Abstract
Rift Valley fever (RVF) is a veterinary and human disease in Africa and the Middle East. The causative agent, RVF virus (RVFV), can be naturally transmitted by mosquito, direct contact, or aerosol. We sought to develop a nonhuman primate (NHP) model of severe RVF in humans to better understand the pathogenesis of RVF and to use for evaluation of medical countermeasures. NHP from four different species were exposed to aerosols containing RVFV. Both cynomolgus and rhesus macaques developed mild fevers after inhalation of RVFV, but no other clinical signs were noted and no macaque succumbed to RVFV infection. In contrast, both marmosets and African green monkeys (AGM) proved susceptible to aerosolized RVF virus. Fever onset was earlier with the marmosets and had a biphasic pattern similar to what has been reported in humans. Beginning around day 8 to day 10 postexposure, clinical signs consistent with encephalitis were noted in both AGM and marmosets; animals of both species succumbed between days 9 and 11 postexposure. Marmosets were susceptible to lower doses of RVFV than AGM. Histological examination confirmed viral meningoencephalitis in both species. Hematological analyses indicated a drop in platelet counts in both AGM and marmosets suggestive of thrombosis, as well as leukocytosis that consisted mostly of granulocytes. Both AGM and marmosets would serve as useful models of aerosol infection with RVFV.
INTRODUCTION
Rift Valley fever (RFV) is an endemic disease of both livestock and human populations in Sub-Saharan Africa and the Middle East (1–10). In livestock, RVF outbreaks are notable for fatalities among younger animals and “abortion storms” among pregnant females, with tremendous economic impact on the affected region (11, 12). Humans can become infected by mosquito bite or contact with infectious animal carcasses, resulting in exposure via either percutaneous, mucosal, or inhalational routes (13–15). While most humans develop an acute febrile disease that resolves in 1 to 2 weeks, a subset develop severe disease which is either hemorrhagic or encephalitic in nature. Approximately 1% of all human RVF cases are fatal. The pathological mechanisms that lead to these different outcomes are not clear.
RVF virus (RVFV) is listed as a category A priority pathogen by the NIH and an overlap select agent by the CDC and USDA because it is easily grown and infectious when aerosolized. No licensed vaccines or therapeutics currently exist for treating human RVFV infection. Licensure is possible only via the FDA's Animal Rule, which allows for animals to be used in place of human clinical efficacy trials when such trials are ethically or logistically impossible (16). The Animal Rule requires that the model be well characterized and relevant to the human disease, and the pathophysiological mechanisms must be similar to the human disease. Additional FDA guidance states that the route of infection must be the same as the expected route of exposure for humans (17). For biodefense, aerosol dispersion of a highly pathogenic agent is the most likely form of an attack on human populations (18).
While rodent models of RVF recapitulate human disease relatively well, nonhuman primate (NHP) models are desirable because they are phylogenetically closer to humans, and for many diseases, NHP are the most relevant model of the human disease. When RVFV was first discovered, a number of NHP species were evaluated as potential models, but most subsequent work has been done in rhesus macaques (13). Work from the late 1980s has shown that after intravenous (i.v.) inoculation with 5 logs of RVFV, 3 of 15 rhesus macaques developed hemorrhagic disease; the remaining animals were viremic but otherwise asymptomatic (19). In a subsequent report, 17 rhesus macaques inoculated i.v. with RVFV were found to be both viremic and febrile; 3 developed hemorrhagic complications, while another 7 had cutaneous petechial hemorrhages but survived (20). Five rhesus macaques exposed to aerosolized RVFV had detectable viremia and leucopenia, but only one of the five had a mild “transient elevation” in temperature (21). None of the rhesus macaques exposed to aerosolized RVFV succumbed to the infection.
Common marmosets have been more recently reported as a possible model of severe RVF (22). Half of the marmosets inoculated with RVFV by either subcutaneous (s.c.) or i.v. routes developed severe hepatic/hemorrhagic disease. All four marmosets infected by intranasal inoculation developed severe disease and succumbed due to encephalitis. This prior report did not establish the viral dose required to reproducibly cause disease in marmosets, nor did it address a true aerosol exposure. There is debate over whether intranasal inoculation mimics inhalation of a small-particle aerosol (18). As part of the process toward meeting the requirements of the FDA's Animal Rule, we have evaluated the disease outcome after aerosol exposure to increasing doses of RVFV in four NHP species that are commonly used in biomedical research.
MATERIALS AND METHODS
Biosafety and regulatory information.
All work with live RVFV was conducted at biosafety level 3 (BSL3) in the University of Pittsburgh Regional Biocontainment Laboratory (RBL). For respiratory protection, all personnel wore powered air-purifying respirators (3M GVP-1 PAPR with an L-series bump cap) or used a class III biological safety cabinet. Vesphene II se (1:128 dilution; Steris Corporation, Erie, PA) was used to disinfect all liquid wastes and surfaces associated with the agent. All solid wastes, used caging, and animal wastes were steam sterilized. Animal carcasses were digested via alkaline hydrolysis (Peerless Waste Solutions, Holland, MI). The University of Pittsburgh Regional Biocontainment Laboratory is a registered entity with the CDC/USDA for work with Rift Valley fever.
Nonhuman primates.
Healthy, adult cynomolgus macaques (Macaca fascicularis), rhesus macaques (Macaca mulatta, of Chinese origin), African green monkeys (AGM) (Chlorocebus aethiops), and common marmosets (Callithrix jacchus) of both sexes were purchased and housed in the RBL at animal BSL3 (ABSL3) for the duration of these studies. Each NHP used in this study was surgically implanted with a telemetry device (Data Sciences International, St. Paul, MN) to monitor body temperature and activity. Baseline telemetry data were collected for 3 to 5 days before exposure to RVFV. NHP that were determined to be either comatose or moribund were euthanized promptly by intravenous (i.v.) injection of sodium pentobarbital; once death was verified, a necropsy was performed on each animal and tissue samples were collected for histological and virological analyses. Cerebrospinal fluid (CSF) samples were collected by spinal tap at necropsy. Research was conducted in compliance with the Animal Welfare Act and other federal statutes and regulations relating to animals. All research described herein adhered to the principles stated in the Guide for the Care and Use of Laboratory Animals. All research described herein adhered to the principles stated in the Public Health Services Policy on Humane Care and Use of Laboratory Animals. The research described herein was approved by the University of Pittsburgh's Institutional Animal Care & Use Committee. The facility where this research was conducted is fully accredited by the Association for Assessment and Accreditation of Laboratory Animal Care International (Rockville, MD).
Virus.
Recombinant RVFV strain ZH501 was kindly provided by B. Miller (CDC, Ft. Collins, CO) and S. Nichol (CDC, Atlanta, GA). Prior to receipt, the virus was generated from reverse genetics plasmids containing the wild-type ZH501 sequence, which was confirmed by sequencing. Virus was propagated on Vero E6 cells using standard methods. For virus quantitation, plaque assays were performed using standard methods.
Aerosol exposures.
Aerosol exposures were conducted as previously described inside a class III biological safety cabinet (23, 24). Briefly, the NHP were anesthetized by intramuscular (i.m.) injection of tiletamine-zolazepam (6 mg/kg of body weight) or ketamine (9 mg/kg for Old World species; 20 mg/kg for marmosets) and a plethysmograph was performed (Buxco Research Systems, Wilmington, NC). Macaques and AGM were exposed using a head-only chamber (Biaera Technologies, Hagerstown, MD), while marmosets were exposed using a rabbit nose-only exposure chamber (CH Technologies, Westwood, NJ) modified to accommodate marmosets. Aerosols were created by a 3-jet Collison nebulizer (BGI, Inc., Waltham, MA) controlled by the AeroMP exposure system (Biaera Technologies). Aerosol samples were collected in an all-glass impinger (AGI; Ace Glass, Vineland, NJ) to determine the presented dose as previously described (25).
H&E staining.
