Abstract
PURPOSE:
To examine treatment trends and costs associated with Dupuytren’s disease (DD) in Canada.
METHODS:
Data regarding fasciectomies, fasciotomies and digit amputations performed for DD from 2005 to 2010 were extracted from the Canadian Institute for Health Information database. The data were analyzed according to year, sex and five-year age groups. The estimated annual physician reimbursement costs for DD in Ontario were calculated using Ontario Health Insurance Plan billing information and the 2010 Physician Schedule of Benefits.
RESULTS:
The number and rate of fasciectomies remained stable from 2005 to 2009 (mean of 4067 and 1.24 per 10,000, respectively), but increased in the 2009/2010 fiscal year (to 4458 and 1.32 per 10,000). The number of fasciotomies increased from 133 in 2005/2006 to 201 in 2008/2009, but dropped to 183 in 2009/2010. The mean number of amputations remained stable (12 procedures).The ratio of males to females undergoing fasciectomies remained stable (4:1). The highest rate of fasciectomies was performed for the age groups 65 to 69 years and 70 to 74 years. Estimated mean physician remuneration for DD in Ontario remained stable ($3.2 million per annum).
DISCUSSION:
The results regarding patient demographics are comparable with results from previous literature. There was a trend toward an increasing number of fasciectomies and fasciotomies annually, with fasciotomies increasing faster than fasciectomies, which is reflective of the aging population and the recent attention to fasciotomies in the literature. The present study was the first to investigate treatment trends and physician reimbursement costs for the management of DD in Canada.
Keywords: Canada, Dupuytren’s disease, Fasciectomy, Fasciotomy, Physician remuneration, Treatment trends
Abstract
OBJECTIF :
Examiner les tendances thérapeutiques et les coûts associés à la maladie de Dupuytren (MD) au Canada.
MÉTHODOLOGIE :
Les chercheurs ont extrait des bases de données de l’Institut canadien d’information sur la santé les données relatives aux fasciectomies, aux fasciotomies et aux amputations de doigts effectuées en raison de la MD entre 2005 et 2010. Ils ont analysé les données selon l’âge, le sexe et les groupes d’âge par tranches de cinq ans. Ils ont calculé les coûts estimatifs annuels du remboursement des médecins attribuables à la MD en Ontario, au moyen de l’information de facturation tirée du Régime d’assurance-maladie de l’Ontario et du barème des prestations des médecins pour 2010.
RÉSULTATS :
Le nombre et le taux de fasciectomies sont demeurés stables de 2005 à 2009 (moyenne de 4 067 et de 1,24 sur 10 000, respectivement), mais ont augmenté pendant l’exercice 2009–2010 (à 4 458 et 1,32 sur 10 000). Le nombre de fasciotomies est passé de 133 à 2005–2006 à 201 en 2008–2009, mais a reculé à 183 en 2009–2010. Le nombre moyen d’amputations est demeuré stable (12 interventions). Le ratio d’hommes qui ont subi une fasciectomie par rapport aux femmes est également demeuré stable (4:1). Le plus fort taux de fasciectomies s’observait dans les groupes de 65 à 69 ans et de 70 à 74 ans. Enfin, la rémunération estimative moyenne des médecins pour soigner la MD en Ontario est demeurée stable (3,2 millions de dollars par année).
EXPOSÉ :
Les résultats relatifs à la démographie des patients sont comparables à ceux des publications antérieures. On a constaté une tendance vers une augmentation annuelle du nombre de fasciectomies et de fasciotomies. L’augmentation des fasciotomies était plus marquée que celle des fasciectomies, ce qui reflète le vieillissement de la population et l’intérêt récent pour les fasciotomies dans les publications. La présente étude était la première à examiner les tendances en matière de traitement et les coûts du remboursement des médecins pour la prise en charge de la MD au Canada.
