Abstract
Treatment failure and parasite drug susceptibility in dermal leishmaniasis caused by Leishmania (Viannia) species are poorly understood. Prospective evaluation of drug susceptibility of strains isolated from individual patients before drug exposure and at clinical failure allows intrinsic and acquired differences in susceptibility to be discerned and analyzed. To determine whether intrinsic susceptibility or loss of susceptibility to miltefosine contributed to treatment failure, we evaluated the miltefosine susceptibility of intracellular amastigotes and promastigotes of six Leishmania (Viannia) braziliensis and six Leishmania (Viannia) panamensis strains isolated sequentially, at diagnosis and treatment failure, from two children and four adults ≥55 years old with concurrent conditions. Four patients presented only cutaneous lesions, one had mucosal disease, and one had disseminated mucocutaneous disease. Expression of the Leishmania drug transporter genes abca2, abca3, abcc2, abcc3, abcg4, abcg6, and LbMT was evaluated by quantitative reverse transcription-PCR (qRT-PCR). Intracellular amastigotes (median 50% effective concentration [EC50], 10.7 μmol/liter) were more susceptible to miltefosine than promastigotes (median EC50, 55.3 μmol/liter) (P < 0.0001). Loss of susceptibility at failure, demonstrated by a miltefosine EC50 of >32 μmol/liter (the upper limit of intracellular amastigote assay), occurred in L. panamensis infection in a child and in L. braziliensis infection in an adult and was accompanied by decreased expression of the miltefosine transporter LbMT (LbMT/β-tubulin, 0.42- to 0.26-fold [P = 0.039] and 0.70- to 0.57-fold [P = 0.009], respectively). LbMT gene polymorphisms were not associated with susceptibility phenotype. Leishmania ABCA3 transporter expression was inversely correlated with miltefosine susceptibility (r = −0.605; P = 0.037). Loss of susceptibility is one of multiple factors involved in failure of miltefosine treatment in dermal leishmaniasis.
INTRODUCTION
Miltefosine, an alkylphosphocholine originally developed as an anticancer drug, is the first oral drug with proven efficacy for treatment of visceral leishmaniasis (VL) within the Indian subcontinent and cutaneous leishmaniasis (CL) caused by species of the Viannia subgenus of Leishmania in South America (1). Miltefosine was approved for treatment of cutaneous leishmaniasis in Colombia in 2004 after demonstrating efficacy comparable to that of pentavalent antimonials against disease caused by Leishmania panamensis (2). Although miltefosine has not been widely used in Latin America, treatment failures and relapses have been observed in randomized controlled clinical trials (3, 4). The efficacy and advantages of this oral drug, particularly for treatment of cutaneous leishmaniasis in children (4) and patients having contraindications for antimonial treatment, warrant measures to prolong its therapeutic life span.
Selective pressure exerted by antimicrobial therapy is influenced by the immune status of the host, susceptibility of the infecting microbial population, drug pharmacokinetics, adherence to treatment, dosing regimen, and use of monotherapy (5). The long half-life (150 to 200 h) and low therapeutic index of miltefosine result in exposure of surviving parasites to subtherapeutic drug concentrations that may persist in plasma up to 6 months after completion of treatment and thereby promote the emergence of resistance (1, 5, 6). Several studies have provided evidence of inter- and intraspecies differences in the susceptibility of Leishmania to antileishmanial drugs, including miltefosine (7, 8). Intrinsic differences in drug susceptibility of parasites transmitted in different geographic areas and foci of transmission are likely to influence the response to treatment and the selection of resistant populations.
Single-nucleotide changes in the transporter protein LdMT have been shown to confer resistance to miltefosine (9). Moreover, such mutations are readily selected by incremental in vitro exposure of promastigotes to miltefosine and confer the resistant phenotype on the amastigote stage (9). Leishmania braziliensis strains evaluated in vitro for susceptibility to miltefosine have generally demonstrated lower susceptibility than L. donovani; this difference has been attributed to lower expression of the miltefosine transporter complex, LbMT/LbRos3, in the plasma membrane of L. braziliensis (8). The expression of this transporter in other species and populations of Leishmania, and the participation of this or other transporters in the response to treatment is unknown.
In vitro susceptibility to antimicrobial agents, including antileishmanial drugs, does not necessarily correlate with treatment outcome (10). Nevertheless, the frequency of treatment failure increases as drug tolerance and resistance increase: infections caused by organisms that are susceptible have a higher rate of response to treatment than infections with drug-resistant organisms (11, 12). Moreover, drug resistance defined by in vitro susceptibility tests is generally an independent risk factor for treatment failure (10). The multifactorial basis of therapeutic response and the intraspecies diversity of Leishmania confound attempts to correlate clinical outcome with in vitro drug susceptibility. Furthermore, investigation of the relationship between in vitro susceptibility and clinical response is severely limited by the inability of health systems to monitor adherence to treatment or clinical response to treatment of cutaneous leishmaniasis. Therefore, the prospective detection of treatment failure is uncommon, and the availability of infecting Leishmania isolated at the time of diagnosis and at treatment failure is rare. Such clinical strains offer insight into host and parasite determinants of therapeutic response.
We examined treatment failure and loss of susceptibility to miltefosine based on clinical response, in vitro susceptibility to miltefosine, and transporter gene expression in L. panamensis and L. braziliensis strains isolated from six dermal leishmaniasis patients before treatment with miltefosine and at clinical failure.
MATERIALS AND METHODS
Study population.
Six dermal leishmaniasis patients who experienced clinical failure after treatment with miltefosine were included in the study (Table 1). Four patients presented 1 to 6 active cutaneous lesions of 1 to 4 months' duration. One patient presented disseminated mucocutaneous disease of 1 month's evolution, and another presented active mucosal disease of 96 months' duration and scarred cutaneous lesions that had occurred 25 years before consultation. Diagnosis and treatment were conducted by health personnel of the Centro Internacional de Entrenamiento e Investigaciones Médicas (CIDEIM). All patients completed treatment with miltefosine at 1.4 to 2.5 mg/kg/day for 28 days.
TABLE 1.