Hematoxylin and eosin (H&E) staining of sections was performed by University of Pittsburgh Research Histology Services. Sections were analyzed by a board-certified anatomic pathologist (T. Oury) and assessed for pathological injury.
Immunohistochemical staining.
Immunohistochemical staining was done as previously described (26). Briefly, the antibodies used were a rabbit anti-RVFV polyclonal antibody (IBT Bioservices catalog no. 04-0001) and an anti-rabbit biotinylated antibody (Vector BA-1100). A negative control was incubated at the same time with nonimmune rabbit IgG (Vector I-1000). Sections from non-virus-infected animals labeled with the anti-RVFV primary antibody were also used as negative controls. After primary and secondary antibody labeling, the slides were washed, incubated with Vectastain ABC Elite (Vector PK-6100), and developed with AEC chromogen (Vector SK-4200). Slides were rinsed in water and counterstained in Gill's hematoxylin (Vector H-3401).
ELISA.
Enzyme-linked immunosorbent assays (ELISA) were done using a previously established ELISA procedure for quantifying serum IgG against RVFV (27). Briefly, dilutions of NHP sera were incubated for 1 h at 37°C on Immulon 2-HB 96-well plates (Fisher Scientific, Pittsburgh, PA) coated with inactivated lysate from MP-12-infected cells. After plates were washed with PBS-Tween, secondary goat anti-monkey IgG-horseradish peroxidase (HRP) (KPL Inc., Gaithersburg, MD) was added to the plates and incubated for an additional hour at 37°C, after which the plates were washed again and ABTS substrate (KPL Inc.) was added for 30 min before the plate was read on a FLUOstar Omega plate reader (BMG Labtech, Offenburg, Germany).
Plaque reduction neutralizing titer (PRNT).
Twofold dilutions of heat-inactivated sera starting at 1:20 were mixed with equal volumes of medium containing 100 PFU of RVFV ZH-501 and incubated overnight at 4°C. The following day, six-well plates containing confluent monolayers of Vero E6 cells were incubated for 1 h at 37°C with the virus-antibody mixtures, after which a medium-agar overlay was added. Three days later, the cells were fixed with 37% formaldehyde, the agar overlay was removed, and crystal violet was added to visualize plaques.
Virology.
For titration of tissue samples, tissue pieces were homogenized in a 2× volume of Dulbecco's modified Eagle's medium (DMEM)-10% fetal bovine serum (FBS) using an Omni tissue homogenizer (Omni International), followed by a standard plaque assay of the homogenate.
Hematology.
Complete blood counts were determined using a VetScan HM2 (Abaxis, Union City, CA), while blood chemistries were determined using the VetScan VS2 (Abaxis).
Telemetry data analysis.
Acquisition and analysis of telemetry data were conducted as previously described (23, 28). Briefly, body temperature was recorded every 10 to 15 min using a DataQuest A.R.T. 4.0 system (Data Sciences International). Data collected before exposure were used to forecast predicted postexposure values using an autoregressive integrated moving average (ARIMA) model in NCSS software (Number Cruncher Statistical Systems, Kaysville, UT). Residual changes were determined by subtracting the predicted value from the actual value recorded for each point. Residual changes greater than three standard deviations were used to compute Rmax (maximum increase from predicted), fever duration (number of hours of significant temperature elevation), and fever-hours (sum of the significant temperature elevations).
Statistical analysis.
The median lethal dose for AGM and marmosets was determined using the staircase up-and-down method (29, 30). For graphing and statistical analyses of data, including analysis of variance (ANOVA) and t tests, Prism 6 (GraphPad, La Jolla, CA) software was used.
RESULTS
Aerosolized RVFV is lethal in AGM and marmosets but not macaques.
The goal of the study reported here was to determine whether lethal disease could be achieved in an NHP model of aerosol infection with RVFV. If lethality was achieved, the second goal was to evaluate the dose response to RVFV infection (i.e., approximate the 50% lethal dose [LD50]) to ensure that doses selected in future natural history or efficacy studies would be sufficient to cause reproducible lethal disease in controls. Based on these stated goals, the NHP used in the initial studies presented here were subjected to minimal manipulation during the course of the experiment in order to accurately determine the LD50 and clinical outcome without confounding effects that may occur when an animal is repeatedly sedated. Therefore, serial sampling was not done in these experiments and will be the subject of future work.
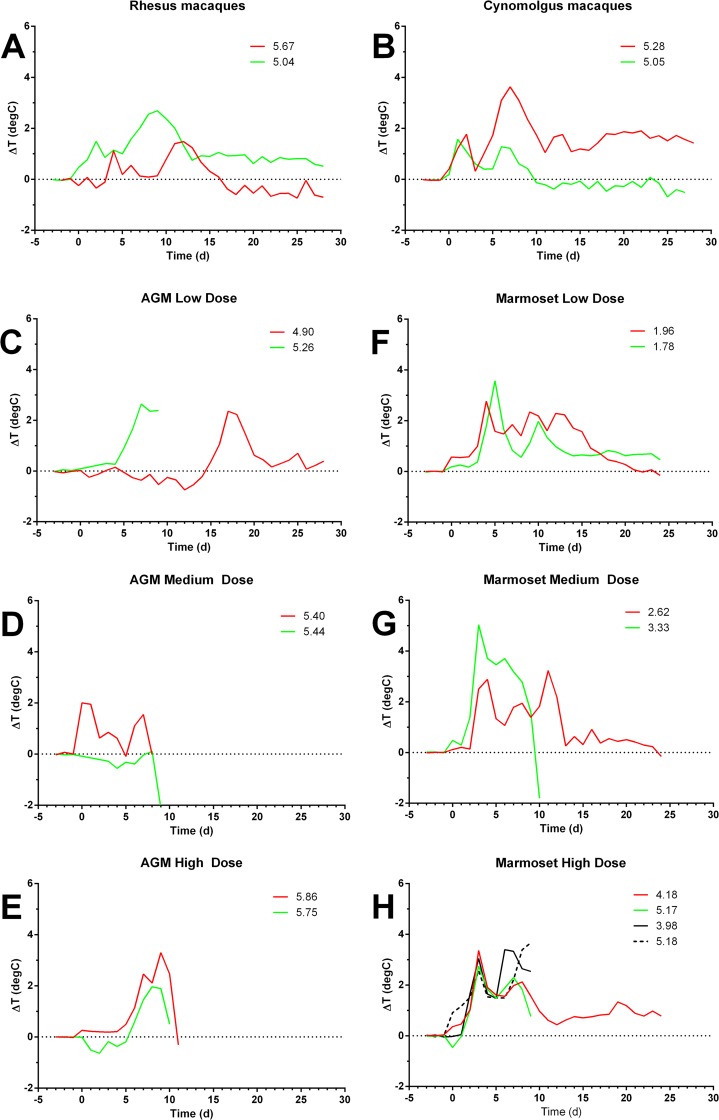
In all four NHP species evaluated, all NHP developed a fever after exposure to aerosolized RVFV (Fig. 1 and Table 1). The severity of fever (as determined by fever duration and fever-hours) was not dependent on the inhaled dose of RVFV in any of the four species. In both rhesus and cynomolgus macaques, a biphasic fever was seen (Fig. 1A and B), but no other clinical signs indicative of disease were noted. None of the macaques succumbed to disease, although for two of the macaques, body temperature remained elevated 30 days after infection.
FIG 1.
Fever response in NHP exposed to aerosolized RVFV. NHP of four different species were exposed to aerosolized RVFV and monitored by radiotelemetry to determine onset, duration, and severity of fever. Graphs show the residual temperature difference (actual temperature minus predicted temperature) for individual animals. The legend on each panel indicates the dose of virus that each NHP received. (A) Rhesus macaques; (B) cynomolgus macaques; (C to E) AGM; (F to H) marmosets.
TABLE 1.
