Abstract
We used a new conceptual framework that integrates tenets from health economics, social epidemiology, and health behavior to analyze the impact of socioeconomic forces on the temporal changes in the socioeconomic status (SES) gap in childhood overweight and obesity in China. In data from the China Health and Nutrition Survey for 1991 to 2006, we found increased prevalence of childhood overweight and obesity across all SES groups, but a greater increase among higher-SES children, especially after 1997, when income inequality dramatically increased. Our findings suggest that for China, the increasing SES gap in purchasing power for obesogenic goods, associated with rising income inequality, played a prominent role in the country’s increasing SES gap in childhood obesity and overweight.
It is well documented that family socioeconomic status (SES) is associated with childhood overweight and obesity1–3; however, the pathways linking SES with overweight and obesity may be strongly conditioned by a country’s stage of economic development. For example, an inverse relationship between SES and obesity is typically observed among children in developed countries,2,4 whereas in many developing countries, overweight and obesity are more common among socioeconomic elites.1,5,6 Several questions are unanswered: What contextual factors connect the stage of economic development with the sign and strength of the association between SES and childhood overweight and obesity? What is the relative importance of these factors? What happens when these contextual factors exert contradictory effects on risk for childhood obesity and overweight? The dramatic social and economic changes in China that took place after 1997 provided a unique opportunity to explore these questions.
Until now, the only study of the change in the SES–overweight and obesity association among Chinese children focused on the annual change in overweight prevalence by income.7 This study found that overweight prevalence increased fastest among high-income children between 1991 and 2004. To date, however, no study has thoroughly explored the contextual factors contributing to the changing relationship between SES and overweight and obesity in children and adolescents, in China or in any other developing country.
The direction of causality between SES and obesity for children is relatively easy to discern, because their SES is predetermined by that of their parents; hence, their obesity status is unlikely to affect their childhood SES.1 We developed a conceptual framework to address specific contextual factors that could shape the SES–childhood overweight and obesity relationship. We test several major tenets of this framework in data collected from 1991 to 2006 by the China Health and Nutrition Survey (CHNS).8
CONCEPTUAL FRAMEWORK
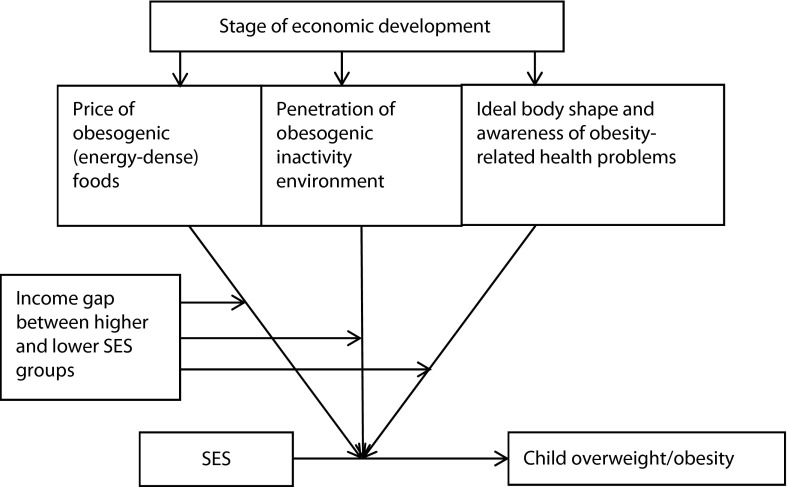
Previous literature on the SES–overweight and obesity relationship suggests that a country’s stage of economic development is key to understanding how this relationship is manifested among its children and adults.6,9,10 We derived a conceptual framework from this literature (Figure 1). The contextual factors we incorporated were (1) the price of energy-dense (obesogenic) foods, (2) the degree of penetration of obesogenic physical inactivity environments, and (3) general awareness of, and incentives to prevent, overweight and obesity. We also considered how income inequality interacted with these 3 factors to affect the magnitude of the SES gap.
FIGURE 1—
Framework for understanding childhood overweight and obesity.
Note. SES = socioeconomic status.
In highly developed countries, energy-dense foods are more widely accessible than are fruit and vegetables. This is largely attributable to the relatively low price of mass-produced dairy products, meat, and processed foods,11,12 made possible by economy-of-scale production, technological innovations in processing and storing foods, and government subsidies.13–15 For example, in the United States, the relative price of sweets and soft drinks decreased much more than the price of fresh vegetables and fruit between 1985 and 2000.11 Low-income people who cope with food insecurity by consuming more energy-dense foods because they are available at low prices have an increased risk of becoming overweight.12,16 In Brazil, a country whose gross national income per capita is among the highest in the developing world, studies found that food insecurity contributed to higher obesity rates among female adolescents and adults.17,18 However, when a country is in an early stage of development, general population access to energy-dense foods tends to be low, because these foods are much more expensive than vegetables, grains, and meals made at home from simple ingredients.19–22 Food scarcity among the poor, when coupled with the greater capacity of higher-SES groups to purchase energy-dense foods, might significantly contribute to a positive association between SES and overweight.21
Income inequality can also shape the SES–overweight and obesity profile by interacting with the price of energy-dense diets to influence societal patterns of body weight. If per capita gross national product is held constant, when the price of energy-dense foods is high, higher income inequality should predict a larger gap between higher-and lower-SES groups in access to expensive foods. Moreover, if the general population lacks knowledge of the health consequences of overweight and obesity, the growing advantage in purchasing power among the high-SES group can more easily be converted into a consumption gap, which, in turn, can lead to an increasing SES gap in overweight and obesity. Consistent with this formulation, Subramanian et al., in a study in India, found that great income inequality was associated with both overconsumption among privileged groups and food insecurity among the poor.22 Another study found that in developing countries with great income inequality, overweight increased more rapidly among the wealthy than among the poor, whereas in developing countries with less income inequality, overweight and obesity increased more among lower-income individuals.6
Obesogenic physical inactivity environments discourage or restrict activities requiring high expenditures of energy.23 The penetration of obesogenic environments is highly correlated with a country’s level of urbanization, transportation infrastructure, and rate of acquisition of new technologies.24 When a country is in the early stages of urbanization, only urban, higher-SES groups are able to take full advantage of the new transportation infrastructure and other labor-saving devices. The resulting reduced daily physical activity puts them at greater risk than the poor of becoming overweight.6
Many underdeveloped countries have a cultural norm that favors larger body sizes.10,21,25 Knowledge about the health risks associated with overweight and obesity have been slow to reach many developing countries,26,27 but those at more advanced stages of development appear to benefit from well-designed intervention programs that increase health-related knowledge and promote widespread changes in the physical activity and food environments.28–32 Brazil has used mass media to deliver public health messages designed to combat sedentary lifestyles and promote better eating habits,17 but such large-scale interventions have yet to be implemented in countries at earlier stages of development, such as China. Phelan et al. plausibly argue that the widespread and persistent inverse SES–health gradient in developed societies results, in part, from the higher-SES groups’ greater access to health-related knowledge33; however, the inclination of affluent families in developing countries to indulge children’s natural preference for sweet and fatty foods34 could render anti-obesity educational efforts, if unaccompanied by other strategies, ineffective.35 Thus, whether SES-related parental advantages in health knowledge lead to anti-obesity health behaviors in children in developing countries is an open question.