Clinical characteristics and miltefosine susceptibility of paired strains isolated from patients treated for cutaneous leishmaniasis with miltefosine who experienced clinical treatment failurea
| Patient | Gender | Age (yrs) | Concurrent condition(s) | Type of lesions | No. of lesions | Duration of lesions (months) | Previous treatment (no. of courses) | Species | EC50 (μmol HePC/liter) |
Parasite survival at 16 μmol HePC/liter (%) |
||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Before Rx | At Rx failure | Before Rx | At Rx failure | |||||||||
| 1 | M | 8 | None | Cutaneous | 5 | 1 | None | L. panamensis | 2.1 ± 0.7 | 2.9 ± 2.2 | 12.0 ± 2.0 | 12.0 ± 5.0 |
| 2 | F | 10 | None | Cutaneous | 3 | 1 | None | L. panamensis | 10.0 ± 3.7 | >32.0 | 33.0 ± 6.0 | 69.0 ± 3.0 |
| 3 | M | 55 | Uncontrolled arterial hypertension | Mucocutaneous | ∼50 | 1 | None | L. panamensis | 15.9 ± 3.2 | ND | 52.0 ± 5.0 | 40.0 ± 10 |
| 4 | F | 64 | Breast adenocarcinoma | Cutaneous | 1 | 4 | Glucantime (2 incomplete) | L. braziliensis | 10.5 ± 4.1 | 8.7 ± 2.5 | 35.0 ± 8.0 | 38.0 ± 9.0 |
| 5 | M | 64 | Heart failure, uncontrolled arterial hypertension | Cutaneous | 6 | 2 | None | L. braziliensis | 20.3 ± 2.5 | >32.0 | 61.0 ± 8.0 | 116 ± 28 |
| 6 | M | 72 | Pharmacological immunosuppression | Mucosal | 2 | 96 | Glucantime (1 complete) | L. braziliensis | 10.7 ± 3.0 | 12.0 ± 5.2 | 46.0 ± 1.0 | 55.0 ± 5.0 |
Susceptibility assays were conducted with intracellular amastigote stage. Data are means ± standard deviations for at least two experimental replicates for clinical isolates. ND, not determined, as data for the dose response curve for 2/3 independent experiments did not allow calculation of confidence intervals. Rx, treatment.
Two of the six patients were children who received directly observed treatment of cutaneous leishmaniasis as participants in a randomized clinical trial (4). They were clinically evaluated at the end of treatment, 13 and 26 weeks after initiation of treatment. Treatment failure in these children was diagnosed by the absence of healing at week 13 in accordance with the study protocol (4). The four adult patients were 55 to 72 years of age, presented concurrent conditions (Table 1), and received miltefosine on an ambulatory basis. Two adults had previously experienced failed treatment with meglumine antimoniate (Glucantime). Failure of miltefosine treatment in these patients occurred at or before 26 weeks following initiation of treatment. In one case, the primary lesion had worsened and new lesions had appeared (six in total) at end of treatment; one had not healed at week 26, and the other two experienced reactivation of cutaneous lesions (10 of the initial 50) or mucosal lesions.
The study protocol was approved by the CIDEIM Ethical Review Board for studies involving human subjects and conducted in accordance with national and international guidelines for Good Clinical Practice. Signed informed consent was obtained from each participant, and for those <18 years of age, consent was also provided by a parent.
Clinical strains of Leishmania.
Leishmania strains were isolated by culture of tissue fluid aspirated from lesion borders at diagnosis before treatment and at clinical failure. Posttreatment strains were isolated from lesions that failed to heal or reactivated or, in one case, from a new lesion that occurred during treatment. The latter patient did not return to an area where the disease is endemic during treatment and hence was not reexposed to transmission. Species identification was achieved using monoclonal antibodies and isoenzyme electrophoresis as previously described (13). The profile of monoclonal antibody reactivity was identical for the pre- and posttreatment strains isolated from each patient. Strains were stored in liquid nitrogen until evaluation of drug susceptibility. In vitro susceptibility to miltefosine (hexadecylphosphocholine [HePC]) was evaluated within four passages from isolation.
Control strains.
Internal controls included a wild-type (WT) miltefosine-sensitive cloned strain of L. panamensis transfected with the luciferase reporter gene (luc), MHOM/COL/03/3594/LUC001, as previously described (14), and a line derived from this strain by exposure of promastigotes to incremental concentrations of HePC (Cayman Chemical Co., Ann Arbor, MI), MHOM/COL/86/1166-LUC056 (15). The latter strain is resistant to 60 μmol HePC/liter as promastigotes. These controls were included in each assay of drug susceptibility of clinical strains. Control parasites were maintained in RPMI 1640 medium (Sigma-Aldrich) containing 10% heat-inactivated fetal bovine serum (HIFBS; Gibco), 1% penicillin-streptomycin solution (10,000 U/ml penicillin G plus 10,000 μg/ml streptomycin; Gibco BRL) and 80 μg/ml Geneticin G418 (Sigma-Aldrich). The miltefosine-resistant line was propagated and maintained in the presence of 60 μmol HePC/liter throughout the study.
In vitro amastigote infection and drug susceptibility assays.
In vitro susceptibility to miltefosine was evaluated in intracellular amastigotes and promastigotes. Drug susceptibility of intracellular amastigotes of clinical strains was evaluated as described by Fernandez et al. (15). Briefly, U-937 macrophages (ATCC CRL-159.3) were cocultured with stationary-phase promastigotes during 2 h at 34°C and a 5:1 parasite to cell ratio, washed with PBS, and incubated for 24 h at 34°C. Miltefosine susceptibility was defined as the 50% effective concentration (EC50), using a concentration range of 0.5 to 32 μmol HePC/liter (0.20 to 13 μg/ml), and as percent parasite survival at the single discriminatory concentration of 16 μmol HePC/liter (6.5 μg/ml) (15) after 48 h of drug exposure. Infection was blindly evaluated by microscopy in 300 macrophages (100 cells per triplicate well) for each drug concentration, and the number of parasites in each infected cell was determined. Percent parasite survival was estimated based on infection of macrophages without drug.
Promastigote susceptibility to miltefosine.
Susceptibility of promastigotes was evaluated during logarithmic growth phase in complete RPMI medium containing 10% HIFBS. Parasites were dispensed at 3 × 105 promastigotes/well in 96-well plates (Becton, Dickinson); four replicates for each drug concentration were evaluated following culture at 26°C for 72 h. The concentration range of 35 μmol/liter (14.3 μg/ml) to 80 μmol/liter (32.6 μg/ml) HePC was employed for promastigotes of clinical strains and extended to 120 μmol/liter (48.9 μg/ml) for the WT and miltefosine-resistant lines. Parasite viability was determined based on acid phosphatase activity (16). Plates were evaluated at 405 nm using an enzyme-linked immunosorbent assay (ELISA) reader (MRX Revelation; Dynex Technologies).
Evaluation of gene expression of LbMT and ABC transporters by RT-PCR.