Comparison of fever and antibody data from NHP exposed to aerosolized RVFV
| Speciesa | Age (yrs) | Weight (kg) | Genderb | Dose (log10 PFU)c | TTD (days)d | Fevere |
Serum antibody |
|||
|---|---|---|---|---|---|---|---|---|---|---|
| Rmax | Duration (h) | Fever-hours | SumODf | PRNT50g | ||||||
| Macaca fascicularis | 8 | 7.8 | M | 5.05 | 3.4 | 134.8 | 150.9 | 2.402 | >81,920 | |
| 9 | 7.2 | M | 5.28 | 4.9 | 646.5 | 1145.3 | 3.651 | >81,920 | ||
| Macaca mulatta | 6 | 9.3 | M | 5.04 | 4.1 | 482.3 | 711.5 | 1.857 | >81,920 | |
| 4 | 7.1 | M | 5.67 | 3.7 | 149.5 | 214.1 | 2.940 | >81,920 | ||
| Chlorocebus aethiops | 4 | 5.8 | M | 4.90 | 3.9 | 128.8 | 211.6 | 3.665 | >81,920 | |
| 8 | 4.8 | F | 5.26 | 10 | 4.7 | 119.3 | 242.3 | 0.178 | 10,240 | |
| 4 | 5.6 | M | 5.40 | 11 | 3.2 | 114.0 | 184.8 | 0.147 | 5,120 | |
| 9 | 7.5 | M | 5.44 | 10 | 1.5 | 11.5 | 11.1 | −0.014 | 1,280 | |
| 8 | 3.81 | F | 5.75 | 11 | 3.6 | 86.5 | 149.3 | 0.248 | >81,920 | |
| 8 | 4.78 | F | 5.86 | 11 | 4.2 | 151.0 | 282.6 | 0.245 | >81,920 | |
| Callithrix jacchus | 2 | 0.28 | M | 1.78 | 4.4 | 392.8 | 470.9 | 1.607 | >81,920 | |
| 2 | 0.44 | M | 1.96 | 4.4 | 399.8 | 592.6 | 1.645 | >81,920 | ||
| 2 | 0.38 | M | 2.62 | 4.8 | 341.5 | 538.9 | 1.418 | >81,920 | ||
| 2 | 0.41 | M | 3.33 | 10 | 6.3 | 192.8 | 527.2 | 0.011 | ND | |
| 2 | 0.36 | M | 3.98 | 10 | 4.8 | 170.0 | 429.2 | 0.185 | >81,920 | |
| 2 | 0.40 | M | 4.18 | 4.9 | 422.5 | 574.3 | 1.394 | >81,920 | ||
| 2 | 0.22 | M | 5.17 | 9 | 3.4 | 161.5 | 287.6 | 0.026 | >81,920 | |
| 2 | 0.39 | M | 5.18 | 10 | 4.1 | 140.5 | 219.1 | 0.020 | 40,960 | |
Macaca fascicularis, cynomolgus macaques; Macaca mulatta, rhesus macaques; Chlorocebus aethiops, AGM; Callithrix jacchus, marmosets.
M, male; F, female.
Dose, log10 PFU inhaled.
TTD, time to death or euthanasia when moribund.
Fever, the maximum difference between actual and predicted body temperature in °C (Rmax), the number of hours NHP displayed significant temperature elevations (duration), and the sum of the significant differences between actual and predicted body temperature (fever-hours).
SumOD, sum of the absorbance values, corrected for negative controls.
PRNT50, reciprocal dilution of sera that gave a 50% reduction in plaques; ND, not determined.
Fatal encephalitis in AGM after aerosol exposure to RVFV.
Six AGM were exposed to increasing doses of aerosolized RVFV; fever responses are shown in Fig. 1, with AGM arbitrarily grouped in twos as “low,” “medium,” or “high” based on the inhaled dose delivered to each AGM. All six AGM developed a fever, and five of the six AGM succumbed to the disease by 10 to 11 days postinfection (Fig. 1C to E). The sole AGM survivor was exposed to the lowest dose evaluated (4.9 log10 PFU). Fever onset was later in the survivor (day 16) than in the other AGM exposed to aerosolized RVFV. Unlike what was seen in the macaques, the fever in AGM was predominantly a single phase; the lone exception had a bacterial infection at the telemetry implant site and developed a fever concurrent with the exposure to RVFV (Fig. 1D). In addition to fever, the 5 AGM that developed severe disease showed signs of dehydration and anorexia. Clinical signs indicative of neurological disease were also evident, particularly excessive drooling, that began around day 9 (Table 2). All AGM that developed neurological disease were moribund on day 10 or 11 postexposure and were subsequently euthanized. Using the staircase method, the LD50 of RVFV in AGM was determined to be 1.17 × 105 PFU.
TABLE 2.
Clinical findings in NHP that succumbed after exposure to aerosolized RVFV
| Clinical sign | No. with clinical sign/total no. |
|
|---|---|---|
| AGM | Marmoset | |
| Biphasic fever | 1/5 | 4/4 |
| Anorexia | 5/5 | 4/4 |
| Dehydration | 5/5 | 1/4 |
| Vomiting | 0/3 | 1/4 |
| Drooling | 5/5 | 0/4 |
| Ataxia | 2/3 | 2/4 |
| Horizontal nystagmus | 1/3 | 0/4 |
| Head-pressing | 1/3 | 0/4 |
| Tremors | 0/3 | 1/4 |