Dupuytren’s disease (DD) is a fibroproliferative disease of the palmar fascia that, through the formation of palmar nodules and fibrous cords, can lead to disabling flexion contractures of the fingers (1,2). DD has been reported to have a global prevalence of 3% (3,4), with the highest prevalence in Northern Europe (5,6). Prevalence increases with age, and males are more commonly affected than females (7,8). Up to 40% of men ≥70 years of age in parts of northern Europe are affected by DD (7,9). Currently, the gold standard of treatment for DD is surgical or open fasciectomy, although closed fasciotomy (also known as percutaneous needle fasciotomy or needle aponeurotomy), and collagenase enzymatic digestion of disease cords are being advocated as nonsurgical alternatives (10,11). Because of the high cost differential in these treatment methods, we were interested in documenting the treatment trends and health care expenditures associated with DD in Canada.
The current study provides an analysis of both inpatient and day-surgery treatment for DD, and includes a description of treatment trends. Unlike other countries, such as France and England, Canada does not have a system of assigning health care expenditures to a specific diagnosis-related group. Instead, it has a system of global funding that roughly assigns funding based on population. Attempts to estimate the costs of treatment for a specific disease in Canada are, therefore, significantly more difficult. We were, however, able to estimate the physician reimbursement costs in Ontario for the management of DD.
METHODS
The data analyzed in the present study were extracted from three sources: the Canadian Institute for Health Information (CIHI); Statistics Canada; and the Ontario Medical Association (OMA).
CIHI
CIHI is a not-for-profit corporation established in 1994 and funded by federal, provincial and territorial governments (12). Presently, it maintains 27 pan-Canada health-related databases. For the purpose of the present study, day surgery and inpatient data were extracted from three CIHI databases: the National Ambulatory Care Reporting System; the Discharge Abstract Database; and the Hospital Morbidity Database. Quebec and Alberta day surgery data were not available because Quebec does not submit day surgery data to CIHI and Alberta did not start submitting day surgery data until April 2010.
Data extraction was limited to 2005 and beyond to avoid inconsistencies in data classification because the transition of data classification systems to the current International Classification of Diseases, 10th Revision (ICD)-10-CA/Canadian Classification of Health Interventions (CCI) was not completed until 2005.
In consultation with multiple CIHI analysts, data extraction was refined to only include encounters with the DD diagnosis codes, which were then subdivided according to procedure type (fasciectomy, fasciotomy and digit amputation), sex and five-year age groups (from 45 to 85 years of age). The diagnosis codes used include M72.0 (palmar fascia fibromatosis [Dupuytren]), and M73.8 (DD associated with diabetes mellitus) from the ICD-10-CA. The procedure codes are based on the CCI and include 1.UY.72.WJ (fasciectomy), 1.UY.72.WK (fasciotomy) and 1.UJ.93.^^ (amputation, phalanx of hand).
The data extraction was independently programmed by two CIHI analysts and these data sets were compared before the final data were released in spreadsheet (Excel, Microsoft Corporation, USA) format.
OMA
As mentioned above, the nature of the global funding formula for health care in Canada makes it exceedingly difficult to estimate hospital costs for the treatment of DD; therefore, physician reimbursement costs were investigated instead. Because physician reimbursement mechanisms are different for each province, the analysis was limited to Ontario. It was believed that Ontario could provide an appropriate representation of trends in physician reimbursement costs because Ontario accounts for a significant proportion of the Canadian population. In the 2011 census of Canada, Ontario accounted for 36.3% of the population of the country, while in the 2006 census, it accounted for 40.7% of the total population (13).
Physician reimbursement costs for Ontario for 2005 to 2010 were calculated based on Ontario Health Insurance Plan (OHIP) physician billings associated with diagnosis code 728 for DD, obtained through the OMA Economics Department. Billings made by all physicians involved in the management of DD patients were included because the diagnosis of DD is often made in the primary care setting and managed conservatively without referral to a surgeon. The 2010 Ontario Ministry of Health and Long-Term Care Physician Schedule of Benefits (SOB) was used to apply the appropriate costs to the OHIP billing codes that were extracted. Because of fee schedule revisions, some codes used in earlier years were missing from the 2010 SOB. An Internet search revealed archived OHIP bulletins regarding changes to the SOB for some of the missing codes. The remuneration for other older billing codes could not be found and were excluded from further data analysis. Premium add-on codes that could be applied to multiple situations were also excluded from the analysis.