In order to explore the relationship between in vitro susceptibility to miltefosine and drug transporters potentially involved in miltefosine transport and multidrug resistance, we evaluated the gene expression profile of the miltefosine transporter LbMT, the multidrug resistance transporters ABCC2 and ABCC3, and the lipid transporters ABCA2, ABCA3, ABCG4, and ABCG6 based on the biochemical homology of miltefosine and phosphatidylcholine and evidence that ABCG4 (17) and ABCG6 (18) are involved in experimentally derived miltefosine resistance.
Gene expression of abca2 (TriTrypDB accession no. LbrM.11.1020), abca3 (LbrM.11.1000), abcc2 (LbrM.23.0230), abcc3 (LbrM.23.0280), abcg4 (LbrM.15.0930), abcg6 (LbrM.35.3110), and LbMT (GenBank accession no. XM_001563228) was evaluated by qRT-PCR. Total RNA was extracted from log-phase promastigotes with TRIzol reagent (Invitrogen), followed by reverse transcription with a high-capacity cDNA reverse transcription kit (Applied Biosystems). Primer pairs were as follows: for abca2, ABCA2-F (5′ACCCTGGCGCGTGAGCTTTC3′) and ABCA2-R (5′AGCGCCTCCACCTCCTCCAG3′); for abca3, ABCA3-F (5′GCGAAGTGGGCGAGGTGCTT3′) and ABCA3-R (5′GTCTGTGACGTGCAGCCGCT3′); for abcc2, ABCC2-F (5′CGAACGAGTAGCGTTGTGAA3′) and ABCC2-R (5′CGAGAAACTCGACACGAACA3′); for abcc3, ABCC3-F (5′CAGAGCGCACTGGTACCAC3′) and ABCC3-R (5′GCAGCTCTGGGTCAGGCTGG3′); for abcg4, ABCG4-F (5′CTCATCACGAACCCCTTTGT3′) and ABCG4-R (5′CCAGTAGCAGCAGATCGTCA3′); for abcg6, ABCG6-F (5′ACGACGCTGCTCGATATCTT3′) and ABCG6-R (5′CTAGTTCCTCGGTCGAGACG3′); for LbMT, LbMT-F (5′GGTGACGTCAGTTGTGCCGC3′) and LbMT-R (5′GACGACATCGGCACGCACCT3′); and for the β-tubulin gene (LbrM.21.2150), βTUB-F (5′CGTGCAGAACAAGAACTCCA3′) and βTUB-R-F (5′CTCGGTGAACTCCATCTCGT3′). qPCR was performed using Sybr green PCR master mix (Applied Biosystems) and a Bio-Rad CFX-96 real-time PCR detection system. Gene expression was quantified based on standard curves for each gene and normalized to β-tubulin gene expression.
SNP genotyping of the LbMT gene.
The presence of C1259A (T420N) and T2567C (L856P) polymorphisms in the LbMT gene, previously reported to be associated with experimentally derived miltefosine resistance (9), and G630A (W210*) analyzed in VL and post-kala-azar dermal leishmaniasis (PKDL) strains of L. donovani (19) were characterized by sequence analysis of PCR products. Total DNA was extracted from logarithmic-phase promastigotes using a DNeasy blood and tissue kit (Qiagen). PCR was carried out using primer sets W210*-F (5′-AGGCGTTCATTGACACATGC-3′) and W210*-R (5′-TACAGGAACTGGTTCAGCGAC-3′); T420N-F (5′-TGGAGTACATGAACAACCGCT-3′) and T420N-R (5′-CTCTTCCTCCTTGCGCAGTC-3′), and L856P-F (5′-TCATTGGGCTGGAAGGTTCA-3′) and L856P-R (5′-GTGTTAGTCCCGAGAAGCCA-3′). Primers were designed using Primer-BLAST based on the L. braziliensis reference sequence XM_001563228. PCR products of approximately 200 bp were extracted from the gel and purified for the sequencing reaction. Sequence analyses, single-nucleotide polymorphism (SNP) identification, and ClustalW multiple sequence alignment were performed using BioEdit v7.2.0. The L. braziliensis LbMT reference sequence LbrM.13.1380 was used as the reference for sequence alignment.
Statistical analyses.
The EC50 was determined using the Probit program of SPSS (version 20). Interstage differences in clinical strains were analyzed using the Mann-Whitney nonparametric test. Area under the dose-response curve (AUC) was used to determine differences in miltefosine susceptibility of clinical strains isolated before treatment and at treatment failure and between sensitive and resistant controls. LbMT gene expression of strains isolated before and after treatment from patients 2 and 5 was analyzed with the Wilcoxon signed-rank test or paired test according to the distribution of the data. The Spearman correlation test was employed to evaluate the association of miltefosine transporter gene expression and susceptibility of clinical strains to miltefosine. The statistical analyses were conducted using GraphPad Prism version 5.0 for Windows. Significance was defined as a P value of <0.05. Principal component analyses (PCA) were performed with quantitative transporter gene expression data using Tanagra software (20).
RESULTS
In vitro susceptibility of promastigote and amastigote stages. (i) WT and the experimentally selected resistant strain of L. panamensis.