| Shallow breathing | 3/5 | 1/4 |
| Blood in urine | 0/5 | 1/4 |
| Foaming at mouth | 0/5 | 1/4 |
| Seizures | 1/5 | 4/4 |
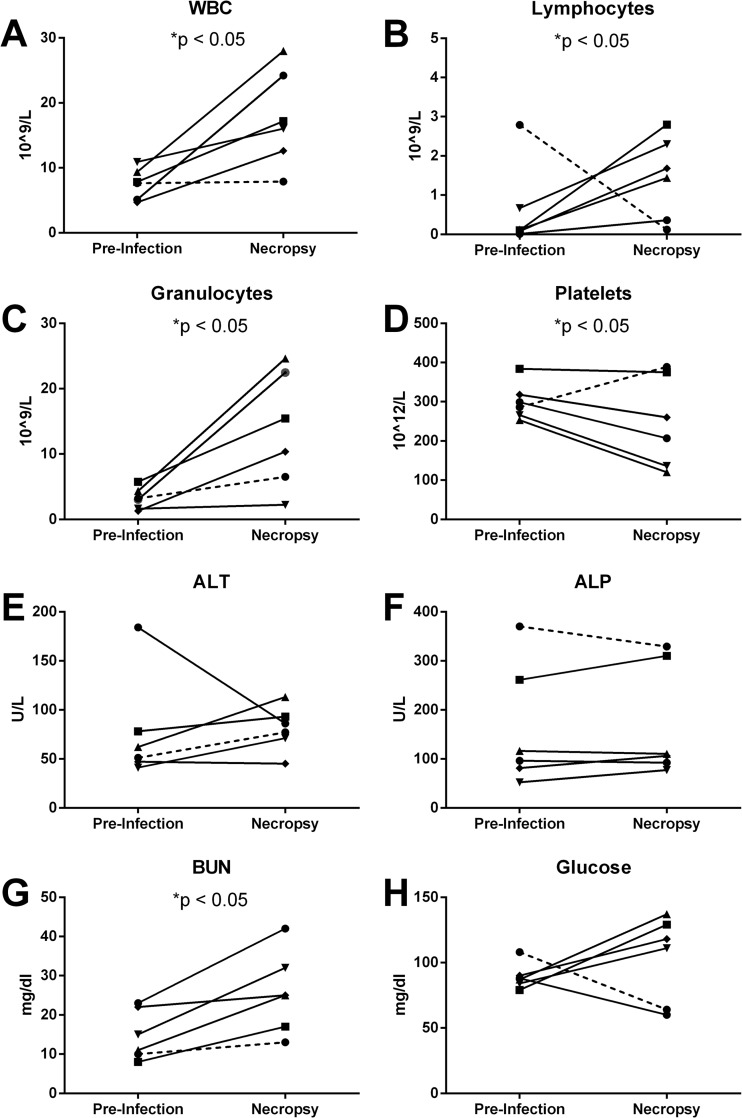
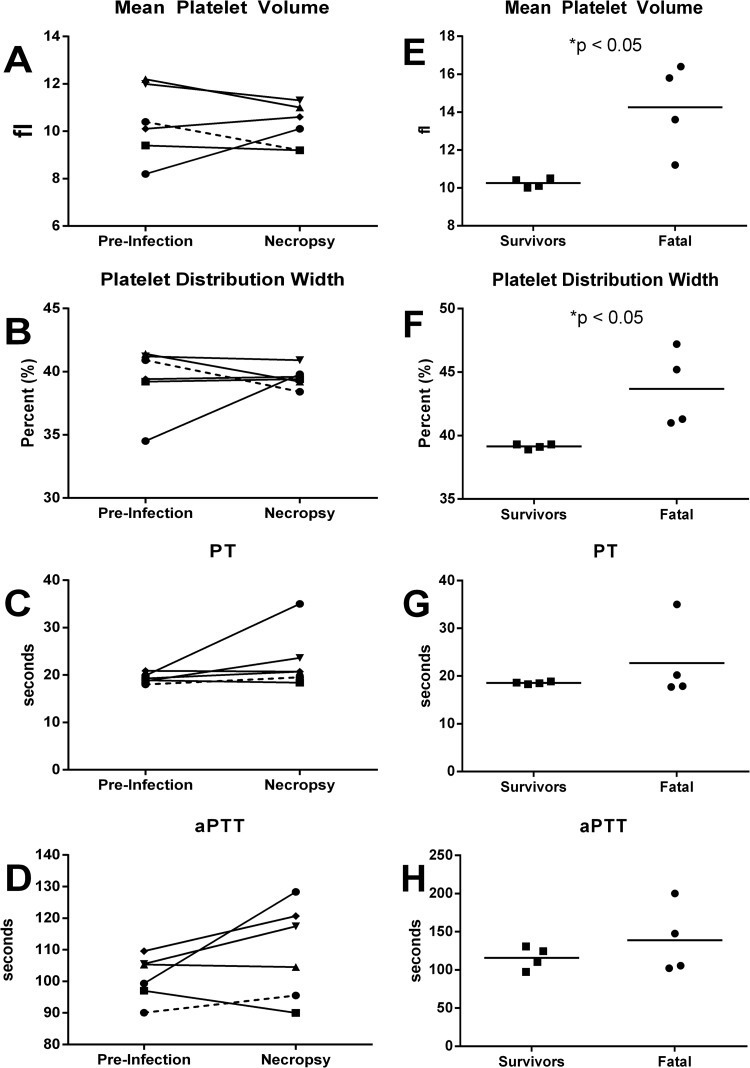
AGM were bled prior to exposure and at the time of euthanasia for evaluation of changes in complete blood count (CBC) and blood chemistry. AGM that succumbed to the infection had a pronounced leukophilia comprised of both lymphocytes and granulocytes (Fig. 2A to C). Platelet counts dropped in four of the five AGM that succumbed, and in three of those four, the levels were below 200, a level considered indicative of thrombosis in humans. However, mean platelet volume (MPV) and platelet distribution width (PDW) were not substantially altered (Fig. 3A and B). Coagulation times were elevated in some of the AGM that succumbed to infection, although overall the increase was not significant (Fig. 3C and D). No significant changes were seen in alanine aminotransferase (ALT) or alkaline phosphatase (ALP) levels, while blood urea nitrogen (BUN) was significantly elevated in four of the five AGM (Fig. 2E to G). Glucose levels were also increased in AGM that developed severe disease, although the difference did not rise to the level of significance (Fig. 2G).
FIG 2.
Hematological changes in AGM after infection with RVFV. Blood samples were collected prior to challenge (baseline) and at necropsy for AGM exposed to aerosolized RVFV. Graphs show the results of CBC and serum chemistry analyses for AGM that survived RVF exposure (dashed line) and AGM that succumbed (solid lines). (A) White blood cells (WBC); (B) lymphocytes; (C) granulocytes; (D) platelets; (E) alanine transaminase (ALT); (F) alkaline phosphatase (ALP); (G) blood urea nitrogen (BUN); (H) glucose.
FIG 3.
Platelet and coagulation changes after infection with RVFV. Blood samples collected from AGM (A to D) and marmosets (E to H) were analyzed for changes in platelets and coagulation parameters. Graphs for AGM show differences between preinfection and at necropsy for the AGM that survived infection (dashed line) compared to AGM that succumbed (solid lines). Graphs for marmosets show differences between marmosets that survived or succumbed to infection at the time of necropsy.
Fatal encephalitis in marmosets after aerosol exposure to RVFV.
A prior report had found that intranasal inoculation of common marmosets with RVFV resulted in the development of fatal encephalitis (22). Because intranasal inoculation is not accepted as a surrogate of aerosol exposure (17) and because the prior studies made no report of any attempt to determine the dose to RVFV, marmosets were subsequently evaluated to determine whether aerosol exposure also resulted in fatal RVFV infection and the dose required to cause disease. Eight marmosets were exposed to increasing doses of aerosolized RVFV (ranging from 1.78 log10 PFU to 5.18 log10 PFU/animal), and all eight developed a fever after exposure. Four of the eight marmosets ultimately succumbed to the disease and were euthanized between 9 and 10 days after infection. The fever was biphasic in marmosets, with an initial peak between days 3 and 6 and a second peak between days 7 and 15. Marmosets developed other clinical signs indicative of disease, including dehydration and anorexia. Late in the course of infection, neurological signs were noted, including stumbling off the perch, instability, and seizures (Table 2). The four marmosets that succumbed lost between 6.7 and 20.3% of their body weight (average, 12.78%) by the time of euthanasia, while surviving marmosets lost 0 to 4.37% (average, 1.09%) after infection and had gained 5 to 15% of body weight by day 28 postinfection (data not shown). The differences in weight loss were statistically significant as determined by a two-tailed t test with Welch's correction (P = 0.0216). By the staircase method, the LD50 of aerosolized RVFV in marmosets was determined to be 3.5 × 103 PFU.