There were a significant number of unusual fee codes; therefore, an a priori decision was made to report only on the billing codes that were likely to be associated with DD. Every fee to be included in or excluded from the cost estimate was discussed with the senior author (BSG), an experienced plastic surgeon. Only 327 of the 1165 fee codes that initially extracted were included in the calculation for the estimate of the annual physician renumeration related to DD treatment.
Statistics Canada
Population demographics were obtained online through the Statistics Canada’s CANSIM database. Population tables were extracted according to province, five-year age groups (from 45 to 84 years) and sex in Canada from 2005 to 2010. The rate of fasciectomies performed was determined by dividing the number of procedures (reported by CIHI) by the Canadian population for that year and reported as per 10,000. Procedure rates were also calculated for each five-year age group.The data analysis was performed using Excel.
RESULTS
The reported number of fasciectomies performed appeared to remain relatively stable from 2005 to 2009, with 4062 procedures in the 2005/2006 fiscal year (April 1 to March 31) to 4097 procedures in 2008/2009. This increased to 4458 procedures in 2009/2010 (Figure 1). Similarly, the rate of fasciectomies remained stable from 2005 to 2009, with a rate of 1.26 per 10,000 people in 2005/2006 to 1.23 in 2008/2009, and increased in 2009/2010 to 1.32 (Figure 2). The number of fasciotomies increased from 133 in 2005/2006 to 201 in 2008/2009, but dropped slightly to 183 in 2009/2010 (Figure 1). The mean number of digit amputations remained relatively stable (12 procedures annually from 2005 to 2010) (Figure 1). The ratio of males to females receiving fasciectomies and fasciotomies remained stable at 4:1 from 2005 to 2010 (Figure 3). The highest number of fasciectomies was performed for the 60 to 64 and 65 to 69 years of age groups (Figure 4). When subdivided according to sex, it was observed that the age range for greatest number of procedures performed remained from 60 to 69 years of age for men, but for women it was from 65 to 74 years of age. The highest rates of fasciectomies performed were for the 65 to 69 and 70 to 74 years of age groups, with mean rates of 5.6 and 5.9 per 10,000 population, respectively (Figure 5).
Figure 1).
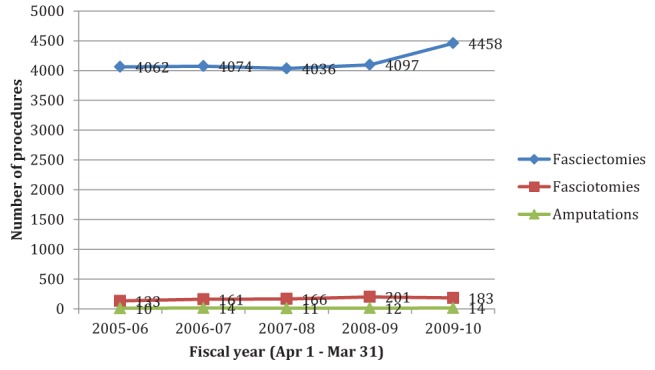
Fasciectomies performed for the treatment of Dupuytren’s disease in Canada remained relatively stable between 2005 and 2009 (from 4062 in 2005/2006 to 4097 in 2008/2009) and increased in 2009/2010 (to 4458). Fasciotomies increased from 133 in 2005/2006 to 201 in 2008/2009, dropping to 183 in 2009/2010. Digit amputations remained relatively stable during this time, with a mean of 12 procedures per fiscal year
Figure 2).
