Abstract
Dysbiosis in the intestinal microbiota of persons with inflammatory bowel disease (IBD) has been described, but there are still varied reports on changes in the abundance of Bifidobacterium and Lactobacillus organisms in patients with IBD. The aim of this investigation was to compare the compositions of mucosa-associated and fecal bacteria in patients with IBD and in healthy controls (HCs). Fecal and biopsy samples from 21 HCs, 21 and 15 Crohn's disease (CD) patients, and 34 and 29 ulcerative colitis (UC) patients, respectively, were analyzed by quantitative real-time PCR targeting the 16S rRNA gene. The bacterial numbers were transformed into relative percentages for statistical analysis. The proportions of bacteria were uniformly distributed along the colon regardless of the disease state. Bifidobacterium was significantly increased in the biopsy specimens of active UC patients compared to those in the HCs (4.6% versus 2.1%, P = 0.001), and the proportion of Bifidobacterium was significantly higher in the biopsy specimens than in the fecal samples in active CD patients (2.7% versus 2.0%, P = 0.012). The Lactobacillus group was significantly increased in the biopsy specimens of active CD patients compared to those in the HCs (3.4% versus 2.3%, P = 0.036). Compared to the HCs, Faecalibacterium prausnitzii was sharply decreased in both the fecal and biopsy specimens of the active CD patients (0.3% versus 14.0%, P < 0.0001 for fecal samples; 0.8% versus 11.4%, P < 0.0001 for biopsy specimens) and the active UC patients (4.3% versus 14.0%, P = 0.001 for fecal samples; 2.8% versus 11.4%, P < 0.0001 for biopsy specimens). In conclusion, Bifidobacterium and the Lactobacillus group were increased in active IBD patients and should be used more cautiously as probiotics during the active phase of IBD. Butyrate-producing bacteria might be important to gut homeostasis.
INTRODUCTION
Crohn's disease (CD) and ulcerative colitis (UC) are two forms of inflammatory bowel disease (IBD), a condition driven by an abnormal immune response to the intestinal microbiota in genetically susceptible hosts (1–3). Dysbiosis of the intestinal microbiota is common in IBD. Evidence from antibiotic treatment of IBD, fecal stream diversion in CD, and experimental models of colitis have shown that microbiotas play an important role in the pathogenesis of IBD, and the improvement of dysbiosis in the intestinal microbiota has been propounded as a new strategy for IBD treatment (4).
Probiotics are live microorganisms that have health benefits to the host when consumed in adequate amounts, and clinical studies indicate that the quantity of Bifidobacterium and Lactobacillus organisms decreases in the intestinal microbiotas of IBD patients (4). Several clinical trials have demonstrated the efficacy of VSL#3, a mixture of eight different probiotics, for the treatment of UC patients (5, 6), and single-species probiotic treatment, such as one with Escherichia coli Nissle 1917, Bifidobacterium, or Lactobacillus rhamnosus GG, also displays efficacy in the management of patients with UC (7–9). Meanwhile, experimental studies in colitis mouse models have demonstrated the potential protective mechanisms of these probiotics, through their reinforcement of the epithelial barrier (10, 11), inhibition of proinflammatory cytokine secretion (12, 13), and modulation of immune responses (14, 15). Few studies have evaluated the effectiveness of probiotics in CD patients. One study suggested that Faecalibacterium prausnitzii prevents 2,4,6-trinitrobenzenesulfonic acid (TNBS)-induced colitis (16).
However, studies have shown that the diversity of the genus Bifidobacterium is not decreased in the feces of patients with active CD (17) and that the numbers of Bifidobacterium organisms do not decrease in active CD patients (18). A twin study even found an increased abundance of Bifidobacterium and F. prausnitzii organisms in the mucosal samples of colonic CD patients, as well as an elevated abundance of Lactobacillus organisms in the mucosal samples of ileal CD patients (19). These reports seem to be in conflict with previous data.
To investigate the changes caused by common probiotics in IBD patients, we used real-time PCR to quantify bacteria in mucosal biopsy specimens and fecal samples of patients with IBD. Furthermore, we also determined the proportional differences of the dominant commensal bacteria between paired fecal and mucosal samples.
MATERIALS AND METHODS
Patients and samples.
Chinese patients of Han ethnicity with UC and CD were consecutively recruited from among the outpatients and inpatients in the Department of Gastroenterology at Zhongnan Hospital of Wuhan University, Wuhan, China. Patients diagnosed with IBD based on data from clinics, radiology, endoscopy, and histology were included in the study. The protocol was approved by the ethics commission of Zhongnan Hospital. The subjects were asked to complete a questionnaire regarding environmental exposure, dietary habits, and antibiotic, probiotic, and drug use. The subjects were required to be adults with an unrestricted diet. Subjects with positive stool cultures of pathogens who were taking antibiotic or probiotic treatments or colon-cleansing products in the 3 months before sampling were excluded. Next, the subjects were invited to participate in the study and provided informed consent. They were asked to expel stool onto a sterile petri dish directly before bowel preparation, and a fresh stool sample was collected on-site and immediately was transferred to the laboratory with an ice box within 1 h and stored at −80°C for further analysis. Subsequently, a magnesium sulfate solution and water were used for bowel preparation, colonoscopy was followed by video endoscopy, and biopsy specimens were taken from different gut locations. The collection procedure for the fecal and biopsy specimens was accomplished within 24 h.
The fecal and biopsy specimens were collected from 76 and 63 subjects, respectively (Table 1). Active CD and active UC were defined as a CD activity index of >150 and a UC activity index of >3 (20, 21), respectively. Meanwhile, 21 healthy controls were matched for stool samples and biopsied tissues, and there were also 8 patients with active CD, 3 patients with CD in remission, 16 patients with active UC, and 4 patients with UC in remission.
TABLE 1.
Numbers of specimens by patient group, disease status, and specimen type
| Patient group | Disease status | Biopsy location | No. of specimens: |
No. of matched biopsy/fecal specimens | |
|---|---|---|---|---|---|
| Biopsy | Feces | ||||
| CD | Active | Ileum | 9 | 15 | 8 |
| Colon | 12 | ||||
| Rectum | 12 | ||||
| Quiescent | Ileum | 2 | 6 | 3 | |
| Colon | 3 | ||||
| Rectum | 3 | ||||
| UC | Active | Colon | 22 | 29 | 16 |
| Rectum | 22 | ||||
| Quiescent | Colon | 5 | 5 | 4 | |
| Rectum | 5 | ||||
| HC | Control | Ileum | 21 | 21 | 21 |
| Colon | 21 | ||||
| Rectum | 21 | ||||
DNA extraction from biopsy and fecal specimen materials.