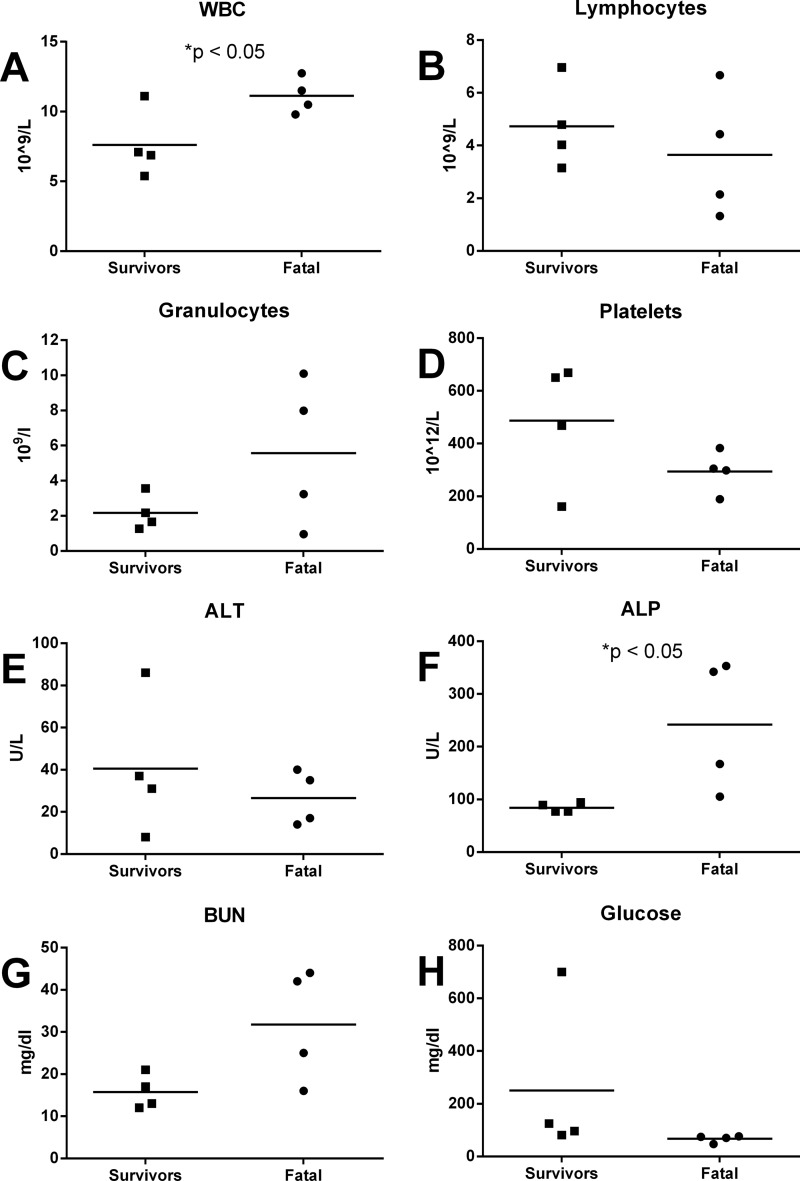
Because of the small size of an adult marmoset (300 to 500 g), it is more difficult to draw repeatedly the blood volumes needed for CBC, chemistries, virology, and serology. Therefore, baseline blood samples were not taken from the marmosets prior to infection with RVFV. CBC and chemistry values were compared between surviving (n = 4) and fatal (n = 4) infections in the marmosets exposed to RVFV. White cell counts were significantly elevated in marmosets that succumbed to infection; this elevation was due primarily to granulocytes and not lymphocytes, although not all marmosets that succumbed had elevated granulocyte counts (Fig. 4A to C). Platelet counts were lower in marmosets that died, although only one dropped below 200 (Fig. 4D). Both MPV and PDW were significantly increased in marmosets that developed severe disease, suggesting replacement with younger platelets (Fig. 3E and F). Coagulation times were only slightly elevated (Fig. 3G and H). Blood chemistries showed no change in ALT levels, but there was a significant elevation of ALP in the marmosets that died (Fig. 4E and F). BUN levels were also elevated in marmosets that succumbed (Fig. 4G). In contrast to the AGM, glucose levels were slightly decreased in marmosets that succumbed (Fig. 4H).
FIG 4.
Hematological changes in marmosets after infection with RVFV. Blood samples were collected at necropsy for marmosets exposed to aerosolized RVFV. Graphs show the results of CBC and serum chemistry analyses for individual marmosets that survived RVF exposure and marmosets that succumbed (symbols), with the averages (horizontal lines) for each group. (A) White blood cells (WBC); (B) lymphocytes; (C) granulocytes; (D) platelets; (E) alanine transaminase (ALT); (F) alkaline phosphatase (ALP); (G) blood urea nitrogen (BUN); (H) glucose.
Immune response in NHP to aerosol RVFV infection.
Prior to infection, none of the NHP had detectable serum antibody to RVFV (data not shown). All surviving NHP of all species had very high titers of serum antibody as measured by both ELISA and PRNT50 (Table 1). Among marmosets and AGM that succumbed, PRNT50 levels were generally strong (≥1,280); however, serum IgG levels against RVFV as measured by ELISA were lower in NHP that succumbed compared to those of survivors (average sum of absorbance values [sumOD], 0.147 and 1.857, respectively, compared across all four species). Those differences were statistically significant by the Mann-Whitney test (P < 0.001).
Pathological changes in the central nervous system of AGM and marmosets infected with aerosolized RVFV.
Tissues were taken at necropsy for assessment of viral load and pathological changes associated with RVF virus infection in all of the exposed NHP. Virus was not found in any tissue examined (see Table 3 for the list of tissues) from any of the NHP that survived aerosol exposure to RVF virus (data not shown). In both AGM and marmosets that succumbed, high levels of RVF virus were found in the brain and spinal cord. The average amount of virus in the brain was 1.5 log10 higher in marmosets than in AGM, although the importance of this difference is not clear (Table 3). Despite the high levels of virus in the brain and spinal cord, no virus was detected in the CSF of either AGM or marmosets. Virus was also detected in the eye of both AGM and marmosets, although not every animal was positive and levels were variable. In AGM, virus was undetectable in most peripheral tissues, including liver, lung, and kidney, with the exception of 2 AGM that had detectable levels of virus in the spleen. In marmosets, by contrast, virus was more widespread in peripheral tissues such as kidney, liver, and lung in addition to the spleen, although the levels were variable, and not every animal had virus in each tissue.
TABLE 3.
Viral load in tissues from NHP that succumbed after exposure to aerosolized RVFVa
| Tissue | AGM |
Marmoset |
||||
|---|---|---|---|---|---|---|
| Avg | Range | No. | Avg | Range | No. | |
| Brain | 6.89 | 6.19–7.27 | 5/5 | 8.17 | 6.21–8.50 | 4/4 |
| CSF | BLD | 0/5 | BLD | 0/4 | ||
| Eye | 4.09 | 2.65–4.55 | 3/5 | 4.80 | 2.15–5.24 | 3/4 |
| Kidney | BLD | 0/5 | 6.68 | 4.52–6.98 | 2/4 | |
| Liver | BLD | 0/5 | 5.41 | 5.41 | 1/4 | |
| Lung | BLD | 0/5 | 4.21 | 3.18–4.49 | 2/4 | |
| Sciatic nerve | BLD | 0/5 | 3.72 | 3.72 | 1/4 | |
| Serum | BLD | 0/5 | BLD | 0/4 | ||
| Spinal cord | 6.73 | 5.37–7.24 | 5/5 | 5.97 | 3.30–6.44 | 3/4 |
| Spleen | 3.58 | 2.18–3.88 | 2/5 | 3.31 | 2.18–3.72 | 3/4 |
Avg and range, log10 PFU/g of tissue; no., number of animals that succumbed out of total; BLD, below limit of detection.
Histologic analysis of tissues from AGM that succumbed showed pathological changes that were largely limited to the brain. The primary pathology in the brain was a lymphohistiocytic meningitis (Fig. 5A) and perivascular lymphocytic inflammation (Fig. 5B). There were occasional findings of increased karyorrhectic neurons with classic fragmented pyknotic nuclei and hypereosinophilic cytoplasm consistent with apoptotic neurons in various regions of the brain (Fig. 5C). There was essentially no inflammatory response to the apoptotic cells in the brain parenchyma with the exception of rare lymphocytes around apoptotic cells. Immunochemical localization of RVFV demonstrated viral infection of neurons in many regions of the brain (Fig. 5D). This was most often observed in the hippocampus, forebrain, basal ganglia, and midbrain but was also seen in the occipital lobe of one monkey and deep cerebellar nuclei of one monkey. No virus was seen in the lymphocytes and histiocytes associated with the meningitis and blood vessels. The liver showed essentially normal histology with rare apoptotic cells. One monkey had a large central hemorrhagic cyst that did not seem to be related to virus pathology. Lung tissue was also normal with the exception that one lung showing marked pulmonary edema (data not shown). No virus was seen by immunochemistry in any of the livers or lungs.
FIG 5.
Representative histologic images from AGM infected with RVFV. Virus-infected brain showing lymphocytic meningitis (A) and perivascular lymphocytic inflammation (B); (C) virus-infected brain showing karyorrhectic neuron with fragmented pyknotic fragmented nucleus and hypereosinophilic cytoplasm consistent with apoptosis with no inflammatory reaction; (D) virus-infected brain demonstrating RVFV-infected neurons in the hippocampus.