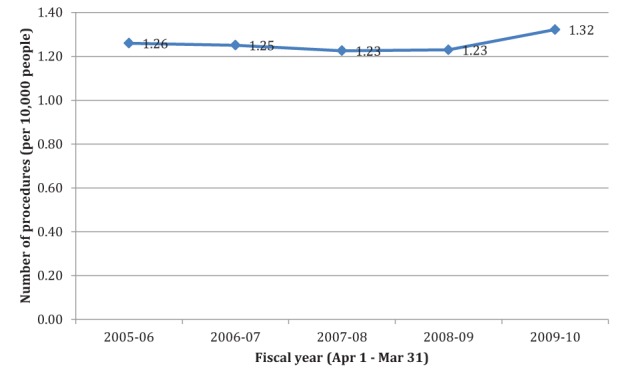
The rate of fasciectomies performed for the treatment of Dupuytren’s disease in Canada between 2005 and 2010 was determined by dividing the number of fasciectomies by the population for that year and reported per 10,000. The rate of fasciectomies remained relatively stable between 2005 and 2009 (from 1.26 procedures per 10,000 people in 2005/2006 to 1.23 per 10,000 in 2008/2009) and increased slightly in 2009/2010 (to 1.32 per 10,000)
Figure 3).
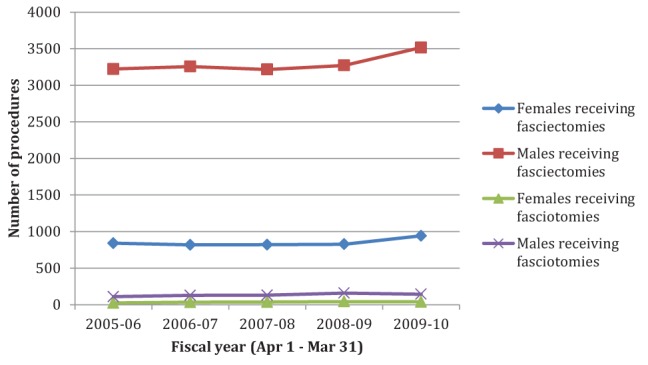
The ratio of males to females receiving fasciectomies and fasciotomies for the treatment of Dupuytren’s disease in Canada both remained relatively stable at 4:1 from 2005 to 2010
Figure 4).
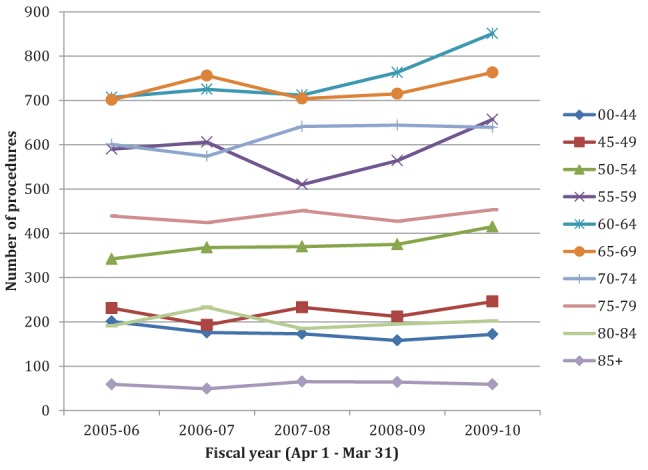
Age-related differences in the number of fasciectomy procedures performed for the treatment of Dupuytren’s disease in Canada from 2005 to 2010 were observed. The greatest numbers of procedures performed were for the 60 to 64 and 65 to 69 years of age groups
Figure 5).