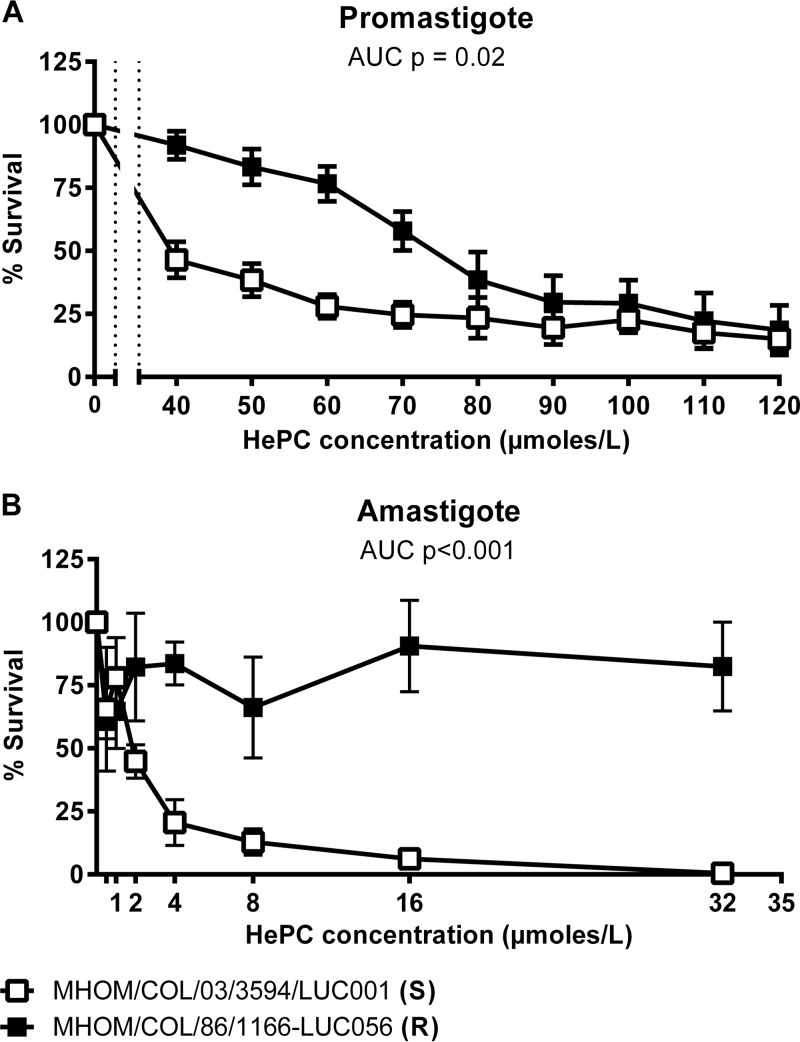
Selection of miltefosine-resistant L. panamensis by exposure of promastigotes to increasing concentrations of miltefosine also resulted in loss of miltefosine susceptibility of intracellular amastigotes. The corresponding dose-response survival curves markedly diverged from that for the WT strain over the range of HePC concentrations evaluated (Fig. 1A and B). The mean EC50 for promastigotes nearly doubled, from 56.1 μmol HePC/liter ± 8.1 (22.9 μg/ml) in the WT strain to 99.4 μmol/liter ± 2.4 (40.5 μg/ml) in the resistant strain (P = 0.05); for amastigotes, the EC50 increased by a factor of 10, from 2.9 ± 1.8 μmol/liter (1.2 μg/ml) to >32 μmol/liter (>13.0 μg/ml) (P = 0.011) in the experimentally selected line. Notably, 32 μmol HePC/liter is the maximum usable dose for in vitro intracellular assays because of the toxicity of higher concentrations for host macrophages, whether primary cells or established cell lines. The difference is further substantiated by analysis of the areas under the curve (AUC) for promastigotes (P = 0.02) and amastigotes (P < 0.001) (Fig. 1).
FIG 1.
Miltefosine susceptibility of the WT and an experimentally selected resistant strain of L. panamensis. The dose response to HePC of WT and experimentally selected miltefosine-resistant controls are presented (means and standard errors of the means [SEM] from three independent experiments) for promastigotes and amastigotes. Survival is presented as the percent survival of promastigotes or intracellular amastigotes compared to drug-free control at each drug concentration. S, sensitive; R, resistant.
(ii) Clinical strains of L. panamensis and L. braziliensis.
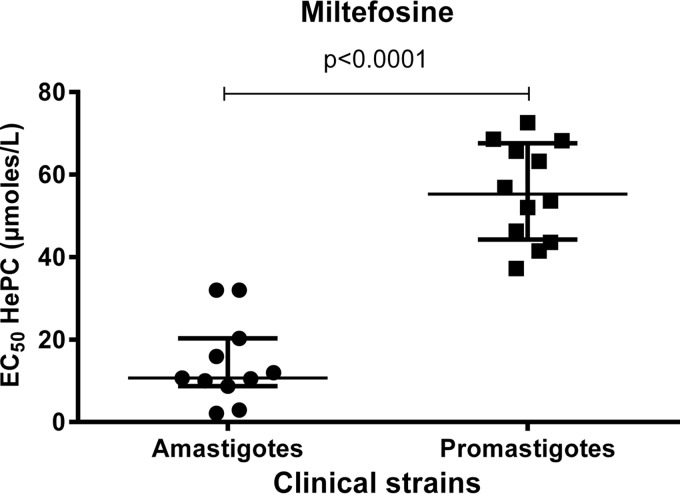
Evaluation of susceptibility of promastigotes and amastigotes of 12 clinical strains, six L. panamensis and six L. braziliensis, isolated before treatment with miltefosine and at treatment failure corroborated the higher in vitro susceptibility of intracellular amastigotes (median EC50, 10.7 μmol HePC/liter [4.4 μg/ml]) than promastigotes (median EC50, 55.3 μmol/liter [22.5 μg/ml]) (Fig. 2) (P < 0.0001). The greater susceptibility to miltefosine of intracellular amastigotes of strains belonging to two species of the subgenus Viannia allowed detection of significant changes in susceptibility of parasites isolated at the time of clinical failure.
FIG 2.
Susceptibility of clinical strains of L. panamensis and L. braziliensis to miltefosine as intracellular amastigotes and promastigotes. Values are median EC50s of clinical strains, evaluated as intracellular amastigotes (n = 11) in at least two independent experiments and as promastigotes (n = 12) in three independent experiments. The EC50 of the strain from patient 3 isolated at treatment failure was not determined; data for the dose-response curve for 2/3 independent experiments did not allow calculation of confidence intervals. Data were analyzed using the Mann-Whitney nonparametric test.
Susceptibility to miltefosine following in vivo exposure and failure of treatment.
In two of six patients, one child (patient 2) and one elderly adult (patient 5), treatment with miltefosine led to emergence of drug-tolerant populations of L. panamensis and L. braziliensis, respectively. Loss of susceptibility was substantiated by the significant increase in survival of intracellular amastigotes at 16 μmol HePC/liter, a concentration previously shown to discriminate between the WT and the experimentally selected tolerant/resistant strain (15). Survival of the L. panamensis strains isolated from patient 2 increased from 33% before treatment to 69% at failure. Similarly, the survival of L. braziliensis strains from patient 5 increased from 61% before treatment to 116% at failure (Table 1). The increased survival of intracellular parasites exposed to incremental concentrations of HePC and the higher EC50 of miltefosine for the strains isolated at failure corroborated their diminished susceptibility compared with the strains isolated before treatment (Table 1; Fig. 3A and B). The EC50 of miltefosine for strains isolated from patients 2 and 5 at treatment failure was >32 μmol/liter, the upper limit of the intracellular assay. Additionally, the dose-response profile of these strains was similar to that of the experimentally derived miltefosine-resistant strain (Fig. 1B). The change in AUC was significant for strains from patient 2 (P < 0.001). The EC50s, dose response curves, and survival of intracellular amastigotes exposed to 16 μmol HePC/liter did not significantly differ for strains isolated before treatment and at failure from the other four patients (Table 1 and Fig. 3).
FIG 3.
Dose response of intracellular amastigotes of clinical strains isolated from patients before treatment with miltefosine and at failure. The susceptibilities of strains isolated from each of the six patients (means and SEM from three independent evaluations) are shown. Response is presented as the percent survival of intracellular amastigotes compared to drug-free controls at each drug concentration.
Although the magnitude of change in susceptibility of promastigotes to miltefosine was less marked and not statistically significant, the diminished susceptibility of promastigotes of strains isolated from patients 2 and 5 after treatment, concurred with results obtained with intracellular amastigotes. Whereas promastigotes of strains from patient 2 presented an increase in EC50 from 41.5 ± 4.1 μmol HePC/liter before treatment to 52.0 ± 12.3 μmol/liter at failure, and the EC50 of strains from patient 5 increased from 56.9 ± 20.7 μmol/liter to 68.6 ± 19.8 μmol/liter, the EC50 had not changed in the other four strain pairs (data not shown).
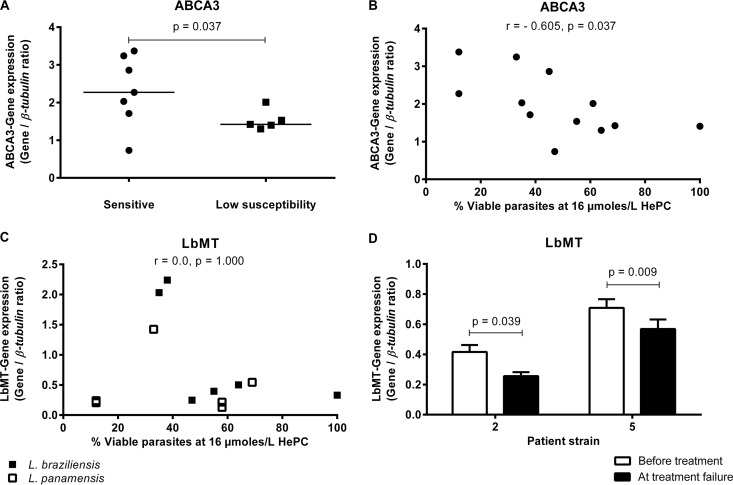
ABC transporter and LbMT expression profile of miltefosine-susceptible and -tolerant/resistant clinical strains.
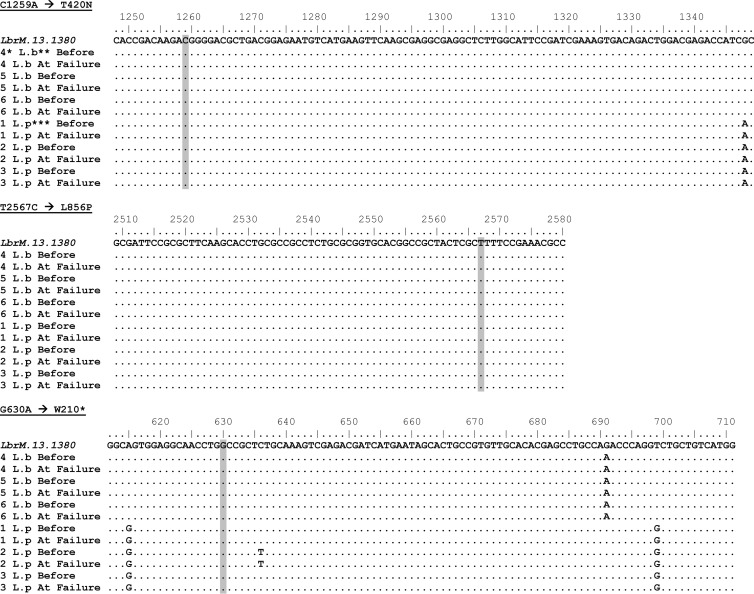
Miltefosine-sensitive strains exhibited significantly higher expression of abca3 than strains having tolerance/low susceptibility to the drug (P = 0.037) (Fig. 4A). Furthermore, correlation analyses revealed a significant inverse relationship (P = 0.037) between abca3 expression and intracellular parasite survival (Fig. 4B). In contrast, expression of abca2, abcg4, abcg6, abcc2, and abcc3 was similar, irrespective of the level of drug susceptibility (data not shown). Gene expression of the miltefosine transporter LbMT did not correlate with the degree of susceptibility to miltefosine of these clinical strains (Fig. 4C). However, significantly decreased expression of this transporter was observed in the strains isolated from patients 2 and 5, which developed tolerance to HePC following treatment of the corresponding patients with miltefosine (strain from patient 2, P = 0.039; strain from patient 5, P = 0.009) (Fig. 4D). Sequence analysis of the LbMT gene at positions 1259 and 2567, previously reported to be associated with LbMT loss of function (9), and at position 630 analyzed in L. donovani strains isolated from patients with VL and PKDL who relapsed after treatment with miltefosine (19) revealed no association between these SNPs and the resistance phenotype of the clinical strains in our study or genetic variations between strains isolated before treatment and at treatment failure from the same patient (Fig. 5). Interestingly, the SNPs A615G, G691A, T699G, and G1348A were species specific, differentiating L. panamensis from L. braziliensis.
FIG 4.
Correlation of ABCA3 and LbMT expression with miltefosine susceptibility of clinical strains of L. panamensis and L. braziliensis. (A) Strains with low miltefosine susceptibility (n = 5) exhibited significantly lower ABCA3 transporter gene expression than sensitive (n = 7) strains. (B) Expression of ABCA3 was inversely correlated with the susceptibility of clinical strains (n = 12) as intracellular parasite survival at 16 μmol/liter of miltefosine. (C) LbMT expression was not correlated with miltefosine susceptibility in clinical strains of L. panamensis and L. braziliensis. The data are from three independent evaluations of 12 clinical strains of L. panamensis and L. braziliensis. (D) Significant reduction of LbMT gene expression was observed in strains of L. panamensis and L. braziliensis exhibiting diminished susceptibility to miltefosine at treatment failure. Data are means and SEM from seven independent experiments.
FIG 5.
Sequence analysis of the LbMT gene. PCR products of the LbMT gene from the 6 pairs of strains (12 strains) isolated before treatment and at treatment failure were sequenced. The presence of G630A, C1259A, and T2567C SNPs (shading) were analyzed in relation to the susceptibility phenotype of each strain, showing no association between these SNPs and susceptibility to miltefosine. *, Numbering refers to the number assigned to the patient from which the strain was isolated. **, L. braziliensis; ***, L. panamensis. Sequences were aligned to the reference L. braziliensis sequence LbrM.13.1380.
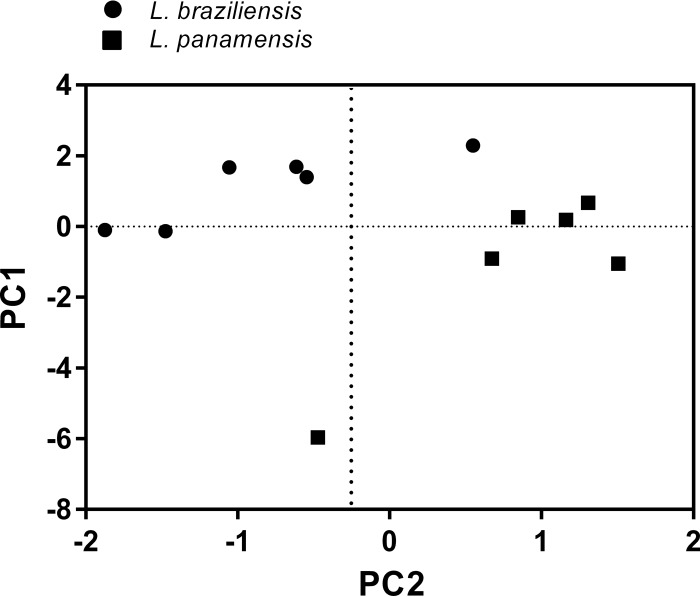
Principal component analysis distinctly grouped strains of L. panamensis and L. braziliensis in relation to principal component 1 (PC1) and PC2 (Fig. 6). Examination of the variables contributing to the different components showed that PC1 comprised abca2, abca3, abcc3, abcg4, and abcg6 transporter genes, while PC2 was dominated by abcc2 and LbMT. These analyses revealed higher levels of PC2 and a trend of increased PC1 for L. panamensis compared to L. braziliensis. PC1 accounted for 61% of gene expression variability and PC2 for 17%.
FIG 6.
Principal component (PC) analysis score plot of transporter gene expression in L. panamensis and L. braziliensis promastigotes. Each point represents an individual strain. PC1 reflects expression of abca2, abca3, abcc3, abcg4, and abcg6 transporter genes, and PC2 reflects expression of abcc2 and LbMT.
DISCUSSION
Prospective evaluation of therapeutic response and miltefosine susceptibility before and after in vivo drug exposure during treatment provides a unique opportunity to discern acquired and intrinsic differences in susceptibility. This study of patients with infections that failed to respond to miltefosine treatment yielded evidence of both intrinsic and acquired differences in drug susceptibility. In one case, resistance emerged from infection with a susceptible strain of L. panamensis, and in another, resistance followed infection with an intrinsically tolerant strain of L. braziliensis. These two cases of loss of susceptibility to miltefosine provide direct evidence that miltefosine administered as monotherapy for cutaneous leishmaniasis can select drug-resistant parasites.
Diminished clinical efficacy of miltefosine after a decade of unregulated use in India had been suspected but has now been documented (21). Strains of L. donovani isolated from visceral leishmaniasis and PKDL patients who relapsed following miltefosine treatment were significantly more tolerant to miltefosine than the corresponding pretreatment strains (19). The selective potential of miltefosine treatment in visceral leishmaniasis was also substantiated by the incremental increase in tolerance of sequential isolates of Leishmania infantum obtained at relapse from an HIV-coinfected patient who received maintenance treatment with miltefosine for several years (22). The emergence of tolerant/resistant Leishmania populations in different clinical, epidemiological, and geographic circumstances underscores the need for measures to protect the effective life of this drug.
Age-associated pharmacokinetic differences, parasite drug susceptibility, and concurrent conditions that alter immune competence evidently contributed to the unfavorable outcome of miltefosine treatment in this group of patients. The 10-year-old child from whom the resistant strain of L. panamensis was isolated at week 13 of follow-up presented no clinical evidence of immune deficiency or comorbidities that might have influenced the failure to heal. However, pharmacokinetic analyses reported by Dorlo and collaborators showing a body size-associated decrease in miltefosine exposure when the body weight dosage used in adults is applied in children (23) support the plausibility of the idea that lower exposure to miltefosine promoted outgrowth of resistant parasites and unsuccessful treatment in this patient. The 8-year-old child with an infection that failed to respond to miltefosine despite the susceptibility of the infecting strain presented a lesion on the ear, a cartilaginous site recognized to be therapeutically challenging (24). Concurrent conditions, including altered renal function, immunosuppression, and hypertension (25), in the elderly adult patients are likely to have contributed to the poor clinical response to miltefosine treatment, independently of the susceptibility of the infecting Leishmania strain to miltefosine. Therefore, even when resistance does emerge, it is unlikely to be the singular cause of treatment failure. Host factors that allow surviving parasites to proliferate may both promote clinical failure and emergence of resistance.
Significantly greater susceptibility of intracellular amastigotes to miltefosine than promastigotes was consistently demonstrated both for clinical strains of L. braziliensis and L. panamensis and for the WT and experimentally selected miltefosine-resistant strain of L. panamensis. Importantly, the susceptibility phenotype was detectable in both life stages. Comparative data on the susceptibility of intracellular amastigotes and promastigotes to miltefosine are limited and generally based on secondary observations of in vitro susceptibility of different Leishmania species/strains, host cells, culture conditions, and assay and readout parameters (26), all of which influence the estimation of effective drug concentrations (15). A detailed comparative study using a single strain of L. donovani suggested that promastigotes and intracellular amastigotes within peritoneal mouse macrophages were comparably susceptible to miltefosine, with a trend toward greater susceptibility of intracellular amastigotes (27). The greater susceptibility of amastigotes may be attributable to increased cytotoxicity within the macrophage, conferred by alkyl-lysophospholipids promoting the death of intracellular parasites either by direct action of the drug or as a secondary effect on host cells as oxidative burst or production of reactive-oxygen metabolites (28). In contrast to other studies, our study included miltefosine-susceptible and -resistant controls that provided internal references for the interpretation of effective concentrations and reduction of parasite burden. Intracellular amastigotes, which approximate the natural therapeutic target, including host cell-dependent mechanisms of action, are considered the gold standard for drug susceptibility assessment (27).
Investigations of laboratory-derived miltefosine-resistant strains showed that differential drug transport contributed to changes in drug susceptibility. Reduced expression of the translocase complex LbMT/LbRos3 conferred the resistant phenotype in L. braziliensis strains through decreased drug uptake (8). Single-nucleotide polymorphisms (SNP) have been associated with functional variations of the LdMT/LdRos3 complex in L. donovani (9). However, our results and those of studies evaluating the relationship of these polymorphisms to drug susceptibility profiles of clinical strains have either not demonstrated an association or not provided consistent evidence thus far (19), substantiating the rationale for analysis of drug susceptibility as a function of transporter gene expression for clinical strains, rather than SNP profiling. Although LbMT expression was not correlated with intrinsic susceptibility to miltefosine in clinical strains of L. braziliensis and L. panamensis (Fig. 4C), decreased expression of LbMT, but not of ABC transporters, occurred in strains that demonstrated loss of susceptibility to miltefosine at treatment failure (Fig. 4D). This suggests that in vivo exposure to miltefosine could promote the selection of less susceptible parasite populations having reduced expression of LbMT. Individual gene expression profiling of ABCA and ABCG lipid transporters revealed an inverse correlation between abca3 and intracellular parasite survival following in vitro exposure to miltefosine (Fig. 4B) supporting the possibility that the level of ABCA3 expression may contribute to intrinsic variations in susceptibility of Leishmania strains to miltefosine. Interestingly, ABCA3 has been shown to localize to intracellular membranes, where it promotes accumulation and storage of phosphatidylcholine (29). Hence, upregulation of Leishmania ABCA3 could promote increased drug accumulation through storage in intracellular vesicles, thereby contributing to a drug-susceptible phenotype. Nevertheless, functional confirmation of the participation and role of ABCA3 in miltefosine susceptibility is necessary.
Finally, the grouping of L. panamensis and L. braziliensis through principal component analysis of transporter gene expression substantiates a species-related profile of expression of these drug transporters. Together, our findings support the operation of multiple and different mechanisms among intrinsic and acquired phenotypes of miltefosine resistance in Leishmania strains and species.
This prospective analysis of strains from patients with dermal leishmaniasis that failed to respond to treatment with miltefosine provides the first direct evidence of the emergence of resistance to miltefosine during treatment of dermal leishmaniasis caused by species of the Leishmania subgenus Viannia. Miltefosine is a second-line treatment in Colombia and has not been widely administered. Rather, it is reserved for patients with contraindications or intolerance for meglumine antimoniate. Understanding and management of risk factors for treatment failure together with implementation of measures to ensure appropriate use and adherence to treatment may prevent the loss of susceptibility to this valuable drug.
ACKNOWLEDGMENTS
We gratefully acknowledge the assistance of Mauricio Perez and Neal Alexander in conducting statistical analyses, Harry Castillo and Mabel Valderrama for their invaluable contribution to the microscopic assessment of intracellular infection, and the clinical team for their assistance in the diagnosis, enrollment, and clinical management of patients. Miltefosine (Impavido) was donated by Paladin Labs Inc., Montreal, Canada.
This research was supported by the Colombian National Departamento Administrativo de Ciencia, Tecnología e Innovación (COLCIENCIAS), contracts 2229-408-20418 and 2229-519-28930. R.O., O.L.F., M.D.M.C., and M.A.G. were supported in part by the Fogarty International Center U.S. under award number D43 TW006589. This work was also supported by the National Institutes of Health Global Infectious Disease Research Training Program, 2D43TW006589-08, and the COLCIENCIAS Young Investigators and Innovators Program, 159-2008 and 797-2009.
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Published ahead of print 21 October 2013
REFERENCES
- 1.Berman J. 2005. Miltefosine to treat leishmaniasis. Expert Opin. Pharmacother. 6:1381–1388. 10.1517/14656566.6.8.1381 [DOI] [PubMed] [Google Scholar]
- 2.Soto J, Arana BA, Toledo J, Rizzo N, Vega JC, Diaz A, Luz M, Gutierrez P, Arboleda M, Berman JD, Junge K, Engel J, Sindermann H. 2004. Miltefosine for new world cutaneous leishmaniasis. Clin. Infect. Dis. 38:1266–1272. 10.1086/383321 [DOI] [PubMed] [Google Scholar]
- 3.Velez I, Lopez L, Sanchez X, Mestra L, Rojas C, Rodriguez E. 2010. Efficacy of miltefosine for the treatment of American cutaneous leishmaniasis. Am. J. Trop. Med. Hyg. 83:351–356. 10.4269/ajtmh.2010.10-0060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rubiano LC, Miranda MC, Muvdi Arenas S, Montero LM, Rodriguez-Barraquer I, Garcerant D, Prager M, Osorio L, Rojas MX, Perez M, Nicholls RS, Gore Saravia N. 2012. Noninferiority of miltefosine versus meglumine antimoniate for cutaneous leishmaniasis in children. J. Infect. Dis. 205:684–692. 10.1093/infdis/jir816 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bryceson A. 2001. A policy for leishmaniasis with respect to the prevention and control of drug resistance. Trop. Med. Int. Health 6:928–934. 10.1046/j.1365-3156.2001.00795.x [DOI] [PubMed] [Google Scholar]
- 6.Dorlo TP, van Thiel PP, Huitema AD, Keizer RJ, de Vries HJ, Beijnen JH, de Vries PJ. 2008. Pharmacokinetics of miltefosine in Old World cutaneous leishmaniasis patients. Antimicrob. Agents Chemother. 52:2855–2860. 10.1128/AAC.00014-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yardley V, Croft SL, De Doncker S, Dujardin JC, Koirala S, Rijal S, Miranda C, Llanos-Cuentas A, Chappuis F. 2005. The sensitivity of clinical isolates of Leishmania from Peru and Nepal to miltefosine. Am. J. Trop. Med. Hyg. 73:272–275 http://www.ajtmh.org/content/73/2/272.long [PubMed] [Google Scholar]
- 8.Sanchez-Canete MP, Carvalho L, Perez-Victoria FJ, Gamarro F, Castanys S. 2009. Low plasma membrane expression of the miltefosine transport complex renders Leishmania braziliensis refractory to the drug. Antimicrob. Agents Chemother. 53:1305–1313. 10.1128/AAC.01694-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Perez-Victoria FJ, Gamarro F, Ouellette M, Castanys S. 2003. Functional cloning of the miltefosine transporter. A novel P-type phospholipid translocase from Leishmania involved in drug resistance. J. Biol. Chem. 278:49965–49971. 10.1074/jbc.M308352200 [DOI] [PubMed] [Google Scholar]
- 10.Doern GV, Brecher SM. 2011. The clinical predictive value (or lack thereof) of the results of in vitro antimicrobial susceptibility tests. J. Clin. Microbiol. 49:S11. 10.1128/JCM.00580-11 [DOI] [Google Scholar]
- 11.Nguyen MH, Yu VL, Morris AJ, McDermott L, Wagener MW, Harrell L, Snydman DR. 2000. Antimicrobial resistance and clinical outcome of Bacteroides bacteremia: findings of a multicenter prospective observational trial. Clin. Infect. Dis. 30:870–876. 10.1086/313805 [DOI] [PubMed] [Google Scholar]
- 12.Cosgrove SE, Sakoulas G, Perencevich EN, Schwaber MJ, Karchmer AW, Carmeli Y. 2003. Comparison of mortality associated with methicillin-resistant and methicillin-susceptible Staphylococcus aureus bacteremia: a meta-analysis. Clin. Infect. Dis. 36:53–59. 10.1086/345476 [DOI] [PubMed] [Google Scholar]
- 13.Saravia NG, Holguin AF, McMahon-Pratt D, D'Alessandro A. 1985. Mucocutaneous leishmaniasis in Colombia: Leishmania braziliensis subspecies diversity. Am. J. Trop. Med. Hyg. 34:714–720 [DOI] [PubMed] [Google Scholar]
- 14.Roy G, Dumas C, Sereno D, Wu Y, Singh AK, Tremblay MJ, Ouellette M, Olivier M, Papadopoulou B. 2000. Episomal and stable expression of the luciferase reporter gene for quantifying Leishmania spp. infections in macrophages and in animal models. Mol. Biochem. Parasitol. 110:195–206. 10.1016/S0166-6851(00)00270-X [DOI] [PubMed] [Google Scholar]
- 15.Fernandez O, Diaz-Toro Y, Valderrama L, Ovalle C, Valderrama M, Castillo H, Perez M, Saravia NG. 2012. Novel approach to in vitro drug susceptibility assessment of clinical strains of Leishmania spp. J. Clin. Microbiol. 50:2207–2211. 10.1128/JCM.00216-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bodley AL, McGarry MW, Shapiro TA. 1995. Drug cytotoxicity assay for African trypanosomes and Leishmania species. J. Infect. Dis. 172:1157–1159. 10.1093/infdis/172.4.1157 [DOI] [PubMed] [Google Scholar]
- 17.Castanys-Muñoz E, Alder-Baerens N, Pomorski T, Gamarro F, Castanys S. 2007. A novel ATP-binding cassette transporter from Leishmania is involved in transport of phosphatidylcholine analogues and resistance to alkyl-phospholipids. Mol. Microbiol. 64:1141–1153. 10.1111/j.1365-2958.2007.05653.x [DOI] [PubMed] [Google Scholar]
- 18.Castanys-Muñoz E, Pérez-Victoria JM, Gamarro F, Castanys S. 2008. Characterization of an ABCG-like transporter from the protozoan parasite Leishmania with a role in drug resistance and transbilayer lipid movement. Antimicrob. Agents Chemother. 52:3573–3579. 10.1128/AAC.00587-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bhandari V, Kulshrestha A, Deep DK, Stark O, Prajapati VK, Ramesh V, Sundar S, Schonian G, Dujardin JC, Salotra P. 2012. Drug susceptibility in Leishmania isolates following miltefosine treatment in cases of visceral leishmaniasis and post kala-azar dermal leishmaniasis. PLoS Negl. Trop. Dis. 6:e1657. 10.1371/journal.pntd.0001657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rakotomalala R. 2005. TANAGRA: a free software for research and academic purposes, p. 697–702 In Proceedings of European Grid Conference 2005, vol 2 RNTI-E-3. (In French.) [Google Scholar]
- 21.Sundar S, Singh A, Rai M, Prajapati VK, Singh AK, Ostyn B, Boelaert M, Dujardin JC, Chakravarty J. 2012. Efficacy of miltefosine in the treatment of visceral leishmaniasis in India after a decade of use. Clin. Infect. Dis. 55:543–550. 10.1093/cid/cis474 [DOI] [PubMed] [Google Scholar]
- 22.Cojean S, Houze S, Haouchine D, Huteau F, Lariven S, Hubert V, Michard F, Bories C, Pratlong F, Le Bras J, Loiseau PM, Matheron S. 2012. Leishmania resistance to miltefosine associated with genetic marker. Emerg. Infect. Dis. 18:704–706. 10.3201/eid1804.110841 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dorlo TP, Huitema AD, Beijnen JH, de Vries PJ. 2012. Optimal dosing of miltefosine in children and adults with visceral leishmaniasis. Antimicrob. Agents Chemother. 56:3864–3872. 10.1128/AAC.00292-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vargas-Gonzalez A, Canto-Lara SB, Damian-Centeno AG, Andrade-Narvaez FJ. 1999. Response of cutaneous leishmaniasis (chiclero's ulcer) to treatment with meglumine antimoniate in Southeast Mexico. Am. J. Trop. Med. Hyg. 61:960–963 [DOI] [PubMed] [Google Scholar]
- 25.Amato VS, Tuon FF, Imamura R, Abegao de Camargo R, Duarte MI, Neto VA. 2009. Mucosal leishmaniasis: description of case management approaches and analysis of risk factors for treatment failure in a cohort of 140 patients in Brazil. J. Eur. Acad. Dermatol. Venereol. 23:1026–1034. 10.1111/j.1468-3083.2009.03238.x [DOI] [PubMed] [Google Scholar]
- 26.Dey T, Afrin F, Anam K, Ali N. 2002. Infectivity and virulence of Leishmania donovani promastigotes: a role for media, source, and strain of parasite. J. Eukaryot. Microbiol. 49:270–274. 10.1111/j.1550-7408.2002.tb00369.x [DOI] [PubMed] [Google Scholar]
- 27.Vermeersch M, da Luz RI, Tote K, Timmermans JP, Cos P, Maes L. 2009. In vitro susceptibilities of Leishmania donovani promastigote and amastigote stages to antileishmanial reference drugs: practical relevance of stage-specific differences. Antimicrob. Agents Chemother. 53:3855–3859. 10.1128/AAC.00548-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Azzouz S, Maache M, Garcia RG, Osuna A. 2005. Leishmanicidal activity of edelfosine, miltefosine and ilmofosine. Basic Clin. Pharmacol. Toxicol. 96:60–65. 10.1111/j.1742-7843.2005.pto960109.x [DOI] [PubMed] [Google Scholar]
- 29.Matsumura Y, Sakai H, Sasaki M, Ban N, Inagaki N. 2007. ABCA3-mediated choline-phospholipids uptake into intracellular vesicles in A549 cells. FEBS Lett. 581:3139–3144. 10.1016/j.febslet.2007.05.078 [DOI] [PubMed] [Google Scholar]