In the marmosets, no abnormal pathology was noted in marmosets that survived. Similar to AGM, histologic analysis of tissues from marmosets that succumbed showed pathological changes that were largely limited to the brain. The primary pathology in the brain was a lymphohistiocytic meningitis (Fig. 6B) and perivascular lymphocytic inflammation (Fig. 6D) with occasional findings of increased karyorrhectic neurons with classic fragmented pyknotic nuclei and hypereosinophilic cytoplasm consistent with apoptotic neurons in various regions of the brain. There was no inflammatory response to the apoptotic cells in the brain parenchyma. Immunochemical localization of RVFV demonstrated viral infection of neurons in many regions of the brain (Fig. 6F and G). This was most often observed in the hippocampus and midbrain but was also seen in the basal ganglia of two monkeys and the occipital lobe of one monkey. No virus was seen in the cerebellum. No virus was seen in the lymphocytes and histiocytes associated with the meningitis and the blood vessels. The liver showed essentially normal histology with rare apoptotic cells, and two livers showed marked steatosis that does not seem to be related to virus, as these were monkeys that received very low doses of virus (91 PFU and 417 PFU, respectively). Lung tissue was also normal, with the exception of one lung showing marked pulmonary edema (data not shown). No virus was seen by immunochemistry in any of the livers or lungs.
FIG 6.
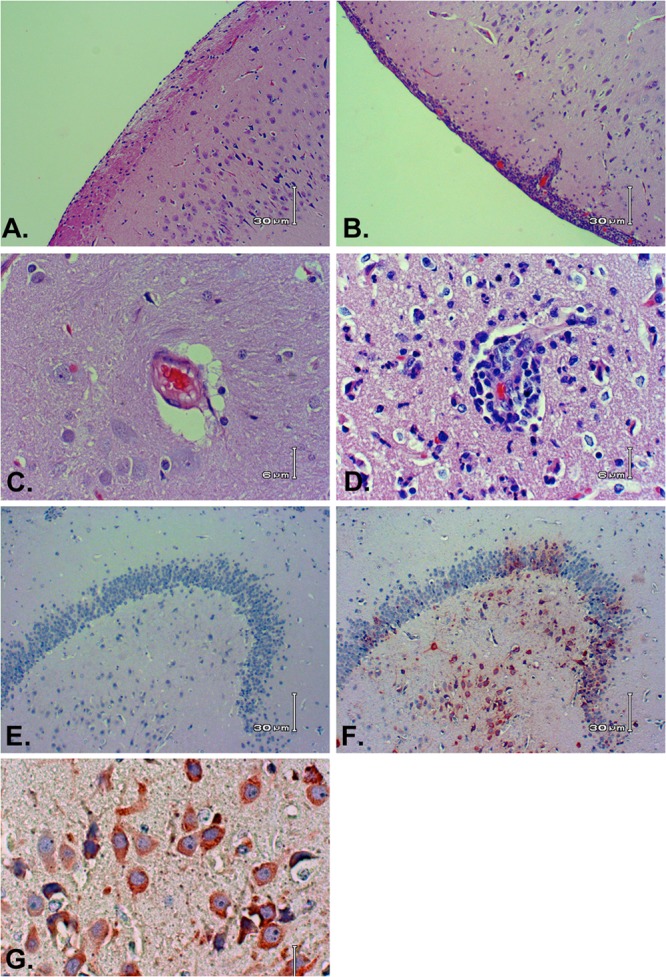
Representative histologic images from marmosets infected with RVFV. Virus-infected brain showing normal meninges (A) compared to lymphocytic meningitis (B); virus-infected brain showing a normal blood vessel (C) compared to a vessel with perivascular lymphocytic inflammation (D); (E) virus-infected brain stained with nonimmune IgG (negative control); (F) same virus-infected brain showing RVFV immunostaining in neurons in the hippocampus; (G) RVFV-infected neurons at higher magnification.
DISCUSSION
Evaluation of medical countermeasures for aerosol exposure to RVFV will necessitate relevant animal models of the human disease that meet the requirements of the FDA's Animal Rule (16). Among the requirements of the rule, the pathophysiological mechanisms resulting in disease must be understood and the route of exposure must be the same as the expected route of exposure for humans. With RVF, humans experience a spectrum of disease; while most develop an acute febrile disease and recover, a small percentage develop severe hepatic disease with hemorrhagic complications or severe encephalitis. Humans contract RVF by mosquitoes carrying the virus and by direct contact with infected animals or inhalation of aerosolized virus (13, 22, 31). It is unclear which transmission route is predominant in natural outbreaks and whether the route of exposure alters the virulence or pathophysiology of RVF. Because RVFV can be infectious when aerosolized, RVFV is considered a potential pathogen that could be used in a bioterror attack (18, 32, 33). Our prior studies in inbred rats illustrated that RVFV can be more virulent (as defined by a lower dose required to cause lethal disease and a shorter time to death) when inhaled than when injected subcutaneously (34). The current study sought to address the questions of whether RVFV is also more virulent in NHP when inhaled and whether a relevant, reproducible NHP model of severe RVF could be established for use in evaluation of potential vaccines and therapeutics.
Rhesus macaques have historically been the NHP species most often used in studying RVF (13). In prior reports with rhesus macaques, infection by a variety of routes produced fever, but only a small number of macaques succumbed with signs of hemorrhagic disease. There are no prior reports of encephalitis in rhesus macaques after RVFV infection, and no deaths have been reported in the few rhesus macaques that have been infected by aerosol (19, 21, 35–40). We also report no deaths after aerosol exposure of rhesus macaques to RVFV, although with the use of radiotelemetry monitoring, we were able to demonstrate a febrile response in these animals after aerosol exposure. The fever data along with serum antibody titers suggest viral replication did occur in the rhesus macaques and that development of fatal RVF disease is a rare outcome in this species. Similar results were seen in the cynomolgus macaques, which had not previously been evaluated for RVF by any route of infection. Both species of macaques may have potential for use as models of the nonlethal febrile disease seen in humans, but neither is useful as a reproducible model of severe RVF manifestations.
Marmosets have been previously shown to be a model of severe RVF (22). Marmosets inoculated with RVFV subcutaneously developed severe hepatic/hemorrhagic disease, while marmosets inoculated intranasally developed fatal encephalitis. However, only a single dose of RVFV was evaluated, and intranasal inoculation is generally not considered an acceptable substitute for aerosol exposure to a pathogen in pivotal efficacy studies (18, 25). Our findings reported here demonstrate that even at the lowest dose tested, 60 PFU, aerosol exposure to RVFV resulted in disease in marmosets as indicated by the febrile response and serum antibody responses after infection, although the LD50 was 2 logs higher at 3.5 × 103. Encephalitis was seen only at higher doses and in marmosets that succumbed to infection. Similar hematological changes were seen to what was reported previously for intranasal inoculation (elevations in ALP and BUN and white blood cell counts); however, we also found a decline in platelet counts and a shift in size, indicating turnover of platelets, which are findings suggestive of the development of thrombosis.
Surprisingly, similar results were seen in the AGM exposed to aerosolized RVFV. Subcutaneous inoculation of AGM with high doses of RVFV failed to induce any notable clinical signs of disease, and none of the AGM succumbed to RVFV by that route of inoculation (D. Smith, personal communication). In our experiments, all six AGM exposed to aerosolized RVFV developed a febrile response, and five of the six succumbed to the infection, all with neurological signs indicative of encephalitis. From this small set of AGM, the LD50 was estimated to be 1.7 × 105 PFU, almost two logs higher than was seen in the marmosets. Similar to the marmosets, elevations in white blood cells and BUN levels were seen in AGM that succumbed to infection as well as a more pronounced decrease in platelet counts. Unlike marmosets, little or no change was seen in ALT or ALP, while glucose levels were increased in four of the five AGM that succumbed.
It is curious that all of the marmosets and AGM that succumbed had good serum neutralizing antibody titers as measured by PRNT50 but poor serum IgG levels as measured by ELISA. This was not an issue with cross-reactivity of the secondary antibody in the ELISA, as strong IgG titers were detected in surviving marmosets and AGM. One possible explanation is that although neutralizing antibody is generated, the overall affinity of IgG for RVFV is weak in animals that succumbed. Alternatively, other antibody isotypes, such as IgM, may comprise the antibody response in NHP that succumbed. This failure to generate high-affinity neutralizing IgG responses suggests a suppressed or misdirected humoral response to the infection. It is also intriguing that in both marmosets and AGM that succumbed, the leukocytosis that was seen in the blood consisted predominantly of granulocytes; neutrophils are not thought to be typically noted in responses to viral pathogens, although an increase in granulocytes has been seen previously with other encephalitic viral diseases (41, 42). Future experiments will evaluate the immunological responses in AGM and marmosets infected with RVFV.