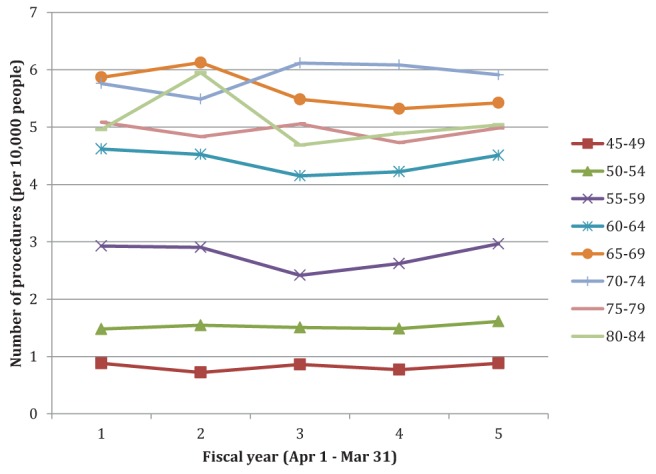
Age-related differences in the rate of fasciectomy procedures performed for the treatment of Dupuytren’s disease in Canada from 2005 to 2010 were observed. The rate of fasciectomies performed was determined by dividing the number of fasciectomies by the population for that year and reported per 10,000. The highest rates of fasciectomies performed were for the 65 to 69 and 70 to 74 years of age groups, with mean rates of 5.6 and 5.9 per 10,000
Annual physician reimbursement expenditures for the management of DD in Ontario appeared to remain stable, with a mean value of $3.2 million per annum from 2005 to 2010 (Figure 6).
Figure 6).
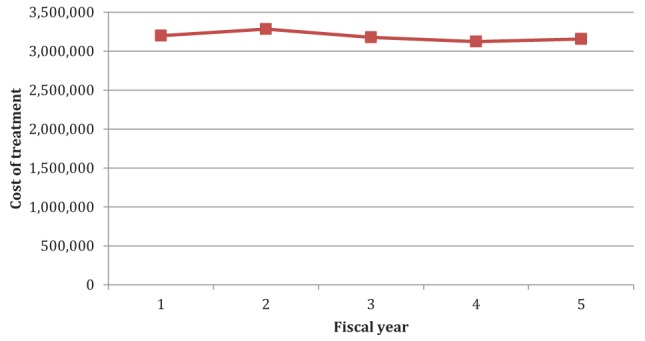
Cumulative annual physician remuneration for the management of Dupuytren’s disease in Ontario was calculated based on Ontario Health Insurance Plan billing information for 2005 to 2010 and the 2010 Ontario Schedule of Benefits. Physician reimbursement expenditures were calculated based on fee codes deemed appropriate for treatment of Dupuytren’s disease (ie, with excluded odd fee codes). Annual physician billings appeared to remain stable, with a mean value of $3.2 million
DISCUSSION
The present study is the first to report the costs and trends associated with treatment of DD in Canada. To our knowledge, only two studies have been published worldwide investigating trends and operative costs associated with the treatment of DD (14,15).
Many of our results were comparable with results from previous literature on DD from other countries. The 4:1 ratio of males to females undergoing fasciectomies and fasciotomies was the same as the ratio of males and females in the study by Gerber et al (15), which investigated patient demographics of individuals receiving surgery for DD in England from 2003 to 2008. Anthony et al (16) observed a 3:1 ratio of males to females diagnosed with DD receiving fasciectomies at two large centres in Boston (Massachusetts, USA) from January 1995 to July 2006. In 1955, Yost et al (17) surveyed patients at a large municipal hospital in Brooklyn (New York, USA) for DD, and also found the ratio of males to females diagnosed with DD to be 3:1.
The age-group and sex-related differences that we observed for the number of fasciectomies performed were also comparable with previous reports. In his review of the epidemiology of DD, Ross (8) noted that men presented for treatment for DD in their fifth decade, 10 years earlier than women. Our data reveal that the highest number of fasciectomies are performed in men 60 to 69 years of age and in women 64 to 74 years of age. We speculate that there may be a lag time between when patients first present to a physician and when they actually undergo surgical treatment. In their study population, Yost et al (17) observed that males had the highest incidence of DD at 66 years of age and females at 70 years of age.