CONTRADICTORY INFLUENCES
In economically advanced societies, such as the United States, the greater health knowledge and access to healthy food and physical activity environments among higher-SES groups undoubtedly explains much of the well-known inverse association between SES and overweight and obesity.12,23 Under these conditions, it is difficult to determine the relative importance of willpower derived from knowledge and access to healthy food and physical activity environments in shaping risk for overweight and obesity. By contrast, when a country is in an early stage of economic development, only higher-SES groups have easy access to sedentary lifestyles and expensive, highly processed foods, the primary risk factors for becoming obese or overweight. Thus, for a limited time, the poor are largely protected from becoming overweight or obese, and they do not have to take special preventive actions to remain thin. During this early, transitional phase of economic development, the higher-SES groups' greater health-related knowledge and access to obesogenic goods and environment could exert contradictory influences on risk for overweight and obesity.
The Ecological Obesity Framework23 posits that willpower arising from knowledge may have only a minor effect on obesity-related health behaviors, relative to environmental influences. The set point of an individual's body fat is determined not only by energy intake and expenditure, but also by physiological adjustment—mechanisms to maintain a constant volume of body fat.23 Only after an individual is exposed to a change of environment for a sufficient time will this set point change in response.23 This framework treats obesity as a normal response to an abnormal environment, rather than a personal disorder requiring treatment.23 It posits that individual-level approaches have only limited efficacy and that understanding, measuring, and altering the obesogenic environment is critical to success.23 From this perspective, the power of knowledge alone to influence body weight may have only limited impact on social patterns of overweight and obesity in a given society.
CHINA
With the newly developed framework as a guide, we explored how the SES–childhood overweight and obesity gap in China changed over time in response to changes in selected contextual factors. Along with rapid economic growth, China experienced a declining relative price of energy-dense foods (except for oil and dairy products, which remained more expensive),19,20 the spread of Western ideals of body shape,27 and increasing penetration of obesogenic physical inactivity environments with urbanization and adoption of labor-saving devices.
Since 1997, China has experienced a sharp increase in income inequality as a result of the deepening of market reforms, especially in urban areas. These reforms have featured large-scale privatization of state-owned enterprises, massive layoffs of urban workers, dismantling of the Mao-era social welfare system, restructuring of the banking system, and, in preparation for China’s entry into the World Trade Organization in 2001, reduction of tariffs, trade barriers, and regulations.36–43 These reforms triggered rapid growth in earnings for the better educated, widening urban–rural income disparity,43 and advantages for administrative and political elites in managerial positions in various levels of government.37 After fluctuating between 0.35 in 1991 and 0.37 in 1997, the Gini coefficient, a widely used measure of income inequality, increased from 0.38 in 1998 to 0.44 in 2004, where it stayed through 2006.38 These figures may underestimate the true magnitude of income inequality in China because they do not account for grey income, the fraction of income that is unreported and is primarily acquired by high-income groups.44
During this same period, physical activity in higher-SES families declined with urbanization, increased access to television and video games,14,45 and increased use of motorized vehicles to transport adults to work and children to school.46 Collectively, these developments made China an ideal setting to examine how the contextual factors outlined in Figure 1 affect the changing association between SES and childhood obesity and overweight.
The declining cost of energy-dense foods,19,20 the spread of obesity-related health knowledge, and the idealization of the Western body shape among higher-SES groups27 suggest that the SES–obesity gap should narrow over time. However, increasing income disparity and the subsequent gaps in purchasing power, along with the relatively high price of energy-dense foods and labor-saving devices, augur a widening of the SES–obesity gap over time. According to the Ecological Obesity Framework,23 purchasing power is the most important constraint on access to obesogenic goods and environment, and because this constraint was relaxed for higher-SES groups after 1997, the positive SES gap of childhood overweight and obesity in China should have increased after 1997 when income inequality in China accelerated.
METHODS
To test our research questions, we used data from the 1991, 1993, 1997, 2000, 2002, 2004, and 2006 waves of the CHNS. This survey uses a multistage, random-cluster process to create samples in 9 provinces that vary substantially in geography, economic development, public resources, and health indicators. Details on the survey methods are available elsewhere.47 Like many longitudinal data sets, CHNS data are vulnerable to attrition. Our analyses showed that, conditional on the set of observed variables, overweight status in the previous wave was not related to attrition status, indicating that attrition was conditionally at random (Appendix A, available as a supplement to this article at http://www.ajph.org). After listwise deletion of all the missing data, our analytic sample comprised 10 186 children and adolescents, aged 2 to 18 years.