The outcomes reported here in NHP, combined with our prior evaluation of aerosol RVFV infection in rats (34), suggest that inhalation of RVFV results in more severe disease than peripheral inoculation, and the disease after aerosol exposure is more likely to be encephalitis rather than hepatic or hemorrhagic disease. Surprisingly, two species found to be highly resistant to parenteral inoculation with RVFV (the Lewis strain of rat and AGM) developed encephalitis and succumbed after exposure to aerosolized RVFV. While one should be cautious in extrapolating this to humans, these data do suggest that the route of exposure alters the pathogenesis and virulence of RVFV and that RVFV is more virulent when inhaled than by other routes of inoculation. If true, RVF as a bioterror threat may be more of a concern than is currently appreciated.
Both AGM and marmosets represent reproducible models of lethal encephalitis resulting from aerosol exposure to RVFV that can serve as tools for evaluating potential vaccines and antiviral compounds. Although differences were noted in the LD50, clinical signs, and hematological and pathological changes seen in terminal infection, overwhelmingly the disease course and outcome were surprisingly similar between AGM and marmosets. It is not possible from these initial studies to decide whether marmosets or AGM are the more relevant animal model of human RVF. This is in large part due to the paucity of human RVF data, particularly for documented aerosol infection. Using the data presented here as a foundation, longitudinal sampling during additional studies in both AGM and marmosets will provide a more detailed examination of the pathophysiological changes that occur after RVFV infection in both species of NHP.
ACKNOWLEDGMENTS
This work was supported by the U.S. Department of Defense Joint Project Manager Medical Countermeasure Systems (JPM-MCS) program through the Defense Threat Reduction Agency (DTRA) contract HDTRA1-10-C-1066. The views expressed here are those of the authors and do not necessarily represent the views or official position of JPM-MCS. JPM-MCS, a component of the Joint Program Executive Office for Chemical and Biological Defense, aims to provide U.S. military forces and the nation with safe, effective, and innovative medical solutions to counter chemical, biological, radiological, and nuclear threats. JPM-MCS facilitates the advanced development and acquisition of medical countermeasures and systems to enhance our nation's biodefense response capability. For more information, visit www.jpeocbd.osd.mil.
We thank the Division of Laboratory Animal Resource's veterinary technicians who work in the University of Pittsburgh's Regional Biocontainment Laboratory and assisted with these studies. We also thank Stuart Nichol (CDC, Atlanta, GA) for kindly providing the recombinant ZH501 strain of RVFV for use in these studies.
REFERENCES
- 1.Ayari-Fakhfakh E, Ghram A, Bouattour A, Larbi I, Gribaa-Dridi L, Kwiatek O, Bouloy M, Libeau G, Albina E, Cetre-Sossah C. 2011. First serological investigation of peste-des-petits-ruminants and Rift Valley fever in Tunisia. Vet. J. 187:402–404. 10.1016/j.tvjl.2010.01.007 [DOI] [PubMed] [Google Scholar]
- 2.Bird BH, Githinji JW, Macharia JM, Kasiiti JL, Muriithi RM, Gacheru SG, Musaa JO, Towner JS, Reeder SA, Oliver JB, Stevens TL, Erickson BR, Morgan LT, Khristova ML, Hartman AL, Comer JA, Rollin PE, Ksiazek TG, Nichol ST. 2008. Multiple virus lineages sharing recent common ancestry were associated with a large Rift Valley fever outbreak among livestock in Kenya during 2006–2007. J. Virol. 82:11152–11166. 10.1128/JVI.01519-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Davies FG, Linthicum KJ, James AD. 1985. Rainfall and epizootic Rift Valley fever. Bull. World Health Organ. 63:941–943 [PMC free article] [PubMed] [Google Scholar]
- 4.Hoogstraal H, Meegan JM, Khalil GM, Adham FK. 1979. The Rift Valley fever epizootic in Egypt 1977–78. 2. Ecological and entomological studies. Trans. R. Soc. Trop. Med. Hyg. 73:624–629. 10.1016/0035-9203(79)90005-1 [DOI] [PubMed] [Google Scholar]
- 5.Jost CC, Nzietchueng S, Kihu S, Bett B, Njogu G, Swai ES, Mariner JC. 2010. Epidemiological assessment of the Rift Valley fever outbreak in Kenya and Tanzania in 2006 and 2007. Am. J. Trop. Med. Hyg. 83:65–72. 10.4269/ajtmh.2010.09-0290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Madani TA, Al-Mazrou YY, Al-Jeffri MH, Mishkhas AA, Al-Rabeah AM, Turkistani AM, Al-Sayed MO, Abodahish AA, Khan AS, Ksiazek TG, Shobokshi O. 2003. Rift Valley fever epidemic in Saudi Arabia: epidemiological, clinical, and laboratory characteristics. Clin. Infect. Dis. 37:1084–1092. 10.1086/378747 [DOI] [PubMed] [Google Scholar]
- 7.Meegan JM, Hoogstraal H, Moussa MI. 1979. An epizootic of Rift Valley fever in Egypt in 1977. Vet. Rec. 105:124–125. 10.1136/vr.105.6.124 [DOI] [PubMed] [Google Scholar]
- 8.Mohamed M, Mosha F, Mghamba J, Zaki SR, Shieh WJ, Paweska J, Omulo S, Gikundi S, Mmbuji P, Bloland P, Zeidner N, Kalinga R, Breiman RF, Njenga MK. 2010. Epidemiologic and clinical aspects of a Rift Valley fever outbreak in humans in Tanzania, 2007. Am. J. Trop. Med. Hyg. 83:22–27. 10.4269/ajtmh.2010.09-0318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shieh WJ, Paddock CD, Lederman E, Rao CY, Gould LH, Mohamed M, Mosha F, Mghamba J, Bloland P, Njenga MK, Mutonga D, Samuel AA, Guarner J, Breiman RF, Zaki SR. 2010. Pathologic studies on suspect animal and human cases of Rift Valley fever from an outbreak in Eastern Africa, 2006–2007. Am. J. Trop. Med. Hyg. 83:38–42. 10.4269/ajtmh.2010.09-0463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wilson ML, Chapman LE, Hall DB, Dykstra EA, Ba K, Zeller HG, Traore-Lamizana M, Hervy JP, Linthicum KJ, Peters CJ. 1994. Rift Valley fever in rural northern Senegal: human risk factors and potential vectors. Am. J. Trop. Med. Hyg. 50:663–675 [DOI] [PubMed] [Google Scholar]
- 11.Bird BH, Nichol ST. 2012. Breaking the chain: Rift Valley fever virus control via livestock vaccination. Curr. Opin. Virol. 2:315–323. 10.1016/j.coviro.2012.02.017 [DOI] [PubMed] [Google Scholar]
- 12.Ikegami T, Makino S. 2011. The pathogenesis of Rift Valley fever. Viruses 3:493–519. 10.3390/v3050493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ross TM, Bhardwaj N, Bissel SJ, Hartman AL, Smith DR. 2012. Animal models of Rift Valley fever virus infection. Virus Res. 163:417–423. 10.1016/j.virusres.2011.10.023 [DOI] [PubMed] [Google Scholar]
- 14.Shimshony A, Barzilai R. 1983. Rift Valley fever. Adv. Vet. Sci. Comp. Med. 27:347–425 [PubMed] [Google Scholar]