DNA was extracted from 200 mg of feces. Briefly, 200 mg of stool was added to a 2-ml microcentrifuge tube prefilled with 300 mg of 0.1-mm glass beads (Sigma, USA) and incubated on ice until the addition of 1.4 ml stool lysis (ASL) buffer from the QIAamp DNA stool minikit (Qiagen, Germany). The samples were immediately subjected to bead beating (45 s; speed, 6.5 m/s) twice using a FastPrep-24 machine (MP Biomedicals, USA) before heat and chemical lysis at 95°C for 5 min. The subsequent steps of DNA extraction were performed according to the QIAamp kit protocol for pathogen detection. The biopsy specimen DNA was extracted using the QIAamp DNA minikit (Qiagen, Germany) according to the manufacturer's instructions, with an additional bead-beating step (45 s; speed, 6.5, performed twice) using a FastPrep-24 at the beginning of the protocol. The extracted DNA was stored at −80°C for further analysis.
Amplification by conventional PCR to check primer specificity.
A Bio-Rad PCR machine (Bio-Rad, USA) was used for conventional PCR to check primer specificity. The primers (Table 2) were purchased from ShengGong BioTech (ShengGong, China). PCR consisted of 35 cycles, with an initial DNA denaturation step at 95°C (30 s), followed by gradient annealing temperature (30 s) and elongation at 72°C (45 s). The procedure was completed with a final elongation step at 72°C (10 min). The determinations of optimum temperature were performed using a MyCycler gradient PCR machine, which was adjusted for various temperature ranges (Bio-Rad, USA).
TABLE 2.
Group- and species-specific 16S rRNA primers used
| Target | Primer direction | Sequence (5′ to 3′) | Annealing Tm (°C) | Product size (bp) | Reference no. |
|---|---|---|---|---|---|
| All bacteria | Forward | ACTCCTACGGGAGGCAGCAGT | 61 | 200 | 44 |
| Reverse | GTATTACCGCGGCTGCTGGCAC | ||||
| Bacteroides | Forward | GTCAGTTGTGAAAGTTTGC | 61.5 | 127 | 45 |
| Reverse | CAATCGGGAGTTCTTCGTG | ||||
| Bifidobacterium | Forward | AGGGTTCGATTCTGCTCAG | 62 | 156 | 45 |
| Reverse | CATCCGGCATTACCACCC | ||||
| C. coccoides group (XIVa) | Forward | AAATGACGGTACCTGACTAA | 60.7 | 440 | 46 |
| Reverse | CTTTGAGTTTCATTCTTGCGAA | ||||
| C. leptum group (IV) | Forward | GTTGACAAAACGGAGGAAGG | 60 | 245 | 38 |
| Reverse | GACGGGCGGTGTGTACAA | ||||
| F. prausnitzii | Forward | AGATGGCCTCGCGTCCGA | 61.5 | 199 | 34 |
| Reverse | CCGAAGACCTTCTTCCTCC | ||||
| Lactobacillus groupb | Forward | GCAGCAGTAGGGAATCTTCCA | 61.5 | 340 | 47 |
| Reverse | GCATTYCACCGCTACACATG | ||||
| E. coli | Forward | GTTAATACCTTTGCTCATTGA | 61 | 340 | 46 |
| Reverse | ACCAGGGTATCTAATCCTGTT | ||||
| β-Globin gene | Forward | CAACTTCATCCACGTTCACC | *a | 268 | 28 |
| Reverse | GAAGAGCCAAGGACAGGTAC |
Based on detected bacterial Tm.
Lactobacillus group PCR primers used to amplify bacteria, including the Lactobacillus, Pediococcus, Leuconostoc, and Weissella group of lactic acid bacteria (LAB).
Real-time PCR.
Bacterial 16S rRNA gene copies were quantified in mucosal tissue and feces using an iCycler real-time PCR detection system (Bio-Rad, USA). Briefly, standard curves were constructed with a 10-fold dilution series of amplified bacterial 16S rRNA genes from the reference strains. To determine the influence of biopsy specimen sizes of mucosal tissue, the human cell numbers were quantified using primers specific for the β-globin gene to determine the total number of mucosa-associated bacteria in the biopsy specimens. To reduce the quantitative error of the detected bacteria and to characterize the changes in bacterial copies, the abundance of 16S rRNA gene copies was calculated from standard curves, and specific bacterial groups were expressed as a percentage of the total bacteria determined by the universal primers. Each reaction was performed in duplicate and repeated three times. The amplifications were performed in a final reaction volume of 20 μl containing 2× SYBR mix (GeneCopoeia, USA), 0.4 μl of each primer at a final concentration of 0.2 μM, 0.4 μl of ROX (5-carboxy-X-rhodamine) reference dye, 2 μl of bacterial DNA, and ultrapure water to 20 μl. The amplification protocol consisted of one cycle of 95°C for 10 min, followed by 40 cycles of 95°C for 10 s, annealing temperature for 30 s, and 72°C elongation for 30 s. The fluorescent products were detected at the last step of each cycle. Melting curve analysis was performed from the annealing temperatures to 95°C at an increase of 0.5°C per 10 s after amplification to monitor the target PCR product specificity and fidelity.
Statistical analysis.
Data analysis was conducted using SPSS 17.0. Comparisons were made using Student's t test or a one-way analysis of variance for variables with normal distributions. For nonnormal distributions, the Mann-Whitney U test was used for comparisons between groups, and the Kruskal-Wallis method was used to compare more than two groups. P values of <0.05 were considered statistically significant. The total bacterial counts (CFU/g) of each bacterium in the fecal samples were log transformed (log10 CFU) for statistical analysis. Specific bacterial counts were expressed as a percentage of the total bacterial counts of each sample.
RESULTS
Clinical characteristics.
The demographic and clinical characteristics of the IBD patients are shown in Tables S1 and S2 in the supplemental material.