Measurement
The dependent variable was childhood overweight and obesity, a binary variable (1 = overweight and obesity; 0 = other) derived from weight and height measured by trained survey team members. We defined childhood overweight and obesity according to a composite scale derived from the Working Group of Obesity in China reference48 and the International Obesity Task Force reference.49 For children and adolescents aged 7 to 18 years, we used the Chinese body mass index (BMI; defined as weight in kilograms divided by the square of height in meters) cutoff. For children aged 2 to 6 years, we used the international BMI categories, because the Chinese reference did not encompass the younger ages. The international reference defines overweight according to data from 6 countries or regions, including Singapore and Hong Kong. The Chinese reference is derived from data on Chinese children and adolescents. Previous studies50,51 indicated that the Chinese reference is the most relevant for detecting metabolic syndrome among Chinese children and adolescents.
Independent variables were gender (1 = boy; 0 = girl); age; survey period (1 = after 1997; 0 = 1997 or earlier); residence (1 = urban; 0 = rural); daily energy, fat, and protein intake; active commuting; per capita household income (adjusted according to the 2006 Consumer Price Index); parental education (1 = ≥ high school; 0 = < high school); parental political elite status, defined as a political official or manager in the state-owned economic sector (1 = political elite; 0 = other); and parental height. We obtained parental variables from the linked data of parents. Wave 2000 and beyond represented the period when market reforms intensified.
The survey measured children's and adolescents' eating behavior and physical activity with a set of questions responded to by children or adolescents themselves if they were aged 10 years or older. Parents assisted with younger children. The CHNS research team constructed several measures of energy intake derived from eating behavior responses. More information on the measurement of nutrition intake in the CHNS is provided in Appendix B (available as a supplement to this article at http://www.ajph.org). Daily intake of energy (in kilocalories), fat (in grams), and protein (in grams) were all 3-day averages. Because the majority of respondents lacked a direct measure of energy expenditure, and because commuting to school has been identified as an important indicator of energy expenditure in China,52,53 we used mode of commuting to school (by foot, bike, bus, or car) as a proxy for energy expenditure. We defined active commuting as traveling by foot or bike and nonactive commuting as traveling by bus or car. We measured obesity-related health knowledge by the following questions, asked of anyone aged 12 years or older in the household: “Do you agree that lots of fruits/vegetables are better?” “Do you agree that lots of sugar is better?” “Do you agree that a diet high in fat is better?” “Do you agree that lots of staple food is better?” “Do you agree that lots of animal foods are better?” “Do you agree that being heavier is better?” Responses to these questions were “strongly disagree,” “disagree,” “neutral,” “agree,” “strongly agree,” and “don’t know.”
Statistical Analysis
We first calculated the prevalence of childhood overweight and obesity for higher- and lower-SES groups defined by parental education, parental political elite status, per capita family income, and residence type from 1991 to 2006. We age-adjusted childhood prevalence with the 2000 census age distribution. To identify SES gaps in childhood overweight and obesity and changes in these gaps before and after 1997, we used generalized estimating equations (GEEs), with controls for children's demographic characteristics, parental height, and province fixed effects. We adjusted for province fixed effects with province-specific dummies to mitigate unobserved heterogeneity among provinces that could affect correlations between SES and childhood overweight and obesity.
We used GEE models because the time-varying error terms within each unit (child) were correlated, violating the independence assumptions of traditional regression procedures. GEE estimators adjusted for the correlation among repeated measures. The advantage of this approach is that, under the assumption of missing at random and with a number of clusters (number of repeated individuals in this case) larger than 40, it provides consistent parameter estimation even if the correlation structure is misspecified.54 We treated the correlation structure as unstructured. Because the outcome variable was binary, we used the logistic specification of the GEE model.
RESULTS
Appendix C (available as a supplement to this article at http://www.ajph.org) presents variable means by survey year. The prevalence of childhood overweight and obesity increased from 8.2% in 1991 to 18.3% in 2006. The fraction of boys also increased, probably because of a strong son preference among Chinese parents and an increasing gender imbalance in births. This imbalance could be attributable to selective abortion of female fetuses, underreporting of female births,55–57 and higher attrition among girls (Appendix A, available as an online supplement).
Socioeconomic Status Trends for Childhood Overweight and Obesity
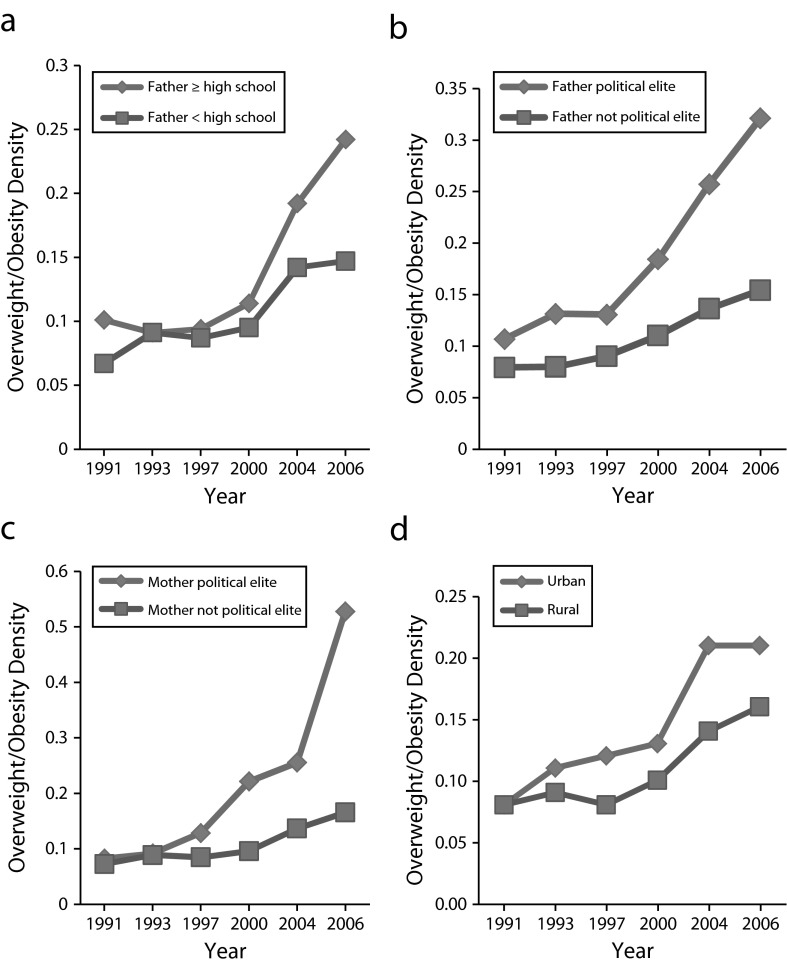
As shown in Figure 2, the prevalence of overweight and obesity increased among all groups between 1991 and 2006, but the rate of increase was greater among higher-SES groups (i.e., children of more educated fathers, children of members of the political elite, and children living in urban areas) than lower-SES groups. This was especially true after 1997, resulting in a widening gap in overweight and obesity by SES. These increased gaps were also in line with the rapid increase in the income gap by SES (Figure 3). Before 1997, the income gap for each indicator was relatively small, but after 1997 the gap increased dramatically.