- 15.Turell MJ, Rossi CA. 1991. Potential for mosquito transmission of attenuated strains of Rift Valley fever virus. Am. J. Trop. Med. Hyg. 44:278–282 [DOI] [PubMed] [Google Scholar]
- 16.FDA 2002. New drug and biological drug products; evidence needed to demonstrate effectiveness of new drugs when human efficacy studies are not ethical or feasible. Final rule. Fed. Regist. 67:37988–37998 [PubMed] [Google Scholar]
- 17.FDA 2009, posting date Guidance for industry: animal models—essential elements to address efficacy under the animal rule. Food and Drug Administration, Washington, DC: http://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/ucm078923.pdf. FDA [Google Scholar]
- 18.Roy CJ, Reed DS, Hutt JA. 2010. Aerobiology and inhalation exposure to biological select agents and toxins. Vet. Pathol. 47:779–789. 10.1177/0300985810378650 [DOI] [PubMed] [Google Scholar]
- 19.Peters CJ, Jones D, Trotter R, Donaldson J, White J, Stephen E, Slone TW., Jr 1988. Experimental Rift Valley fever in rhesus macaques. Arch. Virol. 99:31–44. 10.1007/BF01311021 [DOI] [PubMed] [Google Scholar]
- 20.Morrill JC, Jennings GB, Johnson AJ, Cosgriff TM, Gibbs PH, Peters CJ. 1990. Pathogenesis of Rift Valley fever in rhesus monkeys: role of interferon response. Arch. Virol. 110:195–212. 10.1007/BF01311288 [DOI] [PubMed] [Google Scholar]
- 21.Morrill JC, Peters CJ. 2011. Protection of MP-12-vaccinated rhesus macaques against parenteral and aerosol challenge with virulent Rift Valley fever virus. J. Infect. Dis. 204:229–236. 10.1093/infdis/jir249 [DOI] [PubMed] [Google Scholar]
- 22.Smith DR, Bird BH, Lewis B, Johnston SC, McCarthy S, Keeney A, Botto M, Donnelly G, Shamblin J, Albarino CG, Nichol ST, Hensley LE. 2012. Development of a novel nonhuman primate model for Rift Valley fever. J. Virol. 86:2109–2120. 10.1128/JVI.06190-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Alves DA, Glynn AR, Steele KE, Lackemeyer MG, Garza NL, Buck JG, Mech C, Reed DS. 2010. Aerosol exposure to the Angola strain of Marburg virus causes lethal viral hemorrhagic fever in cynomolgus macaques. Vet. Pathol. 47:831–851. 10.1177/0300985810378597 [DOI] [PubMed] [Google Scholar]
- 24.Reed DS, Lind CM, Sullivan LJ, Pratt WD, Parker MD. 2004. Aerosol infection of cynomolgus macaques with enzootic strains of Venezuelan equine encephalitis viruses. J. Infect. Dis. 189:1013–1017. 10.1086/382281 [DOI] [PubMed] [Google Scholar]
- 25.Roy CJ, Pitt LM. 2005. Infectious disease aerobiology: aerosol challenge methods, p 61–76 In Swearengen JR. (ed), Biodefense: research methodology and animal models. CRC Press, Boca Raton, FL [Google Scholar]
- 26.Kliment CR, Oury TD. 2011. Extracellular superoxide dismutase protects cardiovascular syndecan-1 from oxidative shedding. Free Radic. Biol. Med. 50:1075–1080. 10.1016/j.freeradbiomed.2011.02.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bird BH, Albarino CG, Hartman AL, Erickson BR, Ksiazek TG, Nichol ST. 2008. Rift Valley fever virus lacking the NSs and NSm genes is highly attenuated, confers protective immunity from virulent virus challenge, and allows for differential identification of infected and vaccinated animals. J. Virol. 82:2681–2691. 10.1128/JVI.02501-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Reed DS, Lackemeyer MG, Garza NL, Sullivan LJ, Nichols DK. 2011. Aerosol exposure to Zaire ebolavirus in three nonhuman primate species: differences in disease course and clinical pathology. Microbes Infect. 13:930–936. 10.1016/j.micinf.2011.05.002 [DOI] [PubMed] [Google Scholar]
- 29.Dixon WJ. 1965. The up-and-down method for small samples. J. Am. Stat. Assoc. 60:967–978. 10.1080/01621459.1965.10480843 [DOI] [Google Scholar]
- 30.Rispin A, Farrar D, Margosches E, Gupta K, Stitzel K, Carr G, Greene M, Meyer W, McCall D. 2002. Alternative methods for the median lethal dose (LD(50)) test: the up-and-down procedure for acute oral toxicity. ILAR J. 43:233–243. 10.1093/ilar.43.4.233 [DOI] [PubMed] [Google Scholar]
- 31.Boshra H, Lorenzo G, Busquets N, Brun A. 2011. Rift Valley fever: recent insights into pathogenesis and prevention. J. Virol. 85:6098–6105. 10.1128/JVI.02641-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Brown JL, Dominik JW, Morrissey RL. 1981. Respiratory infectivity of a recently isolated Egyptian strain of Rift Valley fever virus. Infect. Immun. 33:848–853 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Miller WS, Demchak P, Rosenberger CR, Dominik JW, Bradshaw JL. 1963. Stability and infectivity of airborne Yellow fever and Rift Valley fever viruses. Am. J. Hyg. 77:114–121 [Google Scholar]
- 34.Bales JM, Powell DS, Bethel LM, Reed DS, Hartman AL. 2012. Choice of inbred rat strain impacts lethality and disease course after respiratory infection with Rift Valley fever virus. Front. Cell. Infect. Microbiol. 2:105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cosgriff TM, Morrill JC, Jennings GB, Hodgson LA, Slayter MV, Gibbs PH, Peters CJ. 1989. Hemostatic derangement produced by Rift Valley fever virus in rhesus monkeys. Rev. Infect. Dis. 11(Suppl 4):S807–S814 [DOI] [PubMed] [Google Scholar]
- 36.Morrill JC, Czarniecki CW, Peters CJ. 1991. Recombinant human interferon-gamma modulates Rift Valley fever virus infection in the rhesus monkey. J. Interferon Res. 11:297–304. 10.1089/jir.1991.11.297 [DOI] [PubMed] [Google Scholar]
- 37.Morrill JC, Jennings GB, Cosgriff TM, Gibbs PH, Peters CJ. 1989. Prevention of Rift Valley fever in rhesus monkeys with interferon-alpha. Rev. Infect. Dis. 11(Suppl 4):S815–S825 [DOI] [PubMed] [Google Scholar]
- 38.Morrill JC, Knauert FK, Ksiazek TG, Meegan JM, Peters CJ. 1989. Rift Valley fever infection of rhesus monkeys: implications for rapid diagnosis of human disease. Res. Virol. 140:139–146. 10.1016/S0923-2516(89)80091-3 [DOI] [PubMed] [Google Scholar]
- 39.Morrill JC, Peters CJ. 2011. Mucosal immunization of rhesus macaques with Rift Valley fever MP-12 vaccine. J. Infect. Dis. 204:617–625. 10.1093/infdis/jir354 [DOI] [PubMed] [Google Scholar]
- 40.Morrill JC, Peters CJ. 2003. Pathogenicity and neurovirulence of a mutagen-attenuated Rift Valley fever vaccine in rhesus monkeys. Vaccine 21:2994–3002. 10.1016/S0264-410X(03)00131-2 [DOI] [PubMed] [Google Scholar]
- 41.Reed DS, Lackemeyer MG, Garza NL, Norris S, Gamble S, Sullivan LJ, Lind CM, Raymond JL. 2007. Severe encephalitis in cynomolgus macaques exposed to aerosolized eastern equine encephalitis virus. J. Infect. Dis. 196:441–450. 10.1086/519391 [DOI] [PubMed] [Google Scholar]
- 42.Reed DS, Larsen T, Sullivan LJ, Lind CM, Lackemeyer MG, Pratt WD, Parker MD. 2005. Aerosol exposure to western equine encephalitis virus causes fever and encephalitis in cynomolgus macaques. J. Infect. Dis. 192:1173–1182. 10.1086/444397 [DOI] [PubMed] [Google Scholar]