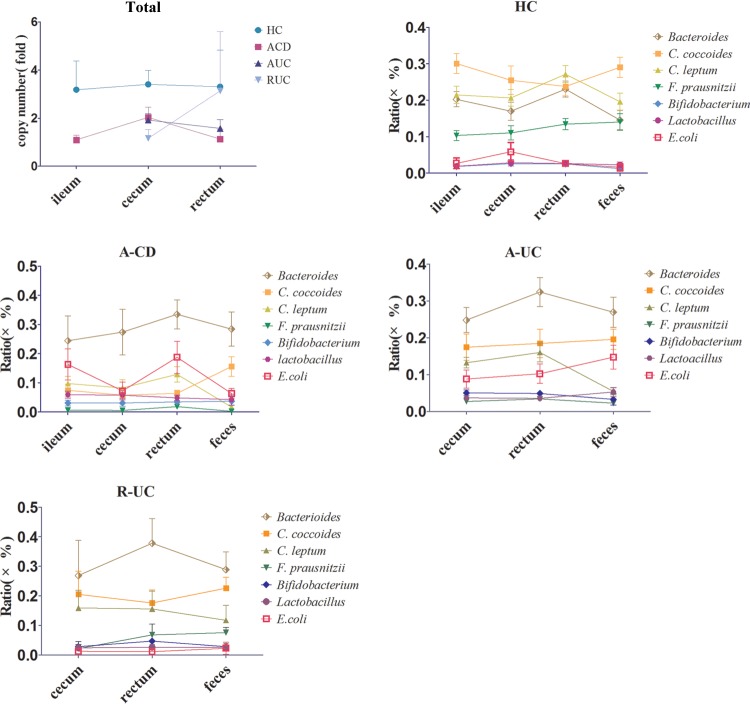
Percent variation of bacteria in feces.
The average bacterial quantifications of feces in each group are summarized in Table 3. The comparisons of the fecal bacteria in all groups are shown in Fig. 1a and b. The total numbers of bacteria in the fecal samples were similar between the healthy control (HC), CD, and UC patients, and no significant differences were observed.
TABLE 3.
Quantification of bacteria in fecal microbiota
| Disease group | % (mean ±SD) of the indicated bacterial species/group: |
||||||
|---|---|---|---|---|---|---|---|
| Bacteroides | C. coccoides | C. leptum | F. prausnitzii | Bifidobacterium | Lactobacillus | E. coli | |
| HC | 14.566 ± 12.161 | 29.048 ± 12.750 | 19.618 ± 10.558 | 14.023 ± 10.593 | 1.244 ± 2.059 | 2.260 ± 3.588 | 1.597 ± 4.483 |
| A-CD | 28.444 ± 22.850 | 15.593 ± 12.977 | 1.703 ± 2.164 | 0.260 ± 0.575 | 1.986 ± 3.442 | 4.268 ± 7.073 | 6.344 ± 6.505 |
| R-CD | 23.957 ± 19.389 | 17.738 ± 10.466 | 5.843 ± 7.541 | 4.266 ± 6.078 | 1.575 ± 1.673 | 2.324 ± 2.537 | 5.676 ± 5.687 |
| A-UC | 26.958 ± 22.101 | 19.583 ± 14.767 | 5.466 ± 5.106 | 2.248 ± 2.860 | 2.943 ± 7.410 | 3.315 ± 3.431 | 14.742 ± 17.474 |
| R-UC | 28.892 ± 13.472 | 22.617 ± 8.247 | 11.784 ± 11.357 | 7.600 ± 3.795 | 2.819 ± 3.326 | 2.615 ± 2.630 | 2.310 ± 4.607 |
FIG 1.

(a) Quantification of total bacteria in feces; (b) quantification of dominant bacteria in feces. HC, healthy control; ACD, active Crohn's disease; RCD, Crohn's disease in remission; AUC, active ulcerative colitis; RUC, ulcerative colitis in remission.*, P < 0.05; **, P < 0.0001.
Interestingly, we unexpectedly observed an increase of Bifidobacterium and the Lactobacillus group in both the active CD (A-CD) and active UC (A-UC) patients, but neither of these populations was significantly different from those in the HCs. However, the proportion of Bifidobacterium was higher in A-UC patients than in A-CD patients. The proportions of Bifidobacterium and the Lactobacillus group were decreased in quiescent-IBD patients compared to active-IBD patients.
We also observed a trend of increased Bacteroides organisms in A-CD and A-UC patients compared to healthy controls, but no significant differences were observed. Furthermore, the proportion of Bacteroides was lower in quiescent-IBD patients than in active-IBD patients. The Clostridium coccoides group decreased significantly in the feces of both A-CD (P = 0.004) and A-UC patients (P = 0.015). The Clostridium leptum group, another main group of the Firmicutes phylum, was decreased in A-CD (P < 0.0001) and A-UC (P < 0.0001) patients and decreased in R-CD patients (P = 0.036) compared to in the HCs. We found that the decreased proportion of C. leptum was higher in A-CD patients than in A-UC patients (P = 0.014). Although the proportions of C. coccoides and C. leptum in feces showed a rising trend in patients with quiescent IBD, there was no significant difference between quiescent IBD and active IBD patients. F. prausnitzii, a representative bacterium of the C. leptum group, was decreased both in patients with A-CD (P < 0.0001) and in those with A-UC (P = 0.001). The decrease in the proportion of F. prausnitzii in patients with A-CD was significant compared with that in A-UC patients (P = 0.01). F. prausnitzii was increased in quiescent IBD patients, but no significant differences were observed compared with patients with active IBD. E. coli, the most abundant bacterium in the Gammaproteobacteria, was increased in both CD and UC patients. The proportion of E. coli increased in active-CD (P = 0.005) and quiescent-CD (P = 0.026) patients compared to that in the HCs. Additionally, the proportion of E. coli increased in active-UC patients (P = 0.001) compared to HCs, and the proportion decreased in quiescent-UC (P = 0.05) patients compared with active-UC patients. Moreover, we found that the increased proportion of E. coli was more striking in the active-UC than in the active-CD patients (P = 0.027).
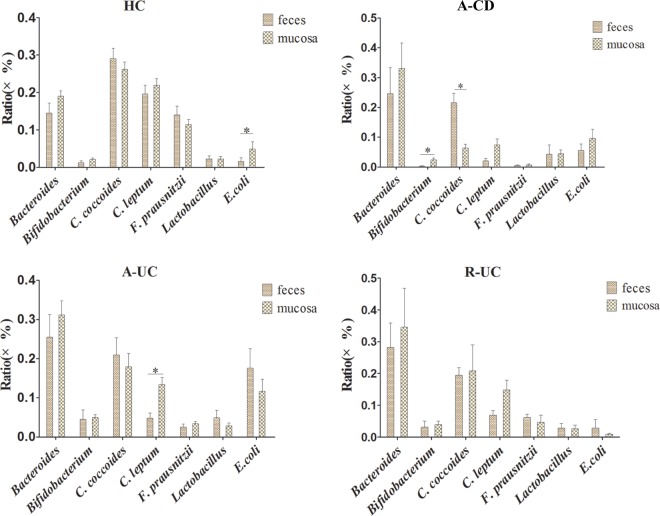
Percent variation of bacteria in different gut locations.