Operative trends
Our results revealed a trend toward an increasing number of fasciectomies and fasciotomies annually, which is reflective of the aging population. Based on population demographics obtained from Statistics Canada, the fastest growing age category for 2005 to 2010 for the Canadian population is 60 to 64 years of age (18). We also observed the number of fasciotomies to be increasing at a faster rate than fasciectomies. This observation is reflective of our own experience at the Hand and Upper Limb Centre at St Joseph’s Health Centre, located in London, Ontario. We have been performing an increasing number of percutaneous needle fasciotomies over the past seven years at the request of our patients because they had heard about this procedure being performed in Europe and the United States (19). The most striking observation of our results was the low number of reported fasciotomies compared with fasciectomies. Whether this is due to under-reporting of fasciotomies, a discrepancy in coding or whether this procedure is simply not offered at other centres is unclear. Unfortunately, the databases that we used are not designed to extract such information.
Physician remuneration in Ontario
Physician remuneration for the management of DD in Ontario appeared to remain relatively stable between 2005 and 2010 despite the increase in fasciectomies performed nationwide. We speculate that this could be due to an increase in the cost effectiveness of the nonsurgical management of DD. The physician reimbursement expenditures we reported for the management of DD in Ontario are only a fraction of the actual health care expenditures for DD because our analysis does not include hospital costs of surgery or expenses from the utilization of allied health professional services such as physiotherapists.
In our calculation of the cost estimate for physician reimbursement expenditures, we applied the 2010 SOB to the billing codes from all five fiscal years (2005 to 2010). An alternative method would be to estimate physician reimbursement costs from billing codes for each year, using the corresponding SOB for that year, to account for changes in the value of each billing code and inflation. However, given that the estimate of physician reimbursement expenditures remained relatively stable from 2005 to 2010, we can extrapolate that the quantities of billings associated with the management of DD remained relatively stable overall and, thus, our method can give an appropriate approximation of costs.
Reliability of database information
CIHI data:
In studies such as these, it is always unclear how reliable the particular databases are. Overall, the accuracy of CIHI data is considered to be high. First, it uses a rigorous protocol and monitors the quality of its databases through annual internal analyses. Second, the accuracy of the CIHI databases have been validated for surveillance data in other areas of medicine. Lee et al (20) found the CIHI data to be highly accurate for common cardiac procedures in Ontario when compared with the Cardiac Care Network clinical registry (gold standard). Similarly, Joseph and Fahey (21) compared perinatal data in CIHI with the Nova Scotia Atlee Perinatal Database and found CIHI databases to have a relatively high degree of accuracy.
Limitations in CIHI data include missing day surgery data from Alberta and Quebec. As well, some institutions did not submit data to CIHI due to staff shortages; therefore, the numbers of procedures we reported may be an underestimate of actual values.
OMA/OHIP data:
With the significant number of discordant fee codes in the OHIP billing data provided by the OMA, we questioned the reliability of the data used to estimate physician reimbursement costs in Ontario. The unusual fee codes were likely a result of clerical errors in billing. We did our best to obtain a true estimate of physician reimbursement expenditures for the management of DD in Ontario by assessing the appropriateness of each billing code extracted. Only 327 of the 1165 original billing codes associated with the diagnosis for DD were included in the final cost estimates. A small percentage of the fee codes included may also have been errors in billing, but we cannot identify these erroneous codes unless we investigate the actual patient charts for which these fee codes were billed.
To further analyze the reliability of the data, we examined the number of R551 billings not associated with the diagnosis 728. As mentioned previously, R551 is the fee code for excision of fascia for DD and should be billed exclusively with 728; therefore, we expected to see few of these. Unexpectedly, there were >700 R551 billed without the DD diagnosis code annually from 2005 to 2010. In addition, we matched the number of fasciectomies, fasciotomies and digit amputations reported in CIHI for Ontario for 2005 to 2010 to the OMA/ OHIP data and found discordance between the two datasets. In general, OMA/OHIP reported more fasciectomies, and less fasciotomies and digit amputations compared with CIHI. This may be a result of coding differences, or physicians billing fasciotomies as fasciectomies through OHIP.