FIGURE 2—
Trend of overweight and obesity density among children and adolescents aged 2 to 18 years by (a) father’s education attainment, (b) father’s political elite status, (c) mother’s political elite status, and (d) urban or rural residence: China Health and Nutrition Survey, 1991–2006.
FIGURE 3—
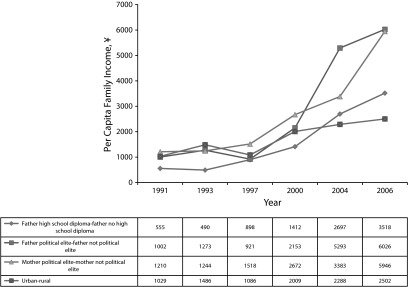
Mean difference in per capita family income for children and adolescents aged 2 to 18 years between higher and lower socioeconomic groups: China Health and Nutrition Survey, 1991–2006.
Note. Family income adjusted according to the Consumer Price Index.
To identify the most robust socioeconomic predictors of childhood overweight and obesity and the magnitude of the increased SES gap after 1997, we estimated a set of GEE models. In model 1 (Table 1), we only controlled for children’s age, gender, parental height, logged per capita family income, post-1997 period, parents’ highest degree and political elite status, urban or rural residence, and province fixed effects. As expected, logged per capita family income was positively associated with risk of overweight and obesity. Being an urban resident increased the risk of becoming overweight or obese; risk of overweight and obesity also increased after 1997.
TABLE 1—
Unstandardized Coefficients of Childhood Overweight or Obesity From Generalized Estimating Equation Models: China Health and Nutrition Survey 1991–2006
| Children and Adolescents Aged 2–18 Years |
Children and Adolescents Aged 6–18 Years |
Children and Adolescents Aged 6–18 Years in 1997, 2000, 2004, 2006a
|
|||||
| Variable | Model 1, b (95% CI) | Model 2, b (95% CI) | Model 3, b (95% CI) | Model 4, b (95% CI) | Model 5, b (95% CI) | Model 6, b (95% CI) | Model 7, b (95% CI) |
| Boys | 0.07 (−0.07, 0.21) | 0.08 (−0.06, 0.21) | 0.09 (−0.06, 0.23) | 0.20* (0.03, 0.38) | 0.19* (0.01, 0.37) | 0.29* (0.001, 0.57) | 0.25* (0.001, 0.51) |
| Logged per capita family income | 0.08* (0.004, 0.16) | 0.08* (0.002, 0.16) | 0.08b (−0.003, 0.16) | 0.12* (0.02, 0.22) | 0.12* (0.02, 0.22) | 0.03* (0.01, 0.06) | 0.03* (0.02, 0.03) |
| Father's education ≥ high school | 0.03 (−0.14, 0.20) | –0.11 (−0.32, 0.10) | –0.13 (−0.34, 0.09) | –0.0549 (−0.28, 0.18) | -0.05 (−0.33, 0.23) | -0.20 (−0.60, 0.21) | -0.20 (−0.68, 0.28) |
| Mother's education ≥ high school | 0.08 (−0.12, 0.28) | 0.07 (−0.16, 0.30) | 0.06 (−0.18, 0.30) | 0.01 (−0.30, 0.31) | 0.05 (−0.27, 0.37) | 0.18 (−0.08, 0.43) | 0.41 (−0.09, 0.90) |
| Urban residence | 0.28** (0.12, 0.45) | 0.25** (0.07, 0.44) | 0.22** (0.08, 0.37) | 0.36* (0.13, 0.60) | 0.34* (0.09, 0.59) | 0.34* (0.04, 0.65) | 0.32b (−0.03, 0.68) |
| Father member of political elite | 0.19 (−0.09, 0.47) | 0.17 (−0.16, 0.50) | 0.16 (−0.19, 0.51) | 0.16 (−0.22, 0.54) | 0.14 (−0.27, 0.54) | 0.36 (−0.27, 1.01) | 0.38 (−0.26, 1.02) |
| Mother member of political elite | 0.02 (−0.50, 0.53) | 0.10 (−0.61, 0.80) | 0.21 (−0.50, 0.91) | -0.50 (−1.45, 0.46) | 0.05 (−0.35, 0.45) | −1.36 (−3.41, 0.67) | −1.36 (−3.42, 0.68) |
| After 1997 market reforms | 0.37** (0.20, 0.50) | 0.20b (−0.004, 0.41) | 0.15* (0.04, 0.27) | 0.23* (0.005, 0.40) | 0.22* (0.02, 0.41) | 0.17 (−0.04, 0.39) | 0.08 (−0.25, 0.41) |
| Father's education ≥ high school × after 1997 | 0.46** (0.09, 0.82) | 0.42* (0.12, 0.73) | 0.47* (0.04, 0.89) | 0.43b (−0.01, 0.87) | 0.44b (0.03, 0.84) | 0.42 (−0.14, 0.99) | |
| Mother's education ≥ high school × after 1997 | –0.05 (−0.44, 0.34) | –0.07 (−0.48, 0.34) | –0.00 (−0.46, 0.45) | –0.08 (−0.56, 0.39) | –0.42 (−1.02, 0.18) | –0.40 (−1.00, 0.20) | |
| Urban residence × after 1997 | 0.09 (−0.24, 0.41) | –0.03 (−0.37, 0.31) | –0.02 (−0.38, 0.35) | –0.07 (−0.45, 0.32) | –0.05 (−0.59, 0.48) | –0.10 (−0.61, 0.41) | |
| Father member of political elite × after 1997 | 0.08 (−0.53, 0.69) | 0.04 (−0.61, 0.69) | 0.14 (−0.51, 0.79) | 0.11 (−0.58, 0.80) | 0.08 (−0.76, 0.91) | 0.07 (−0.78, 0.91) | |
| Mother member of political elite × after 1997 | -0.19 (−1.21, 0.83) | -0.38 (−1.43, 0.68) | 0.12 (−1.16, 1.40) | -0.14 (−1.47, 1.18) | -0.14 (−1.27, 0.99) | -0.12 (−1.05, 0.81) | |
| Energy intake, kcal | 0.0002** (0.00012, 0.00028) | 0.0002** (0.00013, 0.00026) | 0.0002** (0.0000065, 0.0004) | 0.0002* (0.0000084, 0.0004) | |||
| Active commuting | –0.38b (−0.81, 0.06) | ||||||
| Model statistics | |||||||
| Observations, No. | 10 186 | 10 186 | 10 186 | 8053 | 8053 | 3414 | 3414 |
| Children, No. | 5295 | 5295 | 5295 | 4740 | 4740 | 2482 | 2482 |
| Wald χ2 | 487.75 | 497.31 | 508.01 | 356.61 | 369.93 | 182.67 | 187.30 |
Note. CI = confidence interval. The generalized estimating equation model was specified as 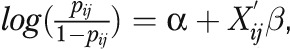 where
where  was the probability of overweight or obesity for individual i at time j, and