To determine whether the percentages of commensals varied significantly in the different gut locations, we compared the bacterial proportions among the three biopsied locations (Fig. 2). The total number of mucosa-associated bacteria in the healthy controls was consistent across the different biopsied locations. The percentages of detected bacteria were almost uniformly distributed along the colon in the healthy controls. The percentages of detected bacteria were also consistent across the different biopsied locations in patients with A-CD. Interestingly, the same results were observed in patients with A-UC and UC in remission (R-UC), in whom the bacteria were almost uniformly distributed along the colon, regardless of whether the area was inflamed.
FIG 2.
Ratios of bacteria in different gut locations and feces. Shown in the upper left graph is the total number of mucosa-associated bacteria at different biopsied locations in different groups. The other five graphs show the dominant probiotic ratios in the feces and different gut locations.
Percent variation of bacteria in mucosal biopsy specimens.
The average bacterial quantifications of the biopsy specimens in each group are summarized in Table 4. The results were also compared to those for HCs. In the present study, we observed a decreased trend in total mucosa-associated bacteria in patients with CD and UC compared to in the HCs, but no significant difference was observed. Because the biopsied sample size of the CD patients in remission (R-CD) group was limited, we did not compare it with that of the healthy controls. A comparison of the bacteria found in the biopsy specimens from all groups is shown in Fig. 3a and b.
TABLE 4.
Quantification of bacteria in mucosal microbiota
| Disease group | % (mean ±SD) of the indicated bacterial species/group: |
||||||
|---|---|---|---|---|---|---|---|
| Bacteroides | C. coccoides | C. leptum | F. prausnitzii | Bifidobacterium | Lactobacillus | E. coli | |
| HC | 19.030 ± 6.599 | 26.182 ± A.980 | 21.957 ± 8.089 | 11.415 ± 6.085 | 2.147 ± 1.514 | 2.262 ± 2.887 | 4.872 ± 8.83 |
| A-CD | 32.263 ± 22.400 | 6.286 ± 3.514 | 8.578 ± 7.604 | 0.817 ± 0.976 | 2.793 ± 2.600 | 3.420 ± 2.169 | 11.666 ± 8.796 |
| A-UC | 28.393 ± 15.356 | 19.045 ± 14.106 | 13.326 ± 6.679 | 2.844 ± 2.243 | 4.653 ± 2.889 | 3.267 ± 2.590 | 9.831 ± 10.984 |
| R-UC | 31.477 ± 22.296 | 19.542 ± 14.444 | 12.754 ± 7.027 | 3.849 ± 4.238 | 3.527 ± 1.981 | 2.349 ± 2.008 | 0.875 ± 0.459 |
FIG 3.
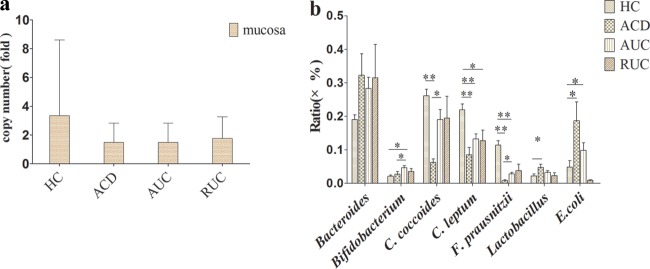
(a) Total mucosa-associated bacteria in different groups. (b) Quantification of dominant bacteria in biopsy specimens. *, P < 0.05; **, P < 0.0001.
Bifidobacterium was increased in patients with A-UC (P = 0.001) compared to in the HCs, and the increased proportion of Bifidobacterium in the biopsy specimens was higher in A-UC than A-CD patients (P = 0.032). Again, the Lactobacillus group unexpectedly presented a significant increase in patients with A-CD (P = 0.036) compared to in the HCs, and although the increased proportion of the Lactobacillus group was higher in patients with A-CD than A-UC, no significant difference was observed. We also observed a rising trend in patients with A-UC, but this trend was not significant. In contrast, the percentages of Bifidobacterium and the Lactobacillus group presented a decreasing trend in patients with quiescent UC, but no significant differences were observed.
We observed a trend of increased Bacteroides in the biopsy specimens from patients with A-CD and A-UC compared to in healthy controls, but no significant difference was observed. The proportion of the C. coccoides group in biopsy specimens was decreased in A-CD patients (P < 0.0001) compared to in the HCs, while no significant decrease was found in patients with A-UC. The decreased proportion of the C. coccoides group was more striking in patients with A-CD compared to A-UC (P = 0.003). The C. leptum group was decreased in patients with A-CD (P < 0.0001) and A-UC (P < 0.0001) compared to HCs, and the decreased proportion was higher in A-CD than A-UC patients, although no significant difference was observed. We observed a significant decrease in the C. leptum group in patients with R-UC (P = 0.016) compared to in the HCs. F. prausnitzii was also decreased in patients with A-CD (P < 0.0001) and A-UC (P < 0.0001) compared to in the HCs, and the decreased proportion of F. prausnitzii was significantly higher in patients with A-CD than in patients with A-UC (P = 0.006). Both the C. coccoides group and F. prausnitzii exhibited a rising trend in patients with quiescent UC compared to those with active UC, but no significant difference was observed. Additionally, E. coli significantly increased in the biopsy specimens in IBD patients. The proportion of E. coli was at a high level in patients with active CD (P = 0.018) compared to in the HCs. Moreover, E. coli also increased in active UC patients (P = 0.016) compare to in the HCs. Although the proportion of E. coli was higher in active CD than in active UC patients, no significant differences were was observed.
Comparison of the ratio between fecal and biopsy specimens.
