of situations that are common features of life in a society (e.g., shopping, banking, employment). This constant vigilance can lead to wear and tear on bodily functions.37
Our measure of racism-related vigilance was based on results from ethnographic work in Black American samples, but our results suggest that similar mechanisms may operate for Hispanics as well. Although the mean vigilance score was lower for Hispanics than for Blacks, we observed a similar positive association between vigilance and hypertension. In a recent laboratory study of Hispanic women, researchers reported greater cardiovascular reactivity in response to a stress test among participants who believed that they were working with others who held prejudiced views of non-White groups.22 The authors concluded that the anticipation of discrimination may be an important source of stress and that “vigilance for prejudice may be a contributing factor to racial/ethnic health disparities.”22(p1020)
Our results support the notion that racism-related vigilance is an important determinant of hypertension in Blacks (and perhaps Hispanics) through the continual activation of the biological stress response systems (e.g., autonomic and hypothalamic–pituitary–adrenal systems) characteristic of this type of anticipatory and perseverative stress. Researchers argue that repeated activation of the biological stress response systems results in their dysfunction, which some have termed allostatic load.38 The body’s inability to respond properly to further stress (acute or chronic, physical or psychological) results in the increased oxidative stress and inflammation that characterize numerous cardiovascular and cardiometabolic diseases.
We found that when vigilance is at its lowest level (zero), racial/ethnic disparities in hypertension were small—and were substantially attenuated after adjustment for hypertension risk factors. Yet, as vigilance increased, disparities increased and were not changed with adjustment for these risk factors. These results suggest that focusing only on conventional risk factors will not eliminate hypertension disparities. Furthermore, despite the focus on conventional risk factors, a recent report on Healthy People 2010 stated that, over the previous decade, racial/ethnic disparities had not changed for 69% of the Healthy People outcomes monitored and had actually increased for 15% of these outcomes.39 Our results support an argument that we need to think more broadly about the contexts that shape health disparities in hypertension.40 Indeed, a growing body of research indicates that the conditions in which individuals live and work have an enormous impact on health before they even make contact with the health care system. Therefore, efforts to reduce these disparities
will require expanding our focus beyond medical care and personal behaviors to the broader social and economic contexts that influence health, in part by enabling or constraining healthy behaviors.41(p10)
Limitations
Our sample was from a single city—Chicago—and although it was representative of the population of the city, future work is needed with other samples. Our data were also cross-sectional, so we could not determine the effect of vigilance on the risk of hypertension. Nonetheless, the data set was large and population based, and it was one of the only data sets available with objectively measured blood pressure and a measure of racism-related vigilance.
Although the Cronbach α for the vigilance measure was only marginally acceptable, this may be attributable to the scale's size: only 3 items. Furthermore, the low α provided for a conservative estimate of the association between vigilance and hypertension prevalence.
Conclusions
We carried out the first examination of racism-related vigilance and its role in hypertension disparities. We showed that racism-related vigilance is associated with hypertension, particularly for Blacks and perhaps for Hispanics, but not for Whites, and that this results in an increasing racial disparity in hypertension as vigilance increases. Our results compel those who seek to eliminate racial and ethnic health disparities to move beyond traditional notions of individual-level risk factors for disease to the broader social determinants that drive racism-related vigilance.
Acknowledgments
The authors thank the Robert Wood Johnson Foundation Health and Society Scholars Program for its financial support. This research was also supported with funding from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (R01HD050467 to J. S. H.).
Human Participant Protection
The University of Michigan institutional review board approved the original survey, and written informed consent was obtained from all survey participants.