was the probability of overweight or obesity for individual i at time j, and was a vector of covariates incorporating all the explanatory variables and child’s age, parental height, and province fixed effects, which were controlled in all the models; b was a vector of coefficients representing the log odds of overweight or obesity. We treated the correlation structure as unstructured.
was a vector of covariates incorporating all the explanatory variables and child’s age, parental height, and province fixed effects, which were controlled in all the models; b was a vector of coefficients representing the log odds of overweight or obesity. We treated the correlation structure as unstructured.
Because information on commuting pattern was collected only for children and adolescents aged 6–18 years surveyed in waves 1997, 2000, 2004 and 2006, model 6 and model 7 incorporated data from these 4 waves.
Estimate approached significance at P < .1.
*P < .05; **P < .01.
In model 2, we added the interaction terms of the socioeconomic indicators with the post-1997 period. Compared with 1997 and earlier, having a father with a high school degree or more had a stronger positive effect on the likelihood of being overweight or obese. In fact, the upper tail of the BMI distribution moved to the right after 1997 only for children whose fathers earned a high school diploma (Appendix D, available as a supplement to this article at http://www.ajph.org), confirming a pronounced effect of father’s education in elevating risk of overweight and obesity following the intensification of market reforms and the concomitant rise in income inequality.
Energy Intake and Expenditure
To identify proximate mechanisms contributing to the widening gap in childhood overweight and obesity by father’s education, we first examined trends in energy intake. Gaps in total daily energy, protein, and fat intake by father’s education increased, especially after 1997 (Appendix E, available as a supplement to this article at http://www.ajph.org). In model 3 (Table 1), control for energy intake reduced the coefficient and the significance level of father’s education by post-1997 period.
We next controlled for energy expenditure, for which commuting mode was the proxy. Because information on commuting was collected only for children and adolescents aged 6 to 18 years surveyed in waves 1997, 2000, 2004, and 2006, we first estimated models with and without controls for energy intake, separately for children and adolescents aged 6 to 18 years (Table 1, models 4 and 5). Except for gender differences in overweight and obesity among children and adolescents aged 6 to 18 years, we found a similar set of coefficients as in the models that incorporated children and adolescents aged 2 to 18 years. Boys were more likely to be overweight or obese in the older age group (6–18 years), consistent with findings by Hsu et al.58
We then restricted the sample to waves from 1997 onward with and without controls for commuting mode (Table 1, models 6 and 7). Active commuting by foot or bicycle reduced the risk of overweight and obesity among children and adolescents aged 6 to 18 years. Interestingly, for this subsample, after we controlled for active commuting mode, the interaction effect of father’s education and post-1997 period was no longer statistically significant.
Effects of Gender and Health Knowledge
Gender-specific analyses (Appendix F, available as a supplement to this article at http://www.ajph.org) revealed that the findings observed for the entire sample were mainly driven by data for boys. For boys, income was positively associated with overweight and obesity, after control for other covariates. For girls, income was no longer a risk factor. After 1997, the risk of being overweight or obese increased for boys but not for girls. The increase in the effect of father’s education level on overweight and obesity after 1997 was significant for boys, but only approached significance for girls. Energy intake did not explain the observed associations between the SES indicators and overweight and obesity.
We compared obesity-related health knowledge by SES and gender in CHNS 2004 and 2006 survey data, which included indicators of health knowledge for respondents aged 12 years and older. Results indicated that many adolescents understood diet concepts concerning obesity (Appendix G, available as a supplement to this article at http://www.ajph.org). We observed significant SES gaps: higher-SES groups were more likely to disagree or strongly disagree that “heavier is better,” “more high-fat food is good for your health,” and “more sugar is good for your health,” despite a larger increase in childhood overweight and obesity during 2004 and 2006 among the higher- than the lower-SES groups.