As the detected bacteria in the intestinal mucosal biopsy specimens showed similar proportions regardless of the biopsied location, we determined whether the proportion was different between biopsy and fecal specimens (Fig. 4). The proportion of E. coli was significantly higher in the biopsy specimens (P = 0.002) than in fecal samples in 21 healthy controls, but no significant differences were observed in the other comparisons. In eight paired A-CD cases, the proportion of Bifidobacterium was increased in biopsy specimens of the active CD patients (P = 0.012) compared to in the fecal samples. The C. coccoides group showed a decrease in the biopsy specimens of A-CD patients (P = 0.003) compared to the fecal samples, but this result was not found in the UC patients. Conversely, the C. leptum group and its representative bacterium F. prausnitzii were decreased in the fecal samples of A-CD patients compared to in the biopsy specimens, but no significant difference was observed. This finding was partly due to the small number of paired cases. However, the C. leptum group showed a decrease in the fecal samples of patients with A-UC (P = 0.001) compared to biopsy specimens, but not in R-UC patients.
FIG 4.
Comparison of the ratios in paired fecal and biopsy samples. *, P < 0.05; **, P < 0.0001.
DISCUSSION
In the present study, we investigated mucosa-associated commensal bacteria, as they adhere strictly to the epithelium and can provide access to the mucosa-associated microbiota of the subjects, which may play a more critical role than fecal microbes in IBD pathogenesis (22). In our study, we found that the proportions of detected mucosa-associated bacteria in healthy gastrointestinal tracts were uniformly distributed along the colon, which was in accordance with the findings from a previous study (23, 24). The total bacterial counts and detected bacteria were similar across the different gut locations in the colon, regardless of the disease state, which was in line with some previous data (24, 25), although reports with conflicts data have also been published (26–30).
As common probiotics, Bifidobacterium and Lactobacillus have received considerable attention. Surprisingly, the proportion of Bifidobacterium was found to be increased in patients with active IBD. These data were partly in agreement with previous data (17), although conflicting data have also been published (31). Comparatively, the proportion of Bifidobacterium was reduced in quiescent CD and UC patients. However, the quantitative PCR (qPCR) results had good agreement only with 454 pyrosequencing in the fecal samples. Moran et al. (32) reported that germ-free interleukin-10-deficient (IL-10−/−) mice administered Bifidobacterium animalis had marked duodenal and mild colonic inflammation and immune responses. Moreover, Medina et al. (33) showed that B. longum diverted immune responses toward a proinflammatory or regulatory profile, consequently producing different effects. In contrast, another study demonstrated that oral Bifidobacterium administration prevented intestinal inflammation through the induction of intestinal IL-10-producing Tr1 cells and ameliorated colitis in immunocompromised mice (35).
In the current study, the Lactobacillus group PCR primers used to amplify bacteria belong to the Lactobacillus, Pediococcus, Leuconostoc, and Weissella groups of lactic acid bacteria (LAB) (25). Unexpectedly, we observed that the Lactobacillus group presented marked increases in patients with active IBD, despite no significant differences in those with active UC. However, in patients with quiescent IBD, the proportion of the Lactobacillus group was similar to that of the HCs in both the fecal and biopsy samples. Because it was difficult to design genus-specific primers to definitively discriminate Lactobacillus, Pediococcus, Leuconostoc, and Weissella group organisms, we quantified the Lactobacillus group with the genus primer, and the species of the Lactobacillus genus are phylogenetically diverse, with >100 species documented to date (36). This result may suggest that other species of the Lactobacillus genus or LAB-producing bacteria were also increased in active-IBD patients. A previous study showed that Lactobacillus can secrete lactocepin and exert anti-inflammatory effects by selectively degrading proinflammatory chemokines (12). Mileti et al. (37) found that Lactobacillus paracasei displayed a delay in the development of colitis and a decreased severity of disease but that L. plantarum and L. rhamnosus GG exacerbated the development of dextran sodium sulfate (DSS)-induced colitis. In contrast, Tsilingiri et al. (39) found that L. plantarum induced an inflammatory response in the healthy tissue cultured ex vivo at the end of incubation that resembled the response induced by Salmonella. Moreover, L. paracasei, L. plantarum, and L. rhamnosus GG were detrimental in the inflamed tissue derived from IBD patients cultured ex vivo, whereas the supernatant from the culture system of L. paracasei directly acted on the tissue and downregulated the proinflammatory activities of the existing leukocytes (39). It remains to be determined which species of Lactobacillus group is increased in patients during the active phase of IBD. Thus, the effects of Bifidobacterium and Lactobacillus in the gut lumen of active IBD patients are of importance and should be determined.
Although the bacteria of the Firmicutes phylum presented a varied degree of decline, the decrease in proportion was greater in patients with A-CD than in patients with A-UC. Moreover, we found that the C. coccoides group, which comprises Clostridium cluster XIVa, including members of other genera, such as Coprococcus, Eubacterium, Lachnospira, and Ruminococcus (38), was more deficient in the biopsy specimens of the A-CD patients than in the fecal samples, and that the reduced proportion was higher than that of C. leptum in the biopsy specimens. In contrast, previous studies reported that F. prausnitzii within the C. leptum group was strikingly low in mucosa-associated microbiotas (40, 41). Based on these results, it is tantalizing to hypothesize that the C. coccoides group was more effective in adhering to the mucosal surface and that the decrease in the C. coccoides group in both the fecal and biopsy specimens of active CD patients, especially with a strikingly decreased proportion in the biopsy specimens, was specific to CD in genetically susceptible individuals.
In our study, we found that the representative bacterium of the C. leptum group, F. prausnitzii, nearly disappeared in both different gut locations and in feces but increased in patients with quiescent IBD. Previous reports showed that F. prausnitzii produces formate and butyrate and that its fermented product d-lactate provides energy for colonic epithelial cells and plays an important role in epithelial barrier integrity and immune modulation (41, 42). Additionally, Sokol et al. (16) demonstrated that F. prausnitzii exhibits a butyrate-independent anti-inflammatory effect in IBD models. Interestingly, however, Hansen et al. (43) found that F. prausnitzii was increased in pediatric CD patients at the onset of disease, but not in patients with UC, suggesting a more dynamic role for this organism in the development of IBD. Moreover, Willing et al. (19) reported an increase in F. prausnitzii in colonic CD in twins with inflammatory bowel disease but a decrease in F. prausnitzii in ileal CD. The biopsy specimens in the study by Hansen et al. were taken from a single site: from the distal colon in controls, or from the most distal inflamed site in IBD. The biggest difference in their data was the inclusion of subjects regardless of whether they accepted the conventional IBD treatment. Therefore, pharmacological treatment may be a potential confounder in the microbial study of IBD. Previous data showed that the abundance of F. prausnitzii decreased strikingly in patients with ileal CD (28, 40), and Sokol et al. (16) also found that F. prausnitzii presented a reduction in resected ileal Crohn mucosa and was associated with endoscopic recurrence at 6 months. However, our data show that F. prausnitzii was consistent at different gut locations in patients with CD. This may be caused by various lifestyle and dietary habits. Our study was focused on the populations of central China, most of whom prefer a high-fiber diet, according to the results of our questionnaire. Additionally, F. prausnitzii represented a higher average proportion (11.4%) in the biopsy specimens of the HCs, and organisms with such high proportions may display varied functions in different mucosal sites. This remains an interesting pursuit for further research.