Although we concluded that the reliability of the OHIP data were questionable for our project, the OHIP database has been used extensively for other research, particularly for disease surveillance (for example, ischemic heart disease and nosocomial infections) as well as outcomes of drug therapy (particularly in older populations) (22–25). The OHIP database has also been validated. For example, Kwong and Manuel (26) compared OHIP physician claims for influenza vaccination against self-reported influenza immunization status by patients through responses to the Canadian Community Health Services Survey and found moderate agreement.
With any study involving database information, one needs to be cognizant of the reliability of the information and accept that some percentage of the data may be due to erroneous input. In particular, the unusual fee codes we encountered in our assessment of physician reimbursement expenditures for the management of DD stress the importance of careful input of billing and diagnosis codes at the level of the individual physician and his/her assistant.
CONCLUSION
At the time the present study was conducted, limited data regarding costs of treatment were available given the lack of national databases with this information, and the lack of a national schedule of tariffs such as in France and England. The present study, however, can act as a starting point for future research on this topic becasuse it was first to describe the treatment trends for DD in Canada. Results from the present study can also provide Canadian medical practitioners involved in the care of patients with DD a better understanding of the characteristics of this patient population and DD treatment trends in this country.
REFERENCES
- 1.Mikkelsen OA. Dupuytren’s disease – a study of the pattern of distribution and stage of contracture in the hand. Hand. 1976;8:265–71. doi: 10.1016/0072-968x(76)90013-9. [DOI] [PubMed] [Google Scholar]
- 2.Rayan GM. Clinical presentation and types of Dupuytren’s disease. Hand Clin. 1999;15:87–96. vii. [PubMed] [Google Scholar]
- 3.Tubiana R, Leclercq C, Hurst LC, Badalamente MA, Mackin EJ, editors. Dupuytren’s Disease. London: Martin Dunitz; 2000. [Google Scholar]
- 4.Gonzalez SM, Gonzalez RI. Dupuytren’s disease. West J Med. 1990;152:430–3. [PMC free article] [PubMed] [Google Scholar]
- 5.Early P. Population studies in Dupuytren’s contracture. J Bone Joint Surg. 1962;44B:602–13. [Google Scholar]
- 6.Hueston JT. Incidence of Dupuytren’s contracture. Med J Aust. 1960;2:999–1002. [PubMed] [Google Scholar]
- 7.Mikkelsen OA. The prevalence of Dupuytren’s disease in Norway. A study in a representative population sampe of the municipality of Haugeund. Acta Chir Scand. 1972;38:695–700. [PubMed] [Google Scholar]
- 8.Ross DC. Epidemiology of Dupuytren’s disease. Hand Clin. 1999;15:53–62. vi. [PubMed] [Google Scholar]
- 9.Gudmundsson KG, Arngrimsson R, Sigfusson N, Bjornsson A, Jonsson T. Epidemiology of Dupuytren’s disease: Clinical, serological, and social assessment. The Reykjavik Study. J Clin Epidemiol. 2000;53:291–6. doi: 10.1016/s0895-4356(99)00145-6. [DOI] [PubMed] [Google Scholar]
- 10.Shaw RB, Jr, Chong AK, Zhang A, Hentz VR, Chang J. Dupuytren’s disease: History, diagnosis, and treatment. Plast Reconstr Surg. 2007;120:44e–54e. doi: 10.1097/01.prs.0000278455.63546.03. [DOI] [PubMed] [Google Scholar]
- 11.O’Gorman DB, Vi L, Gan BS. Molecular mechanisms and treatment strategies for Dupuytren’s disease. Ther Clin Risk Manag. 2010;6:383–90. doi: 10.2147/tcrm.s9165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Canadian Institute for Health Information . At the Heart of Data – Canadian Institute for Health Information Annual Report, 2011–2012. Ottawa: 2012. [Google Scholar]