DISCUSSION
We developed a conceptual framework highlighting contextual factors that may underlie changes over time in the relationship between parental SES and childhood overweight and obesity in developing countries. We took advantage of social processes in China that were set in motion by the deepening of market reforms after 1997 to test several major tenets of the Ecological Obesity Framework.29 Our analysis of CHNS data from 1991 to 2006 revealed an increasing prevalence of overweight and obesity among children and adolescents across all socioeconomic groups, but with a faster acceleration among higher-SES groups. This led to an increasing SES gap in childhood overweight and obesity, especially after 1997. We also found a widening gap in per capita family income after 1997, a result of the intensification of market reforms. The resulting increasing SES income gap increased the purchasing power of high-SES families for obesogenic goods, which amplified their children’s risk for overweight and obesity despite those children’s documented greater obesity-related health knowledge. Although this general pattern held for both boys and girls, it only approached significance for girls. This modest gender difference could be attributable to the fact that girls are generally more attuned to information about healthy diets and lifestyles, a tendency that may be strengthened by the emerging family and societal norms of an extremely slim body ideal for girls, but not boys, in China.27
Overall, our results confirmed key tenets of the Ecological Obesity Framework23; namely, compared with environmental factors, willpower derived from knowledge has only minor effects on obesity-related health behaviors, at least for children and adolescents in post-1997 China. That the observed positive relationship between parental SES and childhood overweight and obesity in China may eventually become an inverse one, as economic development continues and as predicted by Phelan et al.’s fundamental social cause of diseases perspective,33 is a distinct possibility.
Indeed, such a shift in the SES–obesity relationship may already be under way in China, at least among adults. For example, Dearth-Wesley et al. found that between 1991 and 2004, the prevalence of overweight increased faster among low-income than high-income Chinese adults.7 These different trends for adults and children could stem from a shift in the control of children's and adolescents' food choices, from parents to their children. Children have a strong preference for sweet and fatty foods.59 One recent study concluded that in Chinese families, children could influence as much as 70% of their parents’ spending decisions, by contrast with just 40% in the United States.59
Our findings show that public policies are urgently needed to limit the availability of obesogenic foods and alter obesogenic environments to protect China’s youths from becoming overweight or obese. Such policies could include raising taxes on obesogenic foods. In addition, China’s Ministry of Education could take action to increase awareness among school-aged children of the health consequences of obesity and the benefits of regular exercise. Incorporation of regular physical activity into the school days of Chinese children would improve not only their body weight status but also their academic achievement.60 The Chinese government should also assist consumers to make wiser food choices by strengthening regulations on nutrition content labeling. Currently, the power of consumers in China to make informed food decisions is severely limited by inadequate labeling.61
A limitation of our study was that the survey data covered only 9 of China’s 34 provinces. The data were not representative of the poorest provinces or the richest, most urbanized regions. The inclusion of the richest and poorest areas could have strengthened the validity of the framework by exploiting the cross-sectional variation of stage of economic development to assess the relationship between SES and overweight and obesity.
Our study provides a useful framework to examine how contextual factors relating to a country’s stage of economic development can shape pathways through which SES affects childhood overweight and obesity. It also contributes to the literature on how income inequality affects population health by illuminating how income inequality interacts with other contextual factors to alter the relationship between SES and overweight and obesity. Our findings for children and adolescents in China may have important implications for understanding similar processes under way in other rapidly developing countries, which, like China, may be following paths to development that differ from those taken by today’s high-income countries.
Acknowledgments
We thank Amar Hamoudi, Elizabeth Frankenberg, Jacob Vigdor, and other participants in the Sanford Colloquium for suggestions and comments.
Human Participant Protection
This study was exempted by the Duke University institutional review board because we used secondhand data without personal identifiers.
References
- 1.Wang Y, Monteiro C, Popkin BM. Trends of obesity and underweight in older children and adolescents in the United States, Brazil, China, and Russia. Am J Clin Nutr. 2002;75(6):971–977. doi: 10.1093/ajcn/75.6.971. [DOI] [PubMed] [Google Scholar]
- 2.Bilaver LA. Socioeconomic Determinants of Childhood Obesity [dissertation] University of Chicago; 2010. [Google Scholar]
- 3.Murasko JE. Socioeconomic status, height, and obesity in children. Econ Hum Biol. 2009;7(3):376–386. doi: 10.1016/j.ehb.2009.04.004. [DOI] [PubMed] [Google Scholar]
- 4.Ball K, Crawford D. Socioeconomic status and weight change in adults: a review. Soc Sci Med. 2005;60(9):1987–2010. doi: 10.1016/j.socscimed.2004.08.056. [DOI] [PubMed] [Google Scholar]
- 5.Sobal J. Obesity and socioeconomic status: a framework for examining relationships between physical and social variables. Med Anthropol. 1991;13(3):231–247. doi: 10.1080/01459740.1991.9966050. [DOI] [PubMed] [Google Scholar]
- 6.Jones-Smith JC, Gordon-Larsen P, Siddiqi A, Popkin BM. Cross-national comparisons of time trends in overweight inequality by socioeconomic status among women using repeated cross-sectional surveys from 37 developing countries, 1989–2007. Am J Epidemiol. 2011;173(6):667–675. doi: 10.1093/aje/kwq428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dearth-Wesley T, Wang H, Popkin BM. Under- and overnutrition dynamics in Chinese children and adults (1991–2004) Eur J Clin Nutr. 2008;62(11):1302–1307. doi: 10.1038/sj.ejcn.1602853. [DOI] [PubMed] [Google Scholar]
- 8. China. National Institute of Nutrition and Food Hygiene. China Health and Nutrition Survey, 1989–2009 [computer file]. Chapel Hill, NC: Carolina Population Center, University of North Carolina, Chapel Hill, n.d.
- 9.Monteiro CA, Conde WL, Popkin BM. Is obesity replacing or adding to undernutrition? Evidence from different social classes in Brazil. Public Health Nutr. 2002;5(1A):105–112. doi: 10.1079/PHN2001281. [DOI] [PubMed] [Google Scholar]
- 10.McLaren L. Socioeconomic status and obesity. Epidemiol Rev. 2007;29(1):29–48. doi: 10.1093/epirev/mxm001. [DOI] [PubMed] [Google Scholar]
- 11.Putnam JJ, Allshouse JE. Washington, DC: US Department of Agriculture, Economic Research Service; 1999. Food Consumption, Prices, and Expenditures, 1970–97. Statistical bulletin 965. [Google Scholar]
- 12.Drewnowski A, Specter SE. Poverty and obesity: the role of energy density and energy costs. Am J Clin Nutr. 2004;79(1):6–16. doi: 10.1093/ajcn/79.1.6. [DOI] [PubMed] [Google Scholar]
- 13.Drewnowski A. Fat and sugar: an economic analysis. J Nutr. 2003;133(3):838S–840S. doi: 10.1093/jn/133.3.838S. [DOI] [PubMed] [Google Scholar]
- 14.Popkin BM. The nutrition transition and obesity in the developing world. J Nutr. 2001;131(3):871S–873S. doi: 10.1093/jn/131.3.871S. [DOI] [PubMed] [Google Scholar]
- 15.Ng SW, Popkin BM. Impacts of China’s edible oil pricing policy on nutrition. Soc Sci Med. 2008;66(2):414–426. doi: 10.1016/j.socscimed.2007.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Neumark-Sztainer D, Story M, Resnick MD, Blum RW. Correlates of inadequate fruit and vegetable consumption among adolescents. Prev Med. 1996;25(5):497–505. doi: 10.1006/pmed.1996.0082. [DOI] [PubMed] [Google Scholar]
- 17.Kac G, Velásquez-Melendez G, Schlüssel MM, Segall-Côrrea AM, Silva AA, Pérez-Escamilla R. Severe food insecurity is associated with obesity among Brazilian adolescent females. Public Health Nutr. 2012;15(10):1854–1860. doi: 10.1017/S1368980011003582. [DOI] [PubMed] [Google Scholar]
- 18.Velásquez-Melendez G, Schlüssel MM, Brito AS, Silva AA, Lopes-Filho JD, Kac G. Mild but not light or severe food insecurity is associated with obesity among Brazilian women. J Nutr. 2011;141(5):898–902. doi: 10.3945/jn.110.135046. [DOI] [PubMed] [Google Scholar]
- 19.Ge K, Zhai F, Yan H. The Dietary and Nutritional Status of the Chinese Population: 1992 National Nutrition Survey. (Children and Adolescents). Vol 2. Beijing, China: People’s Medical Publishing House; 1999. [Google Scholar]
- 20.Lu Y, Goldman D. The Effects of Relative Food Prices on Obesity—Evidence From China 1991–2006. Washington, DC: National Bureau of Economic Research; 2010. NBER working paper series 15720 [Google Scholar]
- 21.Monteiro CA, Moura EC, Conde WL, Popkin BM. Socioeconomic status and obesity in adult populations of developing countries: a review. Bull World Health Organ. 2004;82(12):940–946. [PMC free article] [PubMed] [Google Scholar]
- 22.Subramanian SV, Perkins JM, Khan KT. Do burdens of underweight and overweight coexist among lower socioeconomic groups in India? Am J Clin Nutr. 2009;90(2):369–376. doi: 10.3945/ajcn.2009.27487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Egger G, Swinburn B. An ecological approach to the obesity pandemic. BMJ. 1997;315:477–480. doi: 10.1136/bmj.315.7106.477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Monda KL, Gordon-Larsen P, Stevens J, Popkin BM. China’s transition: the effects of rapid social change on adult activity patterns and overweight. Soc Sci Med. 2007;64(4):858–870. doi: 10.1016/j.socscimed.2006.10.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Messer E. Small but healthy? Some cultural considerations. Hum Organ. 1989;48(1):39–52. [Google Scholar]
- 26.Cash TF, Pruzinsky T. Body Image: A Handbook of Theory, Research, and Clinical Practice. New York, NY: Guilford Press; 2002. [Google Scholar]
- 27.Luo Y, Parish WL, Laumann EO. A population-based study of body image concerns among urban Chinese adults. Body Image. 2005;2(4):333–345. doi: 10.1016/j.bodyim.2005.09.003. [DOI] [PubMed] [Google Scholar]
- 28.Brownell KD, Kaye FS. A school-based behavior modification, nutrition education, and physical activity program for obese children. Am J Clin Nutr. 1982;35(2):277–283. doi: 10.1093/ajcn/35.2.277. [DOI] [PubMed] [Google Scholar]
- 29.Burke V, Milligan RA, Thompson C et al. A controlled trial of health promotion programs in 11-year-olds using physical activity "enrichment" for higher risk children. J Pediatr. 1998;132(5):840–848. doi: 10.1016/s0022-3476(98)70315-4. [DOI] [PubMed] [Google Scholar]
- 30.Christakis G, Sajecki S, Hillman RW, Miller E, Blumenthal S, Archer M. Effect of a combined nutrition education and physical fitness program on the weight status of obese high school boys. Fed Proc. 1966;25(1):15–19. [PubMed] [Google Scholar]
- 31.Collipp PJ. An obesity program in public schools. Pediatr Ann. 1975;1:276–282. doi: 10.3928/0090-4481-19750501-07. [DOI] [PubMed] [Google Scholar]
- 32.Figueroa-Colon R, Franklin FA, Lee JY, Von Almen TK, Suskind RM. Feasibility of a clinic-based hypocaloric dietary intervention implemented in a school setting for obese children. Obes Res. 1996;4(5):419–429. doi: 10.1002/j.1550-8528.1996.tb00250.x. [DOI] [PubMed] [Google Scholar]
- 33.Phelan JC, Link BG, Diez-Roux A, Kawachi I, Levin B. Fundamental causes of social inequalities in mortality: a test of the theory. J Health Soc Behav. 2004;45(3):265–285. doi: 10.1177/002214650404500303. [DOI] [PubMed] [Google Scholar]