This study design was based on the analysis of bacterial 16S rRNA genes and reflected the gene copy number rather than true cell counts. Also, the rRNA gene analysis did not reflect the functional changes in gastrointestinal tract microbes, such as enhanced virulence, mucosal adherence, and invasion, which do not influence the relative proportions of species in the microbiota. Therefore, further studies should be conducted on the functions of commensal bacteria.
We identified specific commensal bacteria that were significantly increased or decreased in individuals with CD and UC. The butyrate-producing bacteria of Clostridium clusters IV and XIVa were found to be decreased; in particular, F. prausnitzii was decreased in IBD patients. However, Bifidobacterium and the Lactobacillus group were increased in patients with active IBD. Thus, more attention should be paid to butyrate-producing bacteria, and Bifidobacterium and Lactobacillus could then be used more cautiously as probiotics in patients during the acute phase of IBD.
Supplementary Material
ACKNOWLEDGMENTS
We thank all the subjects who volunteered to participate in this study.
This study was supported by Hubei Science & Technology Bureau (grant no. 303131796), the Fundamental Research Funds of the Central University of Ministry of Education of China (grant no. 2012303020201 and 201130302020004), and the National Support Project of the Ministry of Science & Technology of China (grant no. 2012BAI06B03).
We declare no conflicts of interest.
Footnotes
Published ahead of print 13 November 2013
Supplemental material for this article may be found at http://dx.doi.org/10.1128/JCM.01500-13.
REFERENCES
- 1.Chassaing B, Darfeuille-Michaud A. 2011. The commensal microbiota and enteropathogens in the pathogenesis of inflammatory bowel diseases. Gastroenterology 140:1720–1728. 10.1053/j.gastro.2011.01.054 [DOI] [PubMed] [Google Scholar]
- 2.Sartor RB. 2006. Mechanisms of disease: pathogenesis of Crohn's disease and ulcerative colitis. Nature Clin. Pract. Gastroenterol. Hepatol. 3:390–407. 10.1038/ncpgasthep0528 [DOI] [PubMed] [Google Scholar]
- 3.Sartor RB. 2008. Microbial influences in inflammatory bowel diseases. Gastroenterology 134:577–594. 10.1053/j.gastro.2007.11.059 [DOI] [PubMed] [Google Scholar]
- 4.Neish AS. 2009. Microbes in gastrointestinal health and disease. Gastroenterology 136:65–80. 10.1053/j.gastro.2008.10.080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Miele E, Pascarella F, Giannetti E, Quaglietta L, Baldassano RN, Staiano A. 2009. Effect of a probiotic preparation (VSL#3) on induction and maintenance of remission in children with ulcerative colitis. Am. J. Gastroenterol. 104:437–443. 10.1038/ajg.2008.118 [DOI] [PubMed] [Google Scholar]
- 6.Tursi A, Brandimarte G, Papa A, Giglio A, Elisei W, Giorgetti GM, Forti G, Morini S, Hassan C, Pistoia MA, Modeo ME, Rodino' S, D'Amico T, Sebkova L, Sacca' N, Di Giulio E, Luzza F, Imeneo M, Larussa T, Di Rosa S, Annese V, Danese S, Gasbarrini A. 2010. Treatment of relapsing mild-to-moderate ulcerative colitis with the probiotic VSL#3 as adjunctive to a standard pharmaceutical treatment: a double-blind, randomized, placebo-controlled study. Am. J. Gastroenterol. 105:2218–2227. 10.1038/ajg.2010.218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kruis W, Fric P, Pokrotnieks J, Lukás M, Fixa B, Kascák M, Kamm MA, Weismueller J, Beglinger C, Stolte M, Wolff C, Schulze J. 2004. Maintaining remission of ulcerative colitis with the probiotic Escherichia coli Nissle 1917 is as effective as with standard mesalazine. Gut 53:1617–1623. 10.1136/gut.2003.037747 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kato K, Mizuno S, Umesaki Y, Ishii Y, Sugitani M, Imaoka A, Otsuka M, Hasunuma O, Kurihara R, Iwasaki A, Arakawa Y. 2004. Randomized placebo-controlled trial assessing the effect of bifidobacteria-fermented milk on active ulcerative colitis. Aliment. Pharmacol. Ther. 20:1133–1141. 10.1111/j.1365-2036.2004.02268.x [DOI] [PubMed] [Google Scholar]
- 9.Zocco MA, dal Verme LZ, Cremonini F, Piscaglia AC, Nista EC, Candelli M, Novi M, Rigante D, Cazzato IA, Ojetti V, Armuzzi A, Gasbarrini G, Gasbarrini A. 2006. Efficacy of Lactobacillus GG in maintaining remission of ulcerative colitis. Aliment. Pharmacol. Ther. 23:1567–1574. 10.1111/j.1365-2036.2006.02927.x [DOI] [PubMed] [Google Scholar]
- 10.Zakostelska Z, Kverka M, Klimesova K, Rossmann P, Mrazek J, Kopecny J, Hornova M, Srutkova D, Hudcovic T, Ridl J, Tlaskalova-Hogenova H. 2011. Lysate of probiotic Lactobacillus casei DN-114 001 ameliorates colitis by strengthening the gut barrier function and changing the gut microenvironment. PLoS One 6:e27961. 10.1371/journal.pone.0027961 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Patel RM, Myers LS, Kurundkar AR, Maheshwari A, Nusrat A, Lin PW. 2012. Probiotic bacteria induce maturation of intestinal claudin 3 expression and barrier function. Am. J. Pathol. 180:626–635. 10.1016/j.ajpath.2011.10.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.von Schillde MA, Hörmannsperger G, Weiher M, Alpert CA, Hahne H, Bäuerl C, van Huynegem K, Steidler L, Hrncir T, Pérez-Martínez G, Kuster B, Haller D. 2012. Lactocepin secreted by Lactobacillus exerts anti-inflammatory effects by selectively degrading proinflammatory chemokines. Cell Host Microbe 11:387–396. 10.1016/j.chom.2012.02.006 [DOI] [PubMed] [Google Scholar]