- 13.Statistics Canada Population and dwelling counts, for Canada, provinces and territories, 2011 and 2006 censuses (Table) 2012 Population and Dwelling Count Highlight Tables. 2011 Census. Statistics Canada Catalogue no. 98-310-XWE2011002. Released February 8, 2012. < www12.statcan.gc.ca/census-recensement/2011/dp-pd/hlt-fst/pd-pl/Table-Tableau.cfm?LANG=Eng&T=101&S=50&O=A> (Accessed August 27, 2013). [Google Scholar]
- 14.Maravic M, Landais P. Dupuytren’s disease in France –1831 to 2001 – from description to economic burden. J Hand Surg Br. 2005;30:484–7. doi: 10.1016/j.jhsb.2005.05.004. [DOI] [PubMed] [Google Scholar]
- 15.Gerber RA, Perry R, Thompson R, Bainbridge C. Dupuytren’s contracture: A retrospective database analysis to assess clinical management and costs in England. BMC Musculoskelet Disord. 2011;12:73. doi: 10.1186/1471-2474-12-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Anthony SG, Lozano-Calderon SA, Simmons BP, Jupiter JB. Gender ratio of Dupuytren’s disease in the modern U.S. population. Hand. 2008;3:87–90. doi: 10.1007/s11552-007-9076-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yost J, Winters T, Fett HC., Sr Dupuytren’s contracture; a statistical study. Am J Surg. 1955;90:568–71. doi: 10.1016/0002-9610(55)90537-7. [DOI] [PubMed] [Google Scholar]
- 18.Statistics Canada Table 051-0001 – Estimates of population, by age group and sex for July 1, Canada, provinces and territories, annual (persons unless otherwise noted), CANSIM (database). < www5.statcan.gc.ca/cansim/a01?lang=eng> (Accessed November 27, 2011). [Google Scholar]
- 19.Grant A, O’Gorman DB, Gan BS. Management of Dupuytren’s disease with needle aponeurotomy: The Experience at the Hand and Upper Limb Centre, Canada. In: Eaton C, Seegenschmiedt H, Bayat A, Gabbiani G, Werker P, Wach W, editors. Dupuytren’s Disease and Related Hyperproliferative Disorders: Principles, Research, and Clinical Perspectives. Berlin: Springer; 2012. pp. 289–92. [Google Scholar]
- 20.Lee DS, Stitt A, Wang X, et al. Administrative hospitalization database validation of cardiac procedure codes. Med Care. 2013;51:e22–e26. doi: 10.1097/MLR.0b013e3182329778. [DOI] [PubMed] [Google Scholar]
- 21.Joseph KS, Fahey J. Validation of perinatal data in the Discharge Abstract Database of the Canadian Institute for Health Information. Chronic Dis Can. 2009;29:96–100. [PubMed] [Google Scholar]
- 22.Tu K, Mitiku T, Lee DS, Guo H, Tu JV. Validation of physician billing and hospitalization data to identify patients with ischemic heart disease using data from the Electronic Medical Record Administrative data Linked Database (EMRALD) Can J Cardiol. 2010;26:e225–e228. doi: 10.1016/s0828-282x(10)70412-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Daneman N, Simor AE, Redelmeier DA. Validation of a modified version of the national nosocomial infections surveillance system risk index for health services research. Infect Control Hosp Epidemiol. 2009;30:563–9. doi: 10.1086/597523. [DOI] [PubMed] [Google Scholar]
- 24.Park-Wyllie LY, Juurlink DN, Kopp A, et al. Outpatient gatifloxacin therapy and dysglycemia in older adults. N Engl J Med. 2006;354:1352–61. doi: 10.1056/NEJMoa055191. [DOI] [PubMed] [Google Scholar]
- 25.Lipscombe LL, Gomes T, Levesque LE, Hux JE, Juurlink DN, Alter DA. Thiazolidinediones and cardiovascular outcomes in older patients with diabetes. JAMA. 2007;298:2634–43. doi: 10.1001/jama.298.22.2634. [DOI] [PubMed] [Google Scholar]
- 26.Kwong JC, Manuel DG. Using OHIP physician billing claims to ascertain individual influenza vaccination status. Vaccine. 2007;25:1270–4. doi: 10.1016/j.vaccine.2006.10.004. [DOI] [PubMed] [Google Scholar]