- 34.Popkin BM, Adair LS, Ng SW. Global nutrition transition and the pandemic of obesity in developing countries. Nutr Rev. 2012;70(1):3–21. doi: 10.1111/j.1753-4887.2011.00456.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bandura A. Health promotion by social cognitive means. Health Educ Behav. 2004;31(2):143–164. doi: 10.1177/1090198104263660. [DOI] [PubMed] [Google Scholar]
- 36.Meng X. Economic restructuring and income inequality in urban China. Rev Income Wealth. 2004;50(3):357–379. [Google Scholar]
- 37.Xing C, Li S. Residual wage inequality in urban china, 1995–2007. China Econ Rev. 2012;23(2):205–222. [Google Scholar]
- 38.Chen J, Dai D, Pu M, Hou W, Feng Q. The Trend of the Gini Coefficient of China. Manchester, UK: Brooks World Poverty Institute, University of Manchester; 2010. BWPI working paper series 109. [Google Scholar]
- 39.Nee V. A theory of market transition: from redistribution to markets in state socialism. Am Sociol Rev. 1989;54(5):663–681. [Google Scholar]
- 40.Zhou X. Economic transformation and income inequality in urban China: evidence from panel data. Am J Sociol. 2000;105(4):1135–1174. [Google Scholar]
- 41.Zhang J, Zhao Y, Park A, Song X. Economic returns to schooling in urban China, 1988 to 2001. J Comp Econ. 2005;33(4):730–752. [Google Scholar]
- 42.Li H. Economic transition and returns to education in China. Econ Educ Rev. 2003;22(3):317–328. [Google Scholar]
- 43.Zheng H, Li L. Elite exchange and in-group reproduction in urban China [in Chinese] Sociol Stud. 2009;6:65–86. [Google Scholar]
- 44.Wang X, Wing TW. The size and distribution of hidden household income in China. Asian Econ Pap. 2011;10(1):1–31. [Google Scholar]
- 45.Xie B, Chou CP, Spruijt-Metz D et al. Socio-demographic and economic correlates of overweight status in Chinese adolescents. Am J Health Behav. 2007;31(4):339–352. doi: 10.5555/ajhb.2007.31.4.339. [DOI] [PubMed] [Google Scholar]
- 46.Bell AC, Ge K, Popkin BM. The road to obesity or the path to prevention: motorized transportation and obesity in China. Obesity (Silver Spring) 2002;10(4):277–283. doi: 10.1038/oby.2002.38. [DOI] [PubMed] [Google Scholar]
- 47.Popkin BM, Du S, Zhai F, Zhang B. Cohort profile: the China Health and Nutrition Survey—monitoring and understanding socio-economic and health change in China, 1989–2011. Int J Epidemiol. 2010;39(6):1435–1440. doi: 10.1093/ije/dyp322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.China Obesity Task Force. Body mass index reference norm for screening overweight and obesity in Chinese children and adolescents [in Chinese] Zhonghua Liu Xing Bing Xue Za Zhi. 2004;25:97–102. [PubMed] [Google Scholar]
- 49.Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ. 2000;320(7244):1240–1243. doi: 10.1136/bmj.320.7244.1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ma GS, Li Y-P, Hu XQ, Cui ZH, Yang XG, Chen CM Report on childhood obesity in China (2) Verification of BMI classification reference for overweight and obesity in Chinese children and adolescents. Biomed Environ Sci. 2006;19(1):1–7. [PubMed] [Google Scholar]
- 51.Xu Y-Q, Ji C-Y. Report on childhood obesity in China (7). Comparison of NCHS and WGOC. Biomed Environ Sci. 2008;21(4):271–279. [Google Scholar]
- 52.Tudor-Locke C, Ainsworth BE, Adair LS, Du S, Lee N, Popkin BM. Cross-sectional comparison of physical activity and inactivity patterns in Chinese and Filipino youth. Child Care Health Dev. 2007;33(1):59–66. doi: 10.1111/j.1365-2214.2006.00612.x. [DOI] [PubMed] [Google Scholar]
- 53.Shi Z, Lien N, Kumar BN, Holmboe-Ottesen G. Socio-demographic differences in food habits and preferences of school adolescents in Jiangsu Province, China. Eur J Clin Nutr. 2005;59(12):1439–1448. doi: 10.1038/sj.ejcn.1602259. [DOI] [PubMed] [Google Scholar]
- 54.Zeger SL, Liang KY. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986;42(1):121–130. [PubMed] [Google Scholar]
- 55.Merli MG, Smith HL. Has the Chinese family planning policy been successful in changing fertility preferences? Demography. 2002;39(3):557–572. doi: 10.1353/dem.2002.0029. [DOI] [PubMed] [Google Scholar]
- 56.Hesketh T, Qi JD, Tomkins A. Health effects of family size: cross sectional survey in Chinese adolescents. Arch Dis Child. 2003;88(6):467–471. doi: 10.1136/adc.88.6.467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Hesketh T, Lu L, Xing ZW. The effect of China’s one-child family policy after 25 years. N Engl J Med. 2005;353(11):1171–1176. doi: 10.1056/NEJMhpr051833. [DOI] [PubMed] [Google Scholar]
- 58.Hsu YW, Johnson CA, Chou CP et al. Correlates of overweight status in Chinese youth: an East-West paradox. Am J Health Behav. 2011;35(4):496–506. doi: 10.5993/ajhb.35.4.11. [DOI] [PubMed] [Google Scholar]
- 59.McNeal JU, Wu S. Consumer choices are child’s play in China. Asian Wall St J Wkly. October 23, 1995:14. [Google Scholar]
- 60.Strong WB, Malina RM, Blimkie CJ et al. Evidence based physical activity for school-age youth. J Pediatr. 2005;146(6):732–737. doi: 10.1016/j.jpeds.2005.01.055. [DOI] [PubMed] [Google Scholar]
- 61.Tao Y, Li J, Lo YM, Tang Q, Wang Y. Food nutrition labeling practice in China. Public Health Nutr. 2010;14(3):542–550. doi: 10.1017/S1368980010002065. [DOI] [PubMed] [Google Scholar]