References
- 1.Hertz RP, Unger AN, Cornell JA, Saunders E. Racial disparities in hypertension prevalence, awareness, and management. Arch Intern Med. 2005;165(18):2098–2104. doi: 10.1001/archinte.165.18.2098. [DOI] [PubMed] [Google Scholar]
- 2.Mensah GA, Mokdad AH, Ford ES, Greenlund KJ, Croft JB. State of disparities in cardiovascular health in the United States. Circulation. 2005;111(10):1233–1241. doi: 10.1161/01.CIR.0000158136.76824.04. [DOI] [PubMed] [Google Scholar]
- 3.Fuchs FD. Why do Black Americans have higher prevalence of hypertension? An enigma still unsolved. Hypertension. 2011;57(3):379–380. doi: 10.1161/HYPERTENSIONAHA.110.163196. [DOI] [PubMed] [Google Scholar]
- 4.National Center for Health Statistics. Health, United States, 2011: With Special Feature on Socioeconomic Status and Health. Hyattsville, MD: Department of Health and Human Services; 2012. [PubMed] [Google Scholar]
- 5.Writing Members. Lloyd-Jones D, Adams RJ, Brown TM et al. Heart disease and stroke statistics—2010 update: a report from the American Heart Association. Circulation. 2010;121(7):e46–e215. doi: 10.1161/CIRCULATIONAHA.109.192667. [DOI] [PubMed] [Google Scholar]
- 6.Wong MD, Shapiro MF, Boscardin WJ, Ettner SL. Contribution of major diseases to disparities in mortality. N Engl J Med. 2002;347(20):1585–1592. doi: 10.1056/NEJMsa012979. [DOI] [PubMed] [Google Scholar]
- 7.Waidmann T. Estimating the Cost of Racial and Ethnic Health Disparities. Washington, DC: Urban Institute; 2009. [Google Scholar]
- 8.Redmond N, Baer HJ, Hicks LS. Health behaviors and racial disparity in blood pressure control in the national health and nutrition examination survey. Hypertension. 2011;57(3):383–389. doi: 10.1161/HYPERTENSIONAHA.110.161950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Geronimus AT, Bound J, Keene D, Hicken M. Black-White differences in age trajectories of hypertension prevalence among adult women and men, 1999–2002. Ethn Dis. 2007;17(1):40–48. [PubMed] [Google Scholar]
- 10.Dimsdale JE. Psychological stress and cardiovascular disease. J Am Coll Cardiol. 2008;51(13):1237–1246. doi: 10.1016/j.jacc.2007.12.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brosschot JF. Markers of chronic stress: prolonged physiological activation and (un)conscious perseverative cognition. Neurosci Biobehav Rev. 2010;35(1):46–50. doi: 10.1016/j.neubiorev.2010.01.004. [DOI] [PubMed] [Google Scholar]
- 12.Brosschot JF, Gerin W, Thayer JF. The perseverative cognition hypothesis: a review of worry, prolonged stress-related physiological activation, and health. J Psychosom Res. 2006;60(2):113–124. doi: 10.1016/j.jpsychores.2005.06.074. [DOI] [PubMed] [Google Scholar]
- 13.Sternthal MJ, Slopen N, Williams DR. Racial disparities in health: how much does stress really matter? Du Bois Rev. 2011;8(1):95–113. doi: 10.1017/S1742058X11000087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Williams DR, Neighbors HW, Jackson JS. Racial/ethnic discrimination and health: findings from community studies. Am J Public Health. 2003;93(2):200–208. doi: 10.2105/ajph.93.2.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Harrell CJ, Burford TI, Cage BN et al. Multiple pathways linking racism to health outcomes. Du Bois Rev. 2011;8(1):143–157. doi: 10.1017/S1742058X11000178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Phillips B, Mannino DM. Do insomnia complaints cause hypertension or cardiovascular disease? J Clin Sleep Med. 2007;3(5):489–494. [PMC free article] [PubMed] [Google Scholar]
- 17.Krieger N. Racial and gender discrimination: risk factors for high blood pressure? Soc Sci Med. 1990;30(12):1273–1281. doi: 10.1016/0277-9536(90)90307-e. [DOI] [PubMed] [Google Scholar]
- 18.Roberts CB, Vines AI, Kaufman JS, James SA. Cross-sectional association between perceived discrimination and hypertension in African-American men and women: the Pitt County Study. Am J Epidemiol. 2008;167(5):624–632. doi: 10.1093/aje/kwm334. [DOI] [PubMed] [Google Scholar]
- 19.Lindström M. Social capital, anticipated ethnic discrimination and self-reported psychological health: a population-based study. Soc Sci Med. 2008;66(1):1–13. doi: 10.1016/j.socscimed.2007.07.023. [DOI] [PubMed] [Google Scholar]
- 20.Mohseni M, Lindström M. Ethnic differences in anticipated discrimination, generalised trust in other people and self-rated health: a population-based study in Sweden. Ethn Health. 2008;13(5):417–434. doi: 10.1080/13557850802009603. [DOI] [PubMed] [Google Scholar]
- 21.Clark R, Benkert RA, Flack JM. Large arterial elasticity varies as a function of gender and racism—related vigilance in Black youth. J Adolesc Health. 2006;39(4):562–569. doi: 10.1016/j.jadohealth.2006.02.012. [DOI] [PubMed] [Google Scholar]
- 22.Sawyer PJ, Major B, Casad BJ, Townsend SS, Mendes WB. Discrimination and the stress response: psychological and physiological consequences of anticipating prejudice in interethnic interactions. Am J Public Health. 2012;102(5):1020–1026. doi: 10.2105/AJPH.2011.300620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Harrell SP. A multidimensional conceptualization of racism-related stress: implications for the well-being of people of color. Am J Orthopsychiatry. 2000;70(1):42–57. doi: 10.1037/h0087722. [DOI] [PubMed] [Google Scholar]
- 24.Schulz AJ, Kannan S, Dvonch JT et al. Social and physical environments and disparities in risk for cardiovascular disease: the Healthy Environments Partnership conceptual model. Environ Health Perspect. 2005;113(12):1817–1825. doi: 10.1289/ehp.7913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Turner JR. Understanding health disparities: the promise of the stress process model. In: Avison WR, editor. Advances in the Conceptualization of the Stress Process. New York, NY: Springer; 2009. pp. 3–21. [Google Scholar]
- 26.Essed P. Everyday Racism: Reports From Women of Two Cultures. 1st ed. Claremont, CA: Hunter House; 1990. [Google Scholar]
- 27.Feagin JR, Sikes MP. Living With Racism: The Black Middle-Class Experience. Boston, MA: Beacon Press; 1994. [Google Scholar]
- 28.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51(6):1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 29.Bertrand M, Mullainathan S. Are Emily and Greg more employable than Lakisha and Jamal? A field experiment on labor market discrimination. Am Econ Rev. 2004;94(4):991–1013. [Google Scholar]
- 30.Galster G. Racial steering by real estate agents: mechanisms and motives. Rev Black Polit Econ. 1990;19(1):39–63. [Google Scholar]
- 31.Williams DR, Jackson PB. Social sources of racial disparities in health—policies in societal domains, far removed from traditional health policy, can have decisive consequences for health. Health Aff. 2005;24(2):325–334. doi: 10.1377/hlthaff.24.2.325. [DOI] [PubMed] [Google Scholar]
- 32.Schulman KA, Berlin JA, Harless W et al. The effect of race and sex on physicians’ recommendations for cardiac catheterization. N Engl J Med. 1999;340(8):618–626. doi: 10.1056/NEJM199902253400806. [DOI] [PubMed] [Google Scholar]
- 33.Smedley BD, Stith AY, Nelson AR Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care (with CD) Washington, DC: National Academies Press; 2003. [PubMed] [Google Scholar]
- 34.Sue DW, Capodilupo CM, Torino GC et al. Racial microaggressions in everyday life: implications for clinical practice. Am Psychol. 2007;62(4):271–286. doi: 10.1037/0003-066X.62.4.271. [DOI] [PubMed] [Google Scholar]
- 35.Cappuccio FP, D’Elia L, Strazzullo P, Miller MA. Sleep duration and all-cause mortality: a systematic review and meta-analysis of prospective studies. Sleep. 2010;33(5):585–592. doi: 10.1093/sleep/33.5.585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Feagin JR. The continuing significance of race—anti-Black discrimination in public places. Am Sociol Rev. 1991;56(1):101–116. [Google Scholar]
- 37.Sapolsky RM. Social status and health in humans and other animals. Annu Rev Anthropol. 2004;33:393–418. [Google Scholar]
- 38.McEwen BS, Seeman TE. Protective and damaging effects of mediators of stress: elaborating and testing the concepts of allostasis and allostatic load. Ann N Y Acad Sci. 1999;896:30–47. doi: 10.1111/j.1749-6632.1999.tb08103.x. [DOI] [PubMed] [Google Scholar]
- 39.National Center for Health Statistics. Healthy People 2010 Final Review. Hyattsville, MD: Centers for Disease Control and Prevention; 2012. [Google Scholar]
- 40.Braveman PA, Egerter SA, Mockenhaupt RE. Broadening the focus: the need to address the social determinants of health. Am J Prev Med. 2011;40(suppl 1):S4–S18. doi: 10.1016/j.amepre.2010.10.002. [DOI] [PubMed] [Google Scholar]
- 41.Braveman PA, Kumanyika S, Fielding J et al. Health disparities and health equity: the issue is justice. Am J Public Health. 2011;101(suppl 1):S149–S155. doi: 10.2105/AJPH.2010.300062. [DOI] [PMC free article] [PubMed] [Google Scholar]