- 13.Hoermannsperger G, Clavel T, Hoffmann M, Reiff C, Kelly D, Loh G, Blaut M, Hölzlwimmer G, Laschinger M, Haller D. 2009. Post-translational inhibition of IP-10 secretion in IEC by probiotic bacteria: impact on chronic inflammation. PLoS One 4:e4365. 10.1371/journal.pone.0004365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mohamadzadeh M, Pfeiler EA, Brown JB, Zadeh M, Gramarossa M, Managlia E, Bere P, Sarraj B, Khan MW, Pakanati KC, Ansari MJ, O'Flaherty S, Barrett T, Klaenhammer TR. 2011. Regulation of induced colonic inflammation by Lactobacillus acidophilus deficient in lipoteichoic acid. Proc. Natl. Acad. Sci. U. S. A. 108:4623–4630. 10.1073/pnas.1005066107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schmidt EG, Claesson MH, Jensen SS, Ravn P, Kristensen NN. 2010. Antigen-presenting cells exposed to Lactobacillus acidophilus NCFM, Bifidobacterium bifidum BI-98, and BI-504 reduce regulatory T cell activity. Inflamm. Bowel Dis. 16:390–400. 10.1002/ibd.21068 [DOI] [PubMed] [Google Scholar]
- 16.Sokol H, Pigneur B, Watterlot L, Lakhdari O, Bermúdez-Humarán LG, Gratadoux JJ, Blugeon S, Bridonneau C, Furet JP, Corthier G, Grangette C, Vasquez N, Pochart P, Trugnan G, Thomas G, Blottière HM, Doré J, Marteau P, Seksik P, Langella P. 2008. Faecalibacterium prausnitzii is an anti-inflammatory commensal bacterium identified by gut microbiota analysis of Crohn disease patients. Proc. Natl. Acad. Sci. U. S. A. 105:16731–16736. 10.1073/pnas.0804812105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Scanlan PD, Shanahan F, O'Mahony C, Marchesi JR. 2006. Culture-independent analyses of temporal variation of the dominant fecal microbiota and targeted bacterial subgroups in Crohn's disease. J. Clin. Microbiol. 44:3980–3988. 10.1128/JCM.00312-06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Seksik P, Rigottier-Gois L, Gramet G, Sutren M, Pochart P, Marteau P, Jian R, Doré J. 2003. Alterations of the dominant faecal bacterial groups in patients with Crohn's disease of the colon. Gut 52:237–242. 10.1136/gut.52.2.237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Willing BP, Dicksved J, Halfvarson J, Andersson AF, Lucio M, Zheng Z, Järnerot G, Tysk C, Jansson JK, Engstrand L. 2010. A pyrosequencing study in twins shows that gastrointestinal microbial profiles vary with inflammatory bowel disease phenotypes. Gastroenterology 139:1844–1854. 10.1053/j.gastro.2010.08.049 [DOI] [PubMed] [Google Scholar]
- 20.Sutherland LR, Martin F, Greer S, Robinson M, Greenberger N, Saibil F, Martin T, Sparr J, Prokipchuk E, Borgen L. 1987. 5-Aminosalicylic acid enema in the treatment of distal ulcerative colitis, proctosigmoiditis, and proctitis. Gastroenterology 92:1894–1898 [DOI] [PubMed] [Google Scholar]
- 21.Best WR, Becktel JM, Singleton JW, Kern F., Jr 1976. Development of a Crohn's disease activity index. National Cooperative Crohn's Disease Study. Gastroenterology 70:439–444 [PubMed] [Google Scholar]
- 22.Willing B, Halfvarson J, Dicksved J, Rosenquist M, Järnerot G, Engstrand L, Tysk C, Jansson JK. 2009. Twin studies reveal specific imbalances in the mucosa-associated microbiota of patients with ileal Crohn's disease. Inflamm. Bowel Dis. 15:653–660. 10.1002/ibd.20783 [DOI] [PubMed] [Google Scholar]
- 23.Round JL, Mazmanian SK. 2009. The gut microbiota shapes intestinal immune responses during health and disease. Nat. Rev. Immunol. 9:313–323. 10.1038/nri2515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zoetendal EG, von Wright A, Vilpponen-Salmela T, Ben-Amor K, Akkermans AD, de Vos WM. 2002. Mucosa-associated bacteria in the human gastrointestinal tract are uniformly distributed along the colon and differ from the community recovered from feces. Appl. Environ. Microbiol. 68:3401–3407. 10.1128/AEM.68.7.3401-3407.2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Walter J, Hertel C, Tannock GW, Lis CM, Munro K, Hammes WP. 2001. Detection of Lactobacillus, Pediococcus, Leuconostoc, and Weissella species in human feces by using group-specific PCR primers and denaturing gradient gel electrophoresis. Appl. Environ. Microbiol. 67:2578–2585. 10.1128/AEM.67.6.2578-2585.2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lepage P, Seksik P, Sutren M, de la Cochetière MF, Jian R, Marteau P, Doré J. 2005. Biodiversity of the mucosa-associated microbiota is stable along the distal digestive tract in healthy individuals and patients with IBD. Inflamm. Bowel Dis. 11:473–480. 10.1097/01.MIB.0000159662.62651.06 [DOI] [PubMed] [Google Scholar]
- 27.Swidsinski A, Weber J, Loening-Baucke V, Hale LP, Lochs H. 2005. Spatial organization and composition of the mucosal flora in patients with inflammatory bowel disease. J. Clin. Microbiol. 43:3380–3389. 10.1128/JCM.43.7.3380-3389.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Walker AW, Sanderson JD, Churcher C, Parkes GC, Hudspith BN, Rayment N, Brostoff J, Parkhill J, Dougan G, Petrovska L. 2011. High-throughput clone library analysis of the mucosa-associated microbiota reveals dysbiosis and differences between inflamed and noninflamed regions of the intestine in inflammatory bowel disease. BMC Microbiol. 11:7. 10.1186/1471-2180-11-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kleessen B, Kroesen AJ, Buhr HJ, Blaut M. 2002. Mucosal and invading bacteria in patients with inflammatory bowel disease compared with controls. Scand. J. Gastroenterol. 37:1034–1041. 10.1080/003655202320378220 [DOI] [PubMed] [Google Scholar]
- 30.Swidsinski A, Ladhoff A, Pernthaler A, Swidsinski S, Loening-Baucke V, Ortner M, Weber J, Hoffmann U, Schreiber S, Dietel M, Lochs H. 2002. Mucosal flora in inflammatory bowel disease. Gastroenterology 122:44–54. 10.1053/gast.2002.30294 [DOI] [PubMed] [Google Scholar]
- 31.Mylonaki M, Rayment NB, Rampton DS, Hudspith BN, Brostoff J. 2005. Molecular characterization of rectal mucosa-associated bacterial flora in inflammatory bowel disease. Inflamm. Bowel Dis. 11:481–487. 10.1097/01.MIB.0000159663.62651.4f [DOI] [PubMed] [Google Scholar]
- 32.Moran JP, Walter J, Tannock GW, Tonkonogy SL, Sartor RB. 2009. Bifidobacterium animalis causes extensive duodenitis and mild colonic inflammation in monoassociated interleukin-10-deficient mice. Inflamm. Bowel Dis. 15:1022–1031. 10.1002/ibd.20900 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Medina M, Izquierdo E, Ennahar S, Sanz Y. 2007. Differential immunomodulatory properties of Bifidobacterium longum strains: relevance to probiotic selection and clinical applications. Clin. Exp. Immunol. 150:531–538. 10.1111/j.1365-2249.2007.03522.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Conte MP, Schippa S, Zamboni I, Penta M, Chiarini F, Seganti L, Osborn J, Falconieri P, Borrelli O, Cucchiara S. 2006. Gut-associated bacterial microbiota in paediatric patients with inflammatory bowel disease. Gut 55:1760–1767. 10.1136/gut.2005.078824 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jeon SG, Kayama H, Ueda Y, Takahashi T, Asahara T, Tsuji H, Tsuji NM, Kiyono H, Ma JS, Kusu T, Okumura R, Hara H, Yoshida H, Yamamoto M, Nomoto K, Takeda K. 2012. Probiotic Bifidobacterium breve induces IL-10-producing Tr1 cells in the colon. PLoS Pathog. 8:e1002714. 10.1371/journal.ppat.1002714 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Goh YJ, Klaenhammer TR. 2009. Genomic features of Lactobacillus species. Front. Biosci. (Landmark Ed.) 14:1362–1386. 10.2741/3313 [DOI] [PubMed] [Google Scholar]
- 37.Mileti E, Matteoli G, Iliev ID, Rescigno M. 2009. Comparison of the immunomodulatory properties of three probiotic strains of lactobacilli using complex culture systems: prediction for in vivo efficacy. PLoS One 4:e7056. 10.1371/journal.pone.0007056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Matsuki T, Watanabe K, Fujimoto J, Miyamoto Y, Takada T, Matsumoto K, Oyaizu H, Tanaka R. 2002. Development of 16S rRNA-gene-targeted group-specific primers for the detection and identification of predominant bacteria in human feces. Appl. Environ. Microbiol. 68:5445–5451. 10.1128/AEM.68.11.5445-5451.2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tsilingiri K, Barbosa T, Penna G, Caprioli F, Sonzogni A, Viale G, Rescigno M. 2012. Probiotic and postbiotic activity in health and disease: comparison on a novel polarised ex-vivo organ culture model. Gut 61:1007–1015. 10.1136/gutjnl-2011-300971 [DOI] [PubMed] [Google Scholar]
- 40.Frank DN, St Amand AL, Feldman RA, Boedeker EC, Harpaz N, Pace NR. 2007. Molecular-phylogenetic characterization of microbial community imbalances in human inflammatory bowel diseases. Proc. Natl. Acad. Sci. U. S. A. 104:13780–13785. 10.1073/pnas.0706625104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Martinez-Medina M, Aldeguer X, Gonzalez-Huix F, Acero D, Garcia-Gil LJ. 2006. Abnormal microbiota composition in the ileocolonic mucosa of Crohn's disease patients as revealed by polymerase chain reaction-denaturing gradient gel electrophoresis. Inflamm. Bowel Dis. 12:1136–1145. 10.1097/01.mib.0000235828.09305.0c [DOI] [PubMed] [Google Scholar]
- 42.Klampfer L, Huang J, Sasazuki T, Shirasawa S, Augenlicht L. 2003. Inhibition of interferon gamma signaling by the short chain fatty acid butyrate. Mol. Cancer Res. 1:855–862 [PubMed] [Google Scholar]
- 43.Hansen R, Russell RK, Reiff C, Louis P, McIntosh F, Berry SH, Mukhopadhya I, Bisset WM, Barclay AR, Bishop J, Flynn DM, McGrogan P, Loganathan S, Mahdi G, Flint HJ, El-Omar EM, Hold GL. 2012. Microbiota of de-novo pediatric IBD: increased Faecalibacterium prausnitzii and reduced bacterial diversity in Crohn's but not in ulcerative colitis. Am. J. Gastroenterol. 107:1913–1922. 10.1038/ajg.2012.335 [DOI] [PubMed] [Google Scholar]
- 44.Ramirez-Farias C, Slezak K, Fuller Z, Duncan A, Holtrop G, Louis P. 2009. Effect of inulin on the human gut microbiota: stimulation of Bifidobacterium adolescentis and Faecalibacterium prausnitzii. Br. J. Nutr. 101:541–550. 10.1017/S0007114508019880 [DOI] [PubMed] [Google Scholar]
- 45.Ahmed S, Macfarlane GT, Fite A, McBain AJ, Gilbert P, Macfarlane S. 2007. Mucosa-associated bacterial diversity in relation to human terminal ileum and colonic biopsy samples. Appl. Environ. Microbiol. 73:7435–7442. 10.1128/AEM.01143-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Santacruz A, Marcos A, Wärnberg J, Martí A, Martin-Matillas M, Campoy C, Moreno LA, Veiga O, Redondo-Figuero C, Garagorri JM, Azcona C, Delgado M, García-Fuentes M, Collado MC, Sanz Y, EVASYON Study Group 2009. Interplay between weight loss and gut microbiota composition in overweight adolescents. Obesity (Silver Spring) 17:1906–1915. 10.1038/oby.2009.112 [DOI] [PubMed] [Google Scholar]
- 47.Matsuki T, Watanabe K, Fujimoto J, Takada T, Tanaka R. 2004. Use of 16S rRNA gene-targeted group-specific primers for real-time PCR analysis of predominant bacteria in human feces. Appl. Environ. Microbiol. 70:7220–7228. 10.1128/AEM.70.12.7220-7